Abstract
Aims
To estimate physical activity trajectories for persons who quit smoking, and compare them to what would have been expected, had smoking continued.
Design, Setting and Participants
5115 participants to the CARDIA Study, a population-based study of African American and European American people recruited at age 18-30 years in 1985/6 and followed over 25 years.
Measurements
Physical activity was self-reported during clinical examinations at years 0(1985/6),2,5,7,10,15,20 and 25(2010/11); smoking status was reported each year (at examinations or by phone, and imputed where missing). We used mixed linear models to estimate trajectories of physical activity under varying smoking conditions, with adjustment for participant characteristics and secular trends.
Findings
We found significant interactions by race-sex (P=.02 for the interaction with cumulative years of smoking), hence we investigated the subgroups separately. Increasing years of smoking were associated with a decline in physical activity in black and white women and black men (e.g. coefficient for 10 years of smoking:−0.14; 95% CI:−0.20 to −0.07,P<0.001 for white women). An increase in physical activity was associated with years since smoking cessation in white men (coefficient 0.06;95%CI:0 to 0.13,P=0.05). The physical activity trajectory for persons who quit progressively diverged towards higher physical activity from the expected trajectory had smoking continued. For example, physical activity was 34% higher (95%CI:18%,52%;P<0.001) for white women 10 years after stopping compared with continuing smoking for those 10 years(P = 0.21 for race/sex differences).
Conclusions
Smokers who quit have progressively higher levels of physical activity in the years after quitting compared with continuing smokers.
Keywords: Smoking cessation, physical activity, mixed longitudinal model, trajectory analysis, marginal structural model
INTRODUCTION
Smoking and physical inactivity rank among the top 3 modifiable risk factors (along with elevated blood pressure) for chronic disease and premature death.(1) These unhealthy behaviors tend to cluster within person(2) and have been associated with lower education level.(3) Physical activity tends to be lower in smoking adults.(4, 5) Clinicians and policy makers might be interested in knowing how these behaviors cluster within persons over time in order to plan interventions prompting healthy behavior change.(5)
At the population level, both smoking prevalence and physical activity are highest in young adults and tend to decrease with age. Secular trends are also present, with reductions in both smoking prevalence and physical activity in recent years.(6) Additionally, time-varying co-variates associated with both smoking cessation and physical activity, such as marital status, may act as time-dependent confounders and/or mediators.(7, 8) Without appropriate control, factors such as early life PA and marital status may confound relationships between smoking cessation and physical activity over time.(9, 10) Prior studies have not accounted for secular and age trends,(11-14) explored how physical activity trajectory may change with smoking cessation, considered time-dependent confounding-mediating effects, or described how effects vary according to race and sex.
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is ideally suited to explore the association between smoking cessation and changes in physical activity. Using repeated measures of physical activity and cigarette smoking, as well as rich measurements of demographic, social and biological factors collected over 25 years, we estimated the changes in physical activity after smoking cessation, relative to the “counterfactual” – i.e., what would be expected if smoking had continued in that same individual –with adjustment for individual characteristics and secular trends, and tested whether estimates differed by race and sex. We also tested for reverse causality, i.e. if physical activity level before the smoking cessation attempt increased smoking cessation.
METHODS
Study population
We used data collected over 25 years in the Coronary Artery Risk Development in Young Adults (CARDIA) study, a population-based epidemiological study of 5115 adults aged 18 to 30 years at baseline.(15) Participants were recruited in 1985 and 1986 by random selection of telephone numbers from designated census tracts in Birmingham, AL; Chicago, IL; Minneapolis, MN; and by random selection from the membership list of a health care plan in Oakland, CA. The sampling scheme was designed to achieve a balance at each of the 4 sites by race (self-identified “black, not Hispanic” and “white, not Hispanic”), sex, education (high school degree or less, more than high school), and age (18-24 years, 25-30 years). All subjects gave informed consent before entering the study and at each follow-up examination and the approval of institutional review boards was obtained at each site.
Smoking cessation variable
Detailed cigarette smoking behavior was evaluated during each in-person CARDIA examination, at baseline and after 2,5,7,10,15,20 and 25 years, by responses to an interviewer-administered questionnaire.(16) Participants were also asked the number of cigarettes smoked daily at yearly phone follow-up between CARDIA examinations. Current smoking was defined as smoking one cigarette or more per day. Non-daily smokers reporting not smoking one cigarette or more on the day of examination were coded as non-smokers. At baseline, participants were asked the number of years they had smoked in total, the age at which they started smoking regularly (“How old were you when you started smoking cigarettes regularly?”) and years since cessation (“How many years ago did you stop?”), if appropriate. For changes in smoking status, we started the count of the years since cessation, starting or restarting smoking the year following two discordant visits: for example, if a participant reported smoking at year 5, but not at year 6, the count of the years since cessation was started at year 6 and given the value of one. The time-dependent covariate (TDC) capturing total years of smoking was cumulative across smoking episodes. In contrast, the TDC capturing years since smoking cessation was cumulative only within episodes, and was reset to zero when each episode ended; both included exposure ascertained retrospectively before baseline when appropriate.
Exercise variables
Physical activity was assessed by an interviewer-administered questionnaire designed for CARDIA at each CARDIA examination (baseline, year 2,5,7,10,15,20 and 25).(6, 17) The questionnaire asked about frequency of participation in 13 categories of moderate and vigorous recreational sports, exercise, leisure, and occupational activities over the previous 12 months (Appendix Table 1). Reliability and validity of the instrument has been evaluated previously.(6, 17-19) Briefly, the test-retest reliability of the total physical activity score has been shown to be 0.88 over 13 months.(17, 19) The validity of the questionnaire has been assessed through comparison with measurements of aerobic fitness, biologic variables such as blood pressure and HDL cholesterol,(19, 20) and BMI.(18-21) Physical activity scores were calculated in exercise units based on frequency and intensity of each activity. We hypothesized that the association between physical activity and smoking status might differ for occupational-related physical activities and leisure-time physical activity, so we computed a physical activity score excluding the exercise units from “Vigorous job activities (lifting, carrying, digging)” (Appendix Table 1) and used this score as the main outcome. Physical activity prior to the study start was assessed by 1 question asking participants to grade their physical activity level during high school (“Compared to other people your age and sex, how would you rate your physical activity during high school?”).
