Abstract
In this article, we have reviewed the hepatic perfusion disorder (HPD), etiopathogenesis of HPD and corresponding diseases. Review of the literature was based on computer searches (PubMed, Index Medicus) and personal experiences. We considered HPD reflects perfusion differences due to redistribution of arterial blood flow among segments, subsegments and lobes of the liver. The plain CT scan findings of HPD manifests as triangular or wedge-shaped areas of low attenuation. On contrast-enhanced CT scan, HPD manifests multiple (or single) transient wedge-shaped, rotundloid or irregular appearance, homogeneous hyperattenuation (in less cases, hypoattenuation) during the hepatic arterial phase (HAP) and isoattenuated or slightly hyperattenuated areas during the portal arterial phase. Dynamic enhanced magnetic resonance (MR) features are similar to enhanced CT scan. Angiographic findings include non-opacification of portal vein on portograms or wedge-shaped segmental staining in arterial and parenchymal phases on hepatic angiograms. The causes of HPD are arterioportal shunts (APS), intrahepatic vascular compressions and portal vein occlusion, steal phenomenon by hypervascular tumors, vascular variations and any other unknown reasons. It is very important for radiologists to be familiar with the various appearances of HPD to avoid false-positive diagnosis of pseudolesions and not to overestimate the extent of the disease.
Keywords: Etiopathogenesis, Hepatic perfusion disorders, Diseases
INTRODUCTION
Definition of HPD
Hepatic perfusion disorder (HPD) refers to perfusion differences among segments, subsegments and lobes of the liver caused by various etiologies. It is usually transient peripheral and triangular, wedge-shaped or rotundloid hepatic parenchymal enhancement during the hepatic arterial phase (HAP) and returns to normal attenuation/intensity on portal venous phase (PVP) on CT and MR dynamic enhancement, and segmental staining or segmental perfusion defect on angiograms. It usually has a straight margin, and contains normal vessels and without mass effect. With the improvement of temporal resolution of CT and MR, detection rate of this phenomenon has increased recently. However, the nomenclature of this phenomenon is different in different imaging modalities, HPD is a good nomenclature for this phenomenon suitable for any other imaging modalities. This article presents the nomenclature and history of hepatic perfusion disorders and their spectrum with etiopathogenesis.
Nomenclature and history
In 1981, Inamoto et al[1] and Nishikawa et al[2] first described segmental low attenuation areas within the liver not corresponding to mass lesions. This phenomenon was attributed to decreased portal flow. In 1982, Itai et al[3] reported transient hepatic attenuation difference (THAD) during the HAP on CT, and explained the pathophysiology and etiology of this phenomenon. In 1984, Matsui et al[4] described segmental staining on hepatic angiograms and portal vein occlusion on portograms (a sign of intrahepatic portal vein obstruction) in liver tumor cases. They also found that the areas of segmental staining on hepatic angiograms were the ones of hepatic parenchymal enhancement during the HAP on CT. In 1988, Itai et al[5] reported the findings of segmental intensity difference (SID) on MR images. They found that the SID was defined as a zone of homogeneously long T1 and long T2 signal intensity with segmental or subsegmental distribution not corresponding to the areas of the mass. In cases of SID, they studied MR images combined with other images, such as CT scans, ultrasound (US) and angiography, for corresponding abnormalities. The areas of SID were trapezoid hypoechoic areas contacting with the hepatic contour as disclosed on US studies. They also found that many cases with wedge-shaped defects showed by portography and segmental staining on arteriography revealed no areas of low attenuation on plain CT and MR images and no pathologic differences at microscpic examination. In 1997, Gryspeerdt et al[6] reviewed the phenomenon of hepatic perfusion differences on dual-phase spiral CT scan, and first nominated it as hepatic perfusion disorders (HPDs). They considered that various HPDs are related to portal venous inflow obstruction, hepatic venous outflow obstruction (e.g., Budd-Chiari syndrome, cardiac failure, mediastinal fibrosis), mediastinal or thoracic venous inlet obstruction, focal liver lesions, inflammatory processes, normal anatomic variants in the hepatic blood supply, altered hemodynamics after the placement of a transjugular intrahepatic portosystemic shunt, and uncertain causes. In the same year, Lee et al[7] observed the correlation between the arterioportal shunt caused by liver biopsy injury and wedge-shaped early transient enhancement phenomenon of the liver during helical dynamic CT in 21 patients, and nominated it as transient subsegmental parenchymal enhancement (TSPE). After that, many authors reported this phenomenon as THAD and HPD[8-14]. However, THAD reflects an enhanced, redistributing arterial flow to a hepatic segment or lobe on CT; it cannot reflect other imaging modality findings, such as segmental staining on arteriogram, trapezoid hypoechoic areas on US and SID on MR. In our opinion, HPD is a good nomenclature for this phenomenon suitable for any other imaging modalities.
