Abstract
We herein present a case of a 75-year-old female with mucosa-associated lymphoid tissue (MALT) lymphoma of the transverse colon with the stage IE (Ann Arbor classification). Colonoscopy revealed the tumor’s appearance as a IIa plus IIc-like early colon cancer as defined according to the macroscopic classification of the Japanese Research Society for Cancer of Colon, Rectum and Anus, measuring less than 2 cm in diameter. Histologically, the tumor was diagnosed as MALT lymphoma because of the presence of lymphoepithelial lesions consisting of diffuse proliferation of atypical lymphocytes and glandular destruction. The majority of these lymphocytes immunohistochemically stained for the B-lymphocyte marker. The patient first underwent H pylori eradication therapy with Lansap®. However, the tumor size gradually increased over the next 4 mo and the patient eventually underwent surgical resection. The operative procedure included a partial colectomy with dissection of the paracolic lymph nodes. The tumor measured 45 mm x 30 mm in diameter and histological examination showed that the lymphoma cells had infiltrated the muscle layer of the colon without nodal involvement. The patient has had no recurrence postoperatively without any chemotherapy.
Keywords: Mucosa-associated lymphoid tissue, Malignant lymphoma
INTRODUCTION
The term mucosa-associated lymphoid tissue (MALT) lymphoma was first introduced by Isaacson and Wright[1] in 1983. This entity includes low-grade gastric B-cell lymphoma and immunoproliferative small intestinal disease. MALT lymphomas occur in a variety of extra-nodal organs, such as the gastrointestinal (GI) tract and the non-GI tract, in which the stomach is the most common site[2,3]. Since convincing evidence has been presented showing the relationship between H pylori and gastric MALT lymphoma, the therapeutic strategy has been altered for patients with gastric MALT lymphoma in the early stages[4-8]. In contrast, a treatment for colonic MALT lymphoma has not yet been established. In the present report, we describe a case of colonic MALT lymphoma which did not response to H pylori eradication treatment and, therefore, underwent a surgical resection, and also provide a literature review on this rare entity.
CASE REPORT
A 75-year-old female was admitted to Nagasaki Prefectural Shimabara Hospital for surgical treatment of MALT lymphoma of the transverse colon on June 21, 2005. The patient had shown a positive fecal occult blood test on January 20, 2005 without any clinical symptoms and signs. Her past histories included hypertension, diabetes mellitus, and cholecystolithiasis. The results of complete blood counts, blood chemistries and tumor markers, such as carcinoembryonic antigen, were all within the normal limits. Colonoscopy revealed the tumor’s appearance as IIa plus IIc-like early colon cancer[9], measuring less than 2 cm in diameter, in the transverse colon (Figure 1). Biopsy specimens histologically showed lymphoepithelial lesions with diffuse proliferation of atypical small lymphocytes and some glandular destruction. These lymphocytes immunohistochemically showed diffusely positive staining for L-26 (Figure 2) and bcl-2, but negative staining for CD3, CD5, CD10, CD79a, UCHL-1 and cyclin D1. These findings were compatible with MALT lymphoma of the colon. Barium enema showed a flat-elevated lesion in the transverse colon (Figure 3). Abdominal and chest CT demonstrated neither abnormal lesions nor enlargement of lymph node. According to the Ann Arbor classification, this MALT lymphoma belonged to the stage IE. The patient first underwent H pylori eradication therapy with Lansap® because of positive reaction to a urea breath test (UBT). However, over the course of 4 mo, the tumor gradually increased in size, although H pylori were eradicated. The patient was considered to be a non-responder to eradication therapy, and was indicated for surgical resection. A partial colectomy with dissection of the paracolic lymph nodes was performed on June 23, 2005 (Figure 4). The tumor grossly appeared to be a IIa plus IIc-like early colon cancer, measuring 45 mm × 30 mm in diameter. Resected specimens were histologically and immunohistochemically reconfirmed to be MALT lymphoma without nodal involvement. The lymphoma cells infiltrated mainly into the mucosa and submucosal layer, and partly infiltrated into the muscular layer of the colon (Figure 5). The patient has had no recurrence postoperatively without any chemotherapy.
Figure 1.
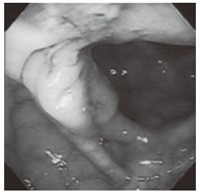
Colonofiberscopy showing the tumor’s appearance as a IIa plus IIc-like early colon cancer.
Figure 2.
