Abstract
Gastric accommodation is important for the under-standing of the pathophysiology in functional dyspepsia and is also relevant for symptom generation in other disorders. The term gastric accommodation has at least three different meanings: The accommodation process, the accommodation reflex, and the accommodation response. The gastric accommodation process is a complex phenomenon that describes how the size of the gastric compartment changes in response to a meal. The electronic barostat is considered the gold standard in assessing gastric accommodation. Imaging methods, including MRI, SPECT, and ultrasonography may also be used, particularly in patients who are stress-responsive, e.g. functional dyspepsia patients, as a non-invasive and less stress-inducing method is favourable. Ultrasonography satisfies these criteria as it does not by itself distort the physiological response in stress-responsive individuals.
Keywords: Ultrasonography, Gastric accommodation, Stomach, Barostat, Gastric relaxation, 3D ultrasound
INTRODUCTION
Gastric accommodation has become a key mechanism for the understanding of the pathophysiology in functional dyspepsia[1,2] and may also be relevant for symptom generation in other disorders[3-6]. Several methods can be used to assess gastric accommodation[7]. The electronic barostat is considered to be the gold standard method for measuring proximal gastric accommodation[8,9]. By applying the barostat, gastric tone is estimated by recording variations in the volume of air within an intragastric bag that is maintained at a constant pressure by the instrument. Accommodation of the proximal stomach is supposed to be reflected in changes of gastric tone. However, the method is invasive, bothersome and affects normal gastric motility[10]. The bag may also alter intragastric distribution and emptying of the meal the direct stimulus imposed by the bag itself on the stomach wall results in increased antral distension[11]. Therefore, non-invasive methods as MRI, SPECT, and ultrasonography are warranted for the study of gastric accommodation.
MRI is a safe and accurate technique to image the entire stomach with detail[12]. After ingestion of a test meal labelled with gadolinium as an MRI marker, images of the gastric region are acquired, typically using a Spin Echo T1-weighted sequence. The MRI technique permits three-dimensional reconstruction of the stomach, enabling total gastric volume measurements during fasting and postprandially. The ratio of these measurements is used to quantify the accommodation response. Single Photon Emission Computed Tomography (SPECT) uses 99mTc uptake into the gastric mucosa for visualisation and volume estimation of the gastric compartment[13]. Comparison of SPECT data with barostat measurements showed that SPECT is able to detect changes in intragastric volume but unable to detect changes in gastric tone and hence accommodation[14].
GASTRIC ACCOMMODATION
Conceptually, the process of gastric accommodation has been explored for over 100 years, evaluating relaxation of the proximal stomach[15]. Receptive relaxation has been defined as a vagal reflex, which dilates the corpus-fundus region of the stomach in response to swallowing, oesophageal stimulation, or vomitation[16-18]. Adaptive relaxation is a intrinsic vagovagal reflex that enables the stomach to increase its volume markedly without a corresponding increase in pressure[19,20]. Adaptive relaxation enables the stomach to maintain a low balanced pressure and to continuously adapt its volume to its content.
However, the term gastric accommodation is too complex to embrace in one definition, mainly because it is utilized in at least three different meanings in the literature: The accommodation process, the accommodation reflex, and the accommodation response. In addition, the term is often used in an everyday language expressing that “the stomach accommodates a meal”. Similarly, it was also used by Paton and Vane in 1963 to describe gastric “expansion to accommodate the fluid”[21]. The gastric accommodation process is a complex phenomenon that describes how the size of the gastric compartment changes in response to a meal[22]. It involves both intra- and extragastric reflexes. The extragastric reflexes comprises both receptive relaxation and intestino-gastric reflexes elicited by balloon distension or nutrient infusion in the duodenum[8,23]. The intragastric reflexes embrace at least adaptive relaxation and relaxation of the proximal stomach induced from antral reflexes[24-26].