Other covariates
Fixed variables throughout the study were race, maximum attained education level, sex, and study center. Maximum educational grade attained for each participant was used as a proxy for socioeconomic status. Time-varying covariates at each CARDIA examination were marital status (married / unmarried), body mass index (BMI), examination year, age, alcohol use (categorical variable: abstinent, moderate and risky) and self-reported depression (depression / no depression). Body mass index (BMI) was calculated at each CARDIA examination as weight in kilograms divided by height in meters squared. Categories of alcohol consumption were based on the sex-specific weekly maximum drinking limits published by the National Institute on Alcohol Abuse and Alcoholism [for men >14 (women >7) standard drinks/week or >4 (>3) drinks/day].(22) Self-reported depression was measured every five years starting at year 5 using the Center for Epidemiologic Studies Depression scale (CES-D).(23) A score of ≥16/60 was used as the cut-off value for both sexes as an indication of the clinically significant depressive symptoms.(24, 25) Presence of a significant medical condition interfering with physical activity was based on two questions that were systematically asked starting at CARDIA examination 7 through 25. Participants were asked to report if they had a medical condition interfering with physical activity and to grade any associated physical impairment on a scale from 1 to 5. A grade of more than 2 for those reporting a medical condition interfering with physical activity was considered significant.
Statistical analysis
We used descriptive statistics to compare participants by smoking status at baseline and whether they had made a quit attempt during follow-up (Table 1). The main outcome variable, physical activity, was log-transformed to correct skewness; exponentiated regression coefficients are therefore interpretable as the percent change in physical activity score expected for each 1-unit change in the independent variable. To account for within-subject correlation of the repeated physical activity scores and model individual departures from the trajectories determined by the fixed effects, we used linear mixed models with correlated random subject-specific intercepts and slopes; we also used a random intercept for study center, to enhance the generalizability of our results.(26) Fully adjusted models included fixed effects for current smoking status (never/past/current), cumulative years of smoking and years since most recent smoking cessation, as well as examination year, age at which smoking was initiated, physical activity level during high school, and years of education, transformed to capture non-linearity. We included non-smokers in the analysis to provide information about the effects of age on physical activity, helping us to disentangle this effect from years of smoking. After assessing interactions, we stratified the analysis by race and sex, fit the model for each of the four race-sex groups. In a final step, we used the regression results to estimate the average increase in physical activity 5, 10, 15 and 20 years after cessation, relative to the expected level of activity if smoking had continued, including both immediate and cumulative effects of the change in smoking status (Appendix Figure 2).
Table 1.
Baseline Characteristics of CARDIA Participants, by smoking behavior during follow-up.
| Variable | Non-smokers at baseline |
Smokers at baseline | P valuel | ||
|---|---|---|---|---|---|
| Never smokers at baseline |
Ex- smokers at baseline |
Documented smoking cessation attempt during follow-up |
No documented smoking cessation attempt throughout follow-upk |
||
| N, (% of total ) a | 2,843 (56) | 678 (14) | 923 (18) | 633 (12) | |
|
Demographics - Age, mean (SD), y |
24.5 (3.7) | 25.9 (3.2) | 25.0 (3.7) | 25.0 (3.6) | <0.01 |
| - Race-sex, No. (%)b Black women |
878 (31) | 128 (19) | 294 (32) | 172 (27) | <0.01 |
| Black men | 614 (22) | 106 (16) | 233 (25) | 192 (30) | |
| White women | 682 (24) | 262 (38) | 203 (22) | 154 (24) | |
| White men | 669 (24) | 182 (27) | 193 (21) | 115 (18) | |
| - College-education at
any examination , No (%) |
1222 (43) | 271 (39) | 162 (18) | 95 (15) | <0.01 |
| - Married, No. (%) | 631 (22) | 200 (29) | 180 (20) | 118 (19) | <0.01 |
|
Physical activity - Total physical activity score, median (IQR)c |
425 (396) | 444 (393) | 411 (355) | 389 (353) | <0.01 |
| - Leisure-time physical
activity score, median (IQR)c |
386 (374) | 401 (356) | 358 (323) | 337 (324) | <0.01 |
| - Ocupation-related
physical activity score, media (IQR)c |
40 (42) | 45 (54) | 52 (72) | 52 (84) | <0.02 |
| - Physical activity level
before high school, mean (SD)d |
3.9 (2) | 3.8 (2) | 3.9 (2) | 3.9 (2) | 0.04 |
|
Smoking variables - Cigarettes per day, median (IQR) |
- | 10 (16) e | 10 (15) | 10 (13) | <0.01 |
| - Years of smoking. median (IQR)f | - | 4.8 (5) | 8.4 (6) | 8.7 (7) | <0.01 |
| - Age at smoking start, mean (SD) | - | 17 (3) | 16 (3) | 16 (3) | 0.9 |
|
Alcohol use
g - Abstainer |
1356 (48) | 229 (34) | 244 (26) | 149 (24) | <0.01 |
| - Light to moderate | 1449 (51) | 420 (63) | 610 (66) | 444 (70) | |
| - Heavy | 30 (1) | 22 (3) | 68 (7) | 37 (6) | |
|
Self-reported significant
medical condition interfering with physical activity at examination 7 h |
330 (14) | 116 (22) | 92 (13) | 60 (13) | <0.01 |
|
Self-reported depression
(CES-D) at examination 5 i |
431 (19) | 154 (20) | 223 (27) | 124 (31) | <0.01 |
|
Anthropomorphic
variables - BMI, mean (SD)j |
24.6 (5.1) | 24.2 (4.5) | 24.4 (4.9) | 24.4 (5.4) | <0.01 |
Abbreviations: BMI: body mass index; CARDIA, Coronary Artery Risk Development in Young Adults study; CES-D: Center for Epidemiologic Studies Depression scale; IQR, interquartile range; SD, standard deviation
36 participants had missing information on smoking status at baseline and are thus excluded from this table.
By design, the CARDIA study sampled self-identified white men, white women, black men and black women in roughly equal numbers for participation in the study.(3)
See Appendix table 1 for detailed description of elements included in the score ( maximum score: 2055).
Self-reported score on a scale from 1-5: 1 corresponding to physically inactive and 5 to very active.(3) 4 missing values for physical activity level before high school.
Self-reported number of cigarettes smoked while still a smoker.
Years of smoking counted as each years of follow-up where participants were coded as current smokers. Years of smoking at baseline were added to the years of smoking at each examination based on the self-report years of smoking at baseline. 13 missing self-reported years of smoking at baseline.