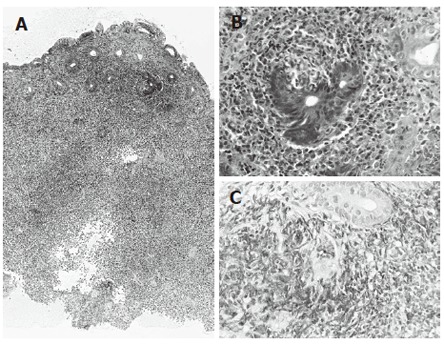
Biopsy specimens histologically showing diffuse proliferation of atypical small lymphocytes in the mucosal layer (A: x 40 magnification, HE) and glandular destruction (B: x 200 magnification, HE). These lymphocytes immunohistochemically showing diffusely positive staining for L-26 (C; x 200 magnification, ABC method).
Figure 3.
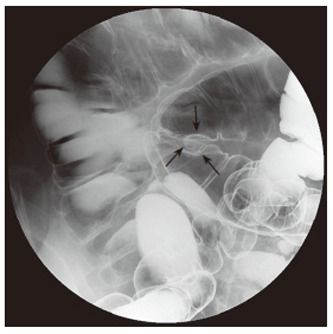
Barium enema showing a flat and well-circumscribed tumor in the transverse colon (arrows).
Figure 4.
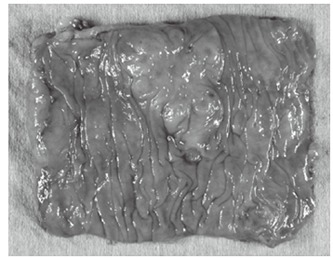
Resected specimens showing a flat-elevated tumor with slight depression, measuring 45 mm x 30 mm in diameter.
Figure 5.

The lymphoma cells mainly infiltrated into the mucosal and submucosal layers, and partly infiltrated into the muscular layer of the colon (x 20 magnification, HE).
DISCUSSION
MALT lymphoma is defined as extra-nodal marginal zone B-cell lymphoma of MALT type in peripheral B-cell lymphoma according to morphologic features, immunophenotype, genetic features, postulated normal counterpart, and clinical features[10,11].
H pylori eradication therapy is currently widely recognized as an initial therapy in cases with low-grade (stage I) gastric MALT lymphoma[12-14]. In contrast, it has not yet been clarified whether H pylori eradication, or chemotherapy, or surgery should be performed in colonic MALT lymphoma compared with gastric MALT lymphoma, because the colorectal MALT lymphomas are rare. The individual clinical details of colorectal MALT lymphoma are summarized in Table 1[15-27]. Some reports have described the successful regression of colorectal MALT lymphoma by means of eradication therapy in H pylori-positive patients[16,20]. Even in cases with colorectal MALT lymphoma negative for H pylori, the regression of the tumor was also recognized as a result of H pylori eradication therapy[19,23,24,27]. In prospective studies of gastric MALT lymphoma, eradication therapy was not effective in patients negative for H pylori[28,29]. Grunberger et al[30] reported that antibiotic eradication therapy was not effective in patients infected with H pylori suffering from extra-gastric MALT lymphoma. Therefore, they suggested that H pylori did not play a role in the development of extra-gastric MALT lymphomas. Similarly, antibiotic eradication therapy was not effective in our present case. These results may suggest that colorectal MALT lymphomas are not directly related to H pylori infection, while gastric MALT lymphomas are strongly associated with H pylori infection. In the future, a definite pathogenesis of colorectal MALT lymphoma should be clarified when cases of colorectal MALT lymphomas have accumulated. As a speculation, colorectal MALT lymphomas may be caused by unknown antibiotic-sensitive microorganisms other than H pylori, although that is not clear. In gastric MALT lymphoma, indeed, Helicobacter heilmannii-associated MALT lymphoma other than H pylori has been reported to be completely regressed by eradication therapy[31].
Table 1.