Imaging features
The plain CT scan findings of HPD manifests as triangular or wedge-shaped areas of low attenuation. The metabolic pathophysiology of the phenomenon is decreased glycogen and subsequent increase of fat and/or edema secondary to venous inflow obstruction due to portal branch occlusion. On contrast-enhanced CT scan, HPD manifested multiple (or single) transient triangular, wedge-shaped, rotundloid or irregular appearance, homogeneous hyperattenuation (in less cases, hypoattenuation when the hepatic artery is compressed or occluded) during the hepatic arterial phase (HAP) and isoattenuated or slightly hyperattenuated areas during the portal arterial phase (PVP) (Figures 1 and 2). Plain MR scan is defined as a segmental or subsegmental iso-intensity on T1- and T2-weighted images (in less cases, long T1 and long T2 signal intensity). Dynamic enhanced MR features are similar to enhanced CT scan. Angiographic findings included non-opacification of portal vein (a sign of intrahepatic portal vein obstruction) on portograms or wedge-shaped segmental staining in arterial and parenchymal phases on hepatic angiograms, and corresponding features are seen if there is an occlusion of hepatic vein or aberrant blood supply. There lacks special report of US features about HPD yet, trapezoid hypoechoic areas on US were found corresponding to SID on MR or THAD on CT images[6]. There is also no report about real-time contrast-enhanced US features of HPD as yet.
Figure 1.
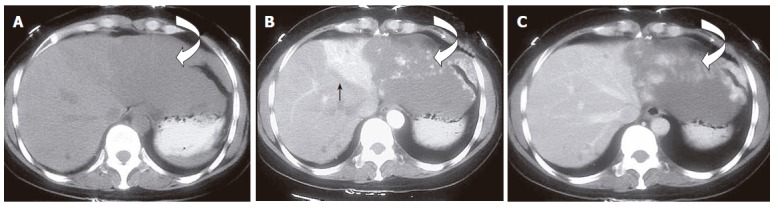
HPD in a 48-year-old woman with cavernous hemangioma. A: Pre- contrast administration transverse CT scan shows a large well-defined hypo-attenuating lesion located in segment II(curved open arrow); B: HAP CT scan shows a nodular enhanced hemangioma (curved open arrow) and wedge-shaped segmental homogeneous hyperattenuating areas (solid arrow) adjacent to the tumor; C: PVP CT scan shows the still nodular enhanced hemangioma (curved) and the peripheral area resumed isoattenuating.
Figure 2.
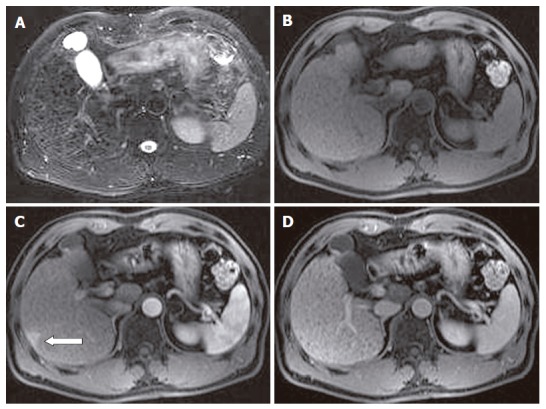
HPD in a 56-year-old man with liver cirrhosis. A: Fat-saturated breath-hold turbo FSE T2-weighted transverse MR scan shows multiple punctuate hypointensity cirrhotic nodules and surrounding reticulated fibrotic liver parenchyma, without any obvious hyperintense tumoral lesions; B: pre- contrast administration transverse spoiled gradient-echo T1-weighted MR image (118/4.1; flip angle, 80°) shows no obvious hypointense tumoral lesions observed; C: transverse contrast-enhanced T1-weighted MR image obtained during HAP shows a subcapsular small patchy hyperintense tumor-like lesion (pseudolesion) (open arrow); D: transverse contrast-enhanced T1-weighted MR image obtained during PVP shows no lesion in that area.
