Abstract
Liver biopsy is generally considered a safe and highly useful procedure. It is frequently performed in an outpatient setting for diagnosis and follow-up in numerous liver disorders. Since its introduction at the end of the 19th century, broad experience, new imaging techniques and special needles have significantly reduced the rate of complications associated with liver biopsy. Known complications of percutaneous biopsy of the liver include hemoperitoneum, subcapsular hematoma, hypotension, pneumothorax and sepsis. Other intra-abdominal complications are less common. Hemobilia due to arterio-biliary duct fistula has been described, which has only rarely been clinically expressed as cholecystitis or pancreatitis. We report a case of a fifteen year-old boy who developed severe acute cholecystitis twelve days after a percutaneous liver biopsy performed in an outpatient setting. The etiology was clearly demonstrated to be hemobilia-associated, and the clinical course required the performance of a laparoscopic cholecystectomy. The post operative course was uneventful and the patient was discharged home. Percutaneous liver biopsy is a safe and commonly performed procedure. However, severe complications can occasionally occur. Both medical and surgical options should be evaluated while dealing with these rare incidents.
Keywords: Hemobilia, Liver biopsy, Cholecystitis
INTRODUCTION
The increasing clinical need for liver biopsies as well as the availability of imaging assistance have changed the nature of this procedure. A previously hazardous intervention requiring hospitalization has changed to a common, easy and safe one.
However, complications of percutaneous biopsy of the liver do occur. Hemoperitoneum, pneumothorax, sub-capsular hematoma, hypotension and sepsis have been previously documented. Hemobilia due to arterio-biliary duct fistula has been reported as well. Rarely, clinical manifestations such as cholecystitis or pancreatitis subsequently evolve.
CASE REPORT
An asymptomatic 15-year old boy presented with persistently elevated liver enzymes initially discovered on routine blood chemistries. History and physical examination revealed an athletic, healthy-appearing young man. He underwent percutaneous liver biopsy to evaluate the possible diagnosis of cryptogenic cirrhosis. The procedure was uneventful and he was discharged on the same day. The biopsy was non-diagnostic.
Twelve days later he presented to the emergency department (ED) complaining of nausea, vomiting and abdominal pain focusing in the right upper quadrant. No fever was noted and he did not appear to be jaundiced. His abdomen was soft, with mild right upper quadrant abdominal tenderness. Blood analysis showed: WBC 14.5 × 103/μL, total bilirubin 1.8 mg/dL, ALT/AST 54/26 U/L, amylase 60 U/L. An ultrasound (US) was performed showing a large blood clot in the gall bladder. There was no thickening of the gall bladder wall and no peri-cholecystic fluid evident on the US examination.
He was discharged home but returned to the ED two days later with similar complaints and physical findings. The US was repeated and the same finding was evident (Figure 1). At this time his white blood cell count was 19.5 × 103/μL, total bilirubin 2.6 mg/dL, ALT/AST 238/74 U/L.
Figure 1.
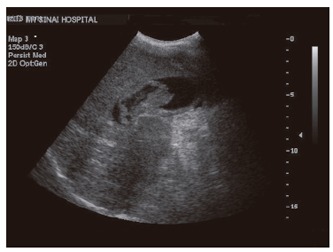
Ultra-sonography of the abdomen showing distended gall bladder containing large blood clot.
Intravenous antibiotics were started, and the following day laparoscopy was performed, revealing a severely acutely inflamed gall bladder and gross evidence of macro- and micro-nodular cirrhosis. Intraoperative cholangiography (IOC) revealed a normal extrahepatic duct system and mildly dilated intrahepatic ducts (Figure 2). Laparoscopic cholecystectomy and liver biopsy were performed. The gall bladder specimen revealed severe wall-thickening, and a thrombus cast of the gall bladder was found within (Figure 3). Liver biopsy revealed end stage liver disease characterized by cirrhosis and marked expansion of portal ducts (Figure 4). The patient recovered uneventfully and was discharged home on postoperative day two.
Figure 2.
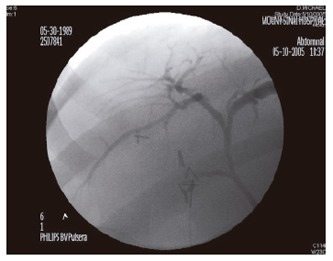
Intra-operative cholangiogram with normal appearing anatomy.
Figure 3.
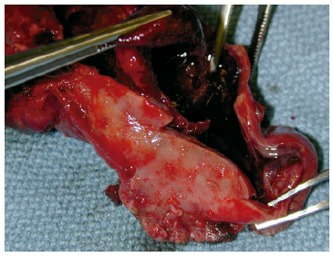
The opened specimen revealing a blood clot.
Figure 4.

Hemtoxilin & eosin stain of the liver sampled from the case.
DISCUSSION
Since liver biopsy was introduced at the end of the 19th century[1], broad experience has been gained in performing this essential procedure. Complications of percutaneous liver biopsy are fortunately uncommon, and have been well described. Ninety- six percent of such complications appear in the first 24 h[2]. The remaining 4% usually have their clinical expression within 10 d. The incidence of complications is known to be higher in patients with either cirrhosis or neoplasm[3]. The delay of twelve days before clinical manifestation of such a significant complication, as occurred in our patient who was ultimately found to have cirrhosis, is quite unusual.
The presence of blood in the biliary tree, hemobilia, was first described in 1948[4]. It was first reported as a complication of liver biopsy in 1967[5]. The incidence of hemobilia attributed to liver biopsy is less than 1%. In the largest reported series of complications induced by liver biopsies, hemobilia was noted in 4 of 68 276 patients (0.006%)[2].
The clinical manifestations of hemobilia vary and may be subtle. When blood flows in the extra-hepatic biliary system, symptoms which are similar to those caused by gall stones might be induced. Blood clots in the gall bladder itself can mimic biliary colic or induce cholecystitis. We found only five previous cases of this in the world’s literature. Clots in the common bile duct can also cause obstructive jaundice and pancreatitis similar to that caused by choledocholithiasis. In this case hemobilia caused by percutaneous liver biopsy led to the formation of a large blood clot in the gall bladder. The clinical signs of biliary colic (and subsequently acute cholecystitis) led to further evaluation and ultimately to a laparoscopic cholecystectomy.
Footnotes
S- Editor Guo SY L- Editor Wang XL E- Editor Liu WF
References
- 1.Sherlock S, Dooley J. Disease of the liver and biliary system. 11th ed. Oxford: Blackwell scientific publication; 2002. [Google Scholar]
- 2.Piccinino F, Sagnelli E, Pasquale G, Giusti G. Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol. 1986;2:165–173. doi: 10.1016/s0168-8278(86)80075-7. [DOI] [PubMed] [Google Scholar]
- 3.McGill DB, Rakela J, Zinsmeister AR, Ott BJ. A 21-year experience with major hemorrhage after percutaneous liver biopsy. Gastroenterology. 1990;99:1396–1400. doi: 10.1016/0016-5085(90)91167-5. [DOI] [PubMed] [Google Scholar]
- 4.Sandblom P. Hemorrhage into the biliary tract following trauma; traumatic hemobilia. Surgery. 1948;24:571–586. [PubMed] [Google Scholar]
- 5.Cox EF. Hemobilia following percutaneous needle biopsy of the liver. Arch Surg. 1967;95:198–201. doi: 10.1001/archsurg.1967.01330140036009. [DOI] [PubMed] [Google Scholar]


