Abstract
Optic neuritis is an inflammation of the optic nerve and may be related to different systemic conditions. The clinical presentation of this pathology usually includes sudden loss of visual acuity (VA) which may be unilateral or bilateral, visual field restriction, pain with eye movements, dyschromatopsia, a relative afferent pupillary defect and optic disk swelling. Optic neuritis in children has specific clinical features and a better prognosis than in adulthood. Although usually appears an underlying viral disease, the main concern for practitioners is the relationship of optic neuritis with multiple sclerosis. In addition to the classical techniques as magnetic resonance imaging (MRI), current tendencies of diagnosis for eye practitioners include new imaging devices as optical coherence tomography (OCT), useful to show a thinning of the retinal fibers layer (RFL) after the inflammatory episode. Regarding the management of these patients, short-term intravenous steroid dosages seem to be the best option to treat acute attacks characterized by a very poor bilateral VA.
Keywords: Optic neuritis, Childhood, Multiple sclerosis, Optical coherence tomography
Resumen
La neuritis óptica es una inflamación del nervio óptico, que puede relacionarse con diferentes condiciones sistémicas. La presentación clínica de esta patología incluye normalmente pérdida súbita de agudeza visual (AV), que puede ser unilateral o bilateral, restricción del campo visual, dolor al mover los ojos, discromatopsia -defecto pupilar aferente relativo- y edema del disco óptico del disco óptico. La neuritis óptica en niños tiene características clínicas especiales, y un mejor pronóstico que en los adultos. Aunque normalmente parece una enfermedad vírica subyacente, la principal dificultad para los especialistas es la relación de la neuritis óptica con la esclerosis múltiple. Además de las pruebas clásicas como la resonancia magnética (RM), las tendencias actuales de diagnóstico para los profesionales de la salud visual incluyen nuevos dispositivos de imagen tales como la tomografía de coherencia óptica (TCO), que es útil para reflejar el adelgazamiento de la capa de fibras de la retina tras el episodio inflamatorio. Respecto al tratamiento de estos pacientes, la administración de esteroides intravenosos a corto plazo parece ser la mejor opción para tratar los ataques agudos, caracterizados por una AV bilateral muy reducida.
Palabras clave: Neuritis óptica, Infancia, Esclerosis múltiple, Tomografía de coherencia óptica
Introduction
Optic neuritis is a primary inflammation of the optic nerve. Clinically, it can appear as an isolated condition or associated to a variety of systemic autoimmune disorders. Its incidence is of 1–5 per 100,000 per year.1–4 It mainly affects the Caucasian population, most often during the spring period, and especially to those living at high geographic latitudes.1 Its origin is inflammatory and the pathophysiology of this condition includes a peripheral activation of T-cells that may cross the blood brain barrier causing a delayed type IV hypersensitivity reaction. This process leads to destruction of myelin,5 with also the involvement of the axon, something that can be confirmed by mean of an optical coherence tomography (OCT) examination. All this process has a negative impact on visual acuity (VA).6
The typical presentation of optic neuritis is a sudden and unilateral visual loss, with VA ranging from levels of 0.8 in decimal scale to no light perception (NPL). Ninety percent of patients refer pain of variable intensity, usually periocular, which is associated with ocular movements or may be a prelude of the episode of optic neuritis. The evolution of this conditions ranges from days to weeks and is common the association to phosphenes and flashes of light. Other clinical finding that can be also associated with optic neuritis is the Uhthoff’ phenomenon that consists on a decreased VA in presence of a high body temperature or during physical exercise.1 Likewise, other clinical features of optic neuritis are abnormal color vision, reduced contrast sensitivity function, visual field loss characterized by central, paracentral or altitudinal scotomas, and the presence of a relative afferent pupillary defect (RAPD), which is more evident in unilateral cases. In some cases, a mild to moderate Tyndall effect may appear in the anterior chamber or in the vitreous as well as a peripheral retinal periphlebitis (12% of patients). This last sign has been proposed as an indicator of a greater probability of developing multiple sclerosis (MS).7 In 36–58% of patients, optic neuritis is accompanied by papillary edema or optic head nerve swelling, whereas in the rest of cases inflammatory involvement occurs in the retrobulbar optic nerve portion and, therefore, the appearance of the optic nerve is normal.8
VA loss and pain are limited in time and occurs during the episode of acute inflammation. From this moment, the remyelination and proliferation of sodium channels in the neuronal segments begins, which is a process that can last even more than two years.9 The same duration has been reported for the reorganization of the cortical activation.10 Final VA is in relation with the severity of the initial VA loss. Ninety-four percent of patients whose VA falls to less than 0.6 during the episode of optic neuritis recover their previous VA. Similarly, 64% of patients whose VA drops to perception of light (PL) recovered a VA of 0.5 or better.11 However, VA tends to fluctuate after an episode of optic neuritis. Furthermore, it is frequent the perception of the Uhthoff’ phenomenon, mentioned above, and the Pullfrich’ phenomenon, which is exemplified with a pendulum seeming to describe an ellipse despite moving in a single plane, as a result of an asymmetric velocity of conduction between both optic nerves.12 As RAPD is dependent on ratio of functional axons between both eyes, all these phenomena described may remain in most cases after the episode of optic neuritis. Likewise, pallor may remain normally in the temporal portion of optic nerve (Fig. 1).
