Abstract
Purpose
To investigate retrospectively, based on routine clinical records in an optometric office, the effect of refractive under-correction of the myopic spectacle prescription on myopic progression in children and young adults.
Methods
Patient records of children and young-adult myopes in a private optometric practice in Glendale, Arizona, USA, were initially reviewed to identify those that met the criteria. Information collected from the patient records included: age, gender, the dates and number of their visits (more than one visit was required for use of the data), final prescription, and non-cycloplegic subjective refraction. For each patient visit, the difference in spherical equivalent (SE) between the subjective refraction for maximum visual acuity and the final prescription was calculated for both the left and right eyes. Myopia progression was defined as the difference in SE between the final subjective refraction of the previous visit and that of the subsequent visit. Based on the study criteria, a total of 275 patient visits were obtained from the data collected in 76 patients.
Results
A significant positive correlation was found between the magnitude of under-correction of the refractive error and myopic progression (r = 0.301, p < 0.01); that is, the greater the under-correction, the greater the myopic progression. In addition, there was a significant positive correlation between myopia progression and subjective refraction (r = 0.166, p = 0.006); that is, the greater the degree of myopia, the greater the effect of under-correction. However, there was no significant correlation between myopia progression and either age (r = −0.11, p = 0.86) or gender (r = −0.82, p = 0.17).
Conclusion
Under-correction of myopia produced a small but progressively greater degree of myopic progression than did full correction. The present finding is consistent with earlier clinical trials and modeling of human myopia.
Keywords: Myopia, Under-correction, Accommodation, Retina-defocus, Near-work
Resumen
Objetivo
Investigar retrospectivamente, basándonos en las historias clínicas rutinarias en un centro optométrico, el efecto de la corrección refractiva insuficiente de la prescripción de gafas para miopía sobre la progresión de esta patología en niños y jóvenes adultos.
Métodos
Se revisaron inicialmente las historias clínicas de niños y jóvenes adultos miopes en un centro optométrico privado de Glendale, Arizona, EEUU, para identificar quiénes cumplían los criterios. La información obtenida de las historias de los pacientes incluyó: edad, sexo, fechas y número de visitas (se requirió más de una visita para poder utilizar la información), prescripción final, y refracción subjetiva no ciclopléjica. Se calculó para cada paciente la diferencia del equivalente esférico (EE) entre la refracción subjetiva para la agudeza visual máxima y la prescripción final, para el ojo derecho y el izquierdo. La progresión de la miopía se definió como la diferencia de EE entre la refracción subjetiva final de la visita anterior y la de la visita siguiente. Basándonos en los criterios de estudio, se obtuvo un total de 275 visitas de pacientes de la información recogida de 76 pacientes.
Resultados
Se halló una correlación positiva considerable entre la magnitud de corrección insuficiente del error refractivo y la progresión de la miopía (r = 0,301, p < 0,01); es decir, cuanto mayor era la insuficiencia de la corrección, mayor era la progresión de la miopía. Además, existía una correlación positiva significativa entre la progresión de la miopía y la refracción subjetiva (r = 0,166, p = 0,006); es decir, cuanto mayor era el grado de miopía, mayor era el efecto de la corrección insuficiente. Sin embargo, no existió correlación significativa entre la progresión de la miopía y la edad (r = −0,11, p = 0,86) o el sexo (r = −0,82, p = 0,17).
Conclusión
La corrección insuficiente de la miopía produjo un pequeño aunque progresivamente mayor grado de progresión de la miopía que la corrección total. El presente hallazgo es consistente con estudios clínicos anteriores y la modelación de la miopía humana.
