Abstract
Anticoagulation is essential to hemodialysis, and unfractionated heparin (UFH) is the most commonly used anticoagulant in the United States. However, there is no universally accepted standard for its administration in long-term hemodialysis. Dosage schedules vary and include weight-based protocols and low-dose protocols for those at high risk of bleeding, as well as regional anticoagulation with heparin and heparin-coated dialyzers. Adjustments are based largely on clinical signs of under- and overanticoagulation. Risks of UFH use include bleeding, heparin-induced thrombocytopenia, hypertriglyceridemia, anaphylaxis, and possibly bone mineral disease, hyperkalemia, and catheter-associated sepsis. Alternative anticoagulants include low-molecular-weight heparin, direct thrombin inhibitors, heparinoids, and citrate. Anticoagulant-free hemodialysis and peritoneal dialysis also are potential substitutes. However, some of these alternative treatments are not as available as or are more costly than UFH, are dependent on country and health care system, and present dosing challenges. When properly monitored, UFH is a relatively safe and economical choice for anticoagulation in long-term hemodialysis for most patients.
Keywords: Heparin, hemodialysis, anticoagulation, complications, bleeding
CASE PRESENTATION
A 50-year-old man with a history of diabetes mellitus and end-stage renal disease (ESRD) became hypotensive 15 minutes into his dialysis session. He had been receiving maintenance hemodialysis through a left arteriovenous fistula 3 times a week for the past 5 years without complication. Per the dialysis unit protocol, the nurses had been administering a bolus of 2,000 IU of heparin at the start of every session, followed by a maintenance infusion of 1,000 IU/h. He does not have a history of a bleeding disorder, but takes 81 mg of aspirin daily. His blood pressure was 142/84 mm Hg at the start of the session, but decreased acutely to 74/54 mm Hg in the first 15 minutes of the session. He denied shortness of breath, chest pain, and subjective fevers or chills, but noted some mild abdominal discomfort and lightheadedness. On physical examination, his temperature was 97°F, pulse was 90 beats/min, blood pressure was 74/54 mm Hg, and respiratory rate was 18 breaths/min. Cardiac and respiratory examination findings were unremarkable, but his abdomen was diffusely tender to palpation. The patient’s blood pressure improved to 85/62 mm Hg after a 250-mL bolus of saline solution. However, his abdominal pain worsened, so the hemodialysis treatment was discontinued and he was sent to the emergency department for further evaluation.
Laboratory measurements obtained in the emergency department were significant for a white blood cell count of 18,000 cells/μL, platelet count of 400,000/μL, and hemoglobin level of 9 g/dL.Aweek earlier, his hemoglobin level had been 11 g/dL. An electrocardiogram was normal, and troponin levels were negative. However, a computed tomographic scan of the abdomen showed a perforated colon secondary to ischemic bowel with substantial gastrointestinal (GI) bleeding, for which he underwent an emergent hemicolectomy. His hospital course was complicated by continued bleeding; by the time of discharge 10 days later, he had been transfused a total of 8 units of packed red blood cells and his hemoglobin level had stabilized at 9.5 g/dL. His platelet levels never decreased, and an enzyme-linked immunosorbent assay was negative for heparin-induced antibodies.
The patient underwent anticoagulant-free hemodialysis acutely. After discharge, he was instructed to avoid taking aspirin. Given the recent hospitalization for a major bleeding event, his primary nephrologist was asked to review the patient’s anticoagulation for long-term hemodialysis.
INTRODUCTION
Hemodialysis is a life-saving procedure currently used by more than 1.4 million patients with ESRD worldwide.1 Although hemodialysis first developed in the 1920s, early use was complicated by clotting of the dialysis circuit.2 It was not until the 1940s, with the introduction of heparin to anticoagulate the circuit, that hemodialysis became feasible for a large population.3 Since then, unfractionated heparin (UFH) has continued to be the most commonly used anticoagulant in the United States due to its availability, affordability, and short half-life.4,5
UFH has several potential risks, primarily bleeding. Hemodialysis patients already have an increased tendency to bleed due to the build up of uremic toxins that cause platelet dysfunction.6-10 Paradoxically, they also have an increased risk of clotting, stemming from endothelial damage and perturbations in the metabolism, expression, and activity of certain procoagulant factors.11 In a prospective cohort study of patients with atrial fibrillation, those with estimated glomerular filtration rate <30 mL/min/1.73 m2 had a 39% greater risk of thromboembolism compared with those with estimated glomerular filtration rate ≥60 mL/min/1.73 m2.12 Clinicians may prescribe anticoagulants to prevent such thromboembolic events, but the medications often exacerbate the bleeding risk. Holden et al10 estimated the incidence rate of major bleeding events in hemodialysis patients to be 3.1-6.3 events/100 person-years, depending on the use of warfarin and aspirin. Phelan et al13 calculated an even higher incidence rate of 10.8 major bleeding events per 100 person-years in hemodialysis patients receiving warfarin, which was significantly higher than the rate of 2.1 in non–dialysis-dependent warfarin users. Three large studies of dialysis patients with atrial fibrillation have found a more than doubling of hemorrhagic stroke in users of warfarin, whereas the association with ischemic stroke was inconsistent.9,14,15 With increasing interest in prolonged dialysis regimens such as daily and nocturnal dialysis, the relative minority of patients receiving these are being exposed to more heparin, which may further increase bleeding events and other complications.
Despite the potential risks, little is known about the safety of using UFH for hemodialysis. Furthermore, although guidelines exist for heparin use in other clinical conditions such as pulmonary embolism, there is no American standard for heparin dosage in long-term intermittent hemodialysis.16 This article reviews the use and safety of UFH as anticoagulation for long-term intermittent hemodialysis and briefly discusses its alternatives.
PHARMACOLOGY
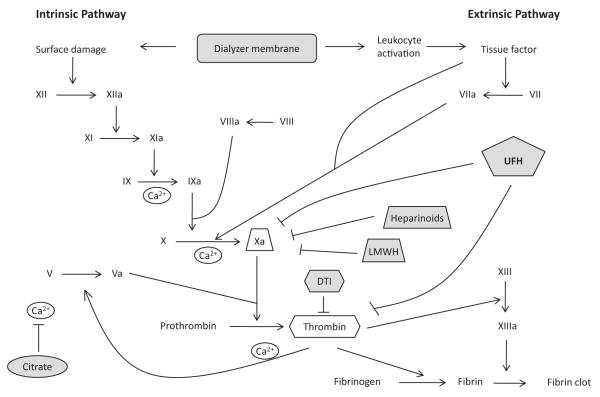
UFH is a sulfate polysaccharide that includes a component that binds and activates antithrombin, inhibiting thrombin and factor Xa and thus stopping the coagulation cascade and promoting anticoagulation (Fig 1).17 UFH activity can be monitored by measuring the activated partial thromboplastin time (aPTT), or the time it takes for a clot to form when treated with an activator and calcium. The half-life of UFH is about 1 hour in patients with kidney failure (vs 30 minutes in patients with normal kidney function), but other facets of hemodialysis, including dialyzer type and dose of erythropoietin, also can affect its activity.4,18-23
Figure 1.
Coagulation cascade. The dialyzer membrane activates the coagulation cascade primarily through the activation of leukocytes, which release tissue factor, triggering the extrinsic pathway. Exposure of the membrane to factor XII may also play a procoagulant role. Unfractionated heparin (UFH) binds to antithrombin, which then inhibits both factor Xa and thrombin, halting the coagulation cascade. Low-molecular-weight heparin (LMWH) primarily acts by inhibiting factor Xa because it generally is too short to link antithrombin and thrombin. Direct thrombin inhibitors (DTIs), as the name implies, stop the cascade by inhibiting thrombin. Heparinoids, similar to LMWH, inhibit factor Xa. Citrate stops coagulation by binding calcium (Ca2+).17
PREPARATION
Although most UFH currently is produced from porcine mucosa, heparin derived from bovine tissue is still available. Interestingly, the source of the drug can influence its effects.24 Bovine heparin causes the same amount of bleeding, but has half the anticoagulant effect of porcine heparin. However, they are sold as equivalent drugs. One study attributed a spike in bleeding complications in Brazil to an increase in the use of bovine versus porcine heparin.24 In the United States, the Food and Drug Administration (FDA) restricts the source of heparin to porcine material out of concern that bovine sources may be contaminated with mad-cow disease.25 However, porcine heparin may carry a greater risk of anaphylaxis (see “Complications”).
Manufacturing standards of all types of heparin came under greater scrutiny in 2008 when a string of adverse reactions in dialysis facilities, including 80 deaths, was linked to contamination of heparin by oversulfated chondroitin sulfate, which was used to lower the cost of production.26,27 Patients reported hypotension, nausea, and shortness of breath within 30 minutes of receiving heparin. The source of the contamination was traced to a single distributor, and multiple batches of heparin were recalled. Since then, the FDA has identified 22 Chinese factories that supplied contaminated heparin and prevented them from importing further products to the United States. Additionally, the FDA now recommends that distributors test every batch of heparin for oversulfated chondroitin sulfate.25
DOSING SCHEDULES
Currently, there is no American standard for heparin dosage in long-term intermittent hemodialysis.16 Instead, dialysis units use a variety of empirically based protocols (Table 1). In general, patients receive a bolus of 2,000-4,000 IU at the start of the dialysis treatment.28 A continuous or hourly intermittent infusion often follows, which provides more consistent levels of anticoagulation (and presumably less risk of bleeding) than a single second bolus.4,30 The hourly rate can range from 500-2,000 IU/h or more, depending on the dose of the initial bolus, and some centers avoid all heparin in the final hour of dialysis to decrease the likelihood of bleeding at the needle sites.4,31 Many dialysis units use weight-based dosing protocols, but interpatient variability in heparin elimination makes these protocols only marginally better at achieving consistent levels of anticoagulation than fixed doses, except at the extremes of weight.31-34
Table 1.
