Abstract
Objective
Current chest compression(CC) guidelines for an infant recommend a two finger(TF) technique with lone rescuer and a two thumb(TT) with two rescuers, and for a child either a One hand(OH) or Two hand(TH) technique with one or two rescuers. The effect of a 30:2 compression:ventilation ratio(C:V) using these techniques on CC quality and rescuer fatigue is unknown. We hypothesized that during lone rescuer CC, TT in infant and TH in child achieves better compression depth(CD) without additional rescuer fatigue compared with TF and OH respectively.
Design
Randomized observational study.
Setting
University affiliated pediatric hospital.
Subjects
Adult healthcare providers certified in BLS or Pediatric Advanced Life Support.
Interventions
Laerdal™ Baby ALS Trainer and Resusci Junior manikin were modified to digitally record compression depth(CD), compression pressure(CP) and compression rate(CR). Sixteen subjects were randomized to each of the four techniques to perform 5 minutes lone rescuer 30:2 C:V CPR. Rescuer heart rate(HR) and respiratory rate(RR) were recorded continuously and the recovery time(RT) interval for HR/RR to return to baseline was determined. Subjects were blinded to data recording. Groups were compared using two-sample, two-sided t-tests.
Measurements and Main Results
Two-thumb technique generated significantly higher CD and peak CP compared to TF (p<0.001); there was no significant difference between OH vs. TH. TF showed decay of CD and CP over time compared to TT. CR(per minute) and actual compressions delivered were not significantly different between groups. No significant difference of fatigue and recovery time were observed, except TT group had greater increase in the rescuer’s HR(bpm) from baseline compared to TF group, p=0.04.
Conclusions
Two-thumb compression provides higher CD and CP compared to TF without any evidence of decay in quality and additional rescuer fatigue over 5 minutes. There was no significant difference in child CC quality or rescuer fatigue between OH and TH. Two-thumb technique is preferred for infant CC and our data supports the current guidelines for child chest compression.
Keywords: Heart massage, Child, Infant, Cardiopulmonary Resuscitation, Fatigue
Introduction
Current Pediatric BLS guideline emphasize good quality chest compressions for effective CPR.(1-3) Different chest compression techniques are used for infants and children. For infants, a two finger (TF) technique is recommended for a lone rescuer while a two thumb (TT) technique is recommended for two rescuers.(2, 3) TF is thought to be feasible for lone rescuer compared to TT because of perceived ease of change from compression to ventilation during CPR. Comparison of these two techniques in an infant swine model of cardiac arrest showed TT is easier, more effective(4) and generated higher arterial and coronary perfusion pressures.(5) An infant manikin study showed higher CP generation with TT technique over 10 minute of CPR.(6) No study has compared Compression Depth (CD), Compression Rate (CR) and rescuer fatigue using the alternate techniques.
For a child, use of either one hand (OH) or two hands (TH) is recommended.(2, 3) This recommendation is consensus based due to the belief that less force is required to perform child CPR compared to an adult and use of OH may have a lower risk of patient injury compared to TH. A previous study showed that TH generated higher CP and was perceived easier for CPR performance over 1-minute.(7) Another recent study compared the two methods in 2-rescuer manikin CPR for one minute and found similar CR but faster decline of rate over time with OH.(8) Most study subjects preferred TH compression for ease of use, while the remainder preferred OH for the perception of better depth control.(8) Although these data suggest more consistent chest compressions with the TH technique, no study has evaluated the effect of either technique on CD and rescuer fatigue especially during prolonged child CPR.
We conducted this study to evaluate the effect of different techniques of infant and child chest compression (CC) on 1) Quality of chest compression (i.e., rate, depth and pressure) and, 2) Development of rescuer fatigue as judged by objective and subjective measurements. We hypothesized that TT compression in infants and TH compression in children results in better depth and rate of chest compressions without additional rescuer fatigue using a 30:2 compression:ventilation (C:V) ratio compared to TF and OH respectively.
