Abstract
Background
Medicare Part D was expected to have differential impacts on patient drug expenditures and utilization based on beneficiaries’ levels of pre-Part D patient drug spending, but it is unknown whether these projections have borne out
Objectives
We sought to evaluate whether and how the policy effect of Medicare Part D on drug expenditures and utilization was modified by levels of pre-Part D drug spending.
Methods
A quasi-experimental, pretest-posttest, nonequivalent control group design was used. Data were obtained from a regional supermarket chain for all prescriptions dispensed between January 1, 2005 and December 31, 2007 (n =1,230,612) to patients age 60 and older as of January 1, 2005 (n = 51,305) to construct 12-month pre-Part D and post-Part D periods. The treatment group was defined as individuals who were eligible via age, for Part D coverage on January 1, 2006 (ages 65+). The control group included individuals aged 60 through 62 on January 1, 2006. Annual medication utilization was measured as the total number of pill-days acquired. Annual drug expenditures were measured as total expenditures, patient out-of-pocket expenditures, and the proportion of total expenditures paid out of pocket by the patient.
Results
Part D resulted in significantly greater reductions in absolute and relative out-of-pocket spending for individuals in the highest pre-Part D drug spending group relative to the moderate and low pre-Part D drug spending groups.
Conclusions
Our findings suggest that, as expected, Part D facilitated access to medications for patients who previously experienced the greatest costs without adversely increasing use and costs among those with the lowest prior cost.
Keywords: Medicare Part D, Utilization, Out-of-pocket Spending, Access
INTRODUCTION
In the early part of this century, high need for medications coupled with limited access to prescription drug insurance and rising medication costs presented considerable challenges for older adults in the United States.1 Estimates from 2002 showed that nearly half of all Medicare beneficiaries lacked drug coverage for at least part of the year,2 and that beneficiaries’ average annual out-of-pocket drug spending had risen from $644 to $996 from 2000–2003.1 Under the Medicare Modernization Act of 2003, the Part D prescription drug benefit became available to all Medicare beneficiaries starting January 1st 2006. The overall goal of this largest expansion in the Medicare program since its inception was to improve coverage for prescription drugs among the Medicare population, and in doing so, ease their financial burden associated with obtaining prescription drugs, and increase access to medications.3
There is evidence that implementing the Part D benefit has reached some level of success in attaining these goals. In the first two years after implementing Medicare Part D, the proportion of Medicare eligible individuals with “creditable” drug coverage (i.e., coverage at least as generous as the standard Part D benefit) increased to approximately 90%.4, 5 Recent reports also have shown that, overall, implementing Part D yielded modest but significant increases in medication utilization and decreases in Medicare beneficiaries’ out-of-pocket drug spending.5–9
These early studies show promising results, but provide little insight regarding the impact of Medicare Part D for individuals with varying levels of prior financial burden for drugs. One report prior to implementation projected that although the distribution of pre-Part D out-of-pocket drug spending among Medicare eligible individuals was widely dispersed, Medicare Part D was expected to lower overall out-of-pocket drug costs primarily by decreasing the number of beneficiaries with the highest out-of-pocket costs.3 However, it is unknown whether these projections have borne out; that is, whether Part D decreased out-of-pocket drug spending among individuals with high pre-enrollment out-of-pocket drug spending, and thus, improved access to medications among a subgroup of beneficiaries who needed it most.
Additionally, all Medicare beneficiaries were offered the opportunity – and encouraged via financial incentives – to enroll in the Part D benefit, including individuals with low out-of-pocket spending burdens.10 These patients may have had low out-of-pocket costs due to low need for medication, or conversely, because they were unable to afford needed prescription medications (i.e., unmet need). Part D relies on the inclusion of individuals with low need for medication (and their contribution of premium payments) to offset costs to the program incurred by those with high medication needs who will utilize more. Part D solvency at least in part, therefore, relies on the assumption that providing a prescription benefit to all beneficiaries does not have the unintended consequence of increasing utilization among those with low medication needs. Understanding the extent to which Part D affected utilization among beneficiaries with prior low medication spending burdens would provide some insight into the ability of Medicare Part D to remain solvent.
We sought to assess whether Part D had the intended effects of helping individuals with high financial burden without increasing use among individuals with low financial burden by examining the Medicare Part D policy effect for subpopulations of Part D eligible older adults based on their level of out-of-pocket drug spending prior to the policy taking effect. Specifically, we sought to 1) evaluate whether the policy effect of Medicare Part D on drug utilization and cost differed by levels of pre-Part D out-of-pocket drug spending, and 2) characterize the Part D policy effect within each level of pre-Part D out-of-pocket spending. For both aims we examined how the outcomes changed from pre-Part D to post-Part D for Medicare eligible individuals compared to a control group of non-eligible individuals.