Sample Dosing Schedules for UFH for Anticoagulation During Long-term Hemodialysis
| Loading Dose | Maintenance Infusion | Parameters for Adjustment |
|---|---|---|
| Standard Protocols | ||
| 25 IU/kg |
|
|
| 2,000 IU |
|
|
| Low-Dose Protocols | ||
| 10 IU/kg |
|
|
| 25 IU/kg |
|
|
Note: The authors recommend the first protocol for all patients. Alternative protocols from the literature are listed; there is no evidence favoring one protocol over another. Standard protocols are appropriate for most patients. Low-dose protocols have been suggested for patients with an increased risk of bleeding.16,28,29
Abbreviation: UFH, unfractionated heparin.
Given the variability in heparin activity, some sources advocate dosing heparin to reach a goal aPTT of 1.5 times the predialysis aPTT instead of relying on fixed or weight-based doses.16,31-34 This approach has been shown to improve dialysis adequacy and increase the number of reuses of a single dialyzer. However, this method involves complicated equations and the need for repeated laboratory tests, which leads to high costs, increased technician time to collect and process the samples, and potential exacerbation of anemia through repeated blood draws.30,32,33,35-37
Instead of formal laboratory measurements, most American dialysis units monitor their patients clinically for signs of under- and overanticoagulation. Visual clots in the circuit and increased postpump arterial pressure are signs of insufficient anticoagulation, whereas extended time needed to achieve hemostasis at the end of the dialysis treatment is the primary sign of overanticoagulation.16 However, dialysis-specific factors, such as low blood flow, high hematocrit, high ultrafiltration rate, vascular access stenosis, and poor needle placement, can contribute to both clotting and bleeding. Thus, clinical assessment is useful for identifying coagulation problems during dialysis, but it cannot reliably predict the risk of bleeding after dialysis.
In contrast to the United States, Europe has published guidelines for heparin administration in long-term hemodialysis, as outlined in the European Best Practices Guidelines: UFH at 50 IU/kg as an initial bolus, then 800-1,500 IU per hour of dialysis.38 However, it is unclear whether implementation of this protocol has decreased the complication rate of heparin use in Europe.
In general, in light of the high risk of possibly devastating bleeding complications in patients undergoing hemodialysis, we believe that a responsible clinical approach is to use the smallest dose necessary to complete the hemodialysis session without clotting of the circuit. This may require an ongoing titration process. For patients with a standard dialysis session of about 4 hours, we recommend an initial bolus of 25 IU/kg followed by a continuous infusion of 1,000 IU/h, to be stopped 30-60 minutes before the end of the session (Table 1). If the patient routinely requires more than 15 minutes to clot at the needle puncture sites despite proper needle insertion technique, the maintenance UFH infusion dose should be decreased by 500 IU/h and eventually may be eliminated if the prolonged bleeding after removal of the needle does not improve with reduced maintenance UFH dose. (Of course, other reasons for prolonged bleeding such as outflow stenosis should be ruled out.) Conversely, if the extracorporeal circuit clots during the run and the practitioner has ruled out vascular access and dialyzer equipment as the causes, the rate of UFH infusion should be increased by 500 IU/h.
REGIONAL ANTICOAGULATION WITH HEPARIN, HEPARIN-COATED DIALYZERS, AND LOW-DOSE HEPARIN
Hemodialysis patients with an even higher risk of bleeding, such as postoperative patients or those with a recent history of a bleeding event, should receive reduced doses of heparin. Regional anticoagulation with heparin, special dialyzers, and low-dose heparin protocols have been used in these situations.
In regional anticoagulation with heparin, heparin is added before the blood enters the dialysis circuit, but is reversed by protamine, which is infused prior to the blood returning to the patient.39 This theoretically prevents exposure of the patient to active heparin. However, the practice has fallen out of favor due to the complexity of the protamine infusion and the rebound anticoagulation resulting from latent detachment of the protamine from heparin in the patient’s body.40,41
Manufacturers also have developed special membranes, such as the AN69 ST membrane, that are coated with a substance that binds heparin.42 Technicians must rinse the system with heparinized saline before dialysis, but either no or only a low level of heparin is needed during dialysis.18,42-44 Given this complexity, the increased cost of the special membranes, the fact that patients are still exposed to a small amount of heparin, and clotting rates that can be as high as 39%, these dialyzers generally have not been as popular as use of the simpler low-dose heparin protocols.
The most practical approach is a low-dose heparin protocol, which is easier to use and more effective than regional anticoagulation with heparin and coated membranes.45 However, similar to regular heparin dosing, there is no standard scale.16,46 Generally, patients receive about half the full dose of heparin as a bolus of 10-25 IU/kg, followed by a maintenance infusion of 10 IU/kg/h (Table 1).16,28,29 Our recommendation is to use the same protocol we suggested previously for all patients (a loading dose of 25 IU/kg, followed by a maintenance infusion of 1,000 IU/h to be stopped 30-60 minutes before the end of the session) because it already delivers a low dose of heparin when appropriately titrated, obviating the need for an explicit low-dose regimen.
COMPLICATIONS OF UFH USE
The benefits of UFH—low cost, availability, short half-life, and reversibility—must be weighed against its risks. There are several known complications of UFH use with varying degrees of impact on the hemodialysis population (Box 1).
Box 1. Risks and Benefits of UFH for Anticoagulation During Long-term Hemodialysis.
Risks
Bleeding
Heparin-induced thrombocytopenia
Hypertriglyceridemia
Anaphylaxis
Hyperkalemiaa
Bone mineral diseasea
Catheter-related sepsis
Benefits
Decreased clotting of the dialysis circuit
Low cost
Widely available
Staff familiarity with use
Short half-life
Reversible with protamine
Abbreviation: UFH, unfractionated heparin.
aEstablished in nondialysis populations.
Bleeding
Because heparin is an anticoagulant, its chief complication is bleeding. Although there are many cases of bleeding in patients receiving heparin with long-term hemodialysis, few large-scale studies have proved that heparin increases bleeding risk in this population.
GI Bleeding
Although one of the most common major bleeding events in hemodialysis patients is GI bleeding, no well-conducted study has shown that heparin increases the risk of GI bleeding.
Wasse et al47 studied a cohort of dialysis patients from the US Renal Data System Morbidity and Mortality Studies to identify risk factors for first hospitalization for upper-GI bleeding. Although heparin use was not analyzed separately, the use of any antiplatelet or anticoagulant medication at baseline was not associated with increased risk of upper-GI bleeding. The study is limited by the possibility of confounding by indication; patients prone to bleeding may have been less likely to be prescribed antiplatelet or anticoagulant medications. Still, the null finding was striking given the size of the cohort.
Chacati and Godon48 conducted an autopsy study of 94 patients with ESRD (75 had been receiving hemodialysis) and 258 controls without ESRD. They assumed that every hemodialysis patient received heparin with dialysis. The prevalence of upper-GI bleeding was lower in patients who had survived hemodialysis for more than a month compared with those who had died before or during the first month of hemodialysis (31% vs 58% and 57%, respectively) and was virtually the same as the control group (35%). This suggests that after the first month, hemodialysis may reverse some of the metabolic derangements that predispose patients with ESRD to GI bleeding and may indicate that heparin does not necessarily confer an increased risk of bleeding in this population.
Winkelmayer et al15 found no difference in GI bleeding rates between dialysis patients with new atrial fibrillation who received warfarin compared with similar patients who did not receive this drug.
Recently, Yang et al49 reported that the trend in acute nonvariceal upper-GI bleeding in dialysis patients did not decrease from 1998 to 2007 despite a contemporary decrease in GI bleeding in the nondialysis population. They speculate that increased use of antiplatelet or anticoagulant medications over time, in part driven by the increased use of hemodialysis versus peritoneal dialysis, may have attributed to this effect. However, they did not have medication information in their data set to test this hypothesis. Also, other characteristics of the dialysis population that have changed over time may be driving the trend, including older age and greater prevalence of comorbid conditions.
Cerebral Hemorrhage
Cerebral hemorrhage is a life-threatening complication highly associated with kidney failure. Some speculate that it was the cause of death of musician Wolfgang Amadeus Mozart, who many believe had kidney failure.50 The relative risk of cerebral hemorrhage in incident dialysis patients compared with the general population is 5.4.51 However, the few data available suggest that heparin does not contribute to this risk.
A recent study found the incidence of cerebral hemorrhage in Japanese long-term hemodialysis patients to be 8.7 events/1,000 patient years.52 However, there was no difference in the dose of heparin given to those who had the event and those who did not or between those who died of their hemorrhage and those who survived. Furthermore, 85% of the patients had their event more than 6 hours after the end of their hemodialysis session. The half-life of heparin is about 1 hour, making heparin an unlikely contributor to cerebral hemorrhage in this group. Moreover, there was no difference in the size of hematomas based on the time of the cerebral hemorrhage from the last hemodialysis session, again suggesting that heparin did not have a role in its exacerbation.
