Abstract
Hypertriglyceridemia is an established cause of pancreatitis. In a case-based approach, we present a review of hypertriglyceridemia and how it can cause pancreatitis. We outline how to investigate and manage such patients. A 35 year old man presented to the emergency department with abdominal pain and biochemical evidence of acute pancreatitis. There was no history of alcohol consumption and biliary imaging was normal. The only relevant past medical history was that of mild hyperlipidemia, treated with diet alone. Physical exam revealed epigastric tenderness, right lateral rectus palsy, lipemia retinalis, bitemporal hemianopsia and a delay in the relaxation phase of his ankle reflexes. Subsequent laboratory investigation revealed marked hypertriglyceridemia and panhypopituarism. An enhanced CT scan of the head revealed a large suprasellar mass impinging on the optic chiasm and hypothalamus. The patient was treated supportively; thyroid replacement and lipid lowering agents were started. He underwent a successful resection of a craniopharyngioma. Post-operatively, the patient did well on hormone replacement therapy. He has had no further attacks of pancreatitis. This case highlights many of the factors involved in the regulation of triglyceride metabolism. We review the common causes of hypertriglyceridemia and the proposed mechanisms resulting in pancreatitis. The incidence and management of hypertriglyceridemia-induced pancreatitis are also discussed.
Keywords: Hypertriglyceridemia, Pancreatitis, Hype-rlipidemia
INTRODUCTION
Acute pancreatitis is a common condition with several possible etiologies. The mortality rate may be up to 20%. While alcohol and gallstones are the most common etiologies, metabolic, structural and iatrogenic causes are responsible for 20%-25% of cases in the United States. Although hyperlipidemia can be associated with acute pancreatitis as an epiphenomenon, hypertriglyceridemia or chylomicronemia is the underlying cause in up to 7% of all cases of pancreatitis. It is the most common cause of acute pancreatitis not due to gallstones or alcohol[1-4]. Hypertriglyceridemia-induced pancreatitis rarely occurs unless triglyceride levels exceed 20 mmol/L[3,5]. For triglyceride levels to exceed 20 mmol/L, most patients will have some form of primary or genetic defect in lipid metabolism. Genetic factors determine over 60% of the variability in serum lipids. As most patients can be effectively treated with existing drug therapy, it is critical that the gastroenterologist recognize these patients and manage them appropriately. Since not all hyperlipidemia is familial in nature, an awareness of the secondary causes of hypertriglyceridemia and factors that can alter triglyceride metabolism is imperative.
In a case-based approach, we present a review of the common causes of hypertriglyceridemia, the proposed mechanisms resulting in pancreatitis as well as further details on the incidence and management of hypertriglyceridemia-induced pancreatitis (Table 1). Although the case presented is an uncommon scenario, it clearly demonstrates how a sequence of metabolic and endocrine abnormalities can lead to a common disease process- acute pancreatitis. The key to investigating, diagnosing and managing this patient was taking a detailed history and performing a thorough physical exam.
Table 1.
Causes of hypertriglyceridemia
| Primary | |
| Familial combined hyperlipidemia | |
| Familial hypertriglyceridemia | |
| Type III hyperlipoproteinemia | |
| Chylomicronemia | |
| Lipoprotein lipase deficiency | |
| Apolipoprotein C-II deficiency | |
| Secondary | |
| Insulin resistance | |
| Diabetes mellitus | |
| Obesity | |
| Hypothyroidism | |
| Alcohol | |
| Diet (excessive carbohydrate intake) | |
| Nephrotic syndrome | |
| Chronic renal failure, uremia | |
| Biliary obstruction/cholestasis | |
| Acute hepatitis | |
| Monoclonal gammopathy | |
| Multiple myeloma | |
| Systemic lupus erythematosus | |
| Stress, Sepsis | |
| Pregnancy | |
| Ileal bypass surgery | |
| Lipodystrophy | |
| Glycogen storage disease | |
| Drugs | |
| Estrogen | |
| Isotretinoin | |
| Β-blockers | |
| Glucocorticoids | |
| Cyclosporine | |
| Bile acid-binding resins | |
| Protease inhibitors | |
| Thiazides | |
| Tamoxifen |
Modified from Fung and Frohlich[44].