Kelly[27] described the accommodation reflex when he demonstrated how intragastric pressure was regulated by gastric “accommodation to distension”. The accommodation reflex is elicited when continuous volume expansion of the proximal stomach reaches a certain level, thus inducing relaxation of smooth muscles of the gastric wall in order to prevent further increase in pressure. This physiological phenomenon is a reflex arc consisting of a mechanoreceptor in the gastrointestinal wall, a neuro-muscular pathway through ENS with a reflex centre, and a well-defined response in the effective organ. The reflex is probably vagally mediated but local axon reflexes may also be involved[20]. The term accommodation response is the effect of the reflex or the result of the process and this is a precise notion for what we intend to measure with different methods.
IMAGING METHODS
A crucial question is whether imaging methods, as MRI, SPECT or ultrasonography, actually can be compared to the measurements made by the barostat. In our opinion, imaging methods and the invasive barostat method do not measure the same aspects of the gastric accommodation process. Thanks to its close contact with the gastric wall the barostat bag adjusts to changes in proximal gastric pressure by changing the intrabag volume. Thus, changes in volume are believed to reflect changes in muscle tone of the wall. However, the quantitative change in volume seen during barostat examinations is only valid during barostat studies using exactly the same equipment and positioning technique. Imaging methods, however, visualize directly the size of the gastric compartments, thus giving an indirect measure of relaxation and contraction. The volume change seen using imaging can thus be explained by additional secretion, air retention or most probable changes in gastric emptying.
The gastric meal accommodation process has two components: Passive meal distension of the gastric compartments and active muscle relaxation of the gastric wall. The first component is best measured with imaging methods whereas the barostat is best suited for studying the second component. Imaging methods at this stage, do not distinguish between enlargements of the stomach due to reflex relaxation or due to meal-induced distension; it just measures the totally accommodated volume. Accordingly, it may not be adequate to compare imaging methods to the barostat for validation of gastric accommodation. Gastric accommodation depends on neuromuscular factors and hence it is also a matter of evaluation of the mechanical properties of the stomach. In this sense the barostat merely detects the existence of change in wall tone, but cannot as the imaging methods, provide data on the distribution of the volume and the normal behaviour of the gastric wall. In biomechanics, it is essential to understand the geometry of the organ and the forces and deformation in different directions in order to better understand the active-passive muscle function and mechano-sensation in health and in diseases such as the functional disorders. This warrants 2D and 3D image analysis of the gastric compartments.
The different imaging methods exhibit different spatial and temporal image resolution, and these factors strongly influence accuracy in volume calculation. MRI and in particular SPECT imaging have poor spatial and temporal resolution compared to ultrasonography. Ultrasonography can provide temporal resolution above 100 fps, if necessary, and a spatial resolution on sub-millimetre level. Also, the “stress-factor” of the imaging methods should be considered in this context because dyspeptic patients in general and vagal reflexes in particular are very sensitive to psychological stress. Everyone who has been inside a narrow, noisy MR scanner knows how frightening this can be. Naturally, the stress-factor is also substantially involved in studies using the barostat. Simply because functional disorders are so strongly associated to psychological factors, the examination should be performed in a quiet and relaxing atmosphere with a minimum of distress. Ultrasonography satisfies these criteria as it is non-invasive and does not by itself distort the physiological response in stress-responsive individuals. Moreover, due to gravity playing a central role in the propulsion of gastric content, the study of meal accommodation should preferably be performed in a “natural position” such as sitting in a chair. Therefore, methods that enable patients to be seated have an advantage over methods requiring patients to be in supine position during the examination.
Ultrasonography
Ultrasonography, a clinical method that is widely available, has shown applicability and validity for the study of gastric accommodation[28]. The 2D method developed by Gilja et al[29] has been used to study gastric accommodation in functional dyspepsia[1,30], diabetes[4], in patients with reflux oesophagitis[5], in liver cirrhosis[31], and in children with recurrent abdominal pain[6]. This 2D method has also been applied to study pharmacological intervention[32] and the effect of a barostat bag in the stomach[11]. Another advantage with 2D ultrasonography is its clinical applicability; it can easily be performed bedside and repeated numerous times in the same subject. At Haukeland University Hospital we have for 20 years used The Ultrasound Meal Accommodation Test (U-MAT) for the work-up of patients with dyspepsia (Table 1). Our mainstream clinical protocol consists of a standard soup meal (500 mL), ultrasound scanning of the proximal and distal stomach using predefined scan sections (Figure 1), calculation of size and volumes of the gastric compartments, evaluation of symptoms and psychological assessment. In our experience, ultrasonography used in this context adds valuable clinical information to the management of these patients.