Palabras clave: Miopía, Corrección insuficiente, Acomodación, Desenfoque retiniano, Trabajo de cerca
Introduction
Myopia is an international public health problem. It was estimated to have a prevalence of approximately 25 percent in the U.S. Caucasian adult population1 between the years of 1971–1972. Notably, between the years of 1999–2004, this increased significantly to approximately 42 percent.2 In Asian countries like Japan, there is yet a higher prevalence of myopia (as high as 66%) among the young-adult population.3 Furthermore, recent studies (e.g., Saw et al.,4) have reported that there is an even greater prevalence of myopia in Asian countries with increasing age, with it ranging from 4 percent by 6 years of age, and to 40 percent by 12 years of age, with a further increase to 75 percent or more by 18 years of age.
Various methods have been employed in an attempt to reduce the progression of myopia.4–7 Spectacles, contact lenses, atropine, and refractive surgery are the primary current options to treat and/or remediate myopia.8,9 For example, the use of plus-powered spectacles when performing near work may provide some degree of success by reducing the chronic amount of potentially myopigenic retinal defocus,10 and furthermore by reducing the blur-driven accommodative magnitude.11 In some studies, bifocal and progressive addition spectacle lenses (PALs) have demonstrated significant differences in reducing the progression of myopia,12 whereas others have not.13 Lastly, and more recently, studies on children have demonstrated that orthokeratology and bifocal contact lenses may arrest myopic development to some extent.8,9,13,14 Thus, this remains an active area of investigation.
Under-correction of the myopic spectacle correction has been discussed in the literature from the mid-1850s (see Curtin5 for a review). While the rationale for prescribing modest myopic under-correction is somewhat vague, it was believed to represent an attempt to reduce the accommodative stimulus and demand at near,7 and thus reduce the blur drive for accommodation, with the related biomechanical aspects of accommodation per se at near (e.g., mechanical stress at the posterior pole) thought to be a myopigenic factor. However, the results have been equivocal.5–7 It may also represent the near lens which “balances” the accommodative and vergence systems.11
Thus, the purpose of the present investigation was to determine retrospectively, based on clinical optometric records, the effect of refractive under-correction of myopic spectacle prescription and its influence on myopic progression in a clinical population of children and young-adult myopes.
Methods
The present study was designed to collect data in myopic patients from a private optometric practice in Glendale, Arizona, USA. All records used in this investigation belonged to one optometrist who had examined the majority of the patients at each visit over a period of 6–8 years.
Three of the authors gathered and assessed all of the patient record data from the optometric practice. Patient records were initially reviewed manually to identify potential myopic subjects. The selection criteria were then as follows: (1) the patient had to be a myope at the initial visit; (2) the patient had to be examined by the same doctor at all visits; (3) the patient had to be free of any ocular, systemic, or neurological abnormalities; (4) each follow-up visit should have occurred over a interval of approximately 1 year; and (5) the patient had to be a full-time spectacle wearer. With these criteria, out of a total of 2000 patients, 76 patients (27 males and 49 females) aged 11 to 33 (mean: 14 ± 5) years, were found to be suitable for analysis (∼4%) (see Table 1). Out of the 76 subjects, 61 subjects were between the ages of 11–19 years, and the remaining 15 were adults between the ages of 20–33 years. The information collected from these patient records included: age, gender, dates and number of their visits (more then one visit was required for use of the data), habitual prescription, final prescription, and non-cycloplegic subjective refraction. All patients had multiple vision examinations, with each visit considered as a separate data entry. Data were included in the analysis only for successive visits having approximately a one-year follow up. Spherical equivalent (SE; sum of the spectacle spherical power plus half of the cylinder power in diopters) refraction was calculated for the subjective refraction at each visit. Subjective refractions were initially performed with the conventional endpoint criterion of maximum plus for maximum visual acuity, and then either the under-correction or full-correction was prescribed. All data were recorded into an Excel spreadsheet for subsequent analysis. Parametric correlational analysis was performed using SPSS software (ver 20.0), with a probability level of 0.05.
Table 1.
