Abstract
Patient adherence (the degree to which patients follow their therapeutic regimen as prescribed within a set period of time) and persistence (the time to treatment discontinuation, with a permissible gap) with drug therapy are essential components of HIV/AIDS treatment. Select community pharmacies offer specialized services for HIV/AIDS patients to help combat some of the barriers to adherence and persistence. We assessed adherence and persistence with antiretroviral therapy (ART) for patients using HIV-specialized pharmacies in nine cities from seven states compared to traditional community pharmacy users over a 1-year period. Data were limited to one pharmacy chain. Propensity scoring was used to obtain 1:1 matches for “Specialized” and “Traditional” pharmacy users based on age, gender, number of prescription-inferred chronic conditions (obtained by mapping a patient's prescriptions to the Medi-Span Drug Indications Database), and presence of prescription anxiety and/or depression medication, resulting in 7064 patients in each group. Proportion of days covered (PDC) was used to measure adherence. Specialized pharmacy users had a significantly greater mean (74.1% versus 69.2%, p<0.0001) and median (90.3% versus 86.3%, p<0.0001) PDC. A greater percentage of patients in the Specialized group were able to obtain a PDC of 95% or better (39.3% versus 35.5%). Patients in the Specialized group were significantly more persistent (p=0.0117). Community pharmacies specialized in HIV services may be effective avenues for helping patients achieve greater adherence and persistence with ART. Given the value of specialized community pharmacies, payers should consider implementing policies to encourage the use of such pharmacies for filling ART.
Introduction
Patient adherence (the degree to which patients follow their therapeutic regimen as prescribed within a set period of time) and persistence (the time to treatment discontinuation, with a permissible gap1) with drug therapy are essential components of HIV/AIDS treatment. Given the difficulty in directly observing patients ingesting their medication and the cost associated with obtaining a blood sample from patients to check drug levels, several proxy measures have been used to measure adherence and persistence, including pill count, electronic monitoring, self-report, and prescription refills. Each of these indirect measures has its benefits and its weaknesses. Patient self-reports are subject to recall bias; the other measures are not. However, all of these measures are limited in that they cannot actually determine if the patient ingested the medication. Electronic monitoring is a more accurate measure, but it is one of the most expensive indirect measures. Prescription refill records can be obtained without much difficulty, but are limited by the pharmacy system.2,3 However, the use of prescription claims data can be a suitable method for assessing adherence to antiretroviral therapy (ART).3,4
Patients with suboptimal antiretroviral adherence and persistence run the risk of treatment failure and subsequent development of resistance mutations. Early studies indicated 95% adherence was needed for viral suppression.5 However, as regimens have improved over the years, viral suppression has been observed with lower levels of adherence.6–8 Other studies have shown the importance of adherence, correlating adherence levels and viral suppression.9–11 While persistence has not been studied as extensively, research shows treatment interruption and discontinuation are associated with drug resistance and increased mortality.3
Despite the recognized importance of adequate ART adherence, an estimated 45% of patients fail to achieve suitable levels.12 Knobel et al.13 found that only 33% of patients in their study were able to maintain an adherence level of at least 90% and in a study by Shuter et al.,7 patients experienced an average adherence rate of 73%. Several factors can impact a patient's adherence and persistence with antiretroviral therapy, including relationship with/trust in provider,14 lack of social support,14,15 regimen complexity,16,17 and misunderstanding of the disease and drug treatment.18
To address these barriers to adherence, select pharmacies have implemented specialized services for HIV patients within traditional community pharmacies. These pharmacies have employed specially trained and educated HIV pharmacists, offering increased patient education, as well as other services which enhance HIV care, such as advanced inventory control and synchronization of refills. By focusing on the specific needs of individuals living with HIV/AIDS, these pharmacies are designed to address several of the factors associated with nonadherence to ART and therefore, may help patients achieve greater adherence and persistence to their ART. A previous study by Hirsch et al.19 found that patients utilizing HIV/AIDS medication therapy management (MTM) programs in place at 10 community pharmacies in California had increased adherence over those using nonspecialized pharmacies. Cocohoba et al.20 also demonstrated increased adherence with use of pharmacies offering specialized HIV/AIDS services in California. To our knowledge, no one has assessed the impact of such services on medication persistence.
