Abstract
Background
The aim of this study was to analyze the influence of active and passive smoking on cardiorespiratory responses in asymptomatic adults during a sub-maximal-exertion incremental test.
Methods
The participants (n = 43) were divided into three different groups: active smokers (n = 14; aged 36.5 ± 8 years), passive smokers (n = 14; aged 34.6 ± 11.9 years) and non-smokers (n = 15; aged 30 ± 8.1 years). They all answered the Test for Nicotine Dependence and underwent anthropometric evaluation, spirometry and ergospirometry according to the Bruce Treadmill Protocol.
Results
VO2max differed statistically between active and non-smokers groups (p < 0.001) and between non-smokers and passive group (p=0.022). However, there was no difference between the passive and active smokers groups (p=0.053). Negative and significant correlations occurred between VO2max and age (r = - 0.401, p = 0.044), percentage of body fat (r = - 0.429, p = 0.011), and waist circumference (WC) (r = - 0.382, p = 0.025).
Conclusion
VO2max was significantly higher in non-smokers compared to active smokers and passive smokers. However, the VO2max of passive smokers did not differ from active smokers.
Keywords: Cardiovascular diseases, Exercise test, Oxygen consumption, Smoking
Background
Cardiorespiratory impairment increases morbidity and is an independent predictor of all-cause mortality [1]. Individuals with low cardiorespiratory capacity are more likely to develop systemic arterial hypertension (SAH) [2], diabetes [3], and metabolic syndrome [4] and have high mortality rates due to cardiovascular disease [5] and cancer (CA) [6] than individuals with high cardiorespiratory capacity. One way to evaluate cardiorespiratory ability is through the cardiopulmonary exercise test (CPET) or ergospirometry. Its effectiveness lies in its reflection of the strength of the cardiorespiratory system and its changes during exercise. One of the parameters used to estimate cardiopulmonary functional capacity is the maximum consumption of oxygen (VO2max) [7,8]. VO2max reflects the maximum capacity of absorption, transportation and consumption of oxygen (O2). VO2max is the most influential parameter of a person’s physical conditioning and is an independent and objective measure for the prognosis of cardiovascular disease [8,9].
Smoking affects the response to the CPET [10,11]. Smokers have lower aerobic capacity and, thus, less oxygen supply while they are exercising. Smoking also requires an additional energetic cost, which is caused by greater respiratory muscle work. Quitting smoking and practicing physical activities regularly can make aerobic function return to normal values [12]. The effects of passive smoking on cardiorespiratory capacity, however, are rarely addressed. A recent randomized clinical trial identified cardiorespiratory and immunological changes in healthy non-smoking individuals; these changes appeared immediately after they were exposed to cigarette smoke [13]. In 2008, Ren et al. [14] performed one of the first studies to evaluate the hemodynamics and cardiopulmonary function of flight attendants who were exposed to cigarette smoke for over five years. These authors noted a connection between passive smoking and SAH, but they did not show significant cardiopulmonary impairment.
Therefore, the main goal of this study was to analyze the influences that active and passive smoking have on cardiorespiratory responses in asymptomatic adults throughout a sub-maximal-exertion incremental test on a treadmill.
Methods
This transversal study was composed of smokers, non-smokers and passive smokers, aged between 18 and 50 years and of both genders. In this study, among participants active smokers were considered those who had smoked at least five cigarettes/day for 10 years prior to the study (active smoker group); whereas passive smokers were those who lived with at least one smoker or interacted with a smoker at work for at least three years prior to the study (passive smoker group); and the non-smokers were those who had never smoked (non-smoker group). Individuals who had cardiorespiratory disease, trauma-orthopedic dysfunction, diabetes or CA were excluded from the study, as were ex-smokers and individuals who had been exposed to toxic inhalants.
The study enrolled 43 adults from the target population. To calculate the sample size, we evaluated a difference in the average cardiorespiratory function in six subjects, considering a standard deviation of 5%, a statistical power of 90% and confidence interval of 95% [15]. This study was approved by the Research Ethics Committee of the University of Santa Cruz do Sul, and free informed consent was obtained under protocol number 2682/2010 from every participant.
Initially, the level of nicotine dependence was evaluated using the Fagerström Test for Nicotine Dependence (FTND) [16-19]. The number of years the individuals smoked and, in case of passive smoking, the period they were exposed to cigarette smoke (minutes/day and the number of years) were also recorded [20,21]. All exams were performed by qualified professionals.
Anthropometric evaluation
The anthropometric evaluation was performed by measuring body mass (kg) and height (cm) using an anthropometric scale. Body mass index (BMI) was calculated following the criteria established by the World Health Organization [22]. Using a non-elastic measuring tape, waist circumference (WC) was measured bilaterally at the midpoint between the iliac crest and the lower costal margin, according to the criteria proposed by Heyward [23], and was classified according to the 1st Brazilian Guideline for Metabolic Syndrome Diagnosis and Treatment [24].
