Abstract
In high-income countries, higher social capital is associated with better health. However, there is little evidence of this association in low- and middle-income countries. We examine the association between social capital (social support and trust) and both self-rated and biologically assessed health outcomes in Chile, a middle-income country that experienced a major political transformation and welfare state expansion in the last two decades. Based on data from the Chilean National Health Survey (2009–10), we modeled self-rated health, depression, measured diabetes and hypertension as a function of social capital indicators, controlling for socio-economic status and health behavior. We used an instrumental variable approach to examine whether social capital was causally associated with health. We find that correlations between social capital and health observed in high-income countries are also observed in Chile. All social capital indicators are significantly associated with depression at all ages, and at least one social capital indicator is associated with self-rated health, hypertension and diabetes at ages 45 and above. Instrumental variable models suggest that associations for depression may reflect a causal effect from social capital indicators on mental well-being. Using aggregate social capital as instrument, we also find evidence that social capital may be causally associated with hypertension and diabetes, early markers of cardiovascular risk. Our findings highlight the potential role of social capital in the prevention of depression and early cardiovascular disease in middle-income countries.
Keywords: Social Capital, Self-reported health, Depression, Cardiovascular, Low and Middle-income Countries
Introduction
Social capital is usually defined as the institutions, relationships and norms that shape the quality and frequency of social interactions. Like human and economic capital, theories advocate that social capital may generate welfare benefits (Bourdieu, 1986). Studies during the last decades suggest that there is a significant association between social capital and self-reported health, mortality and life expectancy (Kawachi & Berkman, 2000; Kawachi et al., 1999; Kawachi et al., 1997; Kennedy et al., 1998; Kim et al., 2008; Lochner et al., 2003; Subramanian et al., 2001). However, this association may differ for various health outcomes. In addition, while most of the literature has focused on high-income countries as qualified by the World Bank (> US $ 12,615 GNI per capita), the influence of social capital on health is less well understood for low- and middle-income countries.
In low- and middle-income countries, welfare state policies and social safety net programs are weaker than in most high-income countries. As a result, access to different forms of social protection is limited and benefits a smaller part of the population (Mesa-Lago, 2007; van Ginneken, 1999). In this context, social capital may be particularly relevant to enhance collective actions within communities, becoming a potential driver of health improvements (Aye et al., 2002; Lindstrom et al., 2006; Mohseni & Lindstrom, 2007). In support of this view, evidence suggests that cohesive communities may be more successful in protecting healthcare facilities from budget cuts (Sampson et al., 1997); organizing public services (Altschuler et al., 2004; Kawachi et al., 1997); reducing crime (Takagi et al., 2012); and promoting economic solidarity (Aye et al., 2002). Social capital may thus allow communities in less developed countries to maintain better living standards and, in the absence of strong social safe net policies, may become a more important driver of population health than in high-income countries.
Most of the evidence in this domain comes from the United States, Europe and Japan (Islam et al., 2006), while few studies have explored this association in other economic and cultural contexts. A recent cross-national study used Gallup World Poll data for 139 countries and found that levels of social support were associated with levels of health satisfaction in most countries, but no association was found for volunteering in most low- and middle-income regions (Kumar et al., 2012). The small sample sizes, the focus on health satisfaction as single outcome and the lack of many control variables however, suggest a cautious interpretation of these findings. Other studies have found evidence that social capital is associated with health in Colombia and Chile (Harpham et al., 2004; Hurtado et al., 2011; Kumar et al., 2012; Sapag et al., 2008), but they were based on restrictive samples, specific health outcomes, and their results may not be generalizable to national populations. Further motivation for this study is provided by studies that have found social capital to be important in low-income communities within high-income countries (Franzini, 2008; Mulvaney-Day et al., 2007).
Chile offers an interesting case study to examine the links between social capital and health. Despite a general trend of economic growth and health improvements during recent decades, significant income and health inequalities persist (Ewig & Palmucci, 2012; Lopez & Miller, 2008). Parallel to this, studies suggest that levels of trust in others and government have substantially declined during recent decades (Gfk, 2012). Improvements in the economy and population health may have been offset by decreasing levels of social capital. In this context, social capital may have become more essential to population health, by promoting collective actions aimed at social and health protection of entire communities.
Previous studies have consistently reported an association between social capital and subjective health, but evidence of an association with objectively measured health remains more tenuous. While social capital has been found to be associated with measures of physical functioning such as grip strength (Sirven & Debrand, 2011), several studies on measured cardiovascular outcomes and markers have found either no association (Siahpush & Singh, 1999) or relatively weak associations (Holtgrave & Crosby, 2006; Kim et al., 2006). Distinguishing objective from subjective measures of health is important for two reasons. First, the association between self-reported health and self-reported social capital may result from a common source bias. For example, individuals experiencing depression may be more likely to report both being in poor health and perceiving lower levels of social capital in their communities, resulting in a spurious, non-causal association. Second, analyzing the association between social capital and biomarkers may provide insights on the potential biological mechanisms linking social capital and overall health.
An important concern is whether the association between social capital and health is causal. While existing studies often control for a variety of potential confounders (Blakely et al., 2006; Kennelly et al., 2003; Lynch et al., 2001), residual confounding and reverse causality remain a concern. An instrumental variable (IV) approach provides an alternative to examine whether this association is causal. For example, a recent study based on data for 11 European countries used the aggregate rate of associational membership to voluntary organizations in the living area as an IV and found that that higher levels of social participation were associated with better health (Sirven et al., 2008). Other studies have used corruption, population density, regional citizenship rates and religious fractionalization as IVs. Some of these studies corroborated some of the observed associations between social capital and health (Kim et al., 2011; Rocco & Suhrcke, 2012). To our knowledge, no studies have used these methods to assess whether social capital is associated with both objective and subjective health in a low- or middle-income country.
