Abstract
Cyproterone acetate (CPA) is a steroidal synthetic progestagen and anti-androgenic compound widely administered in prostate cancer which has been evidentially correlated with a severe hepatotoxic potency. Three male patients aged 78-83 years are presented, in whom severe hepatotoxic reactions emerged after CPA administration. Patients were treated with CPA at the doses of 200-300 mg/d for malignant prostate disease for 3-12 mo prior to the acute manifestation of the hepatic disease. Clinical features compatible with mixed hepatocellular and cholestatic liver disease including jaundice, white stools and dark urine, manifested in all three cases whereas encephalopathy and ascites were present in two of the patients. Other primary causes of hepatotoxicity (alcohol consumption and viral hepatitis) were also verified in two cases, and in those patients biopsy findings revealed the presence of cirrhotic lesions in liver parenchyma. Discontinuation of the therapeutic agent led to the amelioration of the clinical profile in all the patients whereas a patient died 40 d after hospital admission due to sepsis, despite acute liver disease improvement. The current article highlights the hepatotoxic potency of a widely administered therapeutic agent and illustrates the importance of clinical surveillance especially in patients with previous hepatic diseases. Three relevant cases are reported and a review of the published literature is made.
Keywords: Cyproterone acetate, Drug induced hepatotoxicity, Prostate cancer, Idiosyncratic drug reaction, Hepatomitogen action
INTRODUCTION
Androgen deprivation therapy in the form of either orchiectomy or treatment with endogenous estrogens or luteinizing hormone releasing hormone (LHRH) analogues alone or coupled with antiandrogens, produces regression of prostate cancer cells through suppression of serum testosterone levels, and is on that ground regarded as an effective adjuvant therapeutic option. Cyproterone acetate (CPA) is a steroidal synthetic progestagen and antiandrogenic compound widely administered not only in prostate cancer but also in breast cancer, severe acne, female hirsutism, precocious puberty, hyper sexuality and sexual deviation in men. CPA inhibits the peripheral actions of testosterone and suppresses gonadotropin secretion by maintaining the negative feedback on the pituitary. Hepatotoxicity is a serious adverse reaction potentially induced by both steroidal and nonsteroidal antiandrogens. The first case of CPA-induced fulminant hepatitis with a fatal outcome was described in 1989[1]. A variety of hepatotoxic reactions have been documented in the literature including immunoallergic cytotoxic reactions[2], cholestasis, autoimmune hepatitis[3], acute hepatitis[4-10] fulminant hepatic failure[1,2,11-17] cirrhosis[18] and finally CPA has been attributed a hepatocellular mutagenic potency leading to hepatocarcinogenesis[8,19-27]. Clinical features include jaundice, fatigue, nausea, elevated serum levels of liver enzymes, different types of necrosis (bridging, confluent, and centrilobular), inflammation and features of hepatic decompensation[19]. This article highlights the hepatotoxic potency of a widely administered therapeutic agent and illustrates the importance of clinical surveillance. Three relevant cases are presented and a review of the published literature is made.
We searched the database PubMed (1995-2005) using the following key words: “cyproterone acetate hepatotoxicity”, “drug induced hepatotoxicity”. We also included review articles, book chapters, or commonly referenced publications. We reviewed the reference lists of articles identified by the search strategy and selected those we judged relevant. The search was restricted to papers published in English.