CASE PRPORT
A 35-year-old man presented to the emergency department with a 36-h history of severe epigastric pain and vomiting. He also complained of a four-month history of headaches, fatigue, cold intolerance, constipation, reduced libido, and erectile dysfunction. One year prior to presentation, he was told that he had mildly elevated “cholesterol” and was told to modify his diet. His past medical history was otherwise negative. He did not smoke, rarely consumed alcohol (none in the last 14 d) and was not taking any medications. Physical exam found a somnolent but easily rousable male with marked epigastric tenderness. No masses or organomegaly was noted on examination of his abdomen. A right lateral rectus palsy, lipemia retinalis and bitemporal hemianopsia were also noted on exam but there were no signs of increased intracranial pressure. The thyroid exam was normal but the relaxation phase of his ankle reflexes was delayed.
Electrolytes and complete blood count were normal. Serum lipase was 754 U/L (normal 20-190 U/L) and his liver transaminases, alkaline phosphatase and lactate dehydrogenase were normal. Ultrasound detected inflammatory changes in the pancreas but the gallbladder and biliary tree were normal. Serum triglyceride was 38.5 mmol/L (normal 0-2), cholesterol; 12.4 mmol/L (normal 0-5.2), thyroid stimulating hormone; 0.17 (normal 0.4-4.0), free T4; 3.8 pmol/L (normal 10.8-23.8), random cortisol; 62 mmol/L (normal 138-690), serum testosterone < 0.7 nmol/L (normal 10-33), and luteinizing hormone; 0.1 IU/L (normal 1.3-6.3). An enhanced CT scan of the head revealed a large suprasellar mass impinging on the hypothalamus and optic chiasm.
A diagnosis of acute pancreatitis was made. Chylomicronemia caused by central hypothyroidism was the most likely etiology. The patient was treated with intravenous fluids and narcotics for pain control. His epigastric pain resolved over three days. He was given dexamethasone 4 mg three times daily preoperatively and L-thyroxine 50 micrograms daily. The fibric acid derivative gemfibrozil was started at 600 mg twice daily. At craniotomy, a suprasellar craniopharyngioma displacing the optic chiasm and encasing the pituitary stalk was completely removed (Figure 1). He was started on glucocorticoid replacement therapy, L-thyroxine, DDAVP and testosterone for panhypopituitarism. His postoperative course was uncomplicated; he has subsequently remained asymptomatic over a three-year follow-up period.
Figure 1.
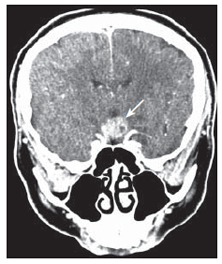
Enhanced CT scan showing a large suprasellar cranio-pharyngioma (arrow).
DISCUSSION
Hypertriglyceridemia-induced pancreatitis
Epidemiology: It is well known that hyperlipidemia is associated with acute pancreatitis, both as a precipitant and as an associated epiphenomenon[1,2]. Hypertriglyceridemia or chylomicronemia may be responsible for 1%-7% of all cases of pancreatitis[3,4]. Failure to consider and investigate chylomicronemia as a cause of pancreatitis may lead to an underestimate of the incidence. Pregnancy or medical conditions such as diabetes (both known to precipitate marked hypertriglyceridemia) should prompt further work-up[6,7]. Chylomicronemia may be the cause of 20% of episodes of acute pancreatitis in non-drinkers free of biliary tract disease. Chang et al found that hypertriglyceridemia was the cause of 56% cases of gestational pancreatitis[7]. In many settings, determining the exact etiology of pancreatitis may be complicated by the role of ethanol in precipitating severe hypertriglyceridemia. The proportion of “alcoholic pancreatitis” caused by direct as opposed to secondary hyperlipidemic effects is unknown.