To determine the body fat percentage (%F), seven skin folds were measured. These measures were different for men and women, according to Jackson and Pollock’s protocol [25,26], and were performed with the Lange® Caliper (Multimed, Skinfold Caliper, Gays Mills, WI, USA). Measures were taken three times in a rotational sequence to obtain an average for each individual at each location. Jackson and Pollock’s approach [25] was used to calculate body density (BD), and the Siri equation was used to obtain %F.
Lung function evaluation
Lung function was evaluated using a portable spirometer (EasyOne®, Model 2001 Diagnostic Spirometer, NDD Medical Technologies, Andover, MA, USA) following the protocol of the American Thoracic Society [27]. The following variables were evaluated: forced vital capacity (FVC), forced expiratory volume (VEF1), VEF1/FVC ratio and peak expiratory flow (PEF). The curves for these parameters were compared to reference values for this population [28].
Cardiorespiratory capacity
Treadmill cardiopulmonary exercise testing was performed using the Bruce protocol [9] and was used to identify and classify cardiorespiratory capacity (Ecafix® EG treadmill-700X, São Paulo, SP, Brazil). An aneroid sphygmomanometer was used to measure systolic arterial pressure (SAP) and diastolic arterial pressure (DAP) every 3 minutes throughout the test [29] and respiratory gas analysis was recorded continuously throughout the test. Simultaneous, respiratory gas analysis was performed using breath by breath analysis of O2 and CO2 on a TEEM 100 Metabolic Analysis System® instrument (Aero Sport, Ann Arbor, MI, USA), as previously validated by Novitsky [30]. All exams were performed in the morning at a controlled room temperature. The oxygen and carbon dioxide sensors were calibrated before each exercise test [31]. The VO2max was defined as the maximum O2 consumption reached during the last minutes of exercise during the exertion test. VO2max was estimated, and the participants were classified according to their functional capacity, following criteria established by Pollock and Wilmore [32]. VO2max was normalized to age, height and gender using the formula published by Jones et al. [33]. The highest HR reached during the exercises was defined as HR reached (HRreached). The highest RQ was termed RQ peak (RQpeak). The test was interrupted if the subject indicated any discomfort that could prevent him/her from continuing the test or when the individual reached 85% of the maximum HR set by the Karvonen formula (220–age). All individuals were informed and educated about the procedure of the test.
Level of physical activity
To quantify their physical activity, all volunteers answered the International Physical Activity Questionnaire (IPAQ–short version). The short version of the IPAQ addresses the number of days and minutes spent practicing physical activities as recreational and occupational activities, transportation and house hold duties. The score was obtained by summing the number of days and minutes or hours of physical activities performed during the week prior to the completion of the questionnaire. The levels of physical activity were classified as sedentary, insufficiently active, active, and intensely active by taking into consideration the frequency, intensity, and length of these activities [34].
In addition to the IPAQ and the Test for Nicotine Dependence, the participants were asked to provide personal details such as age, gender, race and educational background.
Statistical analysis
The statistical software SPSS (version 18.0, SPSS Inc., Chicago, Illinois, USA) was used for statistical analysis. The Shapiro-Wilk test was used to determine the normality of the data distributions. Descriptive statistics (mean, standard deviation and absolute frequency) were calculated for most parameters. Fisher’s exact test was used to compare the categorical variables among groups. One-way analysis of variance (ANOVA) was used to compare mean VO2max, followed by Tukey’s post-hoc test and student’s T-test when necessary. Pearson’s correlation test and Analysis of Covariance (ANCOVA) was also performed to compare VO2max and its covariates age, %F, WC and level of physical activity, among groups. P < 0.05 was considered significant.
Results and discussion
The sample was composed of 43 Caucasian individuals with an average age of 33.5 ± 9.6 years. The individuals were allocated evenly into the active smoker group (n = 14; aged 37.2 ± 7.7 years), passive smoker group (n = 14; aged 33.1 ± 11.8 years) and non-smoker group (n = 15; aged 30.4 ± 8.2 years). Table 1 shows their demographic, anthropometric and basic cardiopulmonary characteristics. Most individuals from the sample (83.3%) had WC within the normal range, but the non-smoker group and the active smoker group had significantly different WC (p = 0.04). The %F was classified as excellent, good, above average or average in 37 individuals (72.9%). The spirometric analysis revealed values within the normal range in all individuals.
Table 1.
