Abstract
Background:
Obesity in youth remains a major public health issue. Yet no effective long-term preventive strategy exists. We previously showed that a school-based socio-ecological approach targeting behavior and social/environmental influences on physical activity (PA) prevented 4-year excessive weight gain in 12-year olds. In this study, we investigated if this efficacy persists 30 months after intervention cessation.
Methods and Findings:
The program targeted students, family, school and the living environment to promote/support PA and prevent sedentary behavior (SB). A total of 732 students from eight randomized middle schools completed the 4-year trial. At the 30-month post-trial follow-up, body mass index (BMI), fat mass index (FMI), leisure PA (LPA), home/school/workplace active commuting, TV/video time (TVT), and attitudes toward PA were measured in 531 adolescents. The beneficial effects of the intervention on the excess BMI increase (+0.01 vs +0.34 kg m−2 in the intervention and control groups, respectively) and on the overweight incidence in initially non-overweight students (4.3% vs 8.6% odds ratio=0.48 (95% confidence interval: 0.23–1.01)) were maintained at the post-trial follow-up. LPA was not maintained at the level achieved during the trial. However, we still observed a prevention of the age-related decrease of the adolescents' percentage reporting regular LPA (−14.4% vs −26.5%) and a higher intention to exercise in the intervention group. The intervention promoted lower TVT (−14.0 vs +13.6 min per day) and higher active commuting changes (+11.7% vs −4.8%). Trends in higher BMI reduction in students with high initial TVT and in the least wealthy group were noted. TVT changes throughout the follow-up predicted excess BMI and FMI changes.
Conclusions:
Long-term multilevel approach targeting PA and SB prevents excessive weight gain up to 30 months after intervention cessation. The efficacy may be higher in the most sedentary and least wealthy adolescents. Healthy PA-related behavior inducing long-lasting weight effects can be promoted in youth providing that an ecological approach is introduced in the prevention strategy.
Keywords: physical activity, sedentary behavior, overweight, cluster randomized study, prevention
Introduction
Although recent studies suggest that the rise in obesity prevalence is slowing down or plateauing across Europe, United States of America or Australia,1 obesity in youth remains a major public health concern with a burdensome impact on health and well-being.2, 3, 4 Given the difficulties to manage obesity once established, this strengthens the need for effective primary prevention strategies in children and teenagers. In this context, physical activity (PA), although not the only determinant of excess weight, is a key recognized element in addressing the obesity epidemic and the associated metabolic and cardiovascular outcomes.5,6
Recent systematic reviews indicate that interventions targeting PA-related behavior may be effective in increasing activity levels and preventing overweight in youth.7, 8, 9, 10 The variety of approaches used and the heterogeneity of the effects may, however, explain why the effective strategies to obtain successful reduction in adiposity remain elusive. A limitation of most previous intervention studies is their lack of long-term follow-up, with only three studies reporting more than 1 year beneficial effects on adiposity.11, 12, 13 Therefore, little is known about sustainability of the effects of PA interventions on adiposity, an important issue for health promotion in general and obesity prevention in particular.7
Over the last years, besides individual and interpersonal factors, larger contextual characteristics have been recognized as important determinants of PA.14 Ecological models indicate that interventions targeting determinants at all levels, including environmental changes to reduce the barriers limiting the adoption of an active lifestyle, offer the best chance of sustained PA changes. Such strategies may also contribute to reducing the gaps in social15 and environmental16 inequities associated with obesity. If not limited to the school setting and integrating other dimensions of the ecological model such as co-participation and community partnering,17 they have the potential to increase not only leisure PA (LPA) but also non-exercise PA (for example, active transport), and to reduce sedentary behavior (SB). This is crucial given that a growing number of data shows that insufficient non-exercise PA and SB are associated with overweight/obesity, independent of the time spent exercising.18, 19, 20 These behavior changes may also be easier to maintain for the less active subjects.
In 2002, we initiated the Intervention Centered on Adolescents' Physical activity and Sedentary behavior (ICAPS) to test this socio-ecological hypothesis. ICAPS, a 4-year randomized controlled trial, enrolled 12-year-old adolescents from eight middle schools in Eastern France. We showed that the comprehensive PA/SB intervention prevented excessive weight gain.21 At the end of the trial, only 4.2% of the initially non-overweight adolescents were overweight in the intervention schools, compared with 9.8% in the control schools. Whether or not the beneficial effects of ICAPS on body mass index (BMI), PA and SB lasted after discontinuation of the intervention remains a central question to test the long-term efficacy of the socio-ecological approach.
In this study, we present the results of the ICAPS extended 30-month post-trial follow-up. We have further examined the influence of some students' characteristics on BMI changes and investigated potential predictors of these changes.
Materials and methods
Research design
ICAPS was a cluster-randomized controlled 4-year intervention study that started in 2002. The rationale, research design, intervention program and process evaluation were previously detailed.21, 22, 23 Briefly, four pairs of matched schools were randomly selected out of all public middle schools of the Department of Bas-Rhin (France). To ensure a broad socioeconomic representation, the randomization was based on stratification on geographical location, city size and location in a low-economic neighborhood. Randomization of intervention status was performed in each pair of schools. All six-graders were eligible for the trial. Four-year results of the ICAPS study were published in 2008.21 The present study, based on the cohort of 732 students who completed the trial, includes data obtained in 531 of them at a median post-trial follow-up of 30 months (26–38 months from the end of the intervention) corresponding to a median total follow-up of 76 months (72–84 months from the beginning of the trial). All study participants and their parents gave written informed consent both for the initial study and the post-trial survey that were approved by local institutional review board (ClinicalTrials.gov NCT00498459).