Colorectal MALT lymphoma in the English literatures
| Author | Yr | Age/Sex | Location/Size | Symptoms/Signs | H pylori | Treatment | Outcome |
| Schmid[15] | 1994 | 65/M | S/2.5 cm | ND | ND | Polypectomy | NED for 9 mo |
| 1994 | 47/M | T/1.5 cm | ND | ND | Polypectomy and chemotherapy | NED for 24 mo | |
| 1994 | 64/M | T/1.5 cm | ND | ND | Left hemicolectomy | Died, 7 d (Cardiac failure) | |
| Matsumoto[16] | 1997 | 72/F | R/ND | Rectal bleeding | + | Eradication | NED for 12 wk |
| Yasui[17] | 1999 | 76/M | C/30 × 15 mm | Fecal occult blood | ND | Partial resection2 | ND |
| Orita[18] | 1999 | 64/F | R/3.4 × 4.8 cm | Fecal occult blood | ND | Abdominoperineal resection | NED for 35 mo |
| Inoue[19] | 1999 | 62/F | R/ND | Hematochezia | - | Eradication | NED for 53 wk |
| Raderer[20] | 2000 | 67/M | D1/1.5 cm | None | + | Eradication | NED for 4 mo |
| Hasegawa[21] | 2000 | 72/F | S/3.0 × 1.5 cm | Abdominal pain, fever | ND | Sigmoidectomy | ND |
| Yoshimura[22] | 2002 | 74/M | T/8 × 4 cm | Fecal occult blood | ND | Chemotherapy | NED for 20 mo |
| Nakase[23] | 2002 | 66/F | D, S, R/ND | Hematochezia | - | Eradication | NED for 1.5 yr |
| 2002 | 33/F | R/ND | Fever, hematochezia | - | Eradication | NED for 10 mo | |
| 2002 | 62/F | R/ND | Hematochezia | - | Eradication | NED for 6 mo | |
| Hisabe[24] | 2002 | 70/F | R/1.5 cm | Abdominal discomfort | - | Eradication | NED for 20 mo |
| Takada[25] | 2003 | 44/M | C/1.1 × 0.9 cm | Fecal occult blood | - | Partial resection2 | ND |
| Lee[26] | 2005 | 47/M | R/ND | Tenesmus, mucoid sool | - | Chemotherapy and radiation | NED for 3 mo |
| Kikuchi[27] | 2005 | 71/M | R/3.5 cm | Fecal occult blood | - | Eradication3 | NED for 12 mo |
| 2005 | 80/F | C, R/2.5 cm | Anal bleeding | - | Eradication | NED for 6 mo | |
| 2005 | 70/F | R/1.5 cm | Abdominal discomfort | - | Eradication | NED for 20 mo | |
| Our case | 2006 | 75/F | T/4.5 × 3.5 cm | Fecal occult blood | + | Partial resection after eradication | NED for 12 mo |
Location; R: Rectum, S: Sigmoid colon; D: Descending colon; T: Transverse colon; C: Cecum; ND: Not described; NED: No evidence of disease.
This patient had MALT lymphomas in the stomach and the descending colon, simultaneously.
These patients performed laparoscopy-assisted colon resection.
This patient has received repeated eradication.
Surgical resection is mandatory when a colorectal MALT lymphoma does not respond to eradication therapy or chemotherapy, and it is localized without dissemination.
In conclusion, the present case with colonic MALT lymphoma eventually underwent surgical resection of the colon after the failure of eradication therapy. Surgical intervention is now the procedure of choice for colorectal MALT lymphoma because its pathogenesis and therapeutic strategy have not yet been established.
Footnotes
S- Editor Liu Y L- Editor Kumar M E- Editor Bi L
References
- 1.Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983;52:1410–1416. doi: 10.1002/1097-0142(19831015)52:8<1410::aid-cncr2820520813>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 2.Thieblemont C, Bastion Y, Berger F, Rieux C, Salles G, Dumontet C, Felman P, Coiffier B. Mucosa-associated lymphoid tissue gastrointestinal and nongastrointestinal lymphoma behavior: analysis of 108 patients. J Clin Oncol. 1997;15:1624–1630. doi: 10.1200/JCO.1997.15.4.1624. [DOI] [PubMed] [Google Scholar]
- 3.Thieblemont C, Berger F, Dumontet C, Moullet I, Bouafia F, Felman P, Salles G, Coiffier B. Mucosa-associated lymphoid tissue lymphoma is a disseminated disease in one third of 158 patients analyzed. Blood. 2000;95:802–806. [PubMed] [Google Scholar]
- 4.Wyatt JI, Rathbone BJ. Immune response of the gastric mucosa to Campylobacter pylori. Scand J Gastroenterol Suppl. 1988;142:44–49. [PubMed] [Google Scholar]
