Abstract
Purpose
To determine the prevalence of refractive conditions in the adult population that visited primary care optometry clinics in Puerto Rico.
Methods
A retrospective cross-sectional study of patients examined at the Inter American University of Puerto Rico School of Optometry Eye Institute Clinics between 2004 and 2010. Subjects considered had best corrected visual acuity by standardized subjective refraction of 20/40 or better. The refractive errors were classified by the spherical equivalent (SE): sphere+½ cylinder. Myopia was classified as a SE>−0.50 D, hyperopia as a SE>+0.50 D, and emmetropia as a SE between −0.50 and +0.50, both included. Astigmatism equal or higher than 0.25 D in minus cylinder form was used. Patients with documented history of cataract extraction (pseudophakia or aphakia), amblyopia, refractive surgery or other corneal/ocular surgery were excluded from the study.
Results
A total of 784 randomly selected subjects older than 40 years of age were selected. The estimated prevalence (95%, confidence interval) among all subjects was hyperopia 51.5% (48.0–55.0), emmetropia 33.8% (30.5–37.2), myopia 14.7% (12.1–17.2) and astigmatism 69.6% (68.8–73.3). Hyperopia was more common in females than males although the difference was not statistically significant. The mean spherical equivalent values was hyperopic until 70 y/o and decreased slightly as the population ages.
Conclusion
Hyperopia is the most common refractive error and its prevalence and seems to increase among the aging population who visited the clinics. Further programs and studies must be developed to address the refractive errors needs of the adult Puerto Rican population.
Keywords: Refractive error, Aging, Hispanics, Latino, Geriatrics
Resumen
Objetivo
Determinar la prevalencia de las condiciones refractivas en la población adulta que acudió a centros de atención optométrica visual primaria en Puerto Rico.
Métodos
Estudio retrospectivo transversal de pacientes examinados en las clínicas oculares de la Escuela de Optometría de la Universidad Interamericana de Puerto Rico entre 2004 y 2010. Los pacientes examinados presentaban una agudeza visual corregida mediante refracción subjetiva estandarizada de 20/40 o más. Los errores refractivos se clasificaron mediante el equivalente esférico (EE): esfera+½ cilindro. La miopía se clasificó como EE>−0.50 D, la hipermetropía como EE>+0.50 D, y la emetropía como EE entre -0,50 y +0,50. El astigmatismo igual o superior a 0,25 D se consideró utilizando la notación de cilindro negativo. Se excluyó del estudio a los pacientes con antecedentes de cirugía de cataratas (pseudofaquia o afaquia), ambliopía, cirugía refractiva u otras cirugías corneales/oculares.
Resultados
Se seleccionó a un total de 784 pacientes mayores de 40 años, elegidos al azar. Las prevalencias estimadas (95%, intervalo de confianza) entre los sujetos examinados fueron: hipermetropía 51,5% (48,0-55,0), emetropía 33,8% (30,5-37,2), miopía 14,7% (12,1-17,2) y astigmatismo 69,6% (68,8-73,3). La hipermetropía fue más común en mujeres que en hombres, aunque la diferencia entre sexos no fue estadísticamente significativa. Los valores del equiva-lente esférico medio se decantaron hacia la hipermetropía hasta los 70 y/o,disminuyendo ligeramente a medida que la población envejecía.
Conclusión
La hipermetropía constituye el error refractivo más común, pareciendo incrementarse su prevalencia con la edad en la población que visitó la clínica. Deberán desarrollarse más programas y estudios para evaluar las necesidades de corrección visual de la población adulta de Puerto Rico.
