Abstract
Background
A growing literature demonstrates that early clinical intervention can reduce risks of adverse psychosocial outcomes. A first step necessary for developing early intervention services is to know the prevalence of clinical disorders, especially in systems that are rebuilding, such as Romania, where the mental health system was dismantled under Ceaucescu. No epidemiologic studies have examined prevalence of psychiatric disorders in young children in Romania.
Objective
To determine the prevalence of psychiatric disorders in Romanian children 18-60 months in pediatric settings.
Methods
Parents of 1003 children 18-60 months in pediatric waiting rooms of two pediatric hospitals completed background information, the Child Behavior Checklist (CBCL). A subgroup over-sampled for high mental health problems were invited to participate in the Preschool Age Psychiatric Assessment.
Results
Rates of mental health problems were similar to the U.S. norms on the CBCL. The weighted prevalence of psychiatric disorders in these children was 8.8%, with 5.4% with emotional disorders and 1.4% with behavioral disorders. Co-morbidity occurred in nearly one fourth of the children with a psychiatric disorder and children who met diagnostic criteria had more functional impairment than those without. Of children who met criteria for a psychiatric disorder, 10% of parents were concerned about their child’s emotional or behavioral health.
Conclusions
This study provides prevalence rates of psychiatric disorders in young Romanian children, clinical characteristic of the children and families that can guide developing system of care. Cultural differences in parental report of emotional and behavioral problems warrant further examination.
Keywords: early childhood, mental health, epidemiology, preschool
Introduction
Until recently, there was little recognition of mental health problems in very young children. A growing empirical base, however, suggests that very young children can suffer from clinically impairing psychiatric syndromes at rates similar those in older children [5, 9, 16, 31, 37, 42, 50]. For major categories of psychiatric disorders, findings support convergent validity and for some disorders, biological correlates have also been identified [36, 44, 51]. These early disorders are associated with impairment in multiple developmental domains including cognitive, social and emotional functioning [35, 50, 54]. Importantly, these patterns are not transient phases, but show persistence well beyond the early childhood years [6, 30, 32, 45]. Although more research into the clinical syndromes is necessary, current data highlight the need to understand the prevalence of these disorders, especially in communities in which mental health services are undergoing revisions or rebuilding. This is particularly true in Romania, where the mental health system was significantly damaged under an oppressive political regime between 1945 and 1989 and is still quite limited and [3, 21]. Understanding early childhood mental health needs in this redeveloping system can guide allocation of scarce psychiatric resources, inform workforce development. Building an infrastructure focused on early childhood and prevention can be a cost effective approach to reduce community mental health and social burdens [23].
Currently, there is little information about rates of psychiatric disorders in Romanian preschool children. One small study reported a prevalence rate of 17% in a community sample of 59 54-month-olds, of whom 13.4% had an internalizing disorder and 6.8% an externalizing disorder [53]. To the best of our knowledge, no other studies have examined rates of disorders in Romania or Central Europe in young children. Studies of young children in Western Europe have primarily used parent checklists or report of previous diagnosis to estimate rates of psychiatric problems in preschoolers, with generally similar findings as in US samples, although several studies have reported prevalence rates of clinical range parent report measures under 10% in preschoolers [19, 24, 26, 39, 46, 48]. In older Romanian children, parents endorsed similar numbers of symptoms as U.S. parents on a parent report checklist [40]. Internationally, among the most important risk factors for child mental health problems include parental psychopathology, parental education, and trauma [7, 24, 52].
In this study, we examined the prevalence of mental health problems, psychiatric disorders, co-morbidity and impairment in 1003 18-60 month old Romanian children in a pediatric setting. We examined correlates of diagnoses and predicted that children with family psychiatric histories, lower levels of parental education, and past traumatic experiences would have higher rates of psychiatric diagnoses.
METHODS
Study Procedures
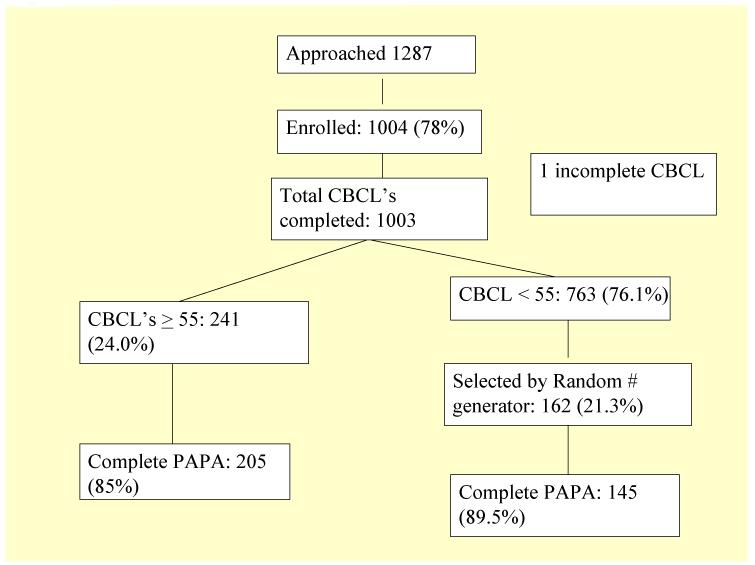
Parents of children ages 18-60 months were recruited in the pediatric waiting rooms of the Dr. Victor Gomoiu Children’s Hospital and Marie Curie Children’s Hospital in Bucharest, Romania. The pediatric waiting room serves as the outpatient pediatric clinic waiting area and triage area for the inpatient service. Parents who consented completed a brief demographic information form and the Child Behavior Checklist (CBCL) in a private room near the waiting room. Following the protocol of a previous study in Romania [55], parent report measures were administered verbally to standardize administration given the range of reading levels in parents. As is done in other epidemiologic studies to ensure adequate numbers of symptomatic participants [16], we over-sampled for children with higher scores on the CBCL, inviting parents whose children scored higher than a T score of 55 (equivalent to the top 33%ile) on the Total Behavior Problem to complete the Preschool Age Psychiatric Assessment (PAPA). Additionally, one out of every five (selected by random number generator) of the children who had a T score of less than 55 were also recruited to complete the PAPA, (see Figure 1). Interviews were completed a mean of 12.9 days after the screening date.
