Abstract
The mammalian Forkhead Box (Fox) transcription factor FoxM1b is implicated in tumorigenesis. However, the presence of expression and role of FoxM1b in gastric cancer remain unknown. Therefore, we investigated FoxM1b expression in 86 cases of primary gastric cancer and 57 normal gastric tissue specimens. We further investigated the underlying mechanisms of altered FoxM1b expression in and the impact of this altered expression on gastric cancer growth and metastasis using in vitro and animal models of gastric cancer. We found weak expression of FoxM1b protein in the mucous neck region of gastric mucosa, whereas we observed strong staining for FoxM1b in tumor-cell nuclei in various gastric tumors and lymph node metastases. A Cox proportional hazards model revealed that FoxM1b expression was an independent prognostic factor in multivariate analysis (P < 0.001). Experimentally, overexpression of FoxM1b by gene transfer significantly promoted the growth and metastasis of gastric cancer cells in orthotopic mouse models, whereas knockdown of FoxM1b expression by small interfering RNA did the opposite. Promotion of gastric tumorigenesis by FoxM1b directly and significantly correlated with transactivation of vascular endothelial growth factor (VEGF) expression and elevation of angiogenesis. Given the importance of FoxM1b to regulation of the expression of genes key to cancer biology overall, dysregulated expression and activation of FoxM1b may play important roles in gastric cancer development and progression.
Keywords: FoxM1b, angiogenesis, metastasis, VEGF, stomach
Introduction
Although the incidence of gastric cancer declined in the West from the 1940s to the 1980s, it remains a major public health problem throughout the world and the cause of 12% of all cancer-related deaths each year (1, 2). The aggressive nature of human gastric cancer is a result of a variety of intracellular events, including activation of various oncogenes, inactivation of tumor suppressor genes, and abnormal expression of growth factors and their receptors (3, 4). These abnormalities affect the downstream signal transduction pathways involved in the control of cancer biology, including an increased angiogenesis phenotype of gastric cancer cells (4–9). Previous studies also showed that microvessel density (MVD) and expression of various angiogenic factors related to tumor development and progression are predictive of survival in patients with gastric cancer (4, 10, 11). However, the molecular mechanisms responsible for abnormal expression of many of these angiogenic factors in gastric cancer, including VEGF, remain unclear. Increasing evidence suggests that VEGF expression is regulated by various hormones and growth factors and oncogenic proteins through various transcription factors, including Sp1, hypoxia-inducible factor-1, signal transducer and activator of transcription 3 (Stat3), and possibly the mammalian Forkhead Box (Fox) transcription factor FoxM1 (12, 13).
FoxM1 shares homology in the winged-helix DNA-binding domain (14–20) and is predominantly expressed at the mRNA level in fetal tissue and also its expression is maintained ubiquitously in all proliferating adult tissues and some cancer cell lines (16, 18–22), whereas its expression is absent from differentiated cells (16, 19). Researchers have shown that FoxM1 is a key cell-cycle regulator of both the transition from G1 to S phase and progression to mitosis (21, 23–28). For example, several studies showed that FoxM1 is essential for mediating the progression from G2 to M phase and chromosome segregation (23, 24) and that loss of FoxM1 expression causes centrosome amplification and mitotic catastrophe (25). Furthermore, FoxM1 regulates the transcription of cell cycle genes essential for G1-S and G2-M progression and for chromosome stability and segregation (21–26, 29–31). Moreover, investigators identified FoxM1 as a novel target of human papillomavirus type 16 E7 protein, which may be important for cell transformation (22). Therefore, altered FoxM1 expression can contribute to oncogenesis, presumably through its critical role in cell proliferation.
This notion is apparently supported by the fact that FoxM1b is highly expressed in various types of cancer (25, 30–41). Interestingly, abnormal activation of FoxM1b may cause overexpression of multiple angiogenic molecules, which in turn render tumor cells highly angiogenic (35). In the present study, we sought to determine the potential role of FoxM1b expression in gastric cancer development and progression and the underlying mechanisms of this expression.
Materials and Methods
Human tissue specimens and patient information
Human gastric tumor specimens preserved in the Gastric Cancer Tissue Bank at The University of Texas M. D. Anderson Cancer Center were used. The patient characteristics information has been described in detail previously (12) and are also summarized in Supplemental Table 1.
Cell Lines and Xenograft Models
The human gastric cancer cell lines NCI-N87, AGS, HTB103, HTB135, SNU1, and SNU-16 were purchased from the American Type Culture Collection (Manassas, VA), the SK-GT5 cell line was obtained from Gary K. Schwartz (Memorial Sloan-Kettering Cancer Center) and TMK-1 cell line was obtained from Masashi Kanai (Kyoto University). The growths of those tumor cell lines in nude mice were determined as described previously (42).
Immunohistochemistry and Quantification of tumor MVD
Sections (5 µm thick) of formalin-fixed, paraffin-embedded gastric tumor specimens were prepared and processed for immunostaining using a rabbit polyclonal antibody against human FoxM1b (K-19 [sc-500]; Santa Cruz Biotechnology; 1:50 dilution), a rabbit polyclonal antibody against human VEGF (clone A-20 [SC-152]; Santa Cruz Biotechnology; 1:100 dilution), a rabbit polyclonal antibody against human PCNA (sc-7907, Santa Cruz; 1:200 dilution) and a monoclonal goat anti-CD34 antibody (PECAM1-M20; Santa Cruz Biotechnology; 1:100 dilution) for MVD. The molecular markers were determined in the different sections of a same tissue block from each patient. Also, frozen sections (5 µm thick) of human gastric tumor xenograft specimens were fixed in acetone for CD31 (BD Pharmingen, San Diego; 1:100 dilution) staining. Quantifications of gene expression and tumor MVD were performed as described previously (12).
Western blot analysis
Whole cell lysates were prepared from human gastric cancer cell lines and human normal gastric tissue and gastric tumor specimens. Standard Western blotting was performed using a polyclonal rabbit antibody against human FoxM1b (K-19 [sc-500]), a polyclonal rabbit antibody against human VEGF, and anti-rabbit IgG, a horseradish peroxidase-linked F(ab')2 fragment obtained from a donkey (Amersham Life Sciences). Equal protein sample loading was monitored by incubating the same membrane filter with an anti-β-actin antibody. The probe proteins were detected using the Amersham ECL system according to the manufacturer’s instructions.
Stable and transient transfection of gastric cancer cells
Full-length human FoxM1b was released by EcoRI and XbaI digestion of the cytomegalovirus human FoxM1b cDNA expression vector (20) and subcloned into pcDNA3.1 (Invitrogen) to generate the pcDNA3.1-FoxM1b plasmid expression vector. Also, four FoxM1-small interfering RNAs (siRNAs) were designed and synthesized by Qiagen to generate a FoxM1b-siRNA expression vector for gene-knockdown studies. An siRNA with the sequence CUCUUCUCCCUCAGAUAUAdTdT (with a target location between nucleotide 2073 and nucleotide 2091 from the translation start site of FoxM1b mRNA) was determined to be the most effective siRNA in inhibiting FoxM1b expression. The FoxM1b-siRNA was further incorporated into the pSilencer plasmid (Ambion). A pSilencer neo vector expressing a hairpin siRNA with limited homology with any known sequences in the human, mouse, and rat genomes (Ambion) was used as a negative control. GT5 and N87 cells were transfected with the FoxM1b-siRNA expression vector or the control vector using Lipofectamine 2000 (Invitrogen). The cells stably transfected were isolated using neomycin (G418) selection after the cells were transfected with pcDNA3.1-FoxM1b or control plasmids.