Table 1.
The ultrasound meal accommodation test
| Time | Protocol |
| Fasting | Ordinary ultrasound examination of the liver, gallbladder, biliary tract, spleen, pancreas, kidneys, and large vessels. |
| Fasting | Evaluation of symptoms by VAS. |
| Fasting | Assessment of motility pattern (phase 1-3) by observing the pattern of contractility in the antrum. |
| Fasting | Measurement of area of the distal stomach (AA). |
| Fasting | Visualisation of the proximal stomach to explore whether it has content. |
| Meal ingestion | 500 mL of preheated meat soup is ingested in 4 min at a constant speed. |
| 2 min pp. | Measurement of the sagittal area (SA), the oblique frontal diameter (OFD), and the antral area (AA). |
| 5 min pp. | Postprandial symptom evaluation. |
| 10 min pp. | SA, OFD, and AA measurement. |
| 20 min pp. | SA, OFD, and AA measurement. |
| 30 min pp. | SA, OFD, and AA measurement. |
Figure 1.
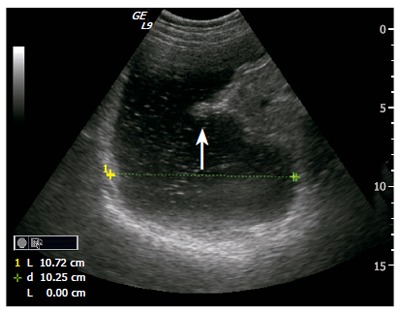
Ultrasonogram showing an oblique frontal section of the proximal stomach in a patient with dyspepsia referred for Ultrasound Meal Accommodation Test (UMAT). The transversal diameter is measured indicating the size of the postprandial proximal stomach and hence indirectly degree of accommodation. Interestingly, one can also observe a gastric contraction (white arrow) in the posterior angular part and progressing towards the antrum.
There are few methods that are capable of measuring all parameters of gastric motility simultaneously. However, many authors have demonstrated that ultrasonography can be used to study not only gastric accommodation, but also gastric emptying[33-39], gastric configuration[40-42], intragastric distribution[43], antral motility[44-46] and distensibility[47,48], transpyloric flow[44,49-51] and strain of the gastric wall[42,52,53]. Of the present available methods, we would argue that ultrasonography is the method that has been shown to estimate most parameters of gastric motility, many of these also simultaneously. Furthermore, we claim that ultrasonography has the strongest potential as a clinical tool compared to MRI, SPECT, and scintigraphy, and particularly in patients with functional disorders.
3D ultrasound
For better visualization of the total stomach and improved calculation of gastric volumes, 3D ultrasound imaging of the gastric compartments was developed[43,54,55] It is important that validation of an imaging method to study gastric accommodation also include evaluation of its accuracy and precision in volume estimation. In our lab, we have utilized two different systems for acquisition of 3D ultrasound images and both systems have been validated in vitro and in vivo. First, we developed a mechanical system with the advantage of an accurate motorized movement of the ultrasound transducer in a tilting fashion. This 3D system demonstrated excellent accuracy and precision in vitro[56,57] and good agreement with MRI in vivo[58]. Subsequently, we applied a magneto-based system (Bird sensor, Ascension Technology Corp., Burlington, VT, USA) that enabled greater flexibility during scanning and larger volumes like the total gastric compartment to be captured (Figure 2). The Bird system also showed excellent accuracy in vitro[43,59-61] and in volume measurement of a thin-walled fluid filled bag in the human stomach the agreement with true volumes was excellent[62]. Accordingly, 3D ultrasonography delivers high resolution, is accurate in volume estimation and is a well-suited tool to monitor volume changes of the stomach during the process of accommodation. However, we acknowledge its limitations: impairment of image quality with air in the GI tract, mainly for use with liquid meals, and scanning of very obese subjects (fortunately dyspeptics are not often obese).