METHODS
Approach to Studying the Medicare Part D Policy Effect
We adopt a broad, population level approach to examine the Medicare Part D policy effect. According to our approach, we are interested in examining whether the initial availability of Medicare Part D in January of 2006 changed relevant drug expenditure and drug utilization outcomes relative to the year immediately preceding the availability of Medicare Part D for a defined population of seniors eligible for Medicare Part D and a defined control population of persons presumably not eligible for Medicare Part D. To statistically test the Medicare Part D policy effect, we use a difference-in-difference (DD) approach. This is a powerful approach to estimate policy effects because it accounts for differences in outcomes between study groups (a group exposed to the policy and a group not exposed (control)) as well as changes in outcomes within groups across time (a period before the policy was in effect and a period after the policy was in effect). Additionally, the DD approach controls for all differences across the study groups that are invariant across time.11 This feature of the DD approach makes it possible to control for individual level characteristics that may confound the Medicare Part D policy effect, even without measuring them. Such factors include stable clinical factors, disease severity and preferences to use medical care that remain the same across the short study period. The DD approach was used in a previous study of the policy effect of Medicare Part D.6
Data Source
Data were obtained from a regional supermarket chain with 22 pharmacies located in the southeastern United States for all prescriptions dispensed between January 1, 2005 and December 31, 2007 (n =1,230,612) to all patients age 60 and older as of January 1, 2005 (n = 51,305). Each record in the database contained information about the patient (a unique, non-identifiable ID number, date of birth, gender, and ZIP code of residence), and the prescription (drug name and strength, National Drug Code, fill date, days supply, quantity dispensed, total payment/price, patient payment, and insurer payment). The study was approved by the University’s Institutional Review Board (IRB).
Design & Sample
We used a quasi-experimental, pretest-posttest, nonequivalent control group design. The pre-intervention period was defined as the 12 months prior to Part D beginning (January 1, 2005 through December 31, 2005). The post-intervention period was the 12 months after Part D began (January 1, 2006 through December 31, 2006). The treatment group included individuals who were eligible, according to age, for Part D coverage on January 1, 2006 (ages 65+). The control group was constructed to include individuals who were ineligible for Medicare coverage during the entire study period, and was comprised of individuals aged 60 through 62 on January 1, 2006. Although it is possible that a small number of individuals in this comparison group were eligible for Medicare coverage due to disability, they were assumed to be ineligible.12 To be included in the analysis, patients were required to have at least one fill in the pre-intervention period (2005) as well as 2006 and 2007. Requiring a fill in 2007 helped ensure that all patients in our sample remained users of the supermarket pharmacy in 2006.
Outcomes
Utilization
Each person’s annual medication utilization was measured as the total number of pill-days, and was calculated by summing the days supply of all prescriptions filled by a person in a year. Therefore, pill-days represent the total number of days supply of medication, across all medications, that a patient acquired in a year. For example, a person who took two medications and acquired exactly enough pills to use these medications as prescribed everyday for a year would have a pill-days value of 730 (2 medications X 365 days supply per medication = 730 pill-days).
Expenditures
We calculated three variables to summarize annual medication expenditures. Total annual medication spending was calculated by summing the total payment from all sources (patient and insurer) across all prescriptions filled in each year for each person. Total patient out-of-pocket drug spending was calculated by summing the patient payment amount across all prescriptions filled in each year. We determined the annual average percent of total payment paid out-of-pocket by each patient, by calculating the ratio of patient out-of-pocket payment to total payment for each prescription fill, and determining the mean of these ratios.
Covariates
Pre-Part D out-of-pocket drug spending
To examine whether effects of Part D varied based on individuals’ levels of out-of-pocket drug spending prior to Part D, we constructed a categorical variable to classify patients based on their total amount of out-of-pocket drug spending in 2005. Cut points were established to partition individuals in the treatment and control groups into approximately equal sized groups (thirds) representing “lowest” (up to $66), “moderate” ($66.01 to $469.61), and “highest” (more than $469.61) out-of-pocket.
Patient Characteristics
Patient age at the beginning of our study period (January 1, 2005) and gender were abstracted from prescription fill records for each patient, for use as control variables in our analyses.
