Abstract
The currently accepted etiopathogenic hypothesis suggests that the chronic intestinal inflammation and related systemic manifestations characteristic of inflammatory bowel disease (IBD) are due to an overly aggressive or pathologic immune response to resident luminal bacterial constituents. Predisposing factors are genetic dysregulation of mucosal immune responses and/or barrier function, with onset triggered by environmental stimuli. These factors and their interactions may also be important determinants of disease phenotype and disease progression. The emergence of immunogenetic phenotypes lends support to the proposed hypothesis that susceptibility genes regulate distinct immune processes, driven by luminal antigens, expressed as specific immune phenotypes which in turn influence clinical phenotypes in IBD patients.
Keywords: Inflammatory bowel disease, Immune reactivity, Disease phenotype
INTRODUCTION
The currently accepted etiopathogenic hypothesis suggests that the chronic intestinal inflammation and related systemic manifestations characteristic of inflammatory bowel disease (IBD) are due to an overly aggressive or pathologic immune response to resident luminal bacterial constituents. Predisposing factors are genetic dysregulation of mucosal immune responses and/or barrier function, with onset triggered by environmental stimuli. These factors and their interactions may also be important determinants of disease phenotype and disease progression. The interaction between genetic susceptibility and luminal bacteria deserves particular attention. The results from animal studies indicate that not all commensal bacterial species are identical in their abilities to induce disease in the face of a common genetic defect. For instance, HLA B27/β2 microglobulin transgenic rats raised under sterile conditions do not develop colitis. However, when colonized with normal specific pathogen-free commensal cecal bacteria, they develop aggressive disease involving the colon and gastro-duodenal area within one month[1]. On the one hand, when colonized with a single bacterial strain, Bacteroides vulgatus, these same genetically susceptible rats develop moderate colitis but no gastro-duodenal disease. When selectively colonized with Eschericia.coli, they exhibit neither disease nor T cell activation[2]. This data suggests that not all commensal bacterial strains trigger an abnormal immune response for a given genetic susceptibility. The same non-pathogenic bacteria, however, may induce inflammation in a different genetically susceptible host. More specifically, further research from the same group demonstrated that Escherichia coli induced only mild cecal inflammation after 3 wk of monoassociation in interleukin 10-/- mice. In contrast, Enterococcus faecalis-monoassociated interleukin 10-/- mice developed distal colitis at 10-12 wk that was progressively more severe and associated with duodenal inflammation and obstruction by 30 wk. Their results suggest that different commensal bacterial species selectively initiate immune-mediated intestinal inflammation with distinctly different kinetics and anatomic distribution in the same host[3]. These findings highlight the fact that both genetic susceptibility and luminal antigenic drive are important determinants of disease susceptibility and modification. Immune reactivity as measured by the serological expression of immune responses to specific bacteria may indeed be representative of this host gene luminal bacterial interaction. If indeed these immune responses represent the sum of a genetic and environmental predisposition to IBD, quantitative and qualitative expression of these immune responses may serve as an immunologic risk marker for IBD phenotypes.
IMMUNE PHENOTYPES
Immune responses to resident intestinal flora in humans have been reported. Duchmann et al demonstrated that CD patients boast reactivity to hundreds of bacterial antigens created from sonification of multiple bacterial specifies including enterobacteria, bacteriodes and bifidobacterium[4]. Immune reactivity to more specific microbial antigens has been reported in the sera of patients with IBD (Table 1).
Table 1.
