Abstract
The skin is a complex organ involved in thermoregulation, gas exchange, protection against pathogens, and barrier function to maintain proper hydration. When dry, the ability for skin to execute these tasks becomes impaired. Dry skin affects almost everyone as we age, but it is also dependent on external factors, such as dry climate, colder temperatures, and repeated washing. In addition, increasing evidence has shown racial variability in the physiological properties of skin, which directly impacts water content of the stratum corneum and sensitivity to exogenously applied agents. A multitude of products have been developed to treat dry skin, and as a group, moisturizers have been designed to either impart or restore hydration in the stratum corneum. Given the large number of moisturizers presently available, depending on individual components, several different mechanisms may be employed to promote skin hydration. As there exists dramatic racial variability in skin properties, certain moisturizers may thus be more effective in some and less effective in others to treat the common condition of dry skin.
Dry skin occurs worldwide, with increasing frequency as we age.1,2 Common sites of involvement include the shins, lower flanks, and posterior axillary line, but in more severe cases, the face and neck may also be affected. Dry skin, also known as xerosis cutis or asteatosis, can result in a rough, scaly quality to the skin. When mild, it can be relatively asymptomatic, but when more pronounced, it may be associated with inflammation and superficial cracking causing unpleasant itching, stinging, and general discomfort.3 In theory, any break in the skin barrier can potentially predispose patients to cutaneous infections. Dry skin has long been noted to be linked to various exogenous factors, such as dry climates, colder winter months, and excessive showering or bathing.4,5 Other factors, such as exposure to various alkali and detergents, particularly in patients with dispositional skin irritability, can serve as a trigger or worsen the ability for skin to maintain moisture.
While ambient and lifestyle factors have been strongly associated with severity of dry skin, various endogenous factors have also gained attention. Malnutrition, renal insufficiency, and hereditary conditions, such as ichthyosis vulgaris and atopy, may also contribute to loss of skin moisture.1 Along these lines, racial differences in skin properties may also explain some of the disparity in dry skin and may provide insight into differences in management for this dermatological disorder. Recent studies have now elucidated multiple racial variations in anatomical and physiological qualities, which, not surprisingly, may alter a disease process or treatment approach.6 With respect to dry skin, racial differences in water loss, water content, lipid content, and skin reactivity have been correlated with disease severity.6
Treatment of dry skin involves the elimination of aggravating factors, and when unrelenting, may sometimes require a course of topical corticosteroid treatment.1 More commonly, though, attention to proper skin care with regular use of moisturizers is stressed.3,4 However, the marketplace is flooded with a great number of products, each containing different components, and selection of the most effective moisturizer may be difficult. Furthermore, given the physiological variations in skin among different races, an ideal moisturizer for one patient may be less useful for another. As billions of dollars are spent yearly on these products, a better understanding of how moisturizers work is thus critical.4 This review will therefore focus on the pathogenesis of dry skin, racial differences in skin properties, and how these may impact selection of an optimal strategy to maintain skin moisture.
PATHOGENESIS OF DRY SKIN
Dry skin occurs worldwide and may affect patients of all ages, but it can probably be found in almost all patients over the age of 60.1,7,8 Skin barrier function resides primarily within the top layer of the epidermis, also known as the stratum corneum or “horny layer.” While important for thermoregulation, gas exchange, and protection against pathogens, this external-most layer also serves to maintain proper hydration.9-11 At birth, the water-handling properties of infant skin are unique and distinct from adults. Though considerably drier during the first month of life, over the next two years, water content in the skin significantly increases, and the stratum corneum that is initially rough becomes far smoother.12-15 This occurs despite lower production levels of sebum and natural moisturizing factor (NMF), a hydroscopic mixture of amino acids, urea, and other compounds.1,14
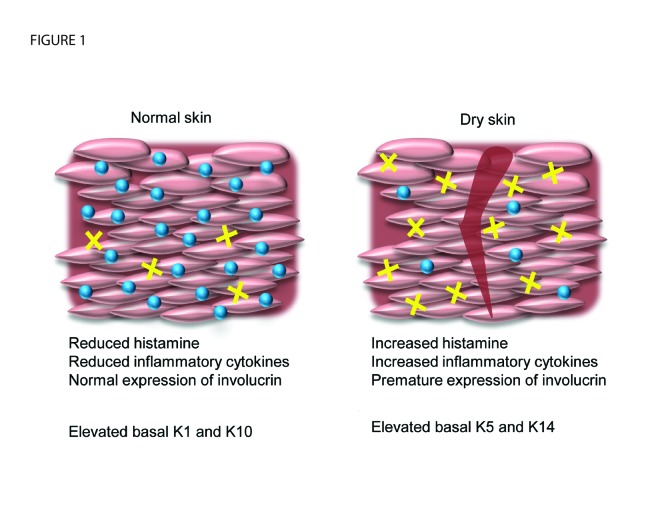
In adults, though deficient production of sebum may contribute to the development of xerosis, a more complex dysfunction of the horny layer is likely responsible for dry skin. By evaluating skin from young and aged patients, Ghadially et al16 found marked abnormalities in barrier integrity and barrier repair associated with dry skin. While the relative distribution of ceramides, cholesterol, and free fatty acids were similar, functional skin changes were attributed to global deficiency in all key stratum corneum lipids, resulting in decreased lamellar bilayers in the stratum corneum interstices with age.16 Studies employing high-performance gas chromatography have also shown altered ratios of fatty acids esterified to ceramide 1, which may increase susceptibility of skin to moisture loss, particularly during drier months.5 In addition, Engelke et al2 reported decreased epidermal prolif-eration in aged, dry skin relative to young, normal skin.2 Significant changes in expression of various keratins were also noted, with decrease in keratins Kl and K10 and increase in basal keratins K5 and K14 detected in dry skin samples.2 Finally, in patients with dry skin, investigations have shown premature expression of involucrin, a protein component that becomes cross-linked to corneo-cyte (the cell type in the stratum corneum) cell membranes, thus increasing cellular stiffness.2,17,18 Collectively, these findings are believed to promote corneo-cyte retention and impair barrier recovery of the horny layer. Furthermore, these physiological changes contribute to reduced water-binding capacity of the skin.
