Abstract
A double-blind, randomized, active placebo-controlled pilot study was conducted to examine safety and efficacy of lysergic acid diethylamide (LSD)-assisted psychotherapy in 12 patients with anxiety associated with life-threatening diseases. Treatment included drug-free psychotherapy sessions supplemented by two LSD-assisted psychotherapy sessions 2 to 3 weeks apart. The participants received either 200 μg of LSD (n = 8) or 20 μg of LSD with an open-label crossover to 200 μg of LSD after the initial blinded treatment was unmasked (n = 4). At the 2-month follow-up, positive trends were found via the State-Trait Anxiety Inventory (STAI) in reductions in trait anxiety (p = 0.033) with an effect size of 1.1, and state anxiety was significantly reduced (p = 0.021) with an effect size of 1.2, with no acute or chronic adverse effects persisting beyond 1 day after treatment or treatment-related serious adverse events. STAI reductions were sustained for 12 months. These results indicate that when administered safely in a methodologically rigorous medically supervised psychotherapeutic setting, LSD can reduce anxiety, suggesting that larger controlled studies are warranted.
Key Words: LSD, psychedelic, psycholytic therapy, hallucinogen, anxiety disorder
LSD is a semisynthetic compound first synthesized in 1938 by Swiss chemist Albert Hofmann at Sandoz laboratories in Basel. Its psychoactive effects were discovered in 1943 (Hofmann, 1979). LSD was named Delysid and distributed by Sandoz as an investigational drug for psychiatric research (Hintzen and Passie, 2010). LSD-assisted psychotherapy was primarily explored for treating alcoholism, neurosis, and psychosomatic disorders (Abramson, 1967).
LSD in oral doses of more than 100 μg produces vivid psychosensory changes, including increased sensory perception, illusionary changes of perceived objects, synesthesia, and enhanced mental imagery. Affectivity is intensified. Thoughts are accelerated, with their scope usually broadened including new associations and modified interpretation and meanings of relationships and objects. Hypermnesia and enhanced memory processes typically occur. Ego identification is usually weakened. The general state of consciousness can be compared to a daydream, but with pronounced affectivity and enhanced production of inner stimuli (Grof, 1975; Hintzen and Passie, 2010). LSD has been described as a “non-specific amplifier of the unconscious” (Grof, 1975). These effects last for 6 to 9 hours and can be used to support and enhance psychotherapeutic processing.
LSD’s effects on brain functioning are complex and not fully understood. LSD influences diverse neurotransmitter systems (Nichols, 2004; Passie et al., 2008), but its psychosensory effects are mainly mediated by activation of the 5-HT2A receptors, with significant modulation by 5-HT2C and 5-HT1A receptors (Nichols, 2004; Vollenweider, 1998). No neuroimaging studies have been conducted with LSD, whereas neuroimaging studies with the LSD-related substances psilocybin (Carhart-Harris et al., 2012; Gouzoulis-Mayfrank et al., 1999; Vollenweider et al., 1997) and dimethyltryptamine (de Araujo et al., 2012; Riba et al., 2006) have yielded inconclusive results, presumably because of methodological challenges. The few congruent results throughout different studies are activation of the right hemisphere, altered thalamic functioning, and increased activity in paralimbic structures and the frontal cortex.
The development of psychotherapy with psychedelic drugs started in the 1950s with two approaches. The “psycholytic” method used lower doses and frequent sessions to enhance the standard psychotherapeutic process (Leuner, 1981). The “psychedelic” method used higher doses in fewer sessions to induce a mystical experience and moments of intense catharsis (Grof, 1980), enabling participants to work through and integrate difficult feelings and situations, thereby reducing anxiety and depression (Grob et al., 2011; Grof and Halifax, 1978; Kurland, 1985). After a trial in 1963 found LSD (combined with counseling) to reduce anxiety, depression, and pain in advanced-stage cancer patients (Kast and Collins, 1964), it was followed by studies with more than 100 advanced-stage cancer patients that established the approach and demonstrated safety and promising results (Kurland, 1985; Yensen and Dryer, 1992). The psychedelic method was most commonly used in patients with terminal cancer (Kurland, 1985; Pahnke et al., 1969). These studies were difficult to design as placebo-controlled studies for ethical reasons and difficult to successfully blind because of the psychoactive intervention.
Research into LSD-assisted psychotherapy rapidly came to a halt when LSD was made illegal in the United States in 1966 because of increased nonmedical use (Grinspoon and Bakalar, 1997). Some LSD-assisted psychotherapy continued in Czechoslovakia, the Netherlands, and Germany during the 1970s (Leuner, 1981) and in Switzerland from 1988 to 1993 (Gasser, 1996). Recently, a small pilot study of psilocybin-assisted psychotherapy with advanced-stage cancer patients in the United States obtained promising results (Grob et al., 2011), with several additional studies currently in process at Johns Hopkins and New York University. This is the first controlled study of LSD-assisted psychotherapy in more than 40 years.
End-of-life issues, including pain management and palliative care, are increasingly recognized as significant public health concerns (Howell et al., 2010; Schweiz Krebsliga, 2005). The target population of this study was chosen because patients with life-threatening illnesses often fail to obtain satisfactory emotional relief from currently available treatment options. Anxiety, depression, chronic pain, as well as unresolved family and relationship issues can become serious problems for these individuals. The present LSD study was designed to evaluate previous findings applying current research methodology.
METHODS
Ethics
This phase 2 double-blind, active placebo-controlled, randomized clinical trial (Multidisciplinary Association for Psychedelic Studies, 2007) was approved by the Ethics Committee of the Canton of Aargau, Swissmedic, the Swiss Federal Office for Public Health (Bundesamt fuer Gesundheit [Swiss Ministry of Health]), and the US Food and Drug Administration (Investigational New Drug no. 101,825) and was conducted in accordance with Good Clinical Practices. After complete description of the study to all participants, written informed consent was obtained.