Hypertriglyceridemia-induced pancreatitis rarely occurs unless triglyceride levels exceed 20 mmol/L[3,5]. In contrast, mild to moderate elevations in triglycerides (2-10 mmol/L) are extremely common in the early phase of acute pancreatitis of any etiology. One study noted such elevations in 47% of randomly selected patients presenting with acute pancreatitis[2]. In the same study, mild to moderate elevations of triglycerides were felt more likely to be an epiphenomenon of the acute pancreatitis rather than a true causal precipitant[2]. It is important to remember that chylomicrons are the product of dietary fat absorption. Enforced abstinence from eating after a diagnosis of pancreatitis may allow rapid metabolism of the triglyceride-rich chylomicrons. Dominguez-Munoz et al found severe elevations (> 20 mmol/L) in 10% of patients but levels rapidly fell in the majority of patients within 72 h of presentation; therefore, a delay in the presentation or consideration of diagnosis can lead to false conclusions about etiology. Triglyceride levels remained mildly elevated for up to 15 d, probably reflecting an underlying lipid disorder[2].
Pathogenesis of hypertriglyceride-induced pancreatitis
The exact mechanisms involved in hypertriglyceridemia-induced pancreatitis are unclear. Chylomicrons are triglyceride-rich lipoprotein particles believed to be responsible for pancreatic inflammation. They usually present in the circulation when serum triglyceride levels exceed 10 mmol/L. These largest of lipoproteins might impair circulatory flow in capillary beds; if this occurs in the pancreas, the resulting ischemia might disturb the acinar structure and expose these triglyceride-rich particles to pancreatic lipase. The pro-inflammatory non-esterified free fatty acids generated from the enzymatic degradation of chylomicron-triglycerides may lead to further damage of pancreatic acinar cells and microvasculature. Subsequent amplification of the release of inflammatory mediators and free radicals may ultimately lead to necrosis, edema, and inflammation[8,9]. This hypothesized sequence of events was substantiated by studies showing both triglycerides and free fatty acids caused edema, hemorrhage and elevated amylase levels[9]. Hypertriglyceridemia has also been shown to exacerbate other experimental models of pancreatitis[10].
Studies using oral lipid-loading tolerance tests have documented elevated post-load plasma triglyceride levels in patients with previous pancreatitis as compared with controls[11,12]. To address whether hyperlipidemia is a pre-existing metabolic disorder or a consequence of acute pancreatitis, Dominguez-Munoz and co-workers addressed the hypothesis that mild to moderate elevation of serum triglyceride levels are likely to be an epiphenomenon of the pancreatic disease whereas the severe hyperchylomicronemia and hypertrygliceridemia required to trigger acute pancreatitis would require a relevant defect in the lipid catabolism and clearance[13]. They looked at a group of ten patients with a history of acute pancreatitis associated with severe elevations of serum triglycerides (> 20 mmol/L) and ten patients with acute pancreatitis and normal lipid values. Four to six months after recovery from the pancreatitis, they administered an infusion of intralipid of 20% and calculated the fractional removal rate (K2) and the maximal clearance capacity (K1) of exogenous triglycerides. All patients with a previous attack of “normo-lipidemic” acute pancreatitis had normal K2 and K1 values. However, five patients (50%) with previous hyperlipidemic acute pancreatitis had an abnormally low clearance capacity of exogenous triglycerides while the remaining five had normal removal values. They concluded that, even in the setting of a marked elevation of serum lipid levels, there may be other etiological factors involved[13]. These findings were supported by a similar earlier study[14].
Interestingly, mutations in the lipoprotein lipase (LPL) gene have been identified in patients with hypertriglyceridemia-induced pancreatitis[15-20]. Specifically, mutations in the LPL gene are thought to be a common cause of pregnancy-induced chylomicronemia. One group described 5 such patients all of whom had different mutations in the LPL gene leading to dramatic reductions in LPL activity[21]. Dysregulation or deficiency of key enzymes and substrates involved in triglyceride metabolism has also been described in patients with recurrent hypertriglyceridemia-induced pancreatitis (Figure 2). Lecithin-cholesterol acyltransferase (LCAT) deficiency is one example[22].
Figure 2.