CASE REPORT
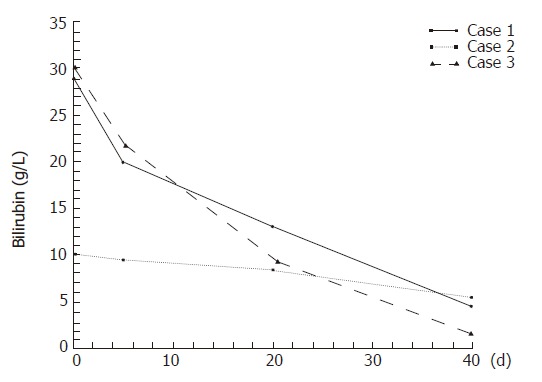
Three male patients aged 78-83 years with clinical features compatible with mixed hepatocellular and cholestatic liver diseases, including jaundice, white stools and dark urine were admitted to Hippocration University Hospital of Athens. Clinical manifestations including encephalopathy (Case 2) and ascites were documented in two of the patients (Case 1 and 2) (Table 1). The main characteristics of patients, as well as the values of bilirubin, aspartate (AST) and alanine aminotransferase (ALT), International Normalized Ratio (INR), albumin, and alkaline phosphatase (ALP) at the time of admission are depicted in Table 1. All three patients had been administered cyproterone acetate for 3-12 mo for prostate cancer without metastasis, at a dose ranging from 200-300 mg/d. Extensive clinical evaluation and exclusion of other potential hepatotoxic causes were performed. No serological evidence of recent acute viral hepatic infection was verified whereas in Case 3, pre-existing chronic inactive hepatitis B virus infection was justified based on compatible serological findings (hepatitis B virus surface (HBs) antigen was positive and hepatitis B virus DNA negative by hybridization assay). In addition, a history of excessive alcohol consumption was documented in Case 1. Autoimmunity markers were negative and no evidence of tumor in the liver or pelvis was seen on the computer tomography scan. Yet the presence of cirrhotic lesions was verified in Cases 1 and 3 on tomography. Liver biopsy was performed in all three Cases (Figure 1). In Cases 1 and 3, cirrhosis with fibrosis and loss of the normal lobular architecture were revealed and attributed to chronic hepatitis B and alcohol consumption. In all three cases, hepatocellular degeneration with ballooning of hepatocytes, portal and lobular inflammation and marked cholestasis with bile plugs were also demonstrated. Discontinuation of the therapeutic agent led to the restoration of the pathological clinical profile in Cases 1 and 3 whereas this was not accomplished in the second patient who died 40 d after hospital admission, due to sepsis, despite acute liver disease improvement. (Figures 2 and 3).
Table 1.
Patients’ laboratory values
| Case | Age (yr) | Use of cyproterone acetate (mo) | Daily dose (mg) | Bilirubin (total/direct, g/L)1 | AST/ALT (IU/L)2 | Alkaline phospatase (IU/L)3 | Albumin (g/L)4 | INR5 |
| 1 | 82 | 12 | 200 | 29.5/18.4 | 935/535 | 300 | 3.9 | 1.4 |
| 2 | 83 | 7 | 300 | 10.1/9.2 | 721/283 | 350 | 4 | 2.24 |
| 3 | 78 | 3 | 300 | 30.0/25.3 | 505/320 | 380 | 4.2 | 1.2 |
Normal values (total) < 1.2 g/L, normal values (direct) < 0.4 g/L;
Normal values < 40 IU/L;
Normal values < 133 IU/L;
Normal values > 3.5 g/L;
Normal values < 1.2
Figure 1.
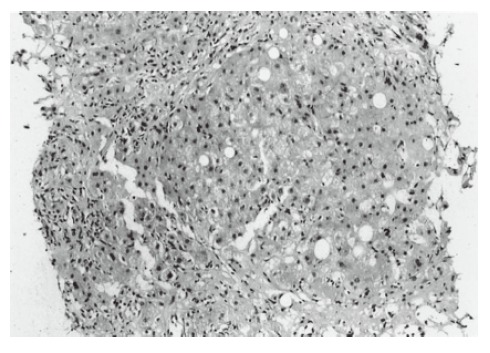
Hepatocellular degeneration, with ballooning of hepatocytes, portal and lobular inflammation and marked cholestasis with bile plugs were demonstrated in liver biopsy findings (liver biopsy from case 2).
Figure 2.

Serum aspartate aminotransferase levels following withdrawal of cyproterone acetate.