Summary of the subject characteristics. Refprogression denotes spherical equivalent refractive error progression in the subsequent visit.
| N = 275 | Maximum | Minimum | Mean | Std. Deviation |
|---|---|---|---|---|
| Age (yrs) | 11.00 | 33.00 | 14.3 | 5.2 |
| Subjective refraction (D) | −10.50 | 0.00 | −3.09 | 2.11 |
| Under-correction (D) | −0.50 | 0.00 | −0.17 | 0.18 |
| Refprogression (D) | −1.25 | +0.25 | −0.27 | 0.27 |
N: total number of patient visits.
The data were further analyzed and categorized. For each patient visit, the difference in SE between the subjective refraction for maximum visual acuity and the final prescription was calculated. The final refractive correction prescribed was based on the case history of the patient and the amount of myopic progression that was found over the previous years. “Myopic progression” was defined as the difference in SE between the subjective refraction of the previous visit and that of the subsequent annual visit. A total of 275 patient visits were used in the analysis. The magnitude of under-correction ranged from zero or none, which represented “no-under-correction”, to −0.50D, which represented “under-correction”. The under-correction magnitude and refractive error progression were determined for each subject, and correlational analyses were performed on the data.
There were a total of 76 patients, with 275 patient visits, involved in the data analysis. This included 44 subject visits with −0.50D, 21 subject visits with −0.37D, 63 subject visits with −0.25D, 22 subject visits with −0.13D under-correction, and 125 subject visits with 0D or full-correction. See Table 2.
Table 2.
Summary of the subject demographics, full/under-correction and mean refractive error change.
| Type of correction | Number of subject visits | Mean age (yrs) | Mean refractive error change |
|---|---|---|---|
| −0.5D | 44 | 12 | −0.45D |
| −0.37D | 21 | 18 | −0.29D |
| −0.25D | 63 | 15 | −0.29D |
| −0.12D | 22 | 14 | −0.28D |
| 0D | 125 | 13 | −0.20D |
All statistical analyses were performed using the SPSS software (version 20.0, IBM, NY, USA) for Macintosh and Prism (GraphPad, La Jolla, CA). Normality of all data distributions was confirmed by Kolmogorov–Smirnov test (alpha = 0.05). All of the data were normally distributed (p > 0.10). Study protocol followed the Declaration of Helsinki. It was approved by the college's internal review board.
Results
A plot of the magnitude of under-correction of the spectacle prescription versus the refractive error change between successive visits is presented in Fig. 1. A significant positive correlation was found between the under-correction of refractive error and the myopic progression (r = 0.301, p < 0.01). That is, the greater the undercorrection, the greater the myopic progression. In addition, there was a significant positive correlation between the myopic progression and the subjective refraction (r = 0.166, p = 0.006). That is, for a given amount of under-correction, the greater the myopic refraction, the greater the degree of myopic progression. However, there was no significant correlation between myopia progression and either age (r = −0.11, p = 0.86) or gender (r = −0.82, p = 0.17). See Table 3.
Figure 1.
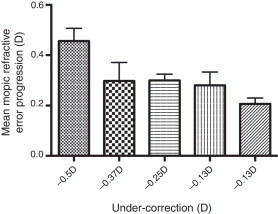
Plot of under-correction of myopia and mean refractive error progression. Plotted is the mean + 1SEM.
Table 3.
Summary of the correlation between different parameters and refractive error progression in the subsequent visit.
| N = 275 | Gender | Age | Subjective | Under-correction |
|---|---|---|---|---|
| Correlation | −0.82 | −0.11 | 0.166 | 0.301 |
| p-value | 0.17 | 0.86 | 0.006 | <0.01 |
N: total number of patient visits.
One-way ANOVA [F(19, 184) = 1.95, p = 0.013], was performed to assess the impact of magnitude of under-correction (OD to −0.5D) on the refractive error change, and a significant effect was observed. In addition, the Bonferroni post hoc analysis was performed. Refractive error change for the 0.5D under-correction was significantly different from every other under-correction and the full-correction magnitudes. This trend was only observed for the other under-correction or full-correction magnitude with respect to the −0.50D under correction comparison. See Table 4.