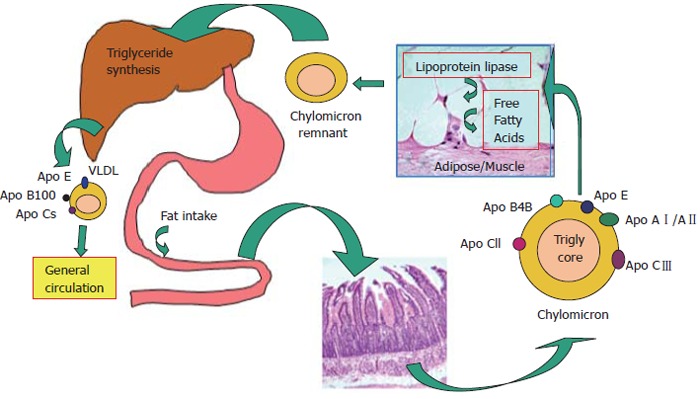
Triglyceride metabolism.
Hyperchylomicronemia and hypothyroidism
All patients that develop significant chylomicronemia are thought to have an underlying genetic disorder of lipoprotein metabolism. A disturbance in lipoprotein lipase activity, the rate-limiting enzyme of triglyceride-rich particle metabolism, is often the culprit. Clinical problems rarely develop unless there is another precipitating condition affecting metabolism such as diabetes, ethanol excess, pregnancy, certain drugs (estrogen[23-26], furosemide[27], isotretinoin[28,29], tamoxifen[30], beta-blockers[31]) or, as in this case, hypothyroidism. Physical findings can include eruptive xanthomas produced by macrophage uptake of chylomicrons which accumulate in the skin over extensor surfaces and lipemia retinalis that is a result of high concentrations of circulating chylomicrons in retinal vessels[32].
Hypothyroidism has a well-established association with hyperlipidemia. Elevations of triglyceride levels are observed in up to 35% of hypothyroid patients[33]. Impaired low-density lipoprotein (LDL) receptor activity may result in decreased clearance and thus an accumulation of LDL particles. A low circulating free thyroid hormone level may also impair lipoprotein lipase activity in adipose tissue. Replacement therapy with L-thyroxine treatment may reverse both of these defects.
Treatment
In the acute setting, pancreatitis due to hyperlipidemia should be treated in much the same manner as other causes of pancreatitis. Currently there is no clear evidence that hyperlipidemia-induced pancreatitis differs from other types of pancreatitis in terms of frequency of necrosis[2], complications or outcomes[3]. A similar approach to medical and diagnostic management is thus indicated. Although chylomicron and triglyceride levels fall rapidly after oral fat intake ceases, efforts to accelerate the removal of the precipitating lipoproteins have been considered.
Direct removal of chylomicrons in the acute setting can be readily achieved by plasmapheresis and there are numerous documented reports[34-37]. Chronic plasmapheresis as prophylaxis has also been reported in patients with recurrent pancreatitis due to severe primary hypertriglyceridemia that was unresponsive to drug and dietary interventions[38]. Recognizing that decreased lipoprotein lipase (LPL) activity is a prominent cause of hypertriglyceridemia has fuelled attempts to enhance LPL activity. Although this is an interesting concept only one small study in the literature has addressed this in which intravenous insulin and heparin, both of which enhance LPL activity, were used to treat a small number of patients with hypertriglyceridemia-induced pancreatitis[39]. They found that the therapy reduced triglyceride levels and appeared to improve the pancreatitis[39]. Diabetic patients should be treated aggressively with intravenous insulin infusions to obtain and maintain euglycemia rapidly.
Patients with known rare defects in lipid metabolism have been treated with replacement therapies with some success. Purified apoC-II infusion has yielded transient normalization of triglyceride levels and clinical improvement in pancreatitis patients with apoC-II deficiency[40].