- 5.Stolte M, Eidt S. Lymphoid follicles in antral mucosa: immune response to Campylobacter pylori. J Clin Pathol. 1989;42:1269–1271. doi: 10.1136/jcp.42.12.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Isaacson PG. Gastric MALT lymphoma: from concept to cure. Ann Oncol. 1999;10:637–645. doi: 10.1023/a:1008396618983. [DOI] [PubMed] [Google Scholar]
- 7.Neubauer A, Thiede C, Morgner A, Alpen B, Ritter M, Neubauer B, Wündisch T, Ehninger G, Stolte M, Bayerdörffer E. Cure of Helicobacter pylori infection and duration of remission of low-grade gastric mucosa-associated lymphoid tissue lymphoma. J Natl Cancer Inst. 1997;89:1350–1355. doi: 10.1093/jnci/89.18.1350. [DOI] [PubMed] [Google Scholar]
- 8.Montalban C, Santon A, Boixeda D, Bellas C. Regression of gastric high grade mucosa associated lymphoid tissue (MALT) lymphoma after Helicobacter pylori eradication. Gut. 2001;49:584–587. doi: 10.1136/gut.49.4.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Japanese Research Society for Cancer of the Colon, Rectum and Anus. General rules for clinical and pathological studies on cancer of colon, rectum and anus (6th ed) Tokyo: Kinbara Shuppan; 1998. pp. 32–36. [Google Scholar]
- 10.Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, Delsol G, De Wolf-Peeters C, Falini B, Gatter KC. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood. 1994;84:1361–1392. [PubMed] [Google Scholar]
- 11.Jaffe ES, Harris NL, Diebold J, Muller-Hermelink HK. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues. A progress report. Am J Clin Pathol. 1999;111:S8–12. [PubMed] [Google Scholar]
- 12.Wotherspoon AC, Ortiz-Hidalgo C, Falzon MR, Isaacson PG. Helicobacter pylori-associated gastritis and primary B-cell gastric lymphoma. Lancet. 1991;338:1175–1176. doi: 10.1016/0140-6736(91)92035-z. [DOI] [PubMed] [Google Scholar]
- 13.Wotherspoon AC, Doglioni C, Diss TC, Pan L, Moschini A, de Boni M, Isaacson PG. Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet. 1993;342:575–577. doi: 10.1016/0140-6736(93)91409-f. [DOI] [PubMed] [Google Scholar]
- 14.Fischbach W, Goebeler-Kolve ME, Dragosics B, Greiner A, Stolte M. Long term outcome of patients with gastric marginal zone B cell lymphoma of mucosa associated lymphoid tissue (MALT) following exclusive Helicobacter pylori eradication therapy: experience from a large prospective series. Gut. 2004;53:34–37. doi: 10.1136/gut.53.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmid C, Vazquez JJ, Diss TC, Isaacson PG. Primary B-cell mucosa-associated lymphoid tissue lymphoma presenting as a solitary colorectal polyp. Histopathology. 1994;24:357–362. doi: 10.1111/j.1365-2559.1994.tb00537.x. [DOI] [PubMed] [Google Scholar]
- 16.Matsumoto T, Iida M, Shimizu M. Regression of mucosa-associated lymphoid-tissue lymphoma of rectum after eradication of Helicobacter pylori. Lancet. 1997;350:115–116. doi: 10.1016/S0140-6736(05)61818-1. [DOI] [PubMed] [Google Scholar]
- 17.Yasui N, Watanabe M, Iwao Y, Sakaguchi AA, Tahara T, Eramoto T, Mukai M, Hibi T, Kitajima M. Laparoscopically assisted bowel resection for primary mucosa-associated lymphoid tissue lymphoma of the cecum. Surg Laparosc Endosc Percutan Tech. 1999;9:156–159. [PubMed] [Google Scholar]
- 18.Orita M, Yamashita K, Okino M, Enoki T, Noshima S, Morita N, Esato K. A case of MALT (mucosa-associated lymphoid tissue) lymphoma occurring in the rectum. Hepatogastroenterology. 1999;46:2352–2354. [PubMed] [Google Scholar]
- 19.Inoue F, Chiba T. Regression of MALT lymphoma of the rectum after anti-H. pylori therapy in a patient negative for H. pylori. Gastroenterology. 1999;117:514–515. doi: 10.1053/gast.1999.0029900514b. [DOI] [PubMed] [Google Scholar]