Participants
Ninety-one percent of eligible students accepted to participate to the initial trial. A total of 732 completed the 4-year trial and constitute the cohort of this report. The main reasons for not completing the trial were school transfers and absence at school on the day of the survey. Students who did not complete the trial were more frequently boys (60.8% vs 46.7%) and slightly older at the time of enrollment in the study (11.9±0.8 years vs 11.6±0.6 years) than those who completed the trial but had similar anthropometric and PA characteristics and were comparable between intervention and control groups.21
Intervention
Intervention students followed a program that began with the first school year and lasted until the end of the fourth school year and was added to the standard curriculum (three 50-min physical education sessions per week). Control students followed their usual school curriculum without any intervention. The intervention was based on the dynamic interplay between PA determinants and targeted not only the individuals but also their family and peers, and their living environment to promote and support adoption of an active lifestyle both inside and outside school, and to limit SB.22,24 Briefly, the program included an educational component. New opportunities for PA were offered taking into account the obstacles to being active. Enjoyment of participation was highlighted to help the less confident children to develop the skills needed to adopt an active lifestyle. Parents, educators, school-staffs and policy-makers were encouraged to provide a supportive environment through regular meetings. Sporting events, ‘cycling to school' days were organized and media diffusion used.
Post-trial follow-up
At the post-trial follow-up, the students were no longer in their initial middle schools and were either in high-schools (61 high-schools) or, for 25% of them, had left school, which explained the 1-year duration of the survey. The students were traced with the support of the county school government or through their last known home address or phone number. Six hundred students out of the seven hundred and thirty-two students who completed the trial were found, and five hundred and thirty-one (88.5%) accepted to participate in the post-trial survey (73.5% and 71.5% of the intervention and control groups, respectively). The survey measures were equally distributed over time between groups, and almost 80% of the adolescents were examined within the first 6 months of the post-trial survey.
Surveys and outcomes
The original trial consisted of a baseline survey that took place between September and October 2002, and annual surveys at the end of each of the 4 school years of intervention (between May and June). The primary outcome was BMI changes. Pre-specified secondary end points included changes in overweight prevalence, body composition, PA and SB, and attitudes toward PA.
The post-trial survey was based on the same standardized procedures than the first surveys. It was performed by trained professionals and interviewers in the school setting or in a health-care center. Height was measured with calibrated wall-mounted stadiometer. Weight and body composition were measured with Tanita TBF310 BIA (Tanita Corporation, Tokyo, Japan) using in-built equations. BMI, excess BMI (calculated by subtracting the gender–age-specific median BMI of the French reference curves25 from BMI), BMI z-score and fat mass index (FMI calculated as fat mass (kg) divided by the square of the height (m2)) were used as adiposity indicators. Even though BMI z-score is optimal for assessing adiposity on a single occasion, excess BMI has been proposed as a better scale for measuring changes over time.25 Overweight was defined according to the International Obesity Task Force gender-age-cutoffs.26 Self-reported LPA was assessed with the Modifiable Activity Questionnaire for adolescents.27 Time spent per week in supervised leisure PA (LPAT; excluding physical education classes) and regular participation in sports clubs (yes/no) were considered. Time spent in front of the TV/video (TVT) and in active commuting between home and school/worksite was recorded. TVT was expressed in minutes per day or in two categories (less or more than 2 h per day). Active commuting was categorized in less or more than 20 min per day. Self-efficacy, intention and social support toward exercise (inverse scores were considered so that higher scores indicate better outcomes) were assessed using the Stanford Adolescent Heart Health Program's questionnaire.28 Socioeconomic status (SES) was assessed by the highest initial occupational category of either parent in three categories (low, medium, high), as determined by the French socio-occupational nomenclature.29
Statistical analysis
Analyses were performed with the SAS software (version 9.3, SAS Institute Inc., Cary, NC, USA). Two-sided t-tests and χ2-tests were used to assess attrition bias between groups. Statistical significance was defined as P<0.05.
The changes in the outcomes during the intervention and at the post-trial follow-up were analyzed using mixed linear models taking into account the cluster randomization and the repeated individual data over time using PROC MIXED and GLIMMIX (SAS Institute Inc.). Schools within baseline stratification, and individuals within schools were considered as random effects. Main effects were intervention group, time and intervention-by-time interaction. Fixed effects were gender, SES, baseline socio-geographic stratification, sexual maturity, sports club participation and the baseline level of the outcome. Based on the Akaike Information Criterion, a spatial power covariance structure was found to be the most appropriate. Within-group changes over time and their differences across groups are presented. Possible heterogeneity of the intervention's effect was tested. Because no interaction with any of the baseline variables (P>0.10) was identified, the models were not adjusted for these interactions. The cumulative incidence of overweight in initially non-overweight students was analyzed using the same models.
In order to identify potential moderators of the intervention's effects on excess BMI and FMI, exploratory analyses stratified on gender, SES, baseline initial weight status (overweight vs non-overweight), sports club participation and high initial TVT were performed. Finally, we tested the association of changes in PA/SB with changes in excess BMI and FMI using the same mixed linear models taking into account the cluster randomization. To do so, two strategies were used. We first introduced in the models, together with the previously described fixed effects, baseline and repeated measurements of LPAT, TVT and active commuting as covariables to successively predict excess BMI and FMI changes over time, and to estimate their mediating effects. We then assessed the associations between the overall changes in PA/SB (from the beginning of the trial to the end of the follow-up) with the overall changes in excess BMI (respectively, FMI) in the combined intervention and control groups. The overall changes of PA/SB were calculated by subtracting the baseline levels of the variables from corresponding measurements during the total follow-up and categorized into tertiles. Because the analyses presented here are only exploratory, no adjustment was made for multiple comparison tests.
