Abstract
AIM: To investigate the significance of angiopoietins, Tie2 and vascular endothelial growth factor (VEGF) expression in the angiogenesis and progress of hepatocellular carcinoma (HCC).
METHODS: Fresh surgically resected specimens of HCC and noncancerous liver (NCL) tissue from 38 patients with HCC were obtained, and expression of angiopoietin-1 (Ang-1), angiopoietin-2 (Ang-2), Tie2, and VEGF messenger RNA (mRNA) was examined by real-time quantitative reverse transcription-polymerase chain reaction (RT-PCR). Expression pattern of each gene in HCC and NCL tissue specimens was compared and the potential role and interaction in angiogenesis of HCC were analyzed. Genes’ expression level and its relationship with tumor’s clinicopathological parameters were also investigated. Immunohistochemical staining of CD34 was performed to determine the microvessel density (MVD) and Ang-2/Ang-1 ratio was calculated. Relationships between Ang-2/Ang-1 ratio, VEGF and MVD and clinicopathological features were also tested so as to evaluate their significance in the progression of HCC.
RESULTS: Ang-2 and VEGF mRNAs in HCC were significantly higher than those in NCL tissue (P < 0.05), whereas the Ang-1 and Tie2 mRNAs showed no statistical significance (P > 0.05), though slightly lower level of Ang-1 mRNA in HCC was observed. Ang-2/Ang-1 ratio and VEGF were both positively correlated to MVD. The Ang-2/ Ang-1 ratio, Ang-2 and VEGF were all associated with tumor’s clinicopathological parameters (P < 0.05) except for histological grades (P > 0.05). Ang-1 and Tie2 levels in different clinicopathological groups were not significantly different (P > 0.05).
CONCLUSION: Dominant Ang-2 expression against Ang-1 through Tie2 receptor in the presence of VEGF plays a critical role in initiating early neovascularization and transformation of noncancerous liver to hepatocellular carcinoma. Its consequently constant operation in formed HCC induces further angiogenesis and progression of HCC.
Keywords: Hepatocellular carcinoma, Vascular endothelial growth factor, Angiopoietin, Tie2, Angiogenesis, Neovascularization
INTRUDUCTION
Hepatocellular carcinoma (HCC) is one of the most malignant tumors in the tropics and the Far East, including China. It is the fourth most common cause of cancer death and accounts for 53% of all liver cancer deaths worldwide[1]. HCC is also a hypervascular carcinoma. It is believed that angiogenesis contributes to its malignant biological characteristics such as invasion and high rates of recurrence and metastasis[2-4]. Angiogenesis is a neovascularization process during which endothelial cells of the pre-existing capillaries proliferate and migrate to form new vascular tips or so-called “vascular sprouts” or “endothelial buds”[5]. The growth, invasion and metastasis of malignant tumors depend on the process of angiogenesis. There is evidence that solid tumors do not grow beyond 2-3 mm3 in volume when vascular sprouts are blocked[6].
Angiogenesis is a very complicated network which is closely regulated by many angiogenic factors. Vascular endothelial growth factor (VEGF) and angiopoietin are the two most important regulators. The latter is a novel family of angiogenic factors including Ang-1, Ang-2, Ang-3, and Ang-4, which have been isolated and identified as a group of ligands of the tyrosine kinase Tie2 receptor[7,8]. Ang-1 and Ang-2 have been reported as the most potent regulators for neovascularization[9] and are the activator and antagonist of Tie2 receptor, where binding of Ang-1 causes autophosphorylation of Tie2 whereas Ang-2 binding suppresses the autophosphorylation[9,10]. It was reported that proper regulation of tyrosine kinase Tie2 is absolutely required for normal vascular development, apparently by regulating vascular remodeling and maturation[11]. Ang-1 helps to maintain and stabilize maturation vessels by promoting interaction between endothelial cells and support cells, such as pericytes. Knockout mice deficient in Ang-1 develop severe vascular defect and die in uterus, similar to Tie2 deficient mice[12]. Ang-2 acts as an alternative ligand for Tie2 and binds to Tie2 with similar affinity, but competitively antagonizes Ang-1 effects with blockage of Tie2 phosphorylation and activation. Functionally, transgenic mice over-expressing Ang-2 show even more severe vascular defects as the Ang-1 or Tie2 deficient mice[13]. In the presence of VEGF, vessel destabilization caused by Ang-2 has been hypothesized to induce angiogenic response, whereas in the absence of VEGF, Ang-2 leads to vessel regression[13,14].