Categories of alcohol consumption were based on the sex-specific weekly maximum drinking limits published by the National Institute on Alcohol Abuse and Alcoholism [for men >14 (women >7) standard drinks/week or >4 (>3) drinks/day].(22)
At examination year 7 through 25, participants were specifically asked to report if they had a medical condition interfering with ability to exercise and to grade how much this condition interfered on a scale from 1 (a little) to 5 (very much). A score of more than 2 was considered significant for the present analyses.
Self-reported depression was measured every five years starting at year 5 examination by using the Center for Epidemiologic Studies Depression scale (CES-D).(23) A score of ≥16 used as the cut-off value for both sexes as an indication of the clinically significant depressive symptoms.(24)
Calculated as weight in kilograms divided by height in meters squared.
Smokers throughout follow-up were smokers who had no documented change in smoking status from study start until the year 25 examination or until they were lost to follow-up.
P values are from a 1-way analysis of variance for age, BMI and age at smoking start; from a χ2 test for race-sex, education, center, income, marital status, significant self-reported medical condition interfering with physical activity and alcohol use category; and from a Kruskal-Wallis nonparametric test for leisure-time physical activity, cigarettes smoked per day and years of smoking. All P values are two sided.
Our linear mixed model could provide biased estimates of the overall effect of smoking cessation on physical activity if smoking status were influenced by earlier physical activity, or if time-dependent confounders of the effect of cessation on physical activity were subsequently influenced by cessation. In these settings, standard regression methods tend to adjust away some part of the overall effect of an exposure mediated through these indirect pathways.(9, 10) Accordingly, we assessed evidence for these problems, then used inverse weighting rather than regression adjustment (Appendix Methods) to address this potential source of bias.(9) We also assessed potential confounding by significant self-reported medical conditions interfering with physical activity, both by adjustment for this variable in the main model and by censoring participants at first report. Finally, we checked sensitivity of the results to two alternate ways of formulating our physical activity variable: 1) using total physical activity score (leisure-time physical activity + occupation-related physical activity), and 2) using occupation-related physical activity only. All analyses were conducted using STATA 12 (StataCorp LP, College Station, TX).
RESULTS
Study population
The 5115 CARDIA participants recruited in 1985-1986 contributed a total of 32,837 clinical examinations and 72,987 phone follow-up examinations over 25 years of follow-up. Of the clinical visits, 310 were excluded for missing data on physical activity and 173 for missing data on smoking, leaving 32,354 examinations (99%) with complete data from 5112 participants (99%). Participants contributed 6.4 clinical examinations and 14.4 phone follow-ups on average. Attrition was more common in tobacco smokers, blacks, men, unmarried and participants with significant depression, higher alcohol use and a lower level of education (Appendix Table 2).
Thirty percent of participants (n=1556) were coded as smokers at baseline (Table 1) and 17% (n=594) at year 25 (Appendix Figure 1 and Appendix Table 2). Smokers tended to stop smoking early in the study with 29% (n=214/731) of past-smokers coded as having stopped within the previous year at the Year 2 examination, compared with 7% at Year 25 (80/1105). Throughout the study, 6% to 13% of smokers were coded as having started or restarted smoking within the previous year. The median number of documented smoking cessation attempts during follow-up was 2 (range 0 to 9).
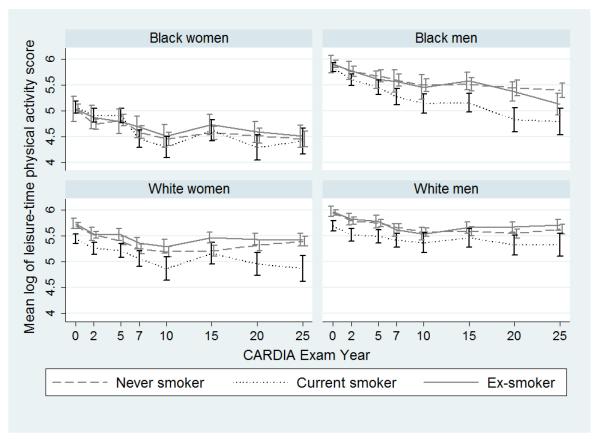
Physical activity varied across participants and declined over time on average in all four race and sex strata (Figure 1). In unadjusted comparisons, physical activity tended to be lowest in current smokers, and higher among men than women.
Figure 1. Unadjusted self-reported leisure-time physical activity score a over 25 years of follow-up according to smoking status b and stratified by sex and race in the Coronary Artery Risk Development in Young Adults (CARDIA) Study.
a Self-reported leisure-time physical activity was assessed at each CARDIA examination (examination year 0, 2 5, 7, 10, 15, 20, 25) (see Appendix table 1 for description of the elements included in the score).
b Participants reporting smoking 1 or more cigarette per day at the CARDIA examination were considered smokers. Ex-smokers were participants not smoking at baseline and reporting having smoked prior to baseline and participants smoking at baseline and not smoking at the considered CARDIA examination.
Smoking cessation and changes in physical activity
We found evidence of important and statistically significant interactions by race-sex (e.g., p=.02 for the interaction with cumulative years of smoking), hence we investigated the subgroups separately. In fully adjusted models, we found a strong association between the cumulative years of smoking and physical activity for all race-sex strata, except for white men where the cumulative years since smoking cessation was significantly associated with physical activity (Table 2). We found no evidence of non-linearity in the years of smoking and years since smoking cessation variables using restricted cubic splines (all P>0.05).
Table 2.