PATHOGENESIS OF HPD
HPDs may be noted to accompany tumors; however, they may occur due to non-tumor vascular reasons as well. Among the reasons of HPD are arterioportal shunts, intrahepatic vascular compression and occlusion, steal phenomenon by hypervascular tumors, vascular abnormalities and hereditary hemorrhagic telangiectasia, and any other unknown reasons (Table 1).
Table 1.
The causes of HPD
| The causes of HPD |
| Arterioportal shunts |
| Trauma |
| Neoplasms |
| Malignant tumors: HCC, cholangiocarcinoma, metastases |
| Benign tumors: hemangioma, FNH |
| Interventional procedures |
| Biopsy |
| Biliary and abscess drainage |
| Various physical treatment of hepatic tumor |
| Percutaneous transhepatic cholangioscopy |
| TIPS |
| Liver cirrhosis |
| Congenital APS |
| Intrahepatic vascular compression and occlusion |
| Neoplasms |
| Malignant tumors: HCC, cholangiocarcinoma, metastases |
| Benign tumors: hemangioma, FNH |
| Inflammatory changes |
| Hepatic abscess, acute cholecystitis, cholangitis. |
| Focal eosinophilic necrosis |
| Hepatic parenchymal compression |
| Rib compression |
| Perihepatic peritoneal tumors |
| Pseudomyxoma peritonei |
| Perihepatic fluid collections |
| Others |
| Right-sided heart failure |
| Pericardial disease |
| Budd-Chiari syndrome |
| Mediastinal fibrosis |
| Steal phenomenon by hypervascular tumors |
| HCC |
| Hypervascular metastases: islet cell tumors, carcinoids, renal cell carcinoma, and breast cancer |
| Vascular abnormalities and hereditary hemorrhagic telangiectasia |
| Vascular variabilities: capsular vein, accessory cystic vein, aberrant right gastric vein |
| Hereditary hemorrhagic telangiectasia |
| Unknown causes |
Arterioportal shunts
A distinctive feature of the liver is its unique dual blood supply, which comes from the hepatic artery (25%) and the portal vein (75%). There can be several potential communications between the vessels, including transsinusoidal, transvasal and transplexal (peribiliary) routes (Figure 3). In some pathologic cases, an organic or functional communication between a hepatic arterial branch and the portal venous system occurs, resulting in redistribution of arterial flow into a focal region of portal venous flow due to high pressure in hepatic artery and low pressure in portal branch. On dynamic enhanced CT/MR scan or hepatic arteriography, HPD manifests as a transient area of high attenuation/intensity or segmental staining due to passage of contrast material from arterial blood into portal vein branch, thus enhancing/staining a focal area of the liver before the adjacent parenchyma is enhanced/stained through the portal venous system. The areas with APS are enhanced or stained intensively due to hyperperfusion; in contrast, the other areas without APS are enhanced or stained normally due to normal perfusion. The helical CT or MR findings of APS are as follows: (1) Early enhancement of the peripheral portal vein branches during the HAP and before the main portal vein is enhanced; and (2) enhancement of the peripheral portal vein branches and main portal vein without enhancement of the superior mesenteric and splenic veins. Hepatic arteriographic findings of APS are early visualization of small portal branches when hepatic artery is visualized.
Figure 3.
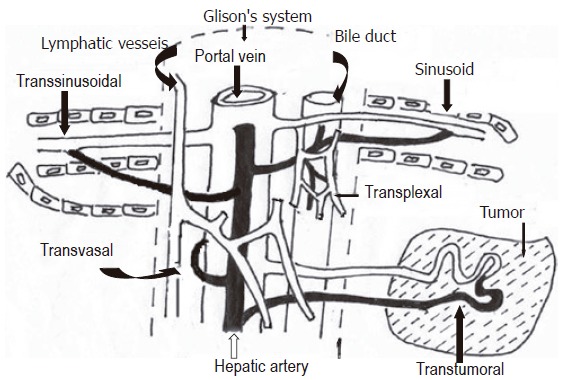
Schematic drawings showing hepatic microvasculature and arterioportal anastomoses or arterioportal shunts, including the transsinusoidal route (between the interlobular arterioles and portal venules or sinusoids) and the transplexal route (peribiliary plexus), transvasal route (perilymphatic vessels) and transtumoral route.