Figure 1.
Recruitment and retention
Participants
The participants were female primary caregivers. Rates of participation and retention are presented in Figure 1. Of the 403 eligible to participate in the diagnostic phase of the study, 305 (87%) completed the PAPA. There was no difference in completion rates between high CBCL and low CBCL participants.
Table 1 presents demographics of the study population, including the total screened sample, the group who completed the PAPA, and those who were invited to complete the PAPA but who declined (“non-completers”). Completers differed from the non-completers only in age - - children with completed psychiatric interviews were younger than those who did not.
TABLE 1.
Demographics of the study population
| Entire sample | PAPA sample | Non-completers | ||
|---|---|---|---|---|
| 1003 | 350 | 54 | ||
| Mean Age months (M, SD) |
41.2 (11.1) | 39.7 (10.9)* | 43.4 (12.0)* | |
| Maternal age (M, SD) |
30.00 (5.1) | 30.2 (4.8) | 29.6 (6.6) | |
| Paternal age (M, SD) |
32.9 (5.8) | 33.3 (5.4) | 32.9 (7.7) | |
| Girls n (%) | 482 (48.2) | 165 (47.1) | 27 (50.0) | |
| Ethnicity n (%) | Romanian | 924 (92.0) | 326 (93.1) | 45 (83.3) |
| Roma | 54 (5.40) | 15 (4.3) | 2 (3.7) | |
| Other/missing | 26 (2.6) | 8 (2.5) | 7 (13.0) | |
| Maternal Education* n (%) |
Less than HS | 381 (38.1) | 109 (31.2) | 20 (37.0) |
| HS degree/some college |
415 (41.5) | 163 (46.6) | 25 (46.3) | |
| College or advanced degree |
192 (19.2) | 77 (22.0) | 4(7.4) | |
| Paternal Education* n (%) |
Less than HS | 365 (36.5) | 101 (28.8) | 24 (44.4) |
| HS degree/some college |
398 (39.8) | 155 (44.3) | 18 (33.4) | |
| College or advanced degree |
194 (19.4) | 66 (21.7) | 7 (13.0) |
t(401) = −2.2, p<0.05
Measures
All measures were translated into Romanian and back translated into English by a native Romanian speaker fluent in English and checked for accuracy.
Child Behavior Checklist 1½-5 (CBCL)
The CBCL is a well-established 100-item questionnaire for use in children 18 months to 60 months [2]. It takes 10-15 minutes to complete and uses a 3-point Likert scale. The CBCL results provide T-scores normed by age and gender. The CBCL has demonstrated extensive internal validity, test-retest reliability and convergent reliability. The validity of the CBCL 1 1/2=−5 has not specifically been tested in Romania, but the companion measure (CBCL 6-18) yields similar levels of symptoms in Romania as in the US [40] and the factor structure of the 1 ½-5 grossly fits that of the US model [28].
Preschool Age Psychiatric Assessment
The Preschool Age Psychiatric Assessment (PAPA) is a comprehensive parent-report psychiatric diagnostic interview for the preschool age that combines interviewer based and respondent based methods [16]. The measure takes approximately 100 minutes to administer and includes 25 diagnostic modules. The PAPA yields symptom counts, level of functional impairment, specific diagnoses, and composite disorders. Algorithms created for the English version of the PAPA were used to generate diagnoses and scale scores from the Romanian PAPA. The test-retest reliability of the PAPA is comparable to that of structured psychiatric interviews used to assess older children and adults [15].
In this study, we examined rates of behavioral disorders (Attention Deficit Hyperactivity Disorder, Oppositional Defiant Disorder, Conduct Disorder), emotional disorders (depressive disorders, specific anxiety disorders), sleep disorders, and reactive attachment disorder. In the post-traumatic stress disorder (PTSD) module, we also counted the number of DSM-IV level stressors the child had experienced. For most disorders, DSM-IV TR criteria were applied. However, developmentally sensitive, empirically-derived criteria from the Research Diagnostic Criteria: Preschool Age were applied for reactive attachment disorder (RAD), depression, and PTSD [1]. In addition, following previously reported methodology, we required functional impairment in addition to the symptom criteria for specific phobias, separation anxiety disorder, and social phobia [15]. The PAPA generates impairment scale, which represents the number of life domains (0-30) in which the child’s symptoms cause functional disability, as previously described [15].
