Abstract
Number of lifetime episodes, duration of current episode, and severity of maternal depression were investigated in relation to family functioning and child adjustment. Participants were the 151 mother–child pairs in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) child multi-site study. Mothers were diagnosed with Major Depressive Disorder; children (80 males and 71 females) ranged in age from 7 to 17 years. Measures of child adjustment included psychiatric diagnoses, internalizing and externalizing symptoms, and functional impairment. Measures of family functioning included family cohesion, expressiveness, conflict, organization, and household control; parenting measures assessed maternal acceptance and psychological control. Children of mothers with longer current depressive episodes were more likely to have internalizing and externalizing symptoms, with this association being moderated by child gender. Mothers with more lifetime depressive episodes were less likely to use appropriate control in their homes.
Keywords: Maternal depression, Family functioning, Child adjustment, Gender
Introduction
Depression affects one in five women over the course of a lifetime and women in their childbearing years are particularly vulnerable (Weissman and Jensen 2002). Longitudinal studies suggest that 50% of the children of depressed mothers will experience their own depression by the time they reach adulthood (e.g., Hammen et al. 1990). These children are also at increased risk for anxiety, conduct, and substance abuse disorders (Weissman et al. 2006). Given the number of families impacted by depression, it is vital to develop a better understanding of the factors that render offspring of depressed women so vulnerable, as such information could inform both treatment and prevention strategies.
Maternal Depression and Family Functioning
Depression is known to affect an individual’s ability to parent effectively and to construct an adaptive and healthy family environment (Cummings et al. 2005; Goodman and Gotlib 2002). Maternal depression is associated with impairments in family relationships, characterized by lower levels of cohesion, warmth, and expressiveness and higher levels of conflict and affectionless control, relative to healthy families. Maternal depression has also been linked to disorganization in family activities and roles (Billings and Moos 1983; Sagrestano et al. 2003). Finally, maternal depression is associated with parenting, with depressed mothers being more irritable, critical, and controlling with their children as well as less warm and supportive, compared to non-depressed mothers (Lovejoy et al. 2000). Theoretical models (Goodman and Gotlib 1999) posit that symptoms of depression, such as sadness, irritability, and fatigue may impact parents’ ability to create and maintain a positive parent–child relationship, manage children’s behavior effectively, and meet the demands of day-to-day family life. As a result, aspects of parenting and family functioning are often theorized to be one mechanism by which maternal depression impacts youth adjustment (Burt et al. 2005).
Severity and Course of Maternal Depression
Depression is a heterogenous disorder that can vary in severity, chronicity, and duration. Some women may have mild symptoms or only one depressive episode, whereas other women may experience severe symptoms, multiple recurrences, or lengthy episodes of treatment refractory depression. Little is known about how characteristics of depression, such as severity and course of illness, may impact associations between maternal depression, family functioning, and offspring adjustment, although theoretical models suggest that these aspects of illness are important (Goodman and Gotlib 2002). There is a documented relation between length of depressive illness (Campbell et al. 1995), number of previous depressive episodes (Frankel and Harmon 1996) and disturbed parent–child interactions. Others have reported that more severe, recurrent, or long-lasting depression in parents was associated with worse outcomes in children (e.g., Brennan et al. 2000). Hammen and Brennan (2003) found that severity of maternal depression was a more potent predictor of children’s outcomes than duration of illness. It is likely that women with more severe depressive symptoms would experience more impairment in their role as a mother. Similarly, it stands to reason that a child exposed to maternal depression for a longer period of time would experience more negative effects relative to a child whose mother recovered quickly or who had only one depressive episode. Despite the intuitive nature of these assumptions, very few studies have examined these specific aspects of maternal depression, given difficulties recruiting a large enough sample of depressed women.
Maternal Depression and Child Gender
Epidemiological studies consistently demonstrate gender effects in the prevalence and age of onset of several emotional and behavioral disorders common in youth (Allgood-Merten et al. 1990; Offord et al. 1991). For example, in the general population, externalizing problems are more common in boys, while internalizing problems are more common in girls. Similarly, although depression occurs equally in young male and female children, it is twice as likely to affect female adolescents, with this gender difference continuing into adulthood (Nolen-Hoeksema and Girgus 1994). Despite these substantial gender differences, most investigations of the impact of maternal depression on youth adjustment do not consider the role of child gender (Sheeber et al. 2002); and as a result, it remains unclear whether gender may moderate the relation between maternal depressive illness and youth adjustment.
Several studies have documented a greater risk to girls from maternal depression than to boys (Davies and Windle 1997; Fergusson et al. 1995). Fergusson et al. (1995) found that maternal depression during middle childhood was related to symptoms of depression among adolescent female offspring, but not to symptoms among adolescent male offspring. Similarly, Davies and Windle (1997) found strong correlations between mothers’ depressive symptoms and daughters’ depressive, conduct, and substance use symptoms, but no correlation between maternal depression and sons’ symptoms. Family discord was found to be a mediator of girls’ adjustment problems in both studies. In contrast, Essex et al. (2003) found that maternal depression and exposure to family conflict produced differing effects by gender, with boys being more likely to display externalizing problems and girls more likely to display internalizing problems. Given these contradictory results, it remains unclear, whether girls are more vulnerable versus differentially vulnerable to the effects of maternal depression and/or family dysfunction, relative to boys (Burt et al. 2005). In other words, previous studies that demonstrated a relation between maternal depression and youth maladjustment only for girls support the idea that girls are more vulnerable to maternal depression than boys. Studies suggesting that girls and boys develop different types of psychopathology in response to maternal depression support the idea of differential vulnerability.
It is possible that maternal depression may impact boys and girls through different mechanisms. In an attempt to explain the higher rates of depression among girls, Hops (1992) posited that families may inadvertently reinforce depressive and/or gender-typic behaviors that interfere with coping in females. Having a depressed mother would provide a model for such depressive behavior and may create added stress for girls (Sheeber et al. 2002). Girls also may be more vulnerable to family dysfunction than boys because they spend more time with their parents (Montemayor 1983) and are socialized to be more relationship- and family-focused (Sheeber et al. 2002). The effect of maternal depression on boys may be transmitted through an entirely different process. For example, it is well known that maternal depression is related to deficits in child discipline (Kochanska et al. 1987) and monitoring (Sagrestano et al. 2003) which could increase risk for behavior problems in boys.