Analysis of VEGF promoter activity
The activity of pV2274, pV109, and mutant VEGF promoter constructs was analyzed as described previously (42). In brief, plasmids containing firefly luciferase reporters were co-transfected into gastric tumor cells in triplicate with an internal control pMiniTK-RL using the Lipofectamine method (Invitrogen). The pMiniTK-RL contained a full-length Renilla luciferase gene under the control of a minimal thymidine kinase promoter (636–757 bp from pTK-RL; Invitrogen). In some of the experiments, the reporters were co-transfected with pcDNA3.1-FoxM1b, pcDNA3.1, or the Validated Stealth RNAi duplex oligonucleaotides for Sp1 (5'-GCAGACACAGCAGCAACAAAUUCUU-3') (Invitrogen). The activity of both the firefly and Renilla luciferase reporters was determined 48 h later using the Dual Luciferase Assay kit (Promega). The specific VEGF promoter activity was calculated as described previously (42).
Endothelial Cell Tube Formation Assay
The tube formation assay was done as described previously (13) with a modification of using conditioned medium from N87 cells, FoxM1b-siRNA- or pcDNA3.1-FoxM1b-transfected N87 cells.
Statistical analysis
The two-tailed chi-square test was used to determine the significance of the difference between the covariates. Survival durations were calculated using the Kaplan-Meier method. The log-rank test was used to compare the cumulative survival in the patient groups. A Cox proportional hazards model was used to calculate univariate and multivariate hazard ratios for the study variables. The FoxM1b and VEGF expression levels, MVD, age, Lauren’s histologic classification, stage (American Joint Committee on Cancer system), and completeness of surgical resection (R0 versus R1 or R2) were included in the model. The significance of the in vitro data was determined using the Student t-test (two-tailed), whereas that of the in vivo data was determined using the two-tailed Mann-Whitney U test. In all of the tests, P values less than 0.05 were considered statistically significant. The SPSS software program (version 12.0; SPSS, Inc.) was used for statistical analyses.
Results
FoxM1b overexpression and its direct association with poor prognosis in patients with gastric cancer
We observed weakly positive FoxM1b staining predominantly in the nuclei of cells in normal gastric mucous neck region and in the cytoplasm of cells in the glandular epithelium, whereas we did not detect FoxM1b expression in the cells located toward the gastric pit. In sharp contrast, we observed much higher levels of FoxM1b expression in the nuclei of various types of gastric cancer cells (Fig. 1A; Supplemental Fig. 1). Consistent with the level of FoxM1b protein expression determined using Western blot analysis (Fig. 1B), our immunostaining results showed that primary gastric tumors and metastatic lymph nodes had significantly higher levels of FoxM1b expression than did normal gastric tissue (Fig. 1C). These results indicated that FoxM1b is commonly overexpressed in human gastric cancers, particularly in metastases.
Figure 1. FoxM1 overexpression and its prognostic significance in gastric cancer.
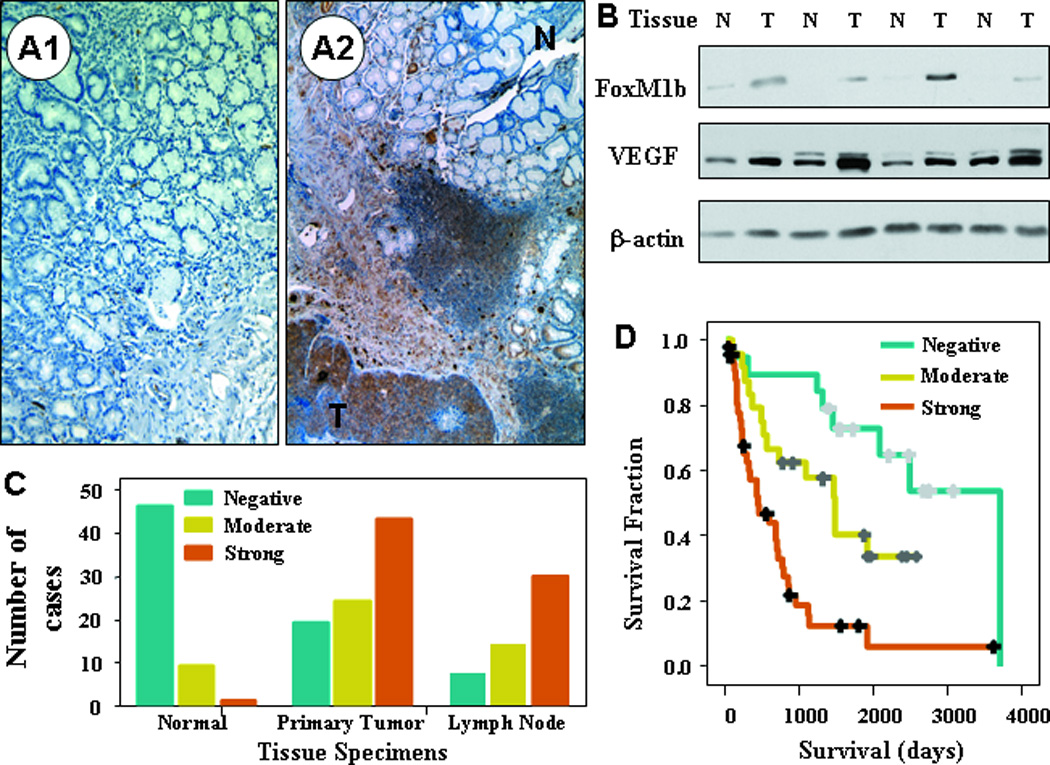
Tissue sections of normal human gastric tissue (57 cases), gastric tumors (86 cases) and lymph node metastases (51 cases) were Immunostained using a specific anti-FoxM1b antibody (A) and FoxM1b expression was confirmed using Western blot analysis with paired normal gastric tissue specimens (n) and gastric tumor specimens (t) (B). The majority of normal gastric mucosal cells (A1) and adjacent normal gastric tissue cells (N) (A2) were negative for FoxM1b expression, whereas gastric tumor cells (T) (A2) were strongly positive for FoxM1b expression. (C) FoxM1b expression levels in primary gastric tumor and lymph node metastasis specimens were significantly higher than those in matched normal tissue specimens (P < 0.001; χ2 test). (D) Kaplan-Meier plots of overall survival in patients who had tumors with negative/weak, moderate, or strong FoxM1b expression. The survival curve for the 43 patients who had tumors with strong FoxM1 expression was significantly worse than that for the 19 patients with negative/weak FoxM1 expression (P < 0.001).
To understand the clinical relevance of FoxM1b overexpression in gastric cancer, we first analyzed the relationship between the level of FoxM1b expression and patient survival. The median survival durations in patients who had tumors with negative, moderate, and strong FoxM1b expression were 89, 48, and 26 months, respectively. Strong FoxM1b expression was associated with an inferior survival duration (P < 0.001) (Fig. 1D). We then entered the patients’ FoxM1b and VEGF expression levels, MVDs, disease stages, completeness of resection, ages at diagnosis, and Lauren’s histologic classifications into a Cox proportional hazards model for multivariate analysis. After adjustment for the effect of covariates, we found that strong FoxM1b expression was an independent predictor of poor survival (P < 0.001) (Supplemental Table 2). Age at diagnosis, completeness of resection, and Lauren’s histological classification did not have a statistically significant effect on survival in the multivariate analysis. We detected no significant differences in the distribution of sex, type of resection, residual disease status, extent of lymphadenectomy, or Lauren’s histological classification between the three FoxM1b expression categories (Supplemental Table 1).
Association of FoxM1b overexpression with increased VEGF expression and MVD in human gastric cancer
Next, we evaluated FoxM1b expression and MVD in the primary gastric tumor specimens obtained from the 86 patients using immunohistochemistry. We observed strong FoxM1b expression in 43 cases (50%), weak expression in 19 cases (22%), and negative expression in 24 cases (28%). Also, we observed a high MVD in 31 cases (36%), a low MVD in 10 cases (12%), and a moderate MVD in 45 cases (52%). FoxM1b expression was significantly correlated with both VEGF expression and MVD (Figs. 2A1 and 2A2). We confirmed these findings by analyzing consecutive primary gastric tumor sections; we found that the FoxM1b expression pattern was consistent with the VEGF expression pattern and MVD status (Figs. 2B and 2C). These data provided clinical evidence supporting our hypothesis that aberrant FoxM1b expression is associated with VEGF expression and increased angiogenesis in gastric cancer.