In this paper, we aim to assess the association between social capital and a variety of both physical and mental health outcomes (self-reported health, depression, diabetes and hypertension) in a nationally representative sample of men and woman in Chile. We test whether the well-documented association between social capital and health in high-income countries is observed in a middle-income country that has suffered major economic and social transformations, and that has a less developed set of social protection programs compared to high-income countries. We hypothesized that in the absence of a well-developed social safety net, social capital may be more strongly associated with health, particularly for older individuals who may rely more heavily on social protection programs than their younger counterparts. Our study builds up on previous literature by using an IV approach to assess whether observed associations may reflect a causal effect from social capital to health, using a variety of instruments at the individual and community level.
Method
Sample
Data came from the Chilean National Health Survey (2009–10), a survey designed to measure individual and household health-related characteristics. Stratified sampling was used to cover both administrative regions and urban/rural locations. Following stratification, random individuals were chosen from randomly selected households in communes chosen proportionally by the number of individuals over 15 years of age. Data collection took place in two stages: the first stage comprised face-to-face interviews to collect information on self-reported health, household characteristics and living conditions; in the second stage, clinical measurements and biological samples were collected by trained nurses. The first stage included 5,434 respondents and had a response rate of 85%. The second stage was restricted to the sub-sample of individuals who agreed to participate in the collection of biological samples (N=4,956, response rate=77%). Response rates were high compared to studies in the US and Europe collecting biological measures (usually 60% or lower). Data are representative of the whole Chilean population based on the statistics from the 2002 Chilean National Census (MINSAL, 2009). Since the objective of this study is to evaluate the effect of social capital on older adult populations we have excluded individuals under the age of 30. Particularly since the prevalence of depression, diabetes and hypertension was less than 5% in the sample for the population under 30 years old. Nevertheless, results incorporating all respondents aged 18 years and older yielded essentially the same results.
Health Measures
Data on self-rated health, measured blood pressure and assessed blood sugar were used as indicators of physical health, while depressive symptom score was used as indicator of mental health. Self-reported health is a common measure in the epidemiological literature and is considered both a valid measurement of general health and a predictor of mortality (Gold et al., 1996; Idler & Benyamini, 1997). The item used was based on the 2003 World Health Survey of the World Health Organization, in which respondents were asked to rate their state of general health on a 5-point scale (very good to very bad). Following prior conventions (Kennedy et al., 1998; Subramanian et al., 2003), self-reported health was collapsed into a binary variable where 1 indicated poor or very poor health. Results based on a continuous version of the self-rated health yielded similar results.
Depressive symptoms were measured based on the latest corrected version of the Composite International Instrument Short-Form for depression included in the National Health Survey (Kessler et al., 1998). The questionnaire included 30 items to identify depressive symptoms and frequency within the last 12 months and included questions on depression, fatigue, weight loss, restless sleep, lack of focus, low self-esteem and suicidal thoughts such as: “In the last 12 months, have you felt lonely, sad or depressed for two or more consecutive weeks?” or “On those two weeks have you thought about death, be it your own, somebody else’s or in general?”. A total score was constructed based on responses to each item. We then dichotomized this variable using a threshold suggested in previous literature (Rioseco et al., 2002), with a value of 1 indicating depressive symptoms potentially signaling depression.
Blood pressure was measured by a trained nurse who took three independent measures of systolic and diastolic pressure with previously validated instruments (Coleman et al., 2005; O’Brien et al., 2001). To verify the reliability of these measures, the nurse conducted a small survey to assess the conditions under which the measurements were collected. In addition, the nurse performed two additional measures with a different instrument on a random sample of respondents. Based on guidelines by the 7th Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (Chobanian et al., 2003) as well as the American Heart Organization and WHO, individuals were classified as having hypertension if their average arterial pressure was above 140/90 mmHg or if they reported taking medication for hypertension at the time of assessment. Blood glucose levels were assessed based on blood samples collected after fasting for at least 8 hours. Individuals where given the instructions to fast for 8 hours before the nurses visit and the adherence to this request was confirmed in the survey conducted by the nurse. The measurements from the blood samples were compared with hemoglucotests in order to assure the validity of the results. Individuals were classified as having diabetes if their blood glycaemia was at least 126 mg/dl or if they reported being diagnosed with diabetes, following current guidelines from the WHO.
Measurements of Social Capital
This study evaluates the impact of three self-reported measurements of social capital: social support, generalized trust and neighborhood trust. Social support can be qualified as instrumental, emotional or informational and is a stress buffer hypothesized to prevent negative consequences on health (Harpham, 2008). Our data included assessments of emotional social support, measured by asking respondents to rate on a 4-point scale (strongly agree, slightly agree, slightly disagree or strongly disagree) the extent to which they agreed with the following statement: “No one cares about what happens to me”. In most analyses, we collapsed this measure into a binary variable based on whether individuals strongly agreed with the above statement versus other categories. We chose this cut-off point because the distribution of this variable was skewed, with 11% of individuals reporting that they strongly agree with this statement.
Generalized trust was measured by asking respondents to rate on the same 4-point scale the extent to which they agreed with the following statement: “It is safer not to trust anyone?”. This was considered a measure of “thin trust,” as it did not refer to an individual’s specific community but to society as a whole. In most analyses, we used a similar cut-off point as before and collapsed this measure into a binary variable.
Neighborhood trust was assessed based on the following item: “Rate your level of confidence from 1 to 7, where 1 is no confidence and 7 is total confidence. In general, how much do you trust the people in your neighborhood?”. This was considered a measure of “thick trust,” as individuals were asked to make judgments with respect to their neighborhood. Responses were categorized into quartiles and subsequently collapsed into a binary variable, with 1 indicating the lowest quartile of Neighborhood Trust.
Other covariates
Control variables included age in years, gender, years of schooling, marital status (single, married or together, divorced or separated and widowed), household size, monthly household income in USD 2009 PPP, employment status (employed, unemployed and looking for employment, retired or disabled, and out of the labor force), smoking status (non-smoker, ex-smoker or smoker), excessive alcohol consumption. Monthly household income was stratified into four categories. The lowest and baseline category corresponded to incomes less than US $389.99 that was approximately equivalent to the individual minimum wage in Chile. The following categories were US $390.00–714.99 and US $715.00–1284.99, representing to lower and higher middle-income families. The highest category included monthly incomes over US $1285.00, corresponding to the wealthier segment of the population. Alcohol consumption was measured with the Alcohol Use Disorders Identification Test (AUDIT). This test identifies dangerous drinking behaviors through a summary score constructed from questions on drinking behavior such as drinking frequency, quantity, or not being able to stop drinking (Bush et al., 1998). A higher AUDIT score represents a more dangerous drinking behavior. All models also included regional fixed effects.