The Current Study
The current study examined associations between features of maternal depression (severity, number of lifetime episodes, and duration of current episode), family and parental functioning, children’s adjustment, and child gender using data collected from the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) Child study. STAR*D Child was an ancillary study to a larger multi-site study of treatment for adults with major depressive disorder (MDD), known as STAR*D (Trivedi et al. 2006). The primary aim of the STAR*D Child study was to examine the impact of remission or amelioration of maternal depression on children’s psychiatric and social functioning (Weissman et al. 2006).
Previous studies of maternal depression have been criticized for inconsistent definitions of depression (e.g., symptom checklists versus diagnostic criteria), or for including women with current versus a lifetime history of MDD, or with multiple types of depressive disorders (e.g., MDD, dysthymia, and adjustment disorders) (Lovejoy et al. 2000). The current study improves upon past research (e.g., Lovejoy et al. 2000) by including only women who were currently in the midst of a clinically diagnosed non-psychotic major depressive episode (MDE). Furthermore, we control for demographic factors commonly related to maternal depression, including socio-economic status, race, and marital status (Weissman et al. 2006).
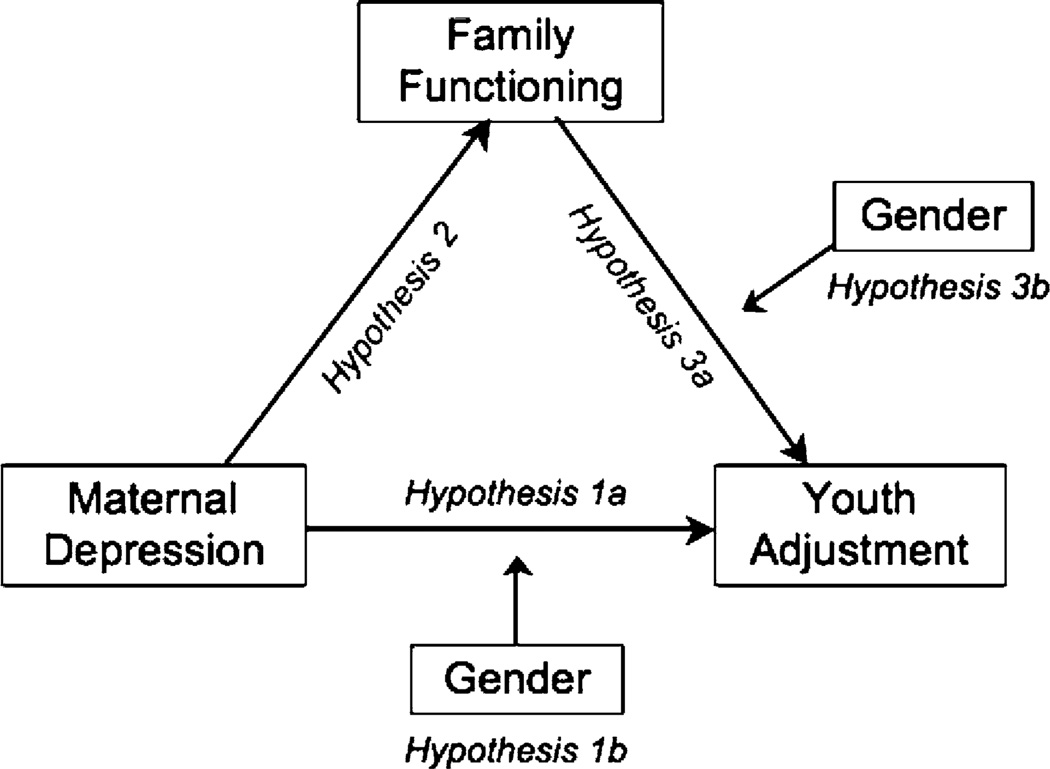
It was hypothesized (Fig. 1) that family/parental functioning would mediate the relation between maternal depression (defined as current symptom severity, duration of current episode, and number of previous MDEs) and offspring adjustment (defined as psychiatric diagnoses, symptoms of psychopathology, and psychosocial impairment). Specifically, we hypothesized (Hypothesis 1a) that higher levels of maternal depression would be related to higher levels of youth maladjustment; (Hypothesis 2) that higher levels of maternal depression would be related to less adaptive family (i.e., impaired relationships and less control/organization of the home) and parental functioning (i.e., less warmth/acceptance and more psychological control); and (Hypothesis 3) that less adaptive family/ parental functioning would be related to higher levels of adjustment problems in youth. We controlled for child age due to differences in the age of onset of internalizing and externalizing problems (Offord et al. 1991).
Fig. 1.
Conceptual model: Family/parental functioning as a mediator and gender as a moderator in the relation between aspects of maternal depression and child adjustment
We also hypothesized that child gender would moderate the relation between maternal depression and youth adjustment (Hypothesis 1b) and between family functioning and youth adjustment (Hypothesis 3b). Girls were expected to be more impaired than boys, with the association between maternal depression and internalizing disorders being greater for girls than boys. Family dysfunction was expected to be more related to adjustment among girls than boys.
Methods
Sample
This study used data collected at the baseline assessment of the ongoing longitudinal STAR*D Child study. The STAR*D study (www.star-d.org) was designed to compare the effectiveness and acceptability of different treatment options for MDD (Rush et al. 2004). Participants in STAR*D were outpatients, age 18–75, with a current diagnosis of non-psychotic MDD (Trivedi et al. 2006). Participants in STAR*D Child were recruited from 8 primary care and 11 psychiatric clinics (Weissman et al. 2006) located in eight different states within the US. Women, 25–60 years of age, with a biological child between 7 and 17 years were eligible for the STAR*D Child study (N = 177). Mothers had to be the primary caretaker for the child at least 50% of the time. Children with confirmed severe developmental disabilities or psychotic disorders were excluded. Ninety-eight percent of the 177 mother–child pairs met all study-entry criteria. Of these 174 families, 151 (87%) consented to participate. Additional information regarding eligibility and recruitment are described elsewhere (Pilowsky et al. 2006). Demographic information is presented in Table 1.
Table 1.