The objective of this study is to expand upon previous research, assessing adherence to ART, as well as persistence for patients utilizing HIV-specialized pharmacies in nine cities from seven states compared to traditional community pharmacies.
Methods
Deidentified pharmacy claims were obtained from a large national (operating in all 50 states) pharmacy chain for the period of September 1, 2010 through August 31, 2011. The analysis was limited to patients who were aged 18 years and older and that filled at least one prescription for an antiretroviral medication (listed in Table 1) during the study period. Patients were also required to have filled a minimum of 30 days supply of antiretroviral medication at the pharmacy chain, in order to exclude patients who had utilized the pharmacy for a short-term or one-time fill. Treatment-naïve and established patients were included in the analysis. Patients were then stratified by type of pharmacy they utilized; patients who exclusively used HIV-specialized pharmacies were included in the “Specialized” group and patients exclusively using traditional community pharmacies without HIV specialization were placed in the “Traditional” group. Patients using both pharmacy types were excluded from the analysis.
Table 1.
Included Antiretroviral Medications
| Nucleoside reverse transcriptase inhibitors (NRTIs) | ||
| Abacavir | Emtricitabine | Lamivudine |
| Zidovudine | Didanosine | Stavudine |
| Tenofovir | ||
| Non-nucleoside reverse transcriptase inhibitors (NNRTIs) | ||
| Etravirine | Rilpivirine | Efavirenz |
| Delavirdine | Nevirapine | |
| Protease inhibitors (PIs) | ||
| Tipranavir | Nelfinavir | Fosamprenavir |
| Indinavir | Ritonavir | Atazanavir |
| Saquinavir | Amprenavir | Darunavir |
| Integrase Inhibitors | Entry Inhibitors | |
| Raltegravir | Maraviroc | Enfuvirtide |
| Combination tablets: | ||
| Abacavir/lamivudine (Epzicom, Viiv Healthcare, Research Triangle Park, NC) | Lopinavir/ritonavir (Kaletra, Abbott Laboratories, Abbott Park, IL) | |
| Abacavir/lamivudine/zidovudine (Trizivir, Viiv Healthcare, Research Triangle Park, NC) | Emtricitabine/tenofovir (Truvada, Gilead, Foster City, CA) | |
| Efavirenz/emtricitabine/tenofovir (Atripla, Gilead, Foster City, CA) | Lamivudine/zidovudine (Combivir, GlaxoSmithKline, Research Triangle Park, NC) | |
| Rilpivirine/tenofovir/emtricitabine (Complera, Gilead, Foster City, CA) | ||
The pharmacy chain included in this study offers enhanced services for HIV patients at hundreds of their traditional retail/community pharmacies in areas with an increased number of HIV patients, herein referred to as “HIV-specialized pharmacies.” These services are tailored according to patient needs and include: medication review, adherence assessment, refill synchronization, and availability of HIV/AIDS medications at all times. Additionally, these pharmacies were staffed with pharmacists specially trained in HIV care. Pharmacist training consisted of an initial 23.5 h of HIV specific continuing education (CE) on topics including the impact of HIV/AIDS stigma on patient care, impact of HIV/AIDS on minority populations, and cultural competency, with an additional 11 hours of CE completed annually. The analysis was limited to HIV-specialized pharmacies with the above described enhanced HIV services in place for at least 1 year. Pharmacies meeting this criterion were from the following geographical areas: Houston, Tampa, Chicago, Miami, Atlanta, St. Louis, Indianapolis, Boston, and Orlando. All nonspecialized community pharmacies located within the same districts and open at least 1 year were selected as controls.
Propensity scoring was used to obtain 1:1 patient matches for Specialized and Traditional pharmacy users, using a “greedy” 5→1 matching algorithm.21,22 This algorithm first matched Specialized patients to Traditional patients on 5 digits of the propensity score. This was repeated for those that did not match using 4 digits of the propensity score, continued down to a 1-digit match. Propensity scores were obtained by fitting the following covariates into a logistic regression model: age, gender, number of prescription-inferred chronic conditions (obtained by mapping a patient's filled prescriptions to the Medi-Span Drug Indications Database), and presence of prescription anxiety and/or depression medication.