The causes of APS include: (1) Trauma: Abdominal trauma sometimes causes an organic communication between the arterial and portal venous systems due to vascular rupture or produces functional APS due to portal or hepatic vein thrombosis; (2) Neoplasms: Hepatic neoplasms include both malignant tumors such as HCC, cholangiocarcinoma and various hypervascular metastases and benign tumors such as hemangioma and focal nodular hyperplasia (FNH)[14]. HCC is either the most common malignancy of the liver or the most common cause of HPD. In cases of peripheral small HCC, APS is induced via the transtumoral route, and in cases of large HCC, APS is induced via the transvasal route (due to portal vein tumor thrombosis), the transtumoral route (through the tumor itself), or the transsinusoidal route (between microscopic hepatic arterioles and portal venules distal to portal vein compression or thrombosis) and a transplexal (peribiliary) route. Cholangiocarcinoma may cause APS when the portal or hepatic vein is compromised. Hypervascular metastasis may cause APS similar to HCC. It was considered that hepatic hemangioma seldom causes APS; however, recent studies have shown that there is transtumoral route of an arterioportal shunt between the hepatic artery and the portal vein[17-19]. The arterioportal shunt of a hemangioma is somewhat different from that of an HCC because most HCCs accompanying an arterioportal shunt tend to be large tumors with portal vein invasion. In small hepatic lesions < 3 cm, the incidence of arterioportal shunt is significantly higher in a small hemangioma than in a small HCC[20]. Small hemangioma with large arterial flow and flash filling has APS and shows HPD more frequently than a large one[17,18]. FNH is supplied by an anomalous enlarged hepatic artery and is neither supplied nor drained by the portal vein. We found that FNH showed HPD in two cases, although the pathogenesis is unknown. There was neither HPD observed in our practice nor articles reported in hepatic adenoma whether it may show HPD is unknown yet; (3) Interventional procedures: Interventional procedures (e.g., hepatic biopsy, biliary and abscess drainage, various physical treatment of hepatic tumor, percutaneous transhepatic cholangioscopy, and transjugular intrahepatic porto-systemic stent shunt) can produce iatrogenic arterioportal fistulas due to portal vein injury[21,22]; (4) Liver cirrhosis: Liver cirrhosis is caused mainly by parenchymal necrosis, which is followed by deposition of connective tissue, nodular hepatocyte regeneration, and distortion of the lobular and vascular hepatic architecture, and false lobules, producing portal hypertension. Liver cirrhosis is known to alter normal hepatic blood flow dynamics, resulting in increased arterial flow and decreased portal venous flow to the liver. APS is believed to be secondary to occlusion of the small hepatic venules and retrograde filling of the small portal vein branches by way of arterioportal anastomoses (transsinusoidal route)[23]. In addition, hypertrophy of the peribiliary plexus and direct anastomosis in the peripheral area of the liver are another routes of APS. Due to false lobules formation and distortion of the vascular hepatic architecture, HPD may appear as small enhancing nodules during HAP in cirrhotic patients and may be confused with small hepatocellular carcinomas. A correct diagnosis can be made by observing the portal phase (rapid wash out with hypoattenuating lesion in HCC, isoattenuating in case of HPD at CT) and the lack of T2 hyperintensity at MRI. MR with reticuloendothelial contrast agents (supermagnetic iron oxide, SPIO) may also be of help (signal loss in HCC, no signal loss in case of HPD); (5) Congenital APS: Some congenital hepatic diseases, such as infantile hepatic hemangioma, arteriovenous malformations (AVMs) and infradiaphragmatic total anomalous pulmonary venous return (TAPVR), can also be associated with APS.