Figure 1.

Optic disk temporal pallor after an episode of bilateral optic neuritis in a 13 years-old patient with a VA of 0.2 (decimal scale).
The diagnosis of optic neuritis is complex and may lead to frequent errors.1 Optic neuritis of the adult is associated with autoimmune (Lupus erythematosus, sarcoidosis, Behçet's disease) and infectious diseases (viral etiology, syphilis, tuberculosis or Lyme disease). The differential diagnosis of optic neuritis also includes optic neuropathies of different etiologies such us compressive, ischemic, hereditary, toxic and nutritional.
Presentation and prognosis of optic neuritis in children
Pediatric optic neuritis is considered as a different entity in comparison to neuritis that can be found in adults. Generally, optic neuritis in the pediatric population has a good prognosis.13,14 It is normally bilateral and occurs after a viral infection (measles, mumps, chicken pox, pertussis, infectious mononucleosis and immunizations). It has also been referred as a result of a biotinidase deficiency.15,16 The clinical diagnosis of the condition is performed according to the following findings: VA loss, which tends to be more severe than in adulthood, the presence of moderate pain during activity of the extrinsic eye muscles, RAPD, dyschromatopsia and the appearance of the optic nerve head.
Specific studies on optic neuritis in children are rare, usually heterogeneous and with a limited number of patients. A meta-analysis conducted by Waldman revealed that most of studies about this topic were observational (case control, cohort studies) or descriptive (case reports, case series) and that was curious the lack of randomized clinical trials in the scientific literature.17 Table 1 shows the results of some relevant studies focused on the classical features of pediatric optic neuritis. The work of Waldman established a clear relationship between the age and the type of presentation, with a greater possibility of unilateralism as the age increases.17 Also, optic atrophy has been identified in 85% of cases of pediatric optic neuritis and does not have a strict correlation with VA,20 although a pale disk at presentation is usually related to a poorer visual outcome than children with normal or swelling optic disk at presentation.21
Table 1.
Results of the studies included in the review.
| Author (year) | Study design | No. of patients analyzed | Average age (years) | Bi (%) | Uni (%) | VFI (%) | ONS (%) |
|---|---|---|---|---|---|---|---|
| Bonhomme et al. (2009)15 | Cohort | 29 | 9.7 ± 3.4 | 65 | 34 | 62 | 69 |
| Brady et al. (1999)19 | Cohort | 25 | 9.4 | 54 | 45 | Not provided | Not provided |
| Waldmann et al. (2011)14 | Meta-analysis | 93 | 9.5 ± 3.6 | 55 | 45 | Not provided | Not provided |
Abbreviations: Uni, unilateral; Bi, bilateral; VFI, visual field involvement; ONS, optic nerve swelling.
Optic neuritis and multiple sclerosis
The clinical pattern of MS at any age is characterized by both sensory and motor symptoms at onset and predominantly monosymptomatic presentation with a relapsing-remiting pattern.22 Optic neuritis may be the first manifestation of MS in adults and children.23 In adults, after an episode of unilateral optic neuritis, the possibility of developing MS reaches 38% in the following 10 years. This percentage rises to 56% if there are brain abnormalities in magnetic resonance imaging (MRI).24 In the pediatric population, limited data are available and statistics are not well-established, as a result of methodological variability, bias and limitations of the studies mentioned above. The rate of conversion to MS is not exactly delimited and different studies have reported results from 4% to 36% (Table 2).21,25,29–34 The largest sample published by Luchinetti et al. reported that 13% of patients with isolated optic neuritis progressed to a clinically or laboratory-supported definite MS by 10 years of follow-up, 19% by 20 years, 22% by 30 years, and 26% by 40 years.25 Age is also a parameter that correlates with the increased risk for developing multiple sclerosis (MS) in childhood, probably as a result of differential factors in the immune system.26 Although the type of presentation (bilateral vs unilateral) is not a factor in the development of MS,17 some authors have found a greater risk in those patients who had sequential (with a difference between both eyes of more than 2 weeks) or recurrent optic neuritis compared to those who had a single episode occurring in either eye or both eyes simultaneously (with a difference between both eyes of less than 2 weeks).17,25
Table 2.