As the stratum corneum dries out, loss of pliability occurs along with formation of small cracks.1 This leaves the skin surface dull, rough, and scaly in appearance. Fine bran-like scales may also be released as powdery clouds during removal of clothing.3 When more advanced, a criss-cross pattern of superficial cracks may be seen appearing like a “dried river bed.” In the most advanced stages, oozing, crusting, and abundant scratch marks can be noted.3 Dry skin may frequently be associated with itching and stinging, both of which may be caused by direct stimulation of cutaneous nerve fibers.1 Symptoms can also be exacerbated by release of histamines and other proinflammatory cytokines secondary to barrier perturbation, mechanical scratching and rubbing, or by the application of irritating or sensitizing substances (Figure 1).1 While mild xerosis may clear within a few days of treatment with moisturizers, more severe cases, such as those seen in atopic patients, may require prolonged therapy with topical corticosteroids. However, in either situation, regular use of occlusives, humectants, emollients, and/or rejuvenators is necessary to minimize relapses.4,19 In addition, use of bath oils and the elimination of factors aggravating dry skin are critical for the treatment of any patient with xerosis.1,20
Figure 1.
Mechanisms of xerosis. Normal skin contains lower levels of histamine and inflammatory cytokines compared to dry skin. Premature expression of involucrin, a protein that forms a protective envelope around corneocytes, has been implicated in the pathophysiology of dry skin. In addition, xerotic skin has been shown to contain higher levels of keratin 5 and 14 and lower levels of keratin 1 and 10 compared to normal skin. The schematic on the right shows the cracked stratum corneum that is characteristic of dry skin and associated with decreased water content (blue spheres) and increased involucrin cross-linking (yellow crosses).
RACIAL DIFFERENCES IN SKIN PROPERTIES
Though dry skin can be found in people of all races, the severity of xerosis can vary quite widely. Because of this, over the past decades several groups have begun attempting to
decipher some of the underlying differences in skin structure and function.21 Most obviously, racial differences in skin color secondary to the presence of melanin has been shown to influence the rate of sun-related skin changes, with Caucasians showing earlier onset of photoaging compared to other subjects.21-23 Many studies have also described the influence of skin pigmentation on the accumulation of natural age-related changes.22,24,25 When considering that the incidence of xerosis increases with maturity, it is therefore not surprising that racial differences in skin properties may significantly influence the ability for skin to retain moisture.24 Unfortunately, many early investigations on the physical and biochemical properties of skin that affect moisture retention were performed primarily on Caucasian skin.6 Furthermore, studies evaluating racial differences have typically been small scale, and in some reports, inter-individual differences related to inconsistencies in anatomical study site were found to be greater than any racial differences observed.6,22 More recent investigations have therefore stressed the use of objective measurements to accurately report racial differences in skin properties. These have included transepidermal water loss, water content, ceramide level, and skin reactivity (Table 1).
TABLE 1.
Differences in racial skin
| TRANSEPIDERMAL WATER LOSS | WATER CONTENT | CERAMIDE LEVEL | SKIN REACTIVITY | |
|---|---|---|---|---|
| Black skin | ++ | + | + | + |
| Caucasian skin | + | ++ | ++ | ++ |
| Asian skin | +++ | +++ | +++ | +++ |
Transepidermal water loss. One of the main roles for the stratum corneum is to maintain an effective barrier against loss of moisture. At any given time, the total amount of water that escapes through the skin is composed of water from imperceptible losses and active sweating.6,26 However, studies focusing on the ability for skin to maintain moisture have relied on evaluation of transepidermal water loss, which has been defined as only the total amount of water vapor loss through skin when there is no sweat gland activity.27 This measure has become one of the most frequently employed determinants of racial skin differences.
Investigations reporting on transepidermal water loss in patients of different races have unfortunately yielded conflicting results, but when collectively interpreting all available data, most studies support some differences between Black, Caucasian, and Asian skin. Using skin harvested from cadavers, Wilson et al28 observed significantly higher transepidermal water loss in African-American skin. By employing an in vitro model, variability in ambient humidity and temperature as well as eccrine sweating could be eliminated. Transepidermal water loss was found to be 2.79μg/cm2/h in Africa-American skin compared to 2.61 μg/cm2/h for Caucasian skin.28 These findings were subsequently confirmed by an in vivo study applying 0.5% and 2.0% sodium lauryl sulfate, a water-soluble irritant, prior to measuring transepidermal water loss.29 In this investigation, Berardesca and Maibach29 determined passive water vapor loss to be 2.7-fold higher in Black skin relative to Caucasian skin.
Contrasting these studies, data regarding transepidermal water loss among Asians have been less conclusive. Comparing skin in similarly aged Japanese and German women, no significant differences could be detected in transepidermal water loss following patch testing on the forearm with 0.25% and 0.5% sodium lauryl sulfate.30 This was similarly noted in a more recent study evaluating other skin sites, including cheek, dorsal hand, and inner arm in Japanese and French patients.31 Interpretation of these data, however, must take into account ambient humidity, which can dramatically alter observations. Contrasting these findings, Kompaore et al reported the highest skin permeability in Asians relative to Black and Caucasians, especially following removal of the stratum corneum by tape stripping.32,33 Rather than directly contradicting previous studies, though, what this observation may demonstrate is that Asian skin has the poorest barrier function upon mechanical challenge. Nonetheless, these data highlight racial differences in skin barrier function, as measured by transepidermal water loss. These findings have important implications for the ability of different skin types to withstand and recover from exogenous insults, absorb topical therapeutic agents, and to maintain moisture under various physiological conditions.