Intrahepatic vascular compressions and occlusion
Intrahepatic vascular includes hepatic artery, portal and hepatic vein, and may be compressed and occluded by many causes: (1) Compressions and occlusion of hepatic artery: As a result of the compression and occlusion of hepatic artery, the hemodynamic balance between the portal vein and the hepatic artery in the affected lobe or segment may change. Different from common features of HPD, areas of hypoattenuation/intensity may be seen on contrast-enhanced CT or MR images and segmental staining defect may be seen on hepatic arteriograms due to decrease in the blood flow of the affected hepatic artery[16]; (2) Compression and obstruction of portal vein: When the compression and obstruction of portal vein occurs, perfusion alterations are produced by increases in arterial flow through transsinusoidal, transvasal, transtumoral, and especially transplexal (peribiliary) routes to compensate for the diminished portal venous flow (functional APS) and by decreased dilution of the contrast material by the non-enhanced portal venous flow[10,14,16]; (3) Compressions and obstruction of hepatic vein: Occlusion of the hepatic veins results in increased sinusoidal pressure and reverses the pressure gradient between the sinusoidal and portal veins. The portal vein then becomes a draining vein and there is an increase in hepatic arterial flow, resulting in a functional APS, as in liver cirrhosis[16].
The causes of compression and obstruction of intrahepatic vessels include: (1) Neoplasms: Hepatic tumors are either sometimes associated with portal vein compromise and or, less frequently, with hepatic vein and artery compromise. As a result of the invasion of the hepatic artery due to tumoral compression and encasement, the blood flow in the compromised areas decreases. The invasion of the portal and hepatic vein due to tumor may result in obstruction due to tumor thrombosis, blood flow decrease or stasis[10]; (2) Inflammatory changes: Local inflammation can cause hyperemia of the hepatic artery and stoppage of regional portal or hepatic venous flow, as in cases of hepatic abscess, acute cholecystitis, cholangitis. The compromised areas include both the inflamed lesion and the surrounding parenchyma[16]. Recently, there is a report that focal eosinophilic necrosis may cause HPD. Pathologically, focal eosinophilic necrosis is a focal area of hepatocellular necrosis caused by severe eosinophilic infiltration of perivascular space. Therefore, one may assume that eosinophilic infiltration of the perivascular space may be the cause of the stoppage of regional portal venous flow, portal thrombosis and occlusion[14]; (3) Hepatic parenchymal compression: When there is increased pressure on the hepatic parenchyma, blood flow through the portal vein is reduced due to portal venous low pressure system and consequently, increased arterial inflow to the affected hepatic segment due to the high pressure arterial system[11]. The causes of hepatic parenchymal compression include rib compression (in some cases, the medially concave rib may constantly compress the hepatic parenchyma), perihepatic peritoneal tumors, such as pseudomyxoma peritonei, and perihepatic fluid collections. This transient hemodynamic change is reversible when the compression is removed; (4) Others: Other causes of compressions and obstruction of intrahepatic vessels include right-sided heart failure, pericardial diseases, Budd-Chiari syndrome, or mediastinal fibrosis, which may result in hepatic vein occlusion[10]. In patients with right-sided heart failure, the contrast agent can be seen within the hepatic veins during HAP due to decreased hepatic vein flow, while during PVP stagnation of the contrast agent within the sinusoids may give rise to a mottled appearance of the parenchyma.
Steal phenomenon by hypervascular tumors
Hypervascular tumors usually include HCC and hypervascular metastases, such as islet cell tumors, carcinoids, renal cell carcinoma, and breast cancer. These hypervascular tumors may result in “hypertrophy” of the hepatic arterial blood supply to the lobe or segment of the liver containing the tumor, and can “steal” arterial blood from the surrounding parenchyma due to siphoning effect, which is similar to the phenomenon of stealing blood caused by AVMs. Then the hepatic parenchyma adjacent to the tumor can receive more than usual arterial blood supply and the perfusion of the remainder of the lobe is reduced. The net effect of this stealing depends on the tumor location, degree of tumor vascularity, and ratio of tumor to parenchyma blood supply[10,25,26].
