Abstract
Ischemic stroke accounts for nearly 80% of stroke cases. Recanalization with thrombolysis is a currently crucial therapeutic strategy for re-building blood supply, but the thrombolytic therapy often companies with cerebral ischemia-reperfusion injury, which are mediated by free radicals. As an important component of free radicals, reactive nitrogen species (RNS), including nitric oxide (NO) and peroxynitrite (ONOO−), play important roles in the process of cerebral ischemia-reperfusion injury. Ischemia-reperfusion results in the production of nitric oxide (NO) and peroxynitrite (ONOO−) in ischemic brain, which trigger numerous molecular cascades and lead to disruption of the blood brain barrier and exacerbate brain damage. There are few therapeutic strategies available for saving ischemic brains and preventing the subsequent brain damage. Recent evidence suggests that RNS could be a therapeutic target for the treatment of cerebral ischemia-reperfusion injury. Herein, we reviewed the recent progress regarding the roles of RNS in the process of cerebral ischemic-reperfusion injury and discussed the potentials of drug development that target NO and ONOO− to treat ischemic stroke. We conclude that modulation for RNS level could be an important therapeutic strategy for preventing cerebral ischemia-reperfusion injury.
Keywords: stroke, cerebral ischemia-reperfusion injury, reactive nitrogen species, nitric oxide, peroxynitrite, drug discovery
Introduction
Stroke is the second leading cause of death and a leading cause of adult disability in human diseases1,2. The latest data indicate that approximately 7 000 000 Americans have suffered a stroke, incurring an annual cost of $40.9 billion3. Ischemic stroke accounts for nearly 80% cases of stroke patients. The process of ischemic stroke begins with blood flow cessation with energy depletion and follows serious pathological changes and brain damages through a series of molecular cascades after cerebral artery occlusion4. The most effective and essential treatment is to recover the blood supply by recanalization of the occluded arteries5,6. However, the recanalization treatment can also aggravate brain damage, referred to as “cerebral ischemia-reperfusion injury”, which has been discovered in patients who have experienced disastrous outcomes due to fatal edema or intracranial hemorrhage following thrombolysis7.
Cerebral ischemia-reperfusion injury can be defined as a deleterious, but salvageable, deterioration of an ischemic injury after reperfusion8. Free radicals are important cytotoxic molecules that play a role in the process of cerebral ischemia reperfusion injury. Two major classes of free radicals are the reactive oxygen species (ROS) and the reactive nitrogen species (RNS). ROS are comprised of active species including hydroxyl radical, superoxide, singlet oxygen, and hydrogen peroxide, etc. Under physiological conditions, ROS serve as redox signaling molecules and have important biological functions. For instance, ROS can enhance the protein kinase C-dependent excitatory postsynaptic potential9 and can inhibit the release of dopamine in the central nervous system10. However, ischemia and reperfusion insults induce the accumulation of excessive ROS, resulting in tissue oxidative damage in ischemic brains11,12. In recent decades, the roles of ROS in cerebral ischemia-reperfusion injury have been intensively investigated. For example, during ischemia-reperfusion injury, ROS accumulation can disrupt cellular signal transduction, activate inflammation factors, induce lipid peroxidations resulting in neural cell death, and contribute to the breakdown of the blood brain barrier (BBB) and enlargement of the infarction13. Antioxidant therapies, such as edaravone, NXY-059 and allopurinol, have been proposed to act as neuroprotective reagents for acute ischemic stroke patients with the potential to improve clinical outcomes14,15,16,17. However, the roles of RNS in cerebral ischemia-reperfusion injury and the potential values of RNS modulators in the treatment of stroke remain to be addressed. In this review, we have focused on the role of RNS, particularly nitric oxide (NO) and peroxynitrite (ONOO−), in cerebral ischemia-reperfusion injury. Subsequently, we have discussed the potential of RNS inhibitors and activators in drug development.
Roles of RNS in cerebral ischemia-reperfusion injury
NO and ONOO− are two common species of RNS that are well documented to be present in cerebral ischemia-reperfusion injury. The low concentration of NO that is produced by endothelial nitric oxide synthase (eNOS) has physiological functions, whereas the high concentration of NO produced from inducible NOS (iNOS) and neuronal NOS (nNOS) is detrimental to the ischemic brain. iNOS and nNOS can lead to inflammation, cell death, BBB hyperpermeability and infarction enlargement. During cerebral ischemia or cerebral ischemia-reperfusion injury, NO is produced simultaneously with superoxide (O2®·) and rapidly reacts with O2®· at a diffusion-limited rate to generate ONOO−. Peroxynitrite can easily permeate lipid bilayers, leading to peroxidation of membrane lipids18,19, mediating nitration of tyrosine residue, inhibiting tyrosine phosphorylation and thereby affecting cellular signal transduction. Peroxynitrite inactivates aconitase and superoxide dismutase (SOD), mediates NO-induced BBB damage20 and triggers apoptotic cell death21. Therefore, RNS are not only critical factors in cerebral ischemia-reperfusion injury but are also important drug targets for ischemic stroke treatment.
Role of NO in the cerebral ischemia-reperfusion injury
NO can be produced from both enzymatic and non-enzymatic pathways. NO can be derived from L-arginine through an enzymatic reaction catalyzed by NO synthases (NOS) and by the enzymatic reduction of available cellular nitrite pools through a diverse class of cytosolic and mitochondrial nitrite reductases. Nitrite is a major metabolic product of NO production and is found in all types of cells and tissues that utilize NO signaling processes22. In most cases, NO is enzymatically generated from the conversion of ℒ-arginine and oxygen by various forms of NOS, including nNOS (type 1), iNOS (type 2), and eNOS (type 3). eNOS and nNOS are calcium-dependent and generally produce nanomolar levels of NO, while iNOS is calcium-independent and produces micromolar levels of NO. iNOS is often activated at the transcriptional level by de novo synthesis in response to many stimulating agents23. The physiological concentration of NO (at levels less than 10 nmol/L) generated from eNOS is essential to neuronal communication, regulation of vascular tone, synaptic transmission, platelet aggregation and inflammatory responses24,25,26,27,28. However, high concentrations of NO generated from calcium-dependent nNOS activation and calcium-independent iNOS activation in macrophages and other cell types are detrimental to the ischemic brain29.
Using electron paramagnetic resonance (EPR) spin trapping techniques, two early studies directly demonstrated the production of NO in the brains of cerebral ischemic animal models30,31. Other studies that adopted different methods, such as porphyrinic microsensor and NO indicator, revealed similar results; NO was significantly induced in the early phase of ischemic stroke32,33. Using in vivo microdialysis to monitor stable NO metabolites (nitrite and nitrate), a previous study has shown a transient increase in NO by 50% for approximately 30 min after reperfusion34. At the early stage of ischemia, transient restriction of the blood supply leads to the increased activity of eNOS, which produces small amounts of NO and protects the brain vasculature35. Simultaneously, energy depletion induces the accumulation of glutamate and triggers the activation of calcium channels, which leads to NO production through nNOS stimulation36,37. At the reperfusion stage, the up-regulated expression of iNOS results in excessive NO formation, and the increased iNOS lasts for more than 7 d36,37. The vast NO production from iNOS and nNOS are neurotoxic. Using EPR spin trapping technology, we previously demonstrated a biphasic production of NO in a rat model of cerebral ischemia-reperfusion injury. The first phase of NO productions was after 1 h of ischemia, and the second phase was at 24 to 48 h of reperfusion after 1 h of ischemia. The first and second phases of NO production were correlated with increased nNOS and iNOS, respectively38.
The increased NO production in ischemic brain plays two roles: one in cell death and the other in BBB disruption. The small amount of NO produced from eNOS exerts neuroprotective effects, whereas the greater amount of NO produced from iNOS and nNOS is neurotoxic. The opposing roles of NO have been attested by both genetic and pharmacological approaches. For example, eNOS knockout mice had larger infarction volumes than those of wild-type mice after cerebral ischemia39, indicating the neuroprotective effects of the NO derived from eNOS. Similar results were obtained from the studies using statins or corticosteroids, which showed that these medications could increase eNOS activity and attenuate the brain damage in an experimental stroke animal model. The neuroprotective mechanisms of those medications include the elevation of cerebral blood flow, the reduction of thrombosis formation, the suppression of NMDA receptor activation, the improvement of inflammatory and oxidative status, and the enhancement of vasorelaxation29,39,40,41. A knockdown of either the iNOS or nNOS gene was found to have a neuroprotective effect in mice that underwent transient or permanent cerebral ischemia42,43. Similarly, selective NOS inhibitors, such as 1400W, BN80933, and ARL17477, revealed preventive effects against ischemic stroke44,45,46. The underlying mechanism of the NO neurotoxicity is primarily through its interaction with protein moieties, which leads to S-glutathiolation47, nitrosothiol formation48, or protein nitrosylation49. The formation of peroxynitrite is also an important neurotoxic mechanism of NO in cerebral ischemia-reperfusion injury50,51 that will be discussed in the next session.