Results
Characteristics of subjects included in the post-trial follow-up study
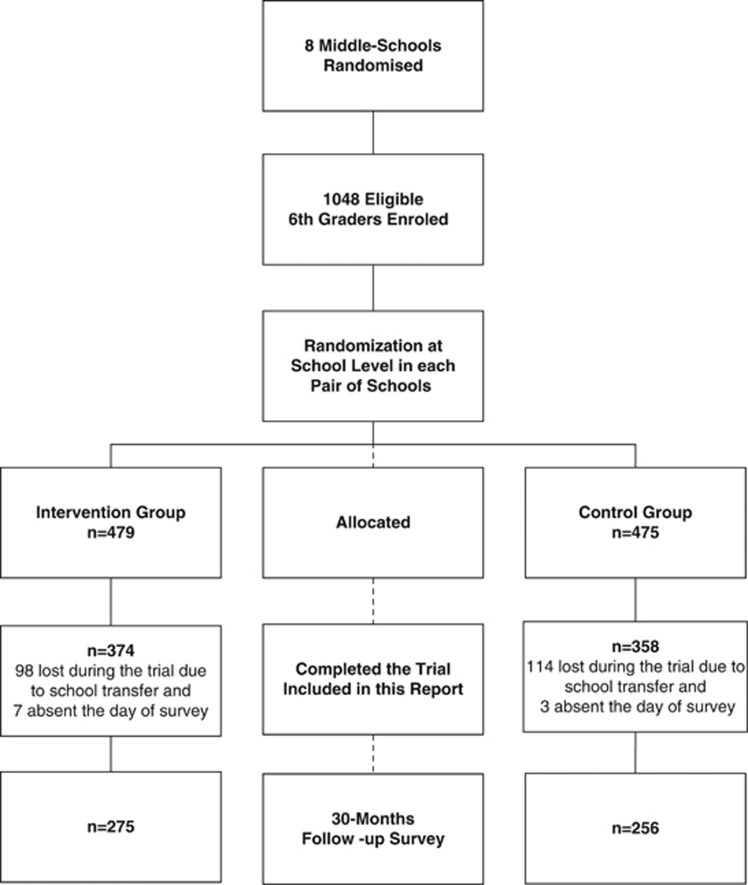
Follow-up outcomes were obtained from 531 participants (Figure 1), with a median post-trial follow-up of 30 months. Baseline characteristics of the 732 six-graders, who completed the trial, and of the 531 subjects measured at the follow-up survey are presented in Table 1. Students who did not complete the post-trial survey were more frequently from low SES (37.4% vs 21% P<0.001) and slightly older at the time of enrollment in the trial (mean±s.d. of 11.8±0.7 vs 11.4±0.5 years; P<0.01), but had the same overweight prevalence (22.9% vs 21.8%). Initial characteristics of the lost-to-follow-up students did not differ between groups, although boys tended to be under-represented in the intervention group (P=0.06).
Figure 1.
Trial chart.
Table 1. Initial characteristics of the cohort participants.
|
Participants who completed the trial |
Participants seen at the post-trial follow-up |
|||
|---|---|---|---|---|
| Intervention | Control | Intervention | Control | |
| N | 374 | 358 | 275 | 256 |
| Age at inclusion (year) | 11.5 (0.6) | 11.60 (0.6) | 11.4 (0.5) | 11.5 (0.5) |
| Males | 44.10% | 49.50% | 41.50% | 49.70% |
| Overweight/obesity prevalence | 21.40% | 22.70% | 21.50% | 22.30% |
| Weight (kg) | 41.6 (9.4) | 42.8 (10.4) | 41.1 (9.1) | 41.6 (9.2) |
| Body mass index (kg m−2) | 18.6 (3.3) | 18.8 (3.5) | 18.5 (3.3) | 18.5 (3.1) |
| Excess body mass index (kg m−2) | 1.56 (3.26) | 1.73 (3.48) | 1.57 (3.27) | 1.48 (3.06) |
| Z body mass index (kg m−2) | 0.56 (1.43) | 0.62 (1.43) | 0.57 (1.44) | 0.54 (1.34) |
| Body fat (%) | 18.2 (8.6) | 18.2 (8.6) | 18.3 (8.4) | 17.8 (8.1) |
| Fat mass index (kg m−2) | 3.63 (2.28) | 3.72 (2.48) | 3.66 (2.26) | 3.53 (2.15) |
| Fat-free mass index (kg m−2) | 14.99 (1.47) | 15.12 (1.53) | 14.91 (1.43) | 15.00 (1.40) |
| Sport-club participation | 63.70% | 57.20% | 66.60% | 60.70% |
| Leisure physical activity time (h per week) | 2.6 (3.1) | 2.5 (3.1) | 2.7 (3.1) | 2.7 (3.1) |
| TV/video time > 2 h | 31.20% | 25.70% | 30.90% | 24.70% |
| TV/video time (min per day) | 110.9 (83.8) | 103.0 (75.3) | 108.5 (82.1) | 98.4 (68.6) |
| Active commuting home/school >20 min | 31.10% | 33.40% | 32.10% | 30.10% |
Values are means (s.d.) or percentages. Overweight is defined according to the International Obesity Task Force gender–age cutoffs. Excess BMI was calculated by subtracting the gender- and age-specific median BMI of the French reference curves25 from BMI.
Anthropometric data
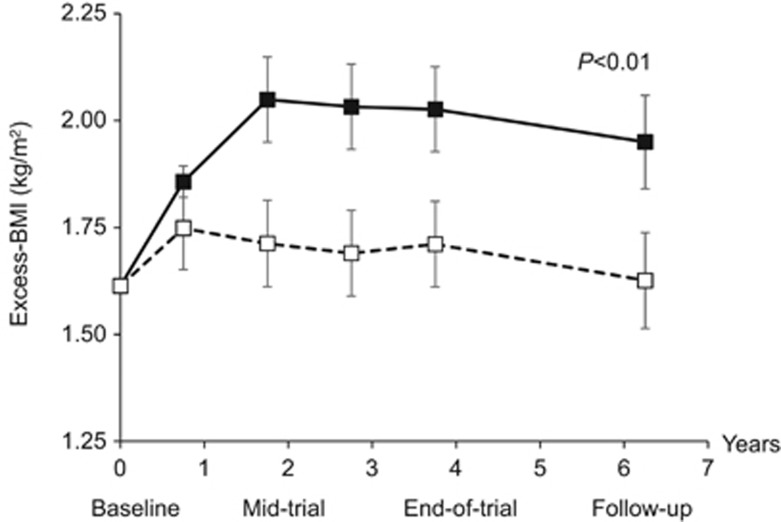
Adjusted mean changes in anthropometric data during the trial and at the post-trial follow-up are presented with their 95% confidence intervals (95% CIs) in Table 2. Evolution of excess BMI is illustrated in Figure 2. In the control group, there was an increase in excess BMI until the second year of the trial (+0.44 kg m−2), followed by a plateau and even a slight decrease during the post-trial follow-up. The intervention reduced the initial excess BMI increase, resulting in a difference across groups that was maintained throughout the entire trial and at the post-trial follow-up with an intervention effect of P=0.01 and a non-significant intervention-by-time P-value. At the post-trial follow-up, the adjusted mean difference in excess BMI across groups was -0.32 kg m−2 (P=0.03), which was similar to the difference observed at the end of the trial. Similar results were observed for BMI and BMI z-score. The intervention also attenuated the initial FMI increase observed in the control group (P=0.03), but the difference across groups was significantly reduced at the end of the trial and at the post-trial follow-up (intervention-by-time interaction P=0.02).