Measures
Medication adherence was measured via a modified proportion of days covered (PDC) calculation, as determined by prescription refill data. Although various methods to calculate medication adherence using pharmacy refill data have been cited in the literature,4 we chose to use the PDC because this is the measure that is recommended by the Pharmacy Quality Alliance.23 Several studies have demonstrated a correlation between prescription refills and virologic outcomes for HIV patients.24–26 PDC was calculated as the total number of days a patient was in possession of an adequate regimen divided by the number of days between the patient's first fill date and last fill date plus the days supply of the last fill, where an adequate regimen consisted of three or more antiretroviral medications, including either a protease inhibitor, non-nucleoside reverse transcriptase inhibitor, raltegravir, enfuvirtide, or maraviroc. If a patient had overlapping fills for the same drug (due to early refilling), the prescription start date was adjusted to be the day after the previous fill had ended. Combination tablets were counted as their respective number of medications. This definition of a highly active antiretroviral regimen was derived from a definition used in large observational studies of the natural and treated history of HIV in men and women in the United States.27,28
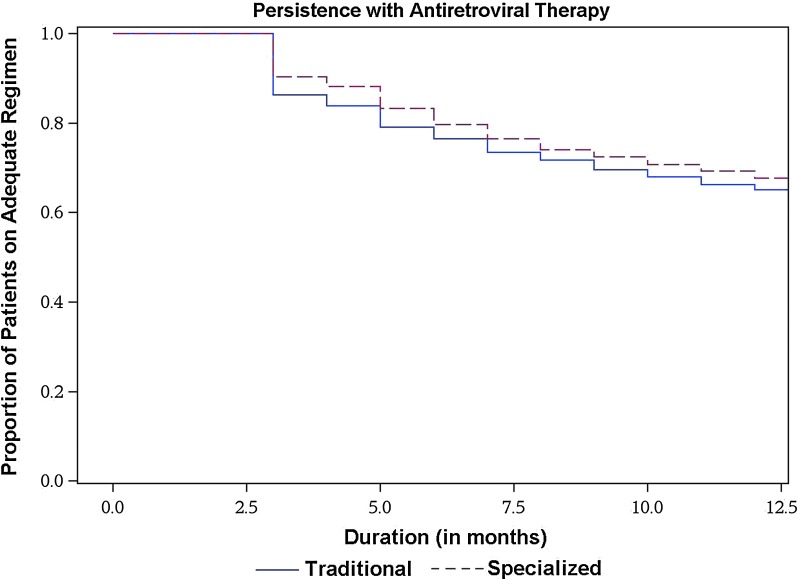
Persistence was measured as the number of days from when a patient was in possession of an adequate regimen to discontinuation of the adequate regimen.1 Patients were considered to have discontinued the adequate regimen if a gap in therapy of more than 30 days occurred. Patients were excluded from the persistence analysis if they were in possession of an adequate regimen for 30 days or less or if they had less than 30 observation days. Results are presented as Kaplan-Meier estimates curves at 30-day intervals. p Value was computed using log-rank test.
Statistical analysis
Student's t and χ2 tests were used to assess differences between groups. A p value of<0.05 was deemed significant. All statistical analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC).
Results
A total of 95 “Specialized” pharmacies and 1462 “Traditional” pharmacies were included in the analysis. Propensity matching resulted in 7064 patients in each group, of which 6978 matches were made at the 5-digit level, 81 at the 2-digit level, and 5 at the 1-digit level. Population characteristics for each group can be found in Table 2. Both groups were predominantly male (73.1%) with an average age of 44.4 years in the Traditional group and 44.9 years in the Specialized group.
Table 2.
Propensity Matched Population Characteristics
| Traditional (n=7064) | Specialized (n=7064) | p Value | |
|---|---|---|---|
| Average age (SD) | 44.4 (11.2) | 44.9 (11.0) | 0.0095 |
| Male, % | 73.1 | 73.1 | 0.9849 |
| Average no. of chronic diseases (SD) | 2.1 (2.2) | 2.1 (2.2) | 0.8748 |
| Presence of anxiety/depression medication | 29.6% | 29.4% | 0.7398 |
SD, standard deviation.