In addition to the cell death, the blood-brain barrier breakdown is another important pathophysiological process in cerebral ischemia-reperfusion injury. The BBB consists of microvascular endothelial cells, astrocytic endfeet and the extracellular matrix (ECM). Tight junctions (TJs), consisting of junction adhesion molecule-1 (JAM-1), occludin and claudins52, in the layer of microvascular endothelial cells are the key elements of the BBB. The cytoplasmic domains of these proteins are anchored to the cytoskeleton through accessory proteins such as those classified in the zonula occludens (ZOs) family. Activation of the matrix metalloproteinases (MMPs) is one of the critical pathways in the BBB opening53,54,55,56. MMPs are a group of proteases with more than 20 members, among which are MMP-2, -3, and -9, the main forms found in the brain. During cerebral ischemia, the activation of MMP-2 was found at the first stage of the BBB opening56,57,58, whereas enhanced MMP-9 activity was related to the second stage59,60. Activated MMPs can hydrolyze the BBB extracellular matrix and TJ proteins and subsequently degrade the extracellular matrix around cerebral blood vessels and neurons. Hypoxia mediates the MMP-9-dependent TJ rearrangement and induces edema formation; thus, inhibition of MMP-9 could be an important therapeutic strategy for the treatment of brain edema61. A systematic review suggests that MMP-9 could be used not only as a drug target but also as a biomarker for monitoring brain damage and predicting hemorrhagic transformation during thrombolytic treatment62. Excessive NO production appears to be related to the BBB breakdown during ischemic stroke. Overexpression of eNOS or treatment with an NO donor has been shown to inhibit the expression of MMP-2 mRNA in endothelial cells63. However, decreased MMP-9 activity was found in nNOS-null mice and in mice treated with a selective nNOS inhibitor64. The nonselective NOS inhibitor NG-nitro-L-arginine methyl ester (L-NAME) significantly reduced the BBB breakdown and MMP-9 activity in a middle cerebral artery occlusion (MCAO) animal model65,66. Therefore, the roles of NO in the activation of MMPs and BBB disruption are related to the amount of NO produced from different subtypes of NOS under different experimental conditions. However, the mechanisms of NO-mediated MMP activation and BBB disruption remain largely unknown. Recent studies conducted by us suggested that caveolins play critical roles in the NO-mediated MMP activation and the BBB disruption during cerebral ischemia-reperfusion injury. Caveolins are 22 kDa proteins found in plasma membrane invaginations known as caveolae (50–100 nanometers), which consist of three subtypes: caveolin-1 (Cav-1), caveolin-2 (Cav-2), and caveolin-3 (Cav-3). Cav-1 can inhibit the expression of NOS and production of NO via the caveolin-binding motif. Cav-1 was immunoprecipitated with eNOS in endothelial cells67 and was found to inhibit eNOS activity through direct binding to eNOS through amino acid residues 82-101 of the Cav-1 binding sequence68,69. Cav-1 binds to iNOS and nNOS in a similar manner as it does to eNOS70,71. To elucidate the potential mechanisms of the NO-mediated MMP activation and BBB disruption, we recently conducted a series of experiments to address the relationship of Cav-1, RNS, and MMP activity and the impact of their interaction on the BBB disruption using both rat and mouse MCAO models. Focal cerebral ischemia-reperfusion down-regulated the expression of Cav-1 in the isolated cortex microvessels, hippocampus and cortex of the ischemic brain. The down-regulation of Cav-1 correlated with the increased activities of MMP-2 and -9, decreased ZO-1 expression and enhanced BBB permeability. Treatment with L-NAME reserved the expression of Cav-1, inhibited MMP activity and reduced BBB permeability. After focal cerebral ischemia-reperfusion, Cav-1-deficient mice displayed higher MMP activities and BBB permeabilities than wild-type mice. The effects of the L-NAME on the MMP activity and BBB permeability were partly reversed in Cav-1-deficient mice. Thus, we proposed a novel mechanism for BBB disruption in cerebral ischemia-reperfusion injury. In ischemic stroke, overproduction of NO from nNOS and iNOS inhibited the Cav-1 expression, while the down-regulation of Cav-1 increased NOS activity and generated more NO38. This positive feedback loop could aggravate the effects of NO on the BBB insult during cerebral ischemia-reperfusion injury. Moreover, the inhibition effects of L-NAME on MMP activity and BBB permeability were partly mediated by Cav-166. Nevertheless, there are some controversial reports in literature. For example, increased Cav-1 expression and phosphorylation were shown to be correlated with the decreased expressions of occludin and claudin-5 in a rat cortical cold injury model72,73. Another study demonstrated that green tea polyphenols reduced the expression of Cav-1 within the microvessel fragments and ameliorated the BBB permeability in cerebral ischemic rats74. The discrepancy in previous studies might be due to the use of different ischemia protocols. Further work addressing the relationship of NO, Cav-1, and MMPs will aid in our understanding of the mechanisms of the BBB disruption and brain damage in cerebral ischemia-reperfusion injury.
Roles of peroxynitrite in ischemic stroke
In addition to NO production in the ischemia-reperfused brain, an overproduction of superoxide is also observed in neurons and endothelial cells during both the ischemic phase and the reperfusion period75,76,77. Thus, the formation of ONOO− is dramatically increased due to the extremely rapid reaction ratio of NO and superoxide [∼1×1010(mol/L)-1 s-1]. The increase in ONOO− levels has been discovered in blood samples of ischemic stroke patients which were collected at 24 h and 48 h after ischemic stroke78,79. Peroxynitrite has about 400 times higher penetrating capacity across lipid bilayers than its parent radical superoxide anions. As a critical neurotoxic factor, peroxynitrite exerts its cytotoxic effects through protein tyrosine nitration, lipid membrane peroxidation, induction of mitochondrial dysfunction, and PARP activation leading to DNA breakage80. Peroxynitrite triggers tyrosine nitration, the addition of a nitro (-NO2) group to the hydroxyl group of tyrosine residues to form 3-nitrotyrosine, which is the footprint of ONOO−51,81. Accumulated 3-nitrotyrosine has been found both in the MCAO animal models and in the autopsies of patients who have died of stroke82,83. By tyrosine nitration, ONOO− could alter protein structure and function, which may cause enzymatic activity inhibition, cytoskeletal disruption and signal transduction dysfunction84. Comprehensive studies have indicated that protein nitration could be one of the critical mechanisms of ONOO−-induced cytotoxicity51. Lipid peroxidation is considered to be another mechanism underlying the cytotoxicity of ONOO−. For example, through a lipid peroxidation reaction, ONOO− can oxidize the low-density lipoprotein and promote the development of atherogenesis85. ONOO− can also oxidize the myelin lipids and contribute to the process of inflammation in the brain tissue86. In addition, peroxynitrite can mediate DNA damage through its activation of the PARP pathway51. Peroxynitrite also induces the generation of DNA single-strand breaks by nitration of guanine nucleotides or by oxidative modification of the sugar-phosphate backbone. The presence of DNA single-strand breaks can further activate PARP. Peroxynitrite has been reported to cause DNA strand breakage and induce PARP activation in various cell types, such as vascular endothelial cells87,88, macrophages89, fibroblasts90, and neurons91. Furthermore, the PARP-deficient mice were less vulnerable than wild-type mice to MCAO-induced cerebral ischemic injury92,93.
In addition to its neurotoxicity, ONOO− also contributes to the BBB breakdown; it can mediate the activation of MMPs and the degradation of the TJ proteins, which subsequently leads to breakdown of the BBB integrity. Peroxynitrite was reported to activate MMP-1, 8, 9 via S-glutathiolation in purified human zymogens in the presence of GSH94. It can also modulate the activity of MMP-2 by modifying a cysteine residue in the auto-inhibitory domain of the zymogen95,96. 3-Morpholinosydnonimine (SIN-1, a ONOO− donor), rather than S-nitroso-N-acetyl-l,l-penicillamine (SNAP, an NO donor), increased the secretion of activated MMP-2 and the expression levels of MT1-MMP through activation of NF-κB97. Furthermore, the synthesized form of ONOO− is found to inactivate tissue inhibitor of MMP 1 (TIMP-1) by triggering TIMP-1 protein fragmentation98. Peroxynitrite inactivates TIMP-4 through the formation of nitration products on four tyrosine residues, subsequently activating MMP-2 in endothelial cells99. Peroxynitrite breaks down and rearranges tight junction proteins, which induces BBB disruption. Peroxynitrite decomposition catalysts (PDCs), such as FeTMPyP and FeTPPS, comprise an important tool for the study of ONOO−. PDCs can potentiate the reduction of NO and O2−, isomerize ONOO− to nitrate and decrease its decomposition to other reactive intermediates. It was reported that FeTMPyP not only protected the BBB integrity in an in vitro BBB model100, but it also prevented MMP activation and neurovascular injury in response to ischemia-reperfusion insults101. Taken together, ONOO− is responsible for the neurotoxicity and the BBB breakdown in cerebral ischemia-reperfusion injury.
RNS as potential molecular targets for drug development strategies
NO and ONOO− are crucial players of RNS in mediating BBB breakdown and brain damage during cerebral ischemia-reperfusion injury. Through complex cellular and biochemical mechanisms, RNS could mediate the degradation of TJs in the BBB and induce the influx of substances into the brain parenchyma from blood vessels, leading to the BBB opening and brain vasogenic edema. Therefore, RNS could be potential drug targets for the treatment of ischemic stroke.
Targeting NO as a drug development strategy
As NO has dual roles in this biological system, the therapeutic strategies should aim to establish balanced levels of NO by increasing the NO level derived from eNOS and decreasing the cytotoxic NO level by inhibiting the production of NO from iNOS and nNOS.
Strategies for increasing substrates of NO production
Basal levels of NO have physiological functions, such as vasodilatation, neuronal communication, and synaptic transmission. NO donors and substrates of eNOS may be applied to improve the outcome of patients with acute ischemia stroke. The NO donor nitrite has been proven to be an effective treatment for transient ischemia102. The NO precursor, L-arginine, increased blood flow, reduced the size of infarction and increased the functional neurological recovery in a rat model of ischemia stroke103. A systematic review summarized a total of 25 studies and concluded that L-arginine is effective in increasing rCBF and reducing the infarction volume in experimental stroke models104. However, L-arginine was found to be useful only for eNOS-deficient mice, but not in wild-type mice29. In addition, the administration of L-arginine may be hazardous to patients who have stimulated NOS activity105. Importantly, one clinical trial showed that L-arginine failed to be beneficial for ischemic stroke patients106. One of the explanations for the failure is that L-arginine may also increase the blood flow in normal brain tissue, thus relatively reducing the blood flow to the ischemia penumbra107. The potential applications of L-arginine for ischemic stroke should be further investigated with well-designed clinical trials.