Basic characteristics of the study sample
|
Characteristics |
Non-smokers |
Passive smokers |
Active smokers |
p |
|---|---|---|---|---|
| (n = 15) | (n = 14) | (n = 14) | ||
| Male gender, n (%) |
6 (40) |
4 (28.5) |
4 (28.5) |
0.97 |
| Age (years old) |
30,4 ± 8.2 |
33.1 ± 11.8 |
37.2 ± 7.7 |
0.16 |
| BMI (kg/m2) |
23.6 ± 4.6 |
24.3 ± 4.2 |
27.2 ± 3.9 |
0.06 |
| WC (cm) |
74.1 ± 12.1† |
77.2 ± 10.7 |
84.1 ± 8.5† |
0.04 |
| %F |
20.9 ± 8.4 |
23.1 ± 6.6 |
24.1 ± 6.2 |
0.51 |
| SAP resting (mmHg) |
117.9 ± 10.4 |
120.3 ± 12.6 |
120.9 ± 9.3 |
0.73 |
| DAP resting (mmHg) |
76.1 ± 9.4 |
74.6 ± 7.4 |
74.6 ± 9.1 |
0.88 |
| FVC (% pred) |
95.8 ± 21.1 |
105 ± 15.8 |
104.2 ± 13.2 |
0.28 |
| FEV1 (% pred) |
89.4 ± 19.5* |
102.8 ± 15.4 |
103 ± 10.8* |
0.03 |
| FEV1/FVC (% pred) | 92.6 ± 9.2 | 97.4 ± 6.5 | 97.1 ± 5.4 | 0.15 |
BMI, body mass index; DAP, diastolic arterial pressure; FEV1, forced expiratory volume in the first second; FEV1/FVC, ratio between FEV1 and FVC; FVC, forced vital capacity; %F, percentage of body fat; SAP, systolic arterial pressure; WC, waist circumference. Values are expressed as the mean ± SD. †Significant difference between non-smokers and active smokers (p = 0.04). *Significant difference between non-smokers and active smokers (p = 0.03). Significance was accepted at p < 0.05.
According to the FTND, nine out of the 16 active smokers had a medium/high/extremely high degree of nicotine addiction. Instead, in seven individuals, the addiction degree was low/awfully low. All active smokers had been smoking for over 10 years. The average number of cigarettes smoked was 20.6 ± 9.6 cigarette/day002E.
Among the passive smokers, most individuals were exposed to cigarette smoke for over an hour per day (62.5%). All of them had experienced this exposure for over three years. Damage caused by smoking affects not only active smokers but also non-smokers who are exposed to cigarette smoke at home, at work, in leisure environments, at school and in other enclosed public areas [35]. Passive smoking has been considered a significant risk factor for the development and evolution of cardiopulmonary dysfunctions, including loss of endothelial function and coronary artery disease [36,37].
There is a connection between passive smoking and loss of lung function [38,21-41]. However, there is little information about the impact of passive smoking on cardiorespiratory capacity. Furthermore, studies that have quantified the exposure to cigarette smoke have used different methods; these differences hamper and complicate the interpretation of the data.
Flouris et al. [13] evaluated cardiorespiratory and immunological responses during physical activity training after cigarette smoke exposure. Seventeen individuals of both genders were exposed to cigarette smoke in a controlled environment with a concentration of carbon monoxide similar to what is found in restaurants and bars. These individuals were monitored during and after the completion of moderate physical activities. The authors found cardiorespiratory (increased RQ) and immunological (increased interleukins) changes immediately after exposure to cigarette smoke.
In contrast, some studies have been inconsistent when showing significant cardiopulmonary effects caused by exposure to cigarette smoke. One of the first studies to evaluate cardiopulmonary hemodynamics and cardiopulmonary capacity related to residual effects of passive smoking, Ren et al. [14] studied 79 flight attendants exposed to cigarette smoke inside aircraft cabins for over five years reported that passive smoking was linked to SAH but did not cause hemodynamic, pulmonary or systemic consequences. However, in our study, there was evidence of significant differences in CPET results between passive smokers and non-smokers, as well as between non-smokers and active smokers groups.
Table 2 shows the values obtained during the CPET in each group. When evaluating VO2max in active, passive and non-smoking individuals using CPET, significant differences were observed between groups (p < 0.001) (Figure 1). When comparing VO2max between groups, after adjustment for age, %F, WC and level of physical activity showed a significant difference between the non-smoker and passive smoker group (p = 0.022) even as non-smoker and active group (p < 0.001). The passive and active smoker groups showed a not significantly VO2maxdifference (p = 0.053).
Table 2.
Variables obtained during the cardiopulmonary exercise test
|
Characteristics |
Non-smokers |
Passive smokers |
Active smokers |
p |
|---|---|---|---|---|
| (n = 15) | (n = 14) | (n = 14) | ||
| VO2max (% pred)* |
118.44 ± 38.11†** |
89.75 ± 7.4† |
75.13 ± 17.78** |
<0.001 |
| RQ peak (l·min-1) |
1.13 ± 0.3 |
1.2 ± 0.4 |
1.1 ± 0.3 |
0.82 |
| HR resting (bpm) |
70.6 ± 14.9 |
73.6 ± 11.8 |
77.6 ± 13.8 |
0.38 |
| HR reached (bpm) |
159.1 ± 19.6 |
160.1 ± 13.6 |
152.7 ± 13.9 |
0.42 |
| SAP resting (mmHg) |
117.9 ± 10.4 |
120.3 ± 12.6 |
120.9 ± 9.3 |
0.73 |
| SAP reached (mmHg) |
151.3 ± 11.2 |
148.9 ± 18.4 |
147.1 ± 9.1 |
0.70 |
| DAD resting (mmHg) |
76 ± 9.4 |
74.6 ± 7.4 |
74.6 ± 9.1 |
0.88 |
| DAP reached (mmHg) | 84.3 ± 5.6 | 85.3 ± 6.3 | 84.6 ± 7.4 | 0.91 |
DAP, diastolic blood pressure; HR; heart rate; RQ, respiratory quotient; SAP, systolic arterial pressure; VO2max, maximum oxygen consumption;. Values are expressed as mean ± SD. p, p-value obtained through analysis of variance (ANOVA). *Analysis of covariance (ANCOVA) was also performed to compare VO2max and its covariates age, %F, WC and level of physical activity, among groups. Significance was accepted at p < 0.05. †Significant difference between non-smokers and passive smokers (p = 0.022). **Significant difference between non-smokers and active smokers (p < 0.001).