Participants
The participants were recruited through general information about the study reported in media, by flyers, presentations in hospitals or cancer support groups, or referral from other physicians. Of 70 participants who were evaluated for eligibility by telephone or e-mail, 20 were further screened in person, and 12 were enrolled in this study (Fig. 1). Eleven of the 12 subjects had no prior experience with LSD. Individuals with current alcohol or drug dependence (except caffeine or nicotine); primary psychotic, bipolar I affective, or dissociative disorders; and neurocognitive impairment and women who were pregnant or nursing were excluded from this study. All participants reported a score of greater than 40 on either the state or the trait scale of the Spielberger State-Trait Anxiety Inventory (STAI; Spielberger et al., 1970). According to the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID), diagnosis (First et al., 2002), half of the subjects were diagnosed with generalized anxiety disorder (GAD). Neither the SCID’s five items about GAD nor criterion E for GAD in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, differentiates between anxiety typically seen with GAD and a reaction to a life-threatening disease (and its consequences). Therefore, even though the SCID generates a diagnosis of GAD, this does not mean that the subjects had the conventional pattern of psychopathology usually associated with GAD. Recruitment took place from 2007 to 2011 until all planned participants were enrolled, and study visits were completed from 2008 to 2012. Table 1 summarizes participant demographic characteristics.
FIGURE 1.
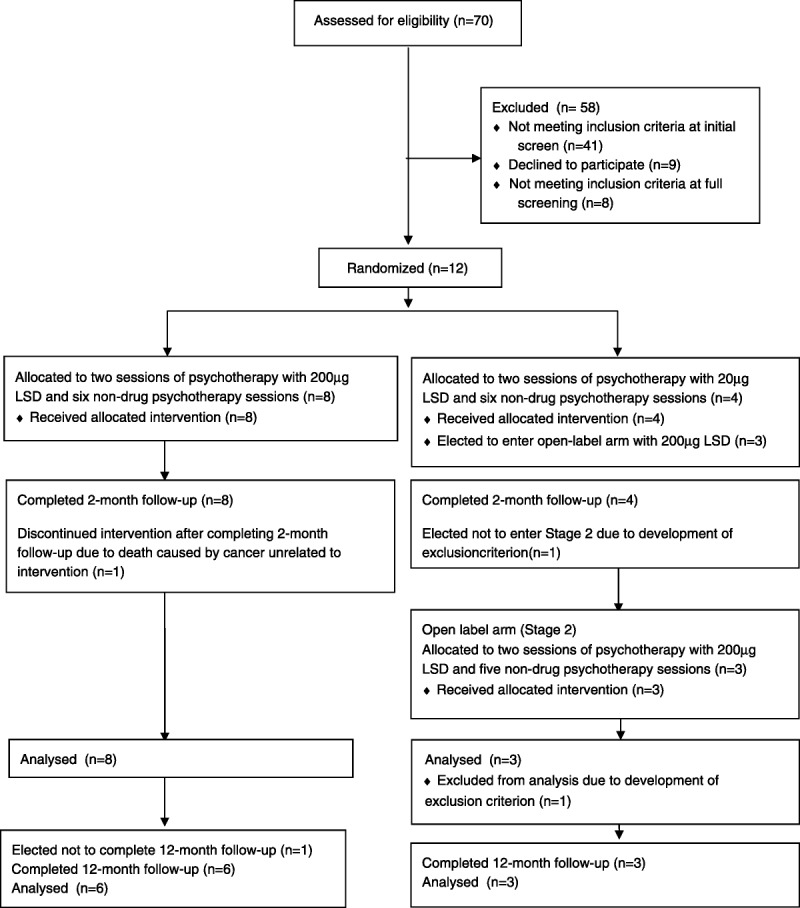
Consolidated standards of reporting trials LSD/anxiety flow diagram.
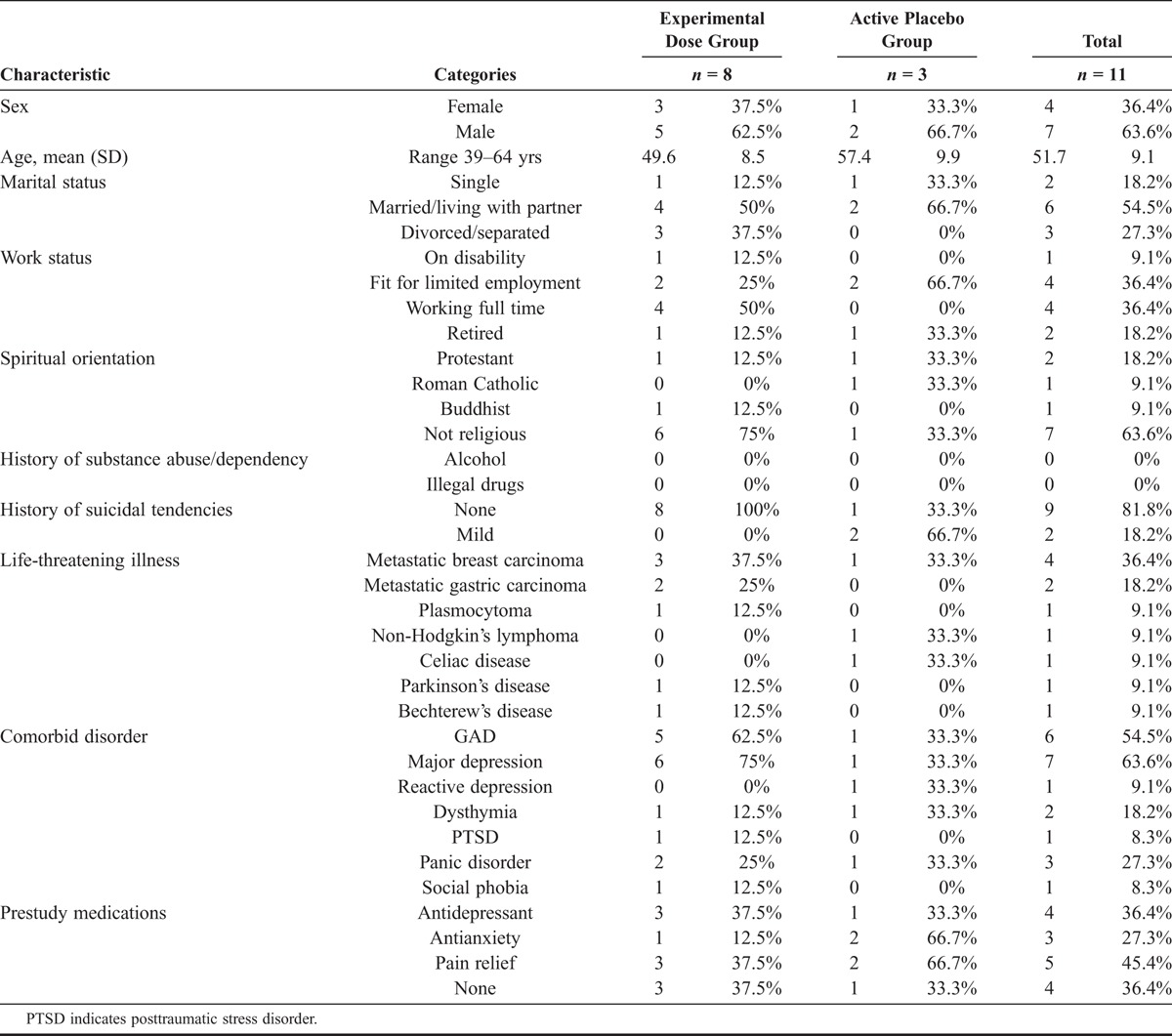
TABLE 1.