Figure 3.
Serum total bilirubin levels following withdrawal of cyproterone acetate.
DISCUSSION
The diagnosis of drug-induced hepatotoxicity is usually based on exclusion of other possible causes of hepatic dysfunction and on the temporal association between drug administration and the onset of liver disease while liver biopsy may allow a correct diagnosis[28,29]. Toxic hepatitis in our patients appeared to be causally related to the administration of cyproterone acetate based on a temporal relationship, negative serology for acute viral infection, negative autoantibody markers and exclusion of drugs or other potentially hepatotoxic agents. Proof is not possible in the absence of the rechallenge for ethical reasons. Pathophysiology of CPA-induced hepatotoxicity remains largely hypothetical. The histological features fit with an idiosyncratic reaction to the drug or its metabolites, or possibly an immunologically mediated reaction[2]. In many cases, a direct drug or metabolite effect is implied attributed to the hepatomitogen action of cyproterone, causing an increase of hepatocytes expressing placental glutathione S-transferase, which are considered preneoplastic elements[30-31]. The combination of Transforming Growth Factor-beta 1 (TGF) expression coupled with a strikingly enhanced sensitivity to the induction of apoptosis might be responsible for both the liver damage and the development of liver tumors observed after CPA supplementation since CPA shortens the lag phase of induction of apoptosis by shifting hepatocytes to a point before S phase, where they are highly susceptible to TGF-beta 1-induced apoptosis[19,32].
Hinkel et al[33] have conducted a retroprospective analysis of 89 patients who received cyproterone acetate for 4 years (50mg/d po range, 2-152 mo) for prostate cancer. Elevated liver enzymes were documented in 28.2% of the patients, yet CPA-induced liver toxicity and carcinogenesis were implied to be totally irrelevant considering the life expectancy of patients with advanced prostate cancer and the high-dose exposure of CPA required to possibly induce liver malignancies. Since then several large series have assessed the same issue with yet controversial results. In 1996, a retrospective study was conducted in 2506 patients receiving CPA (18-136 mg/d for less than 47.5 mo/patient) and a correlation with hepatocarcinogenesis could not be established. And 9.6% of the patients eventually presented with pathological liver profile, yet discontinuation of the therapeutic agent was not regarded necessary in any case[8]. Lin et al[34] assessed 229 patients by retrospective chart review submitted in orchiectomy or LHRH analogues plus antiandrogen for prostate cancer. In 105 patients administered with CPA (150 mg/d), hepatotoxity rates were 9.5%. Serious hepatic injury was documented in 3.8% (4/105) of the patients, mean latency period of hepatotoxity was estimated to be 5.8 ± 1.9 mo and in 9 out of 10 patients CPA-induced hepatotoxity got self resolution after discontinuation of the antiandrogen in an average period of 6.3 ± 4.7 mo[34]. In another study, patients with a preexisting chronic viral hepatitis were recognized as having a higher risk of developing antiandrogen hepatotoxicity[35]. Finally in a series assessing predictive utility of several clinical features, both age and therapeutic indication or the dose prescribed failed to depict with significant accuracy, those patients at risk for presenting hepatic disorders[36].
In the three cases of severe CPA-induced hepatotoxi-city presented in this article patients were administered with CPA at the doses of 200-300 mg/d for malignant prostate disease for 3-12 mo prior to the manifestation of hepatic disease. In two of the patients, other primary causes of hepatotoxicity (excessive alcohol consumption and viral hepatitis) were also verified and in those patients, biopsy findings revealed the presence of cirrhotic lesions in liver parenchyma along with acute cholestatic hepatitis. Discontinuation of the therapeutic agent resulted in the amelioration of the hepatic injury in all the patients whereas Case 2 died 40 d after hospital admission from sepsis.