Water content. Investigations measuring skin moisture or hydration have determined water content using a variety of quantitative methods. Skin capacitance, conductance, impedance, and resistance have all been employed, making comparison of different studies challenging. Stratum corneum high in water content is associated with increased capacitance and conductance due to changes in the electrical properties of skin.34 In contrast, dry skin is typically a weak conductor of electricity and thus has been observed to instead have higher resistance and impedance.34
In 1963, Johnson and Corah35 reported on basal skin resistance in both children and adults. Resting levels of skin resistance were measured over a 10-minute interval and average values were used for comparison between Black and Caucasian skin. Interestingly, for both age groups, Black skin had significantly higher galvanic resistance than comparable Caucasian skin. As resistance is inversely related to water content, it can thus be surmised that skin hydration was lower among the Black subjects.35 Of note, site-specific differences in water content have also been described based on measurement of conductance, with variability noted between the dorsal and volar forearm for multiple racial skin types.36 Relative to Black and Caucasian skin, however, few studies have been performed to quantitatively evaluate skin hydration in Asians. The one available comparative study on Asian skin employed an impedance meter to determine water content and demonstrated significantly higher levels of hydration in Asian skin relative to Black and Caucasian skin.37 These data thus highlight significant heterogeneity in water content for different skin types, and emerging studies have begun to link these variations to other components of the stratum corneum, such as ceramides, lactate, and cholesterol.37,38
Ceramlde level. Ceramides are a family of waxy lipids composed of sphingosine and a fatty acid.39 While they are rarely found at greater than trace levels in most tissues, relatively high levels of ceramides reside in the extracellular interstices of the stratum corneum.40-43 At this site, ceramides may be found in concert with cholesterol and other free fatty acids, and it is believed that the ratio of these components may be essential for normal organization and functioning of the epidermal barrier.40,44 Distinctive ceramides in the skin contain long saturated, non-branching alipathic chains that exist in a gel state, which contribute to lower lateral diffusion and permeability of stratum corneum.39,45
Early studies comparing living and cadaveric skin from the abdomen, back, and thigh found Black skin to have slightly higher levels of epidermal lipid and sterol content relative to Caucasian skin.46 These data, however, were limited by a small sample size and the fact that measurements were made from both living and deceased subjects at different anatomical sites.6 More recently, Sugino et al37 measured ceramide levels in the stratum corneum of four different races and found the highest levels to be in Asian skin. Significantly less ceramide was noted in Caucasian skin (20.4±8.1ug/mg) and the lowest level was found in Black skin (10.7±4.7ug/mg). This was similarly observed by Hellemans et al47 who quantified ceramide levels after hydrolysis and analysis of corresponding sphingoid bases, showing the least amount of lipid in the stratum corneum of Black skin. These data therefore demonstrate levels of stratum corneum lipid to correspond to water content and inversely to measured transepidermal water loss. This point is further highlighted by studies on Asians with dry scalp and dandruff, which have confirmed both lower water content and stratum corneum lipids in these patients.48 Enhancing ceramide levels may thus be one key approach to promote moisturization of dry skin.
Skin reactivity. The sensitivity of skin has long been determined qualitatively using erythema as a surrogate measure.6,49,50 However, as this can be difficult to assess in patients with more pigmentation, determination of redness of the skin has proven far too inaccurate. Instead, studies have now employed objective techniques to evaluate blood flow and these have included laser Doppler velocimetry and photoplethysmography. Laser Doppler velocimetry noninvasively measures the Doppler frequency shift of monochromatic laser light backscattered from moving red blood cells while photoplethysmography records pulsatile changes to the skin synchronized with heartbeat through reflection of infrared light.6,51 Using these techniques, studies have shown Black skin to have the lowest skin reactivity. By applying methyl nicotinate to the volar forearm of both Black and Caucasian patients, a 40-percent lower response was noted in Black skin, as measured by photoplethysmography.52 This was similarly appreciated with 0.5% sodium lauryl sulfate, another vasodilator, in which minimal changes to cutaneous blood flow over baseline were reported in Black skin.29 And when a vasoconstrictive stimulus was given, laser Doppler velocimetry also recorded a 40- to 50-percent smaller change to baseline blood flow in Black compared to Caucasian skin.53
Analogous studies have been performed on Asian skin and have shown the greatest skin reactivity to exist in this group. Comparing Black, Caucasian, and Asian patients, Gean et al54 demonstrated the highest increase in blood flow over time among Asian skin following methyl nicotinate application. Using laser Doppler velocimetry, Kompaore et al33 also found the shortest time to vasodilation in Asians, followed by Caucasians, and then Blacks. These reports thus reveal some degree of diversity in blood vessel reactivity and skin sensitivity between different races. While variability exists in the vasoactive substances employed for each study, the findings nonetheless underscore the importance of racial skin types when considering disparities in observed irritation and selection of pharmacological therapies.6
TYPES OF MOISTURIZERS
The stratum corneum is an interactive, dynamic structure, and maintenance of hydration can impact its barrier function. As a group, moisturizers have thus been designed to either impart or restore hydration in the stratum corneum. All moisturizers also help to provide some form of temporary barrier, allowing time for repair of damaged stratum corneum. And by promoting hydration of the stratum corneum, swelling of the outer layers occurs leading to a more smooth skin surface.55,56 A large number of moisturizers are presently available, and collectively, they remain one of the most prescribed products by dermatologists. Several types of ingredients have been described in recent years, some with complex and sophisticated mechanisms, which function to increase water content in the skin. New moisturizers have now also begun to incorporate more natural ingredients, such as botanicals and vitamins.57-59 Nonetheless, components of moisturizers can be grouped into broad categories: humectants, occlusives, emollients, and constituents of natural moisturizing factor/essential proteins (Table 2).60 In addition, the United States Food and Drug Association (FDA) has recently approved new moisturizers, which fall under the class of medical device. While well-defined categories exist for each of these components, to our knowledge, no level I or II studies have been published directly comparing, in a head-to-head fashion, the efficacy of each in the treatment of dry skin.