Strategies for increasing eNOS activity
Statin is one of the promising agents that could increase the activity of eNOS. Statin can improve eNOS expression both through LDL-dependent and independent pathways108,109. It was reported to reduce both the infarction volume and edema formation in ischemic stroke animal models110,111. The protective effect of statin was completely abolished in eNOS knockout mice, indicating that the protective effects of statin are eNOS-dependent112. Ample preclinical and clinical studies further support the neuroprotective effects of statin, and it is now recommended for the prevention of stroke113,114. However, recent studies suggest that statin treatment exerts negative side effects, including increased incidence of hemorrhagic stroke115,116 and higher risk of infection117. Therefore, further studies by using well-designed clinical trials are necessary to evaluate the application of statin in ischemic stroke treatment. Given that statin has multiple pharmacological activities, the beneficial effects for ischemic stroke treatment cannot be attributed solely to the production of NO via eNOS activation.
nNOS and iNOS inhibitors
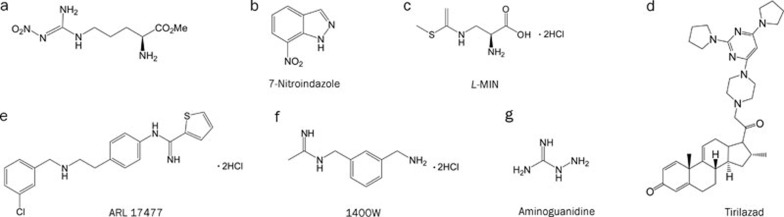
As stated above, a non-selective NOS inhibitor, L-NAME (Figure 1a), can reduce the infarction volume, prevent the BBB breakdown and improve the recovery of neurological functions in cerebral ischemic mouse models118,119. However, L-NAME also targets eNOS, which has protective effects during the ischemic process. Therefore, it is reasonable to use specific NOS inhibitors targeting only nNOS and iNOS in the treatment of ischemic stroke. Delta-(S-methylisothioureido)-L-norvaline (L-MIN) (Figure 1c), an nNOS-specific inhibitor, was reported to reduce infarction size in a rat stroke model120. Similarly, other nNOS inhibitors, including 7-nitroindazole121 (Figure 1b), tirilazad122 (Figure 1d) and ARL-1747744 (Figure 1e), also reduce infarction volume in a rat transient MCAO model. In addition to nNOS inhibitors, selective iNOS inhibitors such as 1400W and aminoguanidine are also promising for protecting brains from ischemic injury. For example, 1400W (Figure 1f) has been shown to attenuate ischemic brain injury. Administration of aminoguanidine (Figure 1g) even as late as 24 h after occlusion could reduce the infarct volume by up to 30%123.
Figure 1.
Chemical structures of NOS inhibitors. a, L-NAME; b, 7-nitroindazole; c, L-MIN; d, Tirilazad; e, ARL 17477; f, 1400W; g, Aminoguanidine.
Overall, although the NOS inhibitors have potential therapeutic values for cerebral ischemia-reperfusion injury in animal models, clinical evidence from human subjects is still lacking. Thus, it is a crucial time to conduct preclinical experiments and clinical trials to evaluate the safety and efficacy of a subset of NOS inhibitors for ischemic stroke treatment.
Peroxynitrite related drug discovery
Given that peroxynitrite is responsible for neurotoxicity in cerebral ischemia-reperfusion injury, drug development for either scavenging or catalytically decomposing peroxynitrite could be a potential valuable therapeutic strategy. However, compared to NO, drug development by targeting peroxynitrite is much slower, partly due to the technical limitations in the direct detection of peroxynitrite.
Development of fluorescent probes for peroxynitrite detection
Unlike NO, which can be directly detected by EPR or fluorescent imaging with various sensitive and specific probes both in vitro and in vivo, peroxynitrite detection is not successful due to less specificity and sensitivity. For instance, dichlorofluorescein (DCF) and rhodamine 123 have been proposed for ONOO− detection, but they cross-react with H2O2, ·OH, ·NO2, ·CO3−, Fe(II), Fe(III)/ascorbate, Fe(III)/EDTA, cytochrome c, and HOCl124,125,126. To resolve this problem, we developed a novel fluorescent probe, named HKGreen-1, that has highly sensitivity and selectivity for ONOO−. In primary cultured neurons, HKGreen-1 staining fluorescence was highly increased in the SIN-1 treatment group, but no fluorescence was observed in the other RNS- and ROS-treated groups127. With this probe, we discovered endogenous ONOO− generation in oxygen-glucose-deprived cortical neurons128. Based on the first generation of HKGreen-1, several modified probes have been produced129,130. These modified probes aim to act as peroxynitrite scavengers with the potential to protect ischemic brains from the ONOO−-mediated injury.
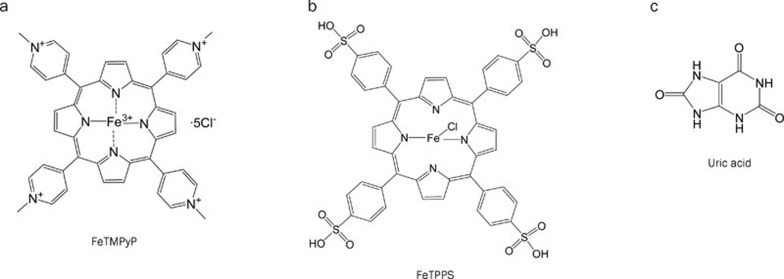
Peroxynitrite decomposition catalysts (PDCs)
FeTMPyP (Figure 2a) and FeTPPS (Figure 2b), two representative PDCs, were reported to reduce infarction size, brain edema, and neurological deficits, partly by reducing the peroxynitrite level, as well as protein nitration even when administered at 6 h after MCAO treatment131. Moreover, the administration of FeTMPyP 30 min prior to reperfusion prevented BBB breakdown by inhibiting MMP activation in a transient MCAO rat model101. FeTMPyP was also reported to improve plasma-induced vascular dysfunction and infarction in a mild hyperglycemic MCAO model132. Interestingly, the effects of FeTMPyP on the infarction volume and neurological defects were further improved when FeTMPyP was combined with a PARP inhibitor in a focal cerebral ischemia model133. Further studies on the long-term outcomes of PDC treatment for ischemic stroke are necessary.
Figure 2.
Chemical structures of PDCs and UA. a, FeTMPyP; b, FeTPPS; c, Uric acid.
Peroxynitrite scavengers
The development of ONOO− scavengers is an attractive strategy for drug discovery in stroke treatment. Herewith, we have summarized the recent progress in this field.
Uric acid
Uric acid is an endogenous peroxynitrite scavenger. The level of serum uric acid (SUA) was remarkably decreased in stroke patients134. Higher SUA levels appear to be associated with better outcome in both patients that have or have not undergone thrombolytic therapy135,136. Extraneous uric acid protected neurons against excitotoxic and metabolic injury by scavenging ONOO−, thereby attenuating mitochondrial damage and lipid peroxidation in vitro. Treatment with uric acid (Figure 2c) remarkably reduced the infarction volume, improved the behavioral outcome and attenuated the inflammatory response in rat MCAO cerebral ischemia models137,138. Uric acid not only possesses neuroprotective effects but also extends the benefits of the recombinant tissue plasminogen activator (rt-PA). Co-treatment of uric acid with rt-PA showed greater protective effects than either treatment did alone138. A phase II clinical trial of combined UA and rt-PA treatment has indicated that the treatment is safe and has the benefit for the increase of SUA level and the inhibitions of lipid peroxidation and MMP-9134,139. A randomized, placebo-controlled phase II trial of combined treatment with UA and rt-PA for acute ischemic stroke patients is ongoing140.
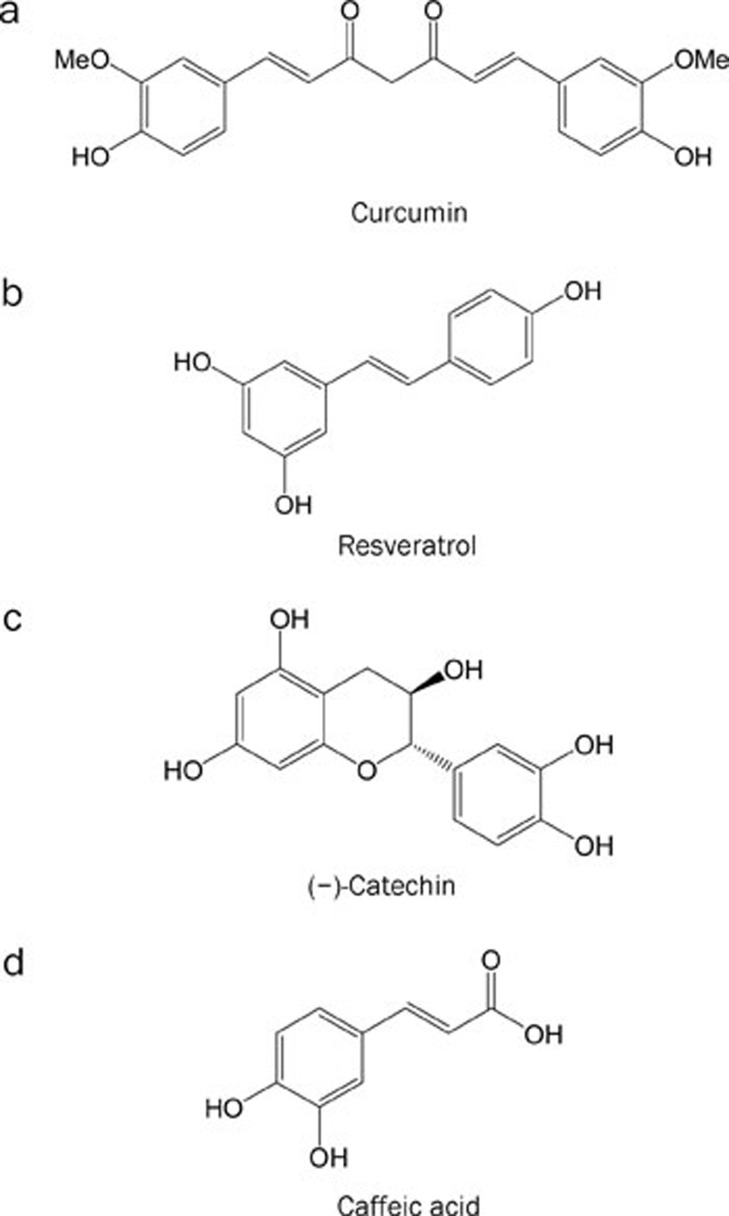
Phenolic compounds
Flavonoids, hydroxycinnamic and hydroxybenzoic acids are natural phenolic compounds. Their antioxidant activities are related to their hydrogen-donating and metal-chelating properties. These compounds can scavenge various species of free radicals, including peroxynitrite, superoxide, H2O2, and ·OH. Several compounds can scavenge ONOO− and have neuroprotective effects in ischemic stroke in vivo. For example, resveratrol (Figure 3b) direct reacts with ONOO− in vitro141 and protects neuronal cells by decreasing oxidative damage and suppressing glial activation141,142,143. Curcumin (Figure 3a) was reported to attenuate the ONOO−-induced BBB breakdown and ameliorate the brain damage during cerebral ischemia-reperfusion injury144. Green tea catechins (Figure 3c) protected the penumbra from ischemic reperfusion injury, which is thought be a result of decreases in iNOS expression and ONOO− level145. Caffeic acid (Figure 3d) was reported to directly react with ONOO−146 and protect ischemic brain tissues in a rat MCAO model147. However, there are few studies about their reaction rates and whether the reactions are direct or indirect in vivo. The overall mechanisms for these compounds to exert protective effects should be further investigated.