Background information
Parents completed a brief form that included child and parent age and education, child ethnicity, medical problems, family history of psychiatric disorders and violence exposure, child history of abuse, number of siblings, out of home child care attendance, parent concern (yes/no) about their child’s emotional or behavioral development, and whether the child had been referred for treatment.
Consent and IRB Approval
This study was approved by the Institutional Review Board at Tulane University School of Medicine and by the Head (Medical Director) of each hospital, who confirmed that all members of their staff involved in the study reviewed an IRB-approved presentation focused on ethical conduct of research.
Statistical Analyses
Algorithms written in SAS 9.2 were used to create diagnoses variables [41]. Analyses were performed using SAS 9.2 and SPSS 17.0 [47]. Using the generalized estimating equations function of SAS PROC GENMOD, we computed weighted analyses from the whole sample to correct for the sampling scheme to derive unbiased estimates of reliability for the Romanian pediatric population. Using weighted prevalence analyses, we examined demographic correlates of psychiatric diagnoses. T-tests were applied to examine differences among continuous variables and chi-square analyses for categorical variables [47]. All prevalence data are presented using weighed correction for sampling unless otherwise stated.
RESULTS
Mental Health Problems
In the total sample, the mean Total Problems scale score on the Child Behavior Checklist was 49.05 with a standard deviation of 8.6, similar to reference norms on U.S. and other European samples [2]. The internalizing and externalizing scale means were 49.3 (SD 9.0) and 50.1 (9.1) respectively. Scores on all three scales were normally distributed. On the Total Problems scale, 72 children (7.2%) had a T score of 63 or above, a mark that represents the top 8% of the normative sample in the U.S. Girls had lower externalizing scale T scores than boys (48.4 vs. 50.1, t(1001) = −3.0, p<0.03). Because the T score is based on US norms, this finding also suggests that Romanian girls had relatively lower levels of reported externalizing signs than seen in the US normative sample, for whom the mean T score is, by definition, 50.
Prevalence of Psychiatric Diagnoses
Table 2 presents the rates of psychiatric disorders. In this group, 8.8% of children met criteria for a psychiatric diagnosis of an emotional, behavioral, or attachment disorder. When sleep disorders were included, 10.4% met criteria for a psychiatric disorder. Children with psychiatric diagnosis were more impaired than those without (1.0 vs. 2.6, t(63.5)=−3.5, p<0.0001).
TABLE 2.
Rates of Psychiatric Diagnoses
| Unweighted Number (n) |
Weighted Prevalence (%) |
Upper, lower 95% OR |
Weighted Prevalence Girls (n=165) |
Weighted Prevalence Boys (n=185) |
|
|---|---|---|---|---|---|
| MDD | 3 | .2 | 0.08, 0.8 | 2 | 0 |
| SAD | 9 | 1.3 | 0.03, 1.3 | 8* | 2* |
| GAD | 12 | 2.5 | 0.9, 4.1 | 11 | 11 |
| Selective Mutism | 2 | .2 | 0.04, 0.4 | 1 | 1 |
| Specific Phobia | 2 | .3 | 0.08,, 1.2 | 1 | 1 |
| Social Phobia | 4 | .6 | .2,, 1.7 | 4 | 1 |
| PTSD | 1 | .2 | 0.02, 1.1 | 1 | 0 |
| ADHD | 4 | .4 | 1 | 2 | |
| Oppositional Defiant Disorder |
6 | .9 | 0.4, 2.1 | 0* | 7* |
| Conduct Disorder | 2 | .2 | .02, 1.1 | 1 | 0 |
| Reactive Attachment Disorder- inhibited |
0 | 0 | 0 | 0 | |
| Reactive Attachment Disorder- disinhibited |
13 | 2.0 | 1.1, 4.3 | 6 | 12 |
| Sleep Disorder | 17 | 4.2 | 2.5, 7.7 | 33* | 7* |
| Any depressive disorder | 10 | 1.4 | .7, 2.7 | 7 | 4 |
| Any Anxiety Disorder | 25 | 4.5 | 3.0, 7.4 | 22 | 16 |
| Any emotional disorder | 30 | 5.4 | 3.5, 8.2 | 18 | 15 |
| Any behavioral Disorder | 10 | 1.4 | .7, 2.8 | 2 | 8 |
| Emotional,behavioral, or attachment disorder |
45 | 8.8 | 6.3, 12.4 | 30 | 34 |
| All Disorders including sleep |
61 | 10.5 | 6.5, 16.9 | 60 | 52 |
(gender difference p≤0.05)
Co-morbidity
Comorbidity, that is meeting criteria for more than one disorder, was seen in 3.9% of the total weighted sample and 22.8% of children with at least 1 diagnosis (unweighted n= 9). Of these, 4 met criteria for two diagnoses, 3 for 3 diagnoses, and 2 for 4 diagnoses. Most common combinations were an emotional diagnosis (anxiety or depression) plus indiscriminate RAD (n=3) or behavioral diagnosis (ADHD, ODD, CD) plus indiscriminate RAD. The number of diagnoses was associated with impairment (r=0.36, p≤0.001).
Sub-threshold clinical syndromes and impairment
A substantial group of children had levels of clinical signs of disorders required for diagnosis but did not meet criteria because parents did not endorse impairment. This issue is most prominent in behavioral disorders, which require functional impairment for the diagnosis. Of the children who met at least 6 hyperactive or inattentive criteria for ADHD, 66.7% (unweighted n= 15) had no reported functional impairment. Overall, only 30% of children who had sufficient number of symptoms to meet diagnostic criteria were functionally impaired by parent report.