Figure 2.
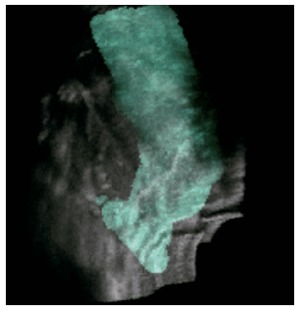
3D image reconstruction based on ultrasound acquisition with a magneto-based position- and orientation measurement system (POM) using GE Logiq 9. The 3D image is overlayed the ordinary gray scale values of ultrasonograms.
Abnormalities of gastric accommodation are a significant finding in several patients groups, not only in patients with functional disorders. Comprehension of gastric geometry, the forces and deformation during meal accommodation, and the active-passive muscle function is important in functional diseases[63]. Of the present available methods, we would argue that ultrasonography is the method that has been shown to estimate most parameters of gastric motility, many of these also simultaneously[64]. Furthermore, we suggest that ultrasonography has the strongest potential as a clinical tool, particularly in patients with functional disorders.
Footnotes
S- Editor Pan BR E- Editor Ma WH
References
- 1.Gilja OH, Hausken T, Wilhelmsen I, Berstad A. Impaired accommodation of proximal stomach to a meal in functional dyspepsia. Dig Dis Sci. 1996;41:689–696. doi: 10.1007/BF02213124. [DOI] [PubMed] [Google Scholar]
- 2.Tack J, Piessevaux H, Coulie B, Caenepeel P, Janssens J. Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology. 1998;115:1346–1352. doi: 10.1016/s0016-5085(98)70012-5. [DOI] [PubMed] [Google Scholar]
- 3.Oliveira RB, Troncon LE, Meneghelli UG, Padovan W, Dantas RO, de Godoy RA. Impaired gastric accommodation to distension and rapid gastric emptying in patients with Chagas' disease. Dig Dis Sci. 1980;25:790–794. doi: 10.1007/BF01345301. [DOI] [PubMed] [Google Scholar]
- 4.Undeland KA, Hausken T, Gilja OH, Aanderud S, Berstad A. Gastric meal accommodation studied by ultrasound in diabetes. Relation to vagal tone. Scand J Gastroenterol. 1998;33:236–241. doi: 10.1080/00365529850170784. [DOI] [PubMed] [Google Scholar]
- 5.Tefera S, Gilja OH, Hatlebakk JG, Berstad A. Gastric accommodation studied by ultrasonography in patients with reflux esophagitis. Dig Dis Sci. 2001;46:618–625. doi: 10.1023/a:1005619803917. [DOI] [PubMed] [Google Scholar]
- 6.Olafsdottir E, Gilja OH, Aslaksen A, Berstad A, Fluge G. Impaired accommodation of the proximal stomach in children with recurrent abdominal pain. J Pediatr Gastroenterol Nutr. 2000;30:157–163. doi: 10.1097/00005176-200002000-00012. [DOI] [PubMed] [Google Scholar]
- 7.De Schepper HU, Cremonini F, Chitkara D, Camilleri M. Assessment of gastric accommodation: overview and evaluation of current methods. Neurogastroenterol Motil. 2004;16:275–285. doi: 10.1111/j.1365-2982.2004.00497.x. [DOI] [PubMed] [Google Scholar]
- 8.Azpiroz F, Malagelada JR. Abdominal bloating. Gastroenterology. 2005;129:1060–1078. doi: 10.1053/j.gastro.2005.06.062. [DOI] [PubMed] [Google Scholar]
- 9.Tack J, Caenepeel P, Fischler B, Piessevaux H, Janssens J. Symptoms associated with hypersensitivity to gastric distention in functional dyspepsia. Gastroenterology. 2001;121:526–535. doi: 10.1053/gast.2001.27180. [DOI] [PubMed] [Google Scholar]