Materials and Methods
This randomized observational study was approved by the University of Florida Health Science Center Institutional Review Board and was deemed compliant with the Health Insurance Portability and Accountability Act of 1996 (HIPPA) regulations.
Manikin Modification data collection system
Standard Laerdal™ (Laerdal Medical, Stavanger, Norway) Resusci Junior manikin (simulating a 6 year old child) and Baby ALS Trainer manikin (simulating a 3 months old baby) were modified in collaboration with the Biomedical Engineering Department at the University of Florida to digitally record CR, CD, CP and total compression cycles(CC).
For chest compression depth recording, a linear potentiometer was fitted between the anterior and posterior chest plates close to the spring housing as shown in Figure 1. The potentiometer displacement readings were transferred to a bioamplifier by ADInstruments Power lab® Systems (Castle Hill, NSW 2154 Australia), which then sent real time continuous compression depth changes to a laptop computer. Computer software (Chart V4.1 by ADInstruments Power lab® Systems; Castle Hill, NSW 2154 Australia) was used to record chest compression depth and to calculate compression rate and speed. Sampling rate for data collection was set at 100 data points per second.
Figure 1.
Experimental setup and manikin modification.
To measure chest compression pressure, a 100 ml bag containing about 80 ml of saline was placed between the manikin chest wall and chest plate as shown in Figure 1. The fluid tubing from the bag was connected to a digital pressure transducer (ISE40 with pressure range 0 -1 Mega Pascal (MPa) SMC Corporation, Indianapolis USA). Data from the transducer was transferred to the bioamplifier and recorded using the same software noted above at a sampling rate of 100 data points per second. Peak and mean compression pressures were calculated using the same software. The pressure transducer was zeroed to atmospheric pressure.
Manikins were placed on a height adjustable hospital stretcher with wheel locks to mimic actual conditions of in-hospital CPR. Bed height was adjusted to the iliac crest of each rescuer for standardization.
Subject Recruitment and Measurement
Inclusion criteria were certified BLS or Pediatric Advanced Life Support (PALS) health care providers. Exclusion criteria were expired certification or any medical condition contraindicating the exertion required for CPR. Informed consent was obtained and demographic information including age, sex, gender, weight, and height was recorded. Other data collection included time since certification, field of work and experience. A standard cardiopulmonary monitor was used to display heart rate (HR) and respiratory rate (RR) via chest leads attached to the rescuer. HR and RR were recorded by the researcher at each minute. At the end of each study session each subject completed a Likert scale questionnaire on their subjective feeling of fatigue and degree of difficulty performing CPR with each technique.
Study protocol
After enrollment, the study objective was explained but the subjects were blinded from the data and parameters being recorded. Subject’s baseline HR and RR was recorded at rest once these values had stabilized. Subjects were then randomized to one of the four pediatric BLS groups 1) Infant TT, 2) Infant TF, 3) Child OH and 4) Child TH. Subjects were instructed to perform CPR at a compression rate of 100/min using a 30:2 C:V ratio and to simulate mouth-to-mouth ventilations, but they received no further instruction on how to perform CPR and there was no pretrial training. The session lasted for a maximum of 5 minutes, or until they were not able to perform any more. After 5 minutes, rescuers rested while being monitored continuously until the HR and RR returned to baseline and they subjectively felt ready to perform CPR again. This time interval was noted as recovery time (RT). Each rescuer completed the study questionnaire regarding the ease of changing from compressions to ventilation and whether their CPR performance was reduced over time secondary to fatigue.
Statistical Analysis
For the data derived from the manikins, the following four dependent variables were utilized by compression cycle: Compression Depth (maximum – minimum in mm), pressure at maximum compression, average pressure per cycle and cycles per minute. In addition, the total number of compression cycles was used as a fifth primary dependent variable. For each personal session (C:V=30:2), we utilized the median taken over all cycles for the first four variables. For cycles per minute, we converted the length of the individual cycle in seconds to cycles per minute. Medians were used to limit the effects of outliers. This resulted in four sets of outcome measures (one for Child OH, one for Child TH, one for infant TT, and one for infant TF). P-values for the individual manikins (Child and Infant separately) are reported using two-sample Student T-tests. As a secondary analysis, we also broke the data down into minute by minute values, and calculated personal slopes for these dependent variables for each of the four tester groups, and compared the techniques within each manikin by two-sample Student t-tests. Secondarily, we also contrasted the means for the techniques within manikin types, at each of the five minutes (1-5) for the two techniques that used the specific manikin. This supplements the slope analysis, which gives a single p-value rather than five separate ones.
