Abstract
In the HIV-infected population there is a high prevalence of psychiatric disorders, conditions that often coexist with drug and alcohol dependence. Symptoms associated with psychiatric disorders are frequently managed with benzodiazepines, a class of medication often abused. We examined whether HIV-infected patients were more likely to fill a benzodiazepine prescription than their uninfected counterparts using a privately insured, nationally representative sample receiving clinical care between January 2007 and December 2009. Odds ratios (OR) and 95% confidence intervals (CI) to quantify the likelihood of receiving a benzodiazepine were calculated using multivariate logistic regression models. We examined the presence of interaction between HIV infection and sex using backward elimination and by comparing stratum specific odds ratios to identify clinically meaningful differences. Overall, 323,796 beneficiaries were included in the sample, of which 723 were HIV-infected. Bivariate analyses showed that compared to the uninfected sample, HIV-infected patients were more likely to have filled a benzodiazepine prescription (24% vs. 19%) during the study period. HIV-infected patients were also more likely to be male (80% vs. 44%), black (21% vs. 7%), and have a diagnosis of depression (12% vs. 8%) or insomnia (6% vs. 3%) than were uninfected patients. Adjusted for other covariates, HIV infection was associated with an increase (OR): 1.68, 95% CI: 1.39, 2.02) in the likelihood of filling a benzodiazepine prescription. When stratified by sex, HIV-infected males were more likely (OR: 1.68, 95% CI: 1.05, 2.67) than uninfected males to fill a benzodiazepine prescription while there was no observed difference in the likelihood of filling a benzodiazepine prescription between HIV-infected and uninfected females (OR: 1.12, 95% CI: 0.73, 1.70). Our findings suggest that HIV-infected patients, particularly HIV-infected males, are more likely to fill benzodiazepine prescriptions than their uninfected counterparts, highlighting the need for further research to investigate reasons for these observed differences.
Keywords: HIV, benzodiazepine, sex differences, psychiatric disorders, drug utilization
INTRODUCTION
The burden of psychiatric disorders in the HIV-infected population exceeds that of the general US population (Bing et al., 2001; Pence, Miller, Whetten, Eron, & Gaynes, 2006) and the 12-month prevalence of psychiatric disorders is estimated at 48% (Bing et al., 2001). This estimate is nearly two times greater than the 26% prevalence rate estimated in the general population (Kessler et al., 2005). The most commonly detected psychiatric disorders in the HIV-infected population include major depression, dysthymia, and generalized anxiety disorder (Bing et al., 2001). Additionally, patients who suffer from psychiatric disorders are likely afflicted with symptoms of insomnia (Karaz, 2010). The estimated prevalence rate for anxiety disorders may be as high as 38% (Elliott, 1998), 32% for depression (Bing et al., 2001) and 78% for insomnia (Rubinstein & Selwyn, 1998), in the HIV-infected population. Each of these estimates exceeds those of the general population: 18% for anxiety (Kessler et al., 2005), 7% for depression (Kessler et al., 2003), and 30% for insomnia (Roth, 2007). Managing symptoms of these comorbidities is especially important in HIV-infected patients as they are associated with suboptimal adherence to antiretrovirals (Ammassari et al., 2001; Pence, Miller, Whetten, Eron, & Gaynes, 2006). High levels of adherence are necessary to achieve optimal viral load suppression and mitigate the development of drug-resistant HIV infection (Bangsberg et al., 2000; Paterson et al., 2000).
Benzodiazepines are the most frequently used psychotropic drug class (Paulose-Ram et al., 2004), and are widely prescribed for the management of symptoms related to anxiety, insomnia, and depression (Shader, Greenblatt, & Balter, 1991; Valenstein et al., 2004). Concerns exist regarding benzodiazepine use in the HIV-infected population due to potential interactions with antiretroviral therapy (Ferrando & Wapenyi, 2002; Greenblatt et al., 2000). Moreover, due to their abuse/misuse potential, benzodiazepines are not recommended for patients with a substance abuse history, a common problem among the HIV-infected population (Bing et al., 2001). To date, few studies have compared the prevalence of benzodiazepine use in the HIV-infected and uninfected populations. Furthermore, no studies have examined benzodiazepine usage by sex despite evidence suggesting prevalence rates of psychiatric disorders differ between males and females in the general and HIV-infected populations (Kessler et al., 2003; Lopes et al., 2012; Vesga-Lopez et al., 2008). The current study uses insurance claims data to examine whether HIV-infected patients are more likely to fill a benzodiazepine prescription than uninfected patients and, investigate sex differences in the likelihood of filling a benzodiazepine prescription among HIV-infected and uninfected patients.