Palabras clave: Error refractivo, Envejecimiento, Hispanos, Latino, Geriatría
Introduction
Uncorrected refractive errors are a common cause of visual impairment worldwide that can be prevented.1 Uncorrected refractive errors have been associated with loss of independence and reduced quality of life.2 Previous studies have reported that prevalence of hyperopia and visual impairment associated with uncorrected refractive errors increases with age.3–5 It has been shown that refractive errors such as hyperopia and astigmatism increase with age and are most frequent in Whites than Hispanics, Blacks or Asians.6 Wang et al. described the prevalence of refractive errors in a population of adult Americans. Adults from 43 to 84 years of age living in Beaver Dam, Wisconsin were evaluated in five-years intervals. They concluded that in the study group hyperopia was more frequent than myopia. They also found that the prevalence of hyperopia increased and myopia decreased with increased age.7
In 2009, Anton et al. determined the prevalence of refractive errors in adults older than 40 years of age in Segovia, Spain, using the spherical equivalent. They found the mean of hyperopia and astigmatism increased with age (P<0.01), hyperopia being more frequent (43.6%) than myopia (25.5%) in older population.8 Munoz et al. estimated the prevalence of blindness and uncorrected refractive errors in a population-based study composed of Mexicans-Americans older than 40 years of age. Visual loss was higher in their population than in whites, but comparable to African-Americans. Of those with visual loss 73% were related to uncorrected refractive errors.9
In Puerto Rico, the older population is the fastest growing segment, projected to represent 35.1% of the total population by 2025.10 The most common complaint, and reason to seek a visual evaluation in the aging adult population is due to refractive changes.3 Although refractive errors are thought to affect the aging Puerto Rican population, there is no study that describes the distribution of the different types of refractive conditions. Although not representative, the refractive errors of an isolated rural Puerto Rican migrant worker population within the Patillas community were studied in an attempt to estimate the prevalence of refractive errors and understand the impact of uncorrected refractive errors in this population.11 The purpose of our study is to determine the prevalence of refractive errors in the adult population that visited primary care optometry clinics in Puerto Rico, and provide data to be used for future references.
Methods
Design
This study is a retrospective cross-sectional study to estimate the prevalence of refractive errors in adults living in Puerto Rico who visited the Inter American University of Puerto Rico School of Optometry Eye Institute clinic system located in the north and south of the island between 2004 and 2010 for comprehensive eye exam (CPT codes 92004 and 92014). Refraction (CPT code 92015) information from those patients was selected retrospectively for the study: 784 record files were retrieved by systematic simple random selection to generate a sample representative of the study. Record file number 100 was the starting point and every ten files were retrieved thereafter. Eligibility criteria included adults, 40 years or older of either gender. Each patient obtained and completed a consent, and use of information authorization form during the registration process. Ethical approval was obtained from the Inter American University of Puerto Rico Institutional Review Board.
Refractive Error Criteria
The refractive assessment was based on subjective refraction with visual acuity assessment using a Snellen chart at 20 feet (6 m). Subjects considered had best corrected visual acuity by standardized subjective refraction of 20/40 or better at 20 feet (6 m) in both eyes. The refractive errors were classified by the spherical equivalent (SE): sphere+½ cylinder. Myopia was classified as a spherical equivalent>−0.50 D, hyperopia as a spherical equivalent>+0.50 D, and emmetropia as spherical equivalent between −0.50 and +0.50. Moderate myopia was defined as a spherical equivalent between −0.50 and −3.00 D, and moderate hyperopia as a spherical equivalent between +0.50 and +3.00. High myopia was defined as a spherical equivalent more than −5.00 D, and high hyperopia more than +5.00 D. Astigmatism in minus cylinder form was used. Astigmatism against the rule (ATR) was defined as axis 90°±30°, astigmatism with the rule (WTR) from 0° to 30° and 150° to 180° and oblique astigmatism (O) 31° to 59° and 121° to 149°. All refractive errors were obtained at the time of the visit using a phoropter with a range from −20.00 D to +20.00 D and cylinder range −0.25 to −6.00 D. Since the refractive error between right and left eye was similar (r=0.87; P>0.05) the right eye was selected for analysis. Patients with documented history of cataract extraction (pseudophakia or aphakia), refractive surgery or other corneal/ocular surgery, amblyopia or any ocular disease were excluded from the study. Descriptive statistics was used for data analysis. A significance level of P<0.05 was used with a 95% confidence. The statistical analysis program SPSS V20 (SPSS Inc., Chicago, IL) was used to perform the calculations.