A similar cohort study of Japanese long-term dialysis patients found that cerebral hemorrhage occurred on average 35.5 hours after the last hemodialysis session, implying that heparin has a minimal, if any, role in the cause.53
Other Bleeding Events
Data for the incidence of retroperitoneal hemorrhage in hemodialysis patients are limited to case series from the 1970s.54-56 All reported patients were receiving heparin with hemodialysis at the time of their event. Milutinovich et al57 performed the most detailed study, a case series of 6 hemodialysis patients, 4 of whom were also on warfarin therapy. The average serum urea nitrogen level was <80 mg/dL; therefore, uremia likely had a limited role in the bleeding. Also, all the events happened during dialysis, during exposure to heparin. Still, the cases are too few to provide a convincing causal relationship between heparin and the bleeding.
Hemodialysis patients are at risk of ophthalmologic bleeding given their high rate of diabetes and hypertension. A series of 66 hemodialysis patients with proliferative diabetic retinopathy who received heparin with dialysis had no increased bleeding complications with vitrectomy compared with reported rates in similar studies in patients with diabetes not on dialysis therapy.58 Another study cited a patient with a spontaneous hyphema who had recently received 10,000 IU of heparin with dialysis, but a subsequent 66 hemodialysis patients who received the same dose or more heparin did not have such a complication.59 Again, the data are limited, but heparin does not appear to increase ophthalmologic bleeding.
Various other bleeding events have been speculated to be related to heparin given during hemodialysis. Galen et al60 reported a case of a pleural effusion converting to a hemorrhagic effusion after starting hemodialysis with heparin. In a case series of 12 patients with ESRD with hemopericardium from the 1960s, 3 worsened in the immediate postdialysis period; this may be the root of the warning against the use of heparin in patients with uremic pericarditis.61 However, no larger patterns between these types of bleeding events and heparin have been shown since.
Heparin-Induced Thrombocytopenia
One of the most serious side effects of heparin is heparin-induced thrombocytopenia (HIT). We provide a brief overview of the syndrome here; for a more in-depth review, we direct readers to a previous article from Davenport62 in the American Journal of Kidney Diseases “In Practice” series.
Two types of HIT exist.63 In the milder form, type I HIT, heparin binds, activates, and depletes platelets. This typically occurs within the first 4 days of starting heparin therapy and thus is seen in incident hemodialysis patients.64 The thrombocytopenia is mild, with average platelet levels of 100 × 109 per 1 L of blood, and typically resolves with time. No antibodies are formed, and heparin therapy does not need to be stopped.
In the more severe potentially life-threatening form, type II HIT, heparin exposure induces both bleeding and thromboembolic complications.62 Heparin binds to platelets, releasing platelet factor 4 (PF4), which in turn binds heparin (Fig 2). Antibodies then can bind to the heparin-PF4 complex, causing a cascade of more platelet aggregation that leads to severe thrombocytopenia (platelets <50 × 109 per 1 L of blood) and subsequent bleeding complications. The binding of these heparin-induced antibodies to endothelial cells also can cause paradoxical thrombus formation with subsequent limb-threatening ischemia and even fatal pulmonary emboli. Type II HIT usually occurs 5-12 days after heparin exposure, but can happen immediately in the case of re-exposure.66 All forms of heparin, including low-molecular-weight formulations, must be discontinued at once, and the current recommendation is to avoid future heparin exposure.62,67 Additionally, patients should undergo systemic anticoagulation with a nonheparin agent, such as lepirudin, argatroban, or danaparoid, for at least 2-3 months to prevent thrombotic complications.67
Figure 2.
Mechanism of thrombosis in heparin-induced thrombocytopenia. Several mechanisms contribute to thrombosis in heparin-induced thrombocytopenia. Platelet factor 4–heparin–immunoglobulin G (IgG) complexes bind to the Fcg receptor IIA on platelets, leading to platelet aggregation, acceleration of soluble clotting reactions (such as the conversion of factor II [prothrombin] to factor IIa [thrombin]), and activation of neighboring endothelial cells. IgG antibodies bind to heparin–platelet factor 4 complexes on the surface of endothelial cells, leading to additional endothelial-cell activation. Endothelial-cell activation in turn may lead to focal changes in the expression of endothelial-derived procoagulants and anticoagulants. Finally, platelet microparticles, which may be increased in heparin-induced thrombocytopenia, have increased procoagulant activity. Reproduced from Aird and Mark65 with the permission of the Massachusetts Medical Society.
The reported prevalence of HIT in long-term hemodialysis patients ranges from 0.26%-3.9%.68-70 Complications of the syndrome vary in severity and frequency in this population. Clotting of the dialysis circuit is a common, but generally benign, complication.69,71 In one single-center study, vascular access thrombosis occurred in 40% of patients with HIT.72 In contrast, in a national survey of HIT in the hemodialysis population in the United Kingdom, serious complications occurred less frequently: only 8% had a deep vein thrombosis, 4% experienced a pulmonary embolism, and 4% experienced a retroperitoneal hemorrhage.68 Other rare complications include case reports of skin necrosis and pseudo-pulmonary embolism.73-76
The diagnosis of HIT must be made based on both clinical criteria and laboratory testing. Because the differential diagnosis for thrombocytopenia is extensive in chronically ill dialysis patients, the 4T scoring system can be used to calculate the probability that a patient has HIT based on the severity of thrombocytopenia, timing of the decrease in platelets, presence of thrombosis or other acute systemic symptoms, and absence of other causes of thrombocytopenia.77 This score aids in the interpretation of laboratory results, which have varying levels of sensitivity and specificity.78 Although immunoassays are widely available and have sensitivities ranging from 80%-100%, their specificity can be as low as 50%. However, the serotonin release assay, a functional test that detects platelet activation when exposed to both heparin and the patient’s serum, is 95% sensitive and specific but not commonly available. Even a combination of functional and immunoassays can have specificity as low as 80% when clinical events are not taken into account. Thus, it is important that the diagnosis be supported both clinically and by laboratory results because the treatment, systemic anticoagulation, is not without risk.
Recently, several studies have demonstrated that simply having heparin-induced antibodies, even without thrombocytopenia, is still associated with a 2- to 7-fold increase in morbidity and mortality in hemodialysis patients.72,79-83 The prevalence of heparin-induced antibodies is as high as 17% in hemodialysis patients; therefore, this is a potentially major determinant of outcome in this population.
Heparin is necessary for the development of heparin-induced antibodies and HIT, but there has been no documentation of a dose-dependent response. In a Japanese study of incident hemodialysis patients, the dose of heparin for those who developed HIT was not significantly different from patients without HIT.69 This leaves little motivation to decrease the dose of heparin used with hemodialysis without further research.
Hypertriglyceridemia
Heparin is known to cause hypertriglyceridemia, likely through the depletion of lipoprotein lipase (LPL), the enzyme that breaks down triglycerides.84 LPL normally is bound to the vascular endothelium, but a bolus of heparin will release LPL into the free circulation. This transiently increases LPL activity, but ultimately depletes its stores, leading to a build-up of triglycerides. Hypertriglyceridemia contributes to atherosclerosis, a leading cause of death in hemodialysis patients, making this a potentially significant side effect of heparin. However, to date, no study has shown that a decrease in triglyceride levels leads to lower morbidity or mortality in this population.
No study has compared triglyceride levels of long-term hemodialysis patients receiving heparin with those of patients receiving heparin-free treatment. However, a number of crossover studies have compared low-molecular-weight heparin (LMWH) to UFH in long-term hemodialysis and its effect on triglycerides because LMWH is believed to deplete LPL less than UFH.85 Most found that triglyceride levels were decreased by as much as 34% when patients switched to LMWH and rebounded when they reverted to UFH; 2 studies found no difference.6,48,86-91
Anaphylaxis
Anaphylaxis is a risk of any drug, including heparin. Although a recent outbreak of allergic-type reactions to UFH that occurred in 2008 has been traced to contamination of the heparin with oversulfated chondroitin sulfate, there was a case of a 77-year-old woman with anaphylaxis that predated the period of contaminated heparin.26 She experienced vomiting, tachypnea, rales, hypoxia, and thrombocytopenia at the start of the hemodialysis treatment with both UFH and LMWH.92 Changes in the dialysis filter did not resolve the symptoms, but replacing heparin with hirudin as the anticoagulant did. Anaphylaxis to UFH in nondialysis patients also has been linked to allergies to porcine products, with at least one case resolving after replacement with bovine heparin.93,94 Hypo-tension, dyspnea, angioedema, urticaria, tachycardia, and diaphoresis are other signs and symptoms of heparin anaphylaxis that may be mistaken for dialyzer reactions; it is important for clinicians to consider heparin sensitivity in the differential diagnosis of acute hemodialysis-related complications. Close monitoring of patients during their initial hemodialysis session is crucial to catching such life-threatening events early.
Bone Mineral Disease
UFH is known to increase the risk of osteoporosis in pregnancy, but limited studies have been done in the hemodialysis population.95 Binici and Gunes96 found no association between heparin use and reduced bone mineral density in hemodialysis patients with metabolic syndrome. Lai et al97 found that bone mineral density was lower in a cohort of 40 stable hemodialysis patients treated with heparin than in age-matched controls without either kidney disease or heparin use, but this was confounded because bone mineral metabolism is deranged in all patients with kidney failure. The role of heparin in bone mineral disease remains unclear in hemodialysis patients.