Figure 3.
Chemical structures of phenolic peroxynitrite scavengers. a, Curcumin; b, Resveratrol; c, (−)-Catechin; d, Caffeic acid.
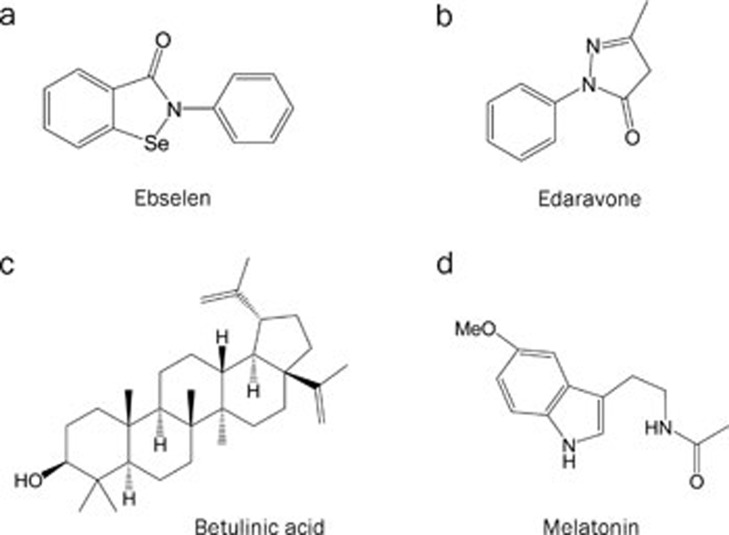
Non-phenolic compounds
Many non-phenolic antioxidant compounds exert strong ONOO− scavenging activities with neuroprotective effects, including cerium oxide148, ebselen149 (Figure 4a), edaravone150,151 (Figure 4b), betulinic acid152 (Figure 4c), and melatonin153,154 (Figure 4d). One such compound, edaravone, has been applied to acute stroke treatment in Japan and China for many years, and it has become a useful neuroprotective agent in clinical treatment in these regions155. One of the potential mechanisms of edaravone is related to decreased nitrotyrosine formation in vivo. However, similar to phenolic compounds, the detailed reaction mechanism(s) remain unknown.
Figure 4.
Chemical structures of non-phenolic peroxynitrite scavengers. a, Ebselen; b, Edaravone; c, Betulinic acid; d, Melatonin.
Regardless of the direct or indirect reaction in vivo, all of the above compounds could ameliorate cerebral ischemia-reperfusion injury through decreasing ONOO− -induced nitrotyrosine formation. Therefore, seeking an ONOO− scavenger or decomposer will likely be an important strategy for drug discovery in the treatment of ischemic stroke.
Conclusion
To date, almost all of the neuroprotective drugs tested were unsuccessful in their clinical trials, and rt-PA is the only FDA-approved drug for ischemic stroke treatment. However, the time window of rt-PA greatly limits its application; most stroke patients are unable to seek medical assistance quickly enough to receive the rt-PA treatment within the necessary 3-h window. Beyond that time window, delayed thrombolysis will induce fatal edema or intracranial hemorrhaging because of the cerebral ischemia-reperfusion injury. A combinatorial application of neuroprotective drugs with thrombolysis drugs would be an effective approach to maximize clinical outcome through extending the time window for thrombolysis, thereby reducing the reperfusion injury and enhancing the recovery of neurological function. During thrombolysis, reperfusion may produce large amounts of NO and ONOO−, which are very important mediators of neurotoxicity and the BBB breakdown. Therefore, targeting these RNS might be valuable for reducing the side effects of thrombolytic agents. Although some drug candidates have been implemented in clinical trials, most candidates are still at the early experimental stages. With gained understanding of the detailed mechanisms of RNS in ischemic stroke and the development of new RNS detection strategies, it will be possible to develop novel RNS-based drug candidates for ischemic stroke.
Acknowledgments
This work was supported by Hong Kong RGC General Research Fund (GRF No 774808M, 777610M, 777611M) and Seed Funding Programme for Basic Research at the University of Hong Kong (201011159053).
References
- Heron M. Deaths: leading causes for 2007. Natl Vital Stat Rep. 2011;59:1–95. [PubMed] [Google Scholar]
- Prevalence of disabilities and associated health conditions among adults — United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50:120–5. [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics — 2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Love S. Oxidative stress in brain ischemia. Brain Pathol. 1999;9:119–31. doi: 10.1111/j.1750-3639.1999.tb00214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brott T, Bogousslavsky J. Treatment of acute ischemic stroke. N Engl J Med. 2000;343:710–22. doi: 10.1056/NEJM200009073431007. [DOI] [PubMed] [Google Scholar]
- Meschia JF, Miller DA, Brott TG. Thrombolytic treatment of acute ischemic stroke. Mayo Clin Proc. 2002;77:542–51. doi: 10.4065/77.6.542. [DOI] [PubMed] [Google Scholar]
- Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. The NINDS t-PA Stroke Study Group. Stroke. 1997;28:2109–18. doi: 10.1161/01.str.28.11.2109. [DOI] [PubMed] [Google Scholar]
- Pan J, Konstas AA, Bateman B, Ortolano GA, Pile-Spellman J. Reperfusion injury following cerebral ischemia: pathophysiology, MR imaging, and potential therapies. Neuroradiology. 2007;49:93–102. doi: 10.1007/s00234-006-0183-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klann E, Roberson ED, Knapp LT, Sweatt JD. A role for superoxide in protein kinase C activation and induction of long-term potentiation. J Biol Chem. 1998;273:4516–22. doi: 10.1074/jbc.273.8.4516. [DOI] [PubMed] [Google Scholar]
- Chen BT, Avshalumov MV, Rice ME. H2O2 is a novel, endogenous modulator of synaptic dopamine release. J Neurophysiol. 2001;85:2468–76. doi: 10.1152/jn.2001.85.6.2468. [DOI] [PubMed] [Google Scholar]
- Heo JH, Han SW, Lee SK. Free radicals as triggers of brain edema formation after stroke. Free Radic Biol Med. 2005;39:51–70. doi: 10.1016/j.freeradbiomed.2005.03.035. [DOI] [PubMed] [Google Scholar]
- Chan PH. Reactive oxygen radicals in signaling and damage in the ischemic brain. J Cereb Blood Flow Metab. 2001;21:2–14. doi: 10.1097/00004647-200101000-00002. [DOI] [PubMed] [Google Scholar]
- Crack PJ, Taylor JM. Reactive oxygen species and the modulation of stroke. Free Radic Biol Med. 2005;38:1433–44. doi: 10.1016/j.freeradbiomed.2005.01.019. [DOI] [PubMed] [Google Scholar]
- Feng S, Yang Q, Liu M, Li W, Yuan W, Zhang S, et al. Edaravone for acute ischaemic stroke. Cochrane Database Syst Rev. 2011;(12):CD007230. doi: 10.1002/14651858.CD007230.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakase T, Yoshioka S, Suzuki A. Free radical scavenger, edaravone, reduces the lesion size of lacunar infarction in human brain ischemic stroke. BMC Neurol. 2011;11:39. doi: 10.1186/1471-2377-11-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lees KR, Zivin JA, Ashwood T, Davalos A, Davis SM, Diener HC, et al. NXY-059 for acute ischemic stroke. N Engl J Med. 2006;354:588–600. doi: 10.1056/NEJMoa052980. [DOI] [PubMed] [Google Scholar]
- Muir SW, Harrow C, Dawson J, Lees KR, Weir CJ, Sattar N, et al. Allopurinol use yields potentially beneficial effects on inflammatory indices in those with recent ischemic stroke: a randomized, double-blind, placebo-controlled trial. Stroke. 2008;39:3303–7. doi: 10.1161/STROKEAHA.108.519793. [DOI] [PubMed] [Google Scholar]
- Beckman JS, Ischiropoulos H, Zhu L, van der Woerd M, Smith C, Chen J, et al. Kinetics of superoxide dismutase- and iron-catalyzed nitration of phenolics by peroxynitrite. Arch Biochem Biophys. 1992;298:438–45. doi: 10.1016/0003-9861(92)90432-v. [DOI] [PubMed] [Google Scholar]
- Marla SS, Lee J, Groves JT. Peroxynitrite rapidly permeates phospholipid membranes. Proc Natl Acad Sci U S A. 1997;94:14243–8. doi: 10.1073/pnas.94.26.14243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jian Liu K, Rosenberg GA. Matrix metalloproteinases and free radicals in cerebral ischemia. Free Radic Biol Med. 2005;39:71–80. doi: 10.1016/j.freeradbiomed.2005.03.033. [DOI] [PubMed] [Google Scholar]
- Estevez AG, Radi R, Barbeito L, Shin JT, Thompson JA, Beckman JS. Peroxynitrite-induced cytotoxicity in PC12 cells: evidence for an apoptotic mechanism differentially modulated by neurotrophic factors. J Neurochem. 1995;65:1543–50. doi: 10.1046/j.1471-4159.1995.65041543.x. [DOI] [PubMed] [Google Scholar]
- Stefano GB, Kream RM. Reciprocal regulation of cellular nitric oxide formation by nitric oxide synthase and nitrite reductases. Med Sci Monit. 2011;17:RA221–6. doi: 10.12659/MSM.881972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer A, Folkerts G, Geppetti P, Groneberg DA. Mediators of asthma: nitric oxide. Pulm Pharmacol Ther. 2002;15:73–81. doi: 10.1006/pupt.2001.0332. [DOI] [PubMed] [Google Scholar]
- Lundberg JO, Weitzberg E, Gladwin MT. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov. 2008;7:156–67. doi: 10.1038/nrd2466. [DOI] [PubMed] [Google Scholar]
- Kiss JP, Vizi ES. Nitric oxide: a novel link between synaptic and nonsynaptic transmission. Trends Neurosci. 2001;24:211–5. doi: 10.1016/s0166-2236(00)01745-8. [DOI] [PubMed] [Google Scholar]
- Forstermann U. Nitric oxide and oxidative stress in vascular disease. Pflugers Arch. 2010;459:923–39. doi: 10.1007/s00424-010-0808-2. [DOI] [PubMed] [Google Scholar]