Therapeutic efforts following recovery from pancreatitis need to be directed at preventing recurrence by controlling triglyceride levels. As most cases of hyperlipidemia occur when a genetically-predisposed individual is exposed to a secondary condition, therapy should be targeted towards the concomitant disorder. Alcohol should be discontinued as should oral estrogen therapy or selective estrogen receptor modulators such as tamoxifen or raloxifene. Diabetes should be treated with oral hypoglycemics and/or insulin aiming for tight glycemic control. Obviously, as in our case, hypothyroidism should be treated with L-thyroxine.
Persistence of hyperlipidemia on a fat-reduced diet should prompt the institution of lipid-lowering agents. The fibric acid derivatives (fibrates), such as gemfibrozil, fenofibrate or bezafibrate, are the drugs of first choice. These agents are generally well tolerated and highly effective if taken regularly and diet restrictions are continued. Niacin is inexpensive and often effective alone or in combination with a fibrate. Side effects such as flushing, hyperuricemia and hepatic transaminasemia may limit the use of niacin as a first line agent. Controversy exists as to whether niacin may exacerbate glucose intolerance in patients with diabetes mellitus. Omega-3 fatty-acid products show promise as adjunctive agents in refractory cases. Medium-chain triglycerides have also been used to prevent acute hyperlipidemic pancreatitis during pregnancy[41] as their absorption doesn’t require chylomicron formation.
Interestingly, in a study of 21 such patients with primary hypertriglyceridemia and a history of recurrent attacks of pancreatitis, lipid lowering toward normal was achieved in all patients with a program of combined dietary and drug therapy[42]. Five patients had recurrent episodes of pancreatitis during the treatment program all of whom were diagnosed subsequently with bulimia[42]. Anti-oxidant therapy (selenium, beta-carotene, vitamin C and α-tocopherol) has been used with success in the reduction of recurrent pancreatitis episodes in patients with familial lipoprotein lipase deficiency who remained markedly hypertriglyceridemic after medical therapy[43]. It is postulated that the antioxidants might protect the pancreatic acinar cells from free radical damage brought on by the ischemia of chylomicron-induced changes in pancreatic capillary circulation[43].
CONCLUSIONS
This case illustrates a sequence of clinical events, due to a combination of genetic and acquired disorders, which resulted in a common medical problem. The main clues to diagnosing this complex chain of events leading to pancreatitis became evident from a thorough history and physical exam. Identifying features of a possible intracranial lesion, hypothyroidism, hypogonadism and hypertriglyceridemia in the context of an understanding of triglyceride metabolism facilitated the diagnosis.
Hypertriglyceridemia is a common clinical problem that can be exacerbated by numerous medications and medical conditions. Markedly elevated triglyceride levels can lead to pancreatitis, a serious and potentially fatal complication. General and specific therapy is available to reduce triglyceride levels during the acute phase of pancreatitis, which may improve the outcome. Nutrition, pharmacologic therapy and avoiding agents that can elevate triglycerides may be essential in preventing further attacks. There are numerous causes of pancreatitis. Various diagnostic tools can be very helpful in determining the cause of pancreatic inflammation; however, the most valuable approach remains a thorough history and physical exam.