Instrumental Variables
Instrumental variable (IV) estimation is used to assess the causal relationship between an endogenous variable and an outcome when controlled experiments are not feasible. An IV is not a covariate in the equation but is correlated with the endogenous variable. Two conditions are required for an IV to be valid: The IV must be correlated with the endogenous independent variable, and it should have no effect on the outcome other than through the endogenous variable.
Our IV analysis seeks to reduce bias caused by reverse causation and residual confounding. In our case a valid IV should be predict social capital, but it should have no direct effect on health other than through social capital. Based on these criteria, we used as our instrument an indicator of whether the respondent or any members of his or her family had been victim of a crime in the last 12 months. Our first rationale to select this instrument was based on the fact that being the victim of a crime is a strong predictor of social capital (Harpham, 2008). Although being victim of a crime may not be completely exogenous as it can depend on factors such as age, gender and place of residence, conditional on controlling for these and other demographic factors, we expected risk to be potentially exogenous. We therefore control for residence and individual characteristics in all of our models.
While victimization may have a direct impact on health, the majority of crimes are small events that will not physically harm the victim, but will have negative consequences on individual levels of social capital (Harpham, 2008). It is possible that even small crimes have an impact on individual stress, potentially violating the assumption that the instrument does not have effects on health other than through social capital. The most important concern is the direct effect of crime on mental health. In this regard, it is indeed difficult to distinguish whether the instrument captures the direct effect of crime on mental health, versus an effect mediated by social capital. However we argue that the effect of non-violent crime on mental health impacts individual perceptions with respect to the safety in their communities, which by definition composes a dimension of social capital. Therefore, the ‘direct’ effects would be conceived partly as the result of reductions in social trust – leading to stress and sense of insecurity – that ultimately impacts mental health. Nevertheless, to assess the potential impact of this or other exclusion criteria not being met, in separate models, we followed the approach in previous studies and used aggregate social capital at the community level as the instrument. Aggregate levels may increase individual levels of social capital, for example, by encouraging imitation or by providing more opportunities for social interaction or other forms of social capital in a community (Becker & Murphy, 2000; Glaeser et al., 2002; Sirven & Debrand, 2008). However, they would be exogenous to the individual and would in principle have no direct effect on an individual’s health. Geography may also confound the results of the IV estimates for aggregate social capital. However, in the conceptualization of both IV models the instrument is considered as ‘exogenous’ to the individual, conditional on a set of confounders for which we control for such as regional and communal covariates.
Procedures
We started by assessing the association between each indicator of social capital and each health outcome using logistic regression, controlling for socio-demographic variables and regional fixed effects. Subsequently, we incorporated health behavior measures to assess to what extent associations were robust to controlling for behavioral differences. We then implemented stratified models to assess whether associations differed by sex, age group (30–44, 45–64 and 65+) and urban/rural residence.
Subsequently, we conducted an IV analysis based on a two-stage least square model. In the first stage, Social Support (SSi), Generalized Trust (GTi) and Neighborhood Trust (NTi) were regressed using ordinary least squares (OLS) on a variable indicating whether the respondent or a family member had been victim of a crime as the IV, controlling for an extensive set of demographics, income, health behavior, small area of residence and average area income (ACIi). Using Di to represent the demographic covariates, Ei the socioeconomic covariates, HBi the health behavior, ACIi the average community income, Rir the regional dummies and IVi the IVs in the model, the first-stage equation for social trust was as follows (similar equations for the other two outcomes were used):
| (1) |
In the second stage, we used predicted values of social support ( ), generalized trust ( ) and neighbourhood trust ( ) from the first equation in a separate equation as covariates to predict health outcomes, controlling for all variables included in the first-stage equation excluding the instrument. As example, the second-stage equation for social capital was as follows:
| (2) |
Results from the IV models are presented next to results from regular OLS models without instruments for comparison. We used the Anderson canonical LM test to assess the strength of the instruments. Additionally, the Durbin-Wu-Hausman endogeneity test was used to evaluate the endogeneity of social support, generalized trust and neighborhood trust against the null hypothesis of exogeneity.
All analyses were conducted using STATA version 12.
Results
Descriptive
Table 1 summarizes the sample descriptive statistics. 8.68% of respondents report being in poor health, 15.98% are classified as depressed, 14.64% as having diabetes and 41.26% are classified as hypertensive. 60.8% reports low high levels of social support, while 12.0% report having low social support. For the other two social capital variables, the observations are well distributed among the different categories, with the number of individuals having low generalized or neighborhood trust being 28.40% and 24.71%, respectively.
Table 1.