- Conti A, Miscusi M, Cardali S, Germano A, Suzuki H, Cuzzocrea S, et al. Nitric oxide in the injured spinal cord: synthases cross-talk, oxidative stress and inflammation. Brain Res Rev. 2007;54:205–18. doi: 10.1016/j.brainresrev.2007.01.013. [DOI] [PubMed] [Google Scholar]
- Moncada S, Palmer RM, Higgs EA. Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacol Rev. 1991;43:109–42. [PubMed] [Google Scholar]
- Samdani AF, Dawson TM, Dawson VL. Nitric oxide synthase in models of focal ischemia. Stroke. 1997;28:1283–8. doi: 10.1161/01.str.28.6.1283. [DOI] [PubMed] [Google Scholar]
- Sato S, Tominaga T, Ohnishi T, Ohnishi ST. EPR spin-trapping study of nitric oxide formation during bilateral carotid occlusion in the rat. Biochim Biophys Acta. 1993;1181:195–7. doi: 10.1016/0925-4439(93)90111-d. [DOI] [PubMed] [Google Scholar]
- Tominaga T, Sato S, Ohnishi T, Ohnishi ST. Potentiation of nitric oxide formation following bilateral carotid occlusion and focal cerebral ischemia in the rat: in vivo detection of the nitric oxide radical by electron paramagnetic resonance spin trapping. Brain Res. 1993;614:342–6. doi: 10.1016/0006-8993(93)91053-u. [DOI] [PubMed] [Google Scholar]
- Kader A, Frazzini VI, Solomon RA, Trifiletti RR. Nitric oxide production during focal cerebral ischemia in rats. Stroke. 1993;24:1709–16. doi: 10.1161/01.str.24.11.1709. [DOI] [PubMed] [Google Scholar]
- Malinski T, Bailey F, Zhang ZG, Chopp M. Nitric oxide measured by a porphyrinic microsensor in rat brain after transient middle cerebral artery occlusion. J Cereb Blood Flow Metab. 1993;13:355–8. doi: 10.1038/jcbfm.1993.48. [DOI] [PubMed] [Google Scholar]
- Fassbender K, Fatar M, Ragoschke A, Picard M, Bertsch T, Kuehl S, et al. Subacute but not acute generation of nitric oxide in focal cerebral ischemia. Stroke. 2000;31:2208–11. doi: 10.1161/01.str.31.9.2208. [DOI] [PubMed] [Google Scholar]
- Bolanos JP, Almeida A. Roles of nitric oxide in brain hypoxia-ischemia. Biochim Biophys Acta. 1999;1411:415–36. doi: 10.1016/s0005-2728(99)00030-4. [DOI] [PubMed] [Google Scholar]
- Grandati M, Verrecchia C, Revaud ML, Allix M, Boulu RG, Plotkine M. Calcium-independent NO-synthase activity and nitrites/nitrates production in transient focal cerebral ischaemia in mice. Br J Pharmacol. 1997;122:625–30. doi: 10.1038/sj.bjp.0701427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iadecola C, Xu X, Zhang F, el-Fakahany EE, Ross ME. Marked induction of calcium-independent nitric oxide synthase activity after focal cerebral ischemia. J Cereb Blood Flow Metab. 1995;15:52–9. doi: 10.1038/jcbfm.1995.6. [DOI] [PubMed] [Google Scholar]
- Shen J, Ma S, Chan P, Lee W, Fung PC, Cheung RT, et al. Nitric oxide down-regulates caveolin-1 expression in rat brains during focal cerebral ischemia and reperfusion injury. J Neurochem. 2006;96:1078–89. doi: 10.1111/j.1471-4159.2005.03589.x. [DOI] [PubMed] [Google Scholar]
- Huang Z, Huang PL, Ma J, Meng W, Ayata C, Fishman MC, et al. Enlarged infarcts in endothelial nitric oxide synthase knockout mice are attenuated by nitro-L-arginine. J Cereb Blood Flow Metab. 1996;16:981–7. doi: 10.1097/00004647-199609000-00023. [DOI] [PubMed] [Google Scholar]
- Rudic RD, Sessa WC. Nitric oxide in endothelial dysfunction and vascular remodeling: clinical correlates and experimental links. Am J Hum Genet. 1999;64:673–7. doi: 10.1086/302304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iadecola C. Bright and dark sides of nitric oxide in ischemic brain injury. Trends Neurosci. 1997;20:132–9. doi: 10.1016/s0166-2236(96)10074-6. [DOI] [PubMed] [Google Scholar]
- Ferriero DM, Holtzman DM, Black SM, Sheldon RA. Neonatal mice lacking neuronal nitric oxide synthase are less vulnerable to hypoxic-ischemic injury. Neurobiol Dis. 1996;3:64–71. doi: 10.1006/nbdi.1996.0006. [DOI] [PubMed] [Google Scholar]
- Iadecola C, Zhang F, Casey R, Nagayama M, Ross ME. Delayed reduction of ischemic brain injury and neurological deficits in mice lacking the inducible nitric oxide synthase gene. J Neurosci. 1997;17:9157–64. doi: 10.1523/JNEUROSCI.17-23-09157.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang ZG, Reif D, Macdonald J, Tang WX, Kamp DK, Gentile RJ, et al. ARL 17477, a potent and selective neuronal NOS inhibitor decreases infarct volume after transient middle cerebral artery occlusion in rats. J Cereb Blood Flow Metab. 1996;16:599–604. doi: 10.1097/00004647-199607000-00009. [DOI] [PubMed] [Google Scholar]
- Chabrier PE, Auguet M, Spinnewyn B, Auvin S, Cornet S, Demerle-Pallardy C, et al. BN 80933, a dual inhibitor of neuronal nitric oxide synthase and lipid peroxidation: a promising neuroprotective strategy. Proc Natl Acad Sci U S A. 1999;96:10824–9. doi: 10.1073/pnas.96.19.10824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmentier S, Bohme GA, Lerouet D, Damour D, Stutzmann JM, Margaill I, et al. Selective inhibition of inducible nitric oxide synthase prevents ischaemic brain injury. Br J Pharmacol. 1999;127:546–52. doi: 10.1038/sj.bjp.0702549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen RA, Adachi T. Nitric-oxide-induced vasodilatation: regulation by physiologic s-glutathiolation and pathologic oxidation of the sarcoplasmic endoplasmic reticulum calcium ATPase. Trends Cardiovasc Med. 2006;16:109–14. doi: 10.1016/j.tcm.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Stamler JS. Redox signaling: nitrosylation and related target interactions of nitric oxide. Cell. 1994;78:931–6. doi: 10.1016/0092-8674(94)90269-0. [DOI] [PubMed] [Google Scholar]
- Matsushita K, Morrell CN, Cambien B, Yang SX, Yamakuchi M, Bao C, et al. Nitric oxide regulates exocytosis by S-nitrosylation of N-ethylmaleimide-sensitive factor. Cell. 2003;115:139–50. doi: 10.1016/s0092-8674(03)00803-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipton SA, Choi YB, Pan ZH, Lei SZ, Chen HS, Sucher NJ, et al. A redox-based mechanism for the neuroprotective and neurodestructive effects of nitric oxide and related nitroso-compounds. Nature. 1993;364:626–32. doi: 10.1038/364626a0. [DOI] [PubMed] [Google Scholar]
- Pacher P, Beckman JS, Liaudet L. Nitric oxide and peroxynitrite in health and disease. Physiol Rev. 2007;87:315–424. doi: 10.1152/physrev.00029.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Maschio A, De Luigi A, Martin-Padura I, Brockhaus M, Bartfai T, Fruscella P, et al. Leukocyte recruitment in the cerebrospinal fluid of mice with experimental meningitis is inhibited by an antibody to junctional adhesion molecule (JAM) J Exp Med. 1999;190:1351–6. doi: 10.1084/jem.190.9.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasche Y, Fujimura M, Morita-Fujimura Y, Copin JC, Kawase M, Massengale J, et al. Early appearance of activated matrix metalloproteinase-9 after focal cerebral ischemia in mice: a possible role in blood-brain barrier dysfunction. J Cereb Blood Flow Metab. 1999;19:1020–8. doi: 10.1097/00004647-199909000-00010. [DOI] [PubMed] [Google Scholar]
- Aoki T, Sumii T, Mori T, Wang X, Lo EH. Blood-brain barrier disruption and matrix metalloproteinase-9 expression during reperfusion injury: mechanical versus embolic focal ischemia in spontaneously hypertensive rats. Stroke. 2002;33:2711–7. doi: 10.1161/01.str.0000033932.34467.97. [DOI] [PubMed] [Google Scholar]
- Pfefferkorn T, Rosenberg GA. Closure of the blood-brain barrier by matrix metalloproteinase inhibition reduces rtPA-mediated mortality in cerebral ischemia with delayed reperfusion. Stroke. 2003;34:2025–30. doi: 10.1161/01.STR.0000083051.93319.28. [DOI] [PubMed] [Google Scholar]
- Yang Y, Estrada EY, Thompson JF, Liu W, Rosenberg GA. Matrix metalloproteinase-mediated disruption of tight junction proteins in cerebral vessels is reversed by synthetic matrix metalloproteinase inhibitor in focal ischemia in rat. J Cereb Blood Flow Metab. 2007;27:697–709. doi: 10.1038/sj.jcbfm.9600375. [DOI] [PubMed] [Google Scholar]
- Chang DI, Hosomi N, Lucero J, Heo JH, Abumiya T, Mazar AP, et al. Activation systems for latent matrix metalloproteinase-2 are upregulated immediately after focal cerebral ischemia. J Cereb Blood Flow Metab. 2003;23:1408–19. doi: 10.1097/01.WCB.0000091765.61714.30. [DOI] [PubMed] [Google Scholar]
- Rosenberg GA. Matrix metalloproteinases in neuroinflammation. Glia. 2002;39:279–91. doi: 10.1002/glia.10108. [DOI] [PubMed] [Google Scholar]