Figure 2. Direct association of FoxM1b and VEGF expression with MVD status.
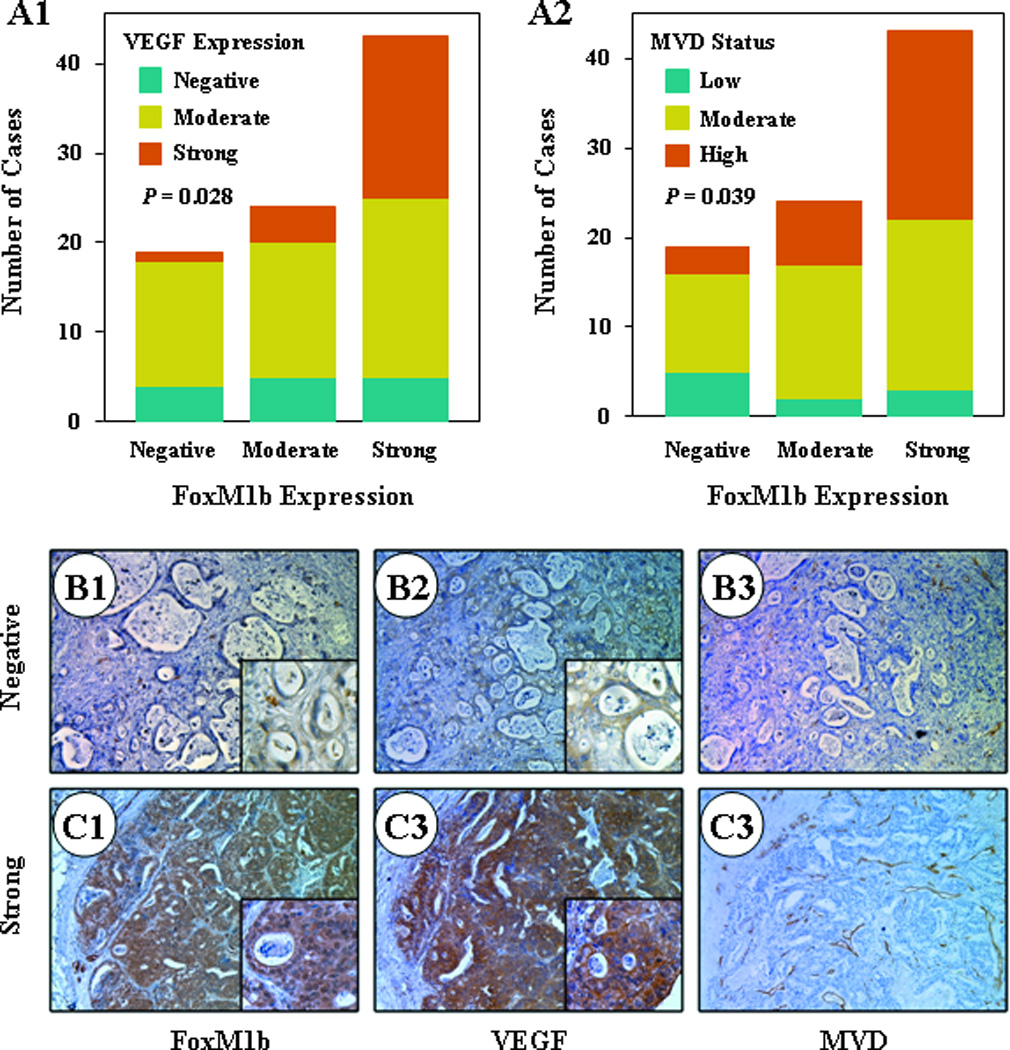
Tissue sections of 86 cases of gastric tumor specimens were immunostained using specific antibodies against FoxM1b, VEGF, and CD34. (A) Direct correlations between VEGF expression and FoxM1b expression (P = 0.028) (A1) and between FoxM1b expression and MVD (P = 0.039) (A2) were analyzed using Pearson’s χ2 test. Three sets of consecutive tissue sections with negative (B) or strong (C) FoxM1b expression were stained for VEGF and CD34. Representative pictures of the sections are shown (original magnification: ×400 for the inserts and ×100 for all others). Of note is that FoxM1b expression directly correlated with VEGF expression and MVD status in the gastric tumor sections.
Regulation of VEGF expression in and angiogenic potential of human gastric cancer cells by FoxM1b
As shown by Western blot analysis, all of the gastric cancer cell lines we tested exhibited high levels of FoxM1b expression (Fig. 3A). To obtain direct evidence of whether FoxM1b regulates the angiogenic phenotype of gastric cancer, we transfected GT5 and N87 cells with the FoxM1b-siRNA expression vector. Using Western blotting, we found that cells transfected with this vector exhibited decreased expression of VEGF but that those transfected with the control vector did not (Figs. 3B1 and 3B2). In contrast, GT5 and N87 cells transfected with pcDNA3.1-FoxM1b exhibited increased expression of VEGF as determined using Western blotting, but GT5 cells transfected with the control expression vector did not (Figs. 3C1 and 3C2). Furthermore, consistent with decreased expression of VEGF, the supernatants of FoxM1b-siRNA--transfected N87 cells seemed to be less angiogenic than the supernatants of control vector-transfected N87 cells as determined using an endothelial cell tube formation assay (Figs. 3D1 and 3E). Furthermore, consistent with increased expression of VEGF, the supernatants of pcDNA3.1-FoxM1b--transfected N87 cells seemed to be more angiogenic than that those of control vector-transfected N87 cells as determined using an endothelial cell tube formation assay (Fig. 3D2). These results suggested that blockade of FoxM1b activity suppresses VEGF expression and impairs the angiogenic phenotype of gastric cancer cells.
Figure 3. Upregulation of VEGF expression by FoxM1b in human gastric cancer cells.
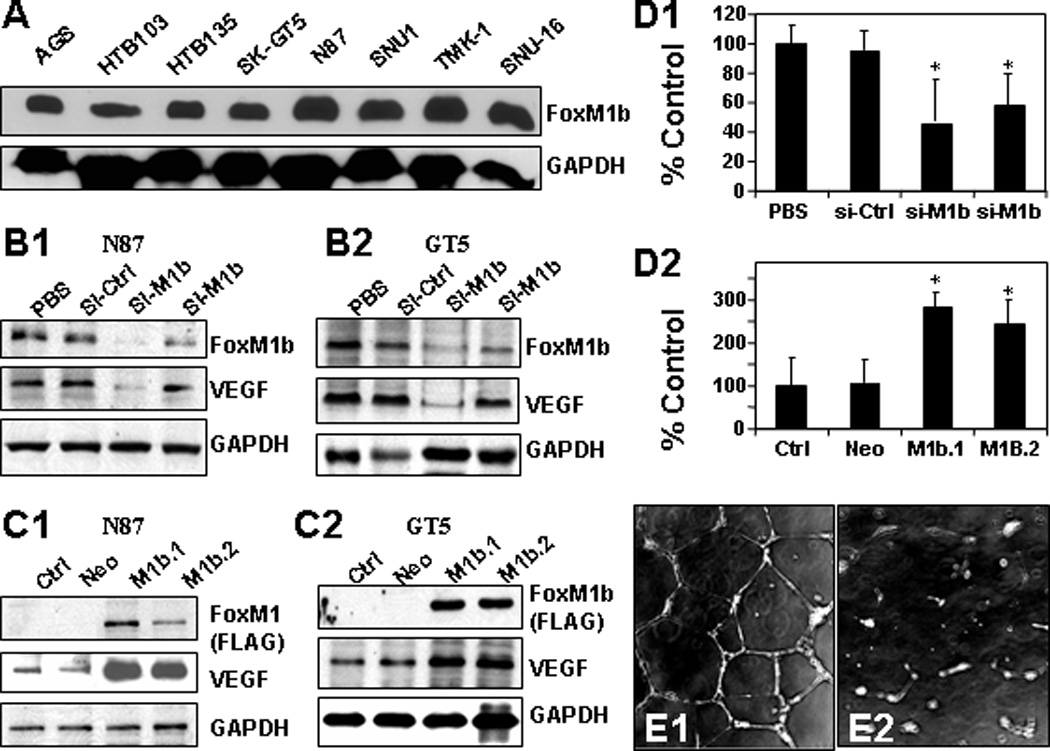
(A) FoxM1 expression in various human gastric cancer cell lines was measured using Western blot analysis. (B) N87 and GT5 cells were transfected with FoxM1b-siRNA (si-M1b) or a control siRNA (si-ctrl). Total protein lysates were harvested from the cell cultures, and the levels of FoxM1b and VEGF expression were determined using Western blot analysis. C) N87 (C1) and GT5 cells (C2) transfected with control pcDNA3 (Neo) or pcDNA3-FoxM1b (M1b) were incubated for 24 h; untreated cells were used as controls (Ctrl). Total protein lysates were harvested from the cell cultures, and the levels of FoxM1b expression (exogenous, as determined using an anti-FLAG antibody) and VEGF expression were determined using Western blot analysis. (D) Promotion of angiogenesis in gastric tumors in vitro by FoxM1b overexpression. Culture supernatants were harvested from untreated N87 cells (Control) and N87 cells transfected with pcDNA3-FoxM1b (M1b), control pcDNA3 (Neo), FoxM1b-siRNA, or a control siRNA. The angiogenic potential of each supernatant was determined using an endothelial cell tube formation assay. The degree of tube formation was calculated as the percentage of the cell surface area versus the total surface area. Control cell cultures were given arbitrary percentage values of 100%. *Statistical significance (P < 0.01) in a comparison of FoxM1b-siRNA--treated and respective control groups (D1) and of pcDNA3-FoxM1b--treated and respective control groups (D2). Representative photos of control (E1) and FoxM1-siRNA--treated (E2) are shown. This was one representative experiment of three with similar results.