Participant Demographic Characteristics
Set
The psychotherapeutic method used in this study was a continuous process lasting several months. Two preparatory psychotherapy sessions served to discuss the participant’s history, social situation, personality, health, mind-set, and emotional situation, also known by the term set (Zinberg, 1986). These also served to explain the action of LSD and structure of the setting, answer questions, and build therapeutic alliance.
Setting
The physical environment within which the experimental sessions took place was a safe, quiet, and pleasant room in a private practice office. The participant was advised to lie on a mattress on the floor or sit comfortably on a chair. Other than going to the bathroom, the participants remained in the treatment room for the entire 8-hour experimental session and overnight with an attendant nearby.
Experimental Drug
LSD was supplied as free base by Lipomed (Arlesheim, Switzerland). Capsules consisting of 200 μg (experimental dose) and 20 μg of LSD (active placebo) were prepared by Bichsel Laboratories (Interlaken, Switzerland). Quality control, randomization, and blinding were performed by R. Brenneisen, PhD, at the Department of Clinical Research, University of Bern, Switzerland. Capsules were of identical size, color, and shape and were bottled in sequentially numbered containers.
Experimental Intervention
The primary intervention consisted of two full-day experimental sessions scheduled 2 to 3 weeks apart with a male/female co-therapist team, embedded within an ongoing process of drug-free psychotherapy sessions for preparatory and integrative purposes.
The participants were randomly assigned to the experimental dose groups, receiving either an oral dose of 200 μg of LSD (n = 8) or an active placebo of 20 μg of LSD (n = 4). The experimental dose was a moderate amount expected to produce the full spectrum of a typical LSD experience, without fully dissolving normal ego structures. The 20-μg dose of LSD was chosen as an active placebo to produce short-lived, mild, and detectable LSD effects that would not substantially facilitate a therapeutic process. The participant, the co-therapists, and the independent rater were blinded to condition assignment.
The participants were required to taper off of antidepressants and antianxiety medications, to avoid alcohol and recreational drugs for 24 hours before, and to abstain from driving for 24 hours after the experimental sessions. On the morning of the experimental sessions, the participants arrived at the office for a short discussion about their current mood and mental state and a urine drug test (Drug Screen Multi5A: amphetamine, cocaine, morphine, methamphetamine, tetrahydrocannabinole; nal von minden GmbH, Moers/Germany). If the subjects tested positive, the session would have been postponed, but this did not occur. After LSD administration, the participants were instructed to focus their awareness and mindful attention inward to follow their personal process of perception, emotion, and cognition. Lengthy discussions between the participants and the co-therapists were discouraged during the acute effects of the LSD. Approximately two thirds of each LSD-assisted experimental session was focused inward with music played to deepen self-awareness and facilitate emotional processing, and one third contained brief conversations. The therapeutic session ended after 8 hours, when the acute effects had subsided, followed by a brief review of the day’s experiences.
After each experimental session, three drug-free psychotherapy sessions lasting 60 to 90 minutes took place, during which the participant’s experiences were reviewed for integration and deepening the therapeutic process. Two months after the second experimental session, a follow-up evaluation was completed, and the treatment period was finished by breaking the blind for each individual. The participants who received the active placebo could cross over to an identical but open-label treatment with 200 μg of LSD. A long-term follow-up evaluation was conducted 12 months after the last experimental session with LSD in either the blinded portion of the study or the open-label crossover.
Assessments
A nurse collected heart rate and blood pressure measurements during experimental sessions. After two experimental sessions, a follow-up physical examination was performed by the participant’s physician. Throughout the study, adverse events (AEs) were collected, and related AEs were recorded during experimental sessions and at the integrative session on the day after. The related AEs contained both AEs that were disturbing for the participant and those that belong to the mode of action of LSD (e.g., visual patterns). Concomitant medications used to treat anxiety, depression, and pain before the study and in between experimental sessions were documented. The subjects tapered off of these types of concomitant medications approximately five half-lives before each experimental session.
Psychometric Measures
The independent rater, an experienced clinical psychologist, conducted the SCID to establish psychiatric diagnoses at screening (Wittchen et al., 1997). The STAI Form X, a widely used self-report instrument for assessing state and trait anxiety in adults, served as the primary outcome measure of anxiety symptoms. Secondary outcome measures included the European Cancer Quality of Life Questionnaire 30-item version 1.0 (EORTC-QLQ-30; Aaronson et al., 1993), the SCL-90-R (Schmitz et al., 2000), and the Hospital Anxiety and Depression Scale (HADS; Herrmann-Lingen et al., 2011). Outcome measures were completed at baseline, 1 week after experimental sessions, 2-month follow-up, and 12-month follow-up. The participants completed a daily dairy on changes in medication, adverse effects of LSD or medications, and pain using the Visual Analog Pain Scale. After each experimental session, the State of Consciousness Questionnaire was completed (Griffiths et al., 2006).