METHODS
We established a four state nationally representative, population-based cohort using data from a large private insurance claims database from January 2007 to December 2009. This claims database includes patient socio-demographics and codes related to interactions with the healthcare system. Beneficiaries were included if they resided in Kentucky, Maryland, North Carolina, or Washington, were between 19 and 64 years of age, and had at least one healthcare claim in 2007 followed by a subsequent claim in either 2008 or 2009. Beneficiaries were identified as HIV-positive if they had at least one healthcare claim in 2007 with the ICD-9 code ‘042’ (Human Immunodeficiency Virus (HIV) disease). The outcome of interest was filling a benzodiazepine prescription. Benzodiazepine fills during the study period were represented by a claim for any benzodiazepine identified using national drug codes. We considered the following covariates assessed in the year 2007: sex, age, race, education, state of residence, continuous insurance enrollment, substance abuse treatment (e.g. residential or non-residential treatment facility), and psychiatric disorders. Bivariate analysis examined the association between HIV-infection and benzodiazepine use. Multivariate logistic regression models adjusted for covariates identified above were used to estimate the adjusted odds ratio (AOR) of filling a benzodiazepine prescription for HIV-infected patients. We examined the presence of interaction between HIV-infection and the covariates using backwards elimination. Statistical significance was considered using the Wald χ2 p-value associated with the interaction term as well as clinically meaningful differences by comparing stratum specific odds ratios. Data use was approved by the XXXXX Institutional Review Board. Statistical analysis was conducted using Stata 12.0 (StataCorp., College Station, TX).
RESULTS
A total of 323,902 beneficiaries met the inclusion criteria for this study. Of these beneficiaries 106 were excluded due to duplicate or conflicting information. Overall, our study cohort consisted of 323,796 beneficiaries, 723 were identified as HIV-infected. Baseline characteristics and benzodiazepine utilization for HIV-infected and uninfected patients are shown in Table 1. Compared to the uninfected population the HIV-infected population had a greater proportion of men (80% versus 44%) and blacks (21% versus 7%). The HIV-infected population also had a greater proportion of patients with a diagnosis of depression (12% versus 8%) or insomnia (6% versus 3%). We observed a greater proportion of HIV-infected patients filled a benzodiazepine prescription during the study period (24% versus 19%) with alprazolam, diazepam, and lorazepam being the most commonly filled benzodiazepines.
Table 1.
Comparison of demographics of HIV-infected and HIV-uninfected patients.
| Variables |
HIV N=723 |
HIV-uninfected N = 323,073 |
p-value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Benzodiazepine Usage | |||||
| Filled Benzodiazepine Prescription | 174 | 24% | 60,420 | 19% | < 0.001 |
| State of Residence | |||||
| Kentucky | 67 | 9% | 36,698 | 11% | 0.077 |
| Maryland | 193 | 27% | 59,635 | 18% | < 0.001 |
| North Carolina | 339 | 47% | 177,680 | 55% | < 0.001 |
| Washington | 124 | 17% | 49,060 | 15% | 0.141 |
| Sex | |||||
| Male | 578 | 80% | 140,605 | 44% | < 0.001 |
| Age | |||||
| Mean Age (for year 2007), SDa | 43.02 | 8.83 | 41.98 | 11.46 | 0.015 |
| Race | |||||
| White | 483 | 67% | 255,735 | 79% | < 0.001 |
| Black | 155 | 21% | 23,085 | 7% | < 0.001 |