Eleven cases assessing CPA-induced fulminant hepatic failure are presented in the literature[1,2,11-17]. According to Friedman et al[13] adverse hepatic reactions occurred more commonly in elderly patients (range, 65-92 years) with malignant diseases who were treated with high doses (range, 100-300 mg) for a prolonged period. Fulminant hepatic failure developed a few weeks to several months after initiation of therapy (range, 2-15 mo). On admission, aminotransferases were 3-27 times that of normal, and a markedly elevated bilirubin of 9-30 times higher than normal were also documented, but the ALP was usually 2 times lower than normal. Clinical features of hepatotoxicity initially included nausea, anorexia and malaise; however, a progressive jaundice eventually ensued. The duration from the onset of jaundice to death was 2-7 wk[13]. Beside acute liver failure, a less severe hepatic reaction can emerge on the ground of CPA-administration. Eight cases of acute hepatitis complicating CPA-treatment have been documented in the literature[4-10]. Doses of 100-150 mg/d are correlated with mild hepatotoxic reactions, mainly elevated transaminase levels, whereas an association between the duration of CPA-treatment and the prevalence of liver enzymes could not be established[8]. Latency before the onset of hepatocellular carcinoma and cirrhosis after CPA therapy is estimated up to several years. Preexisting viral, metabolic, drug-induced or alcoholic liver diseases are found correlated with the development of more severe hepatotoxic reactions. Discontinuation of the antiandrogens results in the resolution of hepatotoxicity. A change to other antiandrogen may be the alternative strategy to CPA-induced hepatic injury although controversy exists upon that issue[9]. After the withdrawal of the causative agent, hepatocellular recovery is achieved within 2-3 mo[19]. Fourteen case reports involving CPA-induced hepatotoxicity are reviewed with regard to the patient’s age, dose of CPA, latency before the onset of jaundice and duration between onset of jaundice and death[13,36] (Table 2). Descriptive statistics including means, medians and standard deviations were calculated, and are displayed in Table 2. Age and CPA doses were plotted in correlation with mortality (Figure 4). Relevant statistics were calculated and no statistically significant correlation was demonstrated between age and doses of CPA and the clinical outcome (death or survival) (P = 0.241 and P = 0.789 for CPA doses and age, respectively; not significant).
Table 2.
CPA-induced hepatotoxicity: review of 14 cases
| Reference | Age (yr) | Liver injury | Doses (mg) | Latency (mo) | Duration1(wk) |
| Levesque[1] | 78 | ALF | 200 | 6 | 2 |
| Parys[11] | 65 | ALF | 300 | 12 | 7 |
| Parys[11] | 83 | ALF | 300 | 15 | 2 |
| Bressollette[16] | 79 | ALF | 300 | 10 | 2 |
| Hirsch[14] | 92 | ALF | 100 | 4 | 5 |
| Murphy[2] | 73 | ALF | 100 | 4 | Alive |
| Lombardi[15] | 84 | ALF | 1 | ||
| Friedmann[13] | 81 | ALF | 300 | 6 | 7 |
| Friedmann[13] | 66 | ALF | 300 | 2 | 4 |
| Giordano[10] | 87 | AH | 300 | Alive | |
| Manolakopoulos[9] | 76 | AH | 150 | 7 | Alive |
| Savidou | 82 | AH | 200 | 12 | Alive |
| Savidou | 83 | AH | 300 | 7 | 6 |
| Savidou | 78 | AH | 300 | 3 | Alive |
| Mean | 79.1 | 242.3 | 7.3 | 4 | |
| Median | 80 | 300 | 6.5 | 4 | |
| SD | 7.4 | 81.2 | 4 | 2.3 |
Duration between onset of jaundice and death; ALF: Acute liver failure; AH: Acute hepatitis.
Figure 4.