Footnotes
Supported by Alberta Heritage Foundation for Medical Research and Canadian Institute of Health Research
S- Editor Wang J L- Editor Alpini GD E- Editor Liu WF
References
- 1.Toskes PP. Hyperlipidemic pancreatitis. Gastroenterol Clin North Am. 1990;19:783–791. [PubMed] [Google Scholar]
- 2.Dominguez-Muñoz JE, Malfertheiner P, Ditschuneit HH, Blanco-Chavez J, Uhl W, Büchler M, Ditschuneit H. Hyperlipidemia in acute pancreatitis. Relationship with etiology, onset, and severity of the disease. Int J Pancreatol. 1991;10:261–267. [PubMed] [Google Scholar]
- 3.Fortson MR, Freedman SN, Webster PD 3rd. Clinical assessment of hyperlipidemic pancreatitis. Am J Gastroenterol. 1995;90:2134–2139. [PubMed] [Google Scholar]
- 4.Searles GE, Ooi TC. Underrecognition of chylomicronemia as a cause of acute pancreatitis. CMAJ. 1992;147:1806–1808. [PMC free article] [PubMed] [Google Scholar]
- 5.Lithell H, Vessby B, Walldius G, Carlson LA. Hypertriglyceridemia--acute pancreatitis--ischemic heart disease. A case study in a pair of monozygotic twins. Acta Med Scand. 1987;221:311–316. [PubMed] [Google Scholar]
- 6.Achard JM, Westeel PF, Moriniere P, Lalau JD, de Cagny B, Fournier A. Pancreatitis related to severe acute hypertriglyceridemia during pregnancy: treatment with lipoprotein apheresis. Intensive Care Med. 1991;17:236–237. doi: 10.1007/BF01709884. [DOI] [PubMed] [Google Scholar]
- 7.Chang CC, Hsieh YY, Tsai HD, Yang TC, Yeh LS, Hsu TY. Acute pancreatitis in pregnancy. Zhonghua Yixue Zazhi (Taipei) 1998;61:85–92. [PubMed] [Google Scholar]
- 8.Havel RJ. Pathogenesis, differentiation and management of hypertriglyceridemia. Adv Intern Med. 1969;15:117–154. [PubMed] [Google Scholar]
- 9.Saharia P, Margolis S, Zuidema GD, Cameron JL. Acute pancreatitis with hyperlipemia: studies with an isolated perfused canine pancreas. Surgery. 1977;82:60–67. [PubMed] [Google Scholar]
- 10.Kimura W, Mössner J. Role of hypertriglyceridemia in the pathogenesis of experimental acute pancreatitis in rats. Int J Pancreatol. 1996;20:177–184. doi: 10.1007/BF02803766. [DOI] [PubMed] [Google Scholar]
- 11.Cameron JL, Capuzzi DM, Zuidema GD, Margolis S. Acute pancreatitis with hyperlipemia. Evidence for a persistent defect in lipid metabolism. Am J Med. 1974;56:482–487. doi: 10.1016/0002-9343(74)90480-x. [DOI] [PubMed] [Google Scholar]
- 12.Guzmán S, Nervi F, Llanos O, León P, Valdivieso V. Impaired lipid clearance in patients with previous acute pancreatitis. Gut. 1985;26:888–891. doi: 10.1136/gut.26.9.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Domínguez-Muñoz JE, Jünemann F, Malfertheiner P. Hyperlipidemia in acute pancreatitis. Cause or epiphenomenon. Int J Pancreatol. 1995;18:101–106. doi: 10.1007/BF02785883. [DOI] [PubMed] [Google Scholar]
- 14.Pfau J. [Acute pancreatitis and hypertriglyceridemia] Rev Med Chil. 1989;117:907–909. [PubMed] [Google Scholar]
- 15.Rouis M, Lohse P, Dugi KA, Lohse P, Beg OU, Ronan R, Talley GD, Brunzell JD, Santamarina-Fojo S. Homozygosity for two point mutations in the lipoprotein lipase (LPL) gene in a patient with familial LPL deficiency: LPL(Asp9-> Asn, Tyr262--> His) J Lipid Res. 1996;37:651–661. [PubMed] [Google Scholar]