- 10.Ropert A, des Varannes SB, Bizais Y, Rozé C, Galmiche JP. Simultaneous assessment of liquid emptying and proximal gastric tone in humans. Gastroenterology. 1993;105:667–674. doi: 10.1016/0016-5085(93)90881-c. [DOI] [PubMed] [Google Scholar]
- 11.Mundt MW, Hausken T, Samsom M. Effect of intragastric barostat bag on proximal and distal gastric accommodation in response to liquid meal. Am J Physiol Gastrointest Liver Physiol. 2002;283:G681–G686. doi: 10.1152/ajpgi.00499.2001. [DOI] [PubMed] [Google Scholar]
- 12.Schwizer W, Steingötter A, Fox M, Zur T, Thumshirn M, Bösiger P, Fried M. Non-invasive measurement of gastric accommodation in humans. Gut. 2002;51 Suppl 1:i59–i62. doi: 10.1136/gut.51.suppl_1.i59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuiken SD, Samsom M, Camilleri M, Mullan BP, Burton DD, Kost LJ, Hardyman TJ, Brinkmann BH, O'Connor MK. Development of a test to measure gastric accommodation in humans. Am J Physiol. 1999;277:G1217–G1221. doi: 10.1152/ajpgi.1999.277.6.G1217. [DOI] [PubMed] [Google Scholar]
- 14.van den Elzen BD, Bennink RJ, Wieringa RE, Tytgat GN, Boeckxstaens GE. Fundic accommodation assessed by SPECT scanning: comparison with the gastric barostat. Gut. 2003;52:1548–1554. doi: 10.1136/gut.52.11.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moritz F. Studien uber die motorische Thatigkeit des Magens. Zeitschr fur Biol. 1895;32:313–369. [Google Scholar]
- 16.Cannon WB, Lieb CW. The receptive relaxation of the stomach. Am J Physiol. 1911;29:267–273. [Google Scholar]
- 17.Grey EG. Observations on the postural activity of the stomach. Am J Physiol. 1918;45:272–285. [Google Scholar]
- 18.Azpiroz F, Malagelada JR. Physiological variations in canine gastric tone measured by an electronic barostat. Am J Physiol. 1985;248:G229–G237. doi: 10.1152/ajpgi.1985.248.2.G229. [DOI] [PubMed] [Google Scholar]
- 19.Jahnberg T, Abrahamsson H, Jansson G, Martinson J. Gastric relaxatory response to feeding before and after vagotomy. Scand J Gastroenterol. 1977;12:225–228. doi: 10.1203/00006450-199404000-00024. [DOI] [PubMed] [Google Scholar]
- 20.Desai KM, Sessa WC, Vane JR. Involvement of nitric oxide in the reflex relaxation of the stomach to accommodate food or fluid. Nature. 1991;351:477–479. doi: 10.1038/351477a0. [DOI] [PubMed] [Google Scholar]
- 21.Paton WD, Vane JR. Analysis of he responses of the isolated stomach to electrical stimulation and to drugs. J Physiol. 1963;165:10–46. doi: 10.1113/jphysiol.1963.sp007040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gilja OH. Ultrasonography for surgeons. Scand J Gastroenterol. 2005;40:615–616. doi: 10.1080/00365520510023233. [DOI] [PubMed] [Google Scholar]
- 23.Azpiroz F, Malagelada JR. Isobaric intestinal distension in humans: sensorial relay and reflex gastric relaxation. Am J Physiol. 1990;258:G202–G207. doi: 10.1152/ajpgi.1990.258.2.G202. [DOI] [PubMed] [Google Scholar]
- 24.Abrahamsson H. Vagal relaxation of the stomach induced from the gastric antrum. Acta Physiol Scand. 1973;89:406–414. doi: 10.1111/j.1748-1716.1973.tb05535.x. [DOI] [PubMed] [Google Scholar]
- 25.Caldarella MP, Azpiroz F, Malagelada JR. Antro-fundic dysfunctions in functional dyspepsia. Gastroenterology. 2003;124:1220–1229. doi: 10.1016/s0016-5085(03)00287-7. [DOI] [PubMed] [Google Scholar]