Data Description for Final Sample
| Survey Response | ||
|---|---|---|
| Health Outcomes | ||
| Poor Health | Yes (n=355, 8.68%) | No (n=3733,91.32%) |
| Depression | Yes (n=574, 15.98%) | No (n=3019, 84.02%) |
| Diabetes | Yes (n=537, 14.64%) | No (n=3131, 85.36%) |
| Hypertension | Yes (n=1598, 41.26%) | No (n=2275, 58.74%) |
| Variables | ||
| Age (Years) | Mean: 53.58 | Range: 30–100 |
| Gender | Base Female (n=2524, 59.97%) | Male (n=1685, 40.03%) |
| Years of Schooling | Mean: 9.15 | Range: 0–23 |
| Urban/Rural | Base Rural (n=671, 15.95%) | Urban (n=3537, 84.05%) |
| Marital Status | Base: Married or Ensemble (n=2562, 54.98%) | Single (n=567, 12.17%) |
| Separated or Divorced (n=1017, 21.82%) | ||
| Widow (n=514, 11.03%) | ||
| Monthly Household Income (in US$ PPP) | Base: $0–$389.99 (n=881, 22.39%) | $390.00–714.99 (n=1389, 35.30%) |
| $715.00–$1,284.99 (n=945, 24.02%) | ||
| $1,285.00- (n=720,18.30%) | ||
| Alcohol (AUDIT) | Mean: 2.39 | Range: 0–34 |
| Smoking | Base: Non Smoker (n=1725, 42.20%) | Ex-Smoker (n=1109, 27.13%) |
| Smoker (n=1254, 30.68%) | ||
| Social Support | Base: Strongly Disagrees (n=2405, 60.08%) | Slightly Disagrees (n=547, 13.66%) |
| Slightly Agrees (n=572, 14.29%) | ||
| Strongly Agrees (n=479, 11.97%) | ||
| Generalized Trust | Base: Strongly Disagrees (n=1038, 25.80%) | Slightly Disagrees (n=858, 21.32%) |
| Slightly Agrees (n=991, 24.63%) | ||
| Strongly Agrees (n=1137, 28.26%) | ||
| Neighbourhood Trust | Base: 4th Quartile/Highest (n=989, 24.19%) | 1st Quartile (n=1331, 32.56%) |
| 2nd Quartile (n=730, 17.86%) | ||
| 3rd Quartile (n=1038, 25.39%) | ||
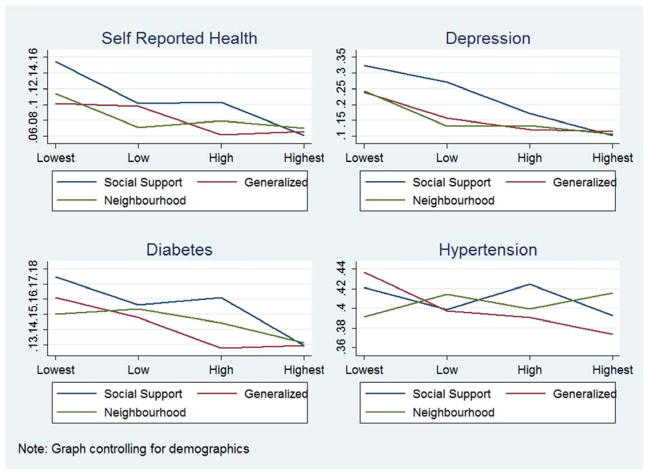
Figure 1 shows to the association of different levels of social capital with the different outcomes. Controlling for demographic covariates, there is a graded negative association between social capital levels and the prevalence of poor health, depression and diabetes, while social capital is not clearly associated with hypertension prevalence.
Figure 1.
Prevalence of poor health for individuals over 30 in the 2009 Chilean National Health Survey
Logistic regression models
The results in Table 2 suggest that both social support and neighborhood trust are consistently associated with self-reported health. Controlling for demographics, socioeconomic indicators and health behaviors, individuals in the lowest level of social support have more than twice the odds of reporting poor health than those with the highest level of social support (OR=2.34, 95% CI: 1.68–3.28). The magnitude of the association is smaller but significant for those who have intermediate levels of social support. Similarly, individuals in the lowest quartile of neighborhood trust have 62% (OR=1.62, 95% CI: 1.16–2.28) higher odds of reporting poor health than those in the higher quartile of trust. Lower levels of generalized trust are also associated with poorer health in models that control only for demographics, but this association is attenuated and no longer significant after controlling for socioeconomic status.
Table 2.
Odds ratios: Association between social capital (social support, generalized trust and neighborhood trust) and self-rated health and depression, ages 30+, National Health Survey, 2009.
| Social Support | Generalized Trust | Neighborhood Trust | |||||||
|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (1) | (2) | (3) | (1) | (2) | (3) | |
| a)Self-reported health | |||||||||
| Strongly Agree or Lowest Quartile (Lowest Social Capital) | 2.42*** [1.77,3.31] | 2.36*** [1.71,3.27] | 2.34*** [1.68,3.28] | 1.21 [0.87,1.68] | 1.11 [0.79,1.55] | 1.1 [0.78,1.56] | 1.60** [1.17,2.19] | 1.56** [1.13,2.15] | 1.62** [1.16,2.28] |
| Slightly Agree or 2nd Quartile | 1.46* [1.06,2.03] | 1.48* [1.06,2.06] | 1.44* [1.02,2.03] | 1.26 [0.90,1.75] | 1.19 [0.85,1.68] | 1.18 [0.83,1.68] | 1.02 [0.70,1.50] | 0.97 [0.65,1.44] | 1.05 [0.70,1.57] |
| Slightly Disagree or 3rd Quartile | 1.52* [1.08,2.13] | 1.43* [1.01,2.04] | 1.4 [0.97,2.01] | 0.76 [0.52,1.12] | 0.77 [0.52,1.15] | 0.78 [0.52,1.17] | 1.22 [0.87,1.71] | 1.19 [0.83,1.68] | 1.25 [0.87,1.80] |
| Strongly Disagree or 4th Quartile (Highest Social Capital) | Ref. | ||||||||
| Observations | 3996 | 3844 | 3580 | 4017 | 3863 | 3595 | 4080 | 3922 | 3650 |
| Log lik. | −1063.8 | −999.1 | −931.7 | −1071.6 | −1005.8 | −937.5 | −1113 | −1043.4 | −973.9 |
| Chi-squared | 179.9 | 206 | 194.3 | 156.9 | 185.9 | 170.8 | 178.5 | 203.8 | 189 |
| b) Depression | |||||||||
| Strongly Agree or Lowest Quartile (Lowest Social Capital) | 3.83*** [2.91,5.03] | 3.87*** [2.93,5.12] | 4.09*** [3.05,5.49] | 2.09*** [1.59,2.75] | 2.03*** [1.53,2.69] | 1.91*** [1.43,2.57] | 2.32*** [1.77,3.03] | 2.20*** [1.67,2.90] | 2.21*** [1.66,2.95] |
| Slightly Agree or 2nd Quartile | 3.09*** [2.38,4.02] | 3.22*** [2.47,4.19] | 3.27*** [2.48,4.32] | 1.27 [0.94,1.70] | 1.29 [0.95,1.74] | 1.28 [0.94,1.75] | 1.28 [0.92,1.78] | 1.22 [0.87,1.70] | 1.24 [0.87,1.75] |
| Slightly Disagree or 3rd Quartile | 1.93*** [1.43,2.59] | 2.01*** [1.49,2.71] | 2.15*** [1.57,2.95] | 0.95 [0.69,1.30] | 0.96 [0.69,1.33] | 0.94 [0.67,1.32] | 1.36* [1.00,1.84] | 1.32 [0.97,1.79] | 1.37 [0.99,1.89] |
| Strongly Disagree or 4th Quartile (Highest Social Capital) | Ref. | ||||||||
| Observations | 3507 | 3371 | 3129 | 3527 | 3390 | 3144 | 3586 | 3445 | 3195 |
| Log lik. | −1319.9 | −1273.4 | −1158.7 | −1367.7 | −1321.9 | −1206.9 | −1392.3 | −1344.6 | −1227.8 |
| Chi-squared | 346.2 | 341.6 | 348.9 | 291.4 | 287.3 | 295.5 | 300 | 293.1 | 304.3 |
Model 1: Controls for Demographics. Model 2: Controls for Demographics and Socio-Economics. Model 3: Controls for Demographics, Socio-Economics and Health Behavior
95% confidence intervals in brackets. Country dummies included in the model but not presented.