Demographic characteristics of sample
| Mother–child dyads (N = 151) | N (%) |
|---|---|
| Child mean age | 11.5 (SD = 2.8) |
| Mother mean age | 37.1 (SD = 6.6) |
| Child gender | |
| Boys | 80 (53) |
| Girls | 71 (47) |
| Child ethnicitya | |
| White | 67 (44) |
| Black | 56 (37) |
| Hispanic | 22 (14) |
| Other | 6 (3) |
| Child current grade | |
| Grades 1–6 | 81 (54) |
| Grades 7–12 | 68 (45) |
| Remedial/resource class | 23 (16) |
| Mother employment status | |
| Employed full or part time | 98 (65) |
| Homemaker | 20 (13) |
| Student/unemployed | 31 (21) |
| Household income | |
| Under $14,999 | 38 (27) |
| $15,000–$39,999 | 58 (40) |
| $40,000 and above | 49 (33) |
| Child living situation | |
| Biological mother only | 72 (47) |
| Both biological parents | 48 (32) |
| Biological mother and step-father | 25 (17) |
All demographic variables were investigated as potential covariates
Child ethnicity and maternal ethnicity were essentially the same, although 12 mothers reported multiple ethnic affiliations, resulting in N = 76 (50%) White and N = 58 (38%) black mothers
Measures
Maternal Depression
Participants in STAR*D received a clinical diagnosis of MDD that was confirmed by the STAR*D Clinical Research Coordinator (CRC) using a checklist interview based on DSM-IV criteria (Rush et al. 2004). Mothers also provided demographic information and a clinical history during their STAR*D baseline interview, which included number of lifetime episodes of MDD and duration of current episode. The 17-item Hamilton Rating Scale for Depression (HRSD17; Hamilton 1967) was used to assess current symptom severity. Scores can range from 0 to 52; range within this sample was 14–42. The HRSD17 is the most widely used measure of depressive symptoms in research settings; it has good reliability and is well-correlated with other observer-rated instruments (Rush et al. 2003).
Children’s Adjustment
We use the term “adjustment” as an umbrella term to capture the following constructs: (1) children’s psychiatric diagnoses, (2) symptoms of psychopathology, and (3) levels of psychosocial impairment.
The Schedule for Affective Disorders and Schizophrenia for School-Age Children- Present and Lifetime Version (K-SADS-PL; Kaufman et al. 1997) is a reliable and valid semistructured interview that generates DSM-IV Axis I child psychiatric diagnoses. In the current study, masters or doctoral level mental health professionals completed a 2-day training program at the Regional Center of the Principal Investigator (Columbia University) on the KSADS diagnostic interview. Inter-rater reliability was established (mean Kappa for diagnosis agreement = 0.87) for all interviewers (Pilowsky et al. 2006). Monthly conference calls were conducted to maintain procedural fidelity and prevent interviewer drift. Mothers and children both served as informants during the KSADS interview; information was collected yielding both current and lifetime psychiatric diagnoses.
The Child Behavior Checklist (CBCL/4–18; Achenbach 1991) was used to assess internalizing and externalizing symptoms as reported by mothers. Numerous studies have reported strong reliability and validity of the CBCL (Achenbach 1991). Coefficient alpha in this sample was 0.82 for the internalizing scale and 0.88 for the externalizing scale.
The Social Adjustment Inventory for Children and Adolescents (SAICA; John et al. 1987) assesses children’s functioning in school, spare time activities, and peer relationships via structured interview with the child. Inter-rater agreement is high for subscales (King et al. 1993), and sound validity has been reported (John et al. 1987). SAICA scales were summed to form one measure of psychosocial impairment, with scores ranging from 7.13 to 15.10 (α = 0.84). Higher scores indicate more impairment.
Family and Parental Functioning
The quality of parent–child relationships and aspects of the family environment were assessed with a variety of instruments.
Parenting
Children completed the Children’s Report of Parenting Behavior Inventory (CRPBI-30: Schludermann and Schludermann 1988), which measures perceptions of their mother’s child-rearing behaviors. It includes a ten-item Acceptance subscale and a nine-item Psychological Control subscale. Acceptance items include maternal warmth, positive affect, and nurturance of the child. Psychological control items include maternal intrusiveness and attempts to manipulate the child through guilt or other negative means. Items are scored on a scale from 0 to 2 and subscales are calculated using means of component items. Internal consistency in this sample was 0.81 for Acceptance and 0.72 for Psychological Control.
Family Functioning
Subscales from The Family Environment Scale (FES: Moos and Moos 1986, 1994) with a theoretical or empirical link to depression were included in this study. These included family cohesion (α = 0.70), expressiveness (e.g., open communication; α = 0.62), conflict (α = 0.71), organization (e.g., structure of family activities and responsibilities; α = 0.71), and control (e.g., existence of household rules; α = 0.42). Analyses suggested that internal consistency on the control subscale was related to age variability within the sample. As a result, we controlled for child age in all analyses. A composite Family Relationships Index (FRI; α = 0.68) was created by summing scores on the cohesion and expressiveness scales and subtracting scores on the conflict scale (Holahan and Moos 1982). Items on the FES are scored either 0 or 1 (true/false) and each scale consists of nine items.
Procedure
Following completion of the STAR*D baseline evaluation, women eligible for STAR*D Child were invited to participate. In accordance with each site’s Institutional Review Board, maternal consent and child assent were obtained. STAR*D Child baseline assessments were completed independently within 2 weeks of the mother’s entry into the STAR*D protocol.
Plan for Analyses
Linear regression analyses were used to test hypotheses (Fig. 1). SEM procedures were not appropriate for this study due to an insufficient number of subjects relative to the number of parameters in the model. Multi-variate models were tested initially, with non-significant predictors trimmed from the models. Established guidelines (Baron and Kenny 1986) were followed to examine whether family/parental functioning mediated the relation between maternal depression and youth adjustment. We first established a relation between maternal depression and youth adjustment (Hypothesis 1a), then tested relations between maternal depression and family/parental functioning (Hypothesis 2), and finally tested relations between family/parental functioning and youth adjustment (Hypothesis 3). Moderation analyses (Hypothesis 1b and 3b) also followed recommendations by Baron and Kenny (1986). Binary logistic regression was used when analyzing children’s diagnostic status. Dependent variables in these models included diagnosis of any depressive, anxiety, or behavioral disorder. Although this was a hypothesis driven study with specific a priori hypotheses, we chose to use a p = 0.025 that was more stringent than the standard p < 0.05 given the number of models tested. We did not use the Bonferroni correction as this is typically recommended for exploratory or post hoc analyses. Child age was controlled in all analyses due to the range of participant ages (7–17 years) and differences in ages of onset of internalizing versus externalizing symptoms. Finally, variables such as race, maternal education, occupational status, marital status, and family income were investigated as potential covariates in all analyses due to their potential relation with maternal depression. If inclusion did not alter findings, these covariates were removed from analyses.
Results
Descriptive and Demographic Information
Table 2 presents means and standard deviation for study variables for boys, girls, and the overall sample and Table 3 presents correlations among these variables.