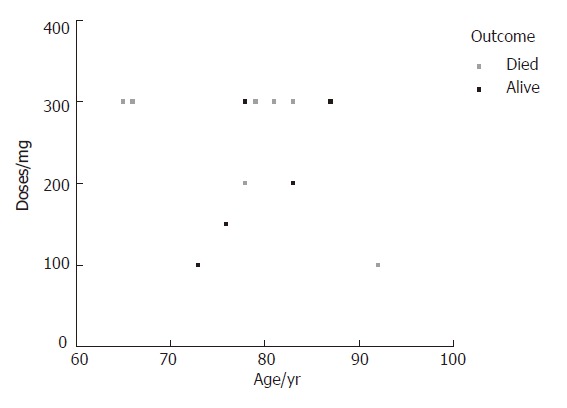
Scatter plot graphed for patient death events in correlation with patient’s age and CPA-doses administered (Table 2).
In conclusion,the aim of this report and review of the literature is to underline the potential hepatotoxicity effect of CPA, which may prove fatal in some cases. Close monitoring of liver function tests is recommended, particularly on the setting of a pre-existing liver disease for which increased risk rate has been implied.
Footnotes
S- Editor Wang J L- Editor Ma JY E- Editor Lu W
References
- 1.Lévesque H, Trivalle C, Manchon ND, Vinel JP, Moore N, Hémet J, Courtois H, Bercoff E, Bourreille J. Fulminant hepatitis due to cyproterone acetate. Lancet. 1989;1:215–216. doi: 10.1016/s0140-6736(89)91225-7. [DOI] [PubMed] [Google Scholar]
- 2.Murphy BJ, Collins BJ. Severe hepatitis and liver failure induced by cyproterone acetate. Aust N Z J Med. 1996;26:724. doi: 10.1111/j.1445-5994.1996.tb02956.x. [DOI] [PubMed] [Google Scholar]
- 3.Kacar S, Akdogan M, Koşar Y, Parlak E, Sasmaz N, Oguz P, Aydog G. Estrogen and cyproterone acetate combination-induced autoimmune hepatitis. J Clin Gastroenterol. 2002;35:98–100. doi: 10.1097/00004836-200207000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Drakos PE, Gez E, Catane R. Hepatitis due to cyproterone acetate. Eur J Cancer. 1992;28A:1931–1932. doi: 10.1016/0959-8049(92)90041-y. [DOI] [PubMed] [Google Scholar]
- 5.Roila F, Crinò L, Carloni G, Natalini G. Cyproterone acetate: hepatotoxicity and prostatic cancer treatment. Ann Oncol. 1993;4:701. doi: 10.1093/oxfordjournals.annonc.a058631. [DOI] [PubMed] [Google Scholar]
- 6.Blake JC, Sawyerr AM, Dooley JS, Scheuer PJ, McIntyre N. Severe hepatitis caused by cyproterone acetate. Gut. 1990;31:556–557. doi: 10.1136/gut.31.5.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meijers WH, Willemse PH, Sleijfer DT, Mulder NH, Grond J. Hepatocellular damage by cyproterone acetate. Eur J Cancer Clin Oncol. 1986;22:1121–1122. doi: 10.1016/0277-5379(86)90017-9. [DOI] [PubMed] [Google Scholar]
- 8.Heinemann LA, Will-Shahab L, van Kesteren P, Gooren LJ. Safety of cyproterone acetate: report of active surveillance. Pharmacoepidemiol Drug Saf. 1997;6:169–178. doi: 10.1002/(SICI)1099-1557(199705)6:3<169::AID-PDS263>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 9.Manolakopoulos S, Bethanis S, Armonis A, Economou M, Avgerinos A, Tzourmakliotis D. Toxic hepatitis after sequential administration of flutamide and cyproterone acetate. Dig Dis Sci. 2004;49:462–465. doi: 10.1023/b:ddas.0000020504.41500.9c. [DOI] [PubMed] [Google Scholar]
- 10.Giordano N, Nardi P, Santacroce C, Geraci S, Gennari C. Acute hepatitis induced by cyproterone acetate. Ann Pharmacother. 2001;35:1053–1055. doi: 10.1177/106002800103500902. [DOI] [PubMed] [Google Scholar]