p < 0.05,
p < 0.01,
p < 0.001
Table 2 shows odds ratios of the association between social capital and depression. There is a consistent association with all three social capital measures, but social support seems to have the strongest association. Individuals in the lowest level of social support are over four times more likely to suffer from depression than individual in the highest level (OR=4.09, 95% CI: 3.05–5.49), and there was a graded association across the entire distribution. Contrary to the results for self-reported health, generalized trust is strongly associated with depression in all the models. Controlling for all covariates, individuals in the lowest level of generalized trust have 91% higher odds (OR=1.91, 95% CI: 1.43–2.57) of suffering from depressive symptoms than those in the highest level of generalized trust. A similar association is observed for neighborhood trust (OR=2.21, 95% CI: 1.66–2.95).
Results for diabetes and hypertension are summarized in Table 3. Social support is significantly associated with diabetes, but there is no association with generalized or neighborhood trust. Controlling for all covariates, this association is only significant for those in the lowest levels of social support (OR=1.37, 95% CI: 1.01–1.86). In contrast, there was no clear association between any measure of social capital and hypertension in any of the models examined. Although individuals in the second highest category of generalized trust are less likely to suffer from hypertension than those with higher generalized trust, this association was not consistent across other categories and social capital variables. There was no significant association for social support or neighborhood trust.
Table 3.
Odds ratios: Association between social capital (social support, generalized trust and neighborhood trust) and diabetes and hypertension, ages 30+, National Health Survey, 2009.
| Social Support | Generalized Trust | Neighborhood Trust | |||||||
|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (1) | (2) | (3) | (1) | (2) | (3) | |
| a)Diabetes | |||||||||
| Strongly Agree or Lowest Quartile (Lowest Social Capital) | 1.35* [1.01,1.82] | 1.33 [0.98,1.80] | 1.37* [1.01,1.86] | 1.06 [0.81,1.40] | 1.07 [0.81,1.41] | 1.06 [0.80,1.41] | 1.24 [0.94,1.62] | 1.25 [0.95,1.65] | 1.20 [0.90,1.58] |
| Slightly Agree or 2nd Quartile | 1.16 [0.88,1.53] | 1.13 [0.85,1.50] | 1.13 [0.84,1.51] | 0.98 [0.74,1.29] | 0.97 [0.73,1.28] | 0.91 [0.68,1.22] | 1.23 [0.91,1.67] | 1.25 [0.91,1.71] | 1.20 [0.87,1.64] |
| Slightly Disagree or 3rd Quartile | 1.19 [0.89,1.59] | 1.21 [0.90,1.63] | 1.15 [0.84,1.56] | 0.79 [0.59,1.08] | 0.76 [0.56,1.05] | 0.74 [0.54,1.02] | 1.21 [0.91,1.59] | 1.19 [0.90,1.58] | 1.16 [0.87,1.55] |
| Strongly Disagree or 4th Quartile (Highest Social Capital) | Ref. | ||||||||
| Observations | 3589 | 3470 | 3416 | 3600 | 3480 | 3425 | 3651 | 3529 | 3474 |
| Log lik. | −1360.9 | −1315.2 | −1268.5 | −1362.7 | −1315.9 | −1267.3 | −1387 | −1340.2 | −1292.5 |
| Chi-squared | 241 | 240.9 | 232 | 239 | 240 | 230.8 | 255.3 | 256.9 | 245.8 |
| b) Hypertension | |||||||||
| Strongly Agree or Lowest Quartile (Lowest Social Capital) | 1.10 [0.86,1.40] | 1.11 [0.87,1.43] | 1.18 [0.92,1.51] | 1.01 [0.81,1.25] | 1.00 [0.80,1.25] | 1.03 [0.82,1.28] | 1.03 [0.83,1.28] | 0.99 [0.80,1.23] | 1.00 [0.80,1.24] |
| Slightly Agree or 2nd Quartile | 0.94 [0.74,1.19] | 0.89 [0.70,1.13] | 0.91 [0.71,1.16] | 0.86 [0.69,1.07] | 0.85 [0.68,1.07] | 0.85 [0.68,1.07] | 1.05 [0.83,1.34] | 1.05 [0.82,1.35] | 1.05 [0.82,1.35] |
| Slightly Disagree or 3rd Quartile | 1.02 [0.81,1.28] | 1.02 [0.81,1.29] | 1.05 [0.84,1.33] | 0.78* [0.62,0.98] | 0.78* [0.61,0.98] | 0.75* [0.59,0.96] | 1.08 [0.87,1.34] | 1.04 [0.83,1.30] | 1.04 [0.84,1.31] |
| Strongly Disagree or 4th Quartile (Highest Social Capital) | Ref. | ||||||||
| Observations | 3739 | 3609 | 3555 | 3756 | 3624 | 3570 | 3813 | 3677 | 3623 |
| Log lik. | −1987.4 | −1919.5 | −1881.3 | −1996.2 | −1926.2 | −1887.8 | −2029.8 | −1958.6 | −1920.9 |
| Chi-squared | 764.9 | 743.6 | 732.9 | 765.3 | 744.2 | 732.4 | 780 | 756.4 | 745 |
Model 1: Controls for Demographics. Model 2: Controls for Demographics and Socio-Economics. Model 3: Controls for Demographics, Socio-Economics and Health Behavior
95% confidence intervals in brackets. Country dummies included in the model but not presented.