Results
Sample distribution by age and sex is shown in Table 1. Distribution of refractive errors among total adult population revealed that 14.7% (95% CI, 12.1–17.2) had myopia, 33.8% (95% CI, 30.5–37.2) were emmetropic and 51.5% (95% CI, 48.0–55.0) had hyperopia. The prevalence of astigmatism among all adults was 67.6% (95% CI, 66.8–71.3). Fig. 1 shows the distribution of refractive errors (myopia, hyperopia and astigmatism) by age group. With increasing age, there is an increase in prevalence of hyperopia and astigmatism. The distribution of the orientation of astigmatism by age is shown in Fig. 2. With increasing age, ATR (against the rule) astigmatism was more common.
Table 1.
Demographic Characteristics of the Sample.
| n (%) | 95% CI | |
|---|---|---|
| Age | ||
| 40–49 | 243 (32.4) | 29.1–35.5 |
| 50–59 | 280 (37.3) | 34.1–40.9 |
| 60–69 | 166 (2.1) | 19.3–25.5 |
| 70–79 | 54 (7.2) | 5.5–9.2 |
| 80–89 | 7 (0.9) | 0.3–1.7 |
| Gender | ||
| Female | 520 (69.3) | 65.9–72.5 |
| Male | 230 (30.7) | 27.5–34.1 |
CI=confidence interval.
Figure 1.
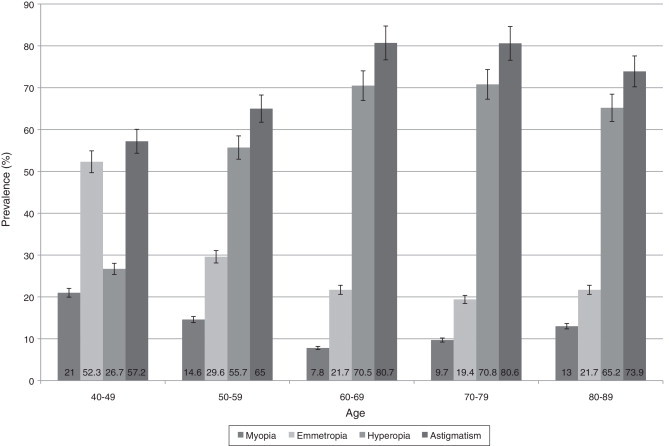
Prevalence of refractive error by age groups. Frequency of hyperopia and astigmatism increases with aging with a small decrease toward 80 y/o. Myopia decreases during aging with a small increase at 80 y/o (Chi-square; p < 005)
Figure 2.
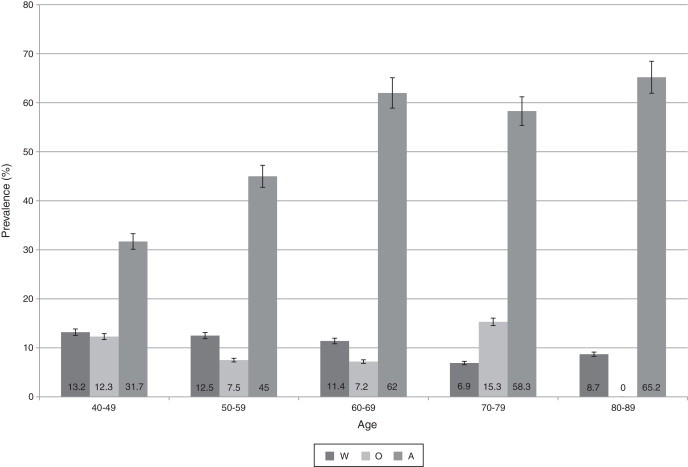
Distribution of the orientation of astigmatism among age group. The frequency of against the rule astigmatism increases with age.(Chi square; p < 0.005) W: with-the-rule; O: oblique; A: against-the-rule
The prevalence of myopia between genders is more common in males (16.8%) than females (13.7%) (p = 0.256). Emmetropia is more frequent in males (38.1%) and females (31.9%) (p = 0.030). Hypepropia is more frequent in females (54.4%) than males (45.1%) (p = 0.052). Average in diopters at different ages of the population studied is shown in Table 2.
Table 2.