Results of different studies regarding the conversion of optic neuritis to multiple sclerosis.
| Author (year) | No. of patients analyzed | Rate of progression to MS | Follow-up (years) | Country |
|---|---|---|---|---|
| Kriss et al. (1988)29 | 39 | 15% | 8.8 | England |
| Kennedy et al. (1961)30 | 18 | 16.5% | Not provided | United States of America |
| Luchinetti et al. (1997)25 | 79 | 19% | 20 | United States of America |
| Lana-Peixoto (2001)31 | 27 | 4% | 16 | Brazil |
| Parkin et al. (1984)32 | 19 | 5.26% | 26 | New Zealand |
| Wilejto et al. (2006)33 | 36 | 36% | 2.4 | Canada |
| Heussinger et al. (2013)34 | 34 | 26.5% | 4.81 | Netherlands |
| Sun et al. (2011)21 | 24 | 12.5% | 11 | Taiwan |
| Hwang et al. (2002)27 | 23 | 4.35% | 5 | Korea |
| Mizota et al. (2004)28 | 41 | 31% | 10.7 | Japan |
Abbreviation: MS, multiple sclerosis.
Ethnicity seems to be another factor to be considered in the developing of MS. Sun et al. found a higher rate of progression to MS after an acute episode of optic neuritis in Taiwanese children comparing to Korean but a lower rate comparing to Japanese children.21,27,28
Brain MRI is the imaging technique of choice after a diagnosis of optic neuritis and should be performed preferably during the following two weeks after the initial symptoms.35 The absence of lesions, typically oval and located in the periventricular white matter areas, is a good prognostic factor for both the recovery of the VA to the previous levels and the decrease of the probability of future development of MS. Bonhomme work suggests that, in the pediatric population, the risk for developing MS after a first episode of optic neuritis is higher if one or more white matter lesions on the baseline MRI are present. In this same work, the authors observed that no patients developed MS in the presence of a negative MRI at the time of the appearance of the episode of optic neuritis.18
Other diagnostic tests that may be used for the diagnosis of the primary demyelinating optic neuritis are lumbar puncture, visual evoked potentials (VEP) and OCT, which can be useful to show a thinning of the nerve fibers layer after an episode of optic neuritis36 (Fig. 2).
Figure 2.
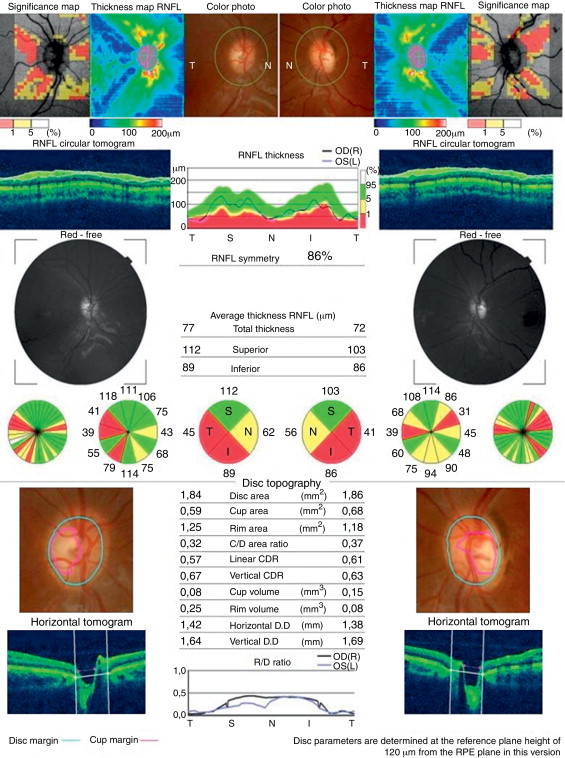
Papillary optical coherence tomography showing a retinal fibers layer thinning in a 13 years-old patient after an acute episode of bilateral optic neuritis.