Data Analysis
In terms of the expenditure and utilization variables in 2005 and 2006, we examined means and standard deviations for individuals eligible for Part D and the control group, along with mean age (as of January 1, 2005) and gender distribution in each pre-Part D out-of-pocket drug spending category. Differences in means within each spending category between study groups within each study year were tested using t-tests. The association of gender and study group within each year was determined using chi-squared tests.
To examine whether the effect of Part D differed based on pre-Part D out-of-pocket drug spending we used a difference-in-difference-in-difference (DDD) modeling approach that controlled for observed changes over time in medication use and expenditures in the control group. We estimated the following linear regression model:
The coefficients B10 and B11 show whether the policy effect of Part D is different between the high and moderate levels of pre-Part D spending and the moderate and low levels of pre-Part D spending, respectively.
To better characterize the effect of Medicare Part D availability on changes in utilization and expenditures from 2005 to 2006 within each level of pre-Part D out-of-pocket drug spending, we estimated separate difference-in-difference (DD) regression models for each of the four outcomes described above using subsamples of the study population based on levels of pre-Part D spending. We used the regression results to estimate adjusted means for each outcome in order to compare the pre-post differences between Part D eligibles and the control group within each pre-Part D spending category.
Because utilization and expenditure data are often non-normal and right-skewed, various data transformations (e.g., logarithmic) are often employed to mitigate any resultant biases to variance estimates.13 Although a logarithmic transformation has attractive statistical properties, there are also conceptual considerations about whether the relationships being examined are additive or multiplicative. For older adults who already tend to have high medication use and expenditures, we believe it unlikely for any policy to have a multiplicative impact on medication use and expenditures. We deemed an additive model to be a more realistic representation of the possible Part D impact in older adults’ utilization and, therefore, made no transformation to outcome variables in the study. To account for possible violations of distributional assumptions, we estimated model standard errors using a bootstrapping approach. Generalized least squares regression was used to estimate all models which adjusts standard errors for clustering within individuals. All analyses were conducted using STATA version 10.0 (STATA Corp, College Station, TX).
RESULTS
Sample Characteristics
In order to explore the generalizability of findings from the study sample, we used data from the 2005 Behavioral Risk Factor Surveillance System (BRFSS) to compare the characteristics of residents from our sample’s geographic area (i.e., the counties in which our sample resided) to characteristics of community-dwelling older (age 65+) adults residing elsewhere in the United States. Individuals in counties represented by our sample were less likely to have less than a high school education (7% vs. 15%, p<.05), were less likely to have a household income under $20,000 (14% vs. 26%, p<.01), had a higher proportion of African-American residents (14% vs. 7%, p<.01), and were less likely to report a delay in seeing a doctor because of cost (2% vs. 6%, p<.05). There were no statistically significant differences with regard to age, sex, insurance coverage, or any of the measures of health status.
Table 1 shows baseline sample characteristics for the Part D eligible and control groups overall and by pre-Part D out-of-pocket spending level. The overall mean age of patients in our sample was 72.8 years (STD=7.6) and 62.0% were female. There were 11,133 and 1,625 individuals identified in the Part D eligible and the control group, respectively. Individuals who were Part D eligible were significantly older (74.5 years vs. 61.0, t = −84.5, p<0.0001) and more likely to be female (62.3% vs. 59.5%, χ2(1 df)= 4.68, p<0.05) than individuals in the control group.
Table 1.