Table 4.
Summary of the significant differences between under or full correction and their refractive error change.
| Full/under-correction | Full/under-correction | Mean difference | Standard error | Significance (p-value) |
|---|---|---|---|---|
| −0.5D | −0.37D | −0.240* | 0.073 | 0.012 |
| −0.25D | −0.169* | 0.056 | 0.028 | |
| −0.12D | −0.252* | 0.072 | 0.006 | |
| 0D | −0.266* | 0.051 | 0.000 | |
| −0.37D | −0.5D | 0.240* | 0.073 | 0.012 |
| −0.25D | 0.071 | 0.067 | 1.000 | |
| −0.12D | −0.012 | 0.081 | 1.000 | |
| 0D | −0.026 | 0.063 | 1.000 | |
| −0.25D | −0.5D | 0.169* | 0.056 | 0.028 |
| −0.37D | −0.071 | 0.067 | 1.000 | |
| −0.12D | −0.083 | 0.066 | 1.000 | |
| 0D | −0.097 | 0.042 | 0.210 | |
| −0.12D | −0.5D | 0.252* | 0.072 | 0.006 |
| −0.37D | 0.012 | 0.081 | 1.000 | |
| −0.25D | 0.083 | 0.066 | 1.000 | |
| 0D | −0.014 | 0.062 | 1.000 | |
| 0D | −0.5D | 0.266* | 0.051 | 0.000 |
| −0.37D | 0.026 | 0.063 | 1.000 | |
| −0.25D | 0.097 | 0.042 | 0.210 | |
| −0.12D | 0.014 | 0.062 | 1.000 | |
Discussion
Under-correction of myopia has been considered a strategy for retardation of either a child's or a young-adult's myopic progression.5 Prescription of spectacle lenses with under-correction of modest magnitude (e.g., 0.50D) was thought to be effective by some, as it reduced the near accommodative stimulus, and in-turn partially reduced the blur-driven accommodative response required for clarity of near vision without much sacrifice to distance visual acuity.10 In addition, it reduced the potentially myopigenic retinal defocus at near, as it also effectively functioned as a low plus lens add for near to reduce the blur-driven component of the overall accommodative stimulus.10,11
The findings from 2 recent clinical trials have demonstrated consistent results regarding under-correction of spectacle refractive correction and its influence on myopia progression. The first was a randomized study performed by Chung et al.,15 on 94 myopic Hong Kong Chinese children aged 9–14 years. Half were prescribed the full cycloplegic distance spectacle refraction, whereas the others were purposely under-corrected by 0.75D, thus allowing them to maintain an acceptable distance visual acuity of at least 20/40. In other words, if the subject's conventionally based distance refractive correction were −2.00D, he/she would be prescribed −1.25D. The other group wore the full-correction (e.g., −2.00D) that provided them with a distance visual acuity of at least 20/20. Their evaluative techniques included static retinoscopy (non-cycloplegic), keratometry, subjective cycloplegic refraction, and a-scan ultrasonography. Subjects were instructed to wear their new subjective, cycloplegic refractive correction during all waking hours. The mean initial refraction in each group was −2.68D. At the end of the 2-year clinical trial period, the rate of myopic progression was significantly greater (p < 0.01) in the under-corrected group (0.5 D per year), as compared with those who were fully corrected (0.38 D per year). The investigators speculated that the human eye cannot detect the sign of the blur-only-based retinal defocus, and thus both myopic and hyperopic retinal defocus may be myopigenic. The results of the above Chung et al.15 study were later confirmed by Adler and Millodot.16 This investigation was conducted in myopic Israeli children (n = 48) between 6 and 15 years of age. Half were fully-corrected with spectacles in the distance, whereas the balance were under-corrected by 0.5 D in the distance, with both groups having the same mean initial myopic refractive error (−2.90 D), similar to that of the Chung et al.,16 study (−2.68D). All were instructed to wear their refractive correction full-time. Details of the clinical test protocol were not provided. At the end of the 18-month clinical trial period, the mean rate of the myopic progression was greater in those that were under-corrected versus their fully-corrected cohort (0.66 D vs 0.55 D per year respectively) (p = 0.05). Thus, both investigations concluded that under-correction of myopia producing myopic defocus at far, and reduced accommodative stimulus/retinal-defocus at near, did not slow the rate of myopic progression, and if anything, it appeared to accelerate it.