There also appeared to be patterns of sub-threshold clinical disorders, in which a substantial proportion of children with 1 fewer criterion than required showed functional impairment. For children with three signs of ODD, 50% (unweighted n=6) were impaired and 20% (unweighted n=10) of those with 2 clinical signs of GAD were impaired.
Demographic Correlates
Child characteristics
The mean age of children who met criteria for a psychiatric diagnosis in this study was slightly lower than those who did not (36.2 vs. 39.3 months, t(74.9)=2.4, p≤0.02). There was no association between gender and diagnosis (x2(1)=2.0, NS). Using weighted analyses, 5.6% of girls and 7.6% of boys met criteria for at least one psychiatric diagnosis. However, girls were more likely to meet criteria for separation anxiety disorder (1.7% vs. 4%, x2 (1)= 4.5, p≤0.03) and had higher rates of sleep disturbances than boys (7.1% vs. 1.0%; x2 (1)= 23.6, p≤0.001). Boys met criteria for ODD at higher rates than girls (1.3% vs. 0%; Fisher’s exact test ≤0.017) and had more signs of ADHD than girls (1.4 vs. 1.1; t(987)=−2.3, p≤0.03).
Children’s potentially traumatic life experiences were associated with psychiatric diagnosis. Children with a diagnosis had experienced more such events than those without a diagnosis (1.0 vs 0.6 t(936)=4.1, p≤0.001). Of children with a diagnosis, 72.5% (unweighted n=39) had experienced at least one potentially traumatic event, compared with 46.7% of those without a diagnosis (x2(4) = 16.8, p≤0.002).
Parent reported early medical problems including pregnancy difficulties, colic, and having a medical problem (predominantly asthma, febrile seizures, and congenital malformation) were all associated with having a diagnosis as well ((x2(1) = 22, p≤0.001; x2(1) = 10.7, p≤0.001; x2(1) = 6.1, p≤0.05, respectively). Interestingly, a history of colic was reported in nearly half of the children with a diagnosis.
Parent characteristics
There was no association with parent age or maternal education level and child psychiatric disorder. However, lower paternal education level was associated with child psychiatric disorder (t(62.8)=4.0, p≤0.001) and higher family income was negatively associated with meeting criteria of a psychiatric diagnoses (t(85.6)= −5.4, p≤0.001). As predicted, family history of psychiatric disorder was also associated with diagnosis (25% vs. 10.0%, x2(1)=10.7, p≤0.001). Although parental concern about the child’s emotional well-being was associated with the presence of a psychiatric diagnosis, (x2 (1)=6.2, p≤0.02), only 10% (7/66) of the parents of children who met criteria for a psychiatric diagnosis reported that they were concerned.
DISCUSSION
This is the first large study to examine rates of psychiatric disorders in very young children in a Romanian pediatric setting. We used a reliable, structured psychiatric interview to elicit symptoms and employed methodology used in other major child psychiatric epidemiologic studies [10, 16]. The mean scores on the CBCL scores suggest that the population had similar levels of parent-reported mental health symptoms as children in the U.S. general population.
In this study, 8.8% of children met diagnostic criteria for a major psychiatric disorder, a group that included anxiety disorders, mood disorders, disruptive behavior disorders, and reactive attachment disorder. Despite the similar scores on the CBCL, the rates of psychiatric disorders in this study appeared somewhat lower than those in U.S. preschool populations, where 12.1% of children met criteria for a diagnosis [15], although similar to a study in Germany using the Strengths and Difficulties Questionnaire, which closely approximate prevalence of diagnoses [22, 39]. The lower rates of psychiatric disorders in young children is consistent with findings in Romanian adults, who also have somewhat lower 12-month prevalence of psychiatric disorders (8.3%) than Western European adults (11.5%) [4, 17]. This pattern suggests the possibility of culturally-related reporting patterns.
Cultural explanations do not explain the difference between rates of psychiatric disorders in this study (10.4% when all disorders were included) and those reported in the smaller group of community comparison children studied as part of the Bucharest Early Intervention Project (BEIP) (16.9%) [53]. The two studies both used the PAPA, making it less likely that measure itself contributed to the difference. Although it is possible that there were systematic differences in administration of the interview, this seems unlikely because the interviewers were trained together. The major differences between the two studies are the much larger sample size and the sampling methodology used in this epidemiologic study, which reduces the impact that any single individual has on the prevalence rate.
In the current study, the relatively low prevalence rate was most notable in the behavioral disorders, whose prevalence was lower than US reports as well as German reports [26]. It seems likely that this pattern is related to the cultural understanding of impairment associated with behavioral patterns, as the CBCL results suggest similar rates of behavioral patterns in our sample as in US norms and other European groups. Impairment associated with the behavioral patterns is an indicator partly of the severity of the behaviors. However, it also reflects the cultural or family developmental expectations and the degree to which accommodating a child’s behavior is considered problematic. In our study, two thirds of the young children who met ADHD symptom criteria were not reported to be impaired. This finding can be compared to a study of older children with ADHD in Germany in which 20% of children who met criteria for ADHD were not impaired [14]. It is possible that, in Romania, these behaviors do not interfere with expectations about a child’s ability to go out in public, interact with others, and learn. The lack of reported impairment may also be explained by the finding that nearly three quarters of children in the study were cared for at home, where adults can tailor the routine to the child, rather than in out-of-home childcare, where more behavioral regulation is generally adaptive and more active or impulsive behaviors may be considered disruptive By contrast, 60% of US children attend out of home placements. [49] The remainder of the demographic factors we examined do not distinguish our sample from US populations. In our study, internalizing disorders were also found to be present at a somewhat lower rates than in other studies [12, 16]. Potential explanations for this difference include fewer opportunities for separation anxiety because of in-home child care, or parental attunement to a child’s internal emotional state. It is possible that concerns about stigma about all types of psychiatric disorders in Romania are associated with minimizing the impact of child symptoms or that limited access to mental health service is associated with increased accommodation to a moderate level functional impairment [27].