Distribution of Refractive Errors by Age.
| Refractive Error (D) | Age Range |
||||
|---|---|---|---|---|---|
| 40–49 | 50–59 | 60–69 | 70–79 | 80–89 | |
| <−5.25 | 2.10% | 1.80% | 1.20% | 0% | 0% |
| −5.00 to −3.25 | 4.10% | 4.30% | 2.40% | 2.80% | 9% |
| −3.00 to −0.75 | 14.80% | 8.60% | 4.20% | 6.90% | 4% |
| −0.50 to 0.50 | 52.30% | 29.60% | 21.70% | 19.40% | 22% |
| 0.75–3.00 | 25.10% | 52.10% | 57.80% | 61.10% | 57% |
| 3.25–5.00 | 0.80% | 3.20% | 12.00% | 9.70% | 9% |
| >5.25 | 0.80% | 0.40% | 0.60% | 0% | 0% |
| Mean RE (SD) | 0.127 (1.86) | 0.737 (2.38) | 1.76 (1.77) | 1.72 (1.86) | 1.55 (1.93) |
| Mean cylinder (IQR) | 0.5 (0.50) | 0.5 (0.50) | 0.75 (0.75) | 0.75 (0.75) | 0.75 (0.50) |
D=diopters; SD=standard deviation; IQR=interquartile range.
Discussion
This study is a clinical retrospective study on a randomly selected subset of Puerto-Rican Adults. The study results provided an understanding of the prevalence of refractive errors in a Puerto Rican clinical adult population. Previously a refractive conditions study of the Puerto Rican population was performed in the rural town of Patillas, and took into account the general population of an isolated community.6 No previous study has been performed to determine the distribution of refractive conditions among people 40 years and older in Puerto Rico.
The changes in refractive errors in adults have been described in numerous studies.1–9,11–13,15,16 It is important to consider that prevalence of refractive errors between different ethnic groups and geographical regions are difficult to compare as a result of differences between criteria and methodological process. This study defined myopia as a spherical equivalent larger than −0.50 D and hyperopia larger than +0.50 D similar to other studies.2,4,7,8,12,15,16 Other studies used a cut off of −1.00 D for myopia and others defined hyperopia as refraction larger than +1.00 D or +3.00 D.6,12,18
Our study shows an increased prevalence of hyperopia with a decreased prevalence of myopia with increased age. Our results are similar to other studies performed in general populations in the United States, Western Europe, Australia and Spain.6–8,15 According to the findings throughout the population studied the most common refractive condition is hyperopia (51.5%) followed by emmetropia (33.8%), then myopia (14.7%). In this study, the spherical equivalent values change toward hyperopia with aging. To compare these results with other studies it is important to take into consideration that the age of the population varies among studies affecting the comparison with our results. Nevertheless, hyperopia has been reported more prevalent in Singapore, 35.9%, Australia, 57.0%, and Spain, 53.5%. Myopia has been found to be more prevalent in the United States, 58.1%, Western European population, 26.6%, and Mexican-Americans, 48.0%, and higher than the prevalence found in our study. Emmetropia is more common at the 40 y/o range with an increase in moderate hyperopia up to 70 y/o with a slight decrease toward the 80 years or more range. Our emmetropia findings are similar to the Chinese, 29.1%, and Australian, 28.0%, when defined as refractive errors between −0.50 D and +0.50 D.
According to the findings throughout the clinical population studied, the prevalence of astigmatism increases with age. Our findings correlate to those of other studies. A decrease in with-the-rule astigmatism with an increase in against-the-rule astigmatism is observed as the population aged.2,6–8,12,15,16 This finding can also be explained as a result of crystalline lens changes during the aging process mentioned elsewhere.3,13,14
The mean values and standard deviation of refractive conditions differ between age groups: 40 to 49 y/o +0.127±1.86 D, 50 to 59 years +0.737±2.38 D, 60 to 69 years +1.76±1.77 D, 70 to 79 years +1.72±1.86 D and from 80 to 89 y/o +1.55±1.93 D (p = 0.003) (Fig. 3). The increase in hyperopia has been attributed to accommodation loss followed by an increase in manifest hyperopia.1,14 Previous studies have identified the hyperopic shift as a result of reduction of the refractive index and gradient index of the lens with concurrent steepening of the lens radii.5,14 The myopic shift in older persons can be attributed to lens opacities.4,13 Mean values obtained follow the same pattern but are slightly higher than other studies. Direct comparison to other studies is not possible due to different definitions of refractive conditions, and age ranges among studies.