Eye practitioners should be also aware of neuromyelitis optica (NMO). This condition, also known as Devic disease, is an autoimmune disorder characterized by optic neuritis and myelitis that spares the brain in early stages. The ocular symptoms of NMO include optic neuritis, vision loss and unilateral or bilateral ocular pain. It is a much more severe condition and causes a greater impairment than MS-associated optic neuritis.37
Treatment
The ONTT (Optic Neuritis Treatment Trial) study was aimed to assess the efficacy of corticosteroids for the treatment of optic neuritis. With this objective, three groups were randomized and treated respectively with a combination of intravenous and oral steroids (250 mg of methylprednisolone 4 times a day for 3 days and oral prednisolone 1 mg/kg for 11 days), only with oral prednisolone (1 mg/kg for 14 days) and a third group with a placebo substance for 14 days. In adults, corticosteroid treatments did not protect against recurrences in a follow-up period of 3 years, although the recovery in the group treated with intravenous corticosteroids was found to be faster. Furthermore, the group treated with oral steroids was observed to have a higher frequency of recurrences during a one-year follow-up in comparison with the other two groups.38 This study, however, does not include pediatric patients and, to the best of our knowledge, there are no similar clinical trials in this type of population. Therefore, the most widespread recommendation among authors for pediatric patients is conservative (wait and see) for unilateral and no severe bilateral cases of pediatric optic neuritis.1,39 Bilateral cases with severe loss of VA are recommended to be treated with a short dosage of intravenous methylprednisolone (15 mg/kg/day for 3 days).1 In steroid-resistant bilateral optic neuritis, plasma exchange (PE) has been proposed as an alternative to achieve full recovery of VA.40
In spite of these guidelines, eye practitioners should remember that acquired optic neuropathy can occur from a myriad of causes, so the prognosis and treatment of optic neuritis also depends on the underlying cause. The treatment of optic neuritis requires first that the physician determine the etiology and comorbidities of the affected patient in order to plan a proper therapeutic plan.41
Conclusions
Optic neuritis is an uncommon condition in the pediatric population and usually underlies a viral cause. The diagnosis is made in the same basis as in the adult population, but its presentation is typically bilateral, with a very low VA and optic nerve swelling. The prognosis is generally good, especially when the patient is younger. In the absence of lesions of the white matter in basal MRI, the probability of developing MS seems to be very limited. Treatment tendencies consist of monitoring, except in bilateral cases with severe loss of VA where, under the physician's criteria, the possibility of short dosages of intravenous corticosteroids may be indicated. Eye care practitioners, as primary care health agents, should be aware of this complex condition in order to provide appropriate information to patients and for an adequate and immediate referral.
Conflict of interest
The author have no conflicts of interest to declare.
References
- 1.Hickman S.J., Dalton C.M., Miller D.H., Plant G.T. Management of acute optic neuritis. Lancet. 2002;360:1953–1962. doi: 10.1016/s0140-6736(02)11919-2. [DOI] [PubMed] [Google Scholar]
- 2.Wakakura M., Ishikawa S., Oono S. Incidence of acute idiophatic optic neuritis and its therapy in Japan. Optic Neuritis Treatment Trial Multicenter Cooperative Research Group. Nihon Ganka Gakkai Zasshi. 1995;99:93–97. [PubMed] [Google Scholar]
- 3.Bojic L., Ivanisevic M., Sinicic A. The incidence of optic neuritis in Split-Dalmatia county, Croatia. Coll Antropol. 2004;28:343–347. [PubMed] [Google Scholar]
- 4.Kinnunen E. The incidence of optic neuritis and its prognosis for multiple sclerosis. Acta Neurol Scand. 1983;68:371–377. doi: 10.1111/j.1600-0404.1983.tb04846.x. [DOI] [PubMed] [Google Scholar]