Table 2.
Maternal depression, family functioning, and children’s adjustment
| Measure | All mean (SD) | Boys mean (SD) | Girls mean (SD) | |
|---|---|---|---|---|
| Maternal | HRSD17 | 24.73 (5.1) | 24.73 (4.65) | 24.72 (5.59) |
| Depression | Number of previous MDEs | 6.27 (12.44) | 6.0 (10.36) | 6.55 (14.54) |
| Duration current MDEa | 22.11 (39.33) | 19.96 (31.77) | 24.60 (46.73) | |
| Family | FES family rel index | 7.25 (4.96) | 7.66 (4.92) | 6.81 (4.99) |
| Functioning | FES organization | 4.82 (2.41) | 5.24 (2.16)* | 4.36 (2.59) |
| FES control | 5.20 (1.88) | 5.56 (1.74)* | 4.81 (1.96) | |
| CRPBI acceptance | 1.63 (0.35) | 1.67 (0.31) | 1.59 (0.39) | |
| CRPBI psych. control | 0.56 (0.40) | 0.55 (0.40) | 0.57 (0.41) | |
| Child | CBCL internalizing | 55.49 (10.45) | 54.82 (10.59) | 56.22 (10.32) |
| Adjustment | CBCL externalizing | 53.39 (10.56) | 53.27 (10.94) | 53.53 (10.19) |
| SAICA summary score | 10.03 (1.67) | 10.06 (1.61) | 9.99 (1.74) |
FES, Family Environment Scale; CRPBI, Children’s Report of Parenting Behavior Inventory; CBCL, Child Behavior Checklist; SAICA, Social Adjustment Inventory for Children and Adolescents
Indicates a significant difference (p< 0.05) between means for boys and girls
Duration of current MDE is reported in months
Table 3.
Correlations among measures of maternal depression, child adjustment, and family functioning
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. HRSD | – | 0.23* | 0.12 | −0.14 | −0.01 | 0.01 | 0.02 | −0.06 | −0.07 | 0.03 | 0.11 |
| 2. #MDEs | – | −0.07 | 0.02 | −0.05 | 0.09 | 0.05 | −0.03 | −0.21* | −0.13 | 0.06 | |
| 3. MDE duration | – | 0.26** | 0.24** | −0.02 | −0.04 | −0.04 | 0.09 | 0.02 | 0.07 | ||
| 4. CBCL INT | – | 0.55** | 0.01 | −0.15 | −0.17* | 0.04 | 0.00 | −0.04 | |||
| 5. CBCL EXT | – | −0.07 | −0.10 | −0.13 | 0.09 | −0.01 | −0.02 | ||||
| 6. SAICA | – | −0.10 | −0.03 | 0.07 | −0.26** | 0.25** | |||||
| 7. FES FRI | – | 0.48** | −0.16* | 0.13 | −0.04 | ||||||
| 8. FES organize | – | 0.15 | 0.15 | −0.11 | |||||||
| 9. FES control | – | 0.01 | 0.04 | ||||||||
| 10. CRPBI accept | – | −0.46** | |||||||||
| 11. CRPBI control | – |
MDEs number of major depressive episodes in mothers’ lifetime; Duration length of current MDE in months; CBCL INT, Child Behavior Checklist Internalizing Subscale; CBCL EXT, Externalizing Subscale; FRI, Family Relationship Index
p<0.05
p<0.01
Mothers
Most mothers reported a moderate to severe level of current depressive symptoms (Table 2) and recurrent depression, with a lifetime average of six MDEs. The duration of mother’s current MDE ranged from less than a month to a maximum of 24 years (mean = 22.1 months, median = 6.6, SD = 39.3). Given the positively skewed distribution of this variable, a square root transformation was performed and this transformed variable was investigated in subsequent analyses. Findings did not change when the transformed variable was used, therefore the original duration variable was used in analyses reported below.
Children
Children were within the normal range in terms of internalizing (T score mean = 55.5, SD = 10.5, range = 31–84) and externalizing (T score mean = 53.4, SD = 10.6, range = 32–82) symptoms. Based on the KSADS, 45% of children received a lifetime psychiatric diagnosis, with 19% of the sample experiencing a lifetime depressive disorder, 20% a lifetime anxiety disorder, and 29% a lifetime disruptive behavior disorder (Pilowsky et al. 2006). Boys had higher rates of KSADS disruptive behavior disorders than did girls (t = 2.0, p = 0.047; N = 28 boys, and N = 15 girls). Boys reported significantly higher levels of family organization and household control (FES) than girls (Table 2). There were no other significant gender differences.
Analyses Addressing Hypotheses
Hypothesis 1a: Relation Between Maternal Depression and Child Adjustment
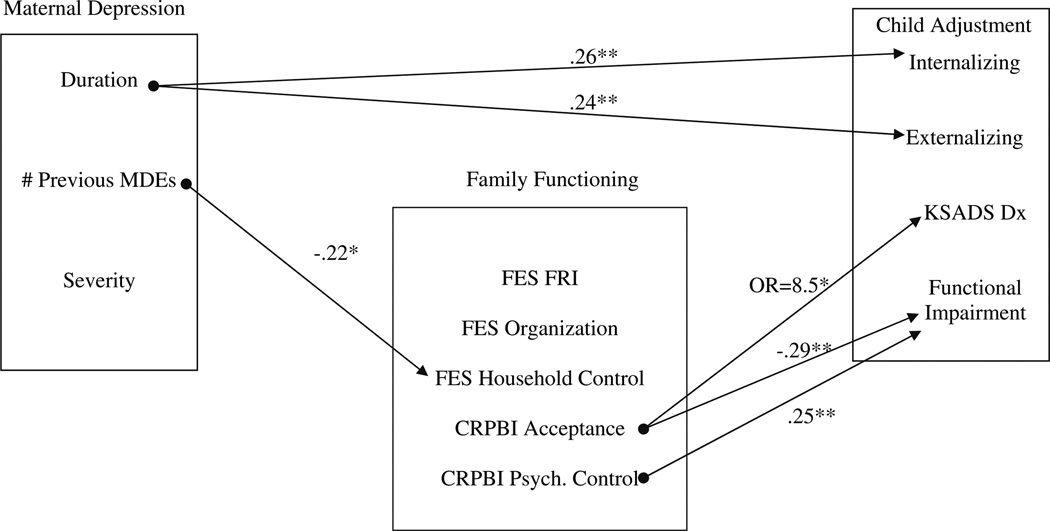
Controlling for child age, the duration of mother’s current depressive episode was significantly and positively related to children’s CBCL internalizing (β = 0.26, p = 0.002) and externalizing scores (β = 0.24, p = 0.003). Neither severity nor number of episodes of maternal depression was related to these scores. There were no significant relations between maternal depression variables and children’s psychosocial impairment, current or lifetime psychiatric diagnoses.