| Hispanic | 32 | 4% | 11,501 | 4% | 0.209 |
| Other | 49 | 7% | 29,917 | 9% | 0.021 |
| Education | |||||
| Less than High School | 6 | 1% | 2,023 | 1% | 0.488 |
| High School Graduate | 237 | 33% | 112,330 | 35% | 0.262 |
| Some College | 345 | 48% | 139,963 | 43% | 0.017 |
| College Graduate | 118 | 16% | 60,340 | 19% | 0.104 |
| Psychiatric Diagnosis | |||||
| Anxiety | 47 | 7% | 21,386 | 7% | 0.989 |
| Depression | 84 | 12% | 26,026 | 8% | < 0.001 |
| Insomnia | 44 | 6% | 9,973 | 3% | < 0.001 |
| Substance Abuse Treatment | |||||
| Receiving Substance Abuse Treatment | 5 | 1% | 1,941 | 1% | 0.752 |
| Enrollment Eligibility | |||||
| Continuously Eligible | 284 | 39% | 145,518 | 45% | 0.002 |
| Gaps in Coverage | 439 | 61% | 177,555 | 55% | 0.002 |
SD: Standard Deviation
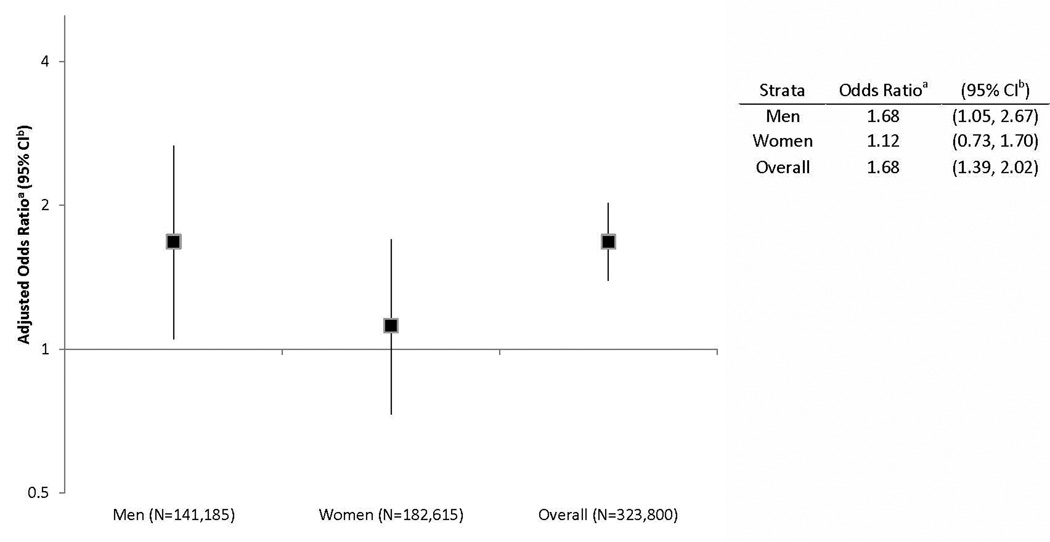
Figure 1 shows the AOR of filling a benzodiazepine prescription for HIV-infected patients stratified by sex relative to the overall estimate of HIV-infected patients. The overall AOR demonstrates that without stratifying by sex, HIV-infected patients have 1.68 times greater odds of filling a benzodiazepine prescription than uninfected patients (95% CI: 1.39, 2.02). When stratified by sex, results from the multivariate regression showed HIV-infected males are 1.68 times more likely to fill a benzodiazepine prescription than uninfected males, adjusting for covariates (95% CI: 1.05, 2.67), while no statistical difference was observed between HIV-infected and uninfected females (AOR: 1.12, 95% CI: 0.73, 1.70). Interaction between HIV-infection and age, race, education, substance abuse treatment, and psychiatric disorders was considered but statistical significance was not achieved at the 0.05 level nor were there any clinically meaningful differences between the strata.
Figure 1.
Likelihood of filling a benzodiazepine prescription among HIV-infected individuals compared to HIV-uninfected individuals stratified by sex. aAdjusted for state of residence, age, race, education, and enrollment eligibility (e.g., continuous insurance coverage, gaps in insurance coverage). bCI: Confidence Interval.
In the overall population the likelihood of filing a benzodiazepine prescription is influenced by the patient’s age, sex, and race, along with treatment for substance abuse and psychiatric disorder diagnosis. With each additional ten years patients age, their odds of filling a benzodiazepine prescription increase 21% (AOR: 1.21, 95% CI: 1.20, 1.22). Additionally, males are less likely than females (AOR: 0.62, 95% CI: 0.61, 0.63) and nonwhite patients are less likely than white patients to fill a benzodiazepine prescription (AOR: 0.72, 95% CI: 0.70, 0.74). Furthermore, treatment for substance abuse (AOR: 1.27, 95% CI: 1.14, 1.42), or having a diagnosis of anxiety (AOR: 5.99, 95% CI: 5.81, 6.18), depression (AOR: 2.48, 95% CI: 2.42, 2.56), or insomnia (AOR: 2.78, 95% CI: 2.65, 2.90) increase the odds of filling a benzodiazepine prescription.
DISCUSSIONS
This study demonstrates that HIV-infected patients are more likely to fill a benzodiazepine prescription than uninfected patients. Furthermore, we show HIV-infected males are more likely than uninfected males to fill a benzodiazepine prescription, with no observed difference between HIV-infected and uninfected females. This difference is notable as concerns exist regarding benzodiazepine use in the HIV-infected population due to their high abuse/misuse potential and the link between substance abuse and poor medication adherence (Arnsten et al., 2002; Singh et al., 1996).