Also secondarily, we compared the rescuer’s mean heart rate increases per minute (slopes), mean respiratory rate increases (slopes), and times to recovery between the two techniques, separately for each manikin type, via two sample Student t-tests. All p-values are two-sided.
Results
Study subject demographic information is shown in Table 1. Most study subjects were experienced pediatric health care providers with an equal distribution of BLS and PALS training. Time since last BLS or PALS certification was comparable among groups. All subjects finished 5 minutes of CPR with each technique.
Table 1.
Study subjects demographics; mean±SD and ranges where appropriate.
| CPR group | Child | Infant | ||
|---|---|---|---|---|
|
| ||||
| CPR technique |
One Hand
(OH) |
Two Hand
(TH) |
Two Thumb
(TT) |
Two Finger
(TF) |
| Number of subjects (n) | 16 | 16 | 16 | 16 |
| Sex Female n (%) | 14(88) | 13(81) | 13(81) | 14(88) |
| Age (years) | 30±7 | 31±7 | 29±9 | 34±9 |
| Range (min – max) | 22 - 51 | 24 - 47 | 22-62 | 23-53 |
| BLS certified (n) | 8 | 8 | 8 | 10 |
| Time since BLS training (months) | 14 | 19 | 12 | 12 |
| PALS certified (n) | 8 | 8 | 8 | 6 |
| Time since PALS training (months) | 17 | 28 | 17 | 17 |
| Type of work | ||||
| Registered nurse | 8 | 2 | 3 | 6 |
| Medical student | 0 | 2 | 2 | 0 |
| Resident in training | 6 | 3 | 5 | 3 |
| Fellow in training | 1 | 4 | 1 | 2 |
| Faculty | 1 | 2 | 0 | 2 |
| Other | 0 | 5 | 5 | 3 |
| Experience in their field (months) | 47±79 | 59±86 | 57±126 | 111±117 |
| Range (min – max) | 1 - 312 | 0 - 336 | 0-504 | 1-360 |
Compression outcome variables
Chest compression outcome variables are summarized in Table 2. All subjects were able to achieve more than 100 compressions per minute and there was no significant difference of actual compressions provided among different techniques although CR was higher in the infant compared to the child group. In the infant group, the mean CD and both peak and mean CP achieved over 5 minutes were significantly higher in TT compared to TF technique. In the child group, the mean CD, and peak and mean CP achieved over 5 minutes were not significantly different between the groups but there was a trend towards a higher CD and peak CP in the TH group.
Table 2.
Chest compression outcome and fatigue variables; OH=One hand, TH=Two hand.