Statistical Analysis
The statistical software Statistical Package for the Social Sciences for Windows, version 18.0 (IBM Corp, New York), was used. Repeated-measures analysis of variance (ANOVA) was used to test for significant changes in anxiety from baseline to subsequent posttreatment measurements. STAI trait and STAI state were analyzed in separate ANOVAs. To account for multiplicity, the alpha level indicating significance was adjusted to 0.025 (two tailed). Effect sizes were estimated using Cohen’s d techniques. Results of the 12-month follow-up were compared with those of the 2-month follow-up with paired t-tests. Secondary outcome measures conducted for exploratory purposes were not used for significance testing to reduce multiplicity.
We were unable to obtain results for two subjects (one experimental dose, one active placebo) from the assessment conducted 1 week after the second experimental session because of intervening cancer treatments. To avoid substantially reducing the sample size because of missing data, the assessment 1 week after the second experimental session was dropped for all subjects from analysis of outcomes. One active placebo participant was excluded from analysis after completing all study procedures because of a correction in the diagnosis of the qualifying disease state, which no longer satisfied the inclusion criteria.
RESULTS
Clinical Response
For STAI trait, Mauchly’s Test of Sphericity was not significant (p = 0.824) and sphericity was assumed. No significant difference was found (p = 0.261) between group mean scores at baseline. The visit × group interaction testing for differences between the groups produced p = 0.033 (F = 4.151, df = 2,18), and observed statistical power was 65.6%, with results trending toward statistical significance. Comparing trait anxiety at baseline with 2-month follow-up yielded an effect size of 1.1. However, only three of eight experimental dose subjects dropped lower than the threshold value of 40 after the intervention. In contrast, all active placebo subjects experienced increases in trait anxiety. Figure 2 shows a clear linear relationship between visit and mean trait anxiety for the experimental dose group, whereas no such relationship exists for the active placebo group. Comparison of 2-month and 12-month follow-up results in the subjects who received 200 μg of LSD in either the blinded sessions or the open-label crossover indicate that the benefits were sustained over time. The mean difference varied only by 0.667 between these assessments, and no significant difference was found with p = 0.825 (two tailed).
FIGURE 2.
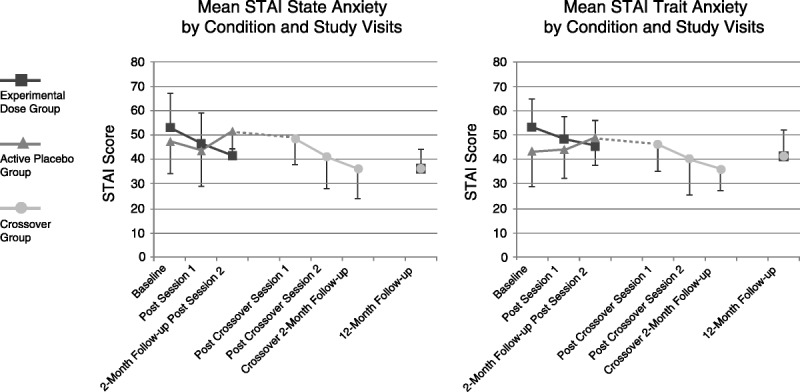
Study outcomes. State and trait anxiety scores in the LSD and placebo group. Values are mean ± SEM of changes from baseline in eight subjects in the LSD group and three subjects in the placebo group. Measures were obtained before the first treatment session (baseline), 1 week after the first treatment (post 1 LSD), 1 week after the second treatment (LSD 2), and at follow-up after 2 months. At 2 months, state anxiety scores were significantly lower in the LSD group compared with the placebo group. The crossover group (n = 3) shows a positive trend of STAI state and trait score reduction. At 12-month follow-up, the state and trait values remain stable compared with the 2-month follow-up.
For STAI state, Mauchly’s Test of Sphericity was not significant (p = 0.813), and sphericity was assumed. No significant difference was found between the groups at baseline (p = 0.563). The visit × group interaction testing for differences between the groups produced p = 0.021 (F = 4.846, df = 2,18), and observed statistical power was 72.7%. Even controlling for multiplicity, the reductions in state anxiety were statistically significant 2 months after two experimental sessions of LSD-assisted psychotherapy. Comparing state anxiety at baseline with 2-month follow-up yielded an effect size of 1.2. However, only three of eight experimental dose subjects dropped lower than the diagnostic cutoff of 40 after the intervention. In contrast, two active placebo subjects experienced increases in state anxiety. Figure 2 shows a clear linear relationship between visit and state anxiety for the experimental dose group, whereas no such relationship exists for the active placebo group. Comparison of 2-month and 12-month follow-up results in the subjects who received 200 μg of LSD in either the blinded sessions or the open-label crossover indicates that the benefits were sustained over time. The mean difference varied only by 1.00 between these assessments, and no significant difference was found with p = 0.531 (two tailed).
Changes in secondary outcome measures were not analyzed for statistical significance because of concerns about multiplicity. However, the results obtained from these measures were, overall, quite supportive of the STAI results (Table 2). Global health scores from the EORTC-QLQ increased from a mean (SD) of 37.4 (10.0) at baseline to 50.0 (14.9) after treatment with two sessions of 200 μg of LSD, whereas mean scores decreased from 44.3 (12.7) to 36.0 (12.8) in the active placebo group. Scores increased on average in the subjects who received 200 μg of LSD treatments and continued to 12-month follow-up, indicating that most of the subjects receiving the experimental dose were able to attain and maintain comparable quality of life with the general European population by participating in this study (Scott et al., 2008).
TABLE 2.