Vascular abnormalities and hereditary hemorrhagic telangiectasia
Vascular variabilities, such as capsular veins drain into adjacent hepatic sinusoids, accessory cystic veins drain into the liver parenchyma of segments IV-V, parabiliary system from the head of the pancreas, duodenum and distal stomach drain into the posterior part of segment IV, veins from the gastric antrum and pancreatic head into segments I and IV, which are third hepatic inflow tracts, may drain the systemic venous circulation into the liver[27-29]. Focal intensively enhanced areas are seen on HAP images of CT or MR, segmental staining is seen on arteriogram because of the early inflow of contrast material compared with the inflow into the surrounding parenchyma, which receives contrast material mainly from the splenic and superior mesenteric veins. Common locations of the HPD caused by vascular variations are adjacent to the gallbladder fossa, anterior to the porta hepatis, adjacent to the falciform ligament, and in the subcapsular area. These HPDs might appear either wedge-shaped and triangular; in less cases, they appear nodular, it makes difficult to differentiate from a true lesion, especially located in subcapsular areas[10]. Sometimes, hepatic arterial supply derived from the cystic artery (hepatic branch artery-ramus profundus) can also produce a hyper-perfusion in a pericystic location during HAP, similar to those produced by the cystic vein.
Hereditary hemorrhagic telangiectasia (HHT, Osler-Weber-Rendu disease) is a vascular disease with autosomal dominant transmission characterized by multiple telangiectases, which are thin-walled, dilated vascular channels with arteriovenous communications. HHT affects mucocutaneous tissue most frequently, but any part of the body can be affected, including the liver. The hepatic changes, including widened and tortuous hepatic arteries, telangiectases, arteriovenous and portovenous fistulas, connective tissue formation with fibrosis and atypical cirrhosis, high cardiac output, secondary congestive heart failure due to a left-to-right intrahepatic shunt, portal hypertension, gastrointestinal hemorrhage, ascites, or encephalopathy[30-32]. APSs are nearly universal in HHT, and HPDs often occur. Contrast-enhanced CT or MR shows heterogeneous perfusion of the hepatic parenchyma with multiple, peripheral, wedge-shaped or irregular areas of intensively enhanced areas during the HAP. Angiography shows diffuse mottled capillary blush with multiple segmental or subsegmental staining.
CONCLUSION
HPDs reflect a hemodynamic change in the normal dual blood supply of the liver in area of surrounding lesion. The nature of HPDs is perfusion differences due to redistribution of arterial blood flow among segments, subsegments and lobes of the liver. Among the reasons of HPD are arterioportal shunts, vascular compression and occlusion, steal phenomenon by hypervascular tumors, vascular variations and any other unknown reasons. It is very important for radiologists to be familiar with the various appearances of HPD to avoid false-positive diagnosis of pseudolesions and not to overestimate the extent of the disease. Because knowing the characteristics of HPDs and differentiating them may prevent the tumor diameter from being measured larger than they actually are in the case of hypervascular tumors such as HCC.
Footnotes
S- Editor Pan BR L- Editor Kumar M E- Editor Bi L
References
- 1.Inamoto K, Sugiki K, Yamasaki H, Miura T. CT of hepatoma: effects of portal vein obstruction. AJR Am J Roentgenol. 1981;136:349–353. doi: 10.2214/ajr.136.2.349. [DOI] [PubMed] [Google Scholar]
- 2.Nishikawa J, Itai Y, Tasaka A. Lobar attenuation difference of the liver on computed tomography. Radiology. 1981;141:725–728. doi: 10.1148/radiology.141.3.6272353. [DOI] [PubMed] [Google Scholar]