| CPR group | Child | Infant |
|---|---|---|
|
| ||
| OH vs. TH mean±SD, p-value | TT vs. TF mean±SD, p-value | |
|
Compression Variables
| ||
| Compression depth (mm) | 29.1±10.2 vs. 32.9±8.5, 0.26 | 13.8±2.5 vs. 8.7±1.9, <0.001 |
| Peak compression pressure (mm Hg) | 259±103 vs. 323±106, 0.09 | 154±54 vs. 85±23, <0.001 |
| Mean compression pressure (mmHg) | 88±37 vs. 101±35, 0.32 | 54±20 vs. 28±12, <0.001 |
| Compression rate/minute | 114±28 vs. 125±35, 0.33 | 138±24 vs. 146±34, 0.45 |
| Actual compressions cycles | 386±113 vs. 417±108, 0.43 | 474±84 vs. 495±114, 0.56 |
|
| ||
|
Fatigue Variables
| ||
| Change/min in heart rate from baseline | 38±15 vs. 41±12, 0.61 | 22±10 vs. 15±6, 0.04 |
| Change/min in resp rate from baseline | 8±5 vs. 8±4, 0.84 | 4±5 vs. 3±4, 0.53 |
| Recovery time to baseline (sec) | 233±116 vs. 293±171, 0.25 | 291±230 vs. 199±125, 0.17 |
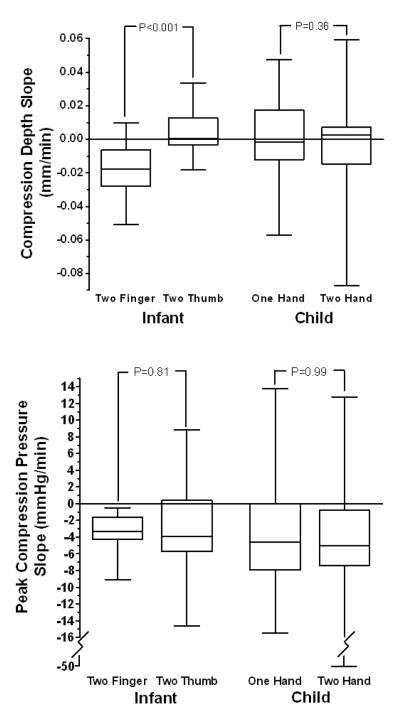
Minute by minute analysis for 5 minutes of CD and peak CP with slopes are shown in Figure 2 for both infant and child chest compression. For infant CC, the TT group not only generated significantly higher CD and peak CP at each minute compared to TF, but there was a significant deterioration of CD with the TF technique over time, p <0.001, as shown Figure 3. For child CC, there was no significant difference between CD or peak CP comparing TH vs. OH technique over time.
Figure 2.
Comparison of mean slopes of compression depth and peak compression pressure over time in infant and child chest compression. Slope less than zero indicates performance deterioration over time. Lower and upper borders of boxes represent the 25th and 75th percentile respectively. Outer lines are the 5th and 95th percentile.
Figure 3.
Infant chest compression depth and peak pressure over time. Data expressed as Mean±SD. Two thumb chest compression is significantly better at each minute compared with two finger compression.
Fatigue variables
Manifestations of fatigue included change in HR and RR from baseline during 5 minutes of CC and recovery time (RT) to baseline (Table 2). During child CC, the rescuer’s HR and RR increased significantly up to 50% above baseline in both groups (data not shown). There was no significant difference in the average increase in HR and RR over 5 minutes or RT within the infant groups or within the child groups. We found no significant difference in the rescuer’s subjective feeling of fatigue between the groups when asked, “At what minute did you want to stop CPR because of fatigue?” There was no significant difference in their perceived ease of changing from compressions to simulated ventilations and achieving a compression rate of 100/minute (Data not shown).
Discussion
Our study of single rescuer infant and child manikin chest compression using health care providers showed that the two thumb technique for infants provided significantly higher compression depth and pressure without evidence of increased fatigue and is superior in maintaining compression quality over 5 minutes compared with the two finger technique. Compression depth achieved with the TF technique was suboptimal for effective infant chest compressions. There was no difference of chest compression quality and maintenance over 5 minutes comparing one hand vs. two hand child chest compression, although there is a significant metabolic stress during child CPR suggested by an almost 50% increase in HR from baseline during 5 minutes regardless of the technique.