- 5.Shams P.N., Plant G.T. Optic neuritis: a review. Int MS J. 2009;16:82–89. [PubMed] [Google Scholar]
- 6.Bertuzzi F., Suzani M., Tagliabue E. Diagnostic validity of optic disc and retinal fiber layer evaluations in detecting structural changes after optic neuritis. Ophthalmology. 2010;117:1256–1264. doi: 10.1016/j.ophtha.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 7.Lightman S., McDonald W.T., Bird A.C. Retinal venous scheathing in optic neuritis: its significance for the pathogenesis of multiple sclerosis. Brain. 1987;110:405–414. doi: 10.1093/brain/110.2.405. [DOI] [PubMed] [Google Scholar]
- 8.Optic Neuritis Study Group The clinical profile of optic neuritis: experience of the Optic Neuritis Treatment Trial. Arch Ophthalmol. 1991;109:1673–1678. doi: 10.1001/archopht.1991.01080120057025. [DOI] [PubMed] [Google Scholar]
- 9.Brusa A., Jones S.J., Plant G.T. Long-term remyelination after optic neuritis: a 2-year visual evoked potential and psychophysical serial study. Brain. 2001;124:468–479. doi: 10.1093/brain/124.3.468. [DOI] [PubMed] [Google Scholar]
- 10.Werring D.J., Bullmore E.T., Toosy A.T. Recovery from optic neuritis is associated with a change in the distribution of cerebral response to visual stimulation: a functional MRI study. J Neurol Neurosurg Psychiatry. 2000;68:441–449. doi: 10.1136/jnnp.68.4.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slamovits T.L., Rosen C.E., Cheng K.P., Striph G.G. Visual recovery in patients with optic neuritis and visual loss to no light perception. Am J Ophthalmol. 1991;111:209–214. doi: 10.1016/s0002-9394(14)72261-5. [DOI] [PubMed] [Google Scholar]
- 12.Slavsgold J.E. Pulfrich pendulum phenomenon in patients with a history of acute optic neuritis. Acta Ophthalmol (Copenh) 1978;56:817–826. doi: 10.1111/j.1755-3768.1978.tb06646.x. [DOI] [PubMed] [Google Scholar]
- 13.Morales D.S., Siatkowski R.M., Howard C.W., Warman R. Optic neuritis in children. J Pediatr Ophthalmol Strabismus. 2000;37:254–259. [PubMed] [Google Scholar]
- 14.Visudhiphan P., Chiemchanya S., Santadusit S. Optic neuritis in children: recurrence and subsequent development of multiple sclerosis. Pediatr Neurol. 1995;13:293–295. doi: 10.1016/0887-8994(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 15.Hayati A.A., Wan-Hitam W.H., Cheong M.T., Yunus R., Shatriah I. Optic neuritis in a child with biotinidase deficiency: case report and literature review. Clin Ophthalmol. 2012;6:389–395. doi: 10.2147/OPTH.S29048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puertas-Bordallo D., Martín Reyes C., Ruiz-Falcó Rojas M.L., Duat Rodríguez A., Valls Ferrán M.I. Optic neuropathy in biotinidase deficiency. Arch Soc Esp Oftalmol. 2004;79:393–396. doi: 10.4321/s0365-66912004000800007. [DOI] [PubMed] [Google Scholar]
- 17.Waldman A.T., Stull L.B., Galetta S.L., Balcer L.J., Liu G.T. Pediatric optic neuritis and risk of multiple sclerosis. J AAPOS. 2011;15:441–446. doi: 10.1016/j.jaapos.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 18.Bonhomme G.R., Waldman A.T., Balcer L.J. Pediatric optic neuritis: brain MRI abnormalities and risk of multiple sclerosis. Neurology. 2009;72:881–885. doi: 10.1212/01.wnl.0000344163.65326.48. [DOI] [PubMed] [Google Scholar]
- 19.Brady K.M., Brar A.S., Lee A.G. Optic neuritis in children: clinical features and visual outcome. J AAPOS. 1999;3:98–103. doi: 10.1016/s1091-8531(99)70078-9. [DOI] [PubMed] [Google Scholar]
- 20.Boomer J.A., Siatkowki R.M. Optic neuritis in adults and children. Semin Ophthalmol. 2003;18:174–180. doi: 10.1080/08820530390895172. [DOI] [PubMed] [Google Scholar]
- 21.Sun M.H., Wang H.S., Chen K.J. Clinical characteristics of optic neuritis in Taiwanese children. Eye. 2011;25:1457–1464. doi: 10.1038/eye.2011.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ness J.M., Chabas D., Sadovnick A.C., Pohl D., Banwell B., Weinstock-Guttman B. Clinical features of children and adolescents with multiple sclerosis. Neurology. 2007;68(suppl 2):S37–S45. doi: 10.1212/01.wnl.0000259447.77476.a9. [DOI] [PubMed] [Google Scholar]