- 3.Itai Y, Moss AA, Goldberg HI. Transient hepatic attenuation difference of lobar or segmental distribution detected by dynamic computed tomography. Radiology. 1982;144:835–839. doi: 10.1148/radiology.144.4.6287520. [DOI] [PubMed] [Google Scholar]
- 4.Matsui O, Takashima T, Kadoya M, Kitagawa K, Kamimura R, Itoh H, Suzuki M, Ida M. Segmental staining on hepatic arteriography as a sign of intrahepatic portal vein obstruction. Radiology. 1984;152:601–606. doi: 10.1148/radiology.152.3.6087404. [DOI] [PubMed] [Google Scholar]
- 5.Itai Y, Ohtomo K, Kokubo T, Okada Y, Yamauchi T, Yoshida H. Segmental intensity differences in the liver on MR images: a sign of intrahepatic portal flow stoppage. Radiology. 1988;167:17–19. doi: 10.1148/radiology.167.1.2831561. [DOI] [PubMed] [Google Scholar]
- 6.Gryspeerdt S, Van Hoe L, Marchal G, Baert AL. Evaluation of hepatic perfusion disorders with double-phase spiral CT. Radiographics. 1997;17:337–348. doi: 10.1148/radiographics.17.2.9084076. [DOI] [PubMed] [Google Scholar]
- 7.Lee SJ, Lim JH, Lee WJ, Lim HK, Choo SW, Choo IW. Transient subsegmental hepatic parenchymal enhancement on dynamic CT: a sign of postbiopsy arterioportal shunt. J Comput Assist Tomogr. 1997;21:355–360. doi: 10.1097/00004728-199705000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Chen JH, Chen WP, Huang CL, Shen WC. Dynamic helical CT as a novel technique for diagnosing hepatic perfusion disorders. Hepatogastroenterology. 1999;46:303–307. [PubMed] [Google Scholar]
- 9.Yamasaki M, Furukawa A, Murata K, Morita R. Transient hepatic attenuation difference (THAD) in patients without neoplasm: frequency, shape, distribution, and causes. Radiat Med. 1999;17:91–96. [PubMed] [Google Scholar]
- 10.Quiroga S, Sebastià C, Pallisa E, Castellà E, Pérez-Lafuente M, Alvarez-Castells A. Improved diagnosis of hepatic perfusion disorders: value of hepatic arterial phase imaging during helical CT. Radiographics. 2001;21:65–81; questionnaire 288-294. doi: 10.1148/radiographics.21.1.g01ja0165. [DOI] [PubMed] [Google Scholar]
- 11.Colagrande S, Carmignani L, Pagliari A, Capaccioli L, Villari N. Transient hepatic attenuation differences (THAD) not connected to focal lesions. Radiol Med. 2002;104:25–43. [PubMed] [Google Scholar]
- 12.Colagrande S, Centi N, Carmignani L, Salvatore Politi L, Villari N. [Meaning and etiopathogenesis of sectorial transient hepatic attenuation differences (THAD)] Radiol Med. 2003;105:180–187. [PubMed] [Google Scholar]
- 13.Colagrande S, Centi N, La Villa G, Villari N. Transient hepatic attenuation differences. AJR Am J Roentgenol. 2004;183:459–464. doi: 10.2214/ajr.183.2.1830459. [DOI] [PubMed] [Google Scholar]
- 14.Kim HJ, Kim AY, Kim TK, Byun JH, Won HJ, Kim KW, Shin YM, Kim PN, Ha HK, Lee MG. Transient hepatic attenuation differences in focal hepatic lesions: dynamic CT features. AJR Am J Roentgenol. 2005;184:83–90. doi: 10.2214/ajr.184.1.01840083. [DOI] [PubMed] [Google Scholar]
- 15.Doppman JL, Dwyer A, Vermess M, Girton M, Sugarbaker P, Miller D, Cornblath M. Segmental hyperlucent defects in the liver. J Comput Assist Tomogr. 1984;8:50–57. doi: 10.1097/00004728-198402000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Köseoğlu K, Taşkin F, Ozsunar Y, Cildağ B, Karaman C. Transient hepatic attenuation differences at biphasic spiral CT examinations. Diagn Interv Radiol. 2005;11:96–101. [PubMed] [Google Scholar]
- 17.Jeong MG, Yu JS, Kim KW. Hepatic cavernous hemangioma: temporal peritumoral enhancement during multiphase dynamic MR imaging. Radiology. 2000;216:692–697. doi: 10.1148/radiology.216.3.r00se08692. [DOI] [PubMed] [Google Scholar]