TABLE 2.
Types of moisturizers
| CLASS | MECHANISM OF ACTION | EXAMPLES |
|---|---|---|
| Humectants | Attract water to the stratum corneum | Glycerin Sorbitol Urea Alpha hydroxy acids Sugars |
| Occlusives | Barrier preventing loss of water | Lanolin Petrolatum Mineral oil Silicones Zinc oxide |
| Emollients | Fills in spaces between corneocytes | Squalene Cholesterol Fatty acids Hyaluronic acid |
| Natural moisturizing factor/essential proteins | Combination of low molecular weight substances which retain water | Amino acids Ammonia Uric acid Glucosamine Creatinine Citrate Organic acids Peptides |
| Nonsteroidal anti-inflammatory | Comparable to low-potency steroid in skin barrier repair | MimyX Cream Atopiclair EpiCeram |
Humectants are substances that attract water when applied to the skin.61 In this manner, they theoretically improve hydration of the stratum corneum. Typical humectants include glycerin, sorbitol, urea, alpha hydroxyacids, and sugars.60 Aside from their hygroscopic properties, some humectants, such as the alpha hydroxy acid ammonium lactate, have also been shown to reduce abnormal thickening of the stratum corneum, increase cohesion between corneocytes, and reduce the appearance of scaling seen in ichthyosis and other hyperkeratotic conditions. Importantly, unless the relative humidity is very high, the source of water for topical humectants is transepidermal and not atmospheric. Therefore, continued evaporation from the skin can exacerbate dryness and lead to a perception of tightness. High concentrations of some humectants, such as urea, glycerin, and propylene glycol, may also be irritating and should be generally avoided in Asian patients with more sensitive skin.62
Occlusives physically block transepidermal water loss in the stratum corneum and help to maintain water content.60,63 Lanolin was one of the first substances to be used as an occlusive and has long been employed as a moisturizer on its own. It is composed of a mix of esters, diesters, high molecular weight hydroxyesters, lanolin alcohols, and lanolin acids. However, while lanolin can be quite effective in minimizing water loss, it has also been associated with contact dermatitis.62 Because of this, use of lanolin should be limited to patients with less reactive skin.64 In place of lanolin, petrolatum has become the principal ingredient used in various moisturizers. Importantly though, with more recent health and environmental concerns being raised regarding derivation of petrolatum from petroleum, alternative occlusives have also been developed, including mineral oil, dimethicone, and zinc oxide. Some of these occlusives also possess an emollient effect, further enhancing its ability to improve overall quality of the skin.
Emollients are frequently incorporated into moisturizers to smooth skin through filling of spaces between the corneocytes. While not usually occlusive, when applied heavily, emollients may also function as a barrier to water loss. They are composed of water-in-oil emulsions, with an oil component ranging from 3 to 25 percent.65 The concentration of oil affects both ease of spread and degree of occlusion.65 Typical emollients used in moisturizers include squalene, cholesterols, and fatty acids. Squalene is a natural organic compound derived from shark liver oil, amaranth seed, wheat germ, or olives.66 When used commercially, squalene is typically hydrogenated to generate a saturated derivative known as squalane, which is less susceptible to oxidation.66,67 At concentrations used in moisturizers, both squalene and squalane have been shown to have little irritant or sensitizer effects.68,69 These may thus be effective in promoting hydration in Asian patients with more sensitive skin. Other emollients include mineral oil and lanolin, which as mentioned above, may also function as occlusives. Synthetic ceramides have also become commercially available and have been shown to be effective in improving dry skin.70 CeraVe® (Valeant Pharmaceuticals North America LLC) is one particular moisturizer that incorporates multiple emollients, including ceramides, cholesterols, and fatty acids. Finally, for patients with more oily skin, oil-free emollient products have been developed containing propylene glycol or glycerin. As expected, both of these have a drying effect and can cause stinging when applied to irritated or sensitive skin.
The term natural moisturizing factor was first coined by Jacobi et al in 1959.71,72 While not universally adopted at first, multiple studies have described similar compounds found in the epidermis in which removal decreased skin hydration.73-75 The NMF contains a combination of several naturally occurring free amino acids, urocanic acid, inorganic salts, sugars, lactic acid, and urea.76 Many of these are highly efficient at attracting and binding water from the atmosphere, allowing adequate hydration of corneocytes even in low humidity environments. Much of the NMF is derived from breakdown of filaggrin, a large histidine-rich protein in newly formed corneocytes involved in aligning keratin filaments.77 Routine washing of skin has been shown to decrease the NMF, and reduced NMF levels have been found in patients with xerosis.78 Because of this, many moisturizers now incorporate various components of the NMF to enhance its hygroscopic properties. Cetaphil® Restoraderm® (Galderma, Fort Worth, Texas) is one commonly used moisturizer incorporating both filaggrin and ceramides. In addition, some moisturizers include essential proteins, such as keratin and elastin. While they may provide some temporary relief through an emollient effect, these proteins are too large to penetrate deeply and they are likely to have minimal effectiveness as moisturizers alone.
