Abstract
Purpose
We recently reported an increasing risk over time of hospitalization among Medicare participants after undergoing an initial prostate biopsy. Less is known about the relative risks of repeat prostate biopsies, which are frequently performed in prostate cancer screening and in active surveillance programs. We determined whether repeat biopsies are associated with an increased risk of hospitalization compared to the initial biopsy.
Materials and Methods
Using SEER (Surveillance, Epidemiology and End Results)-Medicare linked data from 1991 to 2007 we identified 13,883 men who underwent a single prostate biopsy and 3,640 who had multiple biopsies. The 30-day hospitalization rates were compared between these groups, and with a randomly selected control population of 134,977. ICD-9 codes were then used to examine the frequency of serious infectious and noninfectious urological complications as the primary diagnosis for hospital admissions.
Results
Initial and repeat biopsies were associated with a significantly increased risk of hospitalization within a 30-day period compared to randomly selected controls (p <0.0001). However, the repeat biopsy session was not associated with a greater risk of infectious (OR 0.81, 95% 0.49–1.32, p = 0.39) or serious noninfectious urological complications (OR 0.94, 95% CI 0.54–1.62, p = 0.82) compared to the initial biopsy.
Conclusions
Each biopsy was associated with a significant risk of complications compared to randomly selected controls. However, the repeat biopsy procedure itself was not associated with a greater risk of serious complications requiring hospital admission compared to the initial biopsy.
Keywords: prostate, biopsy, infection, hospitalization, patient admission
In 2012 an estimated 241,740 new prostate cancers were diagnosed.1 Many men undergo multiple prostate biopsies in the course of screening, staging and management for prostate cancer.2 Our group previously reported an increase in hospital admissions for infection after an initial prostate biopsy in Medicare participants living in SEER regions.3 Among 17,472 men with an initial prostate biopsy claim from 1991 to 2007, the 30-day hospitalization rates were 2.65-fold higher than among randomly selected controls on multivariable analysis. In addition, there was a significant increase with time in the rate of hospitalizations for biopsy related infections. These observations were possibly attributed to increasing antimicrobial resistance.
A recent study including primarily men undergoing repeat biopsies reported the presence of fluoroquinolone resistant Escherichia coli on 22% of rectal swabs taken before prostate biopsy.4 However, the majority of biopsies did not result in clinical infection. Less has been published about the rates of serious infectious complications among United States men in the repeat biopsy setting. Thus, in this study we determined whether repeat biopsy is associated with a greater risk of complications than initial prostate biopsy.
METHODS
We identified a 5% random sample of male Medicare participants in SEER regions from 1991 to 2007, all of whom were 65 years old or older, and enrolled in Medicare Part A and B for 1 month or more. Carrier or outpatient claims were used to identify individuals who underwent 1 or more transrectal ultrasound guided prostate biopsies using the CPT/HCPCS (Healthcare Common Procedure Coding System) codes 55700 (prostate needle biopsy), or 76872 (transrectal ultrasound) and 76942 (ultrasound guided needle biopsy) together.
For this analysis we considered the first reported claim of a biopsy as the initial biopsy and subsequent claims as repeat biopsies. Men diagnosed with prostate cancer before the initial biopsy were excluded from analysis. As in our prior study,3 we identified a control population of men 65 years old or older in SEER regions enrolled in Medicare Parts A and B for 1 month or more, and selected a random day during their Medicare coverage as a time point for comparison.
As in prior studies we then used ICD-9 codes for hospital admissions within 30 days of prostate biopsy or selection (controls) to examine primary diagnosis codes for biopsy related infectious complications (kidney infection, urinary tract infection, prostatitis, cystitis, sepsis/bacteremia, endocarditis, hypotension and postoperative infection) and noninfectious complications (gastrointestinal hemorrhage, hematuria, acute post-hemorrhagic anemia and urinary symptoms/retention).3 Using these classifications the overall 30-day hospitalization rates were calculated. We also calculated the 30-day rates of hospitalizations for infectious and serious noninfectious biopsy related complications as primary diagnoses.