Study Outcomes
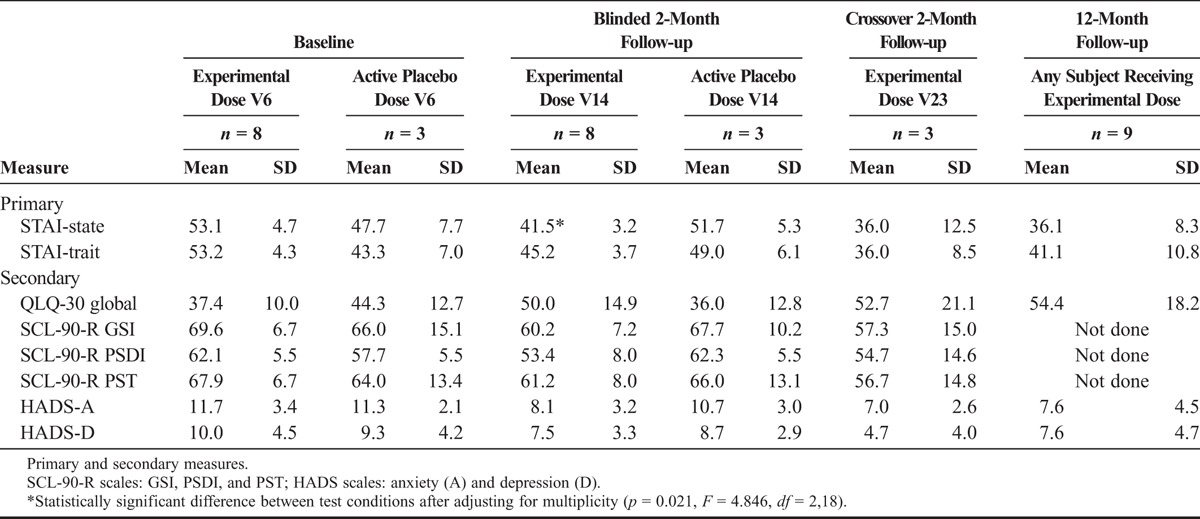
The SCL-90-R is a widely used measure of overall psychological problems and psychopathology. Global Severity Index (GSI) scores from the SCL-90-R decreased from a mean (SD) T-score of 69.6 (6.7) at baseline to 60.2 (7.2) in the experimental dose group whereas increasing from 66.0 (15.1) to 67.7 (10.2) in the active placebo group. The active placebo group experienced an improvement comparable with the full-dose group after receiving the experimental dose in the open-label crossover, with mean (SD) T-scores dropping to 57.3 (15.0). Both Positive Symptom Distress Index (PSDI) and Positive Symptom Total (PST) scores from the SCL-90-R mirrored these improvements, indicating that overall psychopathology improved in this subject sample 2 months after treatment.
The HADS results were also generally supportive of overall improvements in this subject sample. The experimental dose group mean (SD) anxiety scores decreased from 11.7 (3.4) to 8.1 (3.2) after two sessions, whereas the active placebo group anxiety scores decreased only from 11.3 (2.1) to 10.7 (3.0). The active placebo subjects who continued to the crossover experienced an even greater decline lower than the diagnostic cutoff for anxiety to 7.0 (2.6). All subjects who received the experimental dose were lower than the diagnostic cutoff at the 12-month follow-up, with a mean (SD) of 7.6 (4.5). The depression results also mirrored the anxiety results. Overall, the secondary outcome measures of the study were useful in supporting the results of the primary outcome measure.
For all 24 blinded sessions, all participants correctly guessed the dose of LSD that was administered, and both therapists guessed incorrectly in one active placebo session. The therapists were “very certain” in 22 sessions, “certain” in 1 session, and “somewhat certain” in 1 session. The participants were “very certain” in 20 sessions, “certain” in 1 session, “somewhat certain” in 2 sessions, and “not at all certain” in one session. This indicates that the 20-μg dose was too low to achieve successful uncertainty about the dose.
Safety
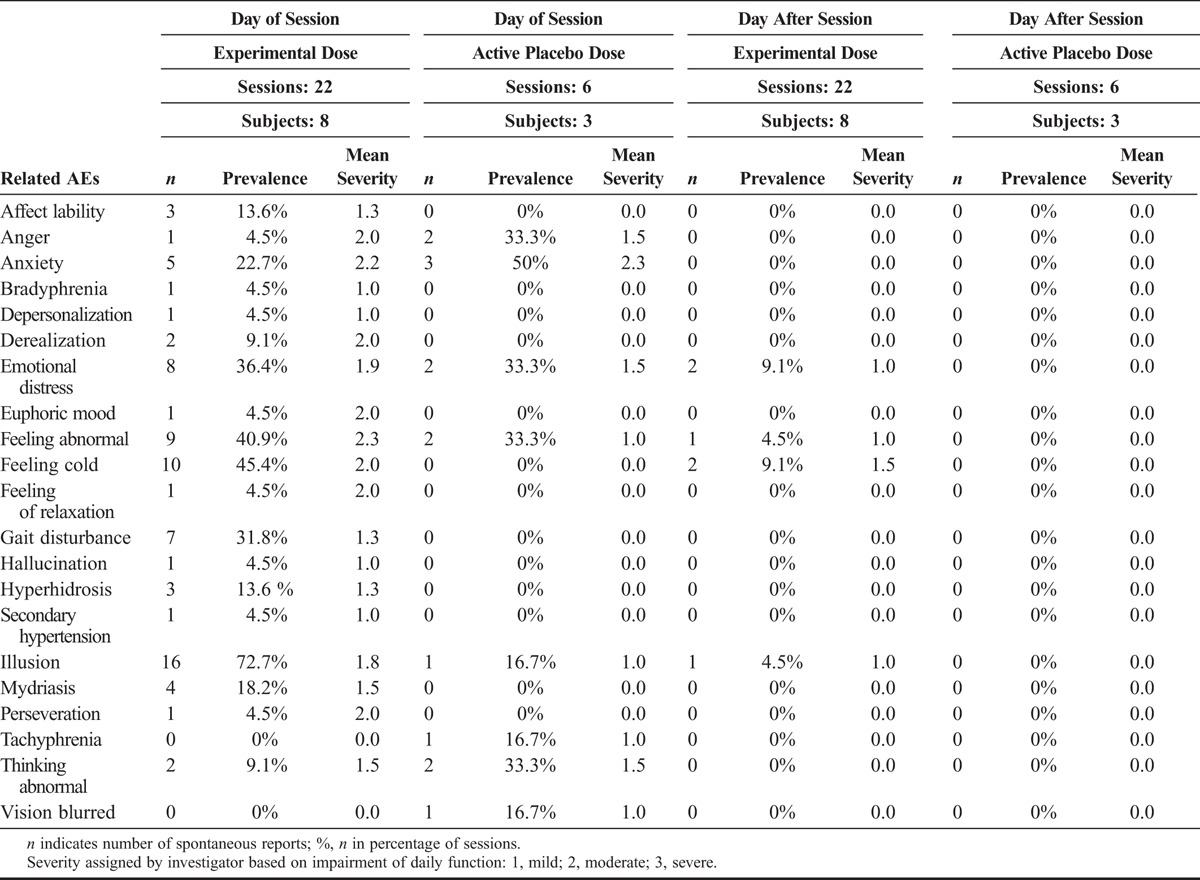
Neither the experimental dose (200 μg of LSD) nor the active placebo (20 μg of LSD) produced any drug-related severe adverse events, that is, no panic reaction, no suicidal crisis or psychotic state, and no medical or psychiatric emergencies requiring hospitalization. Related AEs (Table 3) included both positive and negative effects commonly associated with LSD. The experimental dose subjects experienced more types of AEs (n = 18) than the active placebo subjects (n = 8). In general, AEs were reported more frequently and with increased intensity in the experimental dose sessions. Interestingly, fewer reports of anxiety were received during experimental sessions with 200 μg (22.7%) than with active placebo (50%), and the mean intensity of anxiety was comparable between the groups. However, the subjects reported experiencing mild-to-moderate emotional distress similarly in experimental dose sessions (36.4%) and active placebo sessions (33.3%). Most AEs resolved when drug effects diminished. Only six reports of mild related AEs (illusions, feeling cold or abnormal, and some emotional distress) persisted until the next day. No flashback phenomena or other prolonged effects were observed.