Direct impact of altered FoxM1b expression on the tumorigenicity and metastasis of human gastric cancer cells
To determine the effect of FoxM1b expression on tumor-growth kinetics, we injected pcDNA3.1-FoxM1b--transfected N87 cells into the subcutis (Fig. 4A1) or stomach wall (Fig. 4A2) of mice in groups of five. As compared to control vector-transfected tumor cells, pcDNA3.1-FoxM1b--transfected tumor cells produced larger tumors that metastasized to liver (Fig. 4C1 and C2). Therefore, enforced FoxM1b expression promoted gastric tumor growth and metastasis. This finding was consistent with our observation that elevated FoxM1b expression in primary gastric tumors was significantly correlated with an increased incidence of lymph node metastasis (Supplemental Table 3).
Figure 4. Promotion and inhibition of gastric tumor growth and metastasis by FoxM1b overexpression and knockdown.
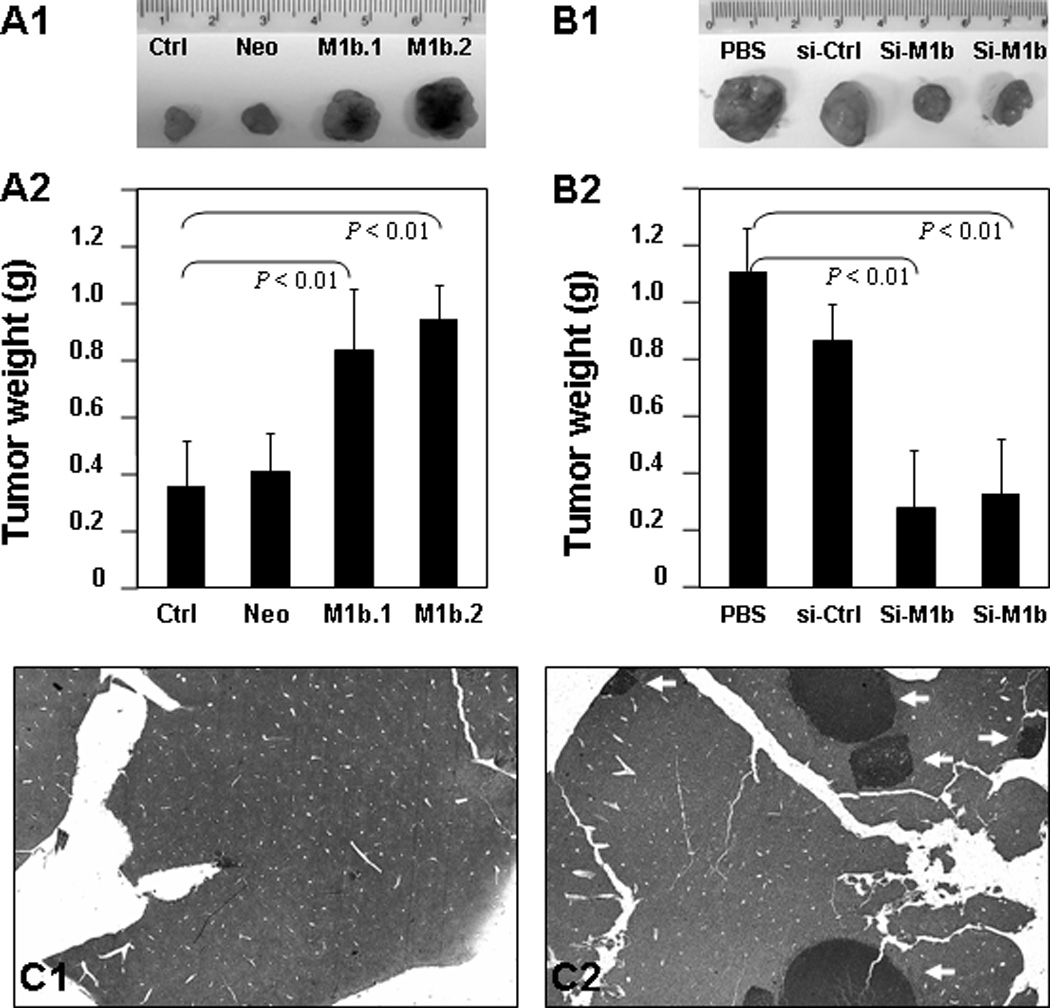
(A) Untreated N87 cells (Ctrl) and N87 cells transfected with pcDNA3-FoxM1b (M1b) or control pcDNA3 (Neo) were injected into the subcutis (A1) or stomach wall (A2) of nude mice (n = 5). (B) Untreated N87 cells (Ctrl) and N87 cells treated with FoxM1b-siRNA (si-M1b) or control siRNA (si-Ctrl) were injected into the subcutis (B1) or stomach wall (B2) of nude mice (n = 5). The resulting subcutaneous gastric tumors were measured, the mean tumor volume (± SD) in each group of mice was calculated, and representative tumor photos were taken (A1 and B1). The tumors were weighed 60 days after the tumor-cell injection or when animals became moribund, and the mean tumor weight (± SD) in each group of mice was calculated (A2 and B2). This was one representative experiment of three with similar results. (C) Representative liver sections with and without gastric cancer metastases (marked by arrowhead) obtained from a mouse with control N87 cells growing in the stomach wall C1) and from a mouse with FoxM1b-overexpressing N87 cells growing in the stomach wall (C2).
Conversely, we established stable FoxM1b-siRNA--transfected N87 cells and then injected them into the subcutis (Fig. 4B1) or stomach wall (Fig. 4B2) of nude mice (1 × 106 per mouse) to evaluate the effect of knockdown of FoxM1b expression on gastric tumor growth. In contrast with the large tumors produced by control cells, FoxM1b-siRNA--transfected N87 cells produced no or small gastric tumors. These results showed that inhibition of FoxM1b expression by FoxM1b-siRNA significantly suppresses the growth and metastasis of human gastric cancer cells.