Summary of Outcome Variables for Individuals Eligible for Part D and the Control Group by Level of Pre-Part D Out-of-Pocket Drug Spending
| Overall | Lowest Level of Pre-Part D Spending | Moderate Level of Pre-Part D Spending | Highest Level of Pre-Part D Spending | |
|---|---|---|---|---|
|
| ||||
| Part D Eligible | n = 11,133 | N = 3,681 | n = 3,778 | n = 3,674 |
|
| ||||
| Total Drug Spending | $1,208 | $123 | $1,018 | $2,490* |
| ($6,276) | ($495) | ($1,452) | ($1,987) | |
|
| ||||
| Patient Out-of-pocket Drug Spending | $530* | $13* | $218 | $1,369* |
| ($852) | ($17.9) | ($118) | ($1,054) | |
|
| ||||
| % Patient Paid Out-of-pocket | 46 | 22* | 50* | 66* |
| (37) | (34) | (33) | (30) | |
|
| ||||
| Pill-days | 680* | 80 | 555* | 1,410 |
| (817) | (322) | (577) | (817) | |
|
| ||||
| Age | 74.5* | 74.1* | 74.3* | 75.2* |
| (6.5) | (6.1) | (6.5) | (6.8) | |
|
| ||||
| % Female | 62.3# | 58.8 | 61.8 | 66.2# |
|
| ||||
|
| ||||
| Control | n = 1,652 | n = 415 | n = 763 | n = 474 |
|
| ||||
| Total Drug Spending | $1,142 | $112 | $691 | $2,769* |
| ($1,559) | ($333) | ($746) | ($1,893) | |
|
| ||||
| Patient Out-of-pocket Drug Spending | $409* | $29* | $220 | $1,045* |
| ($560) | ($17) | ($116) | ($693) | |
|
| ||||
| % Patient Paid Out-of-pocket | 49 | 58* | 48* | 45* |
| (28) | (34) | (26) | (21) | |
|
| ||||
| Pill-days | 620* | 81 | 451* | 1,366 |
| (707) | (222) | (400) | (765) | |
|
| ||||
| Age | 61.0* | 61.0* | 61.0* | 61.0* |
| (.58) | (.58) | (.58) | (.59) | |
|
| ||||
| % Female | 59.5# | 60.0 | 58.7 | 60.3# |
p < 0.05, difference in mean between seniors eligible for Part D and control group overall and within pre-Part D spending level, t-test.
p < 0.05, test of association between seniors eligible for Part D and control group overall and within pre-Part D spending level, chi-squared test.
Note: Numbers in parentheses are standard deviations. Spending categories (Lowest, Moderate, and Highest) were created by determining cut points representing thirds of the distribution of the pre-Part D patient out-of-pocket drug spending variable for seniors eligible for Part D.
Several significant differences between Part D eligibles and the control group within each level of pre-Part D spending were also detected. Among individuals with moderate and highest levels of pre-Part D spending, generally the differences reflect the fact that Part D eligibles used more medications, paid more out-of-pocket for medications, and paid a larger proportion of medication costs out-of-pocket relative to the control group.
Difference in Part D Policy Effect Between Levels of Pre-Part D Out-of-Pocket Drug Spending
The results of the DDD models showed statistically significant differences in the overall policy effect of Part D for most of the outcomes across the three levels of pre-Part D out-of-pocket drug spending (Table 2). The change in all four outcomes for individuals in the highest pre-Part D out-of-pocket drug spending group was significantly different relative to individuals in the lowest pre-Part D out-of-pocket drug spending group. Part D resulted in significantly greater reductions in absolute ($234.2) and relative (6.2 percentage points) out-of-pocket spending for individuals in the highest pre-Part D out-of-pocket drug spending group relative to individuals in the moderate pre-Part D out-of-pocket drug spending group. In terms of differences between the moderate and lowest pre-Part D out-of-pocket drug spending levels, Part D resulted in significantly greater increases in pill-days of medication (51.5 pill days) and significantly greater reductions in the proportion of drug spending paid out-of-pocket (13.9 percentage points).
Table 2.
Results for Part D Policy Effect Across Levels of Pre-Part D Out-of-Pocket Drug Spending (DDD Regression Models)
| Highest vs. Moderate | Highest vs. Lowest | Moderate vs. Lowest | ||
|---|---|---|---|---|
|
| ||||
| Total Spending | 225.2 (−36.4 – 712.6) | 152.7* (20.0 – 300.4) | −72.5 (−568.6 – 141.5) | |
|
| ||||
| Patient Out-of-Pocket Drug | −234.2* | −227.8* | 6.4 | |
| Spending | (−286.3 – −180.1) | (−286.9 – −172.5) | (−15.7 – 28.2) | |
|
| ||||
| % Spending Out-of-Pocket | −6.2* | −20.2* | −13.9* | |
| (−8.7 – −3.9) | (−24.2 – −16.5) | (−17.9 – −10.1) | ||
|
| ||||
| Pill-days | 16.8 | 68.3* | 51.5* | |
| (−30.5 – 64.4) | (17.6 – 114.8) | (15.5 – 84.6) | ||
p < 0.05.
Note: The numbers are coefficients (95% Bias Corrected Confidence Interval). The coefficients represent the difference in the change in the level of a dependent variable in the post-period relative to the pre-period for Part D eligibles relative to the control group between each level of pre-Part D out-of-pocket drug spending. The value of −234.2 in column two for Patient Out-of-Pocket Drug Spending suggests that the policy effect of Part D resulted in a significantly greater reduction in out-of-pocket drug spending of $234 after availability of Part D for eligible seniors with the highest level of pre-part D spending compared to eligible seniors with a moderate level of pre-Part D spending relative to the control group.