Although the exact role of angiopoietin/Tie2 system remains enigmatic, there is evidence that this system in the presence of VEGF is important for the initiation of angiogenesis and vascular sprouting in tumors[15]. It was recently reported that VEGF and aniopoietin/Tie2 system play a key role in the transformation of normal lung to non-small cell lung carcinoma[16]. However, their exact role in the initiation and development of HCC is still unclear. In this study, we investigated the expression of Ang-1, Ang-2, Tie2 and VEGF by real-time quantitative reverse transcription-polymerase chain reaction (RT-PCR). Thirty-eight specimens of HCC and noncancerous liver (NCL) tissues were examined in an attempt to definite their role.
MATERIALS AND METHODS
Patients and specimens
Fresh surgically resected specimens of HCC and noncancerous liver tissue were obtained from 38 patients with HCC who underwent partial hepatectomy in the Department of General Sugery of Zhongnan Hospital, Wuhan University (Wuhan, China) from 2003 to 2005. Demographic data of all patients are shown in Table 1. Thirty-four patients suffered from hepatitis and liver cirrhosis at different extent. Diagnosis of all patients was confirmed by histological examination after operation, and the noncancerous liver tissue was resected. Fully informed consent was obtained from all patients, and the study was performed in accordance with the guidelines of the Helsinki Declaration of 1975 amended in 1983. Those who accepted any therapy or accompanied any other severe complications and those with metastatic liver tumor were excluded. Some samples were frozen in liquid nitrogen immediately after resection and the remaining were fixed in 10% formalin, embedded in paraffin and stained with hematoxylin-eosin for pathological examination. Histological grade was classified according to the criteria of Edmondson and Steiner.
Table 1.
Demographic data and clinicopathological features in 38 cases of HCC
| No. | Sex | Age | Tumor size (cm) | Tumorcapsule | Metastasis | Portal vein invasion | Histological grade | Liver cirrhosis |
| 1 | M | 51 | < 5 | + | - | - | G2 | - |
| 2 | M | 49 | < 5 | + | - | - | G3 | + |
| 3 | M | 31 | > 10 | - | - | - | G2 | + |
| 4 | M | 59 | 5-10 | + | - | - | G3 | + |
| 5 | F | 55 | > 10 | - | - | - | G1 | + |
| 6 | M | 65 | > 10 | - | - | + | G3 | + |
| 7 | M | 56 | > 10 | - | + | + | G2 | + |
| 8 | M | 51 | > 10 | - | - | + | G3 | + |
| 9 | F | 49 | < 5 | + | - | - | G1 | - |
| 10 | M | 50 | 5-10 | - | - | - | G2 | + |
| 11 | M | 53 | > 10 | - | - | + | G2 | + |
| 12 | M | 43 | < 5 | + | - | - | G3 | + |
| 13 | M | 36 | 5-10 | + | - | - | G2 | + |
| 14 | F | 46 | 5-10 | - | - | - | G1 | + |
| 15 | F | 45 | 5-10 | - | - | - | G1 | + |
| 16 | M | 52 | 5-10 | - | - | - | G2 | + |
| 17 | F | 50 | 5-10 | - | - | - | G1 | + |
| 18 | F | 52 | < 5 | + | - | - | G1 | + |
| 19 | F | 61 | > 10 | - | + | + | G1 | + |
| 20 | M | 36 | 5-10 | - | - | - | G2 | + |
| 21 | M | 46 | < 5 | + | - | - | G2 | + |
| 22 | M | 48 | > 10 | - | - | + | G2 | + |
| 23 | F | 63 | < 5 | + | - | - | G1 | + |
| 24 | M | 35 | 5-10 | + | - | - | G2 | - |
| 25 | M | 74 | > 10 | - | + | + | G3 | + |
| 26 | F | 55 | 5-10 | - | - | - | G1 | + |
| 27 | M | 59 | 5-10 | - | - | - | G2 | + |
| 28 | M | 30 | < 5 | + | - | - | G3 | + |
| 29 | F | 56 | 5-10 | - | - | - | G1 | + |
| 30 | M | 60 | 5-10 | - | - | - | G2 | + |
| 31 | F | 65 | < 5 | + | - | - | G1 | + |
| 32 | M | 59 | > 10 | - | + | + | G2 | + |