The results from both of the aforementioned investigations were somewhat unexpected, as previous animal-based studies have demonstrated that purposeful under-correction of myopia slowed the myopic progression.17,18 There was one very early clinical study in humans that was supportive of the animal models. Tokoro and Kabe19 compared the myopia progression rates, as well as corneal power, crystalline lens power, and axial length, during a 3-year period in a total of 33 children who entered the study with low myopia. Of these individuals, 13 were prescribed the full-correction to wear at all times, 10 were provided with an under-correction of one diopter or more to wear at all times, and the remaining 10 were prescribed the full correction and advised ‘to be worn in case of need’. The mean change in refractive error from the study was considerably lower in the under-corrected group (0.47D) as compared to the fully corrected group (0.83D). The axial length increase and crystalline lens power changes were greatest in the full-time full correction group, and least in the under-correction group. However, subgroup sizes were small (n = 10–13). In addition, large magnitudes of under-correction were employed in this investigation, which produced less myopic progression. The fact that the present clinical retrospective study supported the earlier prospective investigations suggests robustness of the full-correction strategy and effect. The present investigation also found a significant correlation between the myopic under-correction magnitude and myopic progression. Similarly, the Adler and Millodot study16 also challenged the notion of under-correcting myopic patients to slow the progression of myopia. They too found an increase in myopic progression in the under-corrected group, similar to that of the Chung et al. group,15 in agreement with the present study. Both studies15,16 concluded that any retinal defocus could be myopigenic, as was earlier speculated by Ong and Ciuffreda,6 at least in humans.
The findings in the present investigation, as well as the aforementioned clinical trials,15,16 however, do not support the conclusions of the very-early under-correction study of Tokoro and Kabe.19 They reported that the mean change in refractive error was reduced in the under-corrected group as compared to the fully-corrected group. However, they19 reported their findings based on small subgroup sample sizes. Thus, based on the findings of the two previous relatively large prospective investigations,15,16 as well as that of the present retrospective study, under-correction does not appear to represent an appropriate treatment modality for slowing myopic progression, at least in humans. This is consistent with the idea that full-correction of myopia is the current standard of care,23 as offered by contemporary optometric clinicians, that would optically position the far point of the eye as close to infinity as possible (i.e., just within the distal edge of the depth-of-focus via the clinical concept of hyperfocal-refraction22,23), thereby reducing any potential under-corrected, retinal defocus-induced, blur signals22 at distance. At near, it would reduce the hyperopic defocus at the fovea.22,23
Newer findings in both human and animal models (e.g., Smith et al.,20) have reported on the possible role played by the peripheral refraction magnitude and direction on axial elongation of the eye, and the related myopic progression. It has been proposed that the interaction of a central myopic refraction and a relatively hyperopic peripheral refraction could produce axial elongation in some myopes, with the unique influence of the periphery on central eye growth. (See Charman and Radhakrishnan21 for a review). The undercorrection at distance would shift the hyperfocal refractive plane more anteriorly, thus reducing the hyperopic retinal defocus in the periphery.22 Per recent theories of central versus peripheral retinal interactions, this should reduce axial elongation, and hence reduce myopia. This notion needs to be tested both in animal studies and in human clinical trials to assess its efficacy.22,23
According to the large body of animal studies, myopic under-correction at distance should result in a reduction in the relative rate of myopic progression, as it induces myopic defocus (See Wallman and Winawer24 for a review). For example, one investigation25 reported that when myopic defocus was imposed in chickens, myopic progression was inhibited. Similar experiments have also been performed on infant rhesus monkeys with positive lenses that were fitted binocularly (e.g., Smith, Hung and Harwerth26). These lenses resulted in a relative decrease in eye growth of the myopia. However, this does not appear to be the case for humans. One reason could be that the animal studies were generally conducted during the very early developmental period of the species, which corresponds to infancy in humans. During this time period, myopia may not have developed significantly in animals. In addition, it is possible that the “STOP” signals27 involved become weaker with age. Lastly, there could also be inter-species differences. Further comparative studies are needed.