- 23.Burman J., Raininko R., Fagius J. Bilateral and recurrent optic neuritis in multiple sclerosis. Acta Neurol Scand. 2011;123:207–210. doi: 10.1111/j.1600-0404.2010.01388.x. [DOI] [PubMed] [Google Scholar]
- 24.Beck R.W., Trobe J.D., Moke P.S. High and low-risk profiles for the development of multiple sclerosis within 10 years after optic neuritis: experience of the Optic Neuritis Treatment Trial. Arch Ophthalmol. 2003;121:944–949. doi: 10.1001/archopht.121.7.944. [DOI] [PubMed] [Google Scholar]
- 25.Luchinetti C.F., Kiers L., O’Duffy A. Risks factors for developing multiple sclerosis after childhood optic neuritis. Neurology. 1997;49:1413–1418. doi: 10.1212/wnl.49.5.1413. [DOI] [PubMed] [Google Scholar]
- 26.Chabas D., Ness J., Belman A. Younger children with MS have a distinct CSF inflammatory profile at disease onset. Neurology. 2010;74:399–405. doi: 10.1212/WNL.0b013e3181ce5db0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hwang J.M., Lee Y.J., Kim M.K. Optic neuritis in Asian children. J Pediatr Ophthalmol Strabismus. 2002;39:26–32. doi: 10.3928/0191-3913-20020101-07. [DOI] [PubMed] [Google Scholar]
- 28.Mizota A., Nimura M., Adachi-Usami E. Clinical characteristics of Japanese children with optic neuritis. Pediatr Neurol. 2004;31:42–45. doi: 10.1016/j.pediatrneurol.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 29.Kriss A., Francis D.A., Cuendet F. Recovery after optic neuritis in children. J Neurol Neurosurg Psychiatry. 1988;51:1253–1258. doi: 10.1136/jnnp.51.10.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kennedy C., Carter S. Relation of optic neuritis to multiple sclerosis in children. Pediatrics. 1961;28:377–387. [PubMed] [Google Scholar]
- 31.Lana-Peixoto M.A., Andrade G.C. The clinical profile of childhood optic neuritis. Arq Neuropsiquiatr. 2001;59:311–317. doi: 10.1590/s0004-282x2001000300001. [DOI] [PubMed] [Google Scholar]
- 32.Parkin P.J., Hierons R., McDonald W.I. Bilateral optic neuritis. A long-term follow-up. Brain. 1984;107:951–964. doi: 10.1093/brain/107.3.951. [DOI] [PubMed] [Google Scholar]
- 33.Wilejto M., Shroff M., Buncic J.R., Kennedt J., Goia C., Banwell B. The clinical features, MRI findings, and outcome of optic neuritis in children. Neurology. 2006;67:258–262. doi: 10.1212/01.wnl.0000224757.69746.fb. [DOI] [PubMed] [Google Scholar]
- 34.Heussinger N., Kontopantelis E., Rompel O., Paulides M., Trollmann R. Predicting multiple sclerosis following isolated optic neuritis in children. Eur J Neurol. 2013;20:1292–1296. doi: 10.1111/ene.12184. [DOI] [PubMed] [Google Scholar]
- 35.Balcer L.J. Optic neuritis. N Engl J Med. 2006;354:1273–1280. doi: 10.1056/NEJMcp053247. [DOI] [PubMed] [Google Scholar]
- 36.Trip S.A., Schlottmann P.G., Jones S.J. Retinal fiber layer axonal loss and visual dysfunction in optic neuritis. Ann Neurol. 2005;58:383–391. doi: 10.1002/ana.20575. [DOI] [PubMed] [Google Scholar]
- 37.Sahraian M.A., Radue E.W., Minagar A. Neuromyelitis óptica: clinical manifestations and neuroimaging features. Neurol Clin. 2013;31:139–152. doi: 10.1016/j.ncl.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 38.Dooley M.C., Foroozan R. Optic neuritis. J Ophth Vis Res. 2010;5:182–187. [PMC free article] [PubMed] [Google Scholar]
- 39.Bonhomme G.R., Mitchell E.B. Treatment of pediatric optic neuritis. Curr Treat Options Neurol. 2012;14:93–102. doi: 10.1007/s11940-011-0159-0. [DOI] [PubMed] [Google Scholar]
- 40.Michaelis I., Bender B., Beringer O., Melms A., Krägeloh-Mann I., Wolff M. Plasma exchange is effective in a 13 year-old girl with steroid-resistant bilateral optic neuritis. Neuropediatrics. 2013 doi: 10.1055/s-0033-1336018. March 6 [ahead of print] [DOI] [PubMed] [Google Scholar]
- 41.Pula J.H., McDonald C.J. Current options for the treatment of optic neuritis. Clin Ophthalmol. 2012;6:1211–1223. doi: 10.2147/OPTH.S28112. [DOI] [PMC free article] [PubMed] [Google Scholar]