Adjusted percent change in leisure-time physical activity according to smoking status CARDIA participants, 1985-2011a
| Black women | Black men | White women | White men | |||||
|---|---|---|---|---|---|---|---|---|
| Model coefficients (95%CI) b |
P valu e |
Model coefficients (95%CI) b |
P value |
Model coefficients (95%CI) b |
P value |
Model coefficients (95%CI) b |
P value |
|
| Smoking status: - Never smoking (reference) |
- | - | - | - | - | - | - | - |
| - Current smoking | −0.12 (−0.33, 0.07) | 0.2 | .03 (−0.13, 0.19) | 0.7 | −0.06 (−0.18, 0.20) | 0.5 | −0.02 (−0.27, 0.04) | 0.8 |
| - Past smoking | −0.11 (−0.31, 0.09) | 0.3 | .10 (−0.06, 0.24) | 0.2 | .01 (−0.18, 0.21) | 0.9 | −0.04 (−0.10, 0.02) | 0.2 |
| Cumulative exposure: - 10 years of smokingc |
−0.10 (−0.18, −0.01) | 0.01 | −0.21 (−0.29, −0.12) | <0.001 | −0.14 (−0.20, −0.07) | <0.001 | −0.03 (−0.10, 0.03) | 0.3 |
| - 10 years since smoking cessationc |
.04 (−0.8, 0.16) | 0.6 | .01 (−0.12, 0.13) | 0.9 | .04 (−0.03, 0.1) | 0.3 | 0.06 (0, 0.13) | 0.05 |
| Overall coefficient of physical activity 10 years after quitting compared with continuing to smoke |
.15 (0.02, 0.28) | 0.03 | .29 (0.16, 0.4) | <0.001 | .25 (0.16, 0.34) | <0.001 | 0.19 (0.11, 0.28) | <0.001 |
| Adjusted % change (95%CI) b |
Adjusted % change (95%CI) b |
Adjusted % change (95%CI) b |
Adjusted % change (95%CI) b |
|||||
| Overall difference in physical activity 10 years after quitting compared with continuing to smoke d |
16 (2, 33) | 0.03 | 34 (18, 52) | <0.001 | 28 (17, 40) | <0.001 | 21 (11, 32) | <0.001 |
We used linear mixed models with correlated random subject-specific intercepts and slopes and random intercepts for study center. Fully adjusted models included fixed effects for the current smoking status (never/past/current), cumulative exposure to years of smoking and years since smoking cessation, as well as examination year, physical activity level before high-school, age at smoking start and 4-knot restricted cubic splines for education. Estimates are from 4 models according to race and sex categories (black women, black men, white women, white men).
The main outcome variable, leisure-time physical activity score, was natural log-transformed to address skewness, so that exponentiated model coefficients are interpretable as the percent change in physical activity score expected for each smoking statuses or for 5-years of smoking of years since smoking cessation.
Computed by multiplying by 10 the adjusted model coefficients for years of smoking or years since smoking cessation.
After fitting the model for each of these four groups, we estimated the average increase in physical activity 5, 10, 15 and 20 years after cessation, relative to the expected level if smoking had continued, accounting for both immediate and cumulative covariates of smoking exposure i.e. by computing the adjusted model coefficients of past smoking – coefficient of current smoking + [number of years since smoking cessation * (coefficient of years since smoking cessation – coefficient of years of smoking)] (Appendix Figure 2). For example, for a black woman, the expected physical activity level after 10 years since smoking cessation compared to the counterfactual of continuing smoking is: exp (−0.11 - (−0.12) + 10*(0.004 - (−0.01)))-1 = exp (0.15) -1= 0.16; in percent=16%.
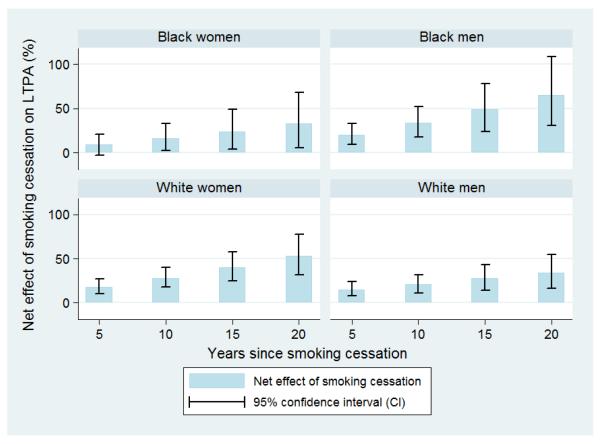
The physical activity trajectory for participants who quit progressively diverged towards higher physical activity from the trajectory that would have been expected had these persons continued smoking (Table 2 and Figure 2). This divergence varied in magnitude by race and sex, but the total divergence (computing using coefficients for both immediate and cumulative smoking behavior covariates, Table 2) remained below the level of significance for a joint test of interaction between sex and race strata (P = 0.21 for interaction by race/sex 10 years after smoking cessation). For example, the net change in physical activity was 28% higher (95%CI:17% to 40%,P<0.001) for white women 10 years after stopping, 16% higher (95%CI:2% to 33%,P<0.03) for black women, 34% (95% CI:18% to 52%,P<0.001) for black men, and 21% (95%CI:11% to 32%,P<0.001) for white men. The net change in physical activity was statistically significant after 10 years in all race-sex strata, and after 5 years in all except for black women.
Figure 2. Difference in self-reported leisure-time physical activity over the years since smoking cessation compared with ongoing smokers.
The main outcome variable, physical activity score, was natural log-transformed to address skewness, so that exponentiated model coefficients are interpretable as the percent change in physical activity. We used linear mixed models with correlated random subject-specific intercepts and slopes and random intercept for study center. Fully adjusted models included fixed effects for the current smoking status (never smoking, current smoking, quit smoking), cumulative exposure to years of smoking and years since smoking cessation, as well as examination year, physical activity level before high-school, age at smoking start and 4-knot restricted cubic splines for education. Estimates are from 4 models according to race and sex categories. We estimated the average increase in physical activity 5, 10, 15 and 20 years after cessation, relative to the expected level if smoking had continued, accounting for both immediate and cumulative effects of the change in smoking status (Appendix Figure 2 and Table 2) (P = 0.38 for interaction by race/sex 10 years after smoking cessation). CI do not cross zero for black women after 5 years; percent change 5 years after smoking cessation: 8% (95% CI: −4, 21%).
Testing causal pathways
We found no evidence of reverse causality, i.e. that physical activity level before the smoking cessation attempt increased smoking cessation (e.g. for black women, the odds ratio (OR) of smoking cessation for lagged values of physical activity was 0.99; 95%CI:0.94 to 1.05, P=0.8). Confounding and mediation analyses suggested that marital status, alcohol use and depression were potential time-dependent confounders and mediators (TDCM) and that BMI was a potential time-dependent mediator (TDM) of the causal pathway from smoking cessation to physical activity (see Appendix Results). Sensitivity analyses including the TDCMs in the main model and using marginal structural models, however, led to qualitatively similar findings but with substantially wider confidence intervals. Inclusion of BMI as a TDM made little difference to results (Table 3). Additional sensitivity analyses including a binary predictor of self-reported significant medical conditions interfering with physical activity in the main model and when censoring 5,747 examinations after which participants reported a medical condition interfering with physical activity (18% of total examination sample) yielded similar results (Appendix Results and Table 3).
Table 3.