- 18.Kim KW, Kim TK, Han JK, Kim AY, Lee HJ, Choi BI. Hepatic hemangiomas with arterioportal shunt: findings at two-phase CT. Radiology. 2001;219:707–711. doi: 10.1148/radiology.219.3.r01ma05707. [DOI] [PubMed] [Google Scholar]
- 19.Chen JH, Shen WC. Hyperdynamic hemangioma with proximal arterioportal shunting: a rare manifestation. Eur Radiol. 2003;13:1920–1922. doi: 10.1007/s00330-002-1688-4. [DOI] [PubMed] [Google Scholar]
- 20.Byun JH, Kim TK, Lee CW, Lee JK, Kim AY, Kim PN, Ha HK, Lee MG. Arterioportal shunt: prevalence in small hemangiomas versus that in hepatocellular carcinomas 3 cm or smaller at two-phase helical CT. Radiology. 2004;232:354–360. doi: 10.1148/radiol.2322030966. [DOI] [PubMed] [Google Scholar]
- 21.Kim SK, Lim HK, Kim YH, Lee WJ, Lee SJ, Kim SH, Lim JH, Kim SA. Hepatocellular carcinoma treated with radio-frequency ablation: spectrum of imaging findings. Radiographics. 2003;23:107–121. doi: 10.1148/rg.231025055. [DOI] [PubMed] [Google Scholar]
- 22.Dromain C, de Baere T, Elias D, Kuoch V, Ducreux M, Boige V, Petrow P, Roche A, Sigal R. Hepatic tumors treated with percutaneous radio-frequency ablation: CT and MR imaging follow-up. Radiology. 2002;223:255–262. doi: 10.1148/radiol.2231010780. [DOI] [PubMed] [Google Scholar]
- 23.Wachsberg RH, Bahramipour P, Sofocleous CT, Barone A. Hepatofugal flow in the portal venous system: pathophysiology, imaging findings, and diagnostic pitfalls. Radiographics. 2002;22:123–140. doi: 10.1148/radiographics.22.1.g02ja20123. [DOI] [PubMed] [Google Scholar]
- 24.Gallego C, Miralles M, Marín C, Muyor P, González G, García-Hidalgo E. Congenital hepatic shunts. Radiographics. 2004;24:755–772. doi: 10.1148/rg.243035046. [DOI] [PubMed] [Google Scholar]
- 25.Colagrande S, Carmignani L, Pagliari A, Capaccioli L, Villari N. Siphoning effect and steal phenomenon combined to focal hepatic lesions on spiral CT. Four cases report. Radiol Med. 2002;103:267–274. [PubMed] [Google Scholar]
- 26.Kanematsu M, Hoshi H, Yamada T, Nandate Y, Kato M, Yokoyama R, Murakami T, Nakamura H. Overestimating the size of hepatic malignancy on helical CT during arterial portography: equilibrium phase CT and pathology. J Comput Assist Tomogr. 1997;21:713–719. doi: 10.1097/00004728-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Deneve E, Caty L, Fontaine C, Guillem P. Simultaneous aberrant left and right gastric veins draining directly into the liver. Ann Anat. 2003;185:263–266. doi: 10.1016/S0940-9602(03)80037-7. [DOI] [PubMed] [Google Scholar]
- 28.Caty L, Denève E, Fontaine C, Guillem P. Concurrent aberrant right gastric vein directly draining into the liver and variations of the hepatic artery. Surg Radiol Anat. 2004;26:70–73. doi: 10.1007/s00276-003-0191-1. [DOI] [PubMed] [Google Scholar]
- 29.Ohkubo M. Aberrant left gastric vein directly draining into the liver. Clin Anat. 2000;13:134–137. doi: 10.1002/(SICI)1098-2353(2000)13:2<134::AID-CA7>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 30.Memeo M, Stabile Ianora AA, Scardapane A, Buonamico P, Sabbà C, Angelelli G. Hepatic involvement in hereditary hemorrhagic telangiectasia: CT findings. Abdom Imaging. 2004;29:211–220. doi: 10.1007/s00261-003-0101-3. [DOI] [PubMed] [Google Scholar]
- 31.Ianora AA, Memeo M, Sabba C, Cirulli A, Rotondo A, Angelelli G. Hereditary hemorrhagic telangiectasia: multi-detector row helical CT assessment of hepatic involvement. Radiology. 2004;230:250–259. doi: 10.1148/radiol.2301021745. [DOI] [PubMed] [Google Scholar]
- 32.Ravard G, Soyer P, Boudiaf M, Terem C, Abitbol M, Yeh JF, Brouard R, Hamzi L, Rymer R. Hepatic involvement in hereditary hemorrhagic telangiectasia: helical computed tomography features in 24 consecutive patients. J Comput Assist Tomogr. 2004;28:488–495. doi: 10.1097/00004728-200407000-00009. [DOI] [PubMed] [Google Scholar]