The 2005 Guidelines recommended TF compression for single rescuer infant CPR while TT compression is preferred with two rescuers.(2, 3) A previous study showed higher CP with the TT technique compared to TF during infant CPR.(6) Data in animals suggest that adequate depth is directly related to cardiac output during CPR.(9) The current American Heart Association (AHA) chest compression guideline recommends compressing ⅓ to ½ of chest anterior-posterior (AP) diameter for adequate chest compression in infants and children.(1) Furthermore, we recognize that the guideline recommendations for the proportional compression depth are not based on evidence. Indeed, a recent study in pigs suggest that optimal compression depth is 25% of the AP diameter.(10) The AP diameter of our infant manikin model was 3.5 inches (88 mm) with maximum achievable compression depth of 1.1 inches (28 mm), and the AP diameter of the child manikin was 5 inches (127 mm) with maximum achievable compression depth of 1.75 inches (44 mm). Hence in both manikins, maximal compression would have allowed rescuers to achieve ⅓ of the AP diameter of the chest, which is the lower limit of adequate depth as recommended in the 2005 guidelines. Our data showed that the TT technique during infant CC achieved significantly higher compression depth and pressure compared to the TF technique. Our data indicated that most of the study subjects did not achieve even ⅓ of the AP diameter. The mean CD with two-thumb was half of the recommended ⅓ AP diameter and the mean CD with two-finger was only one-third of the recommended ⅓ AP diameter. It is clear that the two-thumb technique is superior even though most rescuers did not achieve the recommended depth with either technique; which was present in the first minute suggesting that it was not due to fatigue.
Reduction in the number of satisfactory compressions was noted previously just after 3 minutes of continuous CPR in adult manikin studies.(11-13) Minute to minute analysis of chest compression data showed that the TT technique was effective in maintaining CD and peak CP and there was significant deterioration of CD and CP with the TF technique over time. Therefore, our study shows superior chest compressions with the TT technique in infants during single rescuer CC and is preferred for single rescuers, especially if chest compression is required for prolonged periods.
Higher compression pressures (up to 15%) with the TH method compared to OH was noted in a previous manikin study.(7) Our study showed a trend towards that effect, which may have been non significant due to the small number of study subjects. During child CC most health care providers were able to achieve the minimum recommended compression depth using either method. A previous study found a significant decrease in compression rate over 1 minute with OH,(8) suggesting that the OH method may be associated with earlier fatigue. We did not observe the expected decline of chest compression depth and pressure with the OH technique; rescuers were able to maintain CD and CP over 5 minutes of CC using either technique. Our study suggests that a single rescuer may maintain effective chest compressions for up to five minutes with either OH or TH. It is likely that the size and strength of the rescuer will determine which method is easier to deliver child chest compressions.
Finally we evaluated changes in the rescuer’s HR and RR over 5 minutes, recovery time and the rescuer’s subjective impression of the degree of difficulty and onset of fatigue with each technique. We found a greater increase in HR with the TT technique, suggesting increased metabolic demand compared with TF compressions. There was no difference in RR, recovery times and subjective feeling of fatigue. There was no difference in fatigue comparing TH vs. OH technique. This is different from the observation of fatigue developing during adult manikin CPR,(14) which is likely due to the increased effort needed to compress the adult manikin chest.
Our study has several limitations. Although infant and child manikins are widely applied in CPR training and resuscitation skills studies, there are intrinsic inadequacies in the model. Specifically, manikin chest stiffness and resistance may not accurately represent these characteristics in the same size human body. We designed our study to primarily assess chest compressions and subjects were asked to simulate rescue breathing. It is likely that if asked to assure adequacy of rescue breaths, rescuers may spend more time delivering ventilations hence reducing the compression quality. Finally, the possibility of a Hawthorne effect cannot be excluded despite subject data blinding. Since the subjects knew that they were being observed, their chest compression quality and effort may have been greater than would have been used in actual clinical situation.
Conclusions
This manikin study showed that during lone rescuer infant chest compression, two thumb compression provides higher compression depth and pressure compared to the two finger technique without any evidence of decay in quality or rescuer fatigue over 5 minutes. There is decay in compression depth over time with TF chest compression. There is no significant difference of quality of child chest compressions and fatigue between one hand and two hand, although both techniques pose significant metabolic demand. Our data suggest that the two thumb technique is preferred for infant chest compression and supports the current child chest compression guidelines.