Difference in Part D Policy Within Levels of Pre-Part D Out-of-Pocket Drug Spending
There were statistically significant differences in the total policy effect of Part D within the three out-of-pocket drug spending groups between 2005 and 2006 (Table 3). Among individuals with the highest pre-Part D out-of-pocket drug spending, out-of-pocket spending (both absolute and proportional) decreased significantly more for Part D eligibles relative to the control group, and pill-days of medication increased significantly more for Part D eligibles relative to the control group. The mean adjusted proportion of drug spending paid out-of-pocket decreased 17 percentage points for Part D eligibles compared to 1.6 percentage points for the control group (Figure 1). Prescription utilization increased by 43 pill-days for Part D eligibles compared to a decrease of 13 pill-days for the control group (Figure 2). Mean adjusted out-of-pocket drug spending decreased a total of $288 for Part D eligibles compared to $46 for the control group.
Table 3.
Overall Policy Effect of Part D on Five Outcomes by Pre-Part D Out-of-pocket Drug Spending Levels: 2005–2006
| Highest | Moderate | Lowest | |
|---|---|---|---|
|
| |||
| Total Spending | 119.6 | −105.6 | −33.1 |
| (−10.9 – 273.7) | (−696.7 – 80.5) | (−89.9 – 13.4) | |
|
| |||
| Patient Out-of-Pocket Drug Spending | −241.0* | −6.8 | −13.2 |
| (−286.4 – −180.6) | (−19.7 – 21.1) | (−27.1 – −4.5) | |
|
| |||
| % Spending Out-of-Pocket | −15.3* | −9.1* | 4.9* |
| (−17.1 – −13.3) | (−11.8 – −7.1) | (1.4 – 8.6) | |
|
| |||
| Pill-days | 56.1* | 39.4* | −12.2 |
| (2.5 – 127.6) | (.07 – 68.5) | (−38.9 – 14.2) | |
p < 0.05.
Note: The numbers are coefficients (95% Bias Corrected Confidence Interval). The models controlled for patient age, gender, a group dummy variable, and a study period dummy variable.
Figure 1.
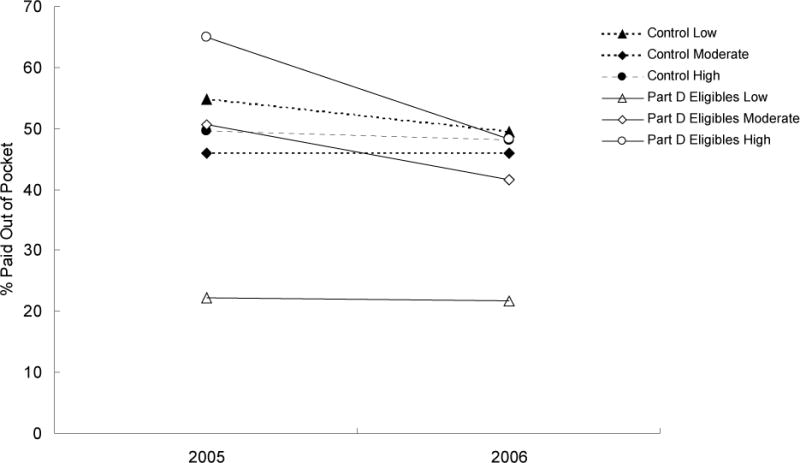
Change in Adjusted Percentage of Prescription Drug Costs Paid Out of Pocket by Medicare Part D Eligibility in 2006 (Part D Eligible versus Control) and 2005 Prescription Spending Levels (Low, Moderate, High).
Note: Dashed lines indicate Control group trends adjusted for age and gender, solid lines indicate Part D Eligible group trends adjusted for age and gender.
Figure 2.