- 20.Raderer M, Pfeffel F, Pohl G, Mannhalter C, Valencak J, Chott A. Regression of colonic low grade B cell lymphoma of the mucosa associated lymphoid tissue type after eradication of Helicobacter pylori. Gut. 2000;46:133–135. doi: 10.1136/gut.46.1.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hasegawa N, Kato K, Yamada K, Morita K, Kuroiwa M, Ito H, Kamioka T, Matsuura T, Sato M, Ono K, et al. Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT) of the sigmoid colon. Gastrointest Endosc. 2000;52:802–804. doi: 10.1067/mge.2000.110737. [DOI] [PubMed] [Google Scholar]
- 22.Yoshimura D, Maruoka A, Maekawa S, Yao T, Harada N, Nawata H. Transverse colon MALT lymphoma with nodal metastasis. Gastrointest Endosc. 2002;55:238–239. doi: 10.1067/mge.2002.120101. [DOI] [PubMed] [Google Scholar]
- 23.Nakase H, Okazaki K, Ohana M, Ikeda K, Uchida K, Uose S, Itoh T, Iwano M, Watanabe N, Yazumi S, et al. The possible involvement of micro-organisms other than Helicobacter pylori in the development of rectal MALT lymphoma in H. pylori-negative patients. Endoscopy. 2002;34:343–346. doi: 10.1055/s-2002-23643. [DOI] [PubMed] [Google Scholar]
- 24.Hisabe T, Imamura K, Furukawa K, Tsuda S, Matsui T, Yao T, Kanda M, Ohshima K, Kikuchi M. Regression of CD5-positive and Helicobacter pylori-negative mucosa-associated lymphoid tissue lymphoma of the rectum after administration of antibiotics: report of a case. Dis Colon Rectum. 2002;45:1267–1270. doi: 10.1007/s10350-004-6404-9. [DOI] [PubMed] [Google Scholar]
- 25.Takada M, Ichihara T, Fukumoto S, Nomura H, Kuroda Y. Laparoscopy-assisted colon resection for mucosa-associated lymphoid tissue (MALT) lymphoma in the cecum. Hepatogastroenterology. 2003;50:1003–1005. [PubMed] [Google Scholar]
- 26.Lee YG, Lee S, Han SW, Lee JS. A case of multiple mucosa-associated lymphoid tissue (MALT) lymphoma of the colon identified as simple mucosal discoloration. J Korean Med Sci. 2005;20:325–328. doi: 10.3346/jkms.2005.20.2.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kikuchi Y, Matsui T, Hisabe T, Wada Y, Hoashi T, Tsuda S, Yao T, Iwashita A, Imamura K. Deep infiltrative low-grade MALT (mucosal-associated lymphoid tissue) colonic lymphomas that regressed as a result of antibiotic administration: endoscopic ultrasound evaluation. J Gastroenterol. 2005;40:843–847. doi: 10.1007/s00535-005-1639-3. [DOI] [PubMed] [Google Scholar]
- 28.Steinbach G, Ford R, Glober G, Sample D, Hagemeister FB, Lynch PM, McLaughlin PW, Rodriguez MA, Romaguera JE, Sarris AH, et al. Antibiotic treatment of gastric lymphoma of mucosa-associated lymphoid tissue. An uncontrolled trial. Ann Intern Med. 1999;131:88–95. doi: 10.7326/0003-4819-131-2-199907200-00003. [DOI] [PubMed] [Google Scholar]
- 29.Ruskoné-Fourmestraux A, Lavergne A, Aegerter PH, Megraud F, Palazzo L, de Mascarel A, Molina T, Rambaud JL. Predictive factors for regression of gastric MALT lymphoma after anti-Helicobacter pylori treatment. Gut. 2001;48:297–303. doi: 10.1136/gut.48.3.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grünberger B, Wöhrer S, Streubel B, Formanek M, Petkov V, Puespoek A, Haefner M, Hejna M, Jaeger U, Chott A, et al. Antibiotic treatment is not effective in patients infected with Helicobacter pylori suffering from extragastric MALT lymphoma. J Clin Oncol. 2006;24:1370–1375. doi: 10.1200/JCO.2005.02.9025. [DOI] [PubMed] [Google Scholar]
- 31.Morgner A, Lehn N, Andersen LP, Thiede C, Bennedsen M, Trebesius K, Neubauer B, Neubauer A, Stolte M, Bayerdörffer E. Helicobacter heilmannii-associated primary gastric low-grade MALT lymphoma: complete remission after curing the infection. Gastroenterology. 2000;118:821–828. doi: 10.1016/s0016-5085(00)70167-3. [DOI] [PubMed] [Google Scholar]