Hypothesis 1b
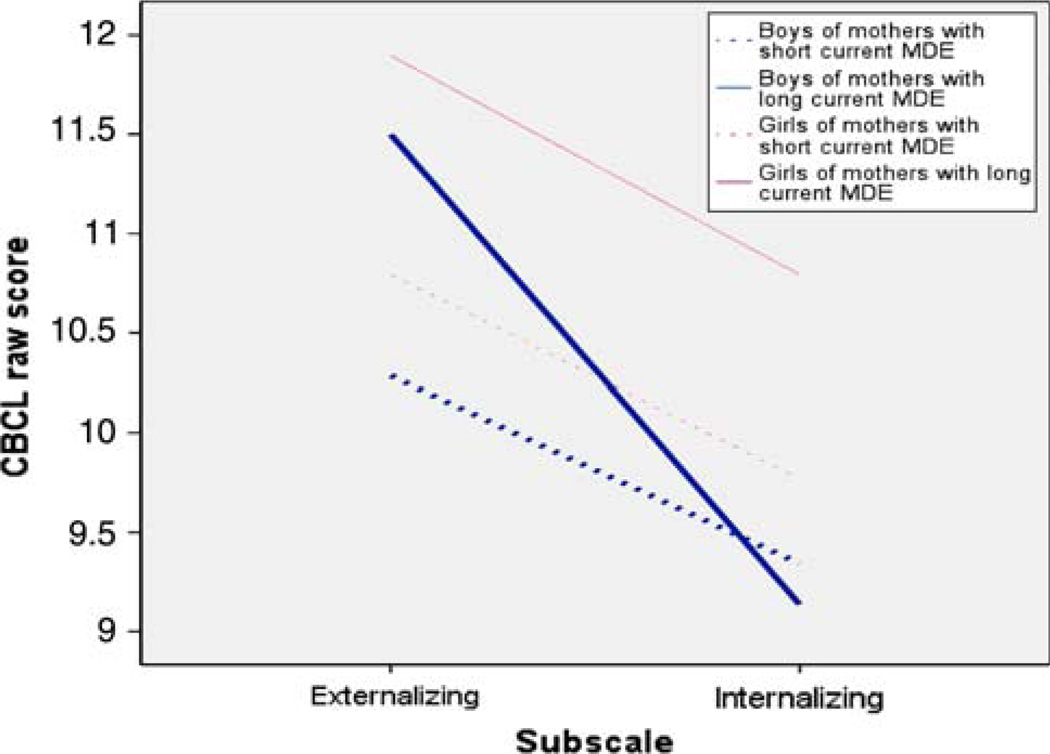
Hypotheses investigating gender as a moderator were initially tested in linear regression by creating an interaction term with the independent variable and gender. Due to a complex interaction, repeated measures ANCOVA was used to allow internalizing and externalizing subscales to be examined in the same model. In this model, the within subjects factor was subscale score (i.e., internalizing or externalizing), the between subjects factor was the sex of the child, and the covariates were duration of maternal depression and child age. Two repeated measures ANCOVA models were conducted. In the first model (main effects only), there were significant effects of child gender and duration of the current MDE. In the second model, all possible interaction terms were added, to allow the model to fit a separate slope for duration of mothers’ depression for each combination of gender, internalizing, and externalizing. In addition to a main effect of duration and a significant two-way interaction between duration and subscale, there was a significant three-way interaction between duration of depression, gender, and CBCL subscale (t = –2.28, p = 0.023). Slopes of each line (Fig. 3) were as follows: Girls internalizing = 0.050, girls externalizing = 0.029, boys internalizing = 0.040, boys externalizing = 0.094. Among girls, there was a larger relation between duration of mothers’ current MDE and internalizing symptoms and, among boys, a larger relation between depression and externalizing symptoms. Post hoc regression analyses with the sample divided by gender, revealed that the duration of mothers’ current MDE was related positively to internalizing problems among girls (β = 0.33, p = 0.007) and to externalizing problems among boys (β = 0.35, p = 0.002).
Fig. 3.
Gender as a moderator in the relation between duration of maternal depression and youth internalizing and externalizing symptoms. Note: MDE major depressive episode. Short and long duration of maternal depression were defined using a median split. This was more appropriate than using SD due to the positively skewed duration variable
Hypothesis 2: Relation Between Maternal Depression and Family Functioning
There was a significant negative relation between mothers’ lifetime MDEs and ratings on the FES of the amount of control parents exercised within their home (β = –0.22, p = 0.024). There were no significant relations between maternal depression and other subscales on the FES or CRPBI.
Hypothesis 3: Relation Between Family Functioning and Child Adjustment
There were no significant associations between measures of family/parental functioning and children’s internalizing and externalizing symptoms. Significant relations were found with respect to youth psychosocial impairment (SAICA). Higher levels of perceived maternal psychological control were related to higher levels of youth impairment (β = 0.25, p = 0.002) whereas higher levels of perceived maternal acceptance were related to lower levels of impairment (β = –0.29, p = 0.001). Although gender did not moderate this relation (Baron and Kenny 1986), subsequent analyses suggest that the relation between parenting and youth impairment is different in subsamples of boys and girls. Among girls, psychological control (β = 0.34, p = 0.009) and acceptance (β = –0.32, p = 0.01) were related to psychosocial impairment; these parenting variables were not related to boys’ psychosocial impairment. Subsample analyses were conducted because of known gender differences in prevalence rates of certain disorders among youth (e.g., Allgood-Merten et al. 1990) and because of the lack of information in the field regarding gender differences in the relations among maternal depression, family functioning, and youth adjustment (Sheeber et al. 2002). There were no relations between measures of family environment and children’s impairment. Controlling for child age, children’s reports of maternal acceptance were positively related to current anxiety disorder diagnoses (OR = 8.54, p = 0.024). There were no significant relations between other aspects of family/parental functioning and children’s diagnostic status.
Mediational Analyses
Although our results suggest a number of important relations between maternal depression, family functioning, and children’s adjustment, consistent relations between variables on all three paths in the mediational model were not found.