For the person based analyses we compared the 13,883 men who underwent a single prostate biopsy, 3,640 who had multiple biopsies and 134,977 randomly selected controls. The objective of this analysis was to determine whether men undergoing biopsy (repeat and initial) were more likely to be hospitalized compared to controls from the population after adjusting for potential confounders. Analysis was also performed to examine the 30-day hospitalization rates for men with repeat biopsies performed within 3 years of the initial biopsy, and whether the time between biopsies was associated with hospitalization.
In addition, we performed a biopsy based analysis to determine whether the repeat biopsy procedure itself was more likely to be followed by a serious complication compared to the initial biopsy procedure. For this analysis we compared 17,561 initial biopsies with 5,682 repeat biopsies.
T tests and chi-square tests were used to compare baseline characteristics among groups. Multivariable logistic regression was used to examine the risk of hospitalization, and infectious and noninfectious complications among the initial biopsy, repeat biopsy and control groups, adjusting for age, race, SEER region, year and Charlson comorbidity scores.5 In these models region was classified as midwest/central vs coastal based on prior studies demonstrating regional variation in antimicrobial resistance patterns.6
We also examined 30-day mortality rates in the initial biopsy, repeat biopsy, and control populations. Multivariable analysis (using the same covariates as previously mentioned) was performed to compare 30-day mortality rates between the biopsy and control groups, and between individuals with or without an infectious complication.
RESULTS
The supplementary table (jurology.com) shows the demographics of the study population, including men 65 years old or older from multiple regions across the United States. Men undergoing multiple biopsies during the study period were significantly younger with fewer comorbidities at study entry than the single biopsy or control groups.
In the repeat biopsy group the mean (±SD) number of biopsy procedures was 2.5 (±0.9), separated by an average of 2.7 (±2.3) years (25th percentile 0.95, 75th percentile 3.8). Time between biopsies was not a significant predictor of hospitalization.
In the person based analysis the 30-day hospitalization rates were significantly higher among men undergoing initial and repeat biopsy compared to randomly selected controls (table 1). However, men who underwent biopsy were significantly less likely to die of all causes within 30 days, suggesting the selection of a healthier population for biopsy. Similarly, in a subset analysis of men undergoing repeat biopsy within 3 years, there was a 2.8-fold increase in overall hospitalizations, a 3.9-fold increase in serious infectious complications and a 16.1-fold increase in noninfectious urological complications, but they were significantly less likely to die of all causes within 30 days (p <0.0001 for all).
Table 1.
Cumulative risk of hospitalization, infection or serious complication within 30 days for men undergoing biopsy compared to controls
| OR (95% CI)* | ||
|---|---|---|
| Hospitalization: | ||
| Only 1 biopsy | 2.98 | (2.77–3.20) |
| Multiple biopsies | 3.40 | (2.99–3.86) |
| Infectious complication: | ||
| Only 1 biopsy | 2.36 | (1.77–3.15) |
| Multiple biopsies | 4.90 | (3.26–7.55) |
| Serious complication: | ||
| Only 1 biopsy | 9.06 | (6.06–13.54) |
| Multiple biopsies | 19.67 | (11.35–34.07) |
| Death: | ||
| Only 1 biopsy | 0.34 | (0.26–0.44) |
| Multiple biopsies | 0.20 | (0.10–0.39) |
All values p <0.0001.
ORs are adjusted for age at first biopsy, race, year of first biopsy, SEER registry and comorbidity score.
As shown in table 2, compared to no biopsy, for every biopsy there was a 1.7-fold increase in overall hospitalizations, a 1.7-fold increase in serious infectious complications and a 2.2-fold increased risk of noninfectious urological complications. Thus, the more biopsies that a man undergoes, the greater his cumulative risk of experiencing a serious complication.
Table 2.
Risk of complications requiring hospital admission per each additional biopsy vs randomly selected controls from the Medicare population
| OR (95% CI) | |
|---|---|
| Hospitalization | 1.69 (1.63–1.75) |
| Infectious complication | 1.68 (1.50–1.87) |
| Serious complication | 2.21 (1.98–2.47) |
| Death | 0.41 (0.33–0.50) |
All values p < 0.0001.