- 16.Jap TS, Jenq SF, Wu YC, Chiu CY, Cheng HM. Mutations in the lipoprotein lipase gene as a cause of hypertriglyceridemia and pancreatitis in Taiwan. Pancreas. 2003;27:122–126. doi: 10.1097/00006676-200308000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Wilson DE, Hata A, Kwong LK, Lingam A, Shuhua J, Ridinger DN, Yeager C, Kaltenborn KC, Iverius PH, Lalouel JM. Mutations in exon 3 of the lipoprotein lipase gene segregating in a family with hypertriglyceridemia, pancreatitis, and non-insulin-dependent diabetes. J Clin Invest. 1993;92:203–211. doi: 10.1172/JCI116551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Henderson H, Leisegang F, Hassan F, Hayden M, Marais D. A novel Glu421Lys substitution in the lipoprotein lipase gene in pregnancy-induced hypertriglyceridemic pancreatitis. Clin Chim Acta. 1998;269:1–12. doi: 10.1016/s0009-8981(97)00144-7. [DOI] [PubMed] [Google Scholar]
- 19.Hsia SH, Connelly PW, Hegele RA. Pancreatitis, hyperlipidemia, and pregnancy in two sisters. Ann Intern Med. 1997;126:88–89. doi: 10.7326/0003-4819-126-1-199701010-00020. [DOI] [PubMed] [Google Scholar]
- 20.Bruin T, Tuzgöl S, van Diermen DE, Hoogerbrugge-van der Linden N, Brunzell JD, Hayden MR, Kastelein JJ. Recurrent pancreatitis and chylomicronemia in an extended Dutch kindred is caused by a Gly154--> Ser substitution in lipoprotein lipase. J Lipid Res. 1993;34:2109–2119. [PubMed] [Google Scholar]
- 21.Ma Y, Ooi TC, Liu MS, Zhang H, McPherson R, Edwards AL, Forsythe IJ, Frohlich J, Brunzell JD, Hayden MR. High frequency of mutations in the human lipoprotein lipase gene in pregnancy-induced chylomicronemia: possible association with apolipoprotein E2 isoform. J Lipid Res. 1994;35:1066–1075. [PubMed] [Google Scholar]
- 22.Watts GF, Mitropoulos KA, al-Bahrani A, Reeves BE, Owen JS. Lecithin-cholesterol acyltransferase deficiency presenting with acute pancreatitis: effect of infusion of normal plasma on triglyceride-rich lipoproteins. J Intern Med. 1995;238:137–141. doi: 10.1111/j.1365-2796.1995.tb00911.x. [DOI] [PubMed] [Google Scholar]
- 23.Al-Awady HM. The etiological factors in 73 cases of acute pancreatitis. Int Surg. 1981;66:145–148. [PubMed] [Google Scholar]
- 24.Isley WL, Oki J. Estrogen-induced pancreatitis after discontinuation of concomitant medroxyprogesterone therapy. Am J Med. 1997;102:416–417. doi: 10.1016/s0002-9343(97)80024-1. [DOI] [PubMed] [Google Scholar]
- 25.Agarwal M, Lunt H, Scott R. Hormone replacement therapy, diabetes and pancreatitis secondary to hypertriglyceridaemia. N Z Med J. 1997;110:426. [PubMed] [Google Scholar]
- 26.Davidoff F, Tishler S, Rosoff C. Marked hyperlipidemia and pancreatitis associated with oral contraceptive therapy. N Engl J Med. 1973;289:552–555. doi: 10.1056/NEJM197309132891103. [DOI] [PubMed] [Google Scholar]
- 27.Call T, Malarkey WB, Thomas FB. Acute pancreatitis secondary to furosemide with associated hyperlipidemia. Am J Dig Dis. 1977;22:835–838. doi: 10.1007/BF01694517. [DOI] [PubMed] [Google Scholar]
- 28.Flynn WJ, Freeman PG, Wickboldt LG. Pancreatitis associated with isotretinoin-induced hypertriglyceridemia. Ann Intern Med. 1987;107:63. doi: 10.7326/0003-4819-107-1-63. [DOI] [PubMed] [Google Scholar]
- 29.McCarter TL, Chen YK. Marked hyperlipidemia and pancreatitis associated with isotretinoin therapy. Am J Gastroenterol. 1992;87:1855–1858. [PubMed] [Google Scholar]
- 30.Elisaf MS, Nakou K, Liamis G, Pavlidis NA. Tamoxifen-induced severe hypertriglyceridemia and pancreatitis. Ann Oncol. 2000;11:1067–1069. doi: 10.1023/a:1008309613082. [DOI] [PubMed] [Google Scholar]
- 31.O'Donoghue DJ. Acute pancreatitis due to nadolol-induced hypertriglyceridaemia. Br J Clin Pract. 1989;43:74–75. [PubMed] [Google Scholar]