Sensitivity of the adjusted percent change in leisure-time physical activity (LTPA) after smoking cessation to varying modeling strategies in CARDIA participants, 1985-2011.
| Main analysis a |
Inclusion of variable on medical condition interfering with physical activityd |
Censoring after self- report of a medical condition interfering with physical activitye |
Inclusion of all potential TDCMs in the main model f |
Inclusion of BMI in the main model |
Main analysis restricted to smokers at baseline g |
Results from
marginal structural models including potential TDCMs, analyses restricted to smokers at baseline i |
Main analysis using total physical activity instead of LTPA onlyl |
||
|---|---|---|---|---|---|---|---|---|---|
| TDCM: marital status, alcohol use and BMI j |
TDCM: marital status, alcohol use, BMI and depression k |
||||||||
| Overall difference in LTPA 10 years after smoking cessation, compared with continuing to smoke |
Adjusted % change (95% CI) b, c |
Adjusted % change (95% CI) b, c |
Adjusted % change (95% CI) b, c |
Adjusted % change (95% CI) b, c |
Adjusted % change (95% CI) b, c |
Adjusted % change (95% CI) b, h |
Adjusted % change (95% CI) b, h |
Adjusted % change (95% CI) b, h |
Adjusted % change (95% CI) b, c |
| - Black women | 16 (1, 32) | 17 (0, 37) | 27 (7, 52) | 16 (0, 34) | 19 (4, 36) | 19 (−8, 56) | 19 (−8, 56) | 16 (−12, 53) | 12 (−2, 28) |
| - Black men | 32 (16, 50) | 34 (15, 57) | 36 (15, 60) | 36 (17, 57) | 38 (21, 57) | 28 (2, 61) | 27 (1, 60) | 27 (1, 60) | 24 (10, 40) |
| - White women | 28 (17, 40) | 34 (20, 50) | 38 (21, 58) | 34 (21, 48) | 28 (18, 40) | 35 (15, 58) | 33 (14, 55) | 33 (14, 55) | 25 (14, 36) |
| - White men | 21 (11, 32) | 17 (5, 30) | 20 (7, 34) | 23 (12, 36) | 23 (13, 34) | 30 (11, 52) | 33 (11, 53) | 30 (11, 52) | 13 (4, 23) |
Abbreviations: BMI: Body mass index; CI: Confidence interval; LTPA: Leisure-time physical activity; TDCM: Time-dependent confounder and mediator
We used linear mixed models with correlated random subject-specific intercepts and slopes and random intercepts for study center. Fully adjusted models included fixed effects for the current smoking status (never smoking, current smoking, quit smoking), cumulative exposure to years of smoking and years since smoking cessation, as well as examination year, study center, physical activity level before high-school, age at smoking start and 4-knot restricted cubic splines for education. Estimates are from 4 models according to race and sex categories (black women, black men, white women, white men).
The main outcome variable, LTPA score, was natural log-transformed to address skewness, so that exponentiated model coefficients are interpretable as the percent change in LTPA score expected after 10 years since smoking cessation.
After fitting the model for each of these four groups, we estimated the average increase in physical activity 10 years after cessation, relative to the expected level if smoking had continued, accounting for both immediate and cumulative covariates of smoking exposure i.e. by computing the adjusted model coefficients of past smoking – coefficient of current smoking + [number of years since smoking cessation * (coefficient of years since smoking cessation – coefficient of years of smoking)] (Table 2 and Appendix Figure 2).
At examination year 7 through 25, participants were specifically asked to report if they had a medical condition interfering with ability to exercise and to grade how much this condition interfered on a scale from 1 (a little) to 5 (very much). A score of more than 2 was considered significant in the present analyses. Restriction of the dataset to examinations 7 through 25.
3,424 examinations after which participants reported a medical condition interfering with physical activity were censored for this analysis (10% of total examination sample). See footnote d for the description of the variable. Restriction of the dataset to examinations 7 through 25.
Potential TDCM were alcohol use (abstainer, light to moderate, heavy), marital status (married/not married), depression (CES-D depression score ≥16/<16) and log-transformed values of BMI . TDCM were defined a-priori such as for BMI or identified in population-averaged logistic regression models (see Appendix Methods and Appendix Results). Start of analyses at the year 5 examination given that the depression score was only measured at the year 5 visit.
Analyses restricted to smokers at baseline, N=1556.
Given that only current smokers at baseline were included, we modified the formula to estimate the average increase in physical activity 10 years after cessation, relative to the expected level if smoking had continued described in footnote c accordingly: adjusted model coefficients of current smoking (current/quit) + [number of years since smoking cessation * (coefficient of years since smoking cessation – coefficient of years of smoking)]
Marginal structural model including lagged values of TDCM defined a priori (BMI) or in population averaged logistic regression models (see Appendix Methods and Appendix Results). In observational studies with time-varying exposures, standard approaches for adjustment of confounding are biased when there exist time-dependent confounders that are also affected by previous exposure.(9) Marginal structural models are based on deriving inverse-probability-of-treatment weights (IPTWs), which are then used in a pooled logistic regression model to estimate the causal effect of treatment on outcome.(53) Analyses stratified by race and sex, restricted to smokers at baseline (n=1556). Given the use of lagged values of TDCMs to estimate the IPTWs, start of the analyses at the year 2 examination for the main MSMs and at the year 6 examination when also including depression. For the model to estimate the numerator of censoring weight, censoring included lost to follow-up, end of the study at year 25 and passage from quitter to relapse smoking. Covariates included for the numerator of censoring and treatment weight were: fixed variables: study center, education modeled as a 4-knot restricted cubic spline and physical activity level before high-school; time-dependent covariates were: smoking status (current/stop), years of smoking, years since smoking cessation and 4-knot restricted cubic splines for age, age at smoking start and examination year. Covariates included for the denominator of censoring and treatment weight were the covariates included in the numerator of censoring weights and the lagged values of physical activity and BMI modeled as 4-knot restricted cubic splines, alcohol use modeled as an ordinal categorical variable and marital status modeled as a binary variable.
BMI calculated as weight in kilograms divided by height in meters squared and log-transformed to address skewness. Categories of alcohol consumption (abstained, light-moderate, heavy) were based on the sex-specific weekly maximum drinking limits published by the National Institute on Alcohol Abuse and Alcoholism [for men >14 (women >7) standard drinks/week or >4 (>3) drinks/day].(22)
Self-reported depression was measured every five years starting at year 5 examination by using the Center for Epidemiologic Studies Depression scale (CES-D).(23) A score of ≥16 used as the cut-off value for both sexes as an indication of the clinically significant depressive symptoms.(24)
Use of the overall physical activity score (leisure-time physical activity + occupation-related physical activity), see Appendix Table 1 for detailed description of the score.