Table 2. Adjusted changes in anthropometric and PA/SB-related variables from baseline to the trial period and the post-trial follow-up.
| Variable | Intra-cluster correlations | Group | Baseline valuesa | Changes after 2 years of triala | Changes at the end of the triala | Changes at the post-trial follow-upa | P intervention | P interaction intervention-by-time |
|---|---|---|---|---|---|---|---|---|
| Excess body mass index (kg m−2) | 0.035 | Intervention | 1.61 | +0.10 (−0.10 to 0.29) | +0.10 (−0.10 to 0.29) | +0.01 (−0.20 to 0.23) | ||
| Control | +0.44 (0.24 to 0.63) | +0.41 (0.22 to 0.61) | +0.34 (0.12 to 0.56) | |||||
| Difference Intervention-Control | −0.34 (−0.62 to 0.05) | −0.32 (−0.60 to 0.03) | −0.32 (−0.64 to 0.01) | <0.01 | 0.99 | |||
| z-Body mass index (kg m−2) | 0.020 | Intervention | 0.60 | −0.03 (−0.10 to 0.05) | −0.08 (−0.16 to −0.01) | −0.14 (−0.23 to −0.06) | ||
| Control | +0.09 (0.02 to 0.16) | +0.03 (−0.04 to 0.10) | −0.03 (−0.12 to 0.05) | |||||
| Difference Intervention-Control | −0.11 (−0.22 to −0.01) | −0.11 (−0.22 to −0.01) | −0.11 (−0.22 to 0.00) | 0.02 | 0.99 | |||
| Body mass index (kg m−2) | 0.039 | Intervention | 18.64 | +1.12 (0.92 to 1.31) | +2.44 (2.25 to 2.63) | +3.54 (3.33 to 3.76) | ||
| Control | +1.45 (1.25 to 1.65) | +2.71 (2.51 to 2.90) | +3.87 (3.65 to 4.09) | |||||
| Difference Intervention-Control | −0.33 (−0.61 to 0.05) | −0.27 (−0.55 to 0.01) | −0.33 (−0.64 to 0.02) | <0.01 | 0.90 | |||
| Fat mass index (kg m−2) | 0.016 | Intervention | 3.65 | +0.23 (0.06 to 0.40) | +0.81 (0.64 to 0.97) | +0.76 (0.57 to 0.94) | ||
| Control | +0.58 (0.41 to 0.75) | +0.92 (0.75 to 1.09) | +0.93 (0.73 to 1.12) | |||||
| Difference intervention-control | −0.35 (−0.59 to 0.11) | −0.11 (−0.35 to 0.13) | −0.17 (−0.44 to 0.10) | 0.03 | 0.02 | |||
| LPAT (h per week) | 0.016 | Intervention | 2.59 | +0.67 (0.28 to 1.07) | +0.90 (0.50 to 1.29) | −0.32 (−0.75 to 0.11) | ||
| Control | +0.19 (−0.21 to 0.59) | −0.05 (−0.45 to 0.35) | −0.74 (−1.19 to 0.29) | |||||
| Difference Intervention-Control | +0.48 (−0.08 to 1.05) | +0.94 (0.38 to 1.51) | +0.42 (−0.21 to 1.04) | <0.001 | 0.03 | |||
| Regular LPA > 30 min per week (%) | 0.084 | Intervention | 60.0 | +30.6 (27.4 to 33.0) | +28.3 (24.8 to 31.1) | −14.4 (−20.6 to 8.1) | ||
| Control | +2.7 (−3.1 to 8.1) | −4.5 (−10.4 to 1.2) | −26.5 (−32.3 to −20.3) | |||||
| OR (95% CI) intervention vs control | 6.0 (3.9 to 9.1) | 6.3 (4.2 to 9.4) | 1.7 (1.2 to 2.4) | <0.001 | <0.001 | |||
| TVT (min per day) | 0.056 | Intervention | 106.2 | −3.3 (−13.9 to 7.3) | −19.9 (−30.4 to −9.3) | −14.0 (−25.3 to −2.8) | ||
| Control | +12.0 (1.2 to 22.8) | −4.7 (−15.5 to 6.1) | +13.6 (1.7 to 25.4) | |||||
| Difference intervention-control | −15.3 (−30.5 to −0.2) | −15.2 (−30.3 to 0.01) | −27.6 (−44.0 to −11.3) | 0.02 | 0.06 | |||
| Active commuting home/schoolb (%) | 0.150 | Intervention | 32.0 | +8.2 (2.7 to 13.9) | +20.7 (15.0 to 26.4) | +11.7 (5.5 to 18.1) | ||
| Control | +1.8 (−3.7 to 7.9) | +15.7 (9.6 to 21.9) | −4.8 (−10.8 to 2.0) | |||||
| OR (95% CI) intervention vs control | 1.3 (0.9 to 1.9) | 1.2 (0.9 to 1.7) | 2.1 (1.4 to 3.5) | <0.001 | 0.09 |
Abbreviations: CI, confidence interval; LPA, leisure physical activity; LPAT, LPA time; OR, odds ratio; PA, physical activity; SB, sedentary behavior; TVT, TV/video time.
Values are adjusted means (95% CI).
>20 min. Changes are calculated with reference to baseline values. Excess BMI was calculated by subtracting the gender–age-specific median BMI of the French reference curves from BMI. Analyses were done by using mixed linear models taking into account the cluster randomization and the repeated individual data over time, with different baseline covariables as fixed effects. The intervention effect represents the global effect of the intervention over time, whereas the intervention-by-time interaction evaluates whether the intervention effect is changing over time, (that is, non-significant result indicates that the effect was maintained at the same level at the post-trial follow-up).