- Lee CZ, Xue Z, Zhu Y, Yang GY, Young WL. Matrix metalloproteinase-9 inhibition attenuates vascular endothelial growth factor-induced intracerebral hemorrhage. Stroke. 2007;38:2563–8. doi: 10.1161/STROKEAHA.106.481515. [DOI] [PubMed] [Google Scholar]
- Rosenberg GA, Yang Y. Vasogenic edema due to tight junction disruption by matrix metalloproteinases in cerebral ischemia. Neurosurg Focus. 2007;22:E4. doi: 10.3171/foc.2007.22.5.5. [DOI] [PubMed] [Google Scholar]
- Bauer AT, Burgers HF, Rabie T, Marti HH. Matrix metalloproteinase-9 mediates hypoxia-induced vascular leakage in the brain via tight junction rearrangement. J Cereb Blood Flow Metab. 2010;30:837–48. doi: 10.1038/jcbfm.2009.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Fernandez M, Bellolio MF, Stead LG. Matrix metalloproteinase-9 as a marker for acute ischemic stroke: a systematic review. J Stroke Cerebrovasc Dis. 2011;20:47–54. doi: 10.1016/j.jstrokecerebrovasdis.2009.10.008. [DOI] [PubMed] [Google Scholar]
- Chen HH, Wang DL. Nitric oxide inhibits matrix metalloproteinase-2 expression via the induction of activating transcription factor 3 in endothelial cells. Mol Pharmacol. 2004;65:1130–40. doi: 10.1124/mol.65.5.1130. [DOI] [PubMed] [Google Scholar]
- Gu Z, Kaul M, Yan B, Kridel SJ, Cui J, Strongin A, et al. S-nitrosylation of matrix metalloproteinases: signaling pathway to neuronal cell death. Science. 2002;297:1186–90. doi: 10.1126/science.1073634. [DOI] [PubMed] [Google Scholar]
- Gursoy-Ozdemir Y, Can A, Dalkara T. Reperfusion-induced oxidative/nitrative injury to neurovascular unit after focal cerebral ischemia. Stroke. 2004;35:1449–53. doi: 10.1161/01.STR.0000126044.83777.f4. [DOI] [PubMed] [Google Scholar]
- Gu Y, Zheng G, Xu M, Li Y, Chen X, Zhu W, et al. Caveolin-1 regulates nitric oxide-mediated matrix metalloproteinases activity and blood-brain barrier permeability in focal cerebral ischemia and reperfusion injury. J Neurochem. 2012;120:147–56. doi: 10.1111/j.1471-4159.2011.07542.x. [DOI] [PubMed] [Google Scholar]
- Garcia-Cardena G, Fan R, Stern DF, Liu J, Sessa WC. Endothelial nitric oxide synthase is regulated by tyrosine phosphorylation and interacts with caveolin-1. J Biol Chem. 1996;271:27237–40. doi: 10.1074/jbc.271.44.27237. [DOI] [PubMed] [Google Scholar]
- Michel JB, Feron O, Sacks D, Michel T. Reciprocal regulation of endothelial nitric-oxide synthase by Ca2+-calmodulin and caveolin. J Biol Chem. 1997;272:15583–6. doi: 10.1074/jbc.272.25.15583. [DOI] [PubMed] [Google Scholar]
- Michel JB, Feron O, Sase K, Prabhakar P, Michel T. Caveolin versus calmodulin. Counterbalancing allosteric modulators of endothelial nitric oxide synthase. J Biol Chem. 1997;272:25907–12. doi: 10.1074/jbc.272.41.25907. [DOI] [PubMed] [Google Scholar]
- Garcia-Cardena G, Martasek P, Masters BS, Skidd PM, Couet J, Li S, et al. Dissecting the interaction between nitric oxide synthase (NOS) and caveolin. Functional significance of the NOS caveolin binding domain in vivo. J Biol Chem. 1997;272:25437–40. doi: 10.1074/jbc.272.41.25437. [DOI] [PubMed] [Google Scholar]
- Felley-Bosco E, Bender FC, Courjault-Gautier F, Bron C, Quest AF. Caveolin-1 down-regulates inducible nitric oxide synthase via the proteasome pathway in human colon carcinoma cells. Proc Natl Acad Sci U S A. 2000;97:14334–9. doi: 10.1073/pnas.250406797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nag S, Venugopalan R, Stewart DJ. Increased caveolin-1 expression precedes decreased expression of occludin and claudin-5 during blood-brain barrier breakdown. Acta Neuropathol. 2007;114:459–69. doi: 10.1007/s00401-007-0274-x. [DOI] [PubMed] [Google Scholar]
- Nag S, Manias JL, Stewart DJ. Expression of endothelial phosphorylated caveolin-1 is increased in brain injury. Neuropathol Appl Neurobiol. 2009;35:417–26. doi: 10.1111/j.1365-2990.2008.01009.x. [DOI] [PubMed] [Google Scholar]
- Zhang S, Liu Y, Zhao Z, Xue Y. Effects of green tea polyphenols on caveolin-1 of microvessel fragments in rats with cerebral ischemia. Neurol Res. 2010;32:963–70. doi: 10.1179/016164110X12700393823570. [DOI] [PubMed] [Google Scholar]
- Fabian RH, DeWitt DS, Kent TA. In vivo detection of superoxide anion production by the brain using a cytochrome c electrode. J Cereb Blood Flow Metab. 1995;15:242–7. doi: 10.1038/jcbfm.1995.30. [DOI] [PubMed] [Google Scholar]
- Peters O, Back T, Lindauer U, Busch C, Megow D, Dreier J, et al. Increased formation of reactive oxygen species after permanent and reversible middle cerebral artery occlusion in the rat. J Cereb Blood Flow Metab. 1998;18:196–205. doi: 10.1097/00004647-199802000-00011. [DOI] [PubMed] [Google Scholar]
- Kim GW, Kondo T, Noshita N, Chan PH. Manganese superoxide dismutase deficiency exacerbates cerebral infarction after focal cerebral ischemia/reperfusion in mice: implications for the production and role of superoxide radicals. Stroke. 2002;33:809–15. doi: 10.1161/hs0302.103745. [DOI] [PubMed] [Google Scholar]
- Al-Nimer MS, Al-Mahdawi AM, Sakeni RA. Assessment of nitrosative oxidative stress in patients with middle cerebral artery occlusion. Neurosciences (Riyadh) 2007;12:31–4. [PubMed] [Google Scholar]
- Nanetti L, Taffi R, Vignini A, Moroni C, Raffaelli F, Bacchetti T, et al. Reactive oxygen species plasmatic levels in ischemic stroke. Mol Cell Biochem. 2007;303:19–25. doi: 10.1007/s11010-007-9451-4. [DOI] [PubMed] [Google Scholar]
- Moro MA, Almeida A, Bolanos JP, Lizasoain I. Mitochondrial respiratory chain and free radical generation in stroke. Free Radic Biol Med. 2005;39:1291–304. doi: 10.1016/j.freeradbiomed.2005.07.010. [DOI] [PubMed] [Google Scholar]
- Kuhn DM, Sakowski SA, Sadidi M, Geddes TJ. Nitrotyrosine as a marker for peroxynitrite-induced neurotoxicity: the beginning or the end of the end of dopamine neurons. J Neurochem. 2004;89:529–36. doi: 10.1111/j.1471-4159.2004.02346.x. [DOI] [PubMed] [Google Scholar]
- Greenacre SA, Ischiropoulos H. Tyrosine nitration: localisation, quantification, consequences for protein function and signal transduction. Free Radic Res. 2001;34:541–81. doi: 10.1080/10715760100300471. [DOI] [PubMed] [Google Scholar]
- Suzuki M, Tabuchi M, Ikeda M, Tomita T. Concurrent formation of peroxynitrite with the expression of inducible nitric oxide synthase in the brain during middle cerebral artery occlusion and reperfusion in rats. Brain Res. 2002;951:113–20. doi: 10.1016/s0006-8993(02)03145-1. [DOI] [PubMed] [Google Scholar]
- Schopfer FJ, Baker PR, Freeman BA. NO-dependent protein nitration: a cell signaling event or an oxidative inflammatory response. Trends Biochem Sci. 2003;28:646–54. doi: 10.1016/j.tibs.2003.10.006. [DOI] [PubMed] [Google Scholar]
- Guy RA, Maguire GF, Crandall I, Connelly PW, Kain KC. Characterization of peroxynitrite-oxidized low density lipoprotein binding to human CD36. Atherosclerosis. 2001;155:19–28. doi: 10.1016/s0021-9150(00)00524-4. [DOI] [PubMed] [Google Scholar]
- Shi H, Noguchi N, Xu Y, Niki E. Formation of phospholipid hydroperoxides and its inhibition by alpha-tocopherol in rat brain synaptosomes induced by peroxynitrite. Biochem Biophys Res Commun. 1999;257:651–6. doi: 10.1006/bbrc.1999.0434. [DOI] [PubMed] [Google Scholar]
- Garcia Soriano F, Virag L, Jagtap P, Szabo E, Mabley JG, Liaudet L, et al. Diabetic endothelial dysfunction: the role of poly(ADP-ribose) polymerase activation. Nat Med. 2001;7:108–13. doi: 10.1038/83241. [DOI] [PubMed] [Google Scholar]
- Szabo C, Cuzzocrea S, Zingarelli B, O'Connor M, Salzman AL. Endothelial dysfunction in a rat model of endotoxic shock. Importance of the activation of poly (ADP-ribose) synthetase by peroxynitrite. J Clin Invest. 1997;100:723–35. doi: 10.1172/JCI119585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zingarelli B, O'Connor M, Wong H, Salzman AL, Szabo C. Peroxynitrite-mediated DNA strand breakage activates poly-adenosine diphosphate ribosyl synthetase and causes cellular energy depletion in macrophages stimulated with bacterial lipopolysaccharide. J Immunol. 1996;156:350–8. [PubMed] [Google Scholar]