Hyperkalemia
Hypoaldosteronism with resultant hyperkalemia is a known side effect of UFH.98 Heparin decreases aldosterone by decreasing both the number and sensitivity of angiotensin II receptors on adrenal zona glomerulosa cells. No studies have examined the difference in potassium levels between long-term hemodialysis patients who do and do not receive heparin, likely because hemodialysis patients commonly are hyperkalemic as a consequence of their kidney failure. Moreover, given the low glomerular filtration rates in this population, the renal effect of aldosterone is at best attenuated. In a crossover study of 11 long-term hemodialysis patients, Hottelart et al92 found that predialysis potassium levels decreased from 5.66 mEq/L to 5.15 mEq/L when patients were given LMWH instead of UFH. This mild decrease could have been due to changes in diet, which were not monitored by the study. Importantly, the dialysate potassium concentration can be changed to address any hyperkalemia that may be associated with heparin, making this a less clinically significant side effect for hemodialysis patients.
Catheter-Related Sepsis
One study has investigated the association between systemic heparin use in hemodialysis patients with catheter-related sepsis.99 In a study published in 2005, heparin was shown to facilitate the creation of biofilm, sheets of bacteria that adhere to the surfaces of devices like catheters, so it potentially can increase the rate of infection.100 In that study, 559 long-term hemodialysis patients using catheters were followed up during a 6-year period. A Cox proportional hazards analysis found that a bolus of UFH midtreatment (but not loading bolus or total UFH dose) was a risk factor for catheter-related sepsis. The authors hypothesize that given the lack of association between infection and total heparin dose, the second bolus may have increased the risk of infection through increased opportunity for contamination of the dialysis circuit, not through promotion of biofilm formation.
ALTERNATIVES TO UFH
Given the limitations of UFH, various alternative anticoagulants have been used in long-term hemodialysis (Table 2). Although they have advantages over UFH, most are prohibitively expensive for wide use, although prices and availability vary by country and health care system.
Table 2.
Alternatives to UFH for Anticoagulation During Long-term Hemodialysis
| Method | Drawbacks | Benefits |
|---|---|---|
| Low-molecular-weight heparin |
|
|
| Direct thrombin inhibitors |
|
|
| Heparinoids |
|
|
| Regional citrate anticoagulation |
|
|
| Anticoagulant-free hemodialysis |
|
|
| Peritoneal dialysis |
|
|
Abbreviations: HIT, heparin-induced thrombocytopenia; UFH, unfractionated heparin.
Note that these agents should be used in conjunction with a systemic nonheparin anticoagulant in the first few months after the diagnosis.
Low-Molecular-Weight Heparin
An alternative to UFH is LMWH. A heparin unit must be at least 18 saccharide units in length or have a molecular weight of 5,400 Da to link antithrombin and thrombin. LMWH, which has an average molecular weight of 4,500-5,000 Da, usually is too short to bind the 2 proteins; instead, LMWH primarily acts by inhibiting factor Xa (Fig 1).17
LMWH is recommended over UFH as anticoagulation in the European Best Practice Guidelines for Hemodialysis.38 Several qualities make it more attractive than UFH. It is easier to dose by weight because it has less nonspecific binding than UFH.101 Its short length also makes it more difficult to form the complex of heparin, PF4, and antibodies that cause HIT.102 As noted, several studies have shown that patients’ lipid profiles improve when switched from UFH to LMWH. Limited data suggest that LMWH also might have fewer bone side effects than UFH.97 LMWH is renally cleared, leading to an increased half-life in patients with ESRD, and protamine cannot reliably reverse its effects; thus, it may theoretically increase bleeding risks. However, a meta-analysis of 11 trials found no increased risk of bleeding compared with UFH when it is used for anticoagulation in long-term hemodialysis.103,104
Various LMWH products are used in Europe, where decreasing prices have made them an economically feasible alternative to UFH.105 They include dalteparin, enoxaparin, nadroparin, reviparin, and tinzaparin. In common practice, doses are adjusted according to clinical parameters, such as clotting of the extracorporeal circuit, and most are effective when given as a single bolus dose at the start of a standard 4-hour session.38,105 Although manufacturers recommend doses on their package insert, most of the LMWHs are effective at preventing clotting of the circuit even at reduced doses, an important consideration for patients who are at greater risks of bleeding.105-116 For example, Davenport105 found that a bolus of 0.5 mg/kg of enoxaparin and 2,500 IU of tinzaparin was sufficient to prevent clots for most patients, although these doses are about half the manufacturer’s recommended dose.
Despite their similarities, different formulations of LMWH have varying pharmacokinetics that affect their administration for nonstandard hemodialysis schedules.105 For example, tinzaparin has a relatively short half-life of 5 hours; thus, most patients need a second bolus when they dialyze for more than 3 hours. However, enoxaparin has a long half-life of up to 24 hours and thus may not be safe for use with daily dialysis unless subsequent doses are decreased to prevent accumulation.
In contrast to Europe, the use of LMWH remains limited in the United States, where it is not approved for use with hemodialysis and remains prohibitively expensive.5,105 The variety of drugs in this class, each with slightly different dosing schedules, also may explain its low rate of use. Despite its low rate of bleeding complications, the lack of a reversal agent further discourages its use among conservative practitioners.
Direct Thrombin Inhibitors
Argatroban and hirudin are direct thrombin inhibitors that have been used successfully to anticoagulate the dialysis circuit in patients with HIT (Fig 1). In a review of 253 long-term hemodialysis patients in whom argatroban was used, only 5 cases of major bleeding were reported.117 However, argatroban should be avoided in patients with liver failure because it is hepatically cleared. There also is no reversal agent for the drug, and it is significantly more expensive than UFH.
Hirudin, which is available in recombinant forms as desirudin, bivalirudin, and lepirudin, is found in leeches; it was the first anticoagulant used for hemodialysis prior to the introduction of heparin.118 A cross-over study of 11 patients showed that hirudin was just as effective as UFH in achieving adequate dialysis (defined by clearance of plasma urea and creatinine) with less platelet accumulation in the filter, but this study did not track long-term bleeding events.119 However, hirudin has a number of complications.118 Monitoring anticoagulation by aPTTs can be inaccurate because the dose-response curve is not linear; at higher concentrations of hirudin, the aPTT underestimates the extent of anticoagulation. It also is highly immunogenic; up to 74% of patients develop antibodies to the drug, which can increase the drug’s half-life. This can easily lead to overanticoagulation, especially in dialysis patients, for whom the typical half-life is already 35 hours because the drug primarily is renally cleared. Similar to argatroban, there is no reversal agent, and it is not as economical as UFH.
Heparinoids
Danaparoid is a heparin derivative, but releases less PF4 than UFH or LMWH and thus has gained use in the HIT population (Fig 1). A review of 122 patients who had a contraindication to heparin use found 14 nonfatal bleeding events and 8 instances of dialysis circuit clotting.120 Danaparoid currently is not available in the United States. Concern that it has proven cross-reactivity with HIT antibodies in a small percentage of patients has slowed its adoption of use in other countries.
Fondaparinux is a synthetic pentasaccharide that binds antithrombin. A small crossover study of 12 patients showed that fondaparinux could sufficiently anticoagulate the dialysis circuit, although less effectively than UFH, as measured by anti-Xa level and a visual scale of clotting of the circuit.121 Half the patients also experienced minor bleeding problems, perhaps because the half-life of the drug is increased in patients with kidney failure. Overall, this relatively new drug is at best appropriate only in patients who may need constant anticoagulation, not just with dialysis.
Regional Citrate Anticoagulation
Citrate is a compound that binds calcium, an essential component of the coagulation cascade (Fig 1). Citrate anticoagulation involves infusing citrate into the circuit before the blood enters the machine and then reversing its effect by adding calcium back to the circuit before it returns to the patient; this theoretically provides regional anticoagulation. Postcircuit calcium replacement also prevents the other complications of acute hypocalcemia, which include tetany, seizures, papilledema, arrhythmia, hypotension, and heart failure. Although used more commonly in continuous modes of hemodialysis, citrate anticoagulation also has been studied in long-term intermittent hemodialysis. A prospective 2-year trial of 59 patients found that it was safe; only 0.2% experienced adverse effects.122 There were no instances of hypernatremia, alkalosis, or hypocalcemia, the most common metabolic complications of the process. However, cost remains a barrier to widespread use. Also, calcium levels must be drawn multiple times during the dialysis session for proper titration of the calcium replacement fluid, which also increases technician labor.
Anticoagulant-Free Dialysis
In cases in which patients have both a contraindication to heparin and an increased risk of bleeding, saline solution is used in place of anticoagulants. Saline boluses of 100-200 mL are injected every 15-60 minutes. Although there is no increased risk of bleeding with saline, the rates of clotting that required a change of the dialyzer range from 3%-10% of sessions, whereas no dialyzers needed to be changed when heparin was used.123-127 The extra volume of saline also increases the ultrafiltration rate, which can lead to hypotension and increased clotting. Finally, the increased technician labor and dialyzer use can double the cost of dialysis, making it a poor choice for long-term outpatient hemodialysis.
Peritoneal Dialysis
Finally, peritoneal dialysis is a sometimes overlooked alternative to heparin-free hemodialysis. The costs are lower, the hypotension that complicates anticoagulant-free hemodialysis generally is avoided, and patients can avoid all heparin by using alternative solutions for their catheter locks. Some patients receive hemodialysis because they have a contraindication to peritoneal dialysis, but in others, it may offer a reasonable treatment alternative.
CONCLUSION
UFH is the most common anticoagulant used for long-term hemodialysis, although the dosage has not been standardized in the United States. Its side effects include bleeding, HIT, hypertriglyceridemia, anaphylaxis, and possibly bone mineral disease, hyperkalemia, and catheter-associated sepsis.