The last group of moisturizers include a new class of compounds recently approved by the FDA as medical devices. This includes MimyX Cream (Stiefel Laboratories, Inc., Research Triangle Park, North Carolina), Atopiclair® (Sinclair IS Pharma, London, United Kingdom), and EpiCeram® (Ceragenix Pharmaceuticals, Inc. Denver, Colorado), all prescription nonsteroidal anti-inflammatory creams designed for dry, atopic skin.79-81 MimyX Cream contains palmitoylethanolamide, a bioactive fat deficient in patients with atopic dermatitis.81 While this may contribute to an emollient effect, MimyX Cream has also been described to have an anti-inflammatory effect comparable to low-potency steroids while lacking any steroidal or calcineurin-inhibitor properties.81 This allows for skin barrier function repair and improvement in water content. Similar to MimyX Cream, Atopiclair® contains no medically active ingredients, but functions as a hydrophilic cream. It is a mix of hyaluronic acid, telmesteine, and glycyrrhetinic acid.79,80 In recent double-blinded studies, patients found Atopiclair offers significant benefits over vehicle-only controls and reduced the total body area affected by atopic dermatitis.82,83 Finally, EpiCeram® is a topical nonsteroidal skin cream containing ceramides, free fatty acids, and cholesterol. Approved as a prescription medical device by the FDA, EpiCeram has been shown in a multi-center, randomized, blinded study to have similar efficacy as fluticasone cream for the treatment of atopic dermatitis.84 Based on these findings, MimyX Cream, Atopiclair, and EpiCeram can all be considered as treatment options, specifically in patients with dry skin secondary to atopic dermatitis. However, as each have been approved as a medical device instead of a drug, they have been less rigorously studied, and data comparing clinical efficacy and safety are limited.80
CONCLUSION
Dry skin is a common problem worldwide and can affect almost everyone as the global population ages. Superficial cracking, itching, and stinging can result in general discomfort, and severity has been linked to multiple exogenous factors, such as dry climates, colder winter months, and excessive showering or bathing. However, as the physiological properties of skin differ widely between races, it is therefore not surprising that given the same external environment, dry skin can be more problematic for some patients. While studies continue to delve deeper into the racial variability of skin, quantifiable parameters have been developed showing differences in transepidermal water loss, water content, ceramide levels, and skin reactivity between Caucasian, Black, and Asian subjects. Although the marketplace is flooded with a diverse array of commercial products, ongoing research in skin moisturizers and ethnic differences in skin biology may allow clinicians to develop targeted, patient-specific regimens to treat dry skin.
Footnotes
DISCLOSURE:The authors report no relevant conflicts of interest.
REFERENCES
- 1.Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 3rd ed. Mosby: New York; 2012. [Google Scholar]
- 2.Engelke M, et al. Effects ol xerosis and aging on epidermal proliferation and differentiation. Br J Dermatol. 1997;137(2):219–225. doi: 10.1046/j.1365-2133.1997.18091892.x. [DOI] [PubMed] [Google Scholar]
- 3.Andriessen A. Prevention, recognition and treatment of dry skin conditions. Br J Nurs. 2013;22(1):26–30. doi: 10.12968/bjon.2013.22.1.26. [DOI] [PubMed] [Google Scholar]
- 4.Guenther L, et al. Pathway to dry skin prevention and treatment. J Cutan Med Surg. 2012;16(1):23–31. doi: 10.1177/120347541201600106. [DOI] [PubMed] [Google Scholar]
- 5.Rogers J, et al. Stratum corneum lipids: the effect of aging and the seasons. Arch Dermatol Res. 1996;288(12):765–770. doi: 10.1007/BF02505294. [DOI] [PubMed] [Google Scholar]
- 6.Wesley NO, Maibach HI. Racial (ethnic) differences in skin properties: the objective data. Am J Clin Dermatol. 2003;4(12):843–860. doi: 10.2165/00128071-200304120-00004. [DOI] [PubMed] [Google Scholar]
- 7.Seyfarth F, et al. Dry skin, barrier function, and irritant contact dermatitis in the elderly. Clin Dermatol. 2011;29(1):31–36. doi: 10.1016/j.clindermatol.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 8.White-Chu EF, Reddy M. Dry skin in the elderly: complexities of a common problem. Clin Dermatol. 2011;29(1):37–42. doi: 10.1016/j.clindermatol.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Meyer-Hoffert U, et al. Flagellin delivery by Pseudomonas aeruginosa rhamnolipids induces the antimicrobial protein psoriasin in human skin. PLoS One. 2011;6(1):el6433. doi: 10.1371/journal.pone.0016433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Telofski LS, Morello AP, Mack Correa MC, et al. The infant skin barrier: can we preserve, protect, and enhance the barrier? Dermatol Res Pract. 2012:198789. doi: 10.1155/2012/198789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larson AA, Dinulos JG. Cutaneous bacterial infections in the newborn. Curr Opin Pediatr. 2005;17(4):481–485. doi: 10.1097/01.mop.0000171321.68806.bd. [DOI] [PubMed] [Google Scholar]