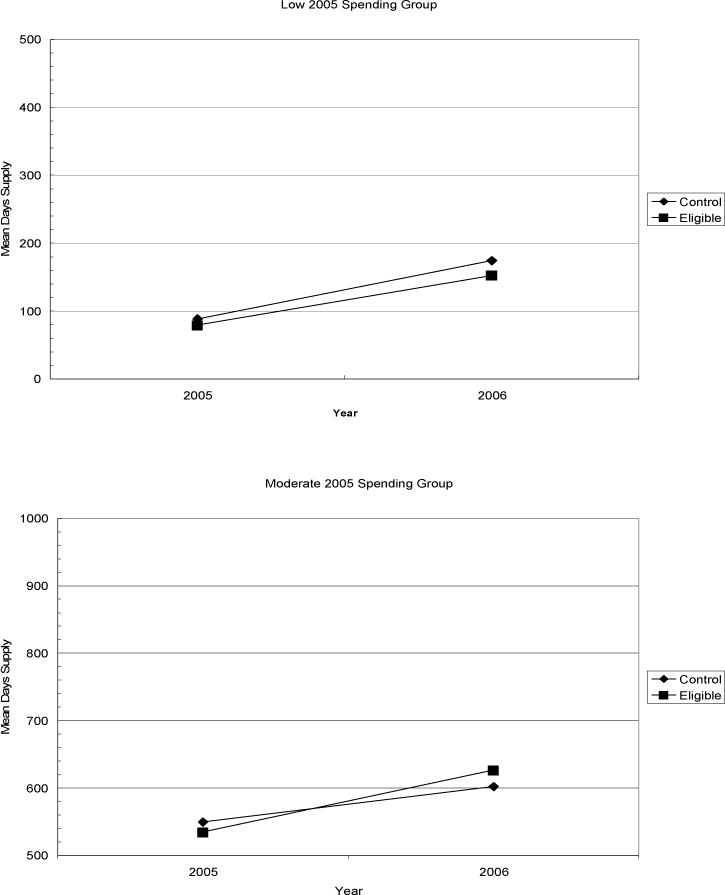
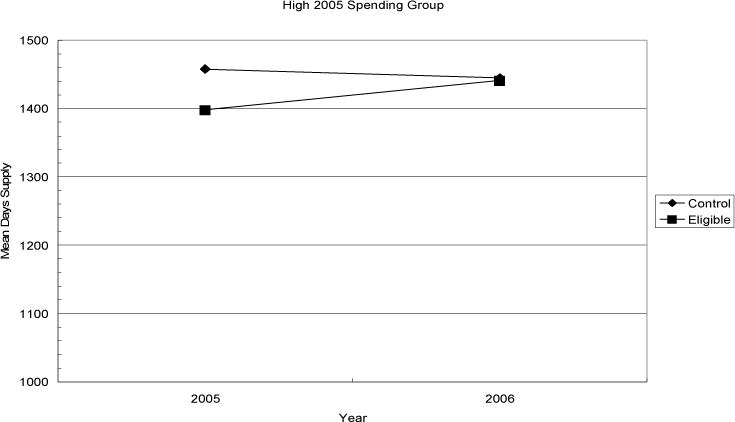
Change in Adjusted Mean Pill Days by Medicare Part D Eligibility in 2006 (Part D Eligible versus Control) and 2005 Prescription Spending Levels (Low, Moderate, High).
Among individuals with moderate pre-Part D out-of-pocket drug spending, the proportion of drug spending paid out-of-pocket decreased significantly more for Part D eligibles relative to the control group and the number of pill-days of medication increased significantly more for Part D eligibles relative to the control group between 2005 and 2006 (Table 3). The proportion of drug spending paid out-of-pocket decreased 9 percentage points for Part D eligibles while individuals in the control group experienced no change (Figure 1). Although both Part D eligibles and the control group experienced an increase in pill-days of medication, the increase for Part D eligibles (91 pill-days) was nearly twice the increase for the control group (53 pill-days) (Figure 2).
Among individuals with the lowest pre-Part D out-of-pocket drug spending, the only statistically significant difference between Part D eligibles and the control group was the change in the proportion of drug spending paid out-of-pocket (Table 3). According to Figure 1, the mean adjusted proportion of drug spending paid out-of-pocket for individuals eligible for Part D increased by 4.9 percentage points relative to controls.
DISCUSSION
There has been great interest in studying the Medicare Part D benefit, (5–9, 14–16) but this study is novel in that it uses pre/post data to characterize effects in seniors eligible for Part D based on their prior level of drug spending burden. A significant strength of this study is our use of a difference-in-difference approach that eliminates substantial sources of bias due to differences between the study groups that remain stable across follow-up. As hypothesized, the overall policy effect of Medicare Part D between 2005 and 2006 was significantly different depending on the level of pre-Part D out-of-pocket drug spending experienced by a Part D eligible senior. For eligible seniors with the highest level of pre-Part D drug spending, out-of-pocket drug spending declined 17.6% and the proportion of drug costs paid out-of-pocket decreased 23.3% after Part D was available. For eligible seniors with a moderate level of pre-Part D out-of-pocket drug spending, the proportion of drug costs paid out-of-pocket decreased 18.1% after Part D was available. A previous study showed that seniors who were the first to enroll in Part D (and who had the highest levels of pre-Part D out-of-pocket drug spending and utilization), experienced an 8.8% decrease in out-of-pocket drug spending after Part D.7 It appears that the availability of relatively generous Part D plans resulted in prescription drugs becoming significantly more affordable for eligible seniors most burdened by out-of-pocket drug costs before Part D availability.