- 11.Parys BT, Hamid S, Thomson RG. Severe hepatocellular dysfunction following cyproterone acetate therapy. Br J Urol. 1991;67:312–313. doi: 10.1111/j.1464-410x.1991.tb15142.x. [DOI] [PubMed] [Google Scholar]
- 12.Castellani P, Bernardini D, Renou C, Zamora C, Portal I, Gauthier A, Botta-Fridlund D. [Fatal sub-fulminant hepatitis caused by cyproterone acetate. A new case] Gastroenterol Clin Biol. 1996;20:915–916. [PubMed] [Google Scholar]
- 13.Friedman G, Lamoureux E, Sherker AH. Fatal fulminant hepatic failure due to cyproterone acetate. Dig Dis Sci. 1999;44:1362–1363. doi: 10.1023/a:1026639432428. [DOI] [PubMed] [Google Scholar]
- 14.Hirsch D, Kovatz S, Bernheim J, Shenkman L. Fatal fulminant hepatitis from cyproterone acetate. Isr J Med Sci. 1994;30:238–240. [PubMed] [Google Scholar]
- 15.Lombardi A, Ferrazza P, Castaldi F, Covotta L, Tesoriere A, Urbano V, Midiri G. [Acute hepatic necrosis in a patient treated with cyproterone acetate] G Chir. 1998;19:161–163. [PubMed] [Google Scholar]
- 16.Bressollette L, Dubois A, Carlhant D, Morand C, Mottier D, Riche C. [Fatal hepatitis caused by cyproterone acetate] Therapie. 1994;49:153. [PubMed] [Google Scholar]
- 17.Antoni M, Bourlière M, Toullec J, Maillot A, Botta-Fridlund D, Gauthier A. [Fatal subfulminant hepatitis caused by cyproterone acetate] Gastroenterol Clin Biol. 1991;15:772–773. [PubMed] [Google Scholar]
- 18.Garty BZ, Dinari G, Gellvan A, Kauli R. Cirrhosis in a child with hypothalamic syndrome and central precocious puberty treated with cyproterone acetate. Eur J Pediatr. 1999;158:367–370. doi: 10.1007/s004310051093. [DOI] [PubMed] [Google Scholar]
- 19.Oberhammer F, Nagy P, Tiefenbacher R, Fröschl G, Bouzahzah B, Thorgeirsson SS, Carr B. The antiandrogen cyproterone acetate induces synthesis of transforming growth factor beta 1 in the parenchymal cells of the liver accompanied by an enhanced sensitivity to undergo apoptosis and necrosis without inflammation. Hepatology. 1996;23:329–337. doi: 10.1002/hep.510230220. [DOI] [PubMed] [Google Scholar]
- 20.Brambilla G, Martelli A. Are some progestins genotoxic liver carcinogens. Mutat Res. 2002;512:155–163. doi: 10.1016/s1383-5742(02)00047-9. [DOI] [PubMed] [Google Scholar]
- 21.Kasper P. Cyproterone acetate: a genotoxic carcinogen. Pharmacol Toxicol. 2001;88:223–231. [PubMed] [Google Scholar]
- 22.Manfredi S, Lenfant L, Gresset AC, Bonnotte B, Lorcerie B, Chauffert B. [Hepatocellular carcinoma in a healthy liver possibly due to long-term use of cyproterone acetate] Presse Med. 2000;29:1983. [PubMed] [Google Scholar]
- 23.Watanabe S, Cui Y, Tanae A, Tanaka T, Fujimoto M, Matsuo Y, Tachibana K, Yamasaki S. Follow-up study of children with precocious puberty treated with cyproterone acetate. Ad hoc Committee for CPA. J Epidemiol. 1997;7:173–178. doi: 10.2188/jea.7.173. [DOI] [PubMed] [Google Scholar]