Regulation of VEGF expression and angiogenesis by FoxM1b in human gastric tumors growing in nude mice
To further identify the mechanisms by which FoxM1b promotes primary gastric tumor growth and metastasis, we examined the effect of FoxM1b expression on tumor angiogenesis in vivo in nude mice. We identified microvessel formation by immunostaining with an anti-CD31 antibody and scoring the number of vessels per high-power field in the sections (Supplemental Fig. 2). Representative VEGF expression levels and MVDs in tumors formed by N87 cells transfected with control pcDNA3, FoxM1b-siRNA, or pcDNA3-FoxM1b were shown in Fig. 5. FoxM1b significantly promoted VEGF expression and induced microvessel formation at higher levels in the primary pcDNA3-FoxM1b tumors than in the control tumors. These results suggested that alteration of tumor growth and metastasis by elevated FoxM1b expression was directly correlated with alteration of VEGF expression and angiogenesis.
Figure 5. FoxM1b and VEGF expression and angiogenesis in human gastric tumor xenografts.
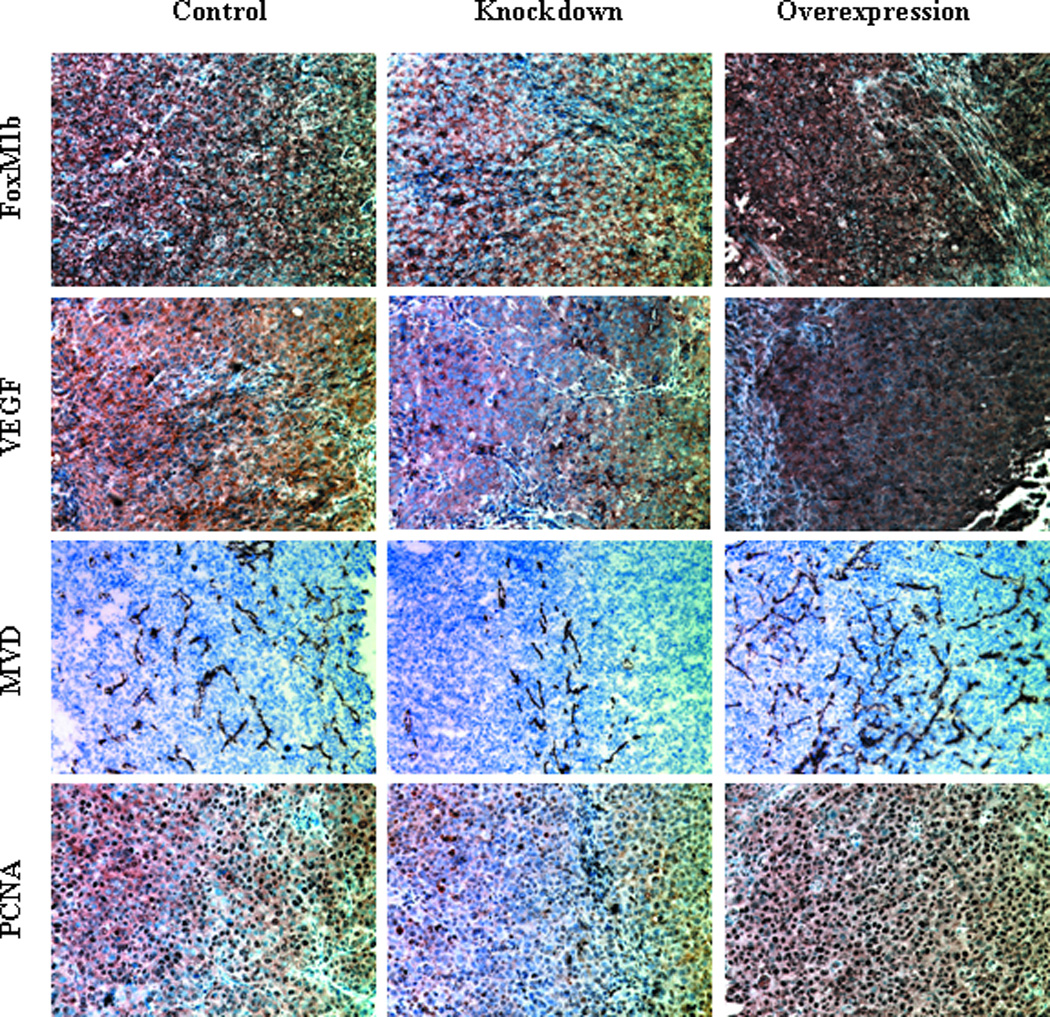
Sections of gastric tumors formed in mice by N87 cells transfected with control pcDNA3.1 (Neo), FoxM1b-siRNA (Knockdown), or pcDNA3.1-FoxM1b (Overexpression) were prepared as described in Fig. 4. The sections were immunostained using antibodies against FoxM1b, VEGF, CD31, and PCNA. The tumor MVD was measured using vessel counting. Representative FoxM1b expression, VEGF expression, tumor MVD, and PCNA expression in the tumors are shown. This was one representative experiment of three with similar results.
Transcriptional activation of VEGF expression in gastric cancer cells by FoxM1b
To determine whether FoxM1b regulates VEGF promoter activity, we co-transfected VEGF promoter-luciferase reporter constructs into GT5 cells with pcDNA3.1-FoxM1b or the control vector pcDNA3.1. Co-transfection with pcDNA3.1-FoxM1b activated the luciferase activity driven by the VEGF promoter. Conversely, we knocked down FoxM1b expression in GT5 cells by co-transfecting them with FoxM1b-siRNA (50 nM) and the VEGF promoter. We observed that FoxM1b-siRNA inhibited the luciferase activity driven by the VEGF promoter in both types of cells (Fig. 6A). Mutations of putative FoxM1b-binding sites (Supplemental Fig. 3) attenuated the induction of VEGF promoters (Fig. 6B). Furthermore, ectopically expressed FoxM1b was phosphorylated in the gastric cancer cells, and the phosphorylation-deficient mutant (T596/A) attenuated its ability to activate VEGF transcriptionally in the gastric cancer cells (Supplemental Fig. 4), supporting that threonine 596 phosphorylation of FoxM1b be critical to its transcriptional activity (43).
Figure 6. Transactivation of VEGF promoters by FoxM1b.