Figure 1.
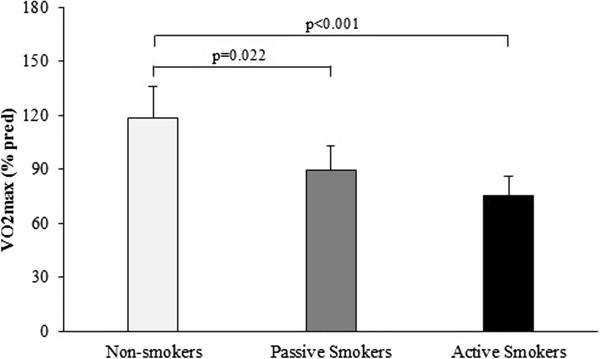
Comparison of VO2 max among groups after adjustment for body mass index and waist circumference.
Several studies have reported a correlation between VO2max and smoking. Kobayashi et al. [15] evaluated the impact of smoking on cardiorespiratory responses during sub-maximal exercise activities. In their study, 18 healthy men were evaluated (nine smokers: average of 15 cigarettes/day for over five years; nine non-smokers). They found that smoke harmed cardiorespiratory function while exercising due to a reduction of the body capacity to carry O2. Laukkanen et al. [6] evaluated determinants of cardiorespiratory capacity in men aged 42 to 60 years and found an inverse correlation between smoking and VO2max[42]. Louie [43] conducted a running test in 27 teenagers smokers or non-smokers and showed that, even in young individuals, smoking was associated with a significant reduction of cardiopulmonary activity and exercise tolerance; this effect remained even at light smoking levels.
According to Kobayashi et al. [15], smoking significantly worsens cardiorespiratory function during moderate to severe exercises. This impairment happens because the body’s capacity to carry O2 is reduced, resulting in a higher anaerobic metabolism, which may lead to injuries on the inside walls of blood vessels, making them more rigid [44]. In our study, there was no difference in RQ among groups, although it was slightly higher in active smokers.
Unverdorben et al. [45] observed higher HR and resting SAP in active smokers than in non-smokers. This fact can be explained by the action of nicotine, which activates the sympathetic nervous system, leading to the release of epinephrine and norepinephrine. The increase in HR may cause heart diseases, which are associated with smoking [46,47]. However, the increase in resting HR may be influenced by psychological stress before performing the CPET. In this study, there were no significant differences among groups in resting HR or resting SAP, although the active smoker group had slightly higher averages.
In our study, the maximum HR reached during the exertion test of the active smoker group was lower compared with the others, as observed by Unverdorben et al. [45]. Smokers who suffer from chronotropic incompetence have a significantly increased risk of death and coronary disease, and HR is an important predictor of all-cause mortality [46]. A longitudinal study performed in 2003 indicated that smoking was negatively associated with the maximum HR obtained during CPET in men and women between 13 and 36 years and that smokers reached a maximum HR lower than in non-smokers [11]. According to Srivastava et al. [46] and Lauer et al. [47], smoking also modifies the chronotropic response to exercise.
Similar to maximum HR, the maximum SAP reached was slightly but not significantly lower in the active and passive smoker groups. This finding indicates that smokers have difficulty in maintaining appropriate cardiac output, which can be explained by chronotropic incompetence. Furthermore, the maximum DAP reached was higher in the active and passive smoker groups compared with the non-smokers, possibly due to a greater vasoconstrictor tone.
According to the IPAQ classifications, most individuals were classified as sedentary or irregularly active (68.8%), with a smaller proportion of active and awfully active individuals (31.3%). No significant results were found when comparing VO2max stratified by level of physical activity between any of two groups (p = 0.063) (Figure 2).
Figure 2.
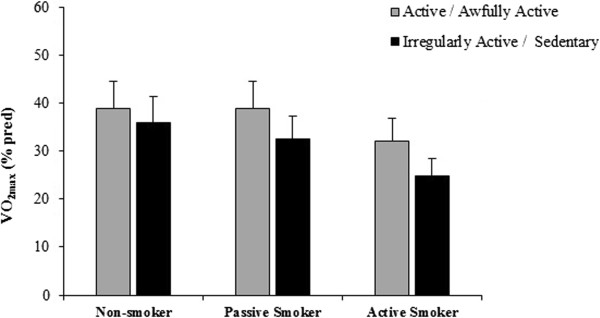
Comparison of VO2 max (% predicted) stratified by level of physical activity in each group analysed.