Patients in the Specialized group had a median PDC of 90.3% (interquartile range [IQR]=60.6–98.7) compared to 86.3% (IQR=47.9–98.1) in the Traditional group (p<0.0001). Mean PDC was also higher for the Specialized group (74.1% [standard deviation {SD}=33.0] versus 69.2% [SD=35.6], p<0.0001). Results by PDC range can be seen in Table 3; a greater percentage of patients in the Specialized group were able to obtain a 95% or better PDC (39.3% versus 35.5%). Furthermore, fewer patients in the Specialized group had an average PDC of less than 50% (20.4% versus 25.8%).
Table 3.
Percentage of Patients by Proportion of Days Covered Range
| Traditional | Specialized | |||
|---|---|---|---|---|
| PDC range | n | % | n | % |
| < 50% | 1826 | 25.8 | 1444 | 20.4 |
| 50–79% | 1234 | 17.5 | 1208 | 17.1 |
| 80–84% | 586 | 8.3 | 623 | 8.8 |
| 85–89% | 383 | 5.4 | 392 | 5.5 |
| 90–94% | 530 | 7.5 | 621 | 8.8 |
| ≥ 95% | 2505 | 35.5 | 2,776 | 39.3 |
PDC, proportion of days covered.
Figure 1 shows the Kaplan-Meier survival estimates for persistence. Patients in the Specialized group were significantly more persistent (p=0.0117). At the end of the study period 1448 patients in the Specialized group were remaining on an adequate regimen compared to 1402 patients in the Traditional group.
FIG. 1.
Kaplan-Meier survival estimates showing patient persistence with adequate antiretroviral regimen. Patients in the Specialized group were significantly more persistent (p=0.0117, log-rank test).
Discussion
Helping a patient achieve greater adherence to their antiretroviral medication and remain on antiretroviral regimens longer, can make a significant impact on their health. Maintaining optimal persistence and adherence to the current regimen delays the development of HIV-related conditions, development of resistance mutations, and limits the number and the complexity of future ART regimens that a patient is prescribed. In our study, HIV-specialized pharmacies had a greater proportion of persistent patients and a greater proportion of patients with a PDC of 95% or greater. While our study cannot definitively determine whether the HIV specific services offered at these pharmacies were the driving force behind these outcomes, it suggests they have potential to play an important role in supporting optimal HIV adherence and persistence.
There are many challenges to determining the impact that HIV-focused pharmacies have on ART adherence and persistence. As with most adherence interventions, HIV-focused community pharmacies have multiple components that are tailored by a pharmacist or staff member to meet the patient's specific needs. Unique contributions that might play a more significant role in HIV-focused pharmacies' success in promoting patient adherence and persistence to ART regimens include fostering trusted relationships, improving ART health literacy via HIV pharmacist expertise, and collaborative communication with physicians and patients to improve treatment regimens. Several of these factors are included in the patient-centered pharmacy services model theorized by Kibicho and Owczarzak29: recognize the patient's individual circumstances, tailor services according to the patient's needs, enable the patient to take charge, team up with other providers, and maintain the patient-pharmacist relationship.
Community pharmacies focused on HIV strive to deliver care that goes beyond traditional pharmaceutical care.29,30 Pharmacists work to diminish the stigma surrounding the fulfillment of ART and to develop a trusting relationship with patients. Provider trust is important for effective management of chronic illness.31–34 If a patient has little faith in their provider they are likely to not follow recommendations,35,36 including taking their medication as prescribed.31,33 Gallup has found pharmacists to be highly trusted providers.37 Often times, patients see their pharmacist more often than their physician.38,39 Pharmacists at the specialized pharmacies provide personalized care to and form personal relationships with their patients.29,30 Therefore, we speculate patients may be more willing to discuss issues with their treatment and to accept and respond to pharmacist recommendations. This could be one mechanism by which HIV-focused pharmacies help patients take their medication as prescribed.
HIV pharmacists may help patients get a better understanding of the disease and drug regimen.30 The ability for a patient to comprehend health information is important. Low health literacy has been linked to negative outcomes, including decreased medication adherence.40 Waite et al.41 examined the relationship between literacy and medication adherence to ART, finding HIV patients with a “low” literacy level were three times more likely to have missed a dose in the past 4 days. A study by Tarn et al.42 indicated that physicians do not always properly educate patients on new drug regimens. HIV-trained pharmacists may therefore be able to complement and reinforce physicians' education of their patients, improving patient understanding and ultimately enhancing adherence to and persistence with medication regimens.