Alternatives include anticoagulation with LMWH, which is easier to dose, but prohibitively expensive in certain countries. Patients with a history of heparin allergy or HIT can receive direct thrombin inhibitors or heparinoids. However, the prolonged half-life and lack of reversal agents for these anticoagulants make them poor choices for patients at high risk of hemorrhage. Both regional citrate anticoagulation and anticoagulant-free hemodialysis are safe alternatives for patients who must avoid systemic anticoagulation; we favor the latter because it is simpler to set up and monitor, although it results in high rates of clotting. Finally, peritoneal dialysis also should be considered because it is less expensive and requires no anticoagulation, although it can be contraindicated for other social and medical reasons.
In general, with appropriate use and monitoring, UFH is a relatively safe and low-cost choice for anticoagulation. Still, these conclusions are drawn from relatively low levels of evidence based on varying dosages of heparin. Large-scale studies (eg, cluster-randomized trials) should be performed on contemporary cohorts to confirm the relative safety of different anticoagulation protocols to identify the therapeutic range at which risks and benefits are optimally balanced.
CASE REVIEW
The patient’s recent life-threatening GI bleed was a relative contraindication to systemic anticoagulation during hemodialysis. His major abdominal surgery made him a poor candidate for peritoneal dialysis, and his dialysis unit was not familiar with regional citrate anticoagulation. Thus, he initially resumed long-term hemodialysis anticoagulant free. However, clotting of the dialyzer required the nurses to change the circuit at least once per session. Because the patient had neither clinical nor laboratory characteristics suggestive of HIT, heparin was not contraindicated. Consequently, 2 weeks after discharge, he was switched to a single loading bolus of 2,000 IU of UFH with no maintenance infusion. He had no further clotting of the dialysis circuit or bleeding complications on this dose.
ACKNOWLEDGEMENTS
We gratefully acknowledge Dr Kristin Sainani’s comments on earlier drafts of this manuscript.
Support: Dr Shen is a 2010 American Kidney Fund-Amgen Clinical Scientist in Nephrology Fellow.
Footnotes
Financial Disclosure: The authors declare that they have no other relevant financial interests.
REFERENCES
- 1.US Renal Data System USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Am J Kidney Dis. 2011;57((1)(suppl 1)):e1–e526. doi: 10.1053/j.ajkd.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 2.Cameron JS. Practical haemodialysis began with cellophane and heparin: the crucial role of William Thalhimer (1884-1961) Nephrol Dial Transplant. 2000;15(7):1086–1091. doi: 10.1093/ndt/15.7.1086. [DOI] [PubMed] [Google Scholar]
- 3.Fellner SK, Purkerson ML. Gordon Murray: heparin, hemodialysis and hubris. Am J Nephrol. 2002;22(2-3):271–277. doi: 10.1159/000063773. [DOI] [PubMed] [Google Scholar]
- 4.Brunet P, Simon N, Opris A, et al. Pharmacodynamics of unfractionated heparin during and after a hemodialysis session. Am J Kidney Dis. 2008;51(5):789–795. doi: 10.1053/j.ajkd.2007.12.040. [DOI] [PubMed] [Google Scholar]
- 5.Cronin RE, Reilly RF. Unfractionated heparin for hemodialysis: still the best option. Semin Dial. 2010;23(5):510–515. doi: 10.1111/j.1525-139X.2010.00770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmitt Y, Schneider H. Low-molecular-weight heparin (LMWH): influence on blood lipids in patients on chronic haemodialysis. Nephrol Dial Transplant. 1993;8(5):438–442. [PubMed] [Google Scholar]
- 7.Ethier J, Bragg-Gresham JL, Piera L, et al. Aspirin prescription and outcomes in hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS) Am J Kidney Dis. 2007;50(4):602–611. doi: 10.1053/j.ajkd.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Saran R, Dykstra DM, Wolfe RA, Gillespie B, Held PJ, Young EW. Association between vascular access failure and the use of specific drugs: the Dialysis Outcomes and Practice Patterns Study (DOPPS) Am J Kidney Dis. 2002;40(6):1255–1263. doi: 10.1053/ajkd.2002.36895. [DOI] [PubMed] [Google Scholar]
- 9.Chan KE, Lazarus JM, Thadhani R, Hakim RM. Anticoagulant and antiplatelet usage associates with mortality among hemodialysis patients. J Am Soc Nephrol. 2009;20(4):872–881. doi: 10.1681/ASN.2008080824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holden RM, Harman GJ, Wang M, Holland D, Day AG. Major bleeding in hemodialysis patients. Clin J Am Soc Nephrol. 2008;3(1):105–110. doi: 10.2215/CJN.01810407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reinecke H, Brand E, Mesters R, et al. Dilemmas in the management of atrial fibrillation in chronic kidney disease. J Am Soc Nephrol. 2009;20(4):705–711. doi: 10.1681/ASN.2007111207. [DOI] [PubMed] [Google Scholar]
- 12.Go AS, Fang MC, Udaltsova N, et al. Impact of proteinuria and glomerular filtration rate on risk of thromboembolism in atrial fibrillation: the Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. Circulation. 2009;119(10):1363–1369. doi: 10.1161/CIRCULATIONAHA.108.816082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Phelan PJ, O’Kelly P, Holian J, et al. Warfarin use in hemodialysis patients: what is the risk? Clin Nephrol. 2011;75(3):204–211. doi: 10.5414/cn106481. [DOI] [PubMed] [Google Scholar]
- 14.Wizemann V, Tong L, Satayathum S, et al. Atrial fibrillation in hemodialysis patients: clinical features and associations with anticoagulant therapy. Kidney Int. 2010;77(12):1098–1106. doi: 10.1038/ki.2009.477. [DOI] [PubMed] [Google Scholar]
- 15.Winkelmayer WC, Liu J, Setoguchi S, Choudhry NK. Effectiveness and safety of warfarin initiation in older hemodialysis patients with incident atrial fibrillation. Clin J Am Soc Nephrol. 2011;6(11):2662–2668. doi: 10.2215/CJN.04550511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blake PG, Daugirdas JT, Ing TS, editors. Handbook of Dialysis. 4th ed Lippincott Williams & Wilkins; Philadelphia, PA: 2007. [Google Scholar]
- 17.Weitz JI. Antiplatelet, anticoagulant, and fibrinolytic drugs. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison’s Principles of Internal Medicine. 18th ed. McGraw-Hill; New York: [Accessed April 16, 2012]. 2012. http://www.accessmedicine.com/content.aspx?aID=9101027. [Google Scholar]
- 18.Chanard J, Lavaud S, Maheut H, Kazes I, Vitry F, Rieu P. The clinical evaluation of low-dose heparin in haemodialysis: a prospective study using the heparin-coated AN69 ST membrane. Nephrol Dial Transplant. 2008;23(6):2003–2009. doi: 10.1093/ndt/gfm888. [DOI] [PubMed] [Google Scholar]
- 19.Lee KB, Kim B, Lee YH, et al. Hemodialysis using heparin-bound Hemophan in patients at risk of bleeding. Nephron Clin Pract. 2004;97(1):c5–c10. doi: 10.1159/000077589. [DOI] [PubMed] [Google Scholar]
- 20.Gunnarsson B, Asaba H, Dawidson S, Wilhelmsson S, Bergstrom J. The effects of three different heparin regimes on heparin concentrations in plasma and fibrin formation in dialyzers. Clin Nephrol. 1981;15(3):135–142. [PubMed] [Google Scholar]
- 21.Norton J, Spiezio R, LaManna L, DeLorme B. Varying heparin requirements in hemodialysis patients receiving erythropoietin. ANNA J. 1992;19(4):367–372. 408. discussion 409. [PubMed] [Google Scholar]
- 22.Veys N, Vanholder R, De Cuyper K, Ringoir S. Influence of erythropoietin on dialyzer reuse, heparin need, and urea kinetics in maintenance hemodialysis patients. Am J Kidney Dis. 1994;23(1):52–59. doi: 10.1016/s0272-6386(12)80812-2. [DOI] [PubMed] [Google Scholar]
- 23.Spinowitz BS, Arslanian J, Charytan C, Golden RA, Rascoff J, Galler M. Impact of epoetin beta on dialyzer clearance and heparin requirements. Am J Kidney Dis. 1991;18(6):668–673. doi: 10.1016/s0272-6386(12)80607-x. [DOI] [PubMed] [Google Scholar]
- 24.Aquino RS, Pereira MS, Vairo BC, et al. Heparins from porcine and bovine intestinal mucosa: are they similar drugs? Thromb Haemost. 2010;103(5):1005–1015. doi: 10.1160/TH09-11-0761. [DOI] [PubMed] [Google Scholar]
- 25.Krauskopf L. [Accessed February 13, 2012];FDA issues plan to avoid heparin contamination. 2012 Reuters.com. http://www.reuters.com/article/2012/02/10/us-fda-heparin-idUSTRE8190RB20120210.