Figure 2.
Evolution of excess BMI during the trial period and at the post-trial follow-up. Values are presented as adjusted means±s.e.m. Black and white squares represent the control and intervention groups, respectively. Excess BMI was calculated by subtracting the gender- and age-specific median BMI of the French reference curves25 from BMI. Analyses were done using mixed linear models taking into account the cluster randomization and the repeated individual data over time, with different baseline covariables as fixed effects.
The reduction in the cumulative overweight incidence in initially non-overweight students induced by the intervention at the end of the trial was maintained after cessation of the program (overall P=0.01). The cumulative incidence rates at the post-trial follow-up were 8.6% (95% CI: 5.5–13.2) in the intervention group and 4.3% (95% CI: 2.4–7.5) in the control group. The corresponding odds ratio (OR) was 0.48 (95% CI: 0.23–1.01).
Physical activity and sedentary behavior
As expected during adolescence, extra-curriculum LPAT dramatically decreased in the control group from an adjusted mean of 2.59 h per week at baseline to 1.85 h per week at the post-trial follow-up. Simultaneously, the percentage of control adolescents reporting a regular LPA practice (that is, greater than 30 min per week) decreased from 60 to 26.5% (Table 2). The higher levels of LPAT induced by the program during the trial (almost 1 h per week more than in the control group at the end of the trial; P<0.001) was not maintained at the same level once the intervention stopped (intervention-by-time interaction P=0.03). However, the decrease of the students' percentage still reporting regular LPA practice at the post-trial follow-up was lower in the intervention than in the control group (−14.4% vs −26.5% OR= 1.7 (95% CI: 1.2–2.4)), resulting in an adjusted mean LPAT at the post-trial survey of 2.27 h per week (+0.42 h per week (95% CI: −0.21 to 1.04)) as compared with control students. The intervention also induced an improvement in the intention to practice exercise that persisted at the time of follow-up (P<0.001). The differences in self-efficacy and perceived social support were, however, no longer significant 30 months after cessation of the intervention (data not shown).
The intervention group also reported a lower TVT (P=0.02) with a difference across groups that not only was maintained at the post-trial follow-up but also even increased (intervention-by-time interaction P=0.06) resulting in an adjusted mean difference across groups of −27.6 min per day. Moreover, although the impact of the program on active commuting was not significant during the 4-year trial, at the post-trial follow-up the percentage of adolescents reporting a regular daily active commuting between home and school/workplace (>20 min per day) had increased by 11.7% in the intervention group, whereas it had decreased by 4.8% in the control group (OR=2.1 (95% CI: 1.4–3.5)).
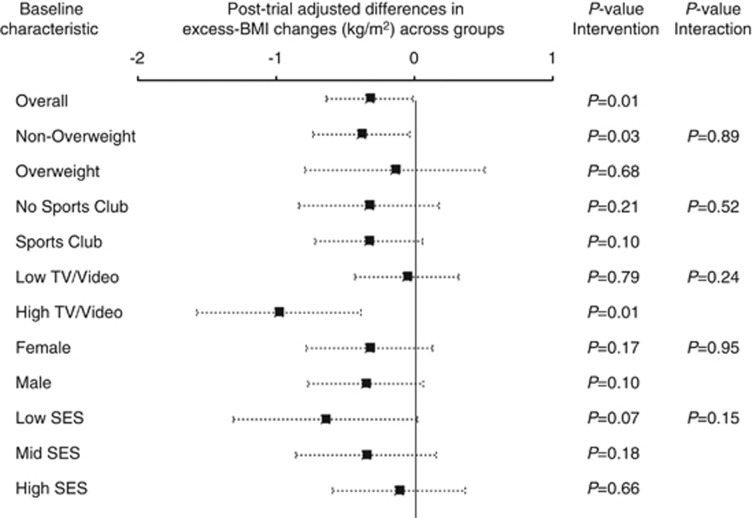
Moderators of the intervention impact on BMI
Although the interactions were not significant (P>0.10), exploratory analyses according to specific baseline characteristics (Figure 3) indicated that the intervention tended to induce a higher decrease in excess BMI in students with high initial TVT levels (>2 h per day) and in the least wealthy group. The adjusted mean difference in excess BMI changes across groups at the post-trial follow-up was −0.98 kg m−2 (95% CI: −1.56 to −0.38) in students with high baseline TVT (>2 h per day) vs −0.05 kg m−2 (95% CI: −0.43 to 0.32) in students with low baseline TVT. The adjusted mean difference in excess BMI changes across groups was −0.64 kg m−2 (95% CI: −1.31 to 0.02) in the least wealthy students vs −0.35 kg m−2 (95% CI: −0.85 to 0.16) in those of middle SES and −0.11 kg m−2 (95% CI: −0.59 to 0.37) in those of high SES. Similarly, the adjusted mean differences in FMI changes across groups tended to be higher in students with high compared with low baseline TVT (−0.55 kg m−2 (95% CI: −1.03 to 0.09) vs 0.01 kg m−2 (95% CI: −0.29 to 0.30)) and in low compared with high SES students (−0.41 kg m−2 (95% CI: −0.95 to 0.12) vs −0.01 kg m−2 (95% CI: −0.39 to 0.36)).
Figure 3.
Differences across groups in excess BMI change at the post-trial follow-up according to different baseline characteristics. The black boxes represent the effect sizes (adjusted mean differences in excess BMI changes) and the horizontal dotted lines represent the 95% confidence intervals, separately for each of the categories of the baseline characteristic of interest. The P-values represent the intervention effect and the heterogeneity across subgroups of baseline characteristics. Excess BMI was calculated by subtracting the gender- and age-specific median BMI of the French reference curves25 from BMI. Analyses were done using mixed linear models taking into account the cluster randomization and the repeated individual data over time, with different baseline covariables as fixed effects.