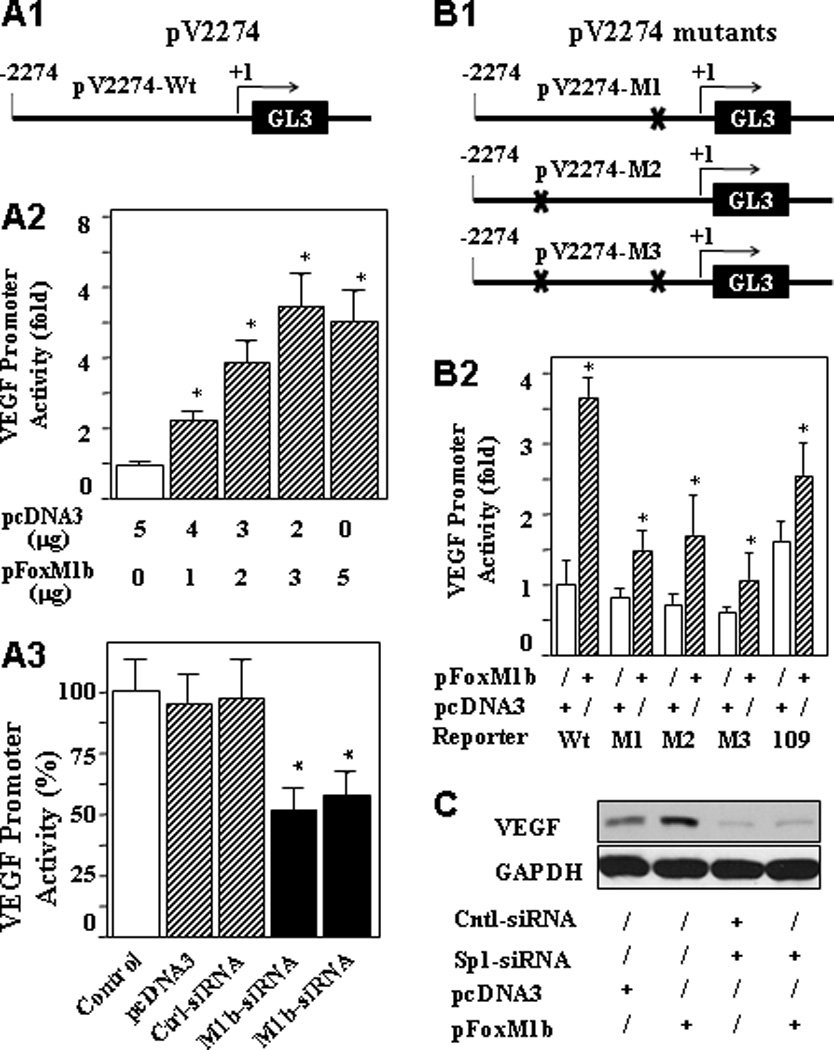
(A) Schematic structure of pV2247 VEGF promoter (A1). The pV2274 reporter was transfected into GT5 cells in triplicate with a FoxM1b expression vector (A2) or FoxM1b-siRNA (A3). pcDNA3.1 and a control siRNA were used as controls. (B) Schematic structure of pV2274 VEGF reporters with mutations in putative FoxM1-binding sites (B1 [“×”]). The VEGF promoter reporters were transfected into GT5 cells in triplicate with or without a FoxM1b expression vector (B2). pcDNA3.1 was used as a control. The relative VEGF promoter activities were measured 24 h after transfection, and the activities in the treated groups were expressed as the fold or percentage of that in their respective control groups. (C) GT5 cells were transfected with a FoxM1b expression vector, Sp1-siRNA, or a combination of the two; pcDNA3 and a control siRNA were used as controls. VEGF expression was determined using Western blot analysis. One representative experiment of two or three with similar results is presented. *Statistical significance (P < 0.01) as compared with that in the respective control groups.
Additionally, knockdown of Sp1 expression attenuated the induction of VEGF by FoxM1b overexpression (Fig. 6C). Chromatin immunoprecipitation and EMSA experiments further showed that FoxM1b was recruited to VEGF promoters (Supplemental Figs. 5 and 6). Moreover, we found that pre-incubation of complexes with an anti-Sp1 antibody prevented the precipitation of FoxM1b-bound DNA by an anti-FoxM1b antibody and subsequent loss of PCR amplification (Supplemental Fig. 7), suggesting that FoxM1b and Sp1 may bind to a similar VEGF promoter region or regions proximal to each other, or interact with each other physically, and FoxM1b may transcriptionally activates VEGF expression in human gastric cancer cells in both an Sp1-dependent and -independent manner.
Discussion
In this study, we discovered four lines of evidence supporting a critical role for FoxM1b in gastric cancer pathogenesis. First, we observed elevated FoxM1b expression and concomitant VEGF overexpression in human gastric cancer cells and that these elevated levels were directly correlated with tumor MVD. Second, overexpression of FoxM1b enhanced the tumorigenicity and metastasis of human gastric cancer cells in animal models, whereas reduced expression of FoxM1b did the opposite. Third, genetically enforced FoxM1b overexpression led to increased VEGF expression in and angiogenic potential of human gastric cancer cells, whereas knockdown of FoxM1b expression did the opposite. Fourth, FoxM1b directly regulated the expression of the VEGF gene at the transcriptional level, which appeared to require intact Sp1 signaling. Therefore, abnormal FoxM1b expression and activation may be molecular markers for poor prognosis for gastric cancer and contribute directly to gastric tumor angiogenesis and aggressive gastric cancer biology.
Studies of prognosis for patients with gastric cancer and of prognostic factors for this disease are important and intriguing and could impact clinical practice. In fact, studies have implicated various factors as prognostic markers of gastric cancer, including MVD and VEGF expression (4, 8). Recently, accumulating evidence has demonstrated that Fox transcriptional factors are involved in VEGF regulation and angiogenesis. For example, Forkhead has exhibited a positive role in mediating induction of VEGF and matrix metalloproteinase-2 (35, 44–47). In the present study, we found direct clinical evidence of a strong correlation among FoxM1b expression and VEGF expression and MVD in human gastric cancer. Although FoxM1b and VEGF expression and MVD were associated with poor survival, FoxM1b expression was apparently a more powerful predictor of clinical outcome of gastric cancer than VEGF expression and MVD were as indicated by a multivariate analysis showing that only FoxM1b expression was an independent prognostic factor. This superiority of FoxM1b as a prognostic factor may support the fact that FoxM1b critically regulates multiple aspects of gastric cancer biology, including the angiogenic phenotype, proliferation, invasiveness, and apoptosis resistance. Consistent with this notion, we demonstrated that FoxM1b seemed to be a powerful predictor of MVD and lymph node metastasis. However, we did not observe a significant relationship between FoxM1b expression and gastric cancer stage. One reason for this lack of a relationship may have been the limited size of our patient cohort. Therefore, more systematic studies of larger patient groups are needed to substantiate whether FoxM1b expression and activation status are powerful, practical predictors of outcome in patients with gastric cancer, particularly in comparison with previously reported prognostic factors such as Stat3 and Sp1 (12, 13).
Previous studies established the critical roles of VEGF expression in tumor angiogenesis (13). The present study is the first to demonstrate that FoxM1b activation is correlated with VEGF expression in human gastric tumor specimens, suggesting a link between FoxM1b activation and VEGF overexpression. By using well-established FoxM1 overexpression and knockdown systems, we were able to show that altered FoxM1b expression significantly impacted VEGF expression in gastric cancer cells. For example, inhibition of FoxM1b expression significantly suppressed VEGF expression in and the angiogenic phenotype of gastric cancer cells. We also found that FoxM1b expression is involved in VEGF promoter activity in gastric cancer cells. Specifically, we identified two potential FoxM1b-binding sites on VEGF promoters. Mutations of these sites profoundly attenuated but did not completely eliminate FoxM1b-mediated transactivation of VEGF promoters. Therefore, these putative binding sites are functional, which we confirmed using a chromatin immunoprecipitation assay, which showed active recruitment of FoxM1b to both binding sites. Conversely, FoxM1b can activate VEGF promoters via other mechanism(s), which was supported by our results showing that pV109 (without any apparent FoxM1b-binding motifs) remained responsive to FoxM1b-mediated transactivation of VEGF promoters. Interestingly, knockdown of Sp1 attenuated FoxM1b-mediated VEGF induction. These results suggested that FoxM1b transactivation of VEGF genes required intact Sp1 signaling, supporting that VEGF expression is regulated by multiple transcription factors, such as hypoxia-inducible factor-1, Sp1, and Stat3, and by cross-talk among them (13). Additionally, FoxM1b may likely target other aspects of VEGF expression. We are currently investigating the mechanisms underlying the potential interactions of FoxM1b with other transcription factors, such as Sp1, on constitutive and inducible VEGF expression to delineate their clinical implications in gastric tumor angiogenesis and progression.
Besides its role in angiogenesis, the implication of a role for FoxM1b in gastric cancer development and progression is supported by lines of evidence suggesting that FoxM1b is essential for cell-cycle progression (16, 21–28, 48, 49). In fact, FoxM1b regulates the expression of various proteins that stimulate cell proliferation in various cancer types (30, 33, 36–38, 49), suggesting that FoxM1b is required for proliferative expansion during tumor progression. Although the present study is the first to provide evidence of a critical role for activated FoxM1b in gastric cancer angiogenesis, it also shows a direct correlation between FoxM1 expression and proliferating cell nuclear antigen (PCNA) expression, supporting a critical role for FoxM1 in cell proliferation. However, whether increased gastric cancer cell proliferation resulted from overexpression directly, increased angiogenesis indirectly, or both is unclear. Nonetheless, both tumor-cell proliferation and angiogenesis are essential for gastric cancer development and progression. Given the demonstrated critical roles of FoxM1b in these two critical aspects of cancer biology, promotion of gastric cancer growth and metastasis by activation of FoxM1b is conceivable, further supporting our finding that FoxM1b is a powerful prognostic factor for gastric cancer.