The overall difference in the odds of filling a benzodiazepine prescription between HIV-infected and uninfected patients may be related to the high prevalence of psychiatric disorders in this population (Bing et al., 2001). However, we adjusted for these conditions in our models suggesting additional factors shown to be associated with benzodiazepine use in this population and not captured within claims data, such as exposure to stressful events related to HIV serostatus and disclosure (Roux et al., 2011), may explain the differences in benzodiazepine use between the HIV-infected and uninfected populations. The high prevalence of substance abuse and dependence in the HIV-infected population (Bing et al., 2001) should also be considered as an explanation of the observed differences in benzodiazepine use. Few studies have compared benzodiazepine use in the HIV-infected and uninfected populations and to our knowledge, this study is the first to examine differences in receipt of benzodiazepines by sex.Roux et al. (2011), investigated factors associated with regular benzodiazepine use in HIV-infected patients but as this study included HIV-infected patients only, comparisons to the uninfected population were not made (Roux et al., 2011).
Reasons for observed differences between males and females in our study may be related to underlying differences in the prevalence of psychiatric disorders, differences in stigmatization, as well as differences in overall health care utilization between HIV-infected men and women.Lopes et al. (2012), showed HIV-infected men were more likely than uninfected men to have a specific DSM-IV diagnosis with no observed differences among women. Our results support these findings as we found HIV-infected men more likely than uninfected men to fill a benzodiazepine prescription, with no observable differences between women. Additionally,Roux et al. (2011), found that individuals belonging to the injecting drug use (IDU) and men who have sex with men (MSM) HIV-transmission groups were more likely than their heterosexual HIV-transmission group counterparts to report regular benzodiazepine use. This finding is likely associated with IDUs and MSM group members perceiving and facing greater discrimination and stigmatization (Herek, Capitanio, & Widaman, 2003). Evidence exists of differences in healthcare utilization between HIV-infected men and women. Hellinger and Encinosa (2004) found HIV-infected men were more likely than HIV-infected women to receive antiretroviral therapy and costlier medications.
Limitations to this study exist. First, this study uses data from a private insurance claims database for four states, and may not accurately represent the overall HIV-infected or uninfected populations. Also, this study does not account for the number of benzodiazepine prescriptions filled or the quantity and dosages of those prescriptions. Additionally, we cannot account for prescriptions acquired through family and friends or paid for using cash. Finally, while our results show HIV-infected patients are more likely to fill a benzodiazepine prescription, we did not differentiate between appropriate and inappropriate use.
Despite these limitations, our findings demonstrate HIV-infected patients, especially HIV-infected males, are more likely to use benzodiazepines. Our findings, in combination with evidence demonstrating sex differences in psychiatric disorders, show the need for further research evaluating reasons for observed differences. Furthermore, intervention studies targeting this at-risk population to reduce the risk of substance abuse and improve HIV clinical care are warranted.
ACKNOWLEDGEMENTS
The authors have no conflicts of interest to declare. The project described was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under the award number UL1TR000117 and the Office of Women’s Health Research and the National Institute on Drug Abuse of the National Institutes of Health under the award number K12DA035150. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
We would like to thank Dr. Karen Blumenschein for her helpful comments and article review.
Footnotes
Results presented at 29th International Conference of Pharmacoepidemiology & Therapeutic Risk Management. Montréal, Canada, August 25–28, 2013.