However, the biopsy based analysis demonstrated that the actual repeat biopsy procedure was not more risky than the initial biopsy (see figure). As previously reported,3 there was a significant increase in the frequency of hospitalization with infectious complications over time after initial biopsy. In absolute terms there were 1,213 hospitalizations (6.9%) within 30 days after an initial biopsy, of which 67 (5.5%) were for infectious and 53 (4.4%) for noninfectious urological complications. After repeat biopsy there were 229 (4.0%) hospitalizations within 30 days, of which 22 (9.6%) were for infectious and 18 (7.9%) for noninfectious urological complications. On multivariable analysis adjusted for age, race, year, SEER registry and comorbidity score, the overall hospitalization rates were significantly lower after repeat biopsy than initial biopsy (OR 0.63, 95% CI 0.54–0.73), but the difference decreased over time. On multivariable analysis there was no significant difference in serious infectious complications (OR 0.81, 95% CI 0.49–1.32, p = 0.39) or noninfectious urological complications (OR 0.94, 95% CI 0.54–1.62, p = 0.82) after repeat biopsy compared to the initial biopsy procedure. The rate of all cause mortality was also not significantly different (OR 0.56, 95% CI 0.27–1.14, p = 0.11).
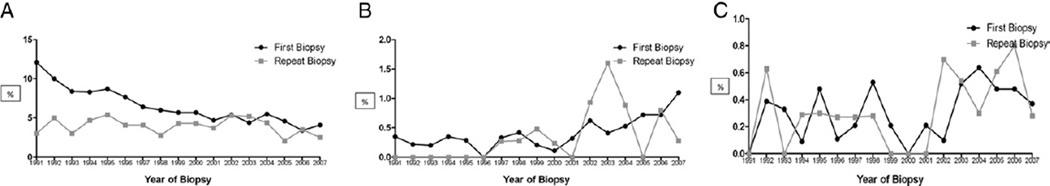
Rates (30-day) of overall hospitalization (A), hospitalization with serious infectious complications (B) and hospitalization with noninfectious urological complications (C) among SEER-Medicare participants after first biopsy vs repeat biopsy.
DISCUSSION
The complications of prostate biopsy have recently received considerable attention, particularly related to controversies about prostate cancer screening.7 In a prior study we found increasing hospitalizations for infectious complications after initial prostate biopsy in elderly United States men.3
Less has been published regarding the complications of repeat prostate biopsy. In a large Canadian study, Nam et al reported that the rate of hospitalization after repeat biopsy was 0.9% in 1996 vs 3.7% in 2005 (p <0.0001).8
An earlier study by Djavan et al of men from the European Prostate Cancer Detection Study reported urinary tract infection with fever after 2.1% of initial vs 1.9% of repeat biopsies (p = 0.02).9 Other minor biopsy related urological complications were not significantly different between the groups.
In the current study we showed that United States men undergoing initial and repeat prostate biopsy were at greater risk for hospitalization within 30 days compared to randomly selected controls. Also, each additional biopsy increased the cumulative risk of serious infectious and noninfectious urological complications. However, the actual repeat biopsy procedure was not associated with a greater risk of serious complications compared to the initial biopsy session. An analogy is that the probability of a second hurricane hitting the same spot is similar to the probability of the first, but the cumulative probability over several summers is greater.
It is noteworthy that 30-day overall mortality rates were significantly lower among men undergoing initial and repeat prostate biopsy compared to controls. These results are encouraging, suggesting that healthier men are being selected for prostate biopsy and confirming prior reports that prostate biopsy is not associated with excess mortality.10 It has been suggested that the risks of serious complications should be taken into consideration for prostate biopsy decisions, but this should not deter healthy men who may benefit from early detection from undergoing a recommended biopsy.11 Prostate cancer screening has been shown to decrease metastasis and mortality from prostate cancer.7
Strengths of the study include the large sample size from a national database. However, several limitations of our study deserve mention. Because the data were derived from coding records, we do not have information on the specific protocol used for each biopsy. For example, it is unknown whether the same antibiotics were used or whether a greater number of biopsy cores were sampled on repeat biopsies. Theoretically, using an antimicrobial agent to which resistance has developed or increasing the bacterial inoculums through a more extensive biopsy would likely result in a greater risk of infectious complications in a repeat biopsy session. However, we did not observe a greater risk of infectious complications with repeat biopsy compared to the first biopsy, suggesting that these factors did not make a major contribution. Our data are also limited to Medicare participants 65 years old or older, and the generalizability to younger men is unknown. Additionally, these data reflect the primary diagnoses for hospital admissions and, therefore, do not capture less serious complications that are managed on an outpatient basis.