As noted earlier, Hirsch et al.19 and Cocohoba et al.20 found that patients in California receiving MTM and utilizing a HIV-specialized pharmacy, respectively, had higher rates of adherence to ART. Our study further demonstrates the ability of such pharmacies to help patients achieve greater levels of adherence. Similar results from seven states imply the generalizability of these results.
Considering community pharmacies with specialized HIV services have been found to impact medication adherence and persistence, it would be of value to determine which particular HIV enhanced services have the greatest impact on adherence and persistence. This would allow a smaller independent pharmacy, which may not be capable of implementing the entire array of enhanced services, to focus on one or two services that could help its patients achieve greater adherence and persistence to their regimens. Additional studies should also assess the impact HIV-specialized pharmacies have on clinical outcomes and medical cost savings.
The findings from this study should be interpreted with caution, as there are several limitations. First, data are limited to prescription claims from one pharmacy chain. If a patient filled prescriptions at another pharmacy, we had no access to those prescription claims, resulting in possible underestimates of adherence and persistence. Given the enhanced services provided by HIV-specialized pharmacies, their users may be more loyal and hence more likely to use (and remain with) the pharmacy chain included in this study. To the contrary, traditional pharmacy users may be more likely to use multiple pharmacy chains that would lead to an underestimation of adherence and persistence in the traditional group. The measures used in the analyses are proxies for the actual rate at which patients took their medication; we were not able to determine if the patient actually ingested the medication. There are several patient-level factors that may impact adherence and persistence that we were not able to control for in this study, such as income, education, race, and history of intravenous drug use. Furthermore, patients who were told by their physician to discontinue medication would have been misclassified as nonadherent/nonpersistent. This study did not determine whether a patient was new to ART. Patients who are new to therapy may have different adherence and persistence patterns. This study employed a strict definition for “adequate” regimen. Therefore, patients who were adherent to a regimen of fewer than three medications, would be classified as nonadherent in this study, as was the case with at least 1014 patients in the Traditional group and 767 patients in the Specialized group. Additionally, we used a gap of 30 days or more for our measure of persistence. This gap may be too liberal since treatment failure may occur at shorter intervals. Finally, there may be selection bias since patients who choose to use specialized HIV pharmacies may have different health behaviors when compared to users of traditional pharmacies.
Community pharmacies specialized in HIV services may be effective avenues for helping patients achieve greater adherence to and persistence with ART. Given the value of specialized community pharmacies, payers should consider implementing policies to encourage the use of such pharmacies for filling ART in preference to generalized community pharmacy or mail order. Recognizing the additional services provided and value added to these patients, policymakers should consider providing additional reimbursement for these services. HIV-specialized pharmacies can serve as a model for other disease states, potentially helping patients achieve better adherence.
Acknowledgment
This study was self-funded by Walgreen Co.
Author Disclosure Statement
P. Murphy, A. Tang, G. Pietrandoni, and J. Hou are employees of Walgreen Co., the funder of this study. Walgreen Co. provides services as described in this article. Drs. Cocohoba and Guglielmo report no relationship or financial interest with any entity that would pose a conflict of interest.