In our study, we expected to find an association between smoking and sedentarism because smoking is described as more prevalent in sedentary individuals and because physical activities can be a protective factor against beginning habits such as smoking [20]. The lack of association between smoking and sedentariness may have been related to the low degree of nicotine dependence because seven out of 15 active smokers had a low or awfully low degree of nicotine dependence. The IPAQ instrument used to identify the level of physical activity takes into consideration several types of activities, including occupational and transportation activities, which represent a large proportion of the total activities that inhabitants of developing countries engage in [48]. This description could explain the number of active/awfully active individuals in this study.
As seen in Table 3, in the whole sample, VO2max was correlated with age, %F and WC respectively. According to Lee et al. [49], cardiorespiratory capacity depends on modifiable factors (e.g., physical activity, smoking, obesity and health conditions) and non-modifiable factors (e.g., age, gender and genotype). After a person’s maximum cardiorespiratory capacity has been reached between 20 and 30 years, a decline associated with age begins, especially if there are body weight gain and reduction of physical activity [50]. This study confirmed that greater age and %F were associated with lower VO2max. Although there was an association among age, %F and WC, these variables did not affect the outcome of VO2max in the groups. Furthermore, no significant differences were observed between the level of physical activities and VO2max, even though VO2max was lower in sedentary individuals than in active ones. These findings support previous studies [51,52]. Cheng et al. [51] reported that smokers and sedentary individuals had the worst results during the Maximum Exertion Test and spirometry.
Table 3.
Correlations between VO 2max and age, percentage of body fat and waist circumference
| VO 2max (% pred) | r | p |
|---|---|---|
| Age (years) |
-0.401 |
0.044* |
| %F |
-0.429 |
0.011* |
| WC (cm) | -0.382 | 0.025* |
VO2max, maximum oxygen consumption; r, Pearson’s correlation coefficient. Significance was accepted at p < 0.05.
*Analysis of Pearson’s correlation test and Analysis of Covariance (ANCOVA) was also performed to compare VO2max and age, percentage of body fat and waist circumference, among groups.
It is important to highlight the methodological limitations of this study. A cross-sectional study is fast and less expensive than other studies, but it is limited by its brief time frame. For this reason, it was not possible to evaluate the temporal relationships between causes and effects. Regarding the determination of tobacco intake of the subjects in this study it was not possible to quantify the level of urinary cotinine, and therefore we used the Fagerström Test for Nicotine Dependence, which is a validated tool to quantify tobacco load [53,54]. The use of questionnaires also limits the strength of our data because questions might not be answered completely due to a lack of understanding or recall by the respondents caused by their low education level or inability to remember some aspects of the evaluation or even because they unconsciously overestimated or underestimated their activities.
Recall bias related to active and passive smoking must also be considered. The ability to determine one’s exposure to tobacco smoke is potentially subject to information bias, which may limit the interpretation of the results. However, we classified passive smokers according to the participants’ self-reports, as in other studies [20,21]. In addition to costing less than other methods, questionnaires to verify passive smoking are valid instruments for projecting the level of cigarette smoke exposure [36,55,56].
In our study the significant difference between passive smokers and non-smokers could be explained by many factors like the amounts of chemical substances coming from environmental smoke that depend on number of smokers, level of cigarette consumption, types of cigarettes smoked (with or without strainer, tar content or nicotine content), proximity to the passive smoker, duration of exposure, size of the exposure space, characteristics of the ventilation system, age of the person exposed, frequency of air exchange in the closed environment, and use of air purifiers [57,58,36]. These variables were not measured in our study, which may have limited the generalizability of our results.
Conclusions
This study, which aimed to identify the effects of smoking on the cardiorespiratory capacity of active and passive smokers, found significant difference between active smokers and non-smokers. Nevertheless, we found no difference between active and passive smokers. VO2max was negatively correlated with age, %F and WC. In contrast, there was no significant correlation between the level of physical activity and VO2max, although sedentary people showed lower maximum oxygen consumption than the more active ones. Because the literature on passive smokers is limited, more studies on the effects of passive smoking on cardiopulmonary fitness are necessary and justified.
Competing interests
The authors declare that they have no competing interests.
Author’s contributions
ATB, FBN, HHP, MBR, VAC and DNP contributed to design the study, write the manuscript and revise editing. ATB, RTJ, RG and DMC contributed to the collection and analysis of statistical data. ATB, RTJ, RG, DMC and DNP contributed to the interpretation of data and revision of the manuscript. ATB, RG, FBN, DMC, HHP, MBR, VAC and DNP performed the final revision of the manuscript. All authors read and approved the manuscript.
Contributor Information
Andresa Thier de Borba, Email: atborba@uol.com.br.
Renan Trevisan Jost, Email: rtjost@gmail.com.
Ricardo Gass, Email: ricardogass@hotmail.com.
Fúlvio Borges Nedel, Email: fulvionedel@gmail.com.
Dannuey Machado Cardoso, Email: dannuey@yahoo.com.br.
Hildegard Hedwig Pohl, Email: hpohl@unisc.br.
Miriam Beatris Reckziegel, Email: miriam@unisc.br.
Valeriano Antonio Corbellini, Email: valer@unisc.br.
Dulciane Nunes Paiva, Email: dulciane@unisc.br.