Figure 3.
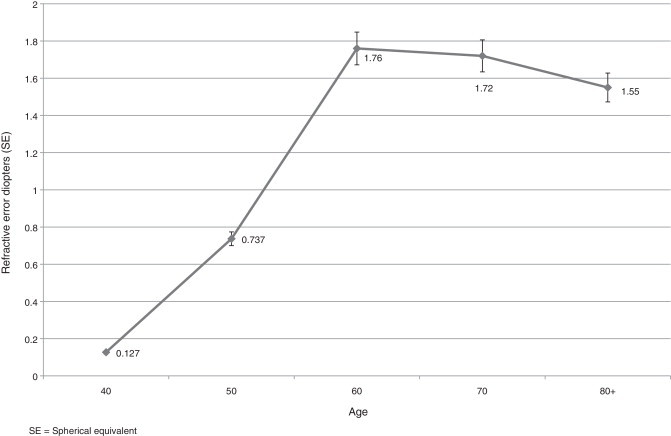
Mean distribution of right eye spherical equivalent in the adult population.
Frequency of refractive conditions according to gender reveals that in females hyperopia and astigmatism are most frequent (54.0% and 39.1% respectively) followed by emmetropia (32.5%) and myopia the least common (13.5%). Males revealed a similar trend: hyperopia (45.2%) as most common, then emmetropia (38.3%), astigmatism (20.1%) and last myopia (16.5%) (Fig. 4). This study found higher prevalence of hyperopia in females than males although statistical significance was not reached. These results are similar to other studies in Spain, Australia and the United States where women revealed more frequent hyperopia than males with the exception of Singapore where women had more myopia. The authors attribute this increased frequency of myopia to the common finding of myopia in the Asian population.16 Myopia was found more frequently in males in most of the studies.6–8 Other studies reported no statistically significant differences between genders.4,7
Figure 4.
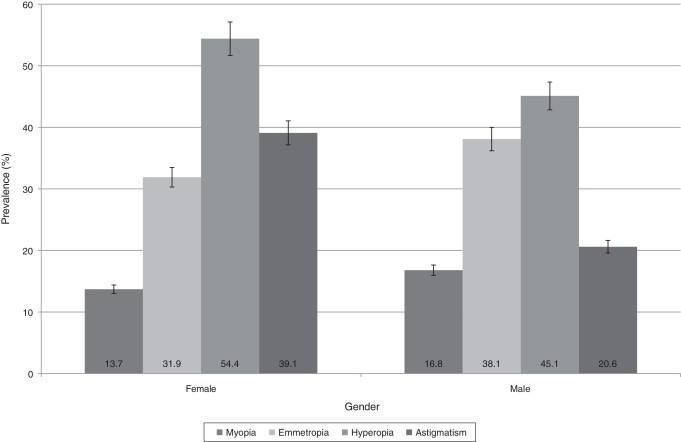
Prevalence of refractive error by gender. Hyperopia and astigmatism are more frequent in females than male (P<0.05)
The results reveal that the frequency of the refractive errors among Puerto Rican adults from a clinical population increases toward hyperopia as the population ages. Hyperopia increases from 26.7% at 40 years of age to 65.2% in persons older than 80 years of age. Other studies have demonstrated a decrease in the prevalence of myopia and an increase in the prevalence of hyperopia and astigmatism with increased age.3–5,11,13–17 Our results concur with those studies even though our study is not population-based. It has been postulated that a decrease in axial length, changes in the cilliary body and a decreased index of refraction at the lens cortex contribute to the shift toward hyperopia.
Conclusion
Hyperopia is the most common refractive error among the aging population visiting the Inter American University of Puerto Rico School of Optometry Eye Institute Clinics. The results are similar to previous studies but this only provides an estimate because it is not a population-based study. Further studies are needed to address and describe the most common preventable cause of visual impairment in the Puerto Rican aging population.