- 26.Blossom DB, Kallen AJ, Patel PR, et al. Outbreak of adverse reactions associated with contaminated heparin. N Engl J Med. 2008;359(25):2674–2684. doi: 10.1056/NEJMoa0806450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dooren JC. [Accessed March 23, 2012];Suppliers linked to impure heparin. Wall Street J. 2012 http://online.wsj.com/article/SB10001424052970203960804577239624228625522.html. [Google Scholar]
- 28.Davenport A. Optimization of heparin anticoagulation for hemodialysis. Hemodial Int. 2011;15(suppl 1):S43–S48. doi: 10.1111/j.1542-4758.2011.00601.x. [DOI] [PubMed] [Google Scholar]
- 29.Ouseph R, Ward RA. Anticoagulation for intermittent hemodialysis. Semin Dial. 2000;13(3):181–187. doi: 10.1046/j.1525-139x.2000.00052.x. [DOI] [PubMed] [Google Scholar]
- 30.Mingardi G, Perico N, Pusineri F, et al. Heparin for hemodialysis: practical guidelines for administration and monitoring. Int J Artif Organs. 1984;7(5):269–274. [PubMed] [Google Scholar]
- 31.Wilhelmsson S, Lins LE. Heparin elimination and hemostasis in hemodialysis. Clin Nephrol. 1984;22(6):303–306. [PubMed] [Google Scholar]
- 32.Ward RA, Farrell PC. Precise anticoagulation for routine hemodialysis using nomograms. Trans Am Soc Artif Intern Organs. 1978;24:439–442. [PubMed] [Google Scholar]
- 33.Low CL, Bailie G, Morgan S, Eisele G. Effect of a sliding scale protocol for heparin on the ability to maintain whole blood activated partial thromboplastin times within a desired range in hemodialysis patients. Clin Nephrol. 1996;45(2):120–124. [PubMed] [Google Scholar]
- 34.Kandrotas RJ, Gal P, Douglas JB, Deterding J. Pharmacokinetics and pharmacodynamics of heparin during hemodialysis: interpatient and intrapatient variability. Pharmacotherapy. 1990;10(5):349–355. [PubMed] [Google Scholar]
- 35.Jannett TC, Wise MG, Shanklin NH, Sanders PW. Adaptive control of anticoagulation during hemodialysis. Kidney Int. 1994;45(3):912–915. doi: 10.1038/ki.1994.121. [DOI] [PubMed] [Google Scholar]
- 36.Ouseph R, Brier ME, Ward RA. Improved dialyzer reuse after use of a population pharmacodynamic model to determine heparin doses. Am J Kidney Dis. 2000;35(1):89–94. doi: 10.1016/S0272-6386(00)70306-4. [DOI] [PubMed] [Google Scholar]
- 37.Ehrmeyer SS, Laessig RH. Regulatory compliance for point-of-care testing: 2009 United States perspective. Clin Lab Med. 2009;29(3):463–478. doi: 10.1016/j.cll.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 38.European Best Practice Guidelines Working Group Section V. Chronic intermittent haemodialysis and prevention of clotting in the extracorporal system. Nephrol Dial Transplant. 2002;17(suppl 7):63–71. doi: 10.1093/ndt/17.suppl_7.63. [DOI] [PubMed] [Google Scholar]
- 39.Gordon LA, Perkins HA, Richards V. Studies in regional heparinization. I. The use of simultaneous neutralization with protamine; preliminary studies. N Engl J Med. 1956;255(22):1025–1029. doi: 10.1056/NEJM195611292552202. [DOI] [PubMed] [Google Scholar]
- 40.Hampers CL, Balufox MD, Merrill JP. Anticoagulation rebound after hemodialysis. N Engl J Med. 1966;275(14):776–778. doi: 10.1056/NEJM196610062751408. [DOI] [PubMed] [Google Scholar]
- 41.Blaufox MD, Hampers CL, Merrill JP. Rebound anticoagulation occurring after regional heparinization for hemodialysis. Trans Am Soc Artif Intern Organs. 1966;12:207–209. [PubMed] [Google Scholar]
- 42.Lavaud S, Paris B, Maheut H, et al. Assessment of the heparin-binding AN69 ST hemodialysis membrane: II. Clinical studies without heparin administration. ASAIO J. 2005;51(4):348–351. doi: 10.1097/01.mat.0000169121.09075.53. [DOI] [PubMed] [Google Scholar]
- 43.Wright MJ, Woodrow G, Umpleby S, Hull S, Brownjohn AM, Turney JH. Low thrombogenicity of polyethylene glycol-grafted cellulose membranes does not influence heparin requirements in hemodialysis. Am J Kidney Dis. 1999;34(1):36–42. doi: 10.1016/s0272-6386(99)70105-8. [DOI] [PubMed] [Google Scholar]
- 44.Evenepoel P. Heparin-coated hemodialyzers—the holy grail for patients at risk of bleeding? Nephron Clin Pract. 2004;97(1):c1–c2. doi: 10.1159/000077587. [DOI] [PubMed] [Google Scholar]
- 45.Swartz RD, Port FK. Preventing hemorrhage in high-risk hemodialysis: regional versus low-dose heparin. Kidney Int. 1979;16(4):513–518. doi: 10.1038/ki.1979.157. [DOI] [PubMed] [Google Scholar]
- 46.Swartz RD. Hemorrhage during high-risk hemodialysis using controlled heparinization. Nephron. 1981;28(2):65–69. doi: 10.1159/000182111. [DOI] [PubMed] [Google Scholar]
- 47.Wasse H, Gillen DL, Ball AM, et al. Risk factors for upper gastrointestinal bleeding among end-stage renal disease patients. Kidney Int. 2003;64(4):1455–1461. doi: 10.1046/j.1523-1755.2003.00225.x. [DOI] [PubMed] [Google Scholar]
- 48.Chachati A, Godon JP. Effect of haemodialysis on upper gastrointestinal tract pathology in patients with chronic renal failure. Nephrol Dial Transplant. 1987;1(4):233–237. [PubMed] [Google Scholar]
- 49.Yang JY, Lee TC, Montez-Rath ME, et al. Trends in acute nonvariceal upper gastrointestinal bleeding in dialysis patients. J Am Soc Nephrol. 2012;23(3):495–506. doi: 10.1681/ASN.2011070658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baroni CD. The pathobiography and death of Wolfgang Amadeus Mozart: from legend to reality. Hum Pathol. 1997;28(5):519–521. doi: 10.1016/s0046-8177(97)90071-x. [DOI] [PubMed] [Google Scholar]
- 51.Seliger SL, Gillen DL, Longstreth WT, Jr, Kestenbaum B, Stehman-Breen CO. Elevated risk of stroke among patients with end-stage renal disease. Kidney Int. 2003;64(2):603–609. doi: 10.1046/j.1523-1755.2003.00101.x. [DOI] [PubMed] [Google Scholar]
- 52.Kawamura M, Fijimoto S, Hisanaga S, Yamamoto Y, Eto T. Incidence, outcome, and risk factors of cerebrovascular events in patients undergoing maintenance hemodialysis. Am J Kidney Dis. 1998;31(6):991–996. doi: 10.1053/ajkd.1998.v31.pm9631844. [DOI] [PubMed] [Google Scholar]
- 53.Iseki K, Kinjo K, Kimura Y, Osawa A, Fukiyama K. Evidence for high risk of cerebral hemorrhage in chronic dialysis patients. Kidney Int. 1993;44(5):1086–1090. doi: 10.1038/ki.1993.352. [DOI] [PubMed] [Google Scholar]
- 54.Bhasin HK, Dana CL. Spontaneous retroperitoneal hemorrhage in chronically hemodialyzed patients. Nephron. 1978;22(4-6):322–327. doi: 10.1159/000181470. [DOI] [PubMed] [Google Scholar]
- 55.Vanichayakornkul S, Cioffi RF, Harper E, O’Connell JM, Shalhoub RJ. Spontaneous retroperitoneal hematoma. A complication of hemodialysis. JAMA. 1974;230(8):1164–1165. [PubMed] [Google Scholar]
- 56.De Santo NG, Capodicasa G, Perna N, De Pascale C, Giordano C. Haematoma of rectus abdominis associated with dialysis. Br Med J. 1972;3(5821):281–282. doi: 10.1136/bmj.3.5821.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Milutinovich J, Follette WC, Scribner BH. Spontaneous retroperitoneal bleeding in patients on chronic hemodialysis. Ann Intern Med. 1977;86(2):189–192. doi: 10.7326/0003-4819-86-2-189. [DOI] [PubMed] [Google Scholar]
- 58.Hayashi H, Kurata Y, Imanaga Y, Goya K, Oshima K. Vitrectomy for diabetic retinopathy in patients undergoing hemodialysis for associated end-stage renal failure. Retina. 1998;18(2):156–159. doi: 10.1097/00006982-199818020-00010. [DOI] [PubMed] [Google Scholar]
- 59.Slusher MM, Hamilton RW. Spontaneous hyphema during hemodialysis [letter] N Engl J Med. 1975;293(11):561. [PubMed] [Google Scholar]
- 60.Galen MA, Steinberg SM, Lowrie EG, Lazarus JM, Hampers CL, Merrill JP. Hemorrhagic pleural effusion in patients undergoing chronic hemodialysis. Ann Intern Med. 1975;82(3):359–361. doi: 10.7326/0003-4819-82-3-359. [DOI] [PubMed] [Google Scholar]
- 61.Alfrey AC, Goss JE, Ogden DA, Vogel JH, Holmes JH. Uremic hemopericardium. Am J Med. 1968;45(3):391–400. doi: 10.1016/0002-9343(68)90073-9. [DOI] [PubMed] [Google Scholar]