- 32.Santamarina-Fojo S. The familial chylomicronemia syndrome. Endocrinol Metab Clin North Am. 1998;27:551–67, viii. doi: 10.1016/s0889-8529(05)70025-6. [DOI] [PubMed] [Google Scholar]
- 33.O'Brien T, Dinneen SF, O'Brien PC, Palumbo PJ. Hyperlipidemia in patients with primary and secondary hypothyroidism. Mayo Clin Proc. 1993;68:860–866. doi: 10.1016/s0025-6196(12)60694-6. [DOI] [PubMed] [Google Scholar]
- 34.Routy JP, Smith GH, Blank DW, Gilfix BM. Plasmapheresis in the treatment of an acute pancreatitis due to protease inhibitor-induced hypertriglyceridemia. J Clin Apher. 2001;16:157–159. doi: 10.1002/jca.1030. [DOI] [PubMed] [Google Scholar]
- 35.Yamauchi H, Sunamura M, Takeda K, Suzuki T, Itoh K, Miyagawa K. Hyperlipidemia and pregnancy associated pancreatitis with reference to plasma exchange as a therapeutic intervention. Tohoku J Exp Med. 1986;148:197–205. doi: 10.1620/tjem.148.197. [DOI] [PubMed] [Google Scholar]
- 36.Ho KM, Yeo J. Plasmapheresis in the management of pancreatitis related to hypertriglyceridaemia. Anaesth Intensive Care. 1999;27:117. [PubMed] [Google Scholar]
- 37.Swoboda K, Derfler K, Koppensteiner R, Langer M, Pamberger P, Brehm R, Ehringer H, Druml W, Widhalm K. Extracorporeal lipid elimination for treatment of gestational hyperlipidemic pancreatitis. Gastroenterology. 1993;104:1527–1531. doi: 10.1016/0016-5085(93)90366-k. [DOI] [PubMed] [Google Scholar]
- 38.Piolot A, Nadler F, Cavallero E, Coquard JL, Jacotot B. Prevention of recurrent acute pancreatitis in patients with severe hypertriglyceridemia: value of regular plasmapheresis. Pancreas. 1996;13:96–99. doi: 10.1097/00006676-199607000-00013. [DOI] [PubMed] [Google Scholar]
- 39.Henzen C, Röck M, Schnieper C, Heer K. [Heparin and insulin in the treatment of acute hypertriglyceridemia-induced pancreatitis] Schweiz Med Wochenschr. 1999;129:1242–1248. [PubMed] [Google Scholar]
- 40.Baggio G, Manzato E, Gabelli C, Fellin R, Martini S, Enzi GB, Verlato F, Baiocchi MR, Sprecher DL, Kashyap ML. Apolipoprotein C-II deficiency syndrome. Clinical features, lipoprotein characterization, lipase activity, and correction of hypertriglyceridemia after apolipoprotein C-II administration in two affected patients. J Clin Invest. 1986;77:520–527. doi: 10.1172/JCI112332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mizushima T, Ochi K, Matsumura N, Ichimura M, Ishibashi T, Tsuboi K, Harada H. Prevention of hyperlipidemic acute pancreatitis during pregnancy with medium-chain triglyceride nutritional support. Int J Pancreatol. 1998;23:187–192. doi: 10.1007/BF02788396. [DOI] [PubMed] [Google Scholar]
- 42.Gavish D, Eisenberg S, Berry EM, Kleinman Y, Witztum E, Norman J, Leitersdorf E. Bulimia. An underlying behavioral disorder in hyperlipidemic pancreatitis: a prospective multidisciplinary approach. Arch Intern Med. 1987;147:705–708. doi: 10.1001/archinte.147.4.705. [DOI] [PubMed] [Google Scholar]
- 43.Heaney AP, Sharer N, Rameh B, Braganza JM, Durrington PN. Prevention of recurrent pancreatitis in familial lipoprotein lipase deficiency with high-dose antioxidant therapy. J Clin Endocrinol Metab. 1999;84:1203–1205. doi: 10.1210/jcem.84.4.5617. [DOI] [PubMed] [Google Scholar]
- 44.Fung MA, Frohlich JJ. Common problems in the management of hypertriglyceridemia. CMAJ. 2002;167:1261–1266. [PMC free article] [PubMed] [Google Scholar]