Pooled frequency of immune responses in CD, UC and non-IBD
| Immune Response | %CD | % UC | % non-IBD |
| ASCA | 60 | < 5 | < 5 |
| Anti-OmpC | 40 | < 5 | < 5 |
| Anti-I2 | 54 | < 10 | 20 |
| Anti-CBir1 | 50 | < 10 | < 10 |
| pANCA | 20-25 | 65 | < 5 |
Antibodies to Saccharomyces cerevisiae (ASCA) was the first CD specific immune response thought to be targeted towards microbial antigens. IgA and IgG antibodies are directed against a specific oligomannosidic epitope present on the cell wall of the yeast saccharomyces[5]. To date it remains unknown as to what the specific microbial antigen ASCA is cross reacting with and giving rise to seropositivity specifically in the sera of patients with CD. ASCA is present in approximately 60% of CD patients, yet less than 5% in UC and non-IBD patients[6-8]. The specificity of ASCA renders a positive test result accurate in differentiating CD from UC and IBD from non-IBD in cases of diagnostic uncertainty. ASCA also remains an important marker of disease severity as defined by the development of complicating disease. More recent research has resulted in the identification of 3 additional markers representative of microbial driven immune responses, antibodies to the E.coli outer-membrane porin C (OmpC), the Pseudomonas fluorescens CD related protein (anti-CD related bacterial sequence {I2}) and the CBir1 flagellin. Antibodies to OmpC, whose antigen is purified from commensal E.coli[9,10], are present in 37%-55% of patients with CD and 2%-11% of patients with UC, while no more than 5% of non-IBD individuals express anti-OmpC[11-13]. I2 was isolated from affected colonic mucosa yet not in the unaffected segments and thus thought to be specific to CD[9]. Immune responses to this antigen are present in up to 55% of CD patients; however the specificity of this antibody has been questioned as it has been detected in the serum of UC patients (10%) and more impressively in up to 20% of non-IBD patients (9, data on file Prometheus Labs). Given its limitation as a diagnostic marker, it is unclear as to whether this immune response will provide additional prognostic information and further studies are needed. Serologic expression cloning was used to identify an immunodominant antigen, CBir1 flagellin, to which strong immune responses (B cell and CD4T cell) occurred in colitic mice[14]. These findings were translated from the bench to the bedside and approximately 50% of CD patients had serum reactivity to CBir1 whereas UC, inflammatory and healthy controls exhibited little to no reactivity to this flagellin[15].
All of the prior immune responses are specific to CD. In contrast perinuclear anti-neutrophil antibody (pANCA) is noted for its association with UC or a UC like phenotype. This IBD-specific ANCA displays a unique perinuclear highlighting (pANCA) on immunoflourence staining and is DNAse sensitive[16]. Although it remains undefined, it has been suggested that the antigen to which pANCA is directed is a nuclear histone (H1)[17]. This antigen is clearly distinct from the proteinase 3 or the myeloperoxidase reactivity observed in those patients with vasculitic disorders. pANCA is likely an autoantibody that is representative of a cross-reactivity with a luminal bacterial antigen[10,18,19]. Despite epidemiological and methodological differences, pANCA has been shown repeatedly to be prevalent in the sera of approximately 60% and 20% of UC and CD patients, respectively[6-8,20-23]. Typically, < 5% of non-IBD patients are pANCA positive.
As seen with the genetic and clinical heterogeneity of CD, studies have shown immune response (immune phenotype) heterogeneity exists among CD patients. Landers et al analyzed immune response heterogeneity in 330 patients and found that ASCA was detected in 56% of patients; 55% were seroreactive to OmpC 50% were seroreactive to I2, and 23% were pANCA[9]. Eighty-five percent responded to at least 1 antigen; only 4% responded to all 4. Among microbial antigens (ASCA, OmpC, I2), 78% responded to at least 1, and 57% were double positive, but only 26% responded to all 3. The level of response was stable over time and with change in disease activity. Among patients with the same qualitative antigen-response profiles, quantitative response differed. Moreover this study demonstrated that CD patients could be clustered into 4 distinct groups depending on their immune response patterns to microbial or autoantigens. One cluster was ASCA, a second was antibodies to OmpC and I2, the third pANCA and the fourth was low or no immune response to any tested antigens.
Subsequent analyses incorporating CBir1demonstrated that antibodies to CBir1 are present in approximately 40% of CD patients negative for antibodies to specific microbial antigens (ASCA, OmpC and I2) which suggests a unique immune phenotype[14]. Immune reactivity to CBir1 may further define CD phenotypes in that anti-CBir1 expression is present in 40%-44% of pANCA positive CD patients vs only 4% in pANCA positive UC patients. This difference may denote a unique etiopathogenic mechanism of disease that helps to further stratify patients based on immunogenetic phenotypes.
CLINICAL AND IMMUNE PHENOTYPES
Disease phenotype is not always a static phenomenon. Retrospective studies have examined the stability of disease phenotypes over the course of disease from time of diagnosis until point of last follow-up. It appears that disease location essentially remains stable over time, yet disease behavior evolves, such that after 20-yr of follow up, at least 80% of patients with originally non-complicating disease progress to complication, either penetrating or stricturing in nature[24-26].These findings suggest that non-complicating (non-penetrating, non-stricturing) disease behavior may not be a stable phenotype but just a temporary state that evolves in to one of the two complicating disease states over time.
Immune responses were first investigated as tools to differentiate UC from CD given the specificity of ASCA for CD and pANCA for UC. Advances in the sensitivity of the test characteristics lead to studies evaluating antibodies as diagnostic tools to differentiate IBD from non-IBD. Although conflicting, studies do support the use of these markers, particularly in children, to guide clinicians in cases of diagnostic uncertainty[8,27,28]. As new markers are identified and the test characteristics improve, the notion of immune responses optimizing diagnostic accuracy may become more clearer and clinically valid.It has become clear, however, that immune responses may also have perhaps a more important mechanistic implication in the pathogenesis of IBD. As alluded to above, these immune reactivities, as measured by the serological expression of immune responses to specific bacteria, may be representative of the host gene luminal bacterial interaction characteristic of IBD. Moreover if these immune responses represent the sum of a genetic and environmental predisposition to IBD, quantitative and qualitative expression of these immune responses may serve as an immunologic risk marker for IBD phenotypes.
The initial immune-clinical phenotype studies demonstrated that although pANCA has been established as a UC-specific marker, approximately 25% of all CD patients also express pANCA. These CD patients are described as "UC-like" and tend to have an uncomplicated disease course[29-31]. In contrast, higher ASCA levels were shown to be associated with earlier age of disease onset, both stricturing and internal penetrating disease behaviors and need for small bowel surgery[30,31]. Further reports have found that patients with Crohn’s disease who are positive for ASCA IgA, IgG, or both, may define a subset of patients with Crohn’s disease at increased risk for early surgery[32]. ASCA has also been shown to be associated with a more aggressive disease course among a cohort of pediatric CD patients[33]. More recently anti-OmpC and anti-I2 have also been shown, like ASCA, to be associated with complicated disease behaviors among adult and pediatric CD patients[12,13,34]. Anti-CBir1 has also been shown to be independently associated with complicated disease behaviors in adult CD patients[14]. Of interest is that these associations were not found in a pediatric CD cohort suggesting potential differences in the mechanistic influence of CBir1 in the pediatric age group[34].
These studies also demonstrated that both the number of immune responses to the different microbial antigens expressed by a given individual as well as the magnitude (titer level) of these immune responses correlated most significantly with the presence of complicated CD phenotypes[12,34] (Figures 1 and 2). In theory, higher levels of immune reactivity may reflect the degree of loss of tolerance to specific microbial antigens rather than a global loss of tolerance. This may translate clinically to the magnitude of effect that specific bacteria have on the degree and extent inflammation resulting in more aggressive disease behaviors. Studies have demonstrated that immune responses to microbial antigens had a stronger association with the presence of complicated disease behaviors than known susceptibility genotypes, such that NOD2 was independently associated with small bowel disease location only and not disease behavior, fibrostenosing disease in particular, as previously reported[35-39]. None of these earlier phenotype correlation studies, however, took into account the assessment of multiple immune phenotypes.
Figure 1.
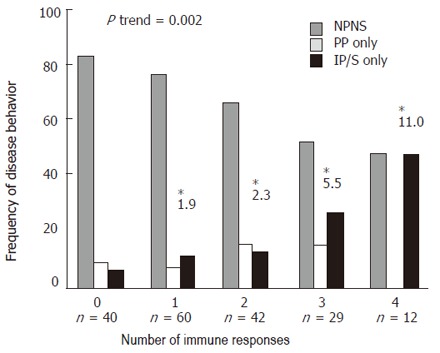
The frequency of disease behavior. The test for trend demonstrated a positive linear trend in the frequency of patients with IP and/or S disease as the number of positive immune responses toward I2, OmpC, ASCA and CBir1 increased (P = 0.002). The odds ratios (OR) reflect the odds of having internal penetrating and/or stricturing disease when positive for any 1, combination of 2, 3 or all 4 immune responses, as compared to those patients negative for all immune responses (baseline group).
Figure 2.

Association of the summed level of antibody responses towards multiple microbial antigens and disease phenotypes. Quartile sums used to reflect lowest (3) to highest titer level (12) for ASCA, anti-I2 and anti-OmpC.
IMMUNOGENETIC PHENOTYPES AND NATURAL HISTORY OF DISEASE
The prospective acquisition and determination of immune reactivity prior to the development of a disease complication is important to be able to truly evaluate the potential predictive value of immune responses in defining the natural history of IBD. It is generally agreed upon that the presence and level of immune responses do not change in a given CD patient[12,33]. We recently published the first prospective evaluation of the prognostic value of immune responses in patients presenting with non complicated CD[34]. This study included only those patients not presenting with internal penetrating and or stricturing disease at diagnosis and continued to be uncomplicated at the time sera was collected for immune response measurement so that it could be ascertained that the complication occurred after the antibodies were measured. Among those who developed a complication during the follow-up, the median time from diagnosis to the onset of the complication was 48 months. As of the last follow up of this cohort, 8% of the group seropositive to at least one serological marker had developed a complication vs only 3% in the seronegative group. Survival analysis (Figure 3) demonstrated that among those patients positive for at least one serology, more progressed to internal penetrating and or stricturing disease than those negative for all serologies. Saying it differently, those patients positive for at least one serology progressed faster that those negative for all serologies. Determining the factors that can predict the progression from uncomplicated to complicated disease states may stratify patients into at risk populations and impact the ultimate therapeutic management of patients with the goal of halting or more importantly preventing progression to complicated behaviors.
Figure 3.
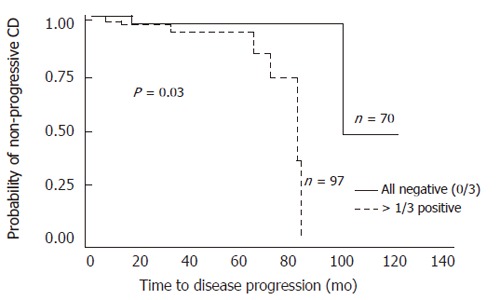
Kaplan Meier survival analysis. Comparison of time to progression from non-complicating to complicating disease behaviors between patients positive for 1 immune response to ASCA, I2 and OmpC (n = 97) (—) and those negative for all 3 (n = 70) (----).
FAMILIAL EXPRESSION OF IMMUNE PHENOTYPES
There has been interest in evaluating whether immune responses are familial traits due to genetic factors. ANCA expression was the first marker to be studied. Several studies have observed an increased frequency of pANCA in unaffected relatives of UC patients but not environmental controls[40,41]. This relationship however has not been observed in all studies[42,43]. Sutton et al demonstrated that the quantitative and qualitative expression of ASCA was familial[44]. Another study confirmed that ASCA occur particularly frequently in CD patients, especially with the presence of a positive family history. However, they are also significantly increased in UC patients with a family history and in a considerable number of unaffected relatives of inflammatory bowel disease families, irrespective of the characteristics of their families (UC, CD, mixed, ASCA positive, and ASCA negative). The presence of ASCA in unaffected relatives might point towards a genetic predisposition to either CD or UC[45]. Studies in a twin population demonstrated an agreement in ASCA titers within concordant monozygotic twin pairs with Crohn’s disease and suggested that the level of increase in ASCA reactivity(magnitude) is genetically determined[46]. None of these studies evaluated the influence of ASCA on the natural history of the affected offspring. A very recent study has shown that antibodies to OmpC have a strong familial aggregation pattern[47]. In this study, expression of anti-OmpC in unaffected family members of multiplex IBD families were compared with controls. As shown in Figure 4, unaffected family members in CD only families had a similar frequency of anti-OmpC to those in mixed families. However, when comparing these two groups with healthy controls, both of them showed a much higher frequency of anti-OmpC expression. In addition, unaffected family members in these two groups displayed a greater prevalence of anti-OmpC than those unaffected from UC only families. This study also addressed whether ASCA and OmpC were co-segregating in patients and unaffected relatives. The results however suggest that anti-OmpC and ASCA may represent related but distinct immune responses in CD patients. More importantly the distinct immune phenotypes may translate into distinct clinical phenotypes.
Figure 4.
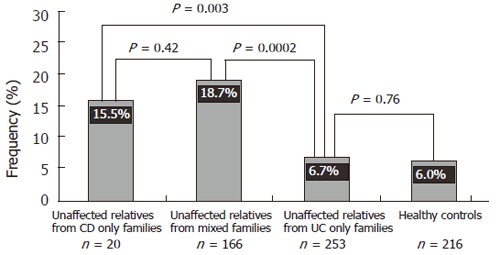
Frequency of anti-OmpC in unaffected relatives from CD only families, mixed families, UC only families, and healthy controls.
SUMMARY
In summary, the emergence of immunogenetic phenotypes lends support to the proposed hypothesis that susceptibility genes regulate distinct immune processes, driven by luminal antigens, expressed as specific immune phenotypes which in turn influence clinical phenotypes in IBD patients. Immune responses to various microbial antigens among patients with CD may be related to different pathophyisological mechanisms of disease and a genetically susceptible host may yield distinct disease characteristics as a result of the immune responsiveness expressed by the at risk individual. Further research is necessary to validate the associations of immune responses to disease behavior and prognosis and for novel immune responses to be identified so to provide more information on the underlying etiopathogenic mechanisms of characteristic of IBD. Advances in this field will afford clinicians the opportunity to create and implement appropriate and timely therapeutic management regimes based on the aggressiveness of the IBD subtype in order to alter and thus improve the long-term prognosis.
Footnotes
S- Editor Pan BR E- Editor Liu Y
References
- 1.Rath HC, Ikeda JS, Linde HJ, Schölmerich J, Wilson KH, Sartor RB. Varying cecal bacterial loads influences colitis and gastritis in HLA-B27 transgenic rats. Gastroenterology. 1999;116:310–319. doi: 10.1016/s0016-5085(99)70127-7. [DOI] [PubMed] [Google Scholar]
- 2.Rath HC, Wilson KH, Sartor RB. Differential induction of colitis and gastritis in HLA-B27 transgenic rats selectively colonized with Bacteroides vulgatus or Escherichia coli. Infect Immun. 1999;67:2969–2974. doi: 10.1128/iai.67.6.2969-2974.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SC, Tonkonogy SL, Albright CA, Tsang J, Balish EJ, Braun J, Huycke MM, Sartor RB. Variable phenotypes of enterocolitis in interleukin 10-deficient mice monoassociated with two different commensal bacteria. Gastroenterology. 2005;128:891–906. doi: 10.1053/j.gastro.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Duchmann R, May E, Heike M, Knolle P, Neurath M, Meyer zum Büschenfelde KH. T cell specificity and cross reactivity towards enterobacteria, bacteroides, bifidobacterium, and antigens from resident intestinal flora in humans. Gut. 1999;44:812–818. doi: 10.1136/gut.44.6.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sendid B, Colombel JF, Jacquinot PM, Faille C, Fruit J, Cortot A, Lucidarme D, Camus D, Poulain D. Specific antibody response to oligomannosidic epitopes in Crohn's disease. Clin Diagn Lab Immunol. 1996;3:219–226. doi: 10.1128/cdli.3.2.219-226.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ruemmele FM, Targan SR, Levy G, Dubinsky M, Braun J, Seidman EG. Diagnostic accuracy of serological assays in pediatric inflammatory bowel disease. Gastroenterology. 1998;115:822–829. doi: 10.1016/s0016-5085(98)70252-5. [DOI] [PubMed] [Google Scholar]
- 7.Quinton JF, Sendid B, Reumaux D, Duthilleul P, Cortot A, Grandbastien B, Charrier G, Targan SR, Colombel JF, Poulain D. Anti-Saccharomyces cerevisiae mannan antibodies combined with antineutrophil cytoplasmic autoantibodies in inflammatory bowel disease: prevalence and diagnostic role. Gut. 1998;42:788–791. doi: 10.1136/gut.42.6.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffenberg EJ, Fidanza S, Sauaia A. Serologic testing for inflammatory bowel disease. J Pediatr. 1999;134:447–452. doi: 10.1016/s0022-3476(99)70202-7. [DOI] [PubMed] [Google Scholar]
- 9.Landers CJ, Cohavy O, Misra R, Yang H, Lin YC, Braun J, Targan SR. Selected loss of tolerance evidenced by Crohn's disease-associated immune responses to auto- and microbial antigens. Gastroenterology. 2002;123:689–699. doi: 10.1053/gast.2002.35379. [DOI] [PubMed] [Google Scholar]
- 10.Cohavy O, Bruckner D, Gordon LK, Misra R, Wei B, Eggena ME, Targan SR, Braun J. Colonic bacteria express an ulcerative colitis pANCA-related protein epitope. Infect Immun. 2000;68:1542–1548. doi: 10.1128/iai.68.3.1542-1548.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beaven SW, Abreu MT. Biomarkers in inflammatory bowel disease. Curr Opin Gastroenterol. 2004;20:318–327. doi: 10.1097/00001574-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Mow WS, Vasiliauskas EA, Lin YC, Fleshner PR, Papadakis KA, Taylor KD, Landers CJ, Abreu-Martin MT, Rotter JI, Yang H, et al. Association of antibody responses to microbial antigens and complications of small bowel Crohn's disease. Gastroenterology. 2004;126:414–424. doi: 10.1053/j.gastro.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 13.Arnott ID, Landers CJ, Nimmo EJ, Drummond HE, Smith BK, Targan SR, Satsangi J. Sero-reactivity to microbial components in Crohn's disease is associated with disease severity and progression, but not NOD2/CARD15 genotype. Am J Gastroenterol. 2004;99:2376–2384. doi: 10.1111/j.1572-0241.2004.40417.x. [DOI] [PubMed] [Google Scholar]
- 14.Targan SR, Landers CJ, Yang H, Lodes MJ, Cong Y, Papadakis KA, Vasiliauskas E, Elson CO, Hershberg RM. Antibodies to CBir1 flagellin define a unique response that is associated independently with complicated Crohn's disease. Gastroenterology. 2005;128:2020–2028. doi: 10.1053/j.gastro.2005.03.046. [DOI] [PubMed] [Google Scholar]
- 15.Lodes MJ, Cong Y, Elson CO, Mohamath R, Landers CJ, Targan SR, Fort M, Hershberg RM. Bacterial flagellin is a dominant antigen in Crohn disease. J Clin Invest. 2004;113:1296–1306. doi: 10.1172/JCI20295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vidrich A, Lee J, James E, Cobb L, Targan S. Segregation of pANCA antigenic recognition by DNase treatment of neutrophils: ulcerative colitis, type 1 autoimmune hepatitis, and primary sclerosing cholangitis. J Clin Immunol. 1995;15:293–299. doi: 10.1007/BF01541319. [DOI] [PubMed] [Google Scholar]
- 17.Eggena M, Cohavy O, Parseghian MH, Hamkalo BA, Clemens D, Targan SR, Gordon LK, Braun J. Identification of histone H1 as a cognate antigen of the ulcerative colitis-associated marker antibody pANCA. J Autoimmun. 2000;14:83–97. doi: 10.1006/jaut.1999.0340. [DOI] [PubMed] [Google Scholar]
- 18.Cohavy O, Harth G, Horwitz M, Eggena M, Landers C, Sutton C, Targan SR, Braun J. Identification of a novel mycobacterial histone H1 homologue (HupB) as an antigenic target of pANCA monoclonal antibody and serum immunoglobulin A from patients with Crohn's disease. Infect Immun. 1999;67:6510–6517. doi: 10.1128/iai.67.12.6510-6517.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seibold F, Brandwein S, Simpson S, Terhorst C, Elson CO. pANCA represents a cross-reactivity to enteric bacterial antigens. J Clin Immunol. 1998;18:153–160. doi: 10.1023/a:1023203118100. [DOI] [PubMed] [Google Scholar]
- 20.Duerr RH, Targan SR, Landers CJ, Sutherland LR, Shanahan F. Anti-neutrophil cytoplasmic antibodies in ulcerative colitis. Comparison with other colitides/diarrheal illnesses. Gastroenterology. 1991;100:1590–1596. doi: 10.1016/0016-5085(91)90657-7. [DOI] [PubMed] [Google Scholar]
- 21.Proujansky R, Fawcett PT, Gibney KM, Treem WR, Hyams JS. Examination of anti-neutrophil cytoplasmic antibodies in childhood inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 1993;17:193–197. doi: 10.1097/00005176-199308000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Winter HS, Landers CJ, Winkelstein A, Vidrich A, Targan SR. Anti-neutrophil cytoplasmic antibodies in children with ulcerative colitis. J Pediatr. 1994;125:707–711. doi: 10.1016/s0022-3476(94)70061-3. [DOI] [PubMed] [Google Scholar]
- 23.Oberstadt K, Schaedel W, Weber M, Classen M, Deusch K. P-ANCA as a differential diagnostic marker in inflammatory bowel disease. Adv Exp Med Biol. 1995;371B:1313–1316. [PubMed] [Google Scholar]
- 24.Louis E, Collard A, Oger AF, Degroote E, Aboul Nasr El Yafi FA, Belaiche J. Behaviour of Crohn's disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49:777–782. doi: 10.1136/gut.49.6.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cosnes J, Cattan S, Blain A, Beaugerie L, Carbonnel F, Parc R, Gendre JP. Long-term evolution of disease behavior of Crohn's disease. Inflamm Bowel Dis. 2002;8:244–250. doi: 10.1097/00054725-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Smith BR, Arnott ID, Drummond HE, Nimmo ER, Satsangi J. Disease location, anti-Saccharomyces cerevisiae antibody, and NOD2/CARD15 genotype influence the progression of disease behavior in Crohn's disease. Inflamm Bowel Dis. 2004;10:521–528. doi: 10.1097/00054725-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Dubinsky MC, Ofman JJ, Urman M, Targan SR, Seidman EG. Clinical utility of serodiagnostic testing in suspected pediatric inflammatory bowel disease. Am J Gastroenterol. 2001;96:758–765. doi: 10.1111/j.1572-0241.2001.03618.x. [DOI] [PubMed] [Google Scholar]
- 28.Peeters M, Joossens S, Vermeire S, Vlietinck R, Bossuyt X, Rutgeerts P. Diagnostic value of anti-Saccharomyces cerevisiae and antineutrophil cytoplasmic autoantibodies in inflammatory bowel disease. Am J Gastroenterol. 2001;96:730–734. doi: 10.1111/j.1572-0241.2001.03613.x. [DOI] [PubMed] [Google Scholar]
- 29.Vasiliauskas EA, Plevy SE, Landers CJ, Binder SW, Ferguson DM, Yang H, Rotter JI, Vidrich A, Targan SR. Perinuclear antineutrophil cytoplasmic antibodies in patients with Crohn's disease define a clinical subgroup. Gastroenterology. 1996;110:1810–1819. doi: 10.1053/gast.1996.v110.pm8964407. [DOI] [PubMed] [Google Scholar]
- 30.Vasiliauskas EA, Kam LY, Karp LC, Gaiennie J, Yang H, Targan SR. Marker antibody expression stratifies Crohn's disease into immunologically homogeneous subgroups with distinct clinical characteristics. Gut. 2000;47:487–496. doi: 10.1136/gut.47.4.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klebl FH, Bataille F, Bertea CR, Herfarth H, Hofstädter F, Schölmerich J, Rogler G. Association of perinuclear antineutrophil cytoplasmic antibodies and anti-Saccharomyces cerevisiae antibodies with Vienna classification subtypes of Crohn's disease. Inflamm Bowel Dis. 2003;9:302–307. doi: 10.1097/00054725-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Forcione DG, Rosen MJ, Kisiel JB, Sands BE. Anti-Saccharomyces cerevisiae antibody (ASCA) positivity is associated with increased risk for early surgery in Crohn's disease. Gut. 2004;53:1117–1122. doi: 10.1136/gut.2003.030734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Desir B, Amre DK, Lu SE, Ohman-Strickland P, Dubinsky M, Fisher R, Seidman EG. Utility of serum antibodies in determining clinical course in pediatric Crohn's disease. Clin Gastroenterol Hepatol. 2004;2:139–146. doi: 10.1016/s1542-3565(03)00321-5. [DOI] [PubMed] [Google Scholar]
- 34.Dubinsky MC, Lin YC, Dutridge D, Picornell Y, Landers CJ, Farrior S, Wrobel I, Quiros A, Vasiliauskas EA, Grill B, et al. Serum immune responses predict rapid disease progression among children with Crohn's disease: immune responses predict disease progression. Am J Gastroenterol. 2006;101:360–367. doi: 10.1111/j.1572-0241.2006.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lesage S, Zouali H, Cézard JP, Colombel JF, Belaiche J, Almer S, Tysk C, O'Morain C, Gassull M, Binder V, et al. CARD15/NOD2 mutational analysis and genotype-phenotype correlation in 612 patients with inflammatory bowel disease. Am J Hum Genet. 2002;70:845–857. doi: 10.1086/339432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahmad T, Armuzzi A, Bunce M, Mulcahy-Hawes K, Marshall SE, Orchard TR, Crawshaw J, Large O, de Silva A, Cook JT, et al. The molecular classification of the clinical manifestations of Crohn's disease. Gastroenterology. 2002;122:854–866. doi: 10.1053/gast.2002.32413. [DOI] [PubMed] [Google Scholar]
- 37.Cuthbert AP, Fisher SA, Mirza MM, King K, Hampe J, Croucher PJ, Mascheretti S, Sanderson J, Forbes A, Mansfield J, et al. The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease. Gastroenterology. 2002;122:867–874. doi: 10.1053/gast.2002.32415. [DOI] [PubMed] [Google Scholar]
- 38.Abreu MT, Taylor KD, Lin YC, Hang T, Gaiennie J, Landers CJ, Vasiliauskas EA, Kam LY, Rojany M, Papadakis KA, et al. Mutations in NOD2 are associated with fibrostenosing disease in patients with Crohn's disease. Gastroenterology. 2002;123:679–688. doi: 10.1053/gast.2002.35393. [DOI] [PubMed] [Google Scholar]
- 39.Kugathasan S, Collins N, Maresso K, Hoffmann RG, Stephens M, Werlin SL, Rudolph C, Broeckel U. CARD15 gene mutations and risk for early surgery in pediatric-onset Crohn's disease. Clin Gastroenterol Hepatol. 2004;2:1003–1009. doi: 10.1016/s1542-3565(04)00452-5. [DOI] [PubMed] [Google Scholar]
- 40.Shanahan F, Duerr RH, Rotter JI, Yang H, Sutherland LR, McElree C, Landers CJ, Targan SR. Neutrophil autoantibodies in ulcerative colitis: familial aggregation and genetic heterogeneity. Gastroenterology. 1992;103:456–461. doi: 10.1016/0016-5085(92)90834-l. [DOI] [PubMed] [Google Scholar]
- 41.Seibold F, Slametschka D, Gregor M, Weber P. Neutrophil autoantibodies: a genetic marker in primary sclerosing cholangitis and ulcerative colitis. Gastroenterology. 1994;107:532–536. doi: 10.1016/0016-5085(94)90181-3. [DOI] [PubMed] [Google Scholar]
- 42.Lee JC, Lennard-Jones JE, Cambridge G. Antineutrophil antibodies in familial inflammatory bowel disease. Gastroenterology. 1995;108:428–433. doi: 10.1016/0016-5085(95)90070-5. [DOI] [PubMed] [Google Scholar]
- 43.Achkar JP, Barmada MM, Duerr RH. Perinuclear neutrophil antibodies are not markers for genetic susceptibility or indicators of genetic heterogeneity in familial ulcerative colitis. Am J Gastroenterol. 2002;97:2343–2349. doi: 10.1111/j.1572-0241.2002.05989.x. [DOI] [PubMed] [Google Scholar]
- 44.Sutton CL, Yang H, Li Z, Rotter JI, Targan SR, Braun J. Familial expression of anti-Saccharomyces cerevisiae mannan antibodies in affected and unaffected relatives of patients with Crohn's disease. Gut. 2000;46:58–63. doi: 10.1136/gut.46.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Annese V, Andreoli A, Andriulli A, Dinca R, Gionchetti P, Latiano A, Lombardi G, Piepoli A, Poulain D, Sendid B, et al. Familial expression of anti-Saccharomyces cerevisiae Mannan antibodies in Crohn's disease and ulcerative colitis: a GISC study. Am J Gastroenterol. 2001;96:2407–2412. doi: 10.1111/j.1572-0241.2001.04043.x. [DOI] [PubMed] [Google Scholar]
- 46.Halfvarson J, Standaert-Vitse A, Järnerot G, Sendid B, Jouault T, Bodin L, Duhamel A, Colombel JF, Tysk C, Poulain D. Anti-Saccharomyces cerevisiae antibodies in twins with inflammatory bowel disease. Gut. 2005;54:1237–1243. doi: 10.1136/gut.2005.066860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mei L, Targan SR, Landers CJ, Dutridge D, Ippoliti A, Vasiliauskas EA, Papadakis KA, Fleshner PR, Rotter JI, Yang H. Familial expression of anti-Escherichia coli outer membrane porin C in relatives of patients with Crohn's disease. Gastroenterology. 2006;130:1078–1085. doi: 10.1053/j.gastro.2006.02.013. [DOI] [PubMed] [Google Scholar]