Another stated goal for Medicare Part D, increasing seniors’ access to prescription drugs, was improved significantly for eligible seniors with a high level of spending burden for prescription drugs. For eligible seniors with the highest and moderate level of pre-Part D out-of-pocket drug spending, drug utilization (pill-days) increased 4.0% and 7.1%, respectively, after Part D availability. A previous study found a 1.1% increase in drug utilization (pill-days) among seniors who initially enrolled in Part D.7 The increase in utilization could be a reflection of seniors meeting a pent-up need for prescription drugs that were not affordable and accessible before Part D availability. Conversely, the increase could be a reflection of utilization of unnecessary drugs due to the availability of generous drug coverage (i.e. moral hazard). Future research is needed to provide an answer to the nature of the increased utilization. At a minimum, the availability of Part D appeared to change the utilization of prescription drugs for eligible seniors, most burdened by drug costs, to a level similar to that of the control group.
Our results suggest that eligible seniors with the lowest level of pre-Part D drug spending experienced only a significant increase in the proportion of drug spending paid out-of-pocket (4.9%), due mainly to a decrease in control group out-of-pocket spending, and no significantly different changes in drug use or absolute out-of-pocket spending. One implication of our results is that enrolling seniors in Part D who do not have significant prior out-of-pocket drug spending for drugs likely is very important to offset the costs associated with publically financing medications for older adults with the greatest needs for medications.
Given that the goal of adding prescription coverage to Medicare was to increase affordability of and access to prescription drugs for eligible seniors, these data suggest Part D may have achieved these goals. Also, changes in total spending on prescription drugs among eligible seniors relative to controls did not differ, suggesting no dramatic changes in overall expenditures among elders (in spite of the slight increase in utilization). Although we focused on economic outcomes (i.e., drug spending) and a broad measure of drug use (i.e., pill-days), future research should also examine how promoting affordability and access to prescription drugs impacted the quality of drug use among seniors and/or health outcomes.
This study has some important limitations to consider when evaluating its results. First, our results represent the patterns of medication use and expenditures from a cohort of older adults filling their prescriptions within a large pharmacy network in a single state, which limits the generalizeability of our findings to older adults in other geographic locations, and from differing socio-economic backgrounds. Indeed, the results of our analysis of BRFSS data suggested that patients in our sample tended to reside in counties that were less socio-economically disadvantaged than the rest of the United States, although they did not differ from the rest of the United States with regard to health insurance and health status, two of the strongest predictors of health care use. Second, by restricting the sample to individuals with prescription fills in each consecutive year, our sample may be biased towards individuals with greater healthcare needs and/or those with greater access to care. Third, this observational study used a quasi-experimental design (non-equivalent control-group, pretest- posttest design) in order to infer the causal effect of Medicare Part D. Although this study design controls for a number of threats to validity including baseline differences in health status and other patient characteristics, threats from differential maturation across treatment and control groups and regression to the mean cannot be ruled out.
Because eligible individuals could continue to enroll in Part D through May 2006 without penalty, potentially leading to a substantial proportion of patients with partial-year coverage in 2006, the results we found for the policy effect of Part D may be attenuated. To examine the potential bias, we estimated difference-in-difference models using 2007 as the post period rather than 2006. The results of these models showed similar results in terms of the number of significant coefficients and the size and direction of coefficients.
Conclusion
Our results suggest that Medicare Part D increased medication affordability and access for eligible seniors with high drug cost burden in the year prior to Part D availability, while not substantially increasing utilization among those with lower prior drug spending burdens. This differential impact suggests that Medicare Part D has been initially successful in achieving its intended effects.
Acknowledgments
The authors acknowledge Kelly Goode, PharmD., Virginia Commonwealth University, School of Pharmacy, for help in acquiring data used or this study.
Contributor Information
David A. Mott, Sonderegger Research Center, University of Wisconsin School of Pharmacy, Madison, WI.
Joshua M. Thorpe, Sonderegger Research Center, University of Wisconsin School of Pharmacy, Madison, WI.
Carolyn T. Thorpe, Health Innovation Program (HIP), Department of Population Health Sciences, University of Wisconsin – Madison, Madison, WI.