References
- 1.Cramer JA. Roy A. Burrell A, et al. Medication compliance and persistence: Terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- 2.Osterberg L. Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 3.Bae JW. Guyer W. Grimm K. Altice FL. Medication persistence in the treatment of HIV infection: A review of the literature and implications for future clinical care and research. AIDS. 2011;25:279–290. doi: 10.1097/QAD.0b013e328340feb0. [DOI] [PubMed] [Google Scholar]
- 4.McMahon JH. Jordan MR. Kelley K, et al. Pharmacy adherence measures to assess adherence to antiretroviral therapy: Review of the literature and implications for treatment monitoring. Clin Infect Dis. 2011;52:493–506. doi: 10.1093/cid/ciq167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paterson DL. Swindells S. Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 6.Saberi P. Caswell N. Amodio-Groton M. Alpert P. Pharmacy-refill measure of adherence to efavirenz can predict maintenance of HIV viral suppression. AIDS Care. 2008;20:741–745. doi: 10.1080/09540120701694006. [DOI] [PubMed] [Google Scholar]
- 7.Shuter J. Forgiveness of non-adherence to HIV-1 antiretroviral therapy. J Antimicrob Chemother. 2008;61:769–773. doi: 10.1093/jac/dkn020. [DOI] [PubMed] [Google Scholar]
- 8.Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43:939–941. doi: 10.1086/507526. [DOI] [PubMed] [Google Scholar]
- 9.Sethi AK. Celentano DD. Gange SJ. Moore RD. Gallant JE. Association between adherence to antiretroviral therapy and human immunodeficiency virus drug resistance. Clin Infect Dis. 2003;37:1112–1118. doi: 10.1086/378301. [DOI] [PubMed] [Google Scholar]
- 10.Nachega JB. Hislop M. Dowdy DW. Chaisson RE. Regensberg L. Maartens G. Adherence to nonnucleoside reverse transcriptase inhibitor–based HIV therapy and virologic outcomes. Ann Intern Med. 2007;146:564–573. doi: 10.7326/0003-4819-146-8-200704170-00007. [DOI] [PubMed] [Google Scholar]
- 11.Maggiolo F. Ravasio L. Ripamonti D, et al. Similar adherence rates favor different virologic outcomes for patients treated with nonnucleoside analogues or protease inhibitors. Clin Infect Dis. 2005;40:158–163. doi: 10.1086/426595. [DOI] [PubMed] [Google Scholar]
- 12.Mills EJ. Nachega JB. Buchan I, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: A meta-analysis. JAMA. 2006;296:679–690. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- 13.Knobel H. Urbina O. Gonzalez A, et al. Impact of different patterns of nonadherence on the outcome of highly active antiretroviral therapy in patients with long-term follow-up. HIV Med. 2009;10:364–369. doi: 10.1111/j.1468-1293.2009.00696.x. [DOI] [PubMed] [Google Scholar]
- 14.Mills EJ. Nachega JB. Bangsberg DR, et al. Adherence to HAART: A systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006;3:e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ammassari A. Trotta MP. Murri R, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: Overview of published literature. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S123–127. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan PS. Campsmith ML. Nakamura GV. Begley EB. Schulden J. Nakashima AK. Patient and regimen characteristics associated with self-reported nonadherence to antiretroviral therapy. PLoS One. 2007;2:e552. doi: 10.1371/journal.pone.0000552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Willig JH. Abroms S. Westfall AO, et al. Increased regimen durability in the era of once-daily fixed-dose combination antiretroviral therapy. AIDS. 2008;22:1951–1960. doi: 10.1097/QAD.0b013e32830efd79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oggins J. Notions of HIV and medication among multiethnic people living with HIV. Health Soc Work. 2003;28:53–62. doi: 10.1093/hsw/28.1.53. [DOI] [PubMed] [Google Scholar]
- 19.Hirsch JD. Rosenquist A. Best BM. Miller TA. Gilmer TP. Evaluation of the first year of a pilot program in community pharmacy: HIV/AIDS medication therapy management for Medi-Cal beneficiaries. J Manag Care Pharm. 2009;15:32–41. doi: 10.18553/jmcp.2009.15.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cocohoba J. Murphy P. Pietrandoni G. Guglielmo J. Improved antiretroviral refill adherence in HIV-focused community pharmacies. (in press). [DOI] [PMC free article] [PubMed]