Predictors of changes in BMI and FMI at the post-trial follow-up
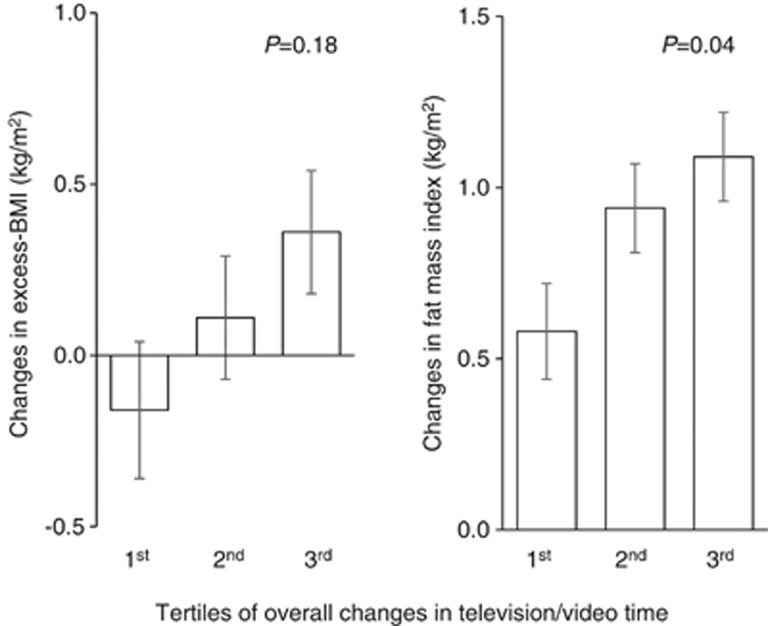
Mixed linear models taking into account the cluster randomization with both baseline and repeated PA/SB data as covariables were used to examine the associations of PA/SB-related behavior with, successively, excess BMI and FMI changes, and to estimate their mediating effect. If TVT changes over time predicted changes in excess BMI and in FMI, no such association was observed with LPAT or active commuting. A change of +1 h per week in TVT throughout the study was associated with changes in excess BMI and FMI of +0.07 kg m−2 (P<0.01 and P<0.05, respectively). Introduction of TVT changes in the models reduced the intervention effect on excess BMI and FMI by 34.8% and 27.4%, respectively, indicating that TVT changes explained about one-third of the overall intervention effect on adiposity.
The Figure 4 further illustrates the positive association between adiposity and TVT changes. In combined groups, overall adjusted changes in excess BMI were, respectively, −0.16 kg m−2 (95% CI: −0.55 to −0.23) and +0.36 kg m−2 (95% CI: 0.01–0.71) in the lowest and highest tertiles of overall TVT changes (P=0.18); overall adjusted changes in FMI were 0.58 kg m−2 (95% CI: 0.31–0.86) and 1.09 kg m−2 (95% CI: 0.84–1.35), respectively (P=0.04).
Figure 4.
Excess BMI and FMI at the post-trial follow-up according to tertiles of overall changes in television/video time during the total follow-up period. Values are presented as adjusted means±s.e.m. for each tertile of overall TV/video time changes. Medians of TV/video changes are, respectively, -56 min per day; 5 min per day and +52 min for each tertile. Excess BMI was calculated by subtracting the gender- and age-specific median BMI of the French reference curves25 from BMI. Analyses were done using mixed linear models taking into account the cluster randomization, with different baseline covariables as fixed effects.
Discussion
We assessed whether the beneficial effect on weight of an ecological intervention targeting both PA and SB in adolescents lasted after the program cessation. We observed a significant effect of the intervention on BMI measured 30 months after the end of the 4-year trial. There was also a significant reduction in the cumulative incidence of overweight in the subgroup of students who were not overweight at the beginning of the trial. The intervention slowed down the well-described adolescence-related decrease in LPA30 that was observed in the control schools, although the high levels of LPAT noted during the trial were not maintained at the post-trial follow-up. It was further associated with a significant reduction in TVT, as a proxy of SB, and an increase in active commuting between home and school or workplace, indicating that the students who received the intervention were able to transfer the competences they acquired during the intervention to their daily life. Exploratory analyses indicated that changes in time spent in front of TV/video mediate, at least in part, the sustained effects of the intervention on BMI. They also suggested that the intervention might contribute to reducing the gap in health social inequities with a higher effect on weight gain in the least wealthy and the most sedentary students.
Maintenance over time of prevention strategies is critical. Although there is some indication that PA interventions may have some efficacy to prevent obesity in children, a great number of studies are of short duration and a very few evaluated the effects of the interventions after the program was stopped.7 Three studies showed a beneficial effect on adiposity that lasted for at least 1 year.11, 12, 13 In two of them, the program combined an educational or behavioral component with a social/environmental component. In the first study,13 schools were encouraged to offer additional physical education classes and advised on changes in and around cafeterias resulting in a reduction in consumption of sugar-containing beverages, which limits the conclusions about the specific effect of the PA-related program. Interestingly, in the second study,12 which combined a fundamental movement skill component through PA classes and a behavioral (PA and SB) component including a parental encouragement to support the behavioral changes, each of the components used alone had some effect on either PA or SB but not on adiposity. Altogether these results support the idea that the multilevel approach used in our study was one of the keys to its sustained efficacy on weight after the end of the program.