p < 0.05,
p < 0.01,
p < 0.001
Stratified Models
The estimates for the stratified models (Table 4) suggest a significant gender and age difference for self-reported health and depression. Social support and neighborhood trust are significant for women both for self-rated health (OR=2.41 and OR=1.58) and depression (OR=3.71 and OR=2.47), while the effect is non-significant for men. All indicators of social capital have significant associations with self-rated health outcomes at ages 45 and 64, while associations are weaker for younger or older age groups. Low social support is associated with higher depression prevalence at all ages, while the effect of trust indicators is significant for those below age 65, with no significant effects among the 65+. In the case of the urban and rural contrast, the effect of social capital on health seems to be similar in both scenarios. Only small differences in magnitude are found for depression.
Table 4.
Odds ratios: Association in stratified models between social capital (social support, generalized trust and neighborhood trust) and self-rated health, depression, diabetes and hypertension, ages 30+, National Health Survey, 2009.
| Gender | Age Group | Urban/Rural | |||||
|---|---|---|---|---|---|---|---|
| Female | Male | 30–44 | 45–64 | 65< | Urban | Rural | |
| Self-Reported Health | |||||||
| Low Social Support | 0.88*** [0.53,1.23] | 0.25 [−0.36,0.85] | 0.41 [−0.20,1.02] | 0.95*** [0.54,1.37] | 0.55* [0.0092,1.08] | 2.25*** [1.61,3.15] | 1.08 [0.46,2.57] |
| Low Generalized Trust | 0.2 [−0.11,0.50] | −0.11 [−0.55,0.33] | −0.15 [−0.64,0.34] | 0.43* [0.088,0.77] | −0.23 [−0.69,0.23] | 1.09 [0.81,1.47] | 1.16 [0.63,2.13] |
| Low Neighbourhood Trust | 0.45** [0.17,0.74] | 0.25 [−0.15,0.65] | 0.013 [−0.44,0.46] | 0.57*** [0.25,0.90] | 0.35 [−0.055,0.76] | 1.46** [1.10,1.94] | 1.59 [0.91,2.77] |
| Depression | |||||||
| Low Social Support | 1.31*** [1.00,1.62] | 0.19 [−0.35,0.73] | 1.03*** [0.61,1.45] | 1.03*** [0.64,1.42] | 0.81** [0.25,1.38] | 2.83*** [2.14,3.76] | 2.48* [1.05,5.84] |
| Low Generlized Trust | 0.90*** [0.65,1.14] | −0.17 [−0.55,0.21] | 0.80*** [0.49,1.11] | 0.69*** [0.39,0.98] | −0.082 [−0.55,0.38] | 1.71*** [1.35,2.15] | 2.28** [1.32,3.92] |
| Low Neighbourhood Trust | 0.91*** [0.67,1.14] | −0.027 [−0.38,0.32] | 0.66*** [0.37,0.96] | 0.71*** [0.44,0.98] | 0.36 [−0.054,0.77] | 1.89*** [1.51,2.36] | 1.83* [1.06,3.18] |
| Diabetes | |||||||
| Low Social Support | 0.21 [−0.14,0.56] | 0.37 [−0.12,0.86] | −0.86* [−1.70,−0.022] | 0.41 [−0.0047,0.82] | 0.53* [0.074,0.98] | 1.39* [1.02,1.90] | 0.78 [0.33,1.85] |
| Low Generalized Trust | 0.092 [−0.18,0.36] | 0.31 [−0.0100,0.63] | −1.23*** [−1.88,−0.58] | 0.54*** [0.27,0.82] | 0.3 [−0.049,0.65] | 1.26 [0.99,1.60] | 0.87 [0.47,1.60] |
| Low Neighbourhood Trust | 0.12 [−0.14,0.37] | −0.027 [−0.38,0.32] | −0.83*** [−1.31,−0.34] | 0.21 [−0.077,0.50] | 0.31 [−0.032,0.66] | 1.08 [0.85,1.37] | 1.02 [0.57,1.84] |
| Hypertension | |||||||
| Low Social Support | 0.062 [−0.23,0.36] | 0.33 [−0.058,0.72] | −0.91*** [−1.44,−0.38] | 0.36* [0.030,0.68] | 0.79** [0.25,1.34] | 1.16 [0.90,1.50] | 1.19 [0.64,2.22] |
| Low Generalized Trust | 0.018 [−0.20,0.23] | 0.38** [0.12,0.64] | −1.07*** [−1.42,−0.72] | 0.40*** [0.18,0.62] | 0.91*** [0.57,1.25] | 1.26* [1.05,1.53] | 0.8 [0.51,1.24] |
| Low Neighbourhood Trust | −0.16 [−0.36,0.044] | 0.13 [−0.13,0.40] | −1.17*** [−1.49,−0.86] | 0.18 [−0.038,0.39] | 0.60*** [0.28,0.92] | 0.95 [0.79,1.14] | 0.96 [0.60,1.53] |
95% confidence intervals in brackets
p < 0.05,
p < 0.01,
p < 0.001
All models control for Demographics, Socio-Economics and Health Behavior
Results for diabetes and hypertension suggest that the lack of a consistent effect for all ages in table 3 is due to offsetting patterns by age. At ages 30–44, lower social support, generalized and neighborhood trust are associated with lower diabetes and hypertension prevalence. In contrast, at ages 45–64, lower generalized trust is associated with increased diabetes and hypertension prevalence, and lower social support is associated with increased diabetes. At ages 65+, lower social support predicts higher diabetes and hypertension prevalence, and lower generalized and neighborhood trust predicts significantly higher hypertension prevalence. These findings suggest that at ages 45+, where diabetes and hypertension prevalence is highest, higher social capital is associated with higher prevalence of measured diabetes and hypertension.