| 33 | M | 61 | > 10 | - | + | + | G2 | + |
| 34 | M | 55 | < 5 | - | - | - | G2 | - |
| 35 | M | 48 | 5-10 | + | - | - | G3 | + |
| 36 | M | 49 | > 10 | - | - | + | G3 | + |
| 37 | F | 50 | 5-10 | - | - | - | G1 | + |
| 38 | M | 58 | > 10 | - | + | + | G3 | + |
Real-time semiquantitative RT-PCT assay
Total RNA was extracted with Trizol reagent (Promega, USA) following the manufacturer’s instructions and quantitated by absorbance analysis at 260 nm. First-strand cDNA was synthesized using first standard buffer, dNTP mixture containing each deoxynucleotide triphosphate base dithiothreitol and moloney murine leukemia virus RT (GIBCO, BRIL) as previously described[17]. Four-fold dilution of the products was used for PCR in a Rotor-Gene2000 real-time PCR machine (Corbett Research, Australia). Primers of each gene are shown in Table 2 as previously described[10]. Glyceraldehyde-3-phosphate dehydrogenase (G3PDH) was used as an internal standard. Reverse transcription was performed at 50°C for 30 min. The samples were subjected to PCR analysis using the following cycling parameters: at 95°C for 10 min, then at 95°C for 15 s and at 60°C for 1 min for 40 cycles. Negative controls (cDNA-free solutions) were included in each reaction. Standard reaction curve was analyzed by Rotor-Gene 5.0 (Corbett Research) software and relative quantity according to standard reaction curve (Rv) was calculated according to the formula Rv = RGene/RG3PDH by computer.
Table 2.
Primer sequences of each gene for real-time RT-PCR assay
| Target gene | Sense | Antisense |
| Ang-1 | ACTGT GCAGA TGTAT ATCAA GC | GTGGA ATCTG TCATA CTGTG AA |
| Ang-2 | GGAAG ACAAG CACAT CATCC | AGTAA GCCTG ATTCC CTTCC |
| Tie2 | TCTGT GCTGT TCCTT CTTGC | CTTGA GTAAC TTCCA GCGGA |
| VEGF | AGCTA CTGCC ATCCA ATCGC | GGGCG AATCC AATTC CAAGA G |
| G3PDH | GTCAA CGGAT TTGGT CTGTA TT | AGTCT TCTGG GTGGC AGTGA T |
Immunohistochemical assessment of vessel density
Paraffin-embedded tissues were sectioned (4 μm). The slides were deparaffined as usual, washed with tris buffered saline (TBS), and then incubated with 10% normal goat serum (Zhongshan Bio. CA). The sections were incubated with appropriately diluted (1:10) rat anti-human CD34 monoclonal antibody (Santa Cruz Biotechnology, CA) for 24 h at 4°C. Primary antibody was removed and washed with TBS, goat-anti-rat IgG peroxidase (Zhongshan Bio. CA) was then added. Finally the slices were stained as usual with haematoxilin and washed with distilled water. Quantification of blood vessels was carried out as previously described[18]. Any brown-stained endothelial cell cluster distinct from adjacent microvessels, tumor cells, or other stromal cells was considered as a single countable microvessel. The most vascular areas of tumors were identified on a low-power field (× 100), and vessels were counted in five high-power fields (× 200). The data were presented as mean ± SD. The process was performed by special pathologists in a blind manner.
Statistical analysis
Data were analyzed for significance with unpaired t test and ANOVA test. Statistical software SPSS 11.5 was used in the analysis. P < 0.05 was considered statistically
significant.
RESULTS
Expression of Ang-1, Ang-2, Tie2 and VEGF in NCL and HCC
The expression of Ang-2 and VEGF mRNA was significantly higher in HCC than in the NCL tissue
(P < 0.05), but the Ang-1 and Tie2 mRNA showed no statistical significance (P > 0.05), though slightly lower level of Ang-1 in HCC was observed (Figure 1).