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- 1.Tarcy-Hornoch K., Ying-Lai M., Varma R, and Los Angeles Latino Eye Study Group Myopic refractive error in adult Latinos: Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2006;47:1845–1852. doi: 10.1167/iovs.05-1153. [DOI] [PubMed] [Google Scholar]
- 2.Uribe J., Swenor B., Muñoz B., West S. Uncorrected refractive error in Latino population: Proyecto Ver. Ophthalmology. 2011;118:805–811. doi: 10.1016/j.ophtha.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Attebo K., Ivers R., Mitchell P. Refractive errors in older population. Ophthalmology. 1999;106:1066–1072. doi: 10.1016/S0161-6420(99)90251-8. [DOI] [PubMed] [Google Scholar]
- 4.Katz J., Tielsch J., Sommer A. Prevalence and risk factors for refractive errors in an adult inner city population. Invest Ophthalmol Vis Sci. 1997;38:334–340. [PubMed] [Google Scholar]
- 5.Lee K., Klein B., Klein R., Wong T. Changes in refraction over 10 years in an adult population: the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 2002;43:2566–2571. [PubMed] [Google Scholar]
- 6.The Eye Diseases Prevalence Research Group: the prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch Ophthalmol. 2004;122:495–505. doi: 10.1001/archopht.122.4.495. [DOI] [PubMed] [Google Scholar]
- 7.Wang Q., Klein B., Klein R., Moss S. Refractive status in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1944;35:4344–4347. [PubMed] [Google Scholar]
- 8.Anton A., Andrada M., Mayo A., Portela J., Merayo J. Epidemiology of refractive errors in an adult European population: the Segovia Study. Ophthal Epidemiol. 2009;16:231–237. doi: 10.3109/09286580903000476. [DOI] [PubMed] [Google Scholar]
- 9.Munoz B., West S., Rodriguez J., Sanchez R., Broman A., Snyder R., Klein R. Blindness, visual impairment and the problem of uncorrected refractive error in a Mexican-American population: Proyecto Ver. Invest Ophthalmol Vis Sci. 2002;43:608–614. [PubMed] [Google Scholar]
- 10.Oficina del Censo [Internet] 2012. San Juan (PR): Junta de Planificación [2010]. Proyección de población por edad y sexo en Puerto Rico años 2000–2025. p. 1. Available from: http://www.censo.gobierno.pr [cited 17.09.12] [Google Scholar]
- 11.Gordon A. Refractive error in a Puerto Rican rural population. J Am Optom Assoc. 1990;61:870–874. [PubMed] [Google Scholar]
- 12.Varma R., Wang M., Ying-Lai M., Donofrio J., Azen S., and The Los Angeles Latino Eye Study The prevalence and risk indicators of uncorrected refractive error and unmet refractive need in Latinos: Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2008;49:5264–5273. doi: 10.1167/iovs.08-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shufelt C., Fraser-Bell S., Ying-Lai M., Torres M., Varma R., and The Los Angeles Latino Eye Study Group Refractive error, ocular biometry, and lens opalescence in an adult population: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2005;46:4450–4460. doi: 10.1167/iovs.05-0435. [DOI] [PubMed] [Google Scholar]
- 14.Ooi C., Grosvenor T. Mechanisms of emmetropization in the aging eye. Optom Vis Sci. 1995;72:60–66. doi: 10.1097/00006324-199502000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Guzowski M., Wang J.J., Rochtchina E., Rose K.A., Mitchell P. Five-year changes in an older population: the Blue Mountains Eye Study. Ophthalmology. 2003;110:1364–1370. doi: 10.1016/S0161-6420(03)00465-2. [DOI] [PubMed] [Google Scholar]
- 16.Wong T.Y., Foster P.J., Hee J., Ng T.P., Tielsch J.M., Chew S.J., Johnson G.J., Seah S.K. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000;41:2486–2494. [PubMed] [Google Scholar]
- 17.Sandhu R.K., Munoz B.E., Swenor B.K., West S.K. Refractive error and visual function difficulty in a Latino Population. Ophthalmology. 2012;119:1731–1736. doi: 10.1016/j.ophtha.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krantz E.M., Cruickshanks K.J., Klein B.E., Klein R., Huang G.H., Nieto F.J. Measuring refraction in adults in epidemiological studies. Arch Ophthalmol. 2010;128:88–92. doi: 10.1001/archophthalmol.2009.349. [DOI] [PMC free article] [PubMed] [Google Scholar]