Instrumental Variable Analysis
Results from first-stage IV regression models using crime victimization and aggregate social capital as separate instruments are summarized in Appendix Table 1. Victimization is a strong predictor of social support and neighborhood trust, but does not predict generalized trust levels. In contrast, average social capital is a sufficiently strong instrument for the three social capital indicators. We discuss findings from both sets of models, but we place more weight on results based on aggregate social capital, as it was a more appropriate instrument for all social capital indicators (Appendix Table 2).
Appendix Table 1.
First Stage Regression Results for Victimization
| (1) Low Social Support | (2) Low Generalized Trust | (3) Low Neighborhood Trust | |
|---|---|---|---|
| Victimization | 0.051* [0.0084,0.093] | 0.031 [−0.022,0.084] | 0.082** [0.026,0.14] |
| Age (Years) | −0.00055 [−0.0016,0.00046] | −0.00037 [−0.0018,0.0011] | −0.0016* [−0.0030,−0.00017] |
| Male | −0.029* [−0.053,−0.0058] | 0.0036 [−0.029,0.036] | −0.067*** [−0.10,−0.033] |
| Urban | 0.064*** [0.036,0.091] | 0.12*** [0.075,0.16] | 0.13*** [0.094,0.17] |
| Household Size | −0.0036 [−0.010,0.0032] | −0.00092 [−0.010,0.0085] | 0.011* [0.0018,0.021] |
| Years of Schooling | −0.0061*** [−0.0093,−0.0028] | −0.013*** [−0.017,−0.0084] | −0.011*** [−0.015,−0.0063] |
| Single | 0.0069 [−0.025,0.039] | −0.017 [−0.061,0.028] | −0.041 [−0.087,0.0044] |
| Separated or Divorced | 0.038** [0.011,0.064] | 0.038* [0.0020,0.075] | 0.046* [0.0084,0.084] |
| Widow | −0.014 [−0.052,0.024] | −0.055* [−0.11,−0.0034] | −0.069* [−0.12,−0.016] |
| US PPP $390.00–$714.99 | −0.031 [−0.063,0.00030] | −0.058** [−0.10,−0.016] | −0.061** [−0.10,−0.019] |
| US PPP $715.00–$1284.99 | −0.048** [−0.084,−0.012] | −0.080** [−0.13,−0.032] | −0.079** [−0.13,−0.030] |
| US PPP $1285< | −0.071*** [−0.11,−0.031] | −0.14*** [−0.20,−0.088] | −0.15*** [−0.21,−0.097] |
| Unemployed | 0.046 [−0.029,0.12] | 0.0021 [−0.092,0.096] | −0.023 [−0.12,0.072] |
| Retired or Disabled | −0.0045 [−0.041,0.032] | −0.0078 [−0.058,0.042] | −0.027 [−0.076,0.022] |
| Outside of the Labor Market | 0.0091 [−0.020,0.039] | 0.032 [−0.0082,0.072] | −0.019 [−0.061,0.022] |
| Average Community Income | −7.0e-09 [−0.000000032,0.000000018] | −6.1e-09 [−0.000000045,0.000000033] | −7.0e-09 [−0.000000051,0.000000037] |
| Constant | 0.20*** [0.12,0.28] | 0.39*** [0.28,0.50] | 0.47*** [0.36,0.58] |
|
| |||
| Observations | 3834 | 3851 | 3908 |
| R-squared | 0.021 | 0.034 | 0.038 |
| F-test | 6.06 | 10.3 | 11.0 |
95% confidence intervals in brackets
p < 0.05,
p < 0.01,
p < 0.001
Appendix Table 2.
First Stage Regressions Average Social Capital
| (1) Low Social Support | (2) Low Generalized Trust | (3) Low Neighborhood Trust | |
|---|---|---|---|
| Individuals with Low Social Capital in Community | 0.24*** [0.17,0.32] | 0.58*** [0.49,0.68] | 0.61*** [0.52,0.71] |
| Age (Years) | −0.00049 [−0.0015,0.00051] | −0.00025 [−0.0017,0.0012] | −0.0013 [−0.0028,0.000069] |
| Male | −0.029* [−0.052,−0.0056] | 0.0016 [−0.031,0.034] | −0.068*** [−0.10,−0.035] |
| Urban | 0.041** [0.012,0.069] | 0.059** [0.018,0.100] | 0.074*** [0.033,0.11] |
| Household Size | −0.0034 [−0.010,0.0033] | −0.0018 [−0.011,0.0075] | 0.011* [0.0016,0.020] |
| Years of Schooling | −0.0053** [−0.0085,−0.0020] | −0.011*** [−0.016,−0.0072] | −0.0091*** [−0.013,−0.0047] |
| Single | 0.0085 [−0.023,0.040] | −0.014 [−0.058,0.030] | −0.037 [−0.081,0.0077] |
| Separated or Divorced | 0.038** [0.012,0.065] | 0.038* [0.0023,0.073] | 0.047* [0.010,0.084] |
| Widow | −0.011 [−0.048,0.026] | −0.053* [−0.10,−0.0023] | −0.060* [−0.11,−0.0085] |
| US PPP $390.00–$714.99 | −0.029 [−0.060,0.0027] | −0.053* [−0.095,−0.012] | −0.054* [−0.095,−0.013] |
| US PPP $715.00–$1284.99 | −0.047** [−0.083,−0.012] | −0.077** [−0.12,−0.030] | −0.076** [−0.12,−0.028] |
| US PPP $1285< | −0.065** [−0.10,−0.025] | −0.13*** [−0.18,−0.075] | −0.13*** [−0.19,−0.076] |
| Unemployed | 0.055 [−0.022,0.13] | −0.0042 [−0.100,0.091] | −0.027 [−0.12,0.067] |
| Retired or Disabled | −0.0027 [−0.039,0.034] | −0.0055 [−0.054,0.043] | −0.025 [−0.074,0.023] |
| Outside of the Labor Market | 0.0086 [−0.021,0.038] | 0.030 [−0.0095,0.069] | −0.020 [−0.060,0.021] |
| Average Community Income | 0.000000011 [−0.000000014,0.000000036] | 0.000000038 [−2.1e-10,0.000000075] | 0.000000038 [−6.5e-09,0.000000083] |
| Constant | 0.077 [−0.0061,0.16] | 0.10 [−0.0099,0.22] | 0.16** [0.044,0.28] |
|
| |||
| Observations | 3845 | 3864 | 3923 |
| R-squared | 0.031 | 0.067 | 0.070 |
| F-test | 8.50 | 20.2 | 21.9 |
95% confidence intervals in brackets
p < 0.05,
p < 0.01,
p < 0.001