Acknowledgements
We would like to thank the pediatric health care providers who contributed to this study with their own enthusiasm and effort, Biomedical Engineering at the University of Florida, Gainesville for help with manikin modification and the General Clinic Research Center at University of Florida, Gainesville for help with data collection and statistical analysis. Funding support for this project was provided in part by the Department of Pediatrics, University of Florida, Gainesville and by the University of Florida General Clinical Research Center, NIH Grant MO1-RR00082.
This research is supported in part by the University Of Florida General Clinical Research Center, NIH Grant MO1-RR00082
Footnotes
Conflict of interest: The authors have no conflict of interest to declare.
References
- 1.2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 2.2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric basic life support. Pediatrics. 2006;117:e989–1004. doi: 10.1542/peds.2006-0219. [DOI] [PubMed] [Google Scholar]
- 3.The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: neonatal resuscitation. Pediatrics. 2006;117:e978–988. doi: 10.1542/peds.2006-0350. [DOI] [PubMed] [Google Scholar]
- 4.Houri PK, Frank LR, Menegazzi JJ, et al. A randomized, controlled trial of two-thumb vs. two-finger chest compression in a swine infant model of cardiac arrest [see comment] Prehosp Emerg Care. 1997;1:65–67. doi: 10.1080/10903129708958789. [DOI] [PubMed] [Google Scholar]
- 5.Menegazzi JJ, Auble TE, Nicklas KA, et al. Two-thumb versus two-finger chest compression during CRP in a swine infant model of cardiac arrest. Ann Emerg Med. 1993;22:240–243. doi: 10.1016/s0196-0644(05)80212-4. [DOI] [PubMed] [Google Scholar]
- 6.Dorfsman ML, Menegazzi JJ, Wadas RJ, et al. Two-thumb vs. two-finger chest compression in an infant model of prolonged cardiopulmonary resuscitation. Acad Emerg Med. 2000;7:1077–1082. doi: 10.1111/j.1553-2712.2000.tb01255.x. [DOI] [PubMed] [Google Scholar]
- 7.Stevenson AG, McGowan J, Evans AL, et al. CPR for children: one hand or two? Resuscitation. 2005;64:205–208. doi: 10.1016/j.resuscitation.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 8.Peska E, Kelly AM, Kerr D, et al. One-handed versus two-handed chest compressions in paediatric cardio-pulmonary resuscitation. Resuscitation. 2006;71:65–69. doi: 10.1016/j.resuscitation.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Babbs CF, Voorhees WD, Fitzgerald KR, et al. Relationship of blood pressure and flow during CPR to chest compression amplitude: evidence for an effective compression threshold. Ann Emerg Med. 1983;12:527–532. doi: 10.1016/s0196-0644(83)80290-x. [DOI] [PubMed] [Google Scholar]
- 10.Ristagno G, Tang W, Chang YT, et al. The quality of chest compressions during cardiopulmonary resuscitation overrides importance of timing of defibrillation. Chest. 2007;132:70–75. doi: 10.1378/chest.06-3065. [DOI] [PubMed] [Google Scholar]
- 11.Ashton A, McCluskey A, Gwinnutt CL, et al. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation. 2002;55:151–155. doi: 10.1016/s0300-9572(02)00168-5. [DOI] [PubMed] [Google Scholar]
- 12.Ochoa FJ, Ramalle-Gomara E, Lisa V, et al. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation. 1998;37:149–152. doi: 10.1016/s0300-9572(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 13.Hightower D, Thomas SH, Stone CK, et al. Decay in quality of closed-chest compressions over time. Ann Emerg Med. 1995;26:300–303. doi: 10.1016/s0196-0644(95)70076-5. [DOI] [PubMed] [Google Scholar]
- 14.Srikantan SK, Berg RA, Cox T, et al. Effect of one-rescuer compression/ventilation ratios on cardiopulmonary resuscitation in infant, pediatric, and adult manikins. Pediatr Crit Care Med. 2005;6:293–297. doi: 10.1097/01.PCC.0000161621.74554.15. [DOI] [PubMed] [Google Scholar]