Finally, the underlying mechanism responsible for FoxM1b overactivation is currently unknown. FoxM1 expression can be induced by diverse stimuli, such as liver regeneration, keratinocyte growth factor expression, and oxidative stress (16, 30). More recently, researchers identified FoxM1b as a novel inhibitory target of p19ARF protein and showed that a modified membrane-transducing peptide derived from the ARF protein (p19ARF) is sufficient to interact with and inhibit FoxM1b, preventing FoxM1b stimulation of anchorage-independent growth of cells on soft agar (49, 50). Further exploration of the molecular mechanisms that result in FoxM1b overactivation may not only shed more light on abnormal FoxM1b activation but also help improve understanding of FoxM1b’s value as a prognostic factor and aid in the development of effective therapies that target FoxM1b (14, 15).
In summary, our study is the first to indicate that FoxM1b directly regulates VEGF gene transcription, which is at least partially responsible for FoxM1b-mediated promotion of human gastric cancer angiogenesis, growth, and metastasis. Therefore, this study identified a novel molecular mechanism for the protumor activity of FoxM1b and provides a better understanding of the molecular basis for aberrant FoxM1b signaling pathways, which may aid the design of effective therapeutic modalities to control gastric cancer growth and metastasis.
Supplementary Material
Acknowledgments
Grant support: Research Scholar Grant CSM-106640 from the America Cancer Society and grant 1R01-CA093829 from the National Cancer Institute, National Institutes of Health (to K.X.) and MD Anderson Cancer Center Development Fund (to D.T.). We thank Don Norwood for editorial comments.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA: a cancer journal for clinicians. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA: a cancer journal for clinicians. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 3.Johnson SM, Evers BM. Translational research in gastric malignancy. Surgical oncology clinics of North America. 2008;17:323–340. doi: 10.1016/j.soc.2008.01.001. viii. [DOI] [PubMed] [Google Scholar]
- 4.Zheng L, Wang L, Ajani J, Xie K. Molecular basis of gastric cancer development and progression. Gastric Cancer. 2004;7:61–77. doi: 10.1007/s10120-004-0277-4. [DOI] [PubMed] [Google Scholar]
- 5.Whisenant J, Bergsland E. Anti-angiogenic strategies in gastrointestinal malignancies. Current treatment options in oncology. 2005;6:411–421. doi: 10.1007/s11864-005-0044-8. [DOI] [PubMed] [Google Scholar]
- 6.Hohenberger P, Gretschel S. Gastric cancer. Lancet. 2003;362:305–315. doi: 10.1016/s0140-6736(03)13975-x. [DOI] [PubMed] [Google Scholar]
- 7.Chan AO, Luk JM, Hui WM, Lam SK. Molecular biology of gastric carcinoma: from laboratory to bedside. J Gastroenterol Hepatol. 1999;14:1150–1160. doi: 10.1046/j.1440-1746.1999.02000.x. [DOI] [PubMed] [Google Scholar]
- 8.Yao JC, Wang L, Wei D, et al. Association between expression of transcription factor Sp1 and increased vascular endothelial growth factor expression, advanced stage, and poor survival in patients with resected gastric cancer. Clin Cancer Res. 2004;10:4109–4117. doi: 10.1158/1078-0432.CCR-03-0628. [DOI] [PubMed] [Google Scholar]
- 9.Jiang Y, Wang L, Gong W, et al. A high expression level of insulin-like growth factor I receptor is associated with increased expression of transcription factor Sp1 and regional lymph node metastasis of human gastric cancer. Clinical & experimental metastasis. 2004;21:755–764. doi: 10.1007/s10585-005-1198-2. [DOI] [PubMed] [Google Scholar]
- 10.Chen CN, Cheng YM, Lin MT, Hsieh FJ, Lee PH, Chang KJ. Association of color Doppler vascularity index and microvessel density with survival in patients with gastric cancer. Annals of surgery. 2002;235:512–518. doi: 10.1097/00000658-200204000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanz-Ortega J, Steinberg SM, Moro E, et al. Comparative study of tumor angiogenesis and immunohistochemistry for p53, c-ErbB2, c-myc and EGFr as prognostic factors in gastric cancer. Histology and histopathology. 2000;15:455–462. doi: 10.14670/HH-15.455. [DOI] [PubMed] [Google Scholar]
- 12.Wang L, Wei D, Huang S, et al. Transcription factor Sp1 expression is a significant predictor of survival in human gastric cancer. Clin Cancer Res. 2003;9:6371–6380. [PubMed] [Google Scholar]
- 13.Gong W, Wang L, Yao JC, et al. Expression of activated signal transducer and activator of transcription 3 predicts expression of vascular endothelial growth factor in and angiogenic phenotype of human gastric cancer. Clin Cancer Res. 2005;11:1386–1393. doi: 10.1158/1078-0432.CCR-04-0487. [DOI] [PubMed] [Google Scholar]
- 14.Gartel AL. FoxM1 inhibitors as potential anticancer drugs. Expert opinion on therapeutic targets. 2008;12:663–665. doi: 10.1517/14728222.12.6.663. [DOI] [PubMed] [Google Scholar]
- 15.Myatt SS, Lam EW. Targeting FOXM1. Nature reviews. 2008;8:242. doi: 10.1038/nrc2223-c2. [DOI] [PubMed] [Google Scholar]
- 16.Ye H, Kelly TF, Samadani U, et al. Hepatocyte nuclear factor 3/fork head homolog 11 is expressed in proliferating epithelial and mesenchymal cells of embryonic and adult tissues. Molecular and cellular biology. 1997;17:1626–1641. doi: 10.1128/mcb.17.3.1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korver W, Roose J, Heinen K, et al. The human TRIDENT/HFH-11/FKHL16 gene: structure, localization, and promoter characterization. Genomics. 1997;46:435–442. doi: 10.1006/geno.1997.5065. [DOI] [PubMed] [Google Scholar]
- 18.Yao KM, Sha M, Lu Z, Wong GG. Molecular analysis of a novel winged helix protein, WIN. Expression pattern, DNA binding property, and alternative splicing within the DNA binding domain. J Biol Chem. 1997;272:19827–19836. doi: 10.1074/jbc.272.32.19827. [DOI] [PubMed] [Google Scholar]
- 19.Korver W, Roose J, Clevers H. The winged-helix transcription factor Trident is expressed in cycling cells. Nucleic Acids Res. 1997;25:1715–1719. doi: 10.1093/nar/25.9.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Westendorf JM, Rao PN, Gerace L. Cloning of cDNAs for M-phase phosphoproteins recognized by the MPM2 monoclonal antibody and determination of the phosphorylated epitope. Proc Natl Acad Sci U S A. 1994;91:714–718. doi: 10.1073/pnas.91.2.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ye H, Holterman AX, Yoo KW, Franks RR, Costa RH. Premature expression of the winged helix transcription factor HFH-11B in regenerating mouse liver accelerates hepatocyte entry into S phase. Molecular and cellular biology. 1999;19:8570–8580. doi: 10.1128/mcb.19.12.8570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luscher-Firzlaff JM, Westendorf JM, Zwicker J, et al. Interaction of the fork head domain transcription factor MPP2 with the human papilloma virus 16 E7 protein: enhancement of transformation and transactivation. Oncogene. 1999;18:5620–5630. doi: 10.1038/sj.onc.1202967. [DOI] [PubMed] [Google Scholar]