Figure 1.
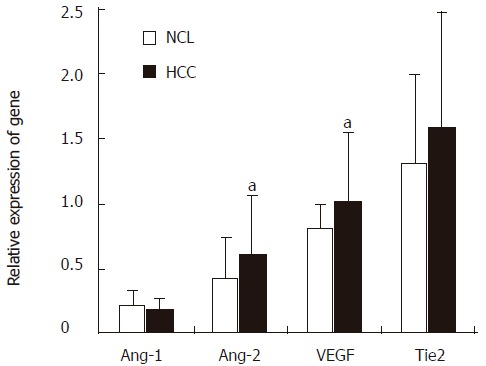
Expression of Ang-1, Ang-2, Tie2 and VEGF in HCC and NCL. HCC: hepatocellular carcinoma; NCL: noncancerous liver tissue. aP < 0.05 vs NCL.
Correlation between Ang-2/Ang-1 ratio, VEGF and MVD
The expression of CD34 in NCL tissue was poor or even negative, but strong in HCC. Microvessel counting revealed that MVD was higher in HCC than in NCL. Because the balance between Ang-1 and Ang-2 mainly defines Tie2 signal, we determined the ratio of Ang-2 to Ang-1 and evaluated its correlation with MVD. VEGF was also involved. The Ang-2/Ang-1 ratio in HCC was positively related to MVD (P = 0.01, r = 0.42) and VEGF (P = 0.01, r = 0.41) (Figure 2).
Figure 2.
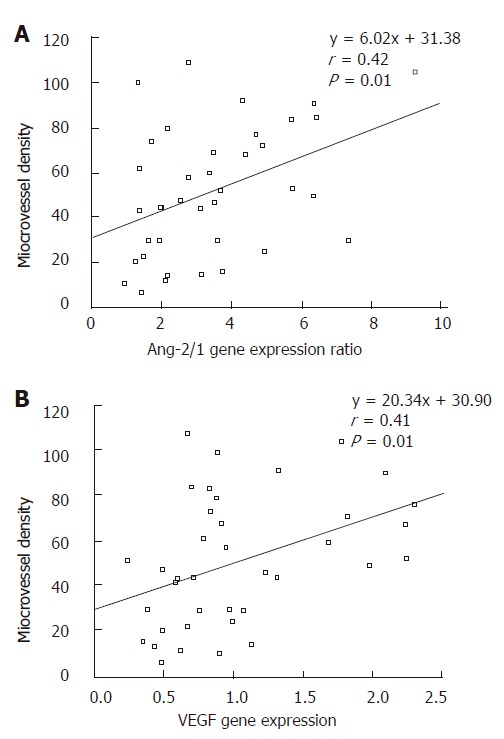
Relationship between Ang-2/Ang-1 ratio and microvessel density (A) and between vascular endothelial growth factor (VEGF) and microvessel density (B).
Relationship between gene expression pattern and clinicopathological parameters
The values of Ang-1, Ang-2, Tie2, VEGF and Ang-2/Ang-1 ratio were classified according to HCC clinicopathological parameters including tumor size, tumor capsule, portal vein invasion, distal metastasis and histological grades. Ang-2, VEGF and Ang-2/Ang-1 ratio were all associated with the above clinicopathological parameters
(P < 0.05) except for histological grades (P > 0.05), whereas Ang-1 and Tie2 showed no relation with any of the clinicopathological parameters (P > 0.05) (Table 3).
Table 3.