- 26.Lunding JA, Tefera S, Bayati A, Gilja OH, Mattsson H, Hausken T, Berstad A. Pressure-induced gastric accommodation studied with a new distension paradigm. Abnormally low accommodation rate in patients with functional dyspepsia. Scand J Gastroenterol. 2006;41:544–552. doi: 10.1080/00365520500353723. [DOI] [PubMed] [Google Scholar]
- 27.Kelly KA. Gastric motility after gastric operations. Surg Annu. 1974;6:103–123. [PubMed] [Google Scholar]
- 28.Odegaard S, Gilja OH, Gregersen H. Basic and new aspects of gastrointestinal ultrasonography. 1sted. Singapore. World Sci. 2005:1–502. [Google Scholar]
- 29.Gilja OH, Hausken T, Odegaard S, Berstad A. Monitoring postprandial size of the proximal stomach by ultrasonography. J Ultrasound Med. 1995;14:81–89. doi: 10.7863/jum.1995.14.2.81. [DOI] [PubMed] [Google Scholar]
- 30.Gilja OH, Hausken T, Bang CJ, Berstad A. Effect of glyceryl trinitrate on gastric accommodation and symptoms in functional dyspepsia. Dig Dis Sci. 1997;42:2124–2131. doi: 10.1023/a:1018839122354. [DOI] [PubMed] [Google Scholar]
- 31.Izbéki F, Kiss I, Wittmann T, Várkonyi TT, Légrády P, Lonovics J. Impaired accommodation of proximal stomach in patients with alcoholic liver cirrhosis. Scand J Gastroenterol. 2002;37:1403–1410. doi: 10.1080/003655202762671279. [DOI] [PubMed] [Google Scholar]
- 32.Vingerhagen S, Hausken T, Gilja OH, Berstad A. Influence of a 5HT1 receptor agonist on gastric accommodation and initial transpyloric flow in healthy subjects. Neurogastroenterol Motil. 2000;12:95–101. doi: 10.1046/j.1365-2982.2000.00184.x. [DOI] [PubMed] [Google Scholar]
- 33.Bateman DN, Whittingham TA. Measurement of gastric emptying by real-time ultrasound. Gut. 1982;23:524–527. doi: 10.1136/gut.23.6.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bolondi L, Bortolotti M, Santi V, Calletti T, Gaiani S, Labò G. Measurement of gastric emptying time by real-time ultrasonography. Gastroenterology. 1985;89:752–759. doi: 10.1016/0016-5085(85)90569-4. [DOI] [PubMed] [Google Scholar]
- 35.Holt S, Cervantes J, Wilkinson AA, Wallace JH. Measurement of gastric emptying rate in humans by real-time ultrasound. Gastroenterology. 1986;90:918–923. doi: 10.1016/0016-5085(86)90868-1. [DOI] [PubMed] [Google Scholar]
- 36.Duan LP, Zheng ZT, Li YN. A study of gastric emptying in non-ulcer dyspepsia using a new ultrasonographic method. Scand J Gastroenterol. 1993;28:355–360. doi: 10.3109/00365529309090256. [DOI] [PubMed] [Google Scholar]
- 37.Ricci R, Bontempo I, Corazziari E, La Bella A, Torsoli A. Real time ultrasonography of the gastric antrum. Gut. 1993;34:173–176. doi: 10.1136/gut.34.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marzio L, Giacobbe A, Conoscitore P, Facciorusso D, Frusciante V, Modoni S. Evaluation of the use of ultrasonography in the study of liquid gastric emptying. Am J Gastroenterol. 1989;84:496–500. [PubMed] [Google Scholar]
- 39.Hveem K, Jones KL, Chatterton BE, Horowitz M. Scintigraphic measurement of gastric emptying and ultrasonographic assessment of antral area: relation to appetite. Gut. 1996;38:816–821. doi: 10.1136/gut.38.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stein WW, Brettel HF, Garten T. [Stomach volume determination using the ultrasonic B picture method] Munch Med Wochenschr. 1972;114:1871–1873. [PubMed] [Google Scholar]