TABLE 3.
Related AEs
Concomitant Medication
During the study, two participants (both experimental dose) received concomitant selective serotonin reuptake inhibitor (SSRI) treatment for depression and tapered off of these medications five half-lives before each experimental session because SSRIs may attenuate the effects of the serotonergically active experimental drug (Bonson et al., 1996). Three participants received benzodiazepines (two experimental dose and one active placebo) as needed. Three participants received pain medication during the study, only one of which was required as rescue medication for a treatment-emergent AE. Acetaminophen was required for this participant for a moderate headache the day after an experimental dose session.
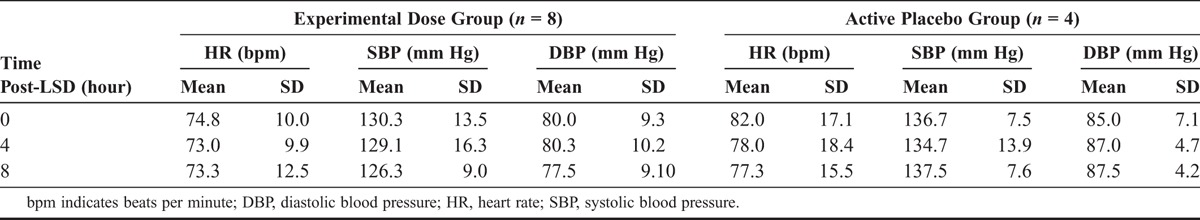
Physiological Measures
Physiological measures were recorded for all participants during experimental sessions. Consistent with the previous findings (Kornetsky, 1957; Sokoloff et al., 1957), LSD did not significantly alter blood pressure or heart rate (Table 4).
TABLE 4.
Physiological Measurements
DISCUSSION
All research with LSD-assisted psychotherapy in the 1950s and the 1960s came to a halt by the early 1970s. Our study, the first in more than 40 years to evaluate safety and efficacy of LSD as an adjunct to psychotherapy, was conducted in participants with anxiety after being diagnosed with a life-threatening illness. In contrast to the shortcomings of older studies, we used a controlled, randomized, and blinded study design to meet contemporary research standards. LSD was given in a psychotherapeutic context to facilitate a deep psychedelic state, allowing the participant to encounter his/her own inner realities during an emotionally intensified dream-like “journey.”
In our study, using appropriate inclusion/exclusion criteria, detailed participant preparation, and a carefully supervised experience in a supportive psychotherapeutic setting, psychological side effects were mild and limited. There were no AEs often attributed to LSD such as prolonged anxiety (“bad trip”) or lasting psychotic or perceptional disorders (flashbacks). Congruent with studies in the past (Hintzen and Passie, 2010), the few mild somatic effects of LSD such as changes in heart rate and blood pressure were of no clinical significance.
The primary outcome variable in this study was of the STAI anxiety measure. Patients with life-threatening illnesses confront an existential threat from shortened life expectancy that often causes periods of suffering, pain, and anxiety. Congruent with earlier studies (Pahnke et al., 1970), the results in the experimental dose group show a significant reduction in state anxiety, as experienced on a daily basis. Furthermore, the more stable personality-inherent feature of anxiety proneness (trait anxiety) showed a strong trend toward reduction. Trait anxiety is not expected to be altered by short-term psychotherapy (Spielberger et al., 1970), but a comparable finding was reported in recent research with psilocybin in cancer patients that reported significant reductions of trait anxiety (although without correction for multiplicity) but not state anxiety (Grob et al., 2011). Therefore, this trait change may be supported by neurobiological effects of adjunctive use of LSD, which was originally introduced for deepening and accelerating psychotherapeutic processing (Abramson, 1967) and, in some studies, was shown to alter personality traits (MacLean et al., 2011; McGlothlin et al., 1967; Savage et al., 1966).
In this study, the experimental dose reduced anxiety when administered in either the blinded treatment or the open-label crossover for the active placebo subjects. These results were stable over time as shown by the 12-month follow-up. Eleven of 12 participants treated were LSD-naive. A moderate dose (200 μg) provided a psychologically manageable first LSD experience. Most of the participants stated a preference for more than two LSD sessions and a longer treatment period. The results demonstrated a decrease in STAI scores most prominently after the second LSD session, suggesting that at least two LSD sessions are needed to demonstrate these effects. A longer treatment period with additional LSD sessions and larger doses may be indicated (Gasser, 1996).