- 23.Wang X, Kiyokawa H, Dennewitz MB, Costa RH. The Forkhead Box m1b transcription factor is essential for hepatocyte DNA replication and mitosis during mouse liver regeneration. Proc Natl Acad Sci U S A. 2002;99:16881–16886. doi: 10.1073/pnas.252570299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laoukili J, Kooistra MR, Bras A, et al. FoxM1 is required for execution of the mitotic programme and chromosome stability. Nat Cell Biol. 2005;7:126–136. doi: 10.1038/ncb1217. [DOI] [PubMed] [Google Scholar]
- 25.Wonsey DR, Follettie MT. Loss of the forkhead transcription factor FoxM1 causes centrosome amplification and mitotic catastrophe. Cancer research. 2005;65:5181–5189. doi: 10.1158/0008-5472.CAN-04-4059. [DOI] [PubMed] [Google Scholar]
- 26.Leung TW, Lin SS, Tsang AC, et al. Over-expression of FoxM1 stimulates cyclin B1 expression. FEBS Lett. 2001;507:59–66. doi: 10.1016/s0014-5793(01)02915-5. [DOI] [PubMed] [Google Scholar]
- 27.Park HJ, Wang Z, Costa RH, Tyner A, Lau LF, Raychaudhuri P. An N-terminal inhibitory domain modulates activity of FoxM1 during cell cycle. Oncogene. 2008;27:1696–1704. doi: 10.1038/sj.onc.1210814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park HJ, Costa RH, Lau LF, Tyner AL, Raychaudhuri P. APC/C-Cdh1 Mediated Proteolysis of the Forkhead Box M1 Transcription Factor is Critical for Regulated Entry into S phase. Molecular and cellular biology. 2008 doi: 10.1128/MCB.00387-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang X, Krupczak-Hollis K, Tan Y, Dennewitz MB, Adami GR, Costa RH. Increased hepatic Forkhead Box M1B (FoxM1B) levels in old-aged mice stimulated liver regeneration through diminished p27Kip1 protein levels and increased Cdc25B expression. J Biol Chem. 2002;277:44310–44316. doi: 10.1074/jbc.M207510200. [DOI] [PubMed] [Google Scholar]
- 30.Teh MT, Wong ST, Neill GW, Ghali LR, Philpott MP, Quinn AG. FOXM1 is a downstream target of Gli1 in basal cell carcinomas. Cancer research. 2002;62:4773–4780. [PubMed] [Google Scholar]
- 31.Kalinichenko VV, Gusarova GA, Kim IM, et al. Foxf1 haploinsufficiency reduces Notch-2 signaling during mouse lung development. Am J Physiol Lung Cell Mol Physiol. 2004;286:L521–L530. doi: 10.1152/ajplung.00212.2003. [DOI] [PubMed] [Google Scholar]
- 32.Lee JS, Chu IS, Heo J, et al. Classification and prediction of survival in hepatocellular carcinoma by gene expression profiling. Hepatology. 2004;40:667–676. doi: 10.1002/hep.20375. [DOI] [PubMed] [Google Scholar]
- 33.Kim IM, Ackerson T, Ramakrishna S, et al. The Forkhead Box m1 transcription factor stimulates the proliferation of tumor cells during development of lung cancer. Cancer research. 2006;66:2153–2161. doi: 10.1158/0008-5472.CAN-05-3003. [DOI] [PubMed] [Google Scholar]
- 34.Obama K, Ura K, Li M, et al. Genome-wide analysis of gene expression in human intrahepatic cholangiocarcinoma. Hepatology. 2005;41:1339–1348. doi: 10.1002/hep.20718. [DOI] [PubMed] [Google Scholar]
- 35.Dai B, Kang SH, Gong W, et al. Aberrant FoxM1B expression increases matrix metalloproteinase-2 transcription and enhances the invasion of glioma cells. Oncogene. 2007 doi: 10.1038/sj.onc.1210443. [DOI] [PubMed] [Google Scholar]
- 36.Liu M, Dai B, Kang SH, et al. FoxM1B is overexpressed in human glioblastomas and critically regulates the tumorigenicity of glioma cells. Cancer research. 2006;66:3593–3602. doi: 10.1158/0008-5472.CAN-05-2912. [DOI] [PubMed] [Google Scholar]
- 37.Yoshida Y, Wang IC, Yoder HM, Davidson NO, Costa RH. The forkhead box M1 transcription factor contributes to the development and growth of mouse colorectal cancer. Gastroenterology. 2007;132:1420–1431. doi: 10.1053/j.gastro.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 38.Kalin TV, Wang IC, Ackerson TJ, et al. Increased levels of the FoxM1 transcription factor accelerate development and progression of prostate carcinomas in both TRAMP and LADY transgenic mice. Cancer research. 2006;66:1712–1720. doi: 10.1158/0008-5472.CAN-05-3138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bektas N, Haaf A, Veeck J, et al. Tight correlation between expression of the Forkhead transcription factor FOXM1 and HER2 in human breast cancer. BMC cancer. 2008;8:42. doi: 10.1186/1471-2407-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chan D, Yu S, Chiu P, et al. Over-expression of FOXM1 transcription factor is associated with cervical cancer progression and pathogenesis. The Journal of pathology. 2008;215:245–252. doi: 10.1002/path.2355. [DOI] [PubMed] [Google Scholar]
- 41.Pilarsky C, Wenzig M, Specht T, Saeger HD, Grutzmann R. Identification and validation of commonly overexpressed genes in solid tumors by comparison of microarray data. Neoplasia. 2004;6:744–750. doi: 10.1593/neo.04277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kanai M, Wei D, Li Q, et al. Loss of Kruppel-like factor 4 expression contributes to Sp1 overexpression and human gastric cancer development and progression. Clin Cancer Res. 2006;12:6395–6402. doi: 10.1158/1078-0432.CCR-06-1034. [DOI] [PubMed] [Google Scholar]
- 43.Major ML, Lepe R, Costa RH. Foxhead Box M1B transcriptional activity requires binding of Cdk-Cyclin complexes for phosphorylation-dependent recruitment of p300/CBP coactivators. Mol Cell Biol. 2004;24:2649–2661. doi: 10.1128/MCB.24.7.2649-2661.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abid MR, Shih SC, Otu HH, et al. A novel class of vascular endothelial growth factor-responsive genes that require forkhead activity for expression. J Biol Chem. 2006;281:35544–35553. doi: 10.1074/jbc.M608620200. [DOI] [PubMed] [Google Scholar]
- 45.Furuyama T, Kitayama K, Shimoda Y, et al. Abnormal angiogenesis in Foxo1 (Fkhr)-deficient mice. J Biol Chem. 2004;279:34741–34749. doi: 10.1074/jbc.M314214200. [DOI] [PubMed] [Google Scholar]
- 46.Gupta S, Joshi K, Wig JD, Arora SK. Intratumoral FOXP3 expression in infiltrating breast carcinoma: Its association with clinicopathologic parameters and angiogenesis. Acta Oncol. 2007;46:792–797. doi: 10.1080/02841860701233443. [DOI] [PubMed] [Google Scholar]
- 47.Banham AH, Boddy J, Launchbury R, et al. Expression of the forkhead transcription factor FOXP1 is associated both with hypoxia inducible factors (HIFs) and the androgen receptor in prostate cancer but is not directly regulated by androgens or hypoxia. Prostate. 2007;67:1091–1098. doi: 10.1002/pros.20583. [DOI] [PubMed] [Google Scholar]
- 48.Trembley JH, Ebbert JO, Kren BT, Steer CJ. Differential regulation of cyclin B1 RNA and protein expression during hepatocyte growth in vivo. Cell Growth Differ. 1996;7:903–916. [PubMed] [Google Scholar]
- 49.Kalinichenko VV, Major ML, Wang X, et al. Foxm1b transcription factor is essential for development of hepatocellular carcinomas and is negatively regulated by the p19ARF tumor suppressor. Genes Dev. 2004;18:830–850. doi: 10.1101/gad.1200704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gusarova GA, Wang IC, Major ML, et al. A cell-penetrating ARF peptide inhibitor of FoxM1 in mouse hepatocellular carcinoma treatment. J Clin Invest. 2007;117:99–111. doi: 10.1172/JCI27527. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