Lastly, further longitudinal investigations are needed in humans, which in essence serve as the gold standard, to understand better the relation between corrective modality and myopic progression. One attempt in this direction is the ongoing investigation in 200 myopic Chinese children aged 7–15 years wearing single vision lenses with an under-correction of 0.50D versus fully corrected children.28 In addition, documenting quantitatively changes in the related ocular components is essential to understand more comprehensively and quantitatively the mechanism of retinal defocus-induced axial elongation leading to myopia progression in humans.
Conclusions
Under-correction of myopia produced a greater degree of myopic progression than did the full-correction. This finding is consistent with nearly all of the earlier studies in humans. Full-correction of myopia would be beneficial and most efficacious in children and young adults with myopia. Clinicians should prescribe the full myopic refraction, in the absence of other contrasting case history aspects.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
- 1.Sperduto R.D., Seigel D., Roberts J., Rowland M. Prevalence of myopia in the United States. Arch Ophthalmol. 1983;101:405–407. doi: 10.1001/archopht.1983.01040010405011. [DOI] [PubMed] [Google Scholar]
- 2.Vitale S., Sperduto R.D., Ferris F.L. Increased prevalence of myopia in the United States between 1971–1972 and 1999–2004. Arch Ophthalmol. 2009;127:1632–1639. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 3.Matsumura H., Hirai H. Prevalence of myopia and refractive changes in students from 3 to 17 years of age. Surv Ophthalmol. 1999;44:S109–S115. doi: 10.1016/s0039-6257(99)00094-6. [DOI] [PubMed] [Google Scholar]
- 4.Saw S.M., Gazzard G., Au Eong K.G., Tan D.T. Myopia: attempts to arrest progression. Br J Ophthalmol. 2004;86:1306–1311. doi: 10.1136/bjo.86.11.1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Curtin B. Harper and Row; Philadelphia: 1985. The myopias: basic science and clinical management. [Google Scholar]
- 6.Ong E., Ciuffreda K.J. Optometric Extension Program Foundation Press; Santa Ana: 1997. Accommodation, Nearwork, and Myopia. [Google Scholar]
- 7.Rosenfield M., Gilmartin B. Butterworth-Heinemann; Boston: 1998. Myopia and nearwork. [Google Scholar]
- 8.Walline J.J., Lindsley K., Vedula S.S., Cotter S.A., Mutti D.O., Twelker J.D. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2011;7:CD004916. doi: 10.1002/14651858.CD004916.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santodomingo-Rubido J., Villa-Collar C., Gilmartin B., Gutiérrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53:5060–5065. doi: 10.1167/iovs.11-8005. [DOI] [PubMed] [Google Scholar]
- 10.Hung G.K., Ciuffreda K.J. Quantitative analysis of the effect of near lens addition on accommodation and myopigenesis. Curr Eye Res. 2000;20:293–312. [PubMed] [Google Scholar]
- 11.Jiang B.C., Bussa S., Tea Y.C., Seger K. Optimal dioptric value of near addition lenses intended to slow myopic progression. Optom Vis Sci. 2008;85:1100–1105. doi: 10.1097/OPX.0b013e31818b9f47. [DOI] [PubMed] [Google Scholar]
- 12.Gwiazda J., Hyman L., Hussein M. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44:1492–1500. doi: 10.1167/iovs.02-0816. [DOI] [PubMed] [Google Scholar]