Limitations of the Study
As a pilot study, this study had limited sample size, which reduced precision in effect size estimates and significance testing. The sample size selected was sufficient for a study primarily focused on safety and feasibility. The imperfect blinding also limits the validity of the results. The problem of the double blind in studies with pharmacologically active substances is a well-known methodological challenge (Mogar, 1967; Salzman, 1969). LSD is a potent psychoactive drug, and participants and therapists are likely to detect whether an experimental dose or an inactive placebo or active placebo of very low dose of LSD was administered. Although using a slightly higher LSD dose in the comparator group can increase blinding, it can also increase efficacy of the comparator, compromising the estimates of effect size. Given the safety of the moderate experimental dose, results might have been improved with a larger dose of 250 μg. Other limitations exist in treating participants with grave somatic diseases because the course of the somatic illness (e.g., worsening or improving) may substantially impact psychological parameters independent of the therapeutic intervention and contribute to missing data. The quality of life questionnaire (EORTC-QLQ), which was chosen as a secondary outcome measure, focuses extensively on physical aspects and was insufficient for evaluating long-term psychological changes. Future studies should include a quality of life measure that focuses on psychological well-being more so than physical aspects of quality of life in this population.
CONCLUSIONS
This pilot study in participants with anxiety associated with the diagnosis of a life-threatening illness has demonstrated safety in 22 psychotherapy sessions assisted by 200 μg of LSD with no drug-related severe adverse events. Group comparison results support positive trends in reduction of anxiety after two sessions of LSD-assisted psychotherapy, with effect size estimates in the range of 1.1 to 1.2. In view of promising historical studies with adjunctive LSD treatment in this population and a recent promising study using psilocybin (Grob et al., 2011), as well as the urgent need for more effective treatments of anxiety in these participants, further study is warranted into the potential of LSD-assisted psychotherapy.
ACKNOWLEDGMENTS
The authors thank B. Speich, M. Jegerlehner, and K. Haenseler for study management and C. Blank and K. Kirchner for study coordination.
The authors dedicate this article to Albert Hofmann, discoverer of LSD, for whom this study and the resumption of research into LSD’s therapeutic potential was “a fulfillment of a longtime wish.”
DISCLOSURES
This study was funded in part by Schweizerische Aerztegesellschaft für Psycholytische Therapie (Swiss Medical Society for Psycholytic Therapy) and Multidisciplinary Association for Psychedelic Studies.
Rick Doblin (president) and Berra Yazar-Klosinski are employees of the main sponsor MAPS. Peter Gasser is president of SAEPT.
Footnotes
Interim findings were presented at The Psychedelic Science in the 21st Century conference, April 15 to 18, 2010, San Jose, California, and the 20th IFP World Congress of Psychotherapy conference, June 16 to 19, 2010, in Lucerne, Switzerland.
Clinical Trial Registration: clinicaltrials.gov identifier: NCT00920387.
REFERENCES
- Aaronson N, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Fletchner H, Fleischman SB, de Haes JC. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 85: 365– 376 [DOI] [PubMed] [Google Scholar]
- Abramson H. (Ed) (1967). The use of LSD in psychotherapy and alcoholism. New York: Bobbs-Merrill [Google Scholar]
- Bonson KR, Buckholtz JW, Murphy DL. (1996). Chronic administration of serotonergic antidepressants attenuates the subjective effects of LSD in humans. Neuropsychopharmacology. 14: 425– 436 [DOI] [PubMed] [Google Scholar]
- Carhart-Harris RL, Erritzoe D, Williams T, Stone JM, Reed LJ, Colasanti A, Tyacke RJ, Leech R, Malizia AL, Murphy K, Hobden P, Evans J, Feilding A, Wise RG, Nutt DJ. (2012). Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin. Proc Natl Acad Sci U S A. 109: 2138– 2143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Araujo DB, Ribeiro S, Cecchi GA, Carvalho FM, Sanchez TA, Pinto JP, de Martinis BS, Crippa JA, Hallak JE, Santos AC. (2012). Seeing with the eyes shut: Neural basis of enhanced imagery following Ayahuasca ingestion. Hum Brain Mapp. 33: 2550– 2560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). New York: New York State Psychiatric Institute [Google Scholar]
- Gasser P. (1996). Die Psycholytische Therapie in der Schweiz von 1988–1993. Schweiz Arch Neurol Psychol. 147: 59– 65 [Google Scholar]
- Gouzoulis-Mayfrank E, Schreckenberger M, Sabri O, Arning C, Thelen B, Spitzer M, Kovar KA, Hermle L, Bull U, Sass H. (1999). Neurometabolic effects of psilocybin, 3,4-methylenedioxyethylamphetamine (MDE) and D-methamphetamine in healthy volunteers. A double-blind, placebo-controlled PET study with [18F]FDG. Neuropsychopharmacology. 20: 565– 581 [DOI] [PubMed] [Google Scholar]
- Griffiths RR, Richards WA, McCann U, Jesse R. (2006). Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology. 187: 268– 283; discussion 284–292 [DOI] [PubMed] [Google Scholar]
- Grinspoon L, Bakalar JB. (1997). Psychedelic drugs reconsidered. New York: Lindesmith Center [Google Scholar]
- Grob CS, Danforth AL, Chopra GS, Hagert M, McKay CR, Halberstadt AL, Greer GR. (2011). Pilot study of psilocybin treatment for anxiety in patients with advanced-stage cancer. Arch Gen Psychiatry. 68: 71– 78 [DOI] [PubMed] [Google Scholar]
- Grof S. (1975). Realms of the human unconscious: Observations from LSD research. New York: Viking Press [Google Scholar]