Relation between gene expression pattern and clinicopathological parameters (mean ± SD)
| Clinical parameters | Ang-2 | Ang-1 | Ang-2/1 | Tie2 | VEGF |
| Tumor size (cm) | |||||
| < 5 (n = 10) | 0.267 ± 0.113 | 0.148 ± 0.089 | 2.175 ± 1.025 | 1.686 ± 0.550 | 0.552 ± 0.205 |
| ≥ 5 (n = 28) | 0.748 ± 0.422 | 0.212 ± 0.082 | 3.880 ± 2.067 | 1.570 ± 0.990 | 1.213 ± 0.537 |
| Histlogical grade | |||||
| G1 (n = 12) | 0.509 ± 0.320 | 0.168 ± 0.064 | 3.106 ± 1.409 | 1.511 ± 0.574 | 0.916 ± 0.497 |
| G2 (n = 16) | 0.633 ± 0.395 | 0.194 ± 0.081 | 3.543 ± 1.925 | 1.470 ± 0.726 | 1.095 ± 0.604 |
| G3 (n = 10) | 0.737 ± 0.512 | 0.234 ± 0.101 | 3.645 ± 2.470 | 1.921 ± 0.138 | 1.097 ± 0.585 |
| Portal vein invasion | |||||
| positive (n = 11) | 1.152 ± 0.376 | 0.232 ± 0.053 | 5.096 ± 1.691 | 1.880 ± 1.494 | 1.791 ± 0.423 |
| negative (n = 27) | 0.405 ± 0.163 | 0.180 ± 0.092 | 2.753 ± 1.631 | 1.488 ± 0.500 | 0.732 ± 0.254 |
| Metastasis | |||||
| positive (n = 6) | 1.320 ± 0.366 | 0.235 ± 0.061 | 5.912 ± 1.847 | 2.262 ± 1.734 | 2.007 ± 0.214 |
| negative (n = 32) | 0.490 ± 0.271 | 0.187 ± 0.088 | 2.967 ± 1.600 | 1.148 ± 0.619 | 0.857 ± 0.415 |
| Tumor capsule | |||||
| positive (n = 13) | 0.308 ± 0.135 | 0.178 ± 0.112 | 2.078 ± 0.887 | 1.733 ± 0.424 | 0.579 ± 0.198 |
| negative (n = 25) | 0.783 ± 0.429 | 0.203 ± 0.068 | 4.135 ± 1.998 | 1.529 ± 1.056 | 1.278 ± 0.558 |
DISSCUSSION
VEGF and angiopoietin are two of the most important regulators for neovascularization. The former is the most potent angiogenic factor that promotes endothelial proliferation and increases vascular permeability by binding to its specific receptors in endothelial cells such as Flt-1, KDR/Flk-1 and Flt-4[19]. Animal models and in vitro experiments have shown that Ang-1, Ang-2 and Tie2 in association with VEGF constitute a system that regulates vascular quiescence and endothelial plasticity, through which a balanced state of vascular maturity and development of complex vascular networks can be achieved[20]. In the current study we investigated the expression of Ang-1, Ang-2, Tie2 and VEGF mRNA in HCC and noncancerous liver in an attempt to definite their exact role in carcinogenesis and progression of HCC via angiogenesis. To avoid possible influence of indefinite borderline carcinoma invasion, the noncancerous liver tissue was obtained from HCC position as far as possible during surgery. Ang-2, as an actively angiogenic factor in the presence of VEGF, is little expressed in physiological condition but highly expressed in several actively neovascularized organs such as endometrium, ovary, placenta etc[9,20-22]. This factor is up-regulated in many carcinomas, such as gastric, ovarian, colorectal and breast cancer, etc [23-26]. In this study, Ang-2 mRNA was significantly up-regulated in HCC compared with the nontumorous liver tissue, which is consistent with previous reports[2,27] and has been regarded as a contributor to recurrence, metastasis and poor prognosis of HCC. Besides, high expression of Ang-2 and low expression Ang-1 were found in HCC in comparison with NCL, indicating that they play a key role in the carcinogenesis and progression of HCC via angiogenesis. Tumorous angiogenesis is very different from the physiological process[28]. During this procession, vascular quiescence and stabilization are mediated by Ang-1, Ang-2 and Tie2 system. Therefore, the pathologic state of imbalanced Ang-2/Ang-1 ratio in the presence of VEGF plays a critical role in the transformation of noncancerous liver to liver cancer by initiating early neovascularization. Vajkoczy et al[29] reported that tumors in their very early stage are initiated by host vessels via VEGF, VEGF receptor-2 and Ang-2. Wong et al[16] also reported that angiopoietins, tie2 and VEGF are differentially expressed in the transformation of normal lung to non-small cell lung carcinomas.