- 41.Whittingham TA, Bateman DN. Measurement of stomach volume by real-time ultrasound. Ultrasound Med Biol. 1983;Suppl 2:459–463. [PubMed] [Google Scholar]
- 42.Liao D, Gregersen H, Hausken T, Gilja OH, Mundt M, Kassab G. Analysis of surface geometry of the human stomach using real-time 3-D ultrasonography in vivo. Neurogastroenterol Motil. 2004;16:315–324. doi: 10.1111/j.1365-2982.2004.00522.x. [DOI] [PubMed] [Google Scholar]
- 43.Gilja OH, Detmer PR, Jong JM, Leotta DF, Li XN, Beach KW, Martin R, Strandness DE Jr. Intragastric distribution and gastric emptying assessed by three-dimensional ultrasonography. Gastroenterology. 1997;113:38–49. doi: 10.1016/s0016-5085(97)70078-7. [DOI] [PubMed] [Google Scholar]
- 44.King PM, Adam RD, Pryde A, McDicken WN, Heading RC. Relationships of human antroduodenal motility and transpyloric fluid movement: non-invasive observations with real-time ultrasound. Gut. 1984;25:1384–1391. doi: 10.1136/gut.25.12.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hausken T, Odegaard S, Berstad A. Antroduodenal motility studied by real-time ultrasonography. Effect of enprostil. Gastroenterology. 1991;100:59–63. doi: 10.1016/0016-5085(91)90582-6. [DOI] [PubMed] [Google Scholar]
- 46.Hveem K, Hausken T, Svebak S, Berstad A. Gastric antral motility in functional dyspepsia. Effect of mental stress and cisapride. Scand J Gastroenterol. 1996;31:452–457. doi: 10.3109/00365529609006764. [DOI] [PubMed] [Google Scholar]
- 47.Hausken T, Berstad A. Wide gastric antrum in patients with non-ulcer dyspepsia. Effect of cisapride. Scand J Gastroenterol. 1992;27:427–432. doi: 10.3109/00365529209000100. [DOI] [PubMed] [Google Scholar]
- 48.Gregersen H, Gilja OH, Hausken T, Heimdal A, Gao C, Matre K, Ødegaard S, Berstad A. Mechanical properties in the human gastric antrum using B-mode ultrasonography and antral distension. Am J Physiol Gastrointest Liver Physiol. 2002;283:G368–G375. doi: 10.1152/ajpgi.00144.2001. [DOI] [PubMed] [Google Scholar]
- 49.Hausken T, Odegaard S, Matre K, Berstad A. Antroduodenal motility and movements of luminal contents studied by duplex sonography. Gastroenterology. 1992;102:1583–1590. doi: 10.1016/0016-5085(92)91717-i. [DOI] [PubMed] [Google Scholar]
- 50.Fujimura J, Haruma K, Hata J, Yamanaka H, Sumii K, Kajiyama G. Quantitation of duodenogastric reflux and antral motility by color Doppler ultrasonography. Study in healthy volunteers and patients with gastric ulcer. Scand J Gastroenterol. 1994;29:897–902. doi: 10.3109/00365529409094860. [DOI] [PubMed] [Google Scholar]
- 51.Hausken T, Gilja OH, Undeland KA, Berstad A. Timing of postprandial dyspeptic symptoms and transpyloric passage of gastric contents. Scand J Gastroenterol. 1998;33:822–827. doi: 10.1080/00365529850171477. [DOI] [PubMed] [Google Scholar]
- 52.Gilja OH, Heimdal A, Hausken T, Gregersen H, Matre K, Berstad A, Ødegaard S. Strain during gastric contractions can be measured using Doppler ultrasonography. Ultrasound Med Biol. 2002;28:1457–1465. doi: 10.1016/s0301-5629(02)00614-2. [DOI] [PubMed] [Google Scholar]