References
- Gander J, Lee DC, Sui X, Hébert JR, Hooker SP, Blair SN. Self-rated health status and cardiorespiratory fitness as predictors of mortality in men. Br J Sports Med. 2011;45(14):1095–1100. doi: 10.1136/bjsm.2010.079855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow CE, LaMonte MJ, Fitzgerald SJ, Kampert JB, Perrin JL, Blair SN. Cardiorespiratory fitness is an independent predictor of hypertension incidence among initially normotensive healthy women. Am J Epidemiol. 2006;163(2):142–150. doi: 10.1093/aje/kwj019. [DOI] [PubMed] [Google Scholar]
- Sawada SS, Lee IM, Naito H, Noguchi J, Tsukamoto K, Muto T, Higaki Y, Tanaka H, Blair SN. Long-term trends in cardiorespiratory fitness and the incidence of type 2 diabetes. Diabetes Care. 2010;33(6):1353–1357. doi: 10.2337/dc09-1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaMonte MJ, Barlow CE, Jurca R, Kampert JB, Church TS, Blair SN. Cardiorespiratory fitness is inversely associated with the incidence of metabolic syndrome: a prospective study of men and women. Circulation. 2005;112(4):505–512. doi: 10.1161/CIRCULATIONAHA.104.503805. [DOI] [PubMed] [Google Scholar]
- Lee CD, Sui X, Hooker SP, Hébert JR, Blair SN. Combined impact of lifestyle factors on cancer mortality in men. Ann Epidemiol. 2011;21(10):749–754. doi: 10.1016/j.annepidem.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laukkanen JA, Pukkala E, Rauramaa R, Makikallio TH, Toriola AT, Kurl S. Cardiorespiratory fitness, lifestyle factors and cancer risk and mortality in Finnish men. Eur J Cancer. 2010;46(2):355–363. doi: 10.1016/j.ejca.2009.07.013. [DOI] [PubMed] [Google Scholar]
- Barros Neto TL, Tebexreni AS, Tambeiro VL. Aplicações práticas da ergoespirometria no atleta. RevSocCardiolEstado de São Paulo. 2001;11(3):695–705. [Google Scholar]
- Flox-Camacho A, Escribano-Subias P, Jiménez-López Guarch C, Fernández-Vaquero A, Martín-Ríos D, de la Calzada-Campo CS. Factors affecting the response to exercise in patients with severe pulmonary arterial hypertension. Arch Bronconeumol. 2011;47(1):10–16. doi: 10.1016/j.arbres.2010.07.013. [DOI] [PubMed] [Google Scholar]
- Araujo CGS, Stein R, Serra SM, Herdy AH. Teste cardiopulmonar de exercício. Arq Bras Cardiol. 2010;95(5 supl 1):1–26. [Google Scholar]
- Turnovska TH, Mandadzhieva SK, Marinov BI, Kostianev SS. Respiratory and cardiovascular functions among smoking and nonsmoking girls from two regions with different air pollution degree. Int J Hyg Environ Health. 2007;210(1):61–68. doi: 10.1016/j.ijheh.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Bernaards CM, Twisk JW, Van Mechelen W, Snel J, Kemper HC. A longitudinal study on smoking in relationship to fitness and heart rate response. Med Sci Sports Exerc. 2003;35(5):793–800. doi: 10.1249/01.MSS.0000064955.31005.E0. [DOI] [PubMed] [Google Scholar]
- Costa AA, ElabrasFilho J, Araújo ML, Ferreira JES, Meirelles LR, Magalhães CK. Programa multiprofissional de controle do tabagismo: aspectos relacionados à abstinência de longo prazo. Rev SOCERJ. 2006;19(5):397–403. [Google Scholar]
- Flouris AD, Metsios GS, Jamurtas AZ, Koutedakis Y. Cardiorespiratory and immune response to physical activity following exposure to a typical smoking environment. Heart. 2010;96(11):860–864. doi: 10.1136/hrt.2009.190744. [DOI] [PubMed] [Google Scholar]
- Ren X, Hsu PY, Dulbecco FL, Fleischmann KE, Gold WM, Redberg RF, Schiller NB. Remote second-hand tobacco exposure in flight attendants is associated with systemic but not pulmonary hypertension. Cardiol J. 2008;15(4):338–343. [PubMed] [Google Scholar]
- Kobayashi Y, Takeuchi T, Hosoi T, Loeppky JA. Effects of habitual smoking on cardiorespiratory responses to sub-maximal exercise. J Physiol Anthropol Appl Human Sci. 2004;23(5):163–169. doi: 10.2114/jpa.23.163. [DOI] [PubMed] [Google Scholar]
- Fagerstrom KO, Schneider NG. Measuring nicotine dependence: a review of the Fagerstrom Tolerance Questionnaire. J BehavMed. 1989;12(2):159–182. doi: 10.1007/BF00846549. [DOI] [PubMed] [Google Scholar]
- Halty LS, Hüttner MD, Netto CO, Santos VA, Martins G. Análise da utilização do Questionário de Tolerância de Fagerström (QTF) como instrumento de medida da dependência nicotínica. J Pneumologia. 2002;28(4):180–186. [Google Scholar]