Results for the IV estimation are summarized in Table 5, alongside results from a regular OLS model. Estimates correspond to the effect of a one-point increase in social support; generalized trust and neighborhood trust scores on each outcome. Standard errors increase considerably yielding some non-significant estimates. Using victimization as an instrument, we find no significant effect of any social capital indicator on self-rated health, yet estimates are positive in all models and substantially larger in the IV as compared to the OLS model. IV models support the hypothesis of a causal effect of social support and neighborhood trust on depression. A one-point increase in social support was associated with a marked increase in the risk of depression (Beta=2.33, 95% CI: 0.27–4.39). Similarly, a one-point increase in neighborhood trust scores was associated with a significant increase in depression risk (Beta=1.33, 95% CI: 0.30–2.26). We found no evidence of a causal effect of any social capital indicator on diabetes and hypertension prevalence.
Table 5.
Coefficients: IV analysis using victimization and average social capital, ages 30+, National Health Survey, 2009.
| OLS | Social Support IV- Victimization |
IV-Average Social Capital |
OLS | Generalized Trust IV- Victimization |
IV-Average Social Capital |
OLS | Neighborhood Trust IV- Victimization |
IV-Average Social Capital |
|
|---|---|---|---|---|---|---|---|---|---|
| a) Self-reported health | 0.066*** [0.032,0.10] | 0.40 [−0.27,1.08] | 0.10 [−0.14,0.35] | 0.0075 [−0.013,0.028] | 0.62 [−0.85,2.10] | 0.04 [−0.069,0.14] | 0.031** [0.012,0.050] | 0.25 [−0.17,0.66] | 0.02 [−0.081,0.12] |
| b) Depression | 0.15*** [0.11,0.20] | 2.33* [0.27,4.39] | 0.67*** [0.28,1.06] | 0.087*** [0.057,0.12] | 10.00 [−41.5,61.6] | 0.26*** [0.11,0.40] | 0.093*** [0.067,0.12] | 1.33* [0.30,2.36] | 0.27*** [0.13,0.41] |
| c) Diabetes | 0.03 [−0.0083,0.067] | −0.26 [−1.15,0.63] | 0.31 [−0.037,0.67] | 0.02 [−0.0085,0.044] | −0.95 [−5.14,3.24] | 0.13 [−0.0024,0.26] | 0.01 [−0.012,0.037] | −0.15 [−0.63,0.34] | 0.13* [0.0039,0.26] |
| d)Hypertension | 0.02 [−0.022,0.065] | 0.54 [−0.56,1.63] | 0.44* [0.024,0.86] | 0.03 [−0.0050,0.058] | 1.14 [−1.76,4.05] | 0.18* [0.0039,0.35] | −0.0024 [−0.032,0.028] | 0.31 [−0.28,0.90] | 0.17* [0.0077,0.33] |
95% confidence intervals in brackets
p < 0.05,
p < 0.01,
p < 0.00
All models control for Demographics, Socio-Economics, Health Behavior and Community Confounders.
Estimates from models based on community social capital are summarized in Table 5 for each indicator. Consistent with results for victimization, we found no evidence of an effect on self-rated health, but strong and consistent effects on depression for all social capital indicators. We also find that lower neighborhood trust is associated with increased diabetes prevalence, while social support and generalized trust are unrelated to diabetes. Contrary to models based on victimization, we now find a consistent and strong effect of social support, generalized trust and neighborhood trust on hypertension prevalence using aggregate social capital as an instrument.
The stratified analyses and IV models address separate issues. The results for the stratified analysis correspond to an evaluation of the impact that social capital across different sub-groups such as gender and age. In contrast, the IV models address the issue of causality by using an exogenous source of variation in the exposure. Results from the IV model are sometimes different than those from regular models, however several potential explanations are included in the discussion.
Discussion
Our study finds that social capital may be an important determinant of mental health. Estimates suggest significant and strong associations between all social capital indicators and depression, which remain strong in IV models. Our findings are consistent with previous evidence from the Netherlands that social capital is more strongly associated with mental than physical health (Drukker et al., 2003), and further suggest that this pattern may be consistent for middle-income countries as well. The potential causal association between social capital and mental health is further supported by recent findings in a twin fixed effect study (Fujiwara & Kawachi, 2008).
At least two possible explanations may account for this finding. First, subjective assessments of mental well-being may be correlated with subjective assessments of social capital due to reverse causality. That is, individuals suffering from depressive symptoms may be more likely to perceive low trust in their neighborhood and perceive lower levels of social support. Results from the IV models, which use potentially exogenous variation in social capital stemming from the timing of crime experiences and aggregate social capital, suggest that this interpretation may not account for our findings for mental health as estimates remain strong and significant. A second possible explanation is that lower social capital catalyzes the deterioration of mental health by directly influencing the ability of individuals to relate satisfactorily to others, increasing loneliness and leading to poorer expectations about the future (Kawachi