- Szabo C, Virag L, Cuzzocrea S, Scott GS, Hake P, O'Connor MP, et al. Protection against peroxynitrite-induced fibroblast injury and arthritis development by inhibition of poly(ADP-ribose) synthase. Proc Natl Acad Sci U S A. 1998;95:3867–72. doi: 10.1073/pnas.95.7.3867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Rosenberg PA. Caspase-1 and poly (ADP-ribose) polymerase inhibitors may protect against peroxynitrite-induced neurotoxicity independent of their enzyme inhibitor activity. Eur J Neurosci. 2004;20:1727–36. doi: 10.1111/j.1460-9568.2004.03651.x. [DOI] [PubMed] [Google Scholar]
- Endres M, Wang ZQ, Namura S, Waeber C, Moskowitz MA. Ischemic brain injury is mediated by the activation of poly(ADP-ribose)polymerase. J Cereb Blood Flow Metab. 1997;17:1143–51. doi: 10.1097/00004647-199711000-00002. [DOI] [PubMed] [Google Scholar]
- Eliasson MJ, Sampei K, Mandir AS, Hurn PD, Traystman RJ, Bao J, et al. Poly(ADP-ribose) polymerase gene disruption renders mice resistant to cerebral ischemia. Nat Med. 1997;3:1089–95. doi: 10.1038/nm1097-1089. [DOI] [PubMed] [Google Scholar]
- Okamoto T, Akaike T, Sawa T, Miyamoto Y, van der Vliet A, Maeda H. Activation of matrix metalloproteinases by peroxynitrite-induced protein S-glutathiolation via disulfide S-oxide formation. J Biol Chem. 2001;276:29596–602. doi: 10.1074/jbc.M102417200. [DOI] [PubMed] [Google Scholar]
- Viappiani S, Nicolescu AC, Holt A, Sawicki G, Crawford BD, Leon H, et al. Activation and modulation of 72 kDa matrix metalloproteinase-2 by peroxynitrite and glutathione. Biochem Pharmacol. 2009;77:826–34. doi: 10.1016/j.bcp.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Rajagopalan S, Meng XP, Ramasamy S, Harrison DG, Galis ZS. Reactive oxygen species produced by macrophage-derived foam cells regulate the activity of vascular matrix metalloproteinases in vitro. Implications for atherosclerotic plaque stability. J Clin Invest. 1996;98:2572–9. doi: 10.1172/JCI119076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Migita K, Maeda Y, Abiru S, Komori A, Yokoyama T, Takii Y, et al. Peroxynitrite-mediated matrix metalloproteinase-2 activation in human hepatic stellate cells. FEBS Lett. 2005;579:3119–25. doi: 10.1016/j.febslet.2005.04.071. [DOI] [PubMed] [Google Scholar]
- Frears ER, Zhang Z, Blake DR, O'Connell JP, Winyard PG. Inactivation of tissue inhibitor of metalloproteinase-1 by peroxynitrite. FEBS Lett. 1996;381:21–4. doi: 10.1016/0014-5793(96)00065-8. [DOI] [PubMed] [Google Scholar]
- Donnini S, Monti M, Roncone R, Morbidelli L, Rocchigiani M, Oliviero S, et al. Peroxynitrite inactivates human-tissue inhibitor of metalloproteinase-4. FEBS Lett. 2008;582:1135–40. doi: 10.1016/j.febslet.2008.02.080. [DOI] [PubMed] [Google Scholar]
- Tan KH, Harrington S, Purcell WM, Hurst RD. Peroxynitrite mediates nitric oxide-induced blood-brain barrier damage. Neurochem Res. 2004;29:579–87. doi: 10.1023/b:nere.0000014828.32200.bd. [DOI] [PubMed] [Google Scholar]
- Suofu Y, Clark J, Broderick J, Wagner KR, Tomsick T, Sa Y, et al. Peroxynitrite decomposition catalyst prevents matrix metalloproteinase activation and neurovascular injury after prolonged cerebral ischemia in rats. J Neurochem. 2010;115:1266–76. doi: 10.1111/j.1471-4159.2010.07026.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung KH, Chu K, Ko SY, Lee ST, Sinn DI, Park DK, et al. Early intravenous infusion of sodium nitrite protects brain against in vivo ischemia-reperfusion injury. Stroke. 2006;37:2744–50. doi: 10.1161/01.STR.0000245116.40163.1c. [DOI] [PubMed] [Google Scholar]
- Morikawa E, Moskowitz MA, Huang Z, Yoshida T, Irikura K, Dalkara T. L-arginine infusion promotes nitric oxide-dependent vasodilation, increases regional cerebral blood flow, and reduces infarction volume in the rat. Stroke. 1994;25:429–35. doi: 10.1161/01.str.25.2.429. [DOI] [PubMed] [Google Scholar]
- Willmot M, Gray L, Gibson C, Murphy S, Bath PMW. A systematic review of nitric oxide donors and L-arginine in experimental stroke; effects on infarct size and cerebral blood flow. Nitric Oxide. 2005;12:141–9. doi: 10.1016/j.niox.2005.01.003. [DOI] [PubMed] [Google Scholar]
- Roth E. The impact of L-arginine-nitric oxide metabolism on ischemia/reperfusion injury. Curr Opin Clin Nutr Metab Care. 1998;1:97. doi: 10.1097/00075197-199801000-00016. [DOI] [PubMed] [Google Scholar]
- Bath P, Willmot M, Leonardi-Bee J, Bath-Hextall F. Nitric oxide donors (nitrates), L-arginine, or nitric oxide synthase inhibitors for acute stroke. Cochrane Database Syst Rev. 2002;4:CD000398. doi: 10.1002/14651858.CD000398. [DOI] [PubMed] [Google Scholar]
- Lassen NA.Pathophysiology of brain ischemia as it relates to the therapy of acute ischemic stroke Clin Neuropharmacol 199013Suppl 3: S1–8. [DOI] [PubMed] [Google Scholar]
- Laufs U, Liao JK. Post-transcriptional regulation of endothelial nitric oxide synthase mRNA stability by Rho GTPase. J Biol Chem. 1998;273:24266. doi: 10.1074/jbc.273.37.24266. [DOI] [PubMed] [Google Scholar]
- Laufs U. Beyond lipid-lowering: effects of statins on endothelial nitric oxide. Eur J Clin Pharmacol. 2003;58:719–31. doi: 10.1007/s00228-002-0556-0. [DOI] [PubMed] [Google Scholar]
- Sironi L, Cimino M, Guerrini U, Calvio AM, Lodetti B, Asdente M, et al. Treatment with statins after induction of focal ischemia in rats reduces the extent of brain damage. Arterioscler Thromb Vasc Biol. 2003;23:322–7. doi: 10.1161/01.atv.0000044458.23905.3b. [DOI] [PubMed] [Google Scholar]
- Prinz V, Laufs U, Gertz K, Kronenberg G, Balkaya M, Leithner C, et al. Intravenous rosuvastatin for acute stroke treatment. Stroke. 2008;39:433–8. doi: 10.1161/STROKEAHA.107.492470. [DOI] [PubMed] [Google Scholar]
- Endres M, Laufs U, Huang Z, Nakamura T, Huang P, Moskowitz MA, et al. Stroke protection by 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase inhibitors mediated by endothelial nitric oxide synthase. Proc Natl Acad Sci U S A. 1998;95:8880. doi: 10.1073/pnas.95.15.8880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- Adams HP, Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38:1655–711. doi: 10.1161/STROKEAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- Collins R, Armitage J, Parish S, Sleight P, Peto R. Effects of cholesterol-lowering with simvastatin on stroke and other major vascular events in 20536 people with cerebrovascular disease or other high-risk conditions. Lancet. 2004;363:757–67. doi: 10.1016/S0140-6736(04)15690-0. [DOI] [PubMed] [Google Scholar]
- Vergouwen MD, de Haan RJ, Vermeulen M, Roos YB. Statin treatment and the occurrence of hemorrhagic stroke in patients with a history of cerebrovascular disease. Stroke. 2008;39:497–502. doi: 10.1161/STROKEAHA.107.488791. [DOI] [PubMed] [Google Scholar]
- Becker K, Tanzi P, Kalil A, Shibata D, Cain K. Early statin use is associated with increased risk of infection after stroke. J Stroke Cerebrovasc Dis. 2011. [DOI] [PMC free article] [PubMed]
- Ding-Zhou L, Marchand-Verrecchia C, Croci N, Plotkine M, Margaill I. L-NAME reduces infarction, neurological deficit and blood-brain barrier disruption following cerebral ischemia in mice. Eur J Pharmacol. 2002;457:137–46. doi: 10.1016/s0014-2999(02)02686-9. [DOI] [PubMed] [Google Scholar]
- Margaill I, Allix M, Boulu RG, Plotkine M. Dose- and time-dependence of L-NAME neuroprotection in transient focal cerebral ischaemia in rats. Br J Pharmacol. 1997;120:160–3. doi: 10.1038/sj.bjp.0700889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagafuji T, Sugiyama M, Muto A, Makino T, Miyauchi T, Nabata H. The neuroprotective effect of a potent and selective inhibitor of type I NOS (L-MIN) in a rat model of focal cerebral ischaemia. Neuroreport. 1995;6:1541. doi: 10.1097/00001756-199507310-00019. [DOI] [PubMed] [Google Scholar]
- Yoshida T, Limmroth V, Irikura K, Moskowitz MA. The NOS inhibitor, 7-nitroindazole, decreases focal infarct volume but not the response to topical acetylcholine in pial vessels. J Cereb Blood Flow Metab. 1994;14:924–9. doi: 10.1038/jcbfm.1994.123. [DOI] [PubMed] [Google Scholar]
- del Pilar Fernandez-Rodriguez M, Belmonte A, Meizoso M, Garcia-Novio M, Garcia-Iglesias E. Effect of tirilazad on brain nitric oxide synthase activity during cerebral ischemia in rats. Pharmacology. 1997;54:108–12. doi: 10.1159/000139476. [DOI] [PubMed] [Google Scholar]
- Iadecola C, Zhang F, Xu X. Inhibition of inducible nitric oxide synthase ameliorates cerebral ischemic damage. Am J Physiol-Regul, Integr Comp Physiol. 1995;268:R286–R92. doi: 10.1152/ajpregu.1995.268.1.R286. [DOI] [PubMed] [Google Scholar]