Discussion
Our results highlight the importance of considering dimensions of maternal depression, such as chronicity and recurrence (Brennan et al. 2000; Goodman and Gotlib 1999) when studying associations among maternal depression, family functioning, and child adjustment. As hypothesized, duration of mother’s current episode of MDD was significantly related to children’s internalizing and externalizing symptoms and this association was moderated by child gender. For girls, longer current maternal depressive episodes were significantly associated with higher levels of internalizing problems; whereas, for boys, longer current maternal depressive episodes were significantly associated with higher levels of externalizing problems. These findings are consistent with theories (e.g., Hops 1992) that suggest that familial mechanisms place girls at risk for depression, but differ from empirical studies that have found girls to be more vulnerable to maternal depression than boys (e.g., Davies and Windle 1997). Our data suggest that boys are vulnerable as well, but may be more prone to externalizing than internalizing symptoms. This pattern is consistent with gender differences in rates of internalizing versus externalizing disorders in youth (e.g., Offord et al. 1991).
Although duration of maternal illness was related to children’s adjustment, there was no relation between mothers’ current symptom severity or number of previous MDEs and children’s adjustment. This is somewhat discrepant with past studies that have included mothers at various stages of illness (e.g., Brennan et al. 2000). Our findings may be due to a restriction of range. All mothers in our study were in a clinically diagnosed episode of MDD and 72% reported a severe level of symptoms (Pilowsky et al. 2006), with little variability across participants; this may have obscured our ability to find significant relations between severity and other variables.
A recurrent course of maternal depression was related to the amount of control mothers exercised within their home. Consistent with literature demonstrating a link between maternal depression and poor child behavior management/ discipline (Lovejoy et al. 2000), this finding suggests that women with recurrent MDEs are less likely to structure their homes using set rules and procedures and less likely to be viewed as “in charge” in the home setting.
In this sample of currently depressed women and their children, measures of parental/family functioning were associated with children’s psychiatric diagnoses and psychosocial impairment. Maternal psychological control (e.g., using guilt-induction to manipulate the child) was associated with more impairment in offspring, whereas maternal acceptance (e.g., smiling and praising often) was associated with less youth impairment. These aspects of parenting may be potential targets of interventions with depressed mothers, as both are related to children’s impairment across three domains: school, peer, and free-time activities. Contrary to expectation, high levels of maternal acceptance were associated with increased odds of anxiety disorders. This finding is in need of replication before interpretation is warranted.
Child gender did not moderate associations between family functioning and child adjustment, although different patterns were evident within subsamples of girls and boys. Among girls, problems in parenting (high psychological control and low maternal acceptance) were related to increased psychosocial impairment. This is consistent with theories suggesting that girls may be particularly sensitive to family discord (e.g., Sheeber et al. 2002). The fact that these associations were found for girls but not boys suggests possible gender differences in the processes by which the parenting of depressed mothers is related to child outcomes.
Duration of maternal illness was associated with symptoms of child psychopathology, but not with aspects of family/parental functioning that were related to child adjustment. Thus, although important direct associations were found, the criteria for mediation were not met. Simple exposure to a depressed mother may account for much of the variance in child outcome. Depressed mothers could impact their children by modeling depressive coping or by exposing them to chronic irritability. Shared biological vulnerabilities may also play a role. Depression may impact family functioning differently depending on child age, SES, or ethnicity and this variability may have obscured our ability to find mediational patterns in the data.
Limitations
Several important limitations of this study should be noted. All data for this study were collected within a 2-week interval, precluding our ability to examine longitudinal/ prospective relations or directional effects. For example, mothers of boys with externalizing problems may be more likely to have depressions of longer duration due to the difficulties associated with parenting these children. It also is possible that an unmeasured variable might influence both mother and child functioning (e.g., maternal depression and daughters’ internalizing symptoms due to common stressors such as economic hardships or abuse). Prospective studies are needed to test the likely possibility of more complex, transactional relations.
Common informant and common method variance were limitations in some analyses. Mothers provided information about their functioning and, for several variables, their children’s functioning. It is possible that mothers were overly negative in their reports about their children’s functioning due to their depression. There is disagreement in the field regarding whether the reports of depressed women are biased by negative mood or whether they accurately reflect deficits in children’s behavior (Najman et al. 2000; Richters 1992). Although this is a potential study limitation, given that all women were depressed and given that the mean of the mother-rated CBCL was within the normal range, it is unlikely that bias could fully account for a relation between length of maternal depression and child adjustment or child gender.
Because of the wide age range of children and the modest sample size, we were not able to examine relations among study variables at specific developmental stages. It is likely that the impact of maternal depression on youth outcomes may be influenced by the child’s age, with some studies suggesting that maternal depression may be more harmful when present during a child’s early life (Forman et al. 2007). Finally, as participants in the larger STAR*D clinical trial, all women in this study were seeking treatment for their depression. Given data to suggest that only 1/3 of mentally ill individuals seek treatment (Kessler et al. 1996), the current sample was not necessarily representative of the larger population of depressed mothers and their families.
Conclusions
This study investigated relations between dimensions of maternal depression, family functioning, and child adjustment in a sample of currently depressed women. The duration of the current maternal depressive episode related to youth psychopathology-specifically to internalizing problems for girls and externalizing problems for boys. A recurrent course of maternal depression was related to lower levels of household control. Finally, mothers’ use of psychological control was related to higher levels of psychosocial impairment for girls, but not boys; and similarly, mothers’ use of warm and accepting parenting techniques was related to improved psychosocial functioning among girls, but not boys.
Fig. 2.
Summary of significant associations among variables in hypothesized model. Note: FES, Family Environment Scale; FRI, Family Relationships Index; CRPBI, Children’s Report of Parenting Behavior Inventory; CBCL, Child Behavior Checklist; SAICA, Social Adjustment Inventory for Children and Adolescents. Values are standardized Beta weights. OR odds ratio. *p<0.05, **p<0.01
Acknowledgments
We are grateful to the seven participating STAR-D Regional Centers: Massachusetts General Hospital, Boston, MA, Primary Investigator: Andrew Nierenberg, MD; University of California, San Diego, CA, Primary Investigator: Sid Zisook, MD; University of Michigan, Ann Arbor, MI, Primary Investigator: Elizabeth Young, MD; University of North Carolina, Chapel Hill, NC, Primary Investigator: Bradley Gaynes, MD, MPH; University of Texas Southwestern Medical Center, Dallas, TX, Primary Investigator: Mustafa Husain, MD; Vanderbilt University, Nashville, TN, Primary Investigator: Steven Hollon, Ph.D.; and Virginia Commonwealth University, Richmond, VA, Co-Principal Investigator: A. Bela Sood, MD. We are also grateful to Ardesheer Talati, Ph.D., Charlene Bryan, MA, Kenneth Guire, MA, and Joe Kazemi, MA for their assistance with analyses and comments on earlier versions of this manuscript. This study was supported by NIMH grant no. R01MH063852 (M. M. Weissman, PI) and by an NIMH contract (no. N01 MH90003) (A. John Rush, PI). Dr. Garber was supported in part by an Independent Scientist Award during completion of this work (K02 MH66249).