CD34 protein, an endothelial-specific marker, was immunohistochemically stained and MVD was determined in HCC in our study. Ang-2/Ang-1 ratio was calculated and statistical analysis showed that Ang-2/1 ratio was positively correlated to MVD, and VEGF, but such relation was not found between Ang-1, Tie2 and MVD. Ang-2/Ang-1 ratio, Ang-2 and VEGF are all associated with tumor’s clinicopathological characteristics such as tumor size, tumor capsule, portal vein invasion and metastasis, indicating that VEGF and angiopoiein/Tie2 system contributes greatly to the progress of HCC by modulating angiogenesis. Continuous growth of carcinoma induces hypoxia and necrosis in central portion, thus reversely up-regulating VEGF[30]. In the presence of Ang-2, tumor and invasion angiogenesis are greatly accelerated. A study[31] on C6 glioma showed that Ang-2 expresses strongly whereas VEGF expresses poorly when the tumor reaches 1mm in diameter, and when the tumor reaches more than 2 mm in diameter necrosis occurs in the central portion, both Ang-2 and VEGF are strongly expressed which induces intensive angiogenesis. Interestingly, in the current study Ang-1, Ang-2, Tie2, VEGF and Ang-2/Ang-1 ratio were all not statistically associated with histological grades of HCC, which is similar to a previous report on ovarian cancer[32].
In conclusion, expression of Ang-2 against Ang-1 through the Tie2 receptor in the presence of VEGF plays a critical role in initiating early neovascularization and induces transformation of noncancerous liver to HCC. The consequently constant immature neovacularization in HCC further promotes angiogenesis and progression of tumors.
ACKNOWLEDGMENTS
The authors anknowledge the technical assistance of Yong-Hua Sun (Genome Department, Institute of Hydrobiology, the Chinese Academy of Sciences) and Bi-Cheng Wang (Department of pathology, Zhongnan Hospital, Wuhan University).
Footnotes
S- Editor Wang J L- Editor Wang XL E- Editor Liu Y
References
- 1.Pisani P, Parkin DM, Bray F, Ferlay J. Erratum: Estimates of the worldwide mortality from 25 cancers in 1990. Int. J. Cancer, 83, 18-29 (1999) Int J Cancer. 1999;83:870–873. doi: 10.1002/(sici)1097-0215(19991210)83:6<870::aid-ijc35>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 2.Poon RT, Ng IO, Lau C, Yu WC, Fan ST, Wong J. Correlation of serum basic fibroblast growth factor levels with clinicopathologic features and postoperative recurrence in hepatocellular carcinoma. Am J Surg. 2001;182:298–304. doi: 10.1016/s0002-9610(01)00708-5. [DOI] [PubMed] [Google Scholar]
- 3.Poon RT, Lau CP, Ho JW, Yu WC, Fan ST, Wong J. Tissue factor expression correlates with tumor angiogenesis and invasiveness in human hepatocellular carcinoma. Clin Cancer Res. 2003;9:5339–5345. [PubMed] [Google Scholar]
- 4.Carr BI. Hepatocellular carcinoma: current management and future trends. Gastroenterology. 2004;127:S218–S224. doi: 10.1053/j.gastro.2004.09.036. [DOI] [PubMed] [Google Scholar]
- 5.Zhang ZL, Liu ZS, Sun Q. Effects of thalidomide on angiogenesis and tumor growth and metastasis of human hepatocellular carcinoma in nude mice. World J Gastroenterol. 2005;11:216–220. doi: 10.3748/wjg.v11.i2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Folkman J. Role of angiogenesis in tumor growth and metastasis. Semin Oncol. 2002;29:15–18. doi: 10.1053/sonc.2002.37263. [DOI] [PubMed] [Google Scholar]
- 7.Pham VN, Roman BL, Weinstein BM. Isolation and expression analysis of three zebrafish angiopoietin genes. Dev Dyn. 2001;221:470–474. doi: 10.1002/dvdy.1157. [DOI] [PubMed] [Google Scholar]