Sensitivity analyses
The overall score, i.e. leisure-time physical activity + occupation-related physical activity, yielded estimates of the association with smoking cessation that were somewhat attenuated (Table 3). Current smoking and past smoking were strongly associated with occupation-related physical activity for black and white men, but not cumulative years of smoking and years since smoking cessation (Appendix Figure 3 and Appendix Table 2; see Appendix Results for additional reports on the sensitivity analyses).
DISCUSSION
In this large prospective cohort of young adults followed over 25 years, we found that smoking cessation was associated with a progressive divergence towards higher physical activity compared to ongoing smoking. This divergence was primarily due to the decline in physical activity that occurred with ongoing smoking in black women, black men and white women. In white men, the divergence was primarily due to an increase in physical activity over the years since smoking cessation. This effect appeared to be independent of age at cessation, calendar year, and other participant characteristics. We found no evidence of reverse causality or alternate explanations for the putative effect of smoking cessation on physical activity, and our findings were relatively consistent when we used alternate statistical methodology.
Prior evidence that levels of physical activity are inversely related to smoking rates mostly comes from cross sectional studies.(12, 14) Several follow-up studies have suggested that individuals who quit smoking are unlikely to spontaneously increase their levels of physical activity in the short term.(27-29) In the context of randomized controlled trials (RCTs) two studies showed an increase in physical activity in participants who quit smoking at one year follow-up.(30, 31) Our results are limited to the long term changes in physical activity occurring after more than 5 years and no RCT has performed such a long follow-up. The few longitudinal cohort studies on the association between smoking cessation and long term changes in physical activity show inconsistent results.(13, 32-35) One longitudinal case-cohort study in Japanese men followed over 7 years suggested an increase in physical activity after smoking cessation.(33) However, there was no adjustment for socio-economic factors. In an analysis of a large sample of 6840 women followed over 11 years in Australia, McDermott et al. found no statistically significant difference in physical activity between quitters and continuing smokers. Laaksonen et al. found that 128 quitters during follow-up were more likely to have an increase in physical activity compared to 544 continuing smokers in a cohort of 5081 participants followed over 7 years.(36) No previous studies evaluated the effects of smoking cessation over time taking into account the age and secular trends that tend to confound physical activity trajectory analyses.
Similar to prior studies, we found that a change in marital status from unmarried to married was associated with both smoking cessation and a reduction in physical activity level (see Appendix Results),(7, 8) and that smoking cessation was associated with a subsequent increase in BMI and a decrease in alcohol consumption.(8, 37, 38) Other studies have also shown that continuing smokers may develop medical conditions interfering with physical activity at higher rate than quitters,(39) and that changes in health behavior can occur after contracting a medical condition.(40, 41) However, no previous study tested the sensitivity of the overall effect of smoking cessation on physical activity to the inclusion of these TDCM in the multivariate models.
The mechanism that might explain a causal effect of smoking cessation on physical activity is unclear. Our results may hint to the Problem Behavior Theory,(42) which posits that changes in unhealthy behavior may be associated with additional positive health behavior changes. The observed effect of smoking cessation on increased physical activity and the absence of effect of physical activity on subsequent smoking cessation suggest that smoking cessation, but not increase in physical activity, may be the “gateway” for positive behavior change.(42-45) Alternatively, a decline in pulmonary function in continuing smokers may mediate the observed effects. Exercise addiction has been previously described,(46) and smoking cessation, considering the addictive effects of smoking, might be associated with a search to replace smoking by a “safe drug” such as physical activity. Prior studies have also described the potential effect of physical activity on short term “craving” in quitters.(44, 47) Differences in some of the coefficients in our model across the subgroups suggest that the causal pathways could differ by race and sex, but we would caution about over interpretation of these differences. Future analyses especially tailored at analyzing mediation should be performed to further describe the causal pathway from smoking cessation to physical activity.
We did not expect to see a change in the trajectory of occupation-related physical activity according to smoking status and therefore removed this variable from the overall score. We found occupation-related physical activity to be associated with both smoking and past smoking in white men and black men, but not over the years since smoking cessation, suggesting that the causal pathway from smoking cessation to changes in physical activity might differ for occupation-related and leisure-time physical activity (see Appendix Results).
Our study has limitations. Smoking status was self-reported at CARDIA examinations and during phone follow-ups; but misclassification of smoking exposure by self-report, measured by comparisons of serum cotinine levels, has been shown to be uncommon within CARDIA.(48) Similarly, the measure of physical activity was based on self-report; but the CARDIA physical activity questionnaire has been previously validated against biological outcomes.(17) Social desirability bias with health conscious participants that successfully quit reporting more physical activity than continuing smokers cannot be excluded.(49) Similarly, we cannot exclude a potential Hawthorne effect, where study participation has an effect on the exposure and outcome.(50) The level of physical activity was only assessed at the time of examination and not at the time of smoking cessation. Given the varying time interval between the examinations from 1 year to 5 years, inference about effects on physical activity during the first 5 years of smoking cessation should be avoided. Attrition occurred for 33% of participants over the 25 years of follow-up and was more common in tobacco smokers; the reported rate smoking at the year 25 examination of 17% is lower than the reported 19%-21% reported by the CDC in 2011 for the age group 45-55 years old.(51) If smokers who left the study were different than those who stayed in the study in terms of their physical activity trajectories, our results could include some bias. The results of the marginal structural model, which includes estimation of the inverse probability of censoring weights showed qualitatively similar results. As with any observational analysis, unmeasured or inadequately modeled confounding effects could be mixed within our estimates. However, the extensive covariate measurements and large sample in our study permitted more extensive efforts to control confounding than were possible in previous studies.(8, 36) We acknowledge the limitations of the causal inferences due to the observational nature of the data, and suggest careful interpretation of the results.
CONCLUSIONS
Our results suggest that when smokers quit, they also tend to maintain a healthier physical activity level compared to continuing smokers. Unlike previous studies, we did not find that physical activity levels prior to cessation were associated with smoking cessation. Clusters of unhealthy behavior have been described;(2) the current analysis suggests that the entry point towards a long term cluster of healthy behavior might start with smoking cessation. Researchers and policy makers planning an intervention aimed at promoting long term healthy behavior change might use these findings to focus on helping smokers quit. These results may also be helpful to clinicians counseling smokers to quit and for smokers interested in imagining their “future selves”, (52) with consideration that smoking cessation may lead to other healthy changes, such as an increase in leisure-time physical activity.