Targeting the different PA components (LPA inside and outside school but also non-exercise activities of light-to-moderate intensity such as active commuting, and SB) was probably crucial to explain the sustained effects on BMI in our study. There is now striking emerging evidence that excessive SB (that is, too much sitting) is an important determinant of overweight and related cardio-metabolic biomarkers in children and adults.19,31 Importantly, the negative relationships observed between SB and the health outcomes are independent of the time spent in exercising.32,33 ICAPS induced a reduction in TVT that was even greater at the post-trial follow-up than during the trial. Moreover, although TVT is an incomplete proxy for total SB, baseline TVT was a moderator of the intervention efficacy on weight, that is, the higher the baseline TVT, the higher the intervention effect on BMI was. TVT changes also predicted adiposity changes during the total follow-up period and partly mediated the effects of the intervention. Altogether, our data indicate that the PA increase induced by the program was likely not due to a displacement of other physical activities, as frequently reported with training programs of higher intensity, but rather to a decrease in time spent on sedentary activities. Besides its direct impact on BMI, TVT reduction may also be an indirect mirror-image of an increase in total PA more important than that reflected by just LPA. Non-supervised LPA and non-exercise PA, known to represent major components of PA-related energy expenditure,20 were not accurately measured in our study. An increase in these components in the intervention group is suggested by the increase in both active commuting between home and school/workplace and intention to practice PA, a score that has been associated with higher actual and prospective PA practice.28
The maintenance of the effects of ICAPS trial may also be due to the unique intervention duration of 4 years; attractive and convenient activities, crucial for improving students' attitudes and skills regarding PA; and an implementation of the program with the individuals and school institutions in link with communities and families, which supported the integration of PA in everyday life and favored long-term changes by inducing new lifestyle habits. We postulate that the comprehensive approach of the individual in its environment was essential not only to enhance motion in the most sedentary and inactive students and changing their self-efficacy and skills regarding PA, but also to improve their perception of the accessibility to PA opportunities in their living environment. Recent studies indicate that, besides objectively measured spatial accessibility to PA facilities, the subjective perception of the environmental characteristics related to PA is an important determinant of PA practices.34
The interaction between weight status at baseline and the impact of intervention on BMI was not significant. However, as indicated by stratified analyses, the effect of the intervention on the post-trial follow-up BMI tended to be lower in initially overweight students than in non-overweight ones. As suggested by the data obtained at the end of the trial showing that a matched group of students, who were unaware of any survey and of any intervention, presented higher BMI and FMI than the students of the control group,21 we cannot exclude that the mid-trial communication of the program in the media at the county level had a contamination effect on overweight control students. However, the modest effect of the intervention in the initially overweight students is also in agreement with clinical studies showing that, if PA is an important component of obesity management, long-term weight loss probably requires specific complementary strategies including dietary counseling and substantial investment of therapists. It seems also attractive to expect that combined nutrition and PA interventions better prevent overweight in children, although more effective interventions are still needed.35
Equity of population-based prevention programs is an important concern. The intervention used here tended to be associated with a higher impact in the less wealthy subgroup of adolescents with an interaction between SES and intervention nearly reaching significance. Although the intervention was not limited to the school setting, the school grounding of the intervention was a unique way of reaching and educating all the children, even the most vulnerable ones and those from the least concerned parents. Moreover, several objective and subjective barriers to be physically active, including individual, social or environmental (cost, low temporal and spatial accessibility, safety), factors are known to be associated with lower SES. We showed that the relationship between a low spatial accessibility to PA facilities is associated with a higher risk of being overweight in low SES children only.16 Thus, we assume that, as previously reported,36 the simultaneous action on the different levels of the socio-ecological models of behavior and health and the co-participation of the targeted populations and institutions were important to reduce the gap in social health inequities.
Although the strengths of our study include the randomized design, the long-term follow-up, the high participation rate in the surveys, the measurement of both BMI and body composition, the assessment of outcomes by recognized methods (for example, Modifiable Activity Questionnaire) with extensive assessment of various dimensions of PA and SB including active commuting, we have to indicate some limitations. The study was originally not designed for stratified analyses as performed in this paper. Therefore, the results of moderation analyses should be taken with caution, especially given that less wealthy children were more often lost at follow-up. Importantly, the loss of children from low SES was similar in the two groups. PA and SB were not objectively assessed (for example, motion sensors), which may limit the insight into the different PA components. Because the intervention was facilitated by the study promoters and because the study was restricted to one French county, its feasibility and effectiveness at the large national level remain to be evaluated. Such a research program that will also investigate the transferability in other age categories is being conducted with the collaboration of the French Public Health Authorities.
In conclusion, our study indicates that an obesity prevention school-based program, based on a comprehensive approach to both PA and SB, prevents excessive weight gain with beneficial effects being maintained up to 30 months after the end of the intervention. The observation that the efficacy may be higher in the more sedentary and less wealthy students is encouraging. These data indicate that prevention of excess weight gain in adolescence is feasible through the synergistic actions of multiple partners and that long-lasting effects can be obtained.
Acknowledgments
This study was supported by grants from National Research Programs (INSERM and INRA PRNA 2002; ANR ALIA 2008); the Regional Health Insurance of Alsace-Moselle; French Public Authorities through the Health, and the Youth and Sports Departments; Conseil General du Bas-Rhin; Municipalities of Drusenheim, Illkirch-Graffenstaden, Obernai and Schiltigheim; and the Wyeth and Lab Fundation. C Simon initiated the ICAPS study, supervised its management and data analysis, and had primary responsibility for writing this paper. C Simon and J Dugas did statistical analyses. C Platat coordinated the study and, along with B Schweitzer and N Copin, was responsible for the data acquisition. F Hausser and S Blanc were involved in the design of the post-trial follow-up study. E Lefai, A Bergouignan and S Blanc assisted in interpretation and writing the manuscript. All authors commented on drafts and approved the manuscript.
The authors declare no conflict of interest.