- 21.Parsons L. Reducing Bias in a Propensity Score Matched-Pair Sample Using Greedy Matching Techniques. Paper presented at: SAS Users Group International Conference; Long Beach, CA. 2001. [Google Scholar]
- 22.Rosenbaum P. Ruben D. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 23.Nau DP. Proportion of Days Covered (PDC) as a Preferred Method of Measuring Medication Adherence. www.pqaalliance.org/files/PDCvsMPRfinal.pdf. [Jun 25;2012 ]. www.pqaalliance.org/files/PDCvsMPRfinal.pdf
- 24.Grossberg R. Gross R. Use of pharmacy refill data as a measure of antiretroviral adherence. Curr HIV/AIDS Rep. 2007;4:187–191. doi: 10.1007/s11904-007-0027-4. [DOI] [PubMed] [Google Scholar]
- 25.Bisson GP. Gross R. Bellamy S, et al. Pharmacy refill adherence compared with CD4 count changes for monitoring HIV-infected adults on antiretroviral therapy. PLoS Med. 2008;5:e109. doi: 10.1371/journal.pmed.0050109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grossberg R. Zhang Y. Gross R. A time-to-prescription-refill measure of antiretroviral adherence predicted changes in viral load in HIV. J Clin Epidemiol. 2004;57:1107–1110. doi: 10.1016/j.jclinepi.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 27.Multicenter AIDS Cohort Study. HAART definition. www.statepi.jhsph.edu/macs/manuscript.html. [May 15;2012 ]. www.statepi.jhsph.edu/macs/manuscript.html
- 28.Women's Interagency HIV Study. Definition of Highly Active Antiretroviral Therapy. http://statepiaps.jhsph.edu/wihs/Invest-info/Def-HAART_0609.pdf. [May 15;2012 ]. http://statepiaps.jhsph.edu/wihs/Invest-info/Def-HAART_0609.pdf
- 29.Kibicho J. Owczarzak J. A patient-centered pharmacy services model of HIV patient care in community pharmacy settings: A theoretical and empirical framework. AIDS Patient Care STDs. 2012;26:20–28. doi: 10.1089/apc.2011.0212. [DOI] [PubMed] [Google Scholar]
- 30.Kibicho J. Owczarzak J. Pharmacists' strategies for promoting medication adherence among patients with HIV. J Am Pharm Assoc. 2011;51:746–755. doi: 10.1331/JAPhA.2011.10190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schneider J. Kaplan SH. Greenfield S. Li W. Wilson IB. Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. J Gen Intern Med. 2004;19:1096–1103. doi: 10.1111/j.1525-1497.2004.30418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Safran DG. Taira DA. Rogers WH. Kosinski M. Ware JE. Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47:213–220. [PubMed] [Google Scholar]
- 33.Piette JD. Heisler M. Krein S. Kerr EA. The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005;165:1749–1755. doi: 10.1001/archinte.165.15.1749. [DOI] [PubMed] [Google Scholar]
- 34.Farin E. Gramm L. Schmidt E. The patient-pysician relationship in patients with chronic low back pain as a predictor of outcomes after rehabilitation. J Behav Med. doi: 10.1007/s10865-012-9419-z. (in press). [DOI] [PubMed] [Google Scholar]
- 35.Thom DH. Campbell B. Patient-physician trust: An exploratory study. J Fam Pract. 1997;44:169–176. [PubMed] [Google Scholar]
- 36.Trachtenberg F. Dugan E. Hall MA. How patients' trust relates to their involvement in medical care. J Fam Pract. 2005;54:344–352. [PubMed] [Google Scholar]
- 37.Jones JM. Record 64% Rate Honesty, Ethics of Members of Congress Low. www.gallup.com/poll/151460/record-rate-honesty-ethics-members-congress-low.aspx. [Apr 05;2012 ]. www.gallup.com/poll/151460/record-rate-honesty-ethics-members-congress-low.aspx
- 38.Spears T. Community Pharmacists Play Key Role in Improving Medication Safety. Pharmacy Times. 2010 [Google Scholar]
- 39.Bunting BA. Asheville Project Update: Results Continue to Exceed ADA Goals. North Carolina Pharmacist. 2000 [Google Scholar]
- 40.Committee on Health Literacy: A Prescription to End Confusion. Washington D.C.: Institute on Medicine; 2004. [Google Scholar]
- 41.Waite KR. Paasche-Orlow M. Rintamaki LS. Davis TC. Wolf MS. Literacy, social stigma, and HIV medication adherence. J Gen Intern Med. 2008;23:1367–1372. doi: 10.1007/s11606-008-0662-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tarn DM. Heritage J. Paterniti DA. Hays RD. Kravitz RL. Wenger NS. Physician communication when prescribing new medications. Arch Intern Med. 2006;166:1855–1862. doi: 10.1001/archinte.166.17.1855. [DOI] [PubMed] [Google Scholar]