Supplementary Material
ACKNOWLEDGEMENTS
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201300025C & HHSN268201300026C), Northwestern University (HHSN268201300027C), University of Minnesota (HHSN268201300028C), Kaiser Foundation Research Institute (HHSN268201300029C), and Johns Hopkins University School of Medicine (HHSN268200900041C). CARDIA is also partially supported by the Intramural Research Program of the National Institute on Aging (NIA) and an intra-agency agreement between NIA and NHLBI (AG0005). This manuscript has been reviewed by CARDIA for scientific content. Dr Auer’s research on cardiovascular prevention is supported by a grant from the Swiss National Science Foundation PBLAP3-136774, the Société Académique Vaudoise and the SICPA Foundation.
Footnotes
Conflict of interest statement: All authors report no conflicts of interest.
References
- 1.World Health Organization . Preventing Chronic Diseases: A Vital Investment. World Health Organization; 2005. [Google Scholar]
- 2.Chiolero A, Wietlisbach V, Ruffieux C, Paccaud F, Cornuz J. Clustering of risk behaviors with cigarette consumption: A population-based survey. Prev Med. 2006;42:348–53. doi: 10.1016/j.ypmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 3.Bild DE, Jacobs DR, Jr., Sidney S, et al. Physical activity in young black and white women. The CARDIA Study. Ann Epidemiol. 1993;3:636–44. doi: 10.1016/1047-2797(93)90087-k. [DOI] [PubMed] [Google Scholar]
- 4.Shishehbor MH, Gordon-Larsen P, Kiefe CI, Litaker D. Association of neighborhood socioeconomic status with physical fitness in healthy young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am Heart J. 2008;155:699–705. doi: 10.1016/j.ahj.2007.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carnethon MR, Gidding SS, Nehgme R, et al. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290:3092–100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 6.Anderssen N, Jacobs DR, Jr., Sidney S, et al. Change and secular trends in physical activity patterns in young adults: a seven-year longitudinal follow-up in the Coronary Artery Risk Development in Young Adults Study (CARDIA) Am J Epidemiol. 1996;143:351–62. doi: 10.1093/oxfordjournals.aje.a008749. [DOI] [PubMed] [Google Scholar]
- 7.Mcdermott L, Dobson A, Russell A. Changes in smoking behaviour among young women over life stage transitions. Aust N Z J Public Health. 2004;28:330–5. doi: 10.1111/j.1467-842x.2004.tb00439.x. [DOI] [PubMed] [Google Scholar]
- 8.Mcdermott L, Dobson A, Owen N. Determinants of continuity and change over 10 years in young women’s smoking. Addiction. 2009;104:478–87. doi: 10.1111/j.1360-0443.2008.02452.x. [DOI] [PubMed] [Google Scholar]
- 9.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11:550–60. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Robins JM, Greenland S, Hu F-C. Estimation of the Causal Effect of a Time-Varying Exposure on the Marginal Mean of a Repeated Binary Outcome. Journal of the American Statistical Association. 1999;94:687–700. [Google Scholar]
- 11.Schroder H, Elosua R, Marrugat J. The relationship of physical activity with dietary cancer-protective nutrients and cancer-related biological and lifestyle factors. Eur J Cancer Prev. 2003;12:339–46. doi: 10.1097/00008469-200308000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Helmert U, Herman B, Shea S. Moderate and vigorous leisure-time physical activity and cardiovascular disease risk factors in West Germany, 1984-1991. Int J Epidemiol. 1994;23:285–92. doi: 10.1093/ije/23.2.285. [DOI] [PubMed] [Google Scholar]
- 13.Kaczynski AT, Manske SR, Mannell RC, Grewal K. Smoking and physical activity: a systematic review. Am J Health Behav. 2008;32:93–110. doi: 10.5555/ajhb.2008.32.1.93. [DOI] [PubMed] [Google Scholar]
- 14.Boutelle KN, Murray DM, Jeffery RW, Hennrikus DJ, Lando HA. Associations between exercise and health behaviors in a community sample of working adults. Prev Med. 2000;30:217–24. doi: 10.1006/pmed.1999.0618. [DOI] [PubMed] [Google Scholar]
- 15.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–16. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 16.Wagenknecht LE, Perkins LL, Cutter GR, et al. Cigarette smoking behavior is strongly related to educational status: the CARDIA study. Prev Med. 1990;19:158–69. doi: 10.1016/0091-7435(90)90017-e. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs DR, Hahn LP, Haskell WL, Pirie P, Sidney S. Validity and Reliability of Short Physical Activity History: Cardia and the Minnesota Heart Health Program. Journal of Cardiopulmonary Rehabilitation and Prevention. 1989;9:448–459. doi: 10.1097/00008483-198911000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sidney S, Jacobs DR, Jr., Haskell WL, et al. Comparison of two methods of assessing physical activity in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol. 1991;133:1231–45. doi: 10.1093/oxfordjournals.aje.a115835. [DOI] [PubMed] [Google Scholar]
- 19.Jacobs DR, Jr., Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993;25:81–91. doi: 10.1249/00005768-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Parker ED, Schmitz KH, Jacobs DR, Dengel DR, Schreiner PJ. Physical activity in young adults and incident hypertension over 15 years of follow-up: the CARDIA study. Am J Public Health. 2007;97:703–9. doi: 10.2105/AJPH.2004.055889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hankinson AL, Daviglus ML, Bouchard C, et al. Maintaining a high physical activity level over 20 years and weight gain. JAMA. 2010;304:2603–10. doi: 10.1001/jama.2010.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Institute on Alcohol Abuse and Alcoholism . Helping Patients Who Drink Too Much: A Clinician’s Guide. National Institutes of Health; Rockville, MD: 2005. [Google Scholar]
- 23.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 24.Radloff LS, Locke BZ. The community mental health assessment survey and the CES D Scale. In: Weissman MM, Myers JK, Ross CE, editors. Community surveys of psychiatric disorders. Rutgers University Press; New Brunswick, NJ: 1986. pp. 177–89. [Google Scholar]
- 25.Rahman A, Gibney L, Person SD, et al. Validity of self-reports of reasons for hospitalization by young adults and risk factors for discordance with medical records: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol. 2005;162:491–8. doi: 10.1093/aje/kwi215. [DOI] [PubMed] [Google Scholar]