- 8.Davis S, Aldrich TH, Jones PF, Acheson A, Compton DL, Jain V, Ryan TE, Bruno J, Radziejewski C, Maisonpierre PC, et al. Isolation of angiopoietin-1, a ligand for the TIE2 receptor, by secretion-trap expression cloning. Cell. 1996;87:1161–1169. doi: 10.1016/s0092-8674(00)81812-7. [DOI] [PubMed] [Google Scholar]
- 9.Hata K, Udagawa J, Fujiwaki R, Nakayama K, Otani H, Miyazaki K. Expression of angiopoietin-1, angiopoietin-2, and Tie2 genes in normal ovary with corpus luteum and in ovarian cancer. Oncology. 2002;62:340–348. doi: 10.1159/000065066. [DOI] [PubMed] [Google Scholar]
- 10.Mitsuhashi N, Shimizu H, Ohtsuka M, Wakabayashi Y, Ito H, Kimura F, Yoshidome H, Kato A, Nukui Y, Miyazaki M. Angiopoietins and Tie-2 expression in angiogenesis and proliferation of human hepatocellular carcinoma. Hepatology. 2003;37:1105–1113. doi: 10.1053/jhep.2003.50204. [DOI] [PubMed] [Google Scholar]
- 11.Sugimachi K, Tanaka S, Taguchi K, Aishima S, Shimada M, Tsuneyoshi M. Angiopoietin switching regulates angiogenesis and progression of human hepatocellular carcinoma. J Clin Pathol. 2003;56:854–860. doi: 10.1136/jcp.56.11.854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suri C, Jones PF, Patan S, Bartunkova S, Maisonpierre PC, Davis S, Sato TN, Yancopoulos GD. Requisite role of angiopoietin-1, a ligand for the TIE2 receptor, during embryonic angiogenesis. Cell. 1996;87:1171–1180. doi: 10.1016/s0092-8674(00)81813-9. [DOI] [PubMed] [Google Scholar]
- 13.Maisonpierre PC, Suri C, Jones PF, Bartunkova S, Wiegand SJ, Radziejewski C, Compton D, McClain J, Aldrich TH, Papadopoulos N, et al. Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science. 1997;277:55–60. doi: 10.1126/science.277.5322.55. [DOI] [PubMed] [Google Scholar]
- 14.Teichert-Kuliszewska K, Maisonpierre PC, Jones N, Campbell AI, Master Z, Bendeck MP, Alitalo K, Dumont DJ, Yancopoulos GD, Stewart DJ. Biological action of angiopoietin-2 in a fibrin matrix model of angiogenesis is associated with activation of Tie2. Cardiovasc Res. 2001;49:659–670. doi: 10.1016/s0008-6363(00)00231-5. [DOI] [PubMed] [Google Scholar]
- 15.Glade Bender J, Cooney EM, Kandel JJ, Yamashiro DJ. Vascular remodeling and clinical resistance to antiangiogenic cancer therapy. Drug Resist Updat. 2004;7:289–300. doi: 10.1016/j.drup.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Wong MP, Chan SY, Fu KH, Leung SY, Cheung N, Yuen ST, Chung LP. The angiopoietins, tie2 and vascular endothelial growth factor are differentially expressed in the transformation of normal lung to non-small cell lung carcinomas. Lung Cancer. 2000;29:11–22. doi: 10.1016/s0169-5002(00)00118-5. [DOI] [PubMed] [Google Scholar]
- 17.Torimura T, Ueno T, Kin M, Harada R, Taniguchi E, Nakamura T, Sakata R, Hashimoto O, Sakamoto M, Kumashiro R, et al. Overexpression of angiopoietin-1 and angiopoietin-2 in hepatocellular carcinoma. J Hepatol. 2004;40:799–807. doi: 10.1016/j.jhep.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 18.Weidner N, Semple JP, Welch WR, Folkman J. Tumor angiogenesis and metastasis--correlation in invasive breast carcinoma. N Engl J Med. 1991;324:1–8. doi: 10.1056/NEJM199101033240101. [DOI] [PubMed] [Google Scholar]
- 19.Yamaguchi R, Yano H, Nakashima Y, Ogasawara S, Higaki K, Akiba J, Hicklin DJ, Kojiro M. Expression and localization of vascular endothelial growth factor receptors in human hepatocellular carcinoma and non-HCC tissues. Oncol Rep. 2000;7:725–729. doi: 10.3892/or.7.4.725. [DOI] [PubMed] [Google Scholar]