- 12.Visscher MO, et al. Changes in diapered and nondiapered infant skin over the first month of life. Pediatr Dermatol. 2000;17(1):45–51. doi: 10.1046/j.1525-1470.2000.01711.x. [DOI] [PubMed] [Google Scholar]
- 13.Saijo S, Tagami H. Dry skin of newborn infants: functional analysis of the stratum corneum. Pediatr Dermatol. 1991;8(2):155–159. doi: 10.1111/j.1525-1470.1991.tb00308.x. [DOI] [PubMed] [Google Scholar]
- 14.Hoeger PH, Enzmann CC. Skin physiology of the neonate and young infant: a prospective study of functional skin parameters during early infancy. Pediatr Dermatol. 2002;19(3):256–262. doi: 10.1046/j.1525-1470.2002.00082.x. [DOI] [PubMed] [Google Scholar]
- 15.Giusti F, et al. Skin barrier, hydration, and pH of the skin of infants under 2 years of age. Pediatr Dermatol. 2001;18(2):93–96. doi: 10.1046/j.1525-1470.2001.018002093.x. [DOI] [PubMed] [Google Scholar]
- 16.Ghadially R, et al. The aged epidermal permeability barrier. Structural, functional, and lipid biochemical abnormalities in humans and a senescent murine model. J Clin Invest. 1995;95(5):2281–2290. doi: 10.1172/JCI117919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eckert RL, Green H. Structure and evolution of the human involucrin gene. Cell. 1986;46(4):583–589. doi: 10.1016/0092-8674(86)90884-6. [DOI] [PubMed] [Google Scholar]
- 18.Eckert RL, et al. Involucrin—structure and role in envelope assembly. J Invest Dermatol. 1993;100(5):613–617. doi: 10.1111/1523-1747.ep12472288. [DOI] [PubMed] [Google Scholar]
- 19.Dyble T, Ashton J. Use of emollients in the treatment of dry skin conditions. Br J Community Nurs. 2011;16(5) doi: 10.12968/bjcn.2011.16.5.214. 214,216,218. [DOI] [PubMed] [Google Scholar]
- 20.Casetti F, et al. Dermocosmetics for dry skin: a new role for botanical extracts. Skin Pharmacol Physiol. 2011;24(6):289–293. doi: 10.1159/000329214. [DOI] [PubMed] [Google Scholar]
- 21.Weigand DA, Haygood C, Gaylor JR. Cell layers and density of Negro and Caucasian stratum corneum. J Invest Dermatol. 1974;62(6):563–568. doi: 10.1111/1523-1747.ep12679412. [DOI] [PubMed] [Google Scholar]
- 22.Rawlings AV. Ethnic skin types: are there differences in skin structure and function? Int J Cosmet Sci. 2006;28(2):79–93. doi: 10.1111/j.1467-2494.2006.00302.x. [DOI] [PubMed] [Google Scholar]
- 23.Riley PA. Melanogenesis and melanoma. Pigment Cell Res. 2003;16(5):548–552. doi: 10.1034/j.1600-0749.2003.00069.x. [DOI] [PubMed] [Google Scholar]
- 24.Taylor SC. Skin of color: biology, structure, function, and implications for dermatologic disease. J Am Acad Dermatol. 2002;46(2 Suppl Understanding):S41–S62. doi: 10.1067/mjd.2002.120790. [DOI] [PubMed] [Google Scholar]
- 25.Freeman RG, et al. Sunlight as a factor influencing the thickness of epidermis. J Invest Dermatol. 1962;39:295–298. doi: 10.1038/jid.1962.115. [DOI] [PubMed] [Google Scholar]
- 26.Elsner P. Bioengineering of the Skin: Skin Biomechanics. Vol. 5. CRC Press; Boca Raton, FL: 2002. ed; p. 296. [Google Scholar]
- 27.Rothman S, editor. Physiology and Biochemistry of the Skin. 2nd ed. University Press; Chicago, IL: 1954. p. 741. [Google Scholar]
- 28.Wilson D, Berardesca E, Maibach HI. In vivo transepidermal water loss and skin surface hydration in assessment of moisturization and soap effects. Int J Cosmet Sci. 1988;10(5):201–211. doi: 10.1111/j.1467-2494.1988.tb00018.x. [DOI] [PubMed] [Google Scholar]
- 29.Berardesca E, Maibach HI. Racial differences in sodium lauryl sulphate induced cutaneous irritation: black and white Contact. Dermatitis. 1988;18(2):65–70. doi: 10.1111/j.1600-0536.1988.tb02741.x. [DOI] [PubMed] [Google Scholar]
- 30.Aramaki J, et al. Differences of skin irritation between Japanese and European women. Br J Dermatol. 2002;146(6):1052–1056. doi: 10.1046/j.1365-2133.2002.04509.x. [DOI] [PubMed] [Google Scholar]
- 31.Yamashita Y, et al. Differences in susceptibility to oxidative stress in the skin of Japanese and French subjects and physiological characteristics of their skin. Skin Pharmacol Physiol. 2012;25(2):78–85. doi: 10.1159/000335259. [DOI] [PubMed] [Google Scholar]
- 32.Kompaore F, Tsuruta H. In vivo differences between Asian, black and white in the stratum corneum barrier function. Int Arch Occup Environ Health. 1993;65(1 Suppl):S223–S225. doi: 10.1007/BF00381346. [DOI] [PubMed] [Google Scholar]
- 33.Kompaore F, Marty JP, Dupont C. In vivo evaluation of the stratum corneum barrier function in blacks, Caucasians and Asians with two noninvasive methods. Skin Pharmacol. 1993;6(3):200–207. doi: 10.1159/000211136. [DOI] [PubMed] [Google Scholar]
- 34.Berardesca E, et al., editors. Bioengineering of the Skin: Methods and Instrumentation. 1st ed. CRC Press, Inc.; Boca Raton, FL: 1995. [Google Scholar]
- 35.Johnson LC, Corah NL. Racial differences in skin resistance. Science. 1963;139(3556):766–767. doi: 10.1126/science.139.3556.766. [DOI] [PubMed] [Google Scholar]
- 36.Berardesca E, et al. In vivo biophysical characterization of skin physiological differences in races. Dermatologica. 1991;182(2):89–93. doi: 10.1159/000247752. [DOI] [PubMed] [Google Scholar]
- 37.Sugino K, Imokawa G, Maibach HI. Ethnic difference of stratum corneum lipid in relation to stratum corneum function. J Invest Dermatol. 1993;100(4):587. [Google Scholar]