- 13.Cho P., Cheung S.W., Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30:71–80. doi: 10.1080/02713680590907256. [DOI] [PubMed] [Google Scholar]
- 14.Aller T.A., Wildsoet C. Bifocal soft contact lenses as a possible myopia control treatment: a case report involving identical twins. Clin Exp Optom. 2008;9:394–399. doi: 10.1111/j.1444-0938.2007.00230.x. [DOI] [PubMed] [Google Scholar]
- 15.Chung K., Mohidin N., O’Leary D.J. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Res. 2002;42:2555–2559. doi: 10.1016/s0042-6989(02)00258-4. [DOI] [PubMed] [Google Scholar]
- 16.Adler D., Millodot M. The possible effect of undercorrection on myopic progression in children. Clin Exp Optom. 2006;89:315–321. doi: 10.1111/j.1444-0938.2006.00055.x. [DOI] [PubMed] [Google Scholar]
- 17.Smith E.L., Hung L.F. The role of defocus in regulating refractive development in infant monkeys. Vision Res. 1999;39:1415–1435. doi: 10.1016/s0042-6989(98)00229-6. [DOI] [PubMed] [Google Scholar]
- 18.Schaeffel F., Troilo D., Wallman J., Howland H.C. Developing eyes that lack accommodation grow to compensate for imposed defocus. Vis Neurosci. 1990;4:177–183. doi: 10.1017/s0952523800002327. [DOI] [PubMed] [Google Scholar]
- 19.Tokoro T., Kabe S. Treatment of the myopia and the changes in optical components. Report II. Full-or under-correction of myopia by glasses. Nihon Ganka Gakkai Zasshi. 1965;69:140–144. [PubMed] [Google Scholar]
- 20.Smith E.L., 3rd, Hung L.F., Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009;49:2386–2392. doi: 10.1016/j.visres.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Charman W.N., Radhakrishnan H. Peripheral refraction and the development of refractive error: a review. Ophthalmic Physiol Opt. 2010;30:321–338. doi: 10.1111/j.1475-1313.2010.00746.x. [DOI] [PubMed] [Google Scholar]
- 22.Ciuffreda K.J., Vasudevan B. Effect of nearwork-induced transient myopia on distance retinal defocus patterns. Optometry. 2010;81:153–156. doi: 10.1016/j.optm.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 23.Ciuffreda K.J. Accommodation, pupil and presbyopia. In: Benjamin W.J., editor. Borish's clinical refraction: principles and practice. Saunders; Philadelphia: 2000. pp. 77–120. [Google Scholar]
- 24.Wallman J., Winawer J. Homeostasis of eye growth and the question of myopia. Neuron. 2004;43:447–468. doi: 10.1016/j.neuron.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 25.Schmid K.L., Wildsoet C.F. The sensitivity of the chick eye to refractive defocus. Ophthalmic Physiol Opt. 1997;17:61–67. [PubMed] [Google Scholar]
- 26.Smith E.L., 3rd, Hung L.F., Harwerth R.S. Effects of optically induced blur on the refractive status of young monkeys. Vision Res. 1994;34:293–301. doi: 10.1016/0042-6989(94)90088-4. [DOI] [PubMed] [Google Scholar]
- 27.Morgan I., Megaw P. Using natural STOP growth signals to prevent excessive axial elongation and the development of myopia. Ann Acad Med Singapore. 2004;33:16–20. [PubMed] [Google Scholar]
- 28.Li S.M., Li S.Y., Liu L.R. Full correction and undercorrection of myopia evaluation trial (FUMET): design and baseline data and baseline data. Clin Exp Ophthalmol. 2012;41:329–338. doi: 10.1111/j.1442-9071.2012.02884.x. [DOI] [PubMed] [Google Scholar]