References
- Olds T, Maher C, Zumin S, Peneau S, Lioret S, Castetbon K, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes. 2011;6:342–360. doi: 10.3109/17477166.2011.605895. [DOI] [PubMed] [Google Scholar]
- Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–1885. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5:4–104. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, Gordon B, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med. 2011;364:1315–1325. doi: 10.1056/NEJMoa1006992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohl HW, Craig CL, Lambert EV, Inoue S, Alkandari JR, Leetongin G, et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380:294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev. 2013;2:CD007651. doi: 10.1002/14651858.CD007651.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;7:CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- Kriemler S, Meyer U, Martin E, van Sluijs EM, Andersen LB, Martin BW. Effect of school-based interventions on physical activity and fitness in children and adolescents: a review of reviews and systematic update. Br J Sports Med. 2011;45:923–930. doi: 10.1136/bjsports-2011-090186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath GW, Parra DC, Sarmiento OL, Andersen LB, Owen N, Goenka S, et al. Evidence-based intervention in physical activity: lessons from around the world. Lancet. 2012;380:272–281. doi: 10.1016/S0140-6736(12)60816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manios Y, Kafatos I, Kafatos A, Preventive M, Nutrition Clinic Research T Ten-year follow-up of the Cretan Health and Nutrition Education Program on children's physical activity levels. Prev Med. 2006;43:442–446. doi: 10.1016/j.ypmed.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Salmon J, Ball K, Hume C, Booth M, Crawford D. Outcomes of a group-randomized trial to prevent excess weight gain, reduce screen behaviours and promote physical activity in 10-year-old children: switch-play. Int J Obes (Lond) 2008;32:601–612. doi: 10.1038/sj.ijo.0803805. [DOI] [PubMed] [Google Scholar]
- Singh AS, APMJ Chin, Brug J, van Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163:309–317. doi: 10.1001/archpediatrics.2009.2. [DOI] [PubMed] [Google Scholar]
- Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJF, Martin BW. Correlates of physical activity: why are some people physically active and others not. Lancet. 2012;380:258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- Lioret S, Touvier M, Dubuisson C, Dufour A, Calamassi-Tran G, Lafay L, et al. Trends in child overweight rates and energy intake in France from 1999 to 2007: relationships with socioeconomic status. Obesity (Silver Spring) 2009;17:1092–1100. doi: 10.1038/oby.2008.619. [DOI] [PubMed] [Google Scholar]
- Casey R, Chaix B, Weber C, Schweitzer B, Charreire H, Salze P, et al. Spatial accessibility to physical activity facilities and to food outlets and overweight in French youth. Int J Obes (Lond) 2012;36:914–919. doi: 10.1038/ijo.2012.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard L, Gauvin L, Raine K. Ecological Models Revisited: Their Uses and Evolution in Health Promotion Over Two Decades. Annu Rev Public Health. 2011;32:307–326. doi: 10.1146/annurev-publhealth-031210-101141. [DOI] [PubMed] [Google Scholar]
- Bergouignan A, Rudwill F, Simon C, Blanc S. Physical inactivity as the culprit of metabolic inflexibility: evidence from bed-rest studies. J Appl Physiol. 2011;111:1201–1210. doi: 10.1152/japplphysiol.00698.2011. [DOI] [PubMed] [Google Scholar]
- Dunstan DW, Howard B, Healy GN, Owen N. Too much sitting—a health hazard. Diabetes Res Clin Pract. 2012;97:368–376. doi: 10.1016/j.diabres.2012.05.020. [DOI] [PubMed] [Google Scholar]
- Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–2667. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- Simon C, Schweitzer B, Oujaa M, Wagner A, Arveiler D, Triby E, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J Obes (Lond) 2008;32:1489–1498. doi: 10.1038/ijo.2008.99. [DOI] [PubMed] [Google Scholar]
- Simon C, Wagner A, Platat C, Arveiler D, Schweitzer B, Schlienger JL, et al. ICAPS: a multilevel program to improve physical activity in adolescents. Diabetes Metab. 2006;32:41–49. doi: 10.1016/s1262-3636(07)70245-8. [DOI] [PubMed] [Google Scholar]
- Simon C, Wagner A, DiVita C, Rauscher E, Klein-Platat C, Arveiler D, et al. Intervention centred on adolescents' physical activity and sedentary behaviour (ICAPS): concept and 6-month results. Int J Obes Relat Metab Disord. 2004;28:S96–S103. doi: 10.1038/sj.ijo.0802812. [DOI] [PubMed] [Google Scholar]
- Rostand F, Simon C, Ulmer Z (eds). Promouvoir l'activité physique des jeunes: Élaborer et développer un projet de type Icaps. Guides INPES; Dossiers en Action; Direct. Thanh Le Luong, 2012. Available from http://www.inpes.fr/CFESBases/catalogue/pdf/1347.pdf .
- Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile. Eur J Clin Nutr. 2005;59:419–425. doi: 10.1038/sj.ejcn.1602090. [DOI] [PubMed] [Google Scholar]
- Cole T, Bellizzi M, Flegal K, Dietz W. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aaron DJ, Kriska AM, Dearwater SR, Anderson RL, Olsen TL, Cauley JA, et al. The epidemiology of leisure physical activity in an adolescent population. Med Sci Sports Exerc. 1993;25:847–853. doi: 10.1249/00005768-199307000-00014. [DOI] [PubMed] [Google Scholar]
- Reynolds KD, Killen JD, Bryson SW, Maron DJ, Taylor CB, Maccoby N, et al. Psychosocial predictors of physical activity in adolescents. Prev Med. 1990;19:541–551. doi: 10.1016/0091-7435(90)90052-l. [DOI] [PubMed] [Google Scholar]
- Insee. French National Institute of Statistics and Economic Studies [Institut national de la statistique et des etudes economiques]. Available from: : http://www.insee.fr/fr/ .
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, et al. Youth risk behaviour surveillance United States 2007. MMWR Surveill Summ. 2008;57:1–131. [PubMed] [Google Scholar]
- Tremblay MS, LeBlanc AG, Kho ME, Saunders TJ, Larouche R, Colley RC, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8:98. doi: 10.1186/1479-5868-8-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancox R, Milne B, Poulton R. Association between child and adolescent television viewing and adult health: a longitudinal birth cohort study. Lancet. 2004;364:257–262. doi: 10.1016/S0140-6736(04)16675-0. [DOI] [PubMed] [Google Scholar]
- Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996-2011. Am J Prev Med. 2011;41:207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- Dunton GF, Kaplan J, Wolch J, Jerrett M, Reynolds KD. Physical environmental correlates of childhood obesity: a systematic review. Obes Rev. 2009;10:393–402. doi: 10.1111/j.1467-789X.2009.00572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoelscher DM, Kirk S, Ritchie L, Cunningham-Sabo L. Position of the Academy of Nutrition and Dietetics: interventions for the prevention and treatment of pediatric overweight and obesity. J Acad Nutr Diet. 2013;113:1375–1394. doi: 10.1016/j.jand.2013.08.004. [DOI] [PubMed] [Google Scholar]
- De Bourdeaudhuij I, Van Cauwenberghe E, Spittaels H, Oppert JM, Rostami C, Brug J, et al. School-based interventions promoting both physical activity and healthy eating in Europe: a systematic review within the HOPE project. Obes Rev. 2011;12:205–216. doi: 10.1111/j.1467-789X.2009.00711.x. [DOI] [PubMed] [Google Scholar]