The findings in this study highlight the cumulative burden associated with psychiatric disorders on young children in Romania. As in other studies, children with psychiatric disorders were impaired and had similar rates of co-morbidity as other studies in preschoolers, indicating that the disorders identified are not benign developmental variations [6, 16, 18, 29, 33, 35]. The finding that traumatic early childhood experiences and family psychiatric history were associated with increased risk of psychopathology in very young children adds to the existing literature demonstrating that very early caregiving risks are reflected in the developing mental health of young children [18, 20, 43] and with adult medical outcomes [13].
Some limitations of this study must be noted. First, although psychiatric diagnostic criteria validity for some diagnoses is empirically supported in the US preschoolers, the validity of most disorders warrant further research, especially in European preschoolers. Although most epidemiologic studies in child psychiatry use parent report (e.g.[11, 16]) parent report is a limited assessment tool which is best supplemented by observational data. Retention in a two-stage study is also an important factor. Although we identified few differences completers and non-completers, we cannot rule out the possibility that systematic patterns in retention failures could exist.
Together, these findings have important implications for the developing infrastructure. First, they remind us that, as in other societies, a substantial proportion of very young Romanians experience debilitating mental health problems that are under-identified and receive almost no treatment. In this study, most children with psychiatric disorders had not previously been identified. Low rates of concern by parents may represent lack of recognition of the patterns, a belief that these patterns are transient, or hopelessness that there is help for these patterns. A system of early identification of these children could allow effective treatment for these children. As the Romanian early childhood mental health system develops, children will benefit from increased identification rates of concerning emotional and behavioral patterns by parents, medical providers, and child care providers and increasing access to adequate mental health care for very young children. The higher risk children for whom targeted screening may be warranted include those with reported history of traumatic experiences, family history of psychiatric disorders, and fewer family resources. In addition, the finding that parent reported pregnancy problems and colic are strongly associated with early childhood diagnoses suggests that these risk factors may also help to identify children at highest risk. Further study is warranted to determine the degree to which pregnancy and infancy medical factors confer prospective risks going forward through biological insults or through the mediation of the parent’s internal representation of the child, that is, how she perceives the child and therefore interacts with the infant. It is also possible, given the design of this study, that these associations are only seen retrospectively in children about whom a parent is concerned and reflect current heightened awareness of possible risk factors rather than independent risk[38]. Regardless of the reason for these associations, understanding demographic, medical, and family factors associated with early childhood psychopathology will be important in early identification and allocation of the precious mental health resources. Many early childhood disorders are responsive to treatment and these early interventions are likely cost effective, especially when considering the mental health, educational, and criminal justice expenditures to society when early mental health problems are not treated [8, 23, 25, 34]. Therefore, identifying high risk children, screening them for psychopathology, and training a workforce to be able to provide appropriate treatment could substantially reduce the developmental risks for these young children.
Acknowledgements
The authors express their appreciation to the families and staff at Dr. Victor Gomoiu Children’s Hospital and the Marie Curie Children’s Hospital.
Funding: This study was funded by the Fundatia Tulane, Bucharest, Romania
We would like to thank the families who participated, our hospital partners at Dr. Victor Gomoiu Children’s Hospital and Marie Curie Children’s Hospital and the the project coordinator, Florin Tibu.
Footnotes
Disclosures of conflicts of interest: None of the authors have competing interests related to this study.
Contributor Information
Mary Margaret Gleason, Tulane University School of Medicine, New Orleans LA, USA.
Andrei Zamfirescu, Victor Gomoiu Children’s Hospital, Bucharest, ROMANIA.
Helen L. Egger, Duke University Medical Center, Durham NC, USA.
Charles A. Nelson, III, Harvard Medical School, Boston MA, USA.
Nathan A. Fox, University of Maryland, College Park MD, USA.
Charles H. Zeanah, Tulane University School of Medicine, New Orleans LA USA.