- 38.Egawa M, Tagami H. Comparison of the depth profiles of water and water-binding substances in the stratum corneum determined in vivo by Raman spectroscopy between the cheek and volar forearm skin: effects of age, seasonal changes and artificial forced hydration. Br J Dermatol. 2008.;158(2):251–260. doi: 10.1111/j.1365-2133.2007.08311.x. [DOI] [PubMed] [Google Scholar]
- 39.Tashiro T, Mori K. Synthesis of sphingolipids with an omega-esterified long acyl chain, ceramide components of the human epidermis. Biosci Biotechnol Biochem. 2012;76(9):1715–1720. doi: 10.1271/bbb.120333. [DOI] [PubMed] [Google Scholar]
- 40.Ishikawa J, Shimotoyodome Y, Ito S, et al. Variations in the ceramide profile in different seasons and regions of the body contribute to stratum corneum functions. Arch Dermatol Res. 2013;305:151–162. doi: 10.1007/s00403-012-1286-5. [DOI] [PubMed] [Google Scholar]
- 41.Elias PM. Structure and function of the stratum corneum extracellular matrix. J Invest Dermatol. 2012;132(9):2131–2133. doi: 10.1038/jid.2012.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goldstein AM, Abramovits W. Ceramides and the stratum corneum: structure, function, and new methods to promote repair. Int J Dermatol. 2003;42(4):256–259. doi: 10.1046/j.1365-4362.2003.01507.x. [DOI] [PubMed] [Google Scholar]
- 43.Wartewig S, Neubert RH. Properties of ceramides and their impact on the stratum corneum structure: a review. Part 1: ceramides. Skin Pharmacol Physiol. 2007;20(5):220–229. doi: 10.1159/000104420. [DOI] [PubMed] [Google Scholar]
- 44.Mcintosh TJ. Organization of skin stratum corneum extracellular lamellae: diffraction evidence for asymmetric distribution of cholesterol. Biophys J. 2003;85(3):1675–1681. doi: 10.1016/S0006-3495(03)74597-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Janssens M, et al. Increase in short-chain ceramides correlates with an altered lipid organization and decreased barrier function in atopic eczema patients. J Lipid Res. 2012;53(12):2755–2766. doi: 10.1194/jlr.P030338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reinertson RP, Wheatley VR. Studies on the chemical composition of human epidermal lipids. J Invest Dermatol. 1959;32(1):49–59. [PubMed] [Google Scholar]
- 47.Hellemans L, et al. Characterization of stratum corneum properties in human subjects from a different ethnic background. J Invest Dermatol. 2005;124(S4):A62. [Google Scholar]
- 48.Harding CR, et al. Dandruff: a condition characterized by decreased levels of intercellular lipids in scalp stratum corneum and impaired barrier function. Arch Dermatol Res. 2002;294(5):221–230. doi: 10.1007/s00403-002-0323-1. [DOI] [PubMed] [Google Scholar]
- 49.Weigand DA, Gaylor JR. Irritant reaction in Negro and Caucasian skin. South Med J. 1974;67(5):548–551. doi: 10.1097/00007611-197405000-00013. [DOI] [PubMed] [Google Scholar]
- 50.Basketter DA, et al. Individual, ethnic and seasonal variability in irritant susceptibility of skin: the implications for a predictive human patch test. Contact Dermatitis. 1996;35(4):208–213. doi: 10.1111/j.1600-0536.1996.tb02359.x. [DOI] [PubMed] [Google Scholar]
- 51.Yamamoto Y, Oberg PA. Measurement of digital blood flow using the laser Doppler, impedance and strain-gauge methods. Med BiolEng Comput. 1990;28(2):113–118. doi: 10.1007/BF02441765. [DOI] [PubMed] [Google Scholar]
- 52.Guy RH, et al. Are there age and racial differences to methyl nicotinate-induced vasodilatation in human skin? J Am Acad Dermatol. 1985;12(6):1001–1006. doi: 10.1016/s0190-9622(85)70128-4. [DOI] [PubMed] [Google Scholar]
- 53.Berardesca E, Maibach H. Cutaneous reactive hyperaemia: racial differences induced by corticoid application. Br J Dermatol. 1989;120(6):787–794. doi: 10.1111/j.1365-2133.1989.tb01376.x. [DOI] [PubMed] [Google Scholar]
- 54.Gean CJ, et al. Cutaneous responses to topical methyl nicotinate in black, oriental, and Caucasian subjects. Arch Dermatol Res. 1989;281(2):95–98. doi: 10.1007/BF00426585. [DOI] [PubMed] [Google Scholar]
- 55.Crowther JM, et al. Measuring the effects of topical moisturizers on changes in stratum corneum thickness, water gradients and hydration in vivo. Br J Dermatol. 2008;159(3):567–577. doi: 10.1111/j.1365-2133.2008.08703.x. [DOI] [PubMed] [Google Scholar]
- 56.Jackson EM. Facial moisturizers and wrinkles. Dermatol Nurs. 1992;4(3):205–207. [PubMed] [Google Scholar]
- 57.Udompataikul M, Srisatwaja W. Comparative trial of moisturizer containing licochalcone A vs. hydrocortisone lotion in the treatment of childhood atopic dermatitis: a pilot study. J Eur Acad Dermatol Venereal. 2011;25(6):660–665. doi: 10.1111/j.1468-3083.2010.03845.x. [DOI] [PubMed] [Google Scholar]
- 58.Tucker-Samaras S, et al. A stabilized 0.1% retinol facial moisturizer improves the appearance of photodamaged skin in an eight-week, double-blind, vehicle-controlled study. J Drags Dermatol. 2009;8(10):932–936. [PubMed] [Google Scholar]
- 59.Gonullu U, et al. Moisturizing potentials of ascorbyl palmitate and calcium ascorbate in various topical formulations. Int J Gosmet Sci. 2004;26(1):31–36. doi: 10.1111/j.0142-5463.2004.00202.x. [DOI] [PubMed] [Google Scholar]
- 60.Draelos ZD. Active agents in common skin care products. Plast Reconstr Surg. 2010;125(2):719–724. doi: 10.1097/PRS.0b013e3181c83192. [DOI] [PubMed] [Google Scholar]