- 62.Davenport A. Antibodies to heparin-platelet factor 4 complex: pathogenesis, epidemiology, and management of heparin-induced thrombocytopenia in hemodialysis. Am J Kidney Dis. 2009;54(2):361–374. doi: 10.1053/j.ajkd.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 63.Chong BH. Heparin-induced thrombocytopenia. Blood Rev. 1988;2(2):108–114. doi: 10.1016/0268-960x(88)90032-x. [DOI] [PubMed] [Google Scholar]
- 64.Davenport A. Heparin-induced thrombocytopenia during renal replacement therapy. Hemodial Int. 2004;8(3):295–303. doi: 10.1111/j.1492-7535.2004.01108.x. [DOI] [PubMed] [Google Scholar]
- 65.Aird WC, Mark EJ. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 15-200. A 53-year-old man with a myocardial infarct and thromboses after coronary-artery bypass grafting. N Engl J Med. 2002;346(20):1562–1570. doi: 10.1056/NEJMcpc020015. [DOI] [PubMed] [Google Scholar]
- 66.King DJ, Kelton JG. Heparin-associated thrombocytopenia. Ann Intern Med. 1984;100(4):535–540. doi: 10.7326/0003-4819-100-4-535. [DOI] [PubMed] [Google Scholar]
- 67.Warkentin TE, Greinacher A, Koster A, Lincoff AM. Treatment and prevention of heparin-induced thrombocytopenia: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133((6)(suppl)):340S–380S. doi: 10.1378/chest.08-0677. [DOI] [PubMed] [Google Scholar]
- 68.Hutchison CA, Dasgupta I. National survey of heparin-induced thrombocytopenia in the haemodialysis population of the UK population. Nephrol Dial Transplant. 2007;22(6):1680–1684. doi: 10.1093/ndt/gfm055. [DOI] [PubMed] [Google Scholar]
- 69.Yamamoto S, Koide M, Matsuo M, et al. Heparin-induced thrombocytopenia in hemodialysis patients. Am J Kidney Dis. 1996;28(1):82–85. doi: 10.1016/s0272-6386(96)90134-1. [DOI] [PubMed] [Google Scholar]
- 70.Chang JJ, Parikh CR. When heparin causes thrombosis: significance, recognition, and management of heparin-induced thrombocytopenia in dialysis patients. Semin Dial. 2006;19(4):297–304. doi: 10.1111/j.1525-139X.2006.00176.x. [DOI] [PubMed] [Google Scholar]
- 71.Matsuo T, Kobayashi H, Matsuo M, et al. Frequency of anti-heparin-PF4 complex antibodies (HIT antibodies) in uremic patients on chronic intermittent hemodialysis. Pathophysiol Hae-most Thromb. 2006;35(6):445–450. doi: 10.1159/000102052. [DOI] [PubMed] [Google Scholar]
- 72.Mureebe L, Coats RD, Silliman WR, Shuster TA, Nichols WK, Silver D. Heparin-associated antiplatelet antibodies increase morbidity and mortality in hemodialysis patients. Surgery. 2004;136(4):848–853. doi: 10.1016/j.surg.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 73.Carrozza P, Gabutti L, Gilliet F, Marone C. Heparin-induced systemic inflammatory response syndrome with progressive skin necrosis in haemodialysis. Nephrol Dial Transplant. 1997;12(11):2424–2427. doi: 10.1093/ndt/12.11.2424. [DOI] [PubMed] [Google Scholar]
- 74.Leblanc M, Roy LF, Legault L, Dufresne LR, Morin C, Thuot C. Severe skin necrosis associated with heparin in hemodialysis. Nephron. 1994;68(1):133–137. doi: 10.1159/000188232. [DOI] [PubMed] [Google Scholar]
- 75.Popov D, Zarrabi MH, Foda H, Graber M. Pseudopulmonary embolism: acute respiratory distress in the syndrome of heparin-induced thrombocytopenia. Am J Kidney Dis. 1997;29(3):449–452. doi: 10.1016/s0272-6386(97)90208-0. [DOI] [PubMed] [Google Scholar]
- 76.Davenport A. Sudden collapse during haemodialysis due to immune-mediated heparin-induced thrombocytopaenia. Nephrol Dial Transplant. 2006;21(6):1721–1724. doi: 10.1093/ndt/gfl124. [DOI] [PubMed] [Google Scholar]
- 77.Warkentin TE, Heddle NM. Laboratory diagnosis of immune heparin-induced thrombocytopenia. Curr Hematol Rep. 2003;2(2):148–157. [PubMed] [Google Scholar]
- 78.Warkentin TE, Greinacher A. Heparin-induced thrombocytopenia: recognition, treatment, and prevention: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126((3)(suppl)):311S–337S. doi: 10.1378/chest.126.3_suppl.311S. [DOI] [PubMed] [Google Scholar]
- 79.Pena de la Vega L, Miller RS, Benda MM, et al. Association of heparin-dependent antibodies and adverse outcomes in hemodialysis patients: a population-based study. Mayo Clin Proc. 2005;80(8):995–1000. doi: 10.4065/80.8.995. [DOI] [PubMed] [Google Scholar]
- 80.Nakamoto H, Shimada Y, Kanno T, Wanaka K, Matsuo T, Suzuki H. Role of platelet factor 4-heparin complex antibody (HIT antibody) in the pathogenesis of thrombotic episodes in patients on hemodialysis. Hemodial Int. 2005;9(suppl 1):S2–S7. doi: 10.1111/j.1542-4758.2005.01163.x. [DOI] [PubMed] [Google Scholar]
- 81.Carrier M, Rodger MA, Fergusson D, et al. Increased mortality in hemodialysis patients having specific antibodies to the platelet factor 4-heparin complex. Kidney Int. 2008;73(2):213–219. doi: 10.1038/sj.ki.5002631. [DOI] [PubMed] [Google Scholar]
- 82.Krane V, Berger M, Lilienthal J, Winkler K, Schambeck C, Wanner C. Antibodies to platelet factor 4-heparin complex and outcome in hemodialysis patients with diabetes. Clin J Am Soc Nephrol. 2010;5(5):874–881. doi: 10.2215/CJN.01170209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Carrier M, Knoll GA, Kovacs MJ, Moore JC, Fergusson D, Rodger MA. The prevalence of antibodies to the platelet factor 4-heparin complex and association with access thrombosis in patients on chronic hemodialysis. Thromb Res. 2007;120(2):215–220. doi: 10.1016/j.thromres.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 84.Nasstrom B, Olivecrona G, Olivecrona T, Stegmayr BG. Lipoprotein lipase during heparin infusion: lower activity in hemodialysis patients. Scand J Clin Lab Invest. 2003;63(1):45–53. doi: 10.1080/00365510310000484. [DOI] [PubMed] [Google Scholar]
- 85.Nasstrom B, Stegmayr B, Olivecrona G, Olivecrona T. Lipoprotein lipase in hemodialysis patients: indications that low molecular weight heparin depletes functional stores, despite low plasma levels of the enzyme. BMC Nephrol. 2004;5:17. doi: 10.1186/1471-2369-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Elisaf MS, Germanos NP, Bairaktari HT, Pappas MB, Koulouridis EI, Siamopoulos KC. Effects of conventional vs. low-molecular-weight heparin on lipid profile in hemodialysis patients. Am J Nephrol. 1997;17(2):153–157. doi: 10.1159/000169090. [DOI] [PubMed] [Google Scholar]
- 87.Wiemer J, Winkler K, Baumstark M, Marz W, Scherberich JE. Influence of low molecular weight heparin compared to conventional heparin for anticoagulation during haemodialysis on low density lipoprotein subclasses. Nephrol Dial Transplant. 2002;17(12):2231–2238. doi: 10.1093/ndt/17.12.2231. [DOI] [PubMed] [Google Scholar]
- 88.Yang C, Wu T, Huang C. Low molecular weight heparin reduces triglyceride, VLDL and cholesterol/HDL levels in hyper-lipidemic diabetic patients on hemodialysis. Am J Nephrol. 1998;18(5):384–390. doi: 10.1159/000013381. [DOI] [PubMed] [Google Scholar]
- 89.Deuber HJ, Schulz W. Reduced lipid concentrations during four years of dialysis with low molecular weight heparin. Kidney Int. 1991;40(3):496–500. doi: 10.1038/ki.1991.237. [DOI] [PubMed] [Google Scholar]
- 90.Kronenberg F, Konig P, Lhotta K, Steinmetz A, Dieplinger H. Low molecular weight heparin does not necessarily reduce lipids and lipoproteins in hemodialysis patients. Clin Nephrol. 1995;43(6):399–404. [PubMed] [Google Scholar]
- 91.Kronenberg F, Konig P, Neyer U, et al. Influence of various heparin preparations on lipoproteins in hemodialysis patients: a multicentre study. Thromb Haemost. 1995;74(4):1025–1028. [PubMed] [Google Scholar]
- 92.Hottelart C, Achard JM, Moriniere P, Zoghbi F, Dieval J, Fournier A. Heparin-induced hyperkalemia in chronic hemodialysis patients: comparison of low molecular weight and unfractionated heparin. Artif Organs. 1998;22(7):614–617. doi: 10.1046/j.1525-1594.1998.06204.x. [DOI] [PubMed] [Google Scholar]
- 93.Bottio T, Pittarello G, Bonato R, Fagiolo U, Gerosa G. Life-threatening anaphylactic shock caused by porcine heparin intravenous infusion during mitral valve repair. J Thorac Cardiovasc Surg. 2003;126(4):1194–1195. doi: 10.1016/s0022-5223(03)00813-4. [DOI] [PubMed] [Google Scholar]