- 53.Matre K, Ahmed AB, Gregersen H, Heimdal A, Hausken T, Ødegaard S, Gilja OH. In vitro evaluation of ultrasound Doppler strain rate imaging: modification for measurement in a slowly moving tissue phantom. Ultrasound Med Biol. 2003;29:1725–1734. doi: 10.1016/j.ultrasmedbio.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 54.Hausken T, Thune N, Matre K, Gilja OH, Odegaard S, Berstad A. Volume estimation of the gastric antrum and the gallbladder in patients with non-ulcer dyspepsia and erosive prepyloric changes, using three-dimensional ultrasonography. Neurogastroenterol Mot. 1994;6:263–270. [Google Scholar]
- 55.Gilja OH, Hausken T, Odegaard S, Berstad A. Three-dimensional ultrasonography of the gastric antrum in patients with functional dyspepsia. Scand J Gastroenterol. 1996;31:847–855. doi: 10.3109/00365529609051991. [DOI] [PubMed] [Google Scholar]
- 56.Thune N, Hausken T, Gilja OH, Matre K. A practical method for estimating enclosed volumes using 3D ultrasound. Eur J Ultrasound. 1996;3:83–92. [Google Scholar]
- 57.Gilja OH, Thune N, Matre K, Hausken T, Odegaard S, Berstad A. In vitro evaluation of three-dimensional ultrasonography in volume estimation of abdominal organs. Ultrasound Med Biol. 1994;20:157–165. doi: 10.1016/0301-5629(94)90080-9. [DOI] [PubMed] [Google Scholar]
- 58.Gilja OH, Smievoll AI, Thune N, Matre K, Hausken T, Odegaard S, Berstad A. In vivo comparison of 3D ultrasonography and magnetic resonance imaging in volume estimation of human kidneys. Ultrasound Med Biol. 1995;21:25–32. doi: 10.1016/0301-5629(94)00082-4. [DOI] [PubMed] [Google Scholar]
- 59.Detmer PR, Bashein G, Hodges T, Beach KW, Filer EP, Burns DH, Strandness DE. 3D ultrasonic image feature localization based on magnetic scanhead tracking: in vitro calibration and validation. Ultrasound Med Biol. 1994;20:923–936. doi: 10.1016/0301-5629(94)90052-3. [DOI] [PubMed] [Google Scholar]
- 60.Leotta DF, Detmer PR, Gilja OH, Jong JM, Martin RW, Primozich JF. Three-dimensional ultrasound imaging using multiple magnetic tracking systems and miniature magnetic sensors. Proc IEEE Int Ultrasonics Symp Seattle WA USA. 1995:1415–1418. [Google Scholar]
- 61.Gilja OH, Hausken T, Olafsson S, Matre K, Odegaard S. In vitro evaluation of three-dimensional ultrasonography based on magnetic scanhead tracking. Ultrasound Med Biol. 1998;24:1161–1167. doi: 10.1016/s0301-5629(98)00098-2. [DOI] [PubMed] [Google Scholar]
- 62.Tefera S, Gilja OH, Olafsdottir E, Hausken T, Hatlebakk JG, Berstad A. Intragastric maldistribution of a liquid meal in patients with reflux oesophagitis assessed by three dimensional ultrasonography. Gut. 2002;50:153–158. doi: 10.1136/gut.50.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gregersen H, Kassab G. Biomechanics of the gastrointestinal tract. Neurogastroenterol Motil. 1996;8:277–297. doi: 10.1111/j.1365-2982.1996.tb00267.x. [DOI] [PubMed] [Google Scholar]
- 64.Berstad A, Gilja OH. Ultrasonographic alterations in functional dyspepsia. In: Odegaard S, Gilja OH, Gregersen H, eds. Basic and new aspects of gastrointestinal ultrasonography. 1st ed. World Sci. 2005:395–420. [Google Scholar]