- 61.Sagiv AE, Dikstein S, Ingber A. The efficiency of humectants as skin moisturizers in the presence of oil. Skin Res Technol. 2001;7(1):32–35. doi: 10.1034/j.1600-0846.2001.007001032.x. [DOI] [PubMed] [Google Scholar]
- 62.Zirwas MJ, Stechschulte SA. Moisturizer allergy: diagnosis and management. J Clin Aesthet Dermatol. 2008;1(4):38–44. [PMC free article] [PubMed] [Google Scholar]
- 63.Ghadially R, Halkier-Sorensen L, Elias PM. Effects of petrolatum on stratum corneum structure and function. J Am Acad Dermatol. 1992;26(3 Pt 2):387–396. doi: 10.1016/0190-9622(92)70060-s. [DOI] [PubMed] [Google Scholar]
- 64.Wehr RF, Krochmal L. Considerations in selecting a moisturizer. Cutis. 1987;39(6):512–515. [PubMed] [Google Scholar]
- 65.Savary G, Grisel M, Picard C. Impact of emollients on the spreading properties of cosmetic products: a combined sensory and instrumental characterization. Colloids Surf B Biointerfaces. 2013;102:371–378. doi: 10.1016/j.colsurfb.2012.07.028. [DOI] [PubMed] [Google Scholar]
- 66.Kim SK, Karadeniz F. Biological importance and applications of squalene and squalane. 4cfo. Food Nutr Res. 2012;65:223–233. doi: 10.1016/B978-0-12-416003-3.00014-7. [DOI] [PubMed] [Google Scholar]
- 67.Wei A, Shibamoto T. Antioxidant activities of essential oil mixtures toward skin lipid squalene oxidized by UV irradiation. Cutan Ocul Toxicol. 2007;26(3):227–233. doi: 10.1080/15569520701224501. [DOI] [PubMed] [Google Scholar]
- 68.Kato S, et al. Biological safety of LipoFullerene composed of squalane and fullerene-C60 upon mutagenesis, photocytotoxicity, and permeability into the human skin tissue. Basic Clin Pharmacol Toxicol. 2009;104(6):483–487. doi: 10.1111/j.1742-7843.2009.00396.x. [DOI] [PubMed] [Google Scholar]
- 69.Busch J. Final report on the safety assessment of squalane and squalene. Int J Toxicol. 1982;1(2):37–56. [Google Scholar]
- 70.Simpson E, et al. Improvement of skin barrier function in atopic dermatitis patients with a new moisturizer containing a ceramide precursor. J Dermatolog Treat. doi: 10.3109/09546634.2012.713461. 2012 Sep 9 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 71.Jacobi OT. About the mechanism of moisture regulation in the horny layer of the skin. Proc Sci Sect Toilet Goods Assoc. 1959;31:22–24. [Google Scholar]
- 72.Imokawa G, Hattori M. A possible function of structural lipids in the water-holding properties of the stratum corneum. J Invest Dermatol. 1985;84:282–284. doi: 10.1111/1523-1747.ep12265365. [DOI] [PubMed] [Google Scholar]
- 73.Spier HW, Pascher G. [The water-soluble components of the peripheral horny layer of the skin (skin surface); quantitative analyses. II. Nitrogen-free acids and bases; water-soluble total sulfur] Arch Klin Exp Dermatol. 1955;201(2):181–192. [PubMed] [Google Scholar]
- 74.Spier HW, Pascher G. [The water soluble elements of the peripheral horny layers of the skin (skin surface); quantitative analysis. I. General comments. Nitrogen containing substances] Arch Klin Exp Dermatol. 1955;199(5):411–427. [PubMed] [Google Scholar]
- 75.Bolliger A, Gross R. Water soluble compounds (non-keratins) associated with the skin flakes of the human scalp. Aust J Exp Biol Med Sci. 1956;34(3):219–224. doi: 10.1038/icb.1956.26. [DOI] [PubMed] [Google Scholar]
- 76.Harding CR, et al. Dry skin, moisturization and corneodesmolysis. Int J Cosmet Sci. 2000;22(1):21–52. doi: 10.1046/j.1467-2494.2000.00001.x. [DOI] [PubMed] [Google Scholar]
- 77.Scott IR, Harding CR, Barrett JG. Histidine-rich protein of the keratohyalin granules. Source of the free amino acids, urocanic acid and pyrrolidone carboxylic acid in the stratum corneum. Biochim Biophys Acta. 1982;719(1):110–117. doi: 10.1016/0304-4165(82)90314-2. [DOI] [PubMed] [Google Scholar]
- 78.Jacobson TM, et al. Effects of aging and xerosis on the amino acid composition of human skin. J Invest Dermatol. 1990;95(3):296–300. doi: 10.1111/1523-1747.ep12484970. [DOI] [PubMed] [Google Scholar]
- 79.Patrizi A, Raone B, Neri I. Atopiclair. Expert Opin Pharmacother. 2009;10(7):1223–1230. doi: 10.1517/14656560902926106. [DOI] [PubMed] [Google Scholar]
- 80.Simpson EL. Atopic dermatitis: a review of topical treatment options. Curr Med Res Opin. 2010;26(3):633–640. doi: 10.1185/03007990903512156. [DOI] [PubMed] [Google Scholar]
- 81.Kircik L. A nonsteroidal lamellar matrix cream containing palmitoylethanolamide for the treatment of atopic dermatitis. J Drugs Dermatol. 2010;9(4):334–338. [PubMed] [Google Scholar]
- 82.Belloni G, Pinelli S, Veraldi S. A randomised, double-blind, vehicle-controlled study to evaluate the efficacy and safety of MAS063D (Atopiclair) in the treatment of mild to moderate atopic dermatitis. Eur J Dermatol. 2005;15(1):31–36. [PubMed] [Google Scholar]
- 83.Abramovits W, et al. Patient-reported outcomes from a multicenter, randomized, vehicle-controlled clinical study of MAS063DP (Atopiclair) in the management of mild-to-moderate atopic dermatitis in adults. J Dermatolog Treat. 2008;19(6):327–332. doi: 10.1080/09546630802232799. [DOI] [PubMed] [Google Scholar]
- 84.Sugarman JL, Parish LC. Efficacy of a lipid-based barrier repair formulation in moderate-to-severe pediatric atopic dermatitis. J Drugs Dermatol. 2009;8(12):1106–1111. [PubMed] [Google Scholar]