REFERENCES
- 1.AACAP Task Force on Research Diagnostic Criteria: Infancy Preschool Age Research diagnostic criteria for infants and preschool children: the process and empirical support. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1504–1512. doi: 10.1097/01.chi.0000091504.46853.0a. [DOI] [PubMed] [Google Scholar]
- 2.Achenbach T, Rescorla L. Manual for the ASEBA Preschool form. University of Vermont; Burlington, VT: 2000. [Google Scholar]
- 3.Adler N, Mueller GO, Ayat M. Psychiatry under tyranny: A report on the political abuse of Romanian psychiatry during the Ceausescu years. Current Psychology. 1993;12:3. doi: 10.1007/BF02737088. [DOI] [PubMed] [Google Scholar]
- 4.Alonso J, Lepine J-P. Overview of key data from the European Study of the Epidemiology of Mental Disorders (ESEMeD) Journal of Clinical Psychiatry. 2007:3–9. [PubMed] [Google Scholar]
- 5.Avan B, Richter LM, Ramchandani PG, Norris SA, Stein A. Maternal postnatal depression and children’s growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Archives of Disease in Childhood. 2010;95:690–695. doi: 10.1136/adc.2009.164848. [DOI] [PubMed] [Google Scholar]
- 6.Briggs-Gowan MJ, Carter AS, Bosson-Heenan J, Guyer AE, Horwitz SM. Are Infant-Toddler Social-Emotional and Behavioral Problems Transient? Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:849–858. doi: 10.1097/01.chi.0000220849.48650.59. [DOI] [PubMed] [Google Scholar]
- 7.Briggs-Gowan MJ, Ford JD, Fraleigh L, McCarthy K, Carter AS. Prevalence of exposure to potentially traumatic events in a healthy birth cohort of very young children in the northeastern United States. Journal of Traumatic Stress. 2010;23:725–733. doi: 10.1002/jts.20593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bywater T, Hutchings J, Daley D, Whitaker C, Yeo ST, Jones K, Eames C, Edwards RT. Long-term effectiveness of a parenting intervention for children at risk of developing conduct disorder. The British Journal of Psychiatry. 2009;195:318–324. doi: 10.1192/bjp.bp.108.056531. [DOI] [PubMed] [Google Scholar]
- 9.Carter AS, Wagmiller R, Gray S, McCarthy KJ, Horwitz SM, Briggs-Gowan MJ. Prevalence of DSM-IV Disorder in a Representative, Healthy Birth Cohort at School Entry: Sociodemographic Risks and Social Adaptation. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;48:676–698. doi: 10.1016/j.jaac.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Costello EJ, Farmer EM, Angold A, Burns BJ, Erkanli A. Psychiatric disorders among American Indian and white youth in Appalachia: the Great Smoky Mountains Study. Am J Public Health. 1997;87:827–832. doi: 10.2105/ajph.87.5.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and Development of Psychiatric Disorders in Childhood and Adolescence. Arch Gen Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 12.Domenech-Llaberia E, Vinas F, Pia E, Jane MC, Mitjavila M, Corbella T, Canals J. Prevalence of major depression in preschool children. European Child & Adolescent Psychiatry. 2009;18:597. doi: 10.1007/s00787-009-0019-6. [DOI] [PubMed] [Google Scholar]
- 13.Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, Anda RF. Insights Into Causal Pathways for Ischemic Heart Disease: Adverse Childhood Experiences Study. Circulation. 2004;110:1761–1766. doi: 10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- 14.Döpfner M, Breuer D, Wille N, Erhart M, Ravens-Sieberer U. How often do children meet ICD-10/DSM-IV criteria of attention deficit-/hyperactivity disorder and hyperkinetic disorder? Parent-based prevalence rates in a national sample--Results of the BELLA study. European Child & Adolescent Psychiatry. 2008;17:59. doi: 10.1007/s00787-008-1007-y. [DOI] [PubMed] [Google Scholar]
- 15.Egger H, Erkanli A, Keeler G, Potts E, Walter B, Angold A. Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA) The Journal of the American Academy of Child and Adolesc Psychiatry. 2006;45:538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- 16.Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- 17.Florescu S, Moldovan M, Mijhaescu-Pintia C, Ciutan M, Sorel GE. Management in Health. 2007. The mental health study-Romania 2007: Prevalence, severity, and treatment of 12 month DSM-IV disorders. [Google Scholar]
- 18.Flouri E, Tzavidis N, Kallis C. Adverse life events, area socioeconomic disadvantage, and psychopathology and resilience in young children: the importance of risk factors’ accumulation and protective factors’ specificity. European Child & Adolescent Psychiatry. 2010;19:535–546. doi: 10.1007/s00787-009-0068-x. [DOI] [PubMed] [Google Scholar]
- 19.Furniss T, Beyer T, Guggenmos J. Prevalence of behavioural and emotional problems among six-years-old preschool children: Baseline results of a prospective longitudinal study. Social Psychiatry and Psychiatric Epidemiology. 2006;41:394. doi: 10.1007/s00127-006-0045-3. [DOI] [PubMed] [Google Scholar]
- 20.Furniss T, Beyer T, Mueller J. Impact of life events on child mental health before school entry at age six. European Child & Adolescent Psychiatry. 2009;18:717–724. doi: 10.1007/s00787-009-0013-z. [DOI] [PubMed] [Google Scholar]