- Mallaina P, Lionis C, Rol H, Imperiali R, Burgess A, Nixon M, Malvestiti FM. Smoking cessation and the risk of cardiovascular disease outcomes predicted from established risk scores: results of the Cardiovascular Risk Assessment among Smokers in Primary Care in Europe (CV-ASPIRE) study. BMC Public Health. 2013;13:362. doi: 10.1186/1471-2458-13-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali R, Meena S, Eastwood B, Richards I, Marsden J. Ultra-rapid screening for substance-use disorders: The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST-Lite) Drug Alcohol Depend. 2013. [DOI] [PubMed]
- Holmen TL, Barrett-Connor E, Clausen J, Holmen J, Bjermer L. Physical exercise, sports, and lung function in smoking versus nonsmoking adolescents. Eur Respir J. 2002;19(1):8–15. doi: 10.1183/09031936.02.00203502. [DOI] [PubMed] [Google Scholar]
- Eisner MD. Environmental tobacco smoke exposure and pulmonary function among adults in NHANES III: impact on the general population and adults with current asthma. Environ Health Perspect. 2002;110(8):765–770. doi: 10.1289/ehp.02110765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452. [PubMed] [Google Scholar]
- Heyward VH. Avaliaçãofísica e prescrição de exercício: técnica savançadas. Porto Alegre: Artmed; 2004. [Google Scholar]
- I Diretriz Brasileira de Diagnóstico e Tratamento da Síndrome Metabólica. Arq Bras Cardiol. 2005;84(Suppl.1) [PubMed] [Google Scholar]
- Jackson AS, Pollock ML, Ward A. Generalized equations for predicting body density of women. Med Sci Sports Exerc. 1980;12(3):175–181. [PubMed] [Google Scholar]
- Jackson AS, Pollock ML. Generalized equations for predicting body density of men. Br J Nutr. 2004;91(1):161–168. [PubMed] [Google Scholar]
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J. ATS/ERS Task Force. ATS/ERS Standardization of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- Pereira CAC, Barreto SP, Simöes JG, Pereira FWL, Gerstler JG, Nakatani J. Valores de referência para a spirometria emuma amostra da populaçäo brasileira adulta. J Pneumol. 1992;18(1):10–22. [Google Scholar]
- VI Diretrizes Brasileiras de Hipertensão. Arq Bras Cardiol. 2010;95(Suppl.1):1–51. [PubMed] [Google Scholar]
- Novitsky S, Segal KR, Chatr-Aryamontri B, Guvakov D, Katch VL. Validity of a new portable indirect calorimeter: the Aero Sport TEEM 100. Eur J Appl Physiol Occup Physiol. 1995;70(5):462–467. doi: 10.1007/BF00618499. [DOI] [PubMed] [Google Scholar]
- Stein R, Andrade J, Pinto VBF. Diretrizes da Sociedade Brasileira de Cardiologia sobre Teste de Esforço. Arq Bras Cardiol. 2002.
- Pollock ML, Wilmore JH. Exercíciosna Saúde e na Doença. Rio de Janeiro: MEDSI; 1993. [Google Scholar]
- Jones NL, Makrides L, Hitchcock C, Chypchar T, McCartney N. Normal standard for an incremental progressive cycle ergometer test. Am Rev Respir Dis. 1985;131:700–708. doi: 10.1164/arrd.1985.131.5.700. [DOI] [PubMed] [Google Scholar]
- Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, Braggion G. Questionário internacional de atividadefísica (IPAQ): Estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fis Saúde. 2001;6(2):5–18. [Google Scholar]
- WünschFilho V, Mirra AP, López RVM, Antunes LF. Tabagismo e câncer no Brasil: evidências e perspectivas. Rev Bras Epidemiol. 2010;13(2):175–187. [Google Scholar]
- Florescu A, Ferrence R, Einarson T, Selby P, Soldin O, Koren G. Methods for quantification of exposure to cigarette smoking and environmental tobacco smoke: focus on developmental toxicology. Ther Drug Monit. 2009;31(1):14–30. doi: 10.1097/FTD.0b013e3181957a3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jousilahti P, Patja K, Salomaa V. Environmental tobacco smoke and the risk of cardiovascular disease. Scand J Work Environ Health. 2002;28(Suppl 2):41–51. [PubMed] [Google Scholar]
- Hirayama T. Non-smoking wives of heavy smokers have a higher risk of lung cancer: a study from Japan. Br Med J (Clin Res Ed) 1981;282(6259):183–185. doi: 10.1136/bmj.282.6259.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lannero E, Wickman M, Pershagen G, Nordvall L. Maternal smoking during pregnancy increases the risk of recurrent wheezing during the first years of life (BAMSE) Respir Res. 2006;7:3. doi: 10.1186/1465-9921-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin P, Jiang CQ, Cheng KK, Lam TH, Lam KH, Miller MR, Zhang WS, Thomas GN, Adab P. Passive smoking exposure and risk of COPD among adults in China: the Guangzhou Biobank Cohort Study. Lancet. 2007;370(9589):751–757. doi: 10.1016/S0140-6736(07)61378-6. [DOI] [PubMed] [Google Scholar]