- 94.Harada A, Tatsuno K, Kikuchi T, et al. Use of bovine lung heparin to obviate anaphylactic shock caused by porcine gut heparin. Ann Thorac Surg. 1990;49(5):826–827. doi: 10.1016/0003-4975(90)90037-7. [DOI] [PubMed] [Google Scholar]
- 95.Schulman S, Hellgren-Wangdahl M. Pregnancy, heparin and osteoporosis. Thromb Haemost. 2002;87(2):180–181. [PubMed] [Google Scholar]
- 96.Binici DN, Gunes N. Risk factors leading to reduced bone mineral density in hemodialysis patients with metabolic syndrome. Ren Fail. 2010;32(4):469–474. doi: 10.3109/08860221003675260. [DOI] [PubMed] [Google Scholar]
- 97.Lai KN, Ho K, Cheung RC, et al. Effect of low molecular weight heparin on bone metabolism and hyperlipidemia in patients on maintenance hemodialysis. Int J Artif Organs. 2001;24(7):447–455. [PubMed] [Google Scholar]
- 98.Edes TE, Sunderrajan EV. Heparin-induced hyperkalemia. Arch Intern Med. 1985;145(6):1070–1072. [PubMed] [Google Scholar]
- 99.Diskin CJ, Stokes TJ, Dansby LM, Radcliff L, Carter TB. Is systemic heparin a risk factor for catheter-related sepsis in dialysis patients? An evaluation of various biofilm and traditional risk factors. Nephron Clin Pract. 2007;107(4):c128–c132. doi: 10.1159/000110032. [DOI] [PubMed] [Google Scholar]
- 100.Shanks RM, Donegan NP, Graber ML, et al. Heparin stimulates Staphylococcus aureus biofilm formation. Infect Immun. 2005;73(8):4596–4606. doi: 10.1128/IAI.73.8.4596-4606.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hetzel GR, Sucker C. The heparins: all a nephrologist should know. Nephrol Dial Transplant. 2005;20(10):2036–2042. doi: 10.1093/ndt/gfi004. [DOI] [PubMed] [Google Scholar]
- 102.Warkentin TE, Levine MN, Hirsh J, et al. Heparin-induced thrombocytopenia in patients treated with low-molecular-weight heparin or unfractionated heparin. N Engl J Med. 1995;332(20):1330–1335. doi: 10.1056/NEJM199505183322003. [DOI] [PubMed] [Google Scholar]
- 103.Lim W, Cook DJ, Crowther MA. Safety and efficacy of low molecular weight heparins for hemodialysis in patients with end-stage renal failure: a meta-analysis of randomized trials. J Am Soc Nephrol. 2004;15(12):3192–3206. doi: 10.1097/01.ASN.0000145014.80714.35. [DOI] [PubMed] [Google Scholar]
- 104.Crowther MA, Berry LR, Monagle PT, Chan AK. Mechanisms responsible for the failure of protamine to inactivate low-molecular-weight heparin. Br J Haematol. 2002;116(1):178–186. doi: 10.1046/j.1365-2141.2002.03233.x. [DOI] [PubMed] [Google Scholar]
- 105.Davenport A. Review article: low-molecular-weight heparin as an alternative anticoagulant to unfractionated heparin for routine outpatient haemodialysis treatments. Nephrology (Carlton) 2009;14(5):455–461. doi: 10.1111/j.1440-1797.2009.01135.x. [DOI] [PubMed] [Google Scholar]
- 106.Borm JJ, Krediet R, Sturk A, ten Cate JW. Heparin versus low molecular weight heparin K 2165 in chronic hemodialysis patients: a randomized cross-over study. Haemostasis. 1986;16(suppl 2):59–68. doi: 10.1159/000215582. [DOI] [PubMed] [Google Scholar]
- 107.Schrader J, Stibbe W, Armstrong VW, et al. Comparison of low molecular weight heparin to standard heparin in hemodialysis/hemofiltration. Kidney Int. 1988;33(4):890–896. doi: 10.1038/ki.1988.81. [DOI] [PubMed] [Google Scholar]
- 108.Anastassiades E, Lane DA, Ireland H, Flynn A, Curtis JR. A low molecular weight heparin (“fragmin”) for routine hemodialysis: a crossover trial comparing three dose regimens with a standard regimen of commercial unfractionated heparin. Clin Nephrol. 1989;32(6):290–296. [PubMed] [Google Scholar]
- 109.Nurmohamed MT, ten Cate J, Stevens P, Hoek JA, Lins RL, ten Cate JW. Long-term efficacy and safety of a low molecular weight heparin in chronic hemodialysis patients. A comparison with standard heparin. ASAIO Trans. 1991;37(3):M459–M461. [PubMed] [Google Scholar]
- 110.Ryan KE, Lane DA, Flynn A, Shepperd J, Ireland HA, Curtis JR. Dose finding study of a low molecular weight heparin, Innohep, in haemodialysis. Thromb Haemost. 1991;66(3):277–282. [PubMed] [Google Scholar]
- 111.Harenberg J, Haaf B, Dempfle CE, Stehle G, Heene DL. Monitoring of heparins in haemodialysis using an anti-factor-Xa-specific whole-blood clotting assay. Nephrol Dial Transplant. 1995;10(2):217–222. [PubMed] [Google Scholar]
- 112.Moia M, Graziani G, Tenconi PM, Martinelli I, Ponticelli C. Rationale for the use of a low molecular weight heparin during hemodialysis with polysulphone membrane in uremic patients. Ann Ital Med Int. 1997;12(2):67–71. [PubMed] [Google Scholar]
- 113.Saltissi D, Morgan C, Westhuyzen J, Healy H. Comparison of low-molecular-weight heparin (enoxaparin sodium) and standard unfractionated heparin for haemodialysis anticoagulation. Nephrol Dial Transplant. 1999;14(11):2698–2703. doi: 10.1093/ndt/14.11.2698. [DOI] [PubMed] [Google Scholar]
- 114.Stefoni S, Cianciolo G, Donati G, et al. Standard heparin versus low-molecular-weight heparin. A medium-term comparison in hemodialysis. Nephron. 2002;92(3):589–600. doi: 10.1159/000064086. [DOI] [PubMed] [Google Scholar]
- 115.Lord H, Jean N, Dumont M, Kassis J, Leblanc M. Comparison between tinzaparin and standard heparin for chronic hemodialysis in a Canadian center. Am J Nephrol. 2002;22(1):58–66. doi: 10.1159/000046675. [DOI] [PubMed] [Google Scholar]
- 116.Leu JG, Chiang SS, Lin SM, Pai JK, Jiang WW. Low molecular weight heparin in hemodialysis patients with a bleeding tendency. Nephron. 2000;86(4):499–501. doi: 10.1159/000045840. [DOI] [PubMed] [Google Scholar]
- 117.Hursting MJ, Murray PT. Argatroban anticoagulation in renal dysfunction: a literature analysis. Nephron Clin Pract. 2008;109(2):c80–c94. doi: 10.1159/000139993. [DOI] [PubMed] [Google Scholar]
- 118.Greinacher A, Warkentin TE. The direct thrombin inhibitor hirudin. Thromb Haemost. 2008;99(5):819–829. doi: 10.1160/TH07-11-0693. [DOI] [PubMed] [Google Scholar]
- 119.van Wyk V, Badenhorst PN, Luus HG, Kotze HF. A comparison between the use of recombinant hirudin and heparin during hemodialysis. Kidney Int. 1995;48(4):1338–1343. doi: 10.1038/ki.1995.419. [DOI] [PubMed] [Google Scholar]
- 120.Magnani HN. A review of 122 published outcomes of danaparoid anticoagulation for intermittent haemodialysis. Thromb Res. 2010;125(4):e171–e176. doi: 10.1016/j.thromres.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 121.Kalicki RM, Aregger F, Alberio L, Lammle B, Frey FJ, Uehlinger DE. Use of the pentasaccharide fondaparinux as an anticoagulant during haemodialysis. Thromb Haemost. 2007;98(6):1200–1207. doi: 10.1160/th07-07-0444. [DOI] [PubMed] [Google Scholar]
- 122.Apsner R, Buchmayer H, Gruber D, Sunder-Plassmann G. Citrate for long-term hemodialysis: prospective study of 1,009 consecutive high-flux treatments in 59 patients. Am J Kidney Dis. 2005;45(3):557–564. doi: 10.1053/j.ajkd.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 123.Caruana RJ, Raja RM, Bush JV, Kramer MS, Goldstein SJ. Heparin free dialysis: comparative data and results in high risk patients. Kidney Int. 1987;31(6):1351–1355. doi: 10.1038/ki.1987.149. [DOI] [PubMed] [Google Scholar]
- 124.Keller F, Seemann J, Preuschof L, Offermann G. Risk factors of system clotting in heparin-free haemodialysis. Nephrol Dial Transplant. 1990;5(9):802–807. doi: 10.1093/ndt/5.9.802. [DOI] [PubMed] [Google Scholar]
- 125.Casati S, Moia M, Graziani G, et al. Hemodialysis without anticoagulants: efficiency and hemostatic aspects. Clin Nephrol. 1984;21(2):102–105. [PubMed] [Google Scholar]
- 126.Preuschof L, Keller F, Seemann J, Offermann G. Heparin-free hemodialysis with prophylactic change of dialyser and blood lines. Int J Artif Organs. 1988;11(4):255–258. [PubMed] [Google Scholar]
- 127.Sanders PW, Taylor H, Curtis JJ. Hemodialysis without anticoagulation. Am J Kidney Dis. 1985;5(1):32–35. doi: 10.1016/s0272-6386(85)80132-3. [DOI] [PubMed] [Google Scholar]