- Grof S. (1980). LSD psychotherapy. Pomona, CA: Hunter House Inc Publishers [Google Scholar]
- Grof S, Halifax J. (1978). The human encounter with death. New York: E P Dutton [Google Scholar]
- Herrmann-Lingen C, Buss U, Snaith RP. (2011). Hospital Anxiety and Depression Scale–Deutsche Version (HADS-D). Bern, Switzerland: Hans Huber [Google Scholar]
- Hintzen A, Passie T. (2010). The pharmacology of LSD. Oxford, England: Oxford University Press [Google Scholar]
- Hofmann A. (1979). How LSD originated. J Psychedelic Drugs. 11: 53– 60 [DOI] [PubMed] [Google Scholar]
- Howell D, Keller-Ollaman S, Olver T, Hack T, Broadfield L, Biggs K, Chung J, Esplen MJ, Gravelle D, Green E, Gerin-Lajoie C, Hamel M, Harth T, Johnston P, Swinton N, Syme A. (2010). A Pan-Canadian practice guideline: Screening, assessment and care of psychosocial distress (depression, anxiety) in adults with cancer. Toronto, Canada: Canadian Partnership Against Cancer (Cancer Journey Action Group) & the Canadian Association of Psychosocial Oncology [Google Scholar]
- Kast E, Collins V. (1964). Study of lysergic acid diethylamide as an analgesic agent. Anesth Analg. 43: 285– 291 [PubMed] [Google Scholar]
- Kornetsky C. (1957). Relation of physiological and psychological effects of lysergic acid diethylamide. AMA Arch Neurol Psychiatry. 77: 657– 658 [DOI] [PubMed] [Google Scholar]
- Kurland AA. (1985). LSD in the supportive care of the terminally ill cancer patient. J Psychoactive Drugs. 17: 279– 290 [DOI] [PubMed] [Google Scholar]
- Leuner H. (1981). Halluzinogene. Bern, Switzerland: Hans Huber Verlag [Google Scholar]
- MacLean KA, Johnson MW, Griffiths RR. (2011). Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness. J Psychopharmacol. 25: 1453– 1461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlothlin W, Cohen S, McGlothlin MS. (1967). Long lasting effects of LSD on normals. Arch Gen Psychiatry. 17: 521– 532 [DOI] [PubMed] [Google Scholar]
- Mogar R. (1967). Psychedelic (LSD) research: A critical review of methods and results. In Bugental J. (Ed), Challenges of humanistic psychology (pp 135– 146). New York: McGraw Hill [Google Scholar]
- Multidisciplinary Association for Psychedelic Studies (2007). LSD-assisted psychotherapy in persons suffering from anxiety associated with life-threatening disesases. A phase II, double-blind, placebo-controlled dose-response pilot study. Clinical trial protocol. Retrieved from: http://www.maps.org/research/lsd/swisslsd/LDA1010707.pdf Accessed December 5, 2007.
- Nichols DE. (2004). Hallucinogens. Pharmacol Ther. 101: 131– 181 [DOI] [PubMed] [Google Scholar]
- Pahnke WN, Kurland AA, Goodman LE, Richards WA. (1969). LSD-assisted psychotherapy with terminal cancer patients. Curr Psychiatr Ther. 9: 144– 152 [PubMed] [Google Scholar]
- Pahnke WN, Kurland AA, Unger S, Savage C, Grof S. (1970). The experimental use of psychedelic (LSD) psychotherapy. JAMA. 212: 1856– 1863 [PubMed] [Google Scholar]
- Passie T, Halpern JH, Stichtenoth DO, Emrich HM, Hintzen A. (2008). The pharmacology of lysergic acid diethylamide: A review. CNS Neurosci Ther. 14: 295– 314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riba J, Romero S, Grasa E, Mena E, Carrio I, Barbanj MJ. (2006). Increased frontal and paralimbic activation following ayahuasca, the pan-Amazonian inebriant. Psychopharmacology. 186: 93– 98 [DOI] [PubMed] [Google Scholar]
- Salzman C. (1969). Controlled therapy research with psychedelic drugs: a critique. In RE Hicks, PJ Fink (Eds), Psychedelic drugs (pp 23–32). New York: Grune & Stratton [Google Scholar]
- Savage C, Fadiman J, Mogar R, Hughes AM. (1966). The effects of psychedelic (LSD) therapy on values, personality, and behavior. Int J Neuropsychiatry. 2: 241– 254 [PubMed] [Google Scholar]
- Schmitz N, Hartkamp N, Kiuse J, Franke GH, Reister G, Tress W. (2000). The Symptom Check-List-90-R (SCL-90-R): A German validation study. Qual Life Res. 9: 185– 193 [DOI] [PubMed] [Google Scholar]
- Schweizerische Krebsliga (2005). Schlussbericht Bestandesaufnahme psychosoziale Onkologie in der Schweiz. Bern, Switzerland: Krebsliga Schweiz [Google Scholar]
- Scott NW, Fayers PM, Aaronson NK, Bottomley A, de Graeff A, Groenvold M, Gundy C, Koller M, Petersen M, Sprangers MAG. (2008). EORTC QLQ-C30 Reference Values. Brussels, Belgium: EORTC Quality of Life Group. [Google Scholar]
- Sokoloff L, Perlin S, Kornetsky C, Kety SS. (1957). The effects of D-lysergic acid diethylamide on cerebral circulation and overall metabolism. Ann N Y Acad Sci. 66: 468– 477 [DOI] [PubMed] [Google Scholar]
- Spielberger CS, Gorsuch RL, Lushene RE. (1970). Manual for the State Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press [Google Scholar]
- Vollenweider FX. (1998). Advances and pathophysiological models of hallucinogenic drug actions in humans: A preamble to schizophrenia research. Pharmacopsychiatry. 31 (suppl 2): 92– 103 [DOI] [PubMed] [Google Scholar]
- Vollenweider FX, Leenders KL, Scharfetter C, Maguire P, Stadelmann O, Angst J. (1997). Positron emission tomography and fluorodeoxyglucose studies of metabolic hyperfrontality and psychopathology in the psilocybin model of psychosis. Neuropsychopharmacology. 16: 357– 372 [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Zaudig M, Fydrich T. (1997). Strukturiertes klinisches Interview für DSM-IV. Achse I und II. Goettingen, Germany: Hogrefe [Google Scholar]
- Yensen R, Dryer D. (1992). Thirty years of psychedelic research: the Spring Grove experiment and its sequels. Unpublished manuscript, based on an address to the European College of Consciousness (ECBS) International Congress in Goettingen, Germany [Google Scholar]
- Zinberg NE. (1986). Drug, set, and setting: The basis for controlled intoxicant use. New Haven, CT: Yale University Press [Google Scholar]