- Gerald LB, Gerald JK, Gibson L, Patel K, Zhang S, McClure LA. Changes in environmental tobacco smoke exposure and asthma morbidity among urban school children. Chest. 2009;135(4):911–916. doi: 10.1378/chest.08-1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laukkanen JA, Laaksonen D, Lakka TA, Savonen K, Rauramaa R, Makikallio T, Kurl S. Determinants of cardiorespiratory fitness in men aged 42 to 60 years with and without cardiovascular disease. Am J Cardiol. 2009;103(11):1598–1604. doi: 10.1016/j.amjcard.2009.01.371. [DOI] [PubMed] [Google Scholar]
- Louie D. The effects of cigarette smoking on cardiopulmonary function and exercise tolerance in teenagers. Can Respir J. 2001;8(4):289–291. doi: 10.1155/2001/701384. [DOI] [PubMed] [Google Scholar]
- Araujo AJ, Menezes AMB, Dórea AJP, Torres BS, Viegas CAA, Silva CAR, Kirchenchtejn C, Orfaliais CS, Sant’anna CC, Botelho C, Gonçalves CMC, Haggsträm FM, Godoy I, Reichert J, Chatkin JM, Ayoub LTV, Pereira LFF, Halty LS, Sales MPU, Oliveira MVC, Castillo PL, Meirelles RHS. Diretrizes para cessação do tabagismo. J Bras Pneumol. 2004;30(supl 2) [Google Scholar]
- Unverdorben M, van der Bijl A, Potgieter L, Venter C, Munjal S, Qiwei L, Meyer B, Rothig HJ. Effects of different levels of cigarette smoke exposure on prognostic heart rate and rate–pressure-product parameters. J Cardiovasc Pharmacol Ther. 2008;13(3):175–182. doi: 10.1177/1074248408321571. [DOI] [PubMed] [Google Scholar]
- Srivastava R, Blackstone EH, Lauer MS. Association of smoking with abnormal exercise heart rate responses and long-term prognosis in a healthy, population-based cohort. Am J Med. 2000;109(1):20–26. doi: 10.1016/s0002-9343(00)00441-1. [DOI] [PubMed] [Google Scholar]
- Lauer MS, Pashkow FJ, Larson MG, Levy D. Association of cigarette smoking with chronotropic incompetence and prognosis in the Framingham Heart Study. Circulation. 1997;96(3):897–903. doi: 10.1161/01.cir.96.3.897. [DOI] [PubMed] [Google Scholar]
- Hallal PC, Victora CG, Wells JC, Lima RC. Physical inactivity: prevalence and associated variables in Brazilian adults. Med Sci Sports Exerc. 2003;35(11):1894–1900. doi: 10.1249/01.MSS.0000093615.33774.0E. [DOI] [PubMed] [Google Scholar]
- Lee DC, Artero EG, Sui X, Blair SN. Mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol. 2010;24(4 Suppl):27–35. doi: 10.1177/1359786810382057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson AS, Sui X, Hebert JR, Church TS, Blair SN. Role of lifestyle and aging on the longitudinal change in cardiorespiratory fitness. Arch Intern Med. 2009;169(19):1781–1787. doi: 10.1001/archinternmed.2009.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng YJ, Macera CA, Addy CL, Sy FS, Wieland D, Blair SN. Effects of physical activity on exercise tests and respiratory function. Br J Sports Med. 2003;37(6):521–528. doi: 10.1136/bjsm.37.6.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair SN, Kohl HW, Barlow CE, Paffenbarger RS, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273(14):1093–1098. [PubMed] [Google Scholar]
- Roberts B, Chikovani I, Makhashvili N, Patel V, McKee M. Tobacco use and nicotine dependence among conflict-affected men in the Republic of Georgia. Int J Environ Res Public Health. 2013;10(6):2185–2197. doi: 10.3390/ijerph10062185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W, Difranza JR, Kennedy DN, Zhang N, Ziedonis D, Ursprung S, King JA. Progressive levels of physical dependence to tobacco coincide with changes in the anterior cingulum bundle microstructure. PLoS One. 2013;8(7):e67837. doi: 10.1371/journal.pone.0067837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gehring U, Leaderer BP, Heinrich J, Oldenwening M, Giovannangelo ME, Nordling E, Merkel G, Hoek G, Bellander T, Brunekreef B. Comparison of parental reports of smoking and residential air nicotine concentrations in children. Occup Environ Med. 2006;63(11):766–772. doi: 10.1136/oem.2006.027151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildirim F, Sermetow K, Aycicek A, Abdurrahim K, Erel O. Aumento do estresse oxidativo em pré-escolares expostos ao tabagismo passivo. J Pediatr. 2011;87(6):523–528. doi: 10.2223/JPED.2139. [DOI] [PubMed] [Google Scholar]
- Câncer INCA. Brasil: Tabagismo passivo. 2010. [cited 2010 02/09]. Available from: http://www1.inca.gov.br/tabagismo/frameset.asp?item=passivo&link=tabagismo.htm.
- Bartal M. Health effects of tobacco use and exposure. Monaldi Arch Chest Dis. 2001;56(6):545–554. [PubMed] [Google Scholar]