- 24.Ohri SK, Gaer JA, Keane PF. Hepatocellular carcinoma and treatment with cyproterone acetate. Br J Urol. 1991;67:213. doi: 10.1111/j.1464-410x.1991.tb15113.x. [DOI] [PubMed] [Google Scholar]
- 25.Kattan J, Spatz A, Culine S, Terrier-Lacombe MJ, Elias D, Droz JP. Hepatocellular carcinoma during hormonotherapy for prostatic cancer. Am J Clin Oncol. 1994;17:390–392. doi: 10.1097/00000421-199410000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Watanabe S, Yamasaki S, Tanae A, Hibi I, Honna T. Three cases of hepatocellular carcinoma among cyproterone users. Ad hoc Committee on Androcur Users. Lancet. 1994;344:1567–1568. doi: 10.1016/s0140-6736(94)90373-5. [DOI] [PubMed] [Google Scholar]
- 27.Rüdiger T, Beckmann J, Queisser W. Hepatocellular carcinoma after treatment with cyproterone acetate combined with ethinyloestradiol. Lancet. 1995;345:452–453. doi: 10.1016/s0140-6736(95)90434-4. [DOI] [PubMed] [Google Scholar]
- 28.Lee WM. Drug-induced hepatotoxicity. N Engl J Med. 2003;349:474–485. doi: 10.1056/NEJMra021844. [DOI] [PubMed] [Google Scholar]
- 29.Kaplowitz N. Drug-induced liver injury. Clin Infect Dis. 2004;38 Suppl 2:S44–S48. doi: 10.1086/381446. [DOI] [PubMed] [Google Scholar]
- 30.Fasciati R, Maier P. EGF- and CPA-induced mitogenic stimuli are differentially down-regulated by TGF-beta1 in cultured rat hepatocytes. Carcinogenesis. 1997;18:911–917. doi: 10.1093/carcin/18.5.911. [DOI] [PubMed] [Google Scholar]
- 31.Löw-Baselli A, Hufnagl K, Parzefall W, Schulte-Hermann R, Grasl-Kraupp B. Initiated rat hepatocytes in primary culture: a novel tool to study alterations in growth control during the first stage of carcinogenesis. Carcinogenesis. 2000;21:79–86. doi: 10.1093/carcin/21.1.79. [DOI] [PubMed] [Google Scholar]
- 32.Oberhammer FA, Qin HM. Effect of three tumour promoters on the stability of hepatocyte cultures and apoptosis after transforming growth factor-beta 1. Carcinogenesis. 1995;16:1363–1371. doi: 10.1093/carcin/16.6.1363. [DOI] [PubMed] [Google Scholar]
- 33.Hinkel A, Berges RR, Pannek J, Schulze H, Senge T. Cyproterone acetate in the treatment of advanced prostatic cancer: retrospective analysis of liver toxicity in the long-term follow-up of 89 patients. Eur Urol. 1996;30:464–470. doi: 10.1159/000474216. [DOI] [PubMed] [Google Scholar]
- 34.Lin AD, Chen KK, Lin AT, Chang YH, Wu HH, Kuo JY, Huang WJ, Hsu YS, Chung HJ, Chang LS. Antiandrogen-associated hepatotoxicity in the management of advanced prostate cancer. J Chin Med Assoc. 2003;66:735–740. [PubMed] [Google Scholar]
- 35.Pu YS, Liu CM, Kao JH, Chen J, Lai MK. Antiandrogen hepatotoxicity in patients with chronic viral hepatitis. Eur Urol. 1999;36:293–297. doi: 10.1159/000020007. [DOI] [PubMed] [Google Scholar]
- 36.Thole Z, Manso G, Salgueiro E, Revuelta P, Hidalgo A. Hepatotoxicity induced by antiandrogens: a review of the literature. Urol Int. 2004;73:289–295. doi: 10.1159/000081585. [DOI] [PubMed] [Google Scholar]