Biographies
Cynthia Ewell Foster is a Clinical Lecturer at the University of Michigan. She received her Ph.D. in child clinical psychology from Loyola University Chicago. Her major research interests include youth depression, suicide prevention, and community interventions.
Melissa Webster is a clinical social worker at the University of Michigan. She received her MSW from the University of Michigan. Her research interests include youth depression and anxiety and suicide prevention.
Myrna Weissman is a Professor of Psychiatry and Epidemiology at Columbia University and the New York State Psychiatric Institute. She is the PI of the STAR*D Child Study. She received a Ph.D. in Chronic Disease Epidemiology from Yale University. Her research has focused on the generational transmission of depression and other psychiatric illnesses.
Daniel Pilowsky is an Assistant Professor of Psychiatry and Public Health (Epidemiology) at Columbia University. He received his MD at the University of Buenos Aires. His research interests include children at risk for depression, interpersonal psychotherapy, and HIV prevention.
Priya Wickramaratne is an Associate Professor of Clinical Biostatistics in Psychiatry at Columbia University. She received her Ph.D. in Biostatistics from Yale University. Her research interests focus on epidemiological methods, observational studies, survival analysis, and generalized linear models.
A. John Rush is a Professor of Clinical Sciences and Psychiatry at the University of Texas Southwestern Medical Center and the Principal Investigator of the STAR*D multi-site study. He received his MD from Columbia College of Physicians and Surgeons. His research interests include mood disorders and their treatment.
Carroll Hughes is a Professor of Psychiatry at the University of Texas Southwestern Medical Center. He received his Ph.D. in clinical psychology at the University of South Carolina. His research interests focus on pediatric depression and the effects of maternal depression on children and adolescents.
Judy Garber is a Professor of Psychology and Human Development at Vanderbilt University. She received her Ph.D. in clinical psychology from the University of Minnesota. Her research focuses on developmental psychopathology, particularly the etiology, treatment, and prevention of youth mood disorders.
Erin Malloy is an Associate Professor at the University of North Carolina, Chapel Hill. She received her medical degree from the University of Florida. Her interests include inpatient treatment of children and adolescents and medical education.
Gabrielle Cerda MD is an Assistant Clinical Professor of Psychiatry and the Medical Director of Children’s Outpatient Psychiatry at the University of California. Her interests include treatment of psychiatric disorders in youth and medical education.
Susan Kornstein MD is Professor of Psychiatry and Obstetrics and Gynecology at Virginia Commonwealth University. She received her MD at Brown University. Her research focuses on women’s health and depression.
Jonathan Alpert is Associate Professor of Psychiatry at Harvard University Medical School and Associate Director of the Depression Clinical and Research Program at Massachusetts General Hospital. He received his MD from Yale University and his Ph.D. from Cambridge University. His research focuses on psychopharmacologic treatment and subtypes of major depression.
Stephen Wisniewski is an Associate Professor of Epidemiology with the University of Pittsburgh. He received his Ph.D. in Epidemiology from the University of Pittsburgh. His research focuses on the design and analysis of clinical trials.
Madhukar Trivedi MD is Professor of Psychiatry, Director of the Mood Disorders Research Program at the University of Texas Southwestern Medical Center and Co-Principal Investigator of the STAR*D multi-site study. He received his MD from Baroda Medical College. His research interests focus on evidence-based treatment of depression.
Maurizio Fava is a Professor of Psychiatry at Harvard University Medical School. He received his MD from the University of Padova School of Medicine. His research focuses on psychopharmacologic treatment of depression.
Cheryl King is an Associate Professor at the University of Michigan. She received her Ph.D. in clinical psychology from Indiana University. Her research interests include youth depression and suicide prevention.
Contributor Information
Cynthia Ewell Foster, Department of Psychiatry, University of Michigan, Child and Adolescent Psychiatry Section, 4250 Plymouth Rd., Ann Arbor, MI 48109, USA.
Melissa C. Webster, Department of Psychiatry, University of Michigan, Child and Adolescent Psychiatry Section, 4250 Plymouth Rd., Ann Arbor, MI 48109, USA
Myrna M. Weissman, Columbia University and the New York State Psychiatric Institute, New York, NY, USA
Daniel J. Pilowsky, Columbia University and the New York State Psychiatric Institute, New York, NY, USA
Priya J. Wickramaratne, Columbia University and the New York State Psychiatric Institute, New York, NY, USA
A. John Rush, University of Texas Southwestern Medical Center, Dallas, TX, USA.
Carroll W. Hughes, University of Texas Southwestern Medical Center, Dallas, TX, USA
Judy Garber, Vanderbilt University, Nashville, TN, USA.
Erin Malloy, University of North Carolina, Chapel Hill, NC, USA.
Gabrielle Cerda, University of California, San Diego, CA, USA.
Susan G. Kornstein, Virginia Commonwealth University, Richmond, VA, USA
Jonathan E. Alpert, Harvard University, Cambridge, MA, USA
Stephen R. Wisniewski, University of Pittsburgh, Pittsburgh, PA, USA
Madhukar H. Trivedi, University of Texas Southwestern Medical Center, Dallas, TX, USA
Maurizio Fava, Harvard University, Cambridge, MA, USA.