- 26.Vittinghoff E, Glidden DV, Shiboski SC, Mcculloch CE. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. Springer; 2012. [Google Scholar]
- 27.Allen SS, Brintnell DM, Hatsukami D, Reich B. Energy intake and physical activity during short-term smoking cessation in postmenopausal women. Addict Behav. 2004;29:947–51. doi: 10.1016/j.addbeh.2004.02.041. [DOI] [PubMed] [Google Scholar]
- 28.Hall SM, Mcgee R, Tunstall C, Duffy J, Benowitz N. Changes in food intake and activity after quitting smoking. J Consult Clin Psychol. 1989;57:81–6. doi: 10.1037//0022-006x.57.1.81. [DOI] [PubMed] [Google Scholar]
- 29.Weg M, Klesges R, Eck Clemens L, Meyers A, Pascale R. The relationships between ethnicity, gender, and short-term changes in energy balance following smoking cessation. International Journal of Behavioral Medicine. 2001;8:163–177. [Google Scholar]
- 30.Bize R, Willi C, Chiolero A, et al. Participation in a population-based physical activity programme as an aid for smoking cessation: a randomised trial. Tob Control. 2010;19:488–94. doi: 10.1136/tc.2009.030288. [DOI] [PubMed] [Google Scholar]
- 31.Ussher M, West R, Mcewen A, Taylor A, Steptoe A. Efficacy of exercise counselling as an aid for smoking cessation: a randomized controlled trial. Addiction. 2003;98:523–532. doi: 10.1046/j.1360-0443.2003.00346.x. [DOI] [PubMed] [Google Scholar]
- 32.Perkins KA, Rohay J, Meilahn EN, et al. Diet, alcohol, and physical activity as a function of smoking status in middle-aged women. Health Psychol. 1993;12:410–5. doi: 10.1037//0278-6133.12.5.410. [DOI] [PubMed] [Google Scholar]
- 33.Nagaya T, Yoshida H, Takahashi H, Kawai M. Cigarette smoking weakens exercise habits in healthy men. Nicotine Tob Res. 2007;9:1027–32. doi: 10.1080/14622200701591575. [DOI] [PubMed] [Google Scholar]
- 34.Sneve M, Jorde R. Cross-sectional study on the relationship between body mass index and smoking, and longitudinal changes in body mass index in relation to change in smoking status: the Tromso Study. Scand J Public Health. 2008;36:397–407. doi: 10.1177/1403494807088453. [DOI] [PubMed] [Google Scholar]
- 35.Kawachi I, Troisi RJ, Rotnitzky AG, Coakley EH, Colditz GA. Can physical activity minimize weight gain in women after smoking cessation? Am J Public Health. 1996;86:999–1004. doi: 10.2105/ajph.86.7.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laaksonen M, Luoto R, Helakorpi S, Uutela A. Associations between health-related behaviors: a 7-year follow-up of adults. Prev Med. 2002;34:162–70. doi: 10.1006/pmed.2001.0965. [DOI] [PubMed] [Google Scholar]
- 37.Lycett D, Munafo M, Johnstone E, Murphy M, Aveyard P. Weight Change Over Eight Years in Relation to Alcohol Consumption in a Cohort of Continuing Smokers and Quitters. Nicotine Tob Res. 2011 doi: 10.1093/ntr/ntr092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aubin HJ, Farley A, Lycett D, Lahmek P, Aveyard P. Weight gain in smokers after quitting cigarettes: meta-analysis. BMJ. 2012;345:e4439. doi: 10.1136/bmj.e4439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hozawa A, Houston T, Steffes MW, et al. The association of cigarette smoking with self-reported disease before middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Prev Med. 2006;42:193–9. doi: 10.1016/j.ypmed.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 40.Ramage-Morin PL, Bernier J, Newsom JT, et al. Adopting leisure-time physical activity after diagnosis of a vascular condition. Health Rep. 2012;23:17–29. [PMC free article] [PubMed] [Google Scholar]
- 41.Newsom JT, Huguet N, Mccarthy MJ, et al. Health behavior change following chronic illness in middle and later life. J Gerontol B Psychol Sci Soc Sci. 2012;67:279–88. doi: 10.1093/geronb/gbr103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jessor R. Problem-behavior theory, psychosocial development, and adolescent problem drinking. Br J Addict. 1987;82:331–42. doi: 10.1111/j.1360-0443.1987.tb01490.x. [DOI] [PubMed] [Google Scholar]
- 43.King TK, Marcus BH, Pinto BM, Emmons KM, Abrams DB. Cognitive-behavioral mediators of changing multiple behaviors: smoking and a sedentary lifestyle. Prev Med. 1996;25:684–91. doi: 10.1006/pmed.1996.0107. [DOI] [PubMed] [Google Scholar]
- 44.Ussher MH, Taylor A, Faulkner G. Exercise interventions for smoking cessation. Cochrane Database Syst Rev. 2012;1:CD002295. doi: 10.1002/14651858.CD002295.pub4. [DOI] [PubMed] [Google Scholar]
- 45.Burke V, Milligan RA, Beilin LJ, et al. Clustering of health-related behaviors among 18-year-old Australians. Prev Med. 1997;26:724–33. doi: 10.1006/pmed.1997.0198. [DOI] [PubMed] [Google Scholar]
- 46.Berczik K, Szabo A, Griffiths MD, et al. Exercise addiction: symptoms, diagnosis, epidemiology, and etiology. Subst Use Misuse. 2012;47:403–17. doi: 10.3109/10826084.2011.639120. [DOI] [PubMed] [Google Scholar]
- 47.Haasova M, Warren FC, Ussher M, et al. The acute effects of physical activity on cigarette cravings: Systematic review and meta-analysis with individual participant data (IPD) Addiction. 2012 doi: 10.1111/j.1360-0443.2012.04034.x. n/a-n/a. [DOI] [PubMed] [Google Scholar]
- 48.Wagenknecht LE, Burke GL, Perkins LL, Haley NJ, Friedman GD. Misclassification of smoking status in the CARDIA study: a comparison of self-report with serum cotinine levels. Am J Public Health. 1992;82:33–6. doi: 10.2105/ajph.82.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adams SA, Matthews CE, Ebbeling CB, et al. The effect of social desirability and social approval on self-reports of physical activity. Am J Epidemiol. 2005;161:389–98. doi: 10.1093/aje/kwi054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mccambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67:267–77. doi: 10.1016/j.jclinepi.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adult participation in recommended levels of physical activity--United States, 2001 and 2003. MMWR Morb Mortal Wkly Rep. 2005;54:1208–12. [PubMed] [Google Scholar]
- 52.Sorrentino RM, Higgins ET. Handbook of Motivation and Cognition: Foundations of Social Behavior. Guilford Press; 1990. [Google Scholar]
- 53.Fewell Z, Hernán MA, Wolfe F, et al. Controlling for time-dependent confounding using marginal structural models. Stata Journal. 2004;4:402–420. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.