- 21.Gater R, Jordanova V, Maric N, Alikaj V, Bajs M, Cavic T, Dimitrov H, Iosub D, Mihai A, Szalontay AS, Helmchen H, Sartorius N. Pathways to psychiatric care in Eastern Europe. The British Journal of Psychiatry. 2005;186:529–535. doi: 10.1192/bjp.186.6.529. [DOI] [PubMed] [Google Scholar]
- 22.Goodman A, Goodman R. Population mean scores predict child mental disorder rates: validating SDQ prevalence estimators in Britain. Journal of Child Psychology and Psychiatry. 2011;52:100–108. doi: 10.1111/j.1469-7610.2010.02278.x. [DOI] [PubMed] [Google Scholar]
- 23.Heckman JJ. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312:1900–1902. doi: 10.1126/science.1128898. [DOI] [PubMed] [Google Scholar]
- 24.Hölling H, Kurth B-M, Rothenberger A, Becker A, Schlack R. Assessing psychopathological problems of children and adolescents from 3 to 17 years in a nationwide representative sample: results of the German health interview and examination survey for children and adolescents (KiGGS) European Child & Adolescent Psychiatry. 2008;17:34. doi: 10.1007/s00787-008-1004-1. [DOI] [PubMed] [Google Scholar]
- 25.Hood KK, Eyberg SM. Outcomes of Parent-Child Interaction Therapy: Mothers’ Reports of Maintenance Three to Six Years After Treatment. Journal of Clinical Child & Adolescent Psychology. 2003;32:419–430. doi: 10.1207/S15374424JCCP3203_10. [DOI] [PubMed] [Google Scholar]
- 26.Huss M, Halling H, Kurth B-M, Schlack R. How often are German children and adolescents diagnosed with ADHD? Prevalence based on the judgment of health care professionals: results of the German health and examination survey (KiGGS) European Child & Adolescent Psychiatry. 2008;17:52. doi: 10.1007/s00787-008-1006-z. [DOI] [PubMed] [Google Scholar]
- 27.Ionescu C. Depression in post-communist Romania. Lancet. 2005;365:345–346. doi: 10.1016/s0140-6736(05)17964-1. [DOI] [PubMed] [Google Scholar]
- 28.Ivanovo MY, Achenbach TM, Rescorla LA, Harder VS, Ang RP, Bilenberg N, Bjarnadottir G, Capron C, De Pauw SSW, Dias P, Dobrean A, Doepfner M, Duyme M, Eapen V, Erol N, Esmaeili EM, Ezpeleta L, Frigerio A, Gonçalves MM, Gudmundsson HS, Jeng S-F, Jetishi P, Jusiene R, Kim Y-A, Kristensen S, Lecannelier F, Leung PWL, Liu J, Montirosso R, Oh KJ, Plueck J, Pomalima R, Shahini M, Silva JR, Simsek Z, Sourander A, Valverde J, Van Leeuwen KG, Woo BSC, Wu Y-T, Zubrick SR, Verhulst FC. Preschool psychopathology reported by parents in 23 societies: Testing the seven-syndrome model of the Child Behavior Checklist for ages 1.5-5. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;49:1215. doi: 10.1016/j.jaac.2010.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Keenan K, Shaw DS, Walsh B, Delliquadri E, Giovannelli J. DSM-III-R disorders in preschool children from low-income families. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:620–627. doi: 10.1097/00004583-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Kim-Cohen J, Arseneault L, Newcombe R, Adams F, Bolton H, Cant L, Delgado K, Freeman J, Golaszewski A, Kelesidi K, Matthews C, Mountain N, Oxley D, Watson S, Werts H, Caspi A, Moffitt TE. Five-year predictive validity of DSM-IV conduct disorder research diagnosis in 4 1/2-5-year-old children. European Child & Adolescent Psychiatry. 2009;18:284–291. doi: 10.1007/s00787-008-0729-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lahey BB, Applegate B. Validity of DSM-IV ADHD. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:502–503. doi: 10.1097/00004583-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Lavigne JV, Arend R, Rosenbaum D, Binns HJ, Christoffel KK, Gibbons RD. Psychiatric disorders with onset in the preschool years: I. Stability of diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1246–1254. doi: 10.1097/00004583-199812000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Lavigne JV, Gibbons RD, Christoffel KK, Arend R, Rosenbaum D, Binns H, Dawson N, Sobel H, Isaacs C. Prevalence rates and correlates of psychiatric disorders among preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:205–214. doi: 10.1097/00004583-199602000-00014. [DOI] [PubMed] [Google Scholar]
- 34.Lieberman AF, Ippen CG, Van Horn PJ. Child-Parent Psychotherapy: 6 month follow-up of a randomized controlled trial. Joural of the American Academy of Child and Adolescent Psychiatry. 2006;45:913–918. doi: 10.1097/01.chi.0000222784.03735.92. [DOI] [PubMed] [Google Scholar]
- 35.Luby JL, Belden AC, Pautsch J, Si X, Spitznagel E. The clinical significance of preschool depression: Impairment in functioning and clinical markers of the disorder. Journal of Affective Disorders. 2009;112:111–119. doi: 10.1016/j.jad.2008.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luby JL, Heffelfinger A, Mrakotsky C, Brown K, Hessler M, Spitznagel E. Alterations in Stress Cortisol Reactivity in Depressed Preschoolers Relative to Psychiatric and No-Disorder Comparison Groups. Arch Gen Psychiatry. 2003;60:1248–1255. doi: 10.1001/archpsyc.60.12.1248. [DOI] [PubMed] [Google Scholar]