CONCLUSIONS
Each prostate biopsy is associated with a significant risk of serious complications requiring hospitalization such that men undergoing multiple biopsies had an increased cumulative risk of experiencing complications. However, the repeat biopsy procedure itself was not associated with a greater risk of infectious or other urological complications compared to the initial biopsy. Decisions about each prostate biopsy procedure must take into consideration the risks and benefits. Thus, these results are useful for counseling patients who are considering a repeat prostate biopsy, such as those with persistently increased prostate specific antigen, men with atypical findings on a prior biopsy and men on active surveillance.
Supplementary Material
Acknowledgments
Supported by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics. This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, National Cancer Institute; the Office of Research, Development and Information, Centers for Medicare & Medicaid Services; Information Management Services, Inc. and the SEER Program tumor registries in the creation of the SEER-Medicare database.
Footnotes
Nothing to disclose.
Supported by the Louis Feil Charitable Lead Trust.
Supported by the Howard Hughes Medical Institute, the National Institutes of Health, the AUA Foundation/Astellas Rising Star in Urology Award and the Patrick C. Walsh Prostate Cancer Research Foundation.
REFERENCES
- 1. [Accessed May 28, 2012];American Cancer Society: Cancer Facts & Figures. 2012 Available at www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-031941.pdf. [Google Scholar]
- 2.Welch HG, Fisher ES, Gottlieb DJ, et al. Detection of prostate cancer via biopsy in the Medicare-SEER population during the PSA era. J Natl Cancer Inst. 2007;99:1395. doi: 10.1093/jnci/djm119. [DOI] [PubMed] [Google Scholar]
- 3.Loeb S, Carter HB, Berndt SI, et al. Complications after prostate biopsy: data from SEER-Medicare. J Urol. 2011;186:1830. doi: 10.1016/j.juro.2011.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liss MA, Chang A, Santos R, et al. Prevalence and significance of fluoroquinolone resistant Escherichia coli in patients undergoing transrectal ultrasound guided prostate needle biopsy. J Urol. 2011;185:1283. doi: 10.1016/j.juro.2010.11.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46:1075. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]
- 6.Zhanel GG, Hisanaga TL, Laing NM, et al. Antibiotic resistance in outpatient urinary isolates: final results from the North American Urinary Tract Infection Collaborative Alliance (NAUTICA) Int J Antimicrob Agents. 2005;26:380. doi: 10.1016/j.ijantimicag.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Schröder FH, Hugosson J, Roobol MJ, et al. Prostate- cancer mortality at 11 years of follow-up. N Engl J Med. 2012;366:981. doi: 10.1056/NEJMoa1113135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nam RK, Saskin R, Lee Y, et al. Increasing hospital admission rates for urological complications after transrectal ultrasound guided prostate biopsy. J Urol. 2010;183:963. doi: 10.1016/j.juro.2009.11.043. [DOI] [PubMed] [Google Scholar]
- 9.Djavan B, Waldert M, Zlotta A, et al. Safety and morbidity of first and repeat transrectal ultrasound guided prostate needle biopsies: results of a prospective European prostate cancer detection study. J Urol. 2001;166:856. [PubMed] [Google Scholar]
- 10.Carlsson SV, Holmberg E, Moss SM, et al. No excess mortality after prostate biopsy: results from the European Randomized Study of Screening for Prostate Cancer. BJU Int. 2011;107:1912. doi: 10.1111/j.1464-410X.2010.09712.x. [DOI] [PubMed] [Google Scholar]
- 11.Loeb S, van den Heuvel S, Zhu X, et al. Reply from Authors re: Alexandre R. Zlotta, Robert K. Nam. To Biopsy or Not to Biopsy—Thou Shall Think Twice. Eur Urol. 2012;61:e53. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