REFERENCES
- Ammassari A, Murri R, Pezzotti P, Trotta MP, Ravasio L, De Longis P, Antinori A. Self-reported symptoms and medication side effects influence adherence to highly active antiretroviral therapy in persons with HIV infection. Journal of Acquired Immune Deficiency Syndromes. 2001;28:445–449. doi: 10.1097/00042560-200112150-00006. [DOI] [PubMed] [Google Scholar]
- Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Homayoon F, Howard AA, Schoenbaum EE. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. Journal of General Internal Medicine. 2002;17:377–381. doi: 10.1046/j.1525-1497.2002.10644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangsberg DR, Hecht FM, Charlebois ED, Zolopa AR, Holodniy M, Sheiner L, Moss A. Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS. 2000;10:357–366. doi: 10.1097/00002030-200003100-00008. [DOI] [PubMed] [Google Scholar]
- Bing EG, Burnman MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, Sharpior M. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Archives of General Psychiatry. 2001;58:721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- Elliott A. Anxiety and HIV Infection. STEP Perspective. 1998;98:11–14. [PubMed] [Google Scholar]
- Ferrando SJ, Wapenyi K. Psychopharmacological treatment of patients with HIV and AIDS. Psychiatric Quarterly. 2002;73:33–49. doi: 10.1023/a:1012840717735. [DOI] [PubMed] [Google Scholar]
- Greenblatt DJ, von Moltke LL, Harmatz JS, Durol AL, Daily JP, Graf JA, Shader RI. Alprazolam-ritonavir interaction: implications for product labeling. Clinical Pharmacology & Therapeutics. 2000;67:335–341. doi: 10.1067/mcp.2000.105757. [DOI] [PubMed] [Google Scholar]
- Hellinger FJ, Encinosa WE. Antiretroviral therapy and health care utilization: a study of privately insured men and women with HIV disease. Health Services Research. 2004;39:949–967. doi: 10.1111/j.1475-6773.2004.00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, Capitanio JP, Widaman KF. Stigma, social risk, and health policy: public attitudes toward HIV surveillance policies and the social construction of illness. Health Psychology. 2003;22(5):533–540. doi: 10.1037/0278-6133.22.5.533. [DOI] [PubMed] [Google Scholar]
- Karaz SS. Insomnia in psychiatric disorders. Clinical Handbook of Insomnia. 2010:229–241. Humana Press. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder. JAMA: the journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes M, Olfson M, Rabkin J, Hasin DS, Alegria AA, Lin KH, Blanco C. Gender, HIV status, and psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2012;73:384–391. doi: 10.4088/JCP.10m06304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squire C, Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Paulose-Ram R, Jonas BS, Orwig D, Safran MA. Prescription psychotropic medication use among the US adult population: results from the third National Health and Nutrition Examination Survey, 1988–1994. Journal of Clinical Epidemiology. 2004;57(3):309–317. doi: 10.1016/j.jclinepi.2003.05.001. [DOI] [PubMed] [Google Scholar]
- Pence BW, Miller WC, Whetten K, Eron JJ, Gaynes BN. Prevalence of DSM-IV-defined mood, anxiety, and substance use disorders in and HIV clinic in the southeastern United States. Journal of Acquired Immune Deficiency Syndromes. 2006;42:298–306. doi: 10.1097/01.qai.0000219773.82055.aa. [DOI] [PubMed] [Google Scholar]
- Roth T. Insomnia: definition, prevalence, etiology, and consequences. Journal of Clinical Sleep Medicine. 2007;3(Suppl. 5):S7–S10. [PMC free article] [PubMed] [Google Scholar]
- Roux P, Fugon L, Michel L, Lert F, Obadia Y, Spire B, Carrieri MP. Determinants of benzodiazepine use in a representative population of HIV-infected individuals: the role of HIV status disclosure (ANRS-EN12-VESPA study) AIDS Care. 2011;23:1163–1170. doi: 10.1080/09540121.2011.555738. [DOI] [PubMed] [Google Scholar]
- Rubinstein ML, Selwyn PA. High prevalence of insomnia in an outpatient population with HIV infection. Journal of Acquired Immune Deficiency Syndromes. 1998;19:260–265. doi: 10.1097/00042560-199811010-00008. [DOI] [PubMed] [Google Scholar]
- Shader RI, Greenblatt DJ, Balter MB. Appropriate use and regulatory control of benzodiazepines. Journal of Clinical Pharmacology. 1991;31:781–784. doi: 10.1002/j.1552-4604.1991.tb01910.x. [DOI] [PubMed] [Google Scholar]
- Singh N, Squier C, Sevek C, Wagener M, Nguyen MH, Yu VL. Determinants of compliance with antiretroviral therapy in patients with human immunodeficiency virus: prospective assessment with implications for enhancing compliance. AIDS Care. 1996;8:261–269. doi: 10.1080/09540129650125696. [DOI] [PubMed] [Google Scholar]
- Valenstein M, Taylor KK, Austin K, Kales HC, McCarthy JF, Blow FC. Benzodiazepine use among depressed patients treated in mental health settings. American Journal of Psychiatry. 2004;161:654–661. doi: 10.1176/appi.ajp.161.4.654. [DOI] [PubMed] [Google Scholar]
- Vesga-Lopez O, Schneier FR, Wang S, Heimberg RG, Liu SM, Hasin DS, Blanco C. Gender differences in generalized anxiety disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Journal of Clinical Psychiatry. 2008;69:1606–1616. [PMC free article] [PubMed] [Google Scholar]