Cheryl A. King, Department of Psychiatry, University of Michigan, Child and Adolescent Psychiatry Section, 4250 Plymouth Rd., Ann Arbor, MI 48109, USA, kingca@umich.edu
References
- Achenbach T. Manual for the CBCL 4–18, 1991 Profile. Burlington, VT: University of Vermont. Department of Psychiatry; 1991. [Google Scholar]
- Allgood-Merten B, Lewinsohn PM, Hops H. Sex differences and adolescent depression. Journal of Abnormal Psychology. 1990;99:55–63. doi: 10.1037//0021-843x.99.1.55. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategies, and statistical considerations. Journal of Personality and Social Psychology. 1986;61:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Billings AG, Moos RH. Comparisons of children of depressed and non-depressed parents: A social-environmental perspective. Journal of Abnormal Child Psychology. 1983;11:463–486. doi: 10.1007/BF00917076. [DOI] [PubMed] [Google Scholar]
- Brennan P, Hammen C, Andersen M, Bor W, Najman J, Williams G. Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Developmental Psychology. 2000;36:759–766. doi: 10.1037//0012-1649.36.6.759. [DOI] [PubMed] [Google Scholar]
- Burt KB, Van Dulmen MHM, Carlivati J, Egeland B, Sroufe LA, Forman DR, Appleyard K, Carlson EA. Mediating links between maternal depression and offspring psychopathology: The importance of independent data. Journal of Child Psychology and Psychiatry. 2005;46:490–499. doi: 10.1111/j.1469-7610.2004.00367.x. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Cohn JF, Meyers TA. Depression in first-time mothers: Mother-infant interaction and depression chronicity. Developmental Psychology. 1995;31:349–357. [Google Scholar]
- Cummings EM, Keller PS, Davies PT. Towards a family process model of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functions. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Davies P, Windle M. Gender-specific pathways between maternal depressive symptoms, family discord, and adolescent adjustment. Developmental Psychology. 1997;33:657–668. doi: 10.1037//0012-1649.33.4.657. [DOI] [PubMed] [Google Scholar]
- Essex MJ, Klein MH, Cho E, Kraemer HC. Exposure to maternal depression and marital conflict: Gender differences in children’s later mental health symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:728–737. doi: 10.1097/01.CHI.0000046849.56865.1D. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MT. Maternal depressive symptoms and depressive symptoms in adolescents. Journal of Child Psychology and Psychiatry. 1995;36:1161–1178. doi: 10.1111/j.1469-7610.1995.tb01363.x. [DOI] [PubMed] [Google Scholar]
- Forman DR, O’Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother–child relationship. Development and Psychopathology. 2007;19:585–602. doi: 10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- Frankel KA, Harmon RJ. Depressed mothers: They don’t always looks as bad as they feel. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:289–298. doi: 10.1097/00004583-199603000-00009. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: APA; 2002. [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry. 2003;60:253–258. doi: 10.1001/archpsyc.60.3.253. [DOI] [PubMed] [Google Scholar]
- Hammen C, Burge D, Burney E, Adrian C. Longitudinal study of diagnoses in children of women with unipolar and bipolar affective disorder. Archives of General Psychiatry. 1990;47:1112–1117. doi: 10.1001/archpsyc.1990.01810240032006. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH. Social support and adjustment: Predictive benefits of social climate indices. American Journal of Community Psychology. 1982;10:403–415. doi: 10.1007/BF00893979. [DOI] [PubMed] [Google Scholar]
- Hops H. Parental depression and child behaviour problems: Implications for behavioural family intervention. Behaviour Change. 1992;9:126–138. [Google Scholar]
- John K, Gammon GD, Prusoff BA, Warner V. The social adjustment inventory for children and adolescents (SAICA): Testing of a new semi-structured interview. Journal of the American Academy of Child and Adolescent Psychiatry. 1987;26:898–911. doi: 10.1097/00004583-198726060-00015. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McKinagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. American Journal of Orthopsychiatry. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- King C, Segal H, Naylor M, Evans T. Family functioning and suicidal behavior in adolescent inpatients with mood disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:1198–1206. doi: 10.1097/00004583-199311000-00013. [DOI] [PubMed] [Google Scholar]
- Kochanska G, Kucynski L, Radke-Yarrow M, Welsh JD. Resolutions of control episodes between well and affectively ill mothers and their young child. Journal of Abnormal Child Psychology. 1987;15:441–456. doi: 10.1007/BF00916460. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Montemayor R. Parents and adolescents in conflict: All the families some of the time and some families most of the time. Journal of Early Adolescence. 1983;3:83–103. [Google Scholar]
- Moos RH, Moos BS. Family environment scale manual. 2nd and 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1986, 1994. [Google Scholar]
- Najman JM, Williams GM, Nikles J, Spence S, Bor W, O’Callaghan M, LeBrocque R, Andersen MJ. Mothers’ mental illness and child behavior problems: Causeeffect association or observation bias? Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:592–602. doi: 10.1097/00004583-200005000-00013. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Offord D, Boyle M, Racine Y. Ontario child health study: Correlates of disorder. In: Chess S, Hertzig M, editors. Annual progress in child psychiatry and child development. Philadelphia: Bruner/Mazel; 1991. [Google Scholar]
- Pilowsky DJ, Wickramaratne P, Rush AJ, Hughes CW, Garber J, Malloy E, et al. Children of currently depressed mothers: A STAR*D ancillary study. Journal of Clinical Psychiatry. 2006;67:126–136. doi: 10.4088/jcp.v67n0119. [DOI] [PubMed] [Google Scholar]
- Richters JE. Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychological Bulletin. 1992;112:485–499. doi: 10.1037/0033-2909.112.3.485. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Fava M, Wisniewski SR, Lavori PW, Trivedi MH, Sackheim HA, et al. Sequenced treatment alternatives to relieve depression (STARD*D): Rationale and design. Controlled Clinical Trials. 2004;25:119–142. doi: 10.1016/s0197-2456(03)00112-0. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-item quick inventory of depressive symptomatology (QIDS, clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Sagrestano LM, Paikoff RL, Holmbeck GN, Fendrick M. A longitudinal examination of familial risk factors for depression among inner-city African American adolescents. Journal of Family Psychology. 2003;17:108–120. [PubMed] [Google Scholar]
- Schludermann EH, Schludermann SM. Children’s Report on Parent Behavior (CRPBI-108, CRPBI-30) for older children and adolescents (Tech. Rep.) Winnipeg, MB, Canada: University of Manitoba, Department of Psychology; 1988. [Google Scholar]
- Sheeber L, Davis B, Hops H. Gender-specific vulnerability to depression in children of depressed mothers. In: Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: APA; 2002. [Google Scholar]
- Trivedi MH, Rush JA, Wisniewski SR, Nierenberg A, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: Implications for clinical practice. American Journal of Psychiatry. 2006;163:28–41. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Jensen P. What research suggests for depressed women with children. Journal of Clinical Psychiatry. 2002;63:641–647. doi: 10.4088/jcp.v63n0717. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, et al. Remissions in maternal depression and child psychopathology: A STAR*D-child report. JAMA. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. The American Journal of Psychiatry. 2006;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]