- 37.Luby JL, Heffelfinger A, Mrakotsky C, Hessler M, Brown K, Hildebrand T. Preschool major depressive disorder: preliminary validation for developmentally modified DSM-IV criteria. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:928–937. doi: 10.1097/00004583-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 38.McIntosh AM, Holmes S, Gleeson S, Burns JK, Hodges AK, Byrne MM, Dobbie R, Miller P, Lawrie SM, Johnstone EC. Maternal recall bias, obstetric history and schizophrenia. The British Journal of Psychiatry. 2002;181:520–525. doi: 10.1192/bjp.181.6.520. [DOI] [PubMed] [Google Scholar]
- 39.Perna L, Bolte G, Mayrhofer H, Spies G, Mielck A. The impact of the social environment on children’s mental health in a prosperous city: an analysis with data from the city of Munich. BMC Public Health. 2010;10:199–209. doi: 10.1186/1471-2458-10-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rescorla L, Achenbach T, Ivanova MY, Dumenci L, Almqvist F, Bilenberg N, Bird H, Chen W, Dobrean A, Döpfner M, Erol N, Fombonne E, Fonseca A, Frigerio A, Grietens H, Hannesdottir H, Kanbayashi Y, Lambert M, Larsson B, Leung P, Liu X, Minaei A, Mulatu MS, Novik TS, Oh K-J, Roussos A, Sawyer M, Simsek Z, Steinhausen H-C, Weintraub S, Weisz J, Metzke CW, Wolanczyk T, Yang H-J, Zilber N, Zukauskiene R, Verhulst F. Behavioral and emotional problems reported by parents of children ages 6 to 16 in 31 societies. Journal of Emotional and Behavioral Disorders. 2007;15:130. [Google Scholar]
- 41.SAS Institute Inc. SAS 9.2. In, Cary, NC: 2008. [Google Scholar]
- 42.Scheeringa MS, Peebles CD, Cook CA, Zeanah CH. Toward establishing procedural, criterion, and discriminant validity for PTSD in early childhood. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:52–60. doi: 10.1097/00004583-200101000-00016. [DOI] [PubMed] [Google Scholar]
- 43.Scheeringa MS, Zeanah CH. Reconsideration of Harm’s Way: Onsets and Comorbidity Patterns of Disorders in Preschool Children and Their Caregivers Following Hurricane Katrina. Journal of Clinical Child and Adolescent Psychology. 2008;37:508–518. doi: 10.1080/15374410802148178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scheeringa MS, Zeanah CH, Myers L, Putnam F. Heart period and variability findings in preschool children with posttraumatic stress symptoms. Biological Psychiatry. 2004;55:685–691. doi: 10.1016/j.biopsych.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 45.Slemming K, Sørensen M, Thomsen P, Obel C, Henriksen T, Linnet K. The association between preschool behavioural problems and internalizing difficulties at age 10-12 years. European Child and Adolescent Psychiatry. 2010;19:787. doi: 10.1007/s00787-010-0128-2. [DOI] [PubMed] [Google Scholar]
- 46.Sourander A. Emotional and behavioural problems in a sample of Finnish three-year-olds. European Child & Adolescent Psychiatry. 2001;10:98–104. doi: 10.1007/s007870170032. [DOI] [PubMed] [Google Scholar]
- 47.SPSS Statistics . SPSS Statistics 17.0. In, Chicago, IL: 2008. [Google Scholar]
- 48.Thompson MJJ, Stevenson J, Sonuga-Barke E, Nott P. Mental health of preschool children and their mothers in a mixed urban/rural population: I. Prevalence and ecological factors. British Journal of Psychiatry. 1996;168:16. doi: 10.1192/bjp.168.1.16. [DOI] [PubMed] [Google Scholar]
- 49.U.S. Census Bureau . In: Child care arrangements of preschoolers by type of arrangement 1991-2005. Census, editor. 2011. [Google Scholar]
- 50.Wakschlag LS, Keenan K. Clinical significance and correlates of disruptive behavior in environmentally at-risk preschoolers. Journal of Clinical Child Psychology. 2001;30:262. doi: 10.1207/S15374424JCCP3002_13. [DOI] [PubMed] [Google Scholar]
- 51.Wakschlag LS, Leventhal BL, Thomas J, Pine DS, Narrow WE, First MB, Sirovatka PJ, Regier DA. Disruptive behavior disorders and ADHD in preschool children: Characterizing heterotypic continuities for a developmentally informed nosology for DSM-V. In: Rieger D, First MB, Narrow WE, editors. Age and gender considerations in psychiatric diagnosis: A research agenda for DSM-V. American Psychiatric Publishing, Inc.; Arlington, VA US: 2007. p. 243. [Google Scholar]
- 52.Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Hughes CW, Garber J, Malloy E, King CA, Cerda G, Sood AB, Alpert JE, Trivedi MH, Rush AJ, for the SDCT Remissions in Maternal Depression and Child Psychopathology: A STAR*D-Child Report. JAMA. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- 53.Zeanah C, Egger H, Smyke A, Nelson C, Fox N, Marshall P, Guthrie D. Institutional rearing and psychiatric disorders in Romanian preschool children. American Journal of Psychiatry. 2009;166:777–785. doi: 10.1176/appi.ajp.2009.08091438. [DOI] [PubMed] [Google Scholar]
- 54.Zeanah CH, Boris NW, Larrieu JA. Infant development and developmental risk: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:165–176. doi: 10.1097/00004583-199702000-00007. [DOI] [PubMed] [Google Scholar]
- 55.Zeanah CH, Egger HL, Smyke AT, Nelson CA, Fox NA, Marshall PJ, Guthrie D. Institutional Rearing and Psychiatric Disorders in Romanian Preschool Children. American Journal of Psychiatry. 2009;166:777–785. doi: 10.1176/appi.ajp.2009.08091438. [DOI] [PubMed] [Google Scholar]