- Gomes A, Fernandes E, Lima JL. Use of fluorescence probes for detection of reactive nitrogen species: a review. J Fluoresc. 2006;16:119–39. doi: 10.1007/s10895-005-0030-3. [DOI] [PubMed] [Google Scholar]
- Wardman P. Fluorescent and luminescent probes for measurement of oxidative and nitrosative species in cells and tissues: progress, pitfalls, and prospects. Free Radic Biol Med. 2007;43:995–1022. doi: 10.1016/j.freeradbiomed.2007.06.026. [DOI] [PubMed] [Google Scholar]
- Wardman P. Methods to measure the reactivity of peroxynitrite-derived oxidants toward reduced fluoresceins and rhodamines. Methods Enzymol. 2008;441:261–82. doi: 10.1016/S0076-6879(08)01214-7. [DOI] [PubMed] [Google Scholar]
- Yang D, Wang HL, Sun ZN, Chung NW, Shen JG. A highly selective fluorescent probe for the detection and imaging of peroxynitrite in living cells. J Am Chem Soc. 2006;128:6004–5. doi: 10.1021/ja0603756. [DOI] [PubMed] [Google Scholar]
- Yang D, Sun ZN, Peng T, Wang HL, Shen JG, Chen Y, et al. Synthetic fluorescent probes for imaging of peroxynitrite and hypochlorous acid in living cells. Methods Mol Biol. 2010;591:93–103. doi: 10.1007/978-1-60761-404-3_5. [DOI] [PubMed] [Google Scholar]
- Sun ZN, Wang HL, Liu FQ, Chen Y, Tam PK, Yang D. BODIPY-based fluorescent probe for peroxynitrite detection and imaging in living cells. Org Lett. 2009;11:1887–90. doi: 10.1021/ol900279z. [DOI] [PubMed] [Google Scholar]
- Peng T, Yang D. HKGreen-3: a rhodol-based fluorescent probe for peroxynitrite. Org Lett. 2010;12:4932–5. doi: 10.1021/ol102182j. [DOI] [PubMed] [Google Scholar]
- Thiyagarajan M, Kaul CL, Sharma SS. Neuroprotective efficacy and therapeutic time window of peroxynitrite decomposition catalysts in focal cerebral ischemia in rats. Br J Pharmacol. 2004;142:899–911. doi: 10.1038/sj.bjp.0705811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palomares SM, Gardner-Morse I, Sweet JG, Cipolla MJ. Peroxynitrite decomposition with FeTMPyP improves plasma-induced vascular dysfunction and infarction during mild but not severe hyperglycemic stroke. J Cereb Blood Flow Metab. 2012;32:1035–45. doi: 10.1038/jcbfm.2012.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma SS, Munusamy S, Thiyagarajan M, Kaul CL. Neuroprotective effect of peroxynitrite decomposition catalyst and poly(adenosine diphosphate-ribose) polymerase inhibitor alone and in combination in rats with focal cerebral ischemia. J Neurosurg. 2004;101:669–75. doi: 10.3171/jns.2004.101.4.0669. [DOI] [PubMed] [Google Scholar]
- Amaro S, Soy D, Obach V, Cervera A, Planas AM, Chamorro A. A pilot study of dual treatment with recombinant tissue plasminogen activator and uric acid in acute ischemic stroke. Stroke. 2007;38:2173–5. doi: 10.1161/STROKEAHA.106.480699. [DOI] [PubMed] [Google Scholar]
- Chamorro A, Obach V, Cervera A, Revilla M, Deulofeu R, Aponte JH. Prognostic significance of uric acid serum concentration in patients with acute ischemic stroke. Stroke. 2002;33:1048–52. doi: 10.1161/hs0402.105927. [DOI] [PubMed] [Google Scholar]
- Amaro S, Urra X, Gomez-Choco M, Obach V, Cervera A, Vargas M, et al. Uric acid levels are relevant in patients with stroke treated with thrombolysis. Stroke. 2011;42:S28–32. doi: 10.1161/STROKEAHA.110.596528. [DOI] [PubMed] [Google Scholar]
- Yu ZF, Bruce-Keller AJ, Goodman Y, Mattson MP. Uric acid protects neurons against excitotoxic and metabolic insults in cell culture, and against focal ischemic brain injury in vivo. J Neurosci Res. 1998;53:613–25. doi: 10.1002/(SICI)1097-4547(19980901)53:5<613::AID-JNR11>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Romanos E, Planas AM, Amaro S, Chamorro A. Uric acid reduces brain damage and improves the benefits of rt-PA in a rat model of thromboembolic stroke. J Cereb Blood Flow Metab. 2007;27:14–20. doi: 10.1038/sj.jcbfm.9600312. [DOI] [PubMed] [Google Scholar]
- Amaro S, Obach V, Cervera A, Urra X, Gomez-Choco M, Planas AM, et al. Course of matrix metalloproteinase-9 isoforms after the administration of uric acid in patients with acute stroke: a proof-of-concept study. J Neurol. 2009;256:651–6. doi: 10.1007/s00415-009-0153-6. [DOI] [PubMed] [Google Scholar]
- Amaro S, Canovas D, Castellanos M, Gallego J, Marti-Febregas J, Segura T, et al. The URICO-ICTUS study, a phase 3 study of combined treatment with uric acid and rtPA administered intravenously in acute ischaemic stroke patients within the first 4.5 h of onset of symptoms. Int J Stroke. 2010;5:325–8. doi: 10.1111/j.1747-4949.2010.00448.x. [DOI] [PubMed] [Google Scholar]
- Holthoff JH, Woodling KA, Doerge DR, Burns ST, Hinson JA, Mayeux PR. Resveratrol, a dietary polyphenolic phytoalexin, is a functional scavenger of peroxynitrite. Biochem Pharmacol. 2010;80:1260–5. doi: 10.1016/j.bcp.2010.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin JA, Lee H, Lim YK, Koh Y, Choi JH, Park EM. Therapeutic effects of resveratrol during acute periods following experimental ischemic stroke. J Neuroimmunol. 2010;227:93–100. doi: 10.1016/j.jneuroim.2010.06.017. [DOI] [PubMed] [Google Scholar]
- Wang Q, Xu J, Rottinghaus GE, Simonyi A, Lubahn D, Sun GY, et al. Resveratrol protects against global cerebral ischemic injury in gerbils. Brain Res. 2002;958:439–47. doi: 10.1016/s0006-8993(02)03543-6. [DOI] [PubMed] [Google Scholar]
- Dohare P, Garg P, Jain V, Nath C, Ray M. Dose dependence and therapeutic window for the neuroprotective effects of curcumin in thromboembolic model of rat. Behav Brain Res. 2008;193:289–97. doi: 10.1016/j.bbr.2008.06.012. [DOI] [PubMed] [Google Scholar]
- Suzuki M, Tabuchi M, Ikeda M, Umegaki K, Tomita T. Protective effects of green tea catechins on cerebral ischemic damage. Med Sci Monit. 2004;10:BR166–74. [PubMed] [Google Scholar]
- Kerry N, Rice-Evans C. Peroxynitrite oxidises catechols to o-quinones. FEBS Lett. 1998;437:167–71. doi: 10.1016/s0014-5793(98)01223-x. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Fang SH, Ye YL, Chu LS, Zhang WP, Wang ML, et al. Caffeic acid ameliorates early and delayed brain injuries after focal cerebral ischemia in rats. Acta Pharmacol Sin. 2006;27:1103–10. doi: 10.1111/j.1745-7254.2006.00406.x. [DOI] [PubMed] [Google Scholar]
- Estevez AY, Pritchard S, Harper K, Aston JW, Lynch A, Lucky JJ, et al. Neuroprotective mechanisms of cerium oxide nanoparticles in a mouse hippocampal brain slice model of ischemia. Free Radic Biol Med. 2011;51:1155–63. doi: 10.1016/j.freeradbiomed.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Koizumi H, Fujisawa H, Suehiro E, Shirao S, Suzuki M. Neuroprotective effects of ebselen following forebrain ischemia: involvement of glutamate and nitric oxide. Neurol Med Chir (Tokyo) 2011;51:337–43. doi: 10.2176/nmc.51.337. [DOI] [PubMed] [Google Scholar]
- Yoshida H, Yanai H, Namiki Y, Fukatsu-Sasaki K, Furutani N, Tada N. Neuroprotective effects of edaravone: a novel free radical scavenger in cerebrovascular injury. CNS Drug Rev. 2006;12:9–20. doi: 10.1111/j.1527-3458.2006.00009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banno M, Mizuno T, Kato H, Zhang G, Kawanokuchi J, Wang J, et al. The radical scavenger edaravone prevents oxidative neurotoxicity induced by peroxynitrite and activated microglia. Neuropharmacology. 2005;48:283–90. doi: 10.1016/j.neuropharm.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Lu Q, Xia N, Xu H, Guo L, Wenzel P, Daiber A, et al. Betulinic acid protects against cerebral ischemia-reperfusion injury in mice by reducing oxidative and nitrosative stress. Nitric Oxide. 2011;24:132–8. doi: 10.1016/j.niox.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Gilad E, Cuzzocrea S, Zingarelli B, Salzman AL, Szabo C. Melatonin is a scavenger of peroxynitrite. Life Sci. 1997;60:PL169–74. doi: 10.1016/s0024-3205(97)00008-8. [DOI] [PubMed] [Google Scholar]
- Pei Z, Pang SF, Cheung RT. Administration of melatonin after onset of ischemia reduces the volume of cerebral infarction in a rat middle cerebral artery occlusion stroke model. Stroke. 2003;34:770–5. doi: 10.1161/01.STR.0000057460.14810.3E. [DOI] [PubMed] [Google Scholar]
- Lapchak PA. A critical assessment of edaravone acute ischemic stroke efficacy trials: is edaravone an effective neuroprotective therapy. Expert Opin Pharmacother. 2010;11:1753–63. doi: 10.1517/14656566.2010.493558. [DOI] [PMC free article] [PubMed] [Google Scholar]