Abstract
AIM: To evaluate the frequency, clinical and paraclinical features of hepatopulmonary syndrome (HPS) and to determine their predictive values in diagnosis of this syndrome in patients in Iran.
METHODS: Fifty four cirrhotic patients underwent contrast enhanced echocardiography to detect intrapulmonary and intracardiac shunts by two cardiologists. Arterial blood oxygen, O2 gradient (A-a) and orthodoxy were measured by arterial blood gas (ABG) test. The patients positive for diagnostic criteria of HPS were defined as clinical HPS cases and those manifesting the intrapulmonary arterial dilation but no other criteria (arterial blood hypoxemia) were defined as lHPS cases. HPS frequency, sensitivity, positive and negative predictive values of clinical and paraclinical features were studied.
RESULTS: Ten (18.5%) and seven (13%) cases had clinical and subclinical HPS, respectively. The most common etiology was hepatitis B. Dyspnea (100%) and cyanosis (90%) were the most prevalent clinical features. Dyspnea and clubbing were the most sensitive and specific clinical features respectively. No significant relationship was found between HPS and splenomegaly, ascites, edema, jaundice, oliguria, and collateral veins. HPS was more prevalent in hepatitis B. PaO2 < 70 and arterial-alveolar gradient had the highest sensitivity in HPS patients. Orthodoxy specificity was 100%.
CONCLUSION: Clubbing with positive predictive value (PPV) of 75% and dyspnea with negative predictive value (NPV) of 75% are the best clinical factors in diagnosis of HPS syndrome. PaO2 < 70 and P (A-a) O2 > 30 and their sum, are the most valuable negative and positive predictive values in HPS patients.
Keywords: Hepatopulmonary syndrome, Cirrhosis, Contrast enhanced echocardiography
INTRODUCTION
Ascites by elevating the diaphragm and confounding the ventilation/perfusion might lead to mild hypoxemia in most patients due to chronic hepatic involvement, not regarding the etiology. When cirrhotic patients have no sign of any cardiovascular diseases, severe hypoxemia(PO2 < 60mmHg) strongly recommends hepatopulmonary syndrome[1-3]. Hepatopulmonary syndrome is one of the pulmonary complications of cirrhosis which affects the treatment and disease prognosis and is a factor for arterial blood oxygen reduction. The diagnosis of this syndrome is confirmed by presence of cirrhosis in liver biopsy, absence of cardiovascular diseases, arterial blood oxygen reduction found in arterial blood gas (ABG) tests and pulmonary vein dilation in imaging[4]. Many studies have been performed on evaluating the prevalence, etiology, clinical features, early diagnosis, treatment and prognosis of this syndrome worldwide. The aim of this study was to evaluate the clinical and paraclinical characteristics and their predictive values in diagnosis of this syndrome.
MATERIALS AND METHODS
This study was performed in 54 randomly chosen cirrhotic patients referred to Gasteroenterology Department of Taleghani Hospital in 2004. In the patients who entered the study, cirrhosis was confirmed by biopsy, clinical and paraclinical evaluations. Echocardiography and pulmonary function tests were done for all patients and plain chest x-ray was taken. Those with cardiovascular and known respiratory diseases were excluded from this study. The patients with ascites underwent large volume paracentesis. These 54 patients underwent contrast enhanced echocardiography performed by two cardiologists from Cardiovascular Department of Talaghani Hospital. The procedure was performed by injecting agitated saline into patient’s right hand cubital vein. Left and right sides of the heart were evaluated by echo after 5 beats. Presence of opacity after 5 beats in the left heart was determined as intrapulmonary shunt. If opacity was present immediately after injection, it was a sign of intracardiac shunt. ABG test was performed in patients at supine. After one hour in vertical position, the oxygenation saturation, arterial blood oxygen, (A-a) O2 gradient and orthodoxy were evaluated. Physical examination was performed to detect clinical features including clubbing in fingers and toes, central and peripheral cyanosis, presence of spider angioma, telangiectasia, jaundice, collateral veins in abdomen, ascites, consciousness, splenomegaly, dyspnea, peripheral edema, palmar erythema, oliguria or anuria and pleural effusion for the underlying etiology. All patients were tested for hepatitis B, hepatitis C, biliary, autoimmune, metabolic, cardiac, alcoholic and idiopathic etiologies. Complete blood count (CBC), liver function test (LFT), creatinine, prothrombin time (PT), partial thromboplastin time (PTT), albumin and other routine tests were measured in all patients. Ascitic fluid was tested for protein, albumin and white blood cells.
The patients presenting the three diagnostic criteria of hepatopulmonary syndrome, including hepatic cirrhosis, arterial blood deoxygenation (PO2 < 80 mmHg) and intrapulmonary arterial dilation were defined as clinical hepatopulmonary cases. Those presenting intrapulmonary arterial dilation but no other two criteria (arterial blood hypoxemia) were defined as subclinical hepatopulmonary cases. The study was carried out in accordance with the Helsinki Declaration and approved by the Ethics Committee of the Research Center for Gastroenterology and Liver Disease, Shaheed Beheshti University of Medical Sciences. The data were presented by descriptive statistics. The variables were compared by χ2 test. Sensitivity, specificity, positive and negative predictive values of clinical and paraclinical features in diagnosis of hepatopulmonary syndrome were evaluated. P < 0.05 was considered statistically significant.
RESULTS
Among the 54 patients who participated in the study, 10(18.5%) met the clinical hepatopulmonary syndrome criteria and 7(13%) with intrapulmonary arterial dilation (but no other criteria) were defined as subclinical hepatopulmonary cases. Most frequent age group was 71-80 years. Figure 1 shows the age distribution. The most common etiology was HBV, but there was no significant relation. Figure 2 shows the prevalence of HPS etiologies.
Figure 1.
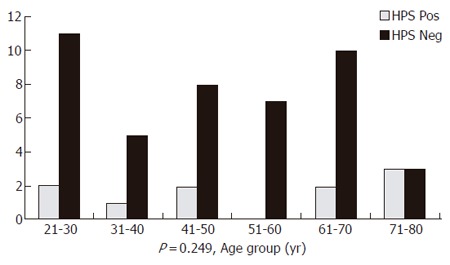
Age distribution in patients with hepatopulmonary syndrome.
Figure 2.
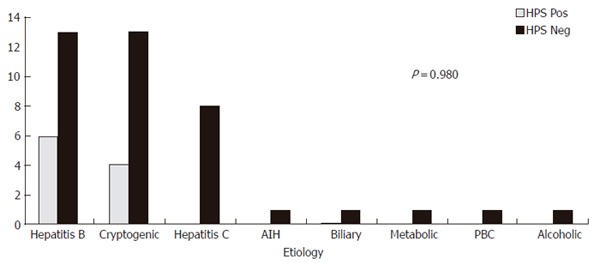
Causes of liver disease in patients with hepatopulmonary syndrome.
By paying attention to the frequency of clinical features in HPS patients, dyspnea (100%) and cyanosis (90%) were the most prevalent. Dyspnea and clubbing were the most sensitive and specific clinical features. Table 1 presents the characteristics and diagnostic values of signs and symptoms in HPS patients.
Table 1.
Characteristics and diagnostic values of signs and symptoms in hepatopulmonary syndrome
| Symptoms and signs |
Frequency
in HPS (%) |
Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | P | |
| Pos | Neg | ||||||
| Cyanosis | 90 | 15.9 | 90 | 80.1 | 60 | 97 | <0.0001 |
| Clubbing | 80 | 9.1 | 80 | 90.9 | 75 | 95 | <0.0001 |
| Dyspnea | 100 | 25 | 100 | 75 | 50 | 100 | <0.0001 |
| Palmar erythema | 80 | 29.5 | 80 | 70.5 | 38 | 94 | 0.003 |
| Spider angioma | 80 | 29.5 | 80 | 70.5 | 38 | 94 | 0.005 |
HPS: hepatopulmonary syndrome, PPV: positive predictive value, NPV: negative predictive value.
No significant relation was found between splenomegaly, ascites, edema, jaundice, oliguria, collateral veins and hepatopulmonary syndrome. Table 2 presents the patients with or without hepatopulmonary syndrome. HPS was more common in class C. Table 3 presents the diagnostic value of arterial blood gas in HPS. PaO2 and arterial–alveolar oxygen gradients were most sensitive in diagnosis of HPS. Orthodoxy specificity was 100%.
Table 2.
Child class in hepatopulmonary syndrome and subclinical patients
| Child classification | HPS positive | HPS negative | Total |
| Class A | 0 | 5 | 5 |
| Class B | 2 | 27 | 29 |
| Class C | 8 | 12 | 20 |
| Total | 10 | 44 | 54 |
Table 3.
Diagnostic value of arterial blood gases in hepatopulmonary syndrome
| Laboratory results |
Frequency
(%) |
Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | P | |
| Pos | Neg | ||||||
| Pa02 < 70 and (A-a)02>30 | 100 | 4.5 | 100 | 92 | 85 | 100 | < 0.0001 |
| Pa02 < 70 | 100 | 4.5 | 100 | 95 | 83 | 100 | < 0.0001 |
| a02 < 65 | 70 | 4.5 | 70 | 98 | 77 | 95 | < 0.0001 |
| Pa02 < 60 | 30 | 4.5 | 30 | 92 | 66 | 87 | 0.039 |
| (A-a)02>15 | 100 | 75 | 100 | 25 | 23 | 10 | 0.1 |
| (A-a)02>20 | 100 | 63.6 | 100 | 36 | 26 | 100 | 0.24 |
| (A-a)02>30 | 100 | 31.8 | 100 | 70 | 88 | 89 | 0.001 |
| (A-a)02>40 | 90 | 11.4 | 90 | 88 | 65 | 75 | < 0.0001 |
| Orthodoxy>10 | 60 | 0 | 60 | 100 | 15 | 93 | < 0.001 |
DISCUSSION
Hepatopulmonary syndrome includes the triad of liver disease, arterial blood deoxygenation and pulmonary vein dilation. Although the mortality of this syndrome is high, its influence on patient survival is unknown. In our study, the prevalence of hepatopulmonary syndrome was 18.5% and the prevalence of pulmonary vein dilation was 13%. Our findings are compatible with those of other studies in this field[1-5].
In our study, age and Child class C were significantly associated with HPS, suggesting that this syndrome is related with development of cirrhosis. Studies have shown a relation between HPS and cyanosis, clubbing and orthodoxy, although spider angioma is significantly related to intrapulmonary vein dilation[1]. The same results were observed in our study also. Cyanosis, clubbing and orthodoxy had positive and negative predictive values of 75% and 100% in hepatopulmonary syndrome.
Previous studies showed that the most common underlying etiologies of HPS were cryptogenic cirrhosis and cirrhosis due to hepatitis B[3,4]. The reported positive predictive values were 37% and 53% for (A-a) O2 gradients and 93% and 94% for PaO2[3,4]. Orthodoxy has been reported to be 88%, but in our study it was 66% and no significant statistical relation was found[6-7]. These clinical results strongly lead to diagnosis of HPS and the above tests can be used in screening patients.
In conclusion, hepatopulmonary syndrome and intrapulmonary vein dilation are relatively frequent in patients with portal hypertension. Clubbing with the highest positive predictive value (75%) and dyspnea with the highest negative predictive value (100%) are the best clinical features in HPS patients. Further studies are needed to confirm our results.
Footnotes
S- Editor Guo SY L- Editor Wang XL E- Editor Bi L
References
- 1.Lima BL, França AV, Pazin-Filho A, Araújo WM, Martinez JA, Maciel BC, Simões MV, Terra-Filho J, Martinelli AL. Frequency, clinical characteristics, and respiratory parameters of hepatopulmonary syndrome. Mayo Clin Proc. 2004;79:42–48. doi: 10.4065/79.1.42. [DOI] [PubMed] [Google Scholar]
- 2.Schenk P, Fuhrmann V, Madl C, Funk G, Lehr S, Kandel O, Müller C. Hepatopulmonary syndrome: prevalence and predictive value of various cut offs for arterial oxygenation and their clinical consequences. Gut. 2002;51:853–859. doi: 10.1136/gut.51.6.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hira HS, Kumar J, Tyagi SK, Jain SK. A study of hepatopulmonary syndrome among patients of cirrhosis of liver and portal hypertension. Indian J Chest Dis Allied Sci. 2003;45:165–171. [PubMed] [Google Scholar]
- 4.Anand AC, Mukherjee D, Rao KS, Seth AK. Hepatopulmonary syndrome: prevalence and clinical profile. Indian J Gastroenterol. 2001;20:24–27. [PubMed] [Google Scholar]
- 5.Schenk P, Schöniger-Hekele M, Fuhrmann V, Madl C, Silberhumer G, Müller C. Prognostic significance of the hepatopulmonary syndrome in patients with cirrhosis. Gastroenterology. 2003;125:1042–1052. doi: 10.1016/s0016-5085(03)01207-1. [DOI] [PubMed] [Google Scholar]
- 6.Mimidis KP, Vassilakos PI, Mastorakou AN, Spiropoulos KV, Lambropoulou-Karatza CA, Thomopoulos KC, Tepetes KN, Nikolopoulou VN. Evaluation of contrast echocardiography and lung perfusion scan in detecting intrapulmonary vascular dilatation in normoxemic patients with early liver cirrhosis. Hepatogastroenterology. 1998;45:2303–2307. [PubMed] [Google Scholar]
- 7.Aller R, Moya JL, Moreira V, Boixeda D, Cano A, Picher J, García-Rull S, de Luis DA. Diagnosis of hepatopulmonary syndrome with contrast transesophageal echocardiography: advantages over contrast transthoracic echocardiography. Dig Dis Sci. 1999;44:1243–1248. doi: 10.1023/a:1026657114256. [DOI] [PubMed] [Google Scholar]