- 20.Patan S. Vasculogenesis and angiogenesis. Cancer Treat Res. 2004;117:3–32. doi: 10.1007/978-1-4419-8871-3_1. [DOI] [PubMed] [Google Scholar]
- 21.Hirchenhain J, Huse I, Hess A, Bielfeld P, De Bruyne F, Krüssel JS. Differential expression of angiopoietins 1 and 2 and their receptor Tie-2 in human endometrium. Mol Hum Reprod. 2003;9:663–669. doi: 10.1093/molehr/gag083. [DOI] [PubMed] [Google Scholar]
- 22.Leach L, Babawale MO, Anderson M, Lammiman M. Vasculogenesis, angiogenesis and the molecular organisation of endothelial junctions in the early human placenta. J Vasc Res. 2002;39:246–259. doi: 10.1159/000063690. [DOI] [PubMed] [Google Scholar]
- 23.Ochiumi T, Tanaka S, Oka S, Hiyama T, Ito M, Kitadai Y, Haruma K, Chayama K. Clinical significance of angiopoietin-2 expression at the deepest invasive tumor site of advanced colorectal carcinoma. Int J Oncol. 2004;24:539–547. [PubMed] [Google Scholar]
- 24.Sun XD, Liu XE, Wu JM, Cai XJ, Mou YP, Li JD. Expression and significance of angiopoietin-2 in gastric cancer. World J Gastroenterol. 2004;10:1382–1385. doi: 10.3748/wjg.v10.i9.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang L, Yang N, Park JW, Katsaros D, Fracchioli S, Cao G, O'Brien-Jenkins A, Randall TC, Rubin SC, Coukos G. Tumor-derived vascular endothelial growth factor up-regulates angiopoietin-2 in host endothelium and destabilizes host vasculature, supporting angiogenesis in ovarian cancer. Cancer Res. 2003;63:3403–3412. [PubMed] [Google Scholar]
- 26.Sfiligoi C, de Luca A, Cascone I, Sorbello V, Fuso L, Ponzone R, Biglia N, Audero E, Arisio R, Bussolino F, et al. Angiopoietin-2 expression in breast cancer correlates with lymph node invasion and short survival. Int J Cancer. 2003;103:466–474. doi: 10.1002/ijc.10851. [DOI] [PubMed] [Google Scholar]
- 27.Deli G, Jin CH, Mu R, Yang S, Liang Y, Chen D, Makuuchi M. Immunohistochemical assessment of angiogenesis in hepatocellular carcinoma and surrounding cirrhotic liver tissues. World J Gastroenterol. 2005;11:960–963. doi: 10.3748/wjg.v11.i7.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Papetti M, Herman IM. Mechanisms of normal and tumor-derived angiogenesis. Am J Physiol Cell Physiol. 2002;282:C947–C970. doi: 10.1152/ajpcell.00389.2001. [DOI] [PubMed] [Google Scholar]
- 29.Vajkoczy P, Farhadi M, Gaumann A, Heidenreich R, Erber R, Wunder A, Tonn JC, Menger MD, Breier G. Microtumor growth initiates angiogenic sprouting with simultaneous expression of VEGF, VEGF receptor-2, and angiopoietin-2. J Clin Invest. 2002;109:777–785. doi: 10.1172/JCI14105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang GW, Yang LY, Lu WQ. Expression of hypoxia-inducible factor 1alpha and vascular endothelial growth factor in hepatocellular carcinoma: Impact on neovascularization and survival. World J Gastroenterol. 2005;11:1705–1708. doi: 10.3748/wjg.v11.i11.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holash J, Wiegand SJ, Yancopoulos GD. New model of tumor angiogenesis: dynamic balance between vessel regression and growth mediated by angiopoietins and VEGF. Oncogene. 1999;18:5356–5362. doi: 10.1038/sj.onc.1203035. [DOI] [PubMed] [Google Scholar]
- 32.Hata K, Nakayama K, Fujiwaki R, Katabuchi H, Okamura H, Miyazaki K. Expression of the angopoietin-1, angopoietin-2, Tie2, and vascular endothelial growth factor gene in epithelial ovarian cancer. Gynecol Oncol. 2004;93:215–222. doi: 10.1016/j.ygyno.2003.12.031. [DOI] [PubMed] [Google Scholar]