David H. Kreling, Sonderegger Research Center, University of Wisconsin School of Pharmacy, Madison, WI.
Abhijit S. Gadkari, Sonderegger Research Center, University of Wisconsin School of Pharmacy, Madison, WI
References
- 1.The Henry J. Kaiser Family Foundation. Fact Sheet:Medicare:Medicare and Prescription Drugs. The Henry J. Kaiser Family Foundation; Apr, 2003. [Google Scholar]
- 2.Cubanski J, Voris M, Kitchman M, Neuman T, Potetz L. Medicare Chartbook. 3. The Henry J. Kaiser Family Foundation; Summer. p. 2005. [Google Scholar]
- 3.Mays J, Brenner M, Neuman T, Cubanski J, Claxton G. Estimates of Medicare Beneficiaries’ Out-of-Pocket Drug Spending in 2006 Modeling the Impact of MMA. Actuarial Research Corporation and The Henry J. Kaiser Family Foundation; Nov, 2004. [Google Scholar]
- 4.Cubanski J, Neuman T, Strollo M, Damico A, Gonzales R. Examining Sources of Coverage Among Medicare Beneficiaries: Supplemental Insurance, Medicare Advantage, and Prescription Drug Coverage Findings from the Medicare Current Beneficiary Survey, 2006. The Henry J. Kaiser Family Foundation; Aug, 2008. [Google Scholar]
- 5.Joyce GF, Goldman DP, Vogt WB, Sun E, Jena AB. Medicare Part D after 2 years. Am J Manag Care. 2009 Aug;15(8):536–44. [PMC free article] [PubMed] [Google Scholar]
- 6.Lichtenberg FR, Sun SX. The impact of Medicare Part D on prescription drug use by the elderly. Health Aff. 2007;26(6):1735–44. doi: 10.1377/hlthaff.26.6.1735. [DOI] [PubMed] [Google Scholar]
- 7.Yin W, Basu A, Zhnag JX, Rabbani A, Meltzer DO, Alexander GC. The effect of the Medicare Part D prescription benefit on drug utilization and expenditures. Ann Intern Med. 2008 Feb 5;148(3):169–77. doi: 10.7326/0003-4819-148-3-200802050-00200. [DOI] [PubMed] [Google Scholar]
- 8.Schneeweiss S, Patrick A, Pedan A, Varasteh L, Levin R, Liu N, Shrank W. The effect of Medicare Part D coverage on drug use and cost sharing among seniors without prior drug benefits. Health Aff. 2009;28:w305–w316. doi: 10.1377/hlthaff.28.2.w305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ketchum J, Simon K. Medicare Part D’d effects on elderly drug costs and utilization. Cambridge, MA: National Bureau of Economic Research; Sep, 2008. (NBER working paper no. 14326). [Google Scholar]
- 10.Centers for Medicare and Medicaid Services. Medicare Program; Medicare Prescription Drug Benefit; Final Rule, 42 CFR. Federal Register. 2005;70(18) [PubMed] [Google Scholar]
- 11.Allison PD. Using panel data to estimate the effects of events. Soc Meth & Res. 1994;23:174–199. [Google Scholar]
- 12.Centers for Medicare and Medicaid Services. Medicare Enrollment: National Trends 1966–2008. http://www.cms.hhs.gov/MedicareEnRpts/Downloads/HISMI08.pdf (accessed July 17, 2009). [PubMed]
- 13.Diehr P, Yanez D, Ash A, Hornbrook M, Lin DY. Methods for analyzing health care utilization and costs. Annu Rev Public Health. 1999;20:125–44. doi: 10.1146/annurev.publhealth.20.1.125. [DOI] [PubMed] [Google Scholar]
- 14.Hoadley J, Hargrave E, Cubanski J, Nueman T. The Medicare Part D coverage gap: costs and consequences in 2007. Washington, DC: Kaiser Family Foundation; Aug, 2008. [Google Scholar]
- 15.Raebel M, Delate T, Ellis J, Bayliss E. Effects of reaching the drug benefit threshold on Medicare members’ healthcare utilization during the first year of Medicare Part D. Med Care. 2008;46:1116–1122. doi: 10.1097/MLR.0b013e318185cddd. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, Donohue J, Newhouse J, Lave J. The effects of the coverage gap on drug spending: a closer look at Medicare Part D. Health Aff. 2009;28:w317–w325. doi: 10.1377/hlthaff.28.2.w317. [DOI] [PMC free article] [PubMed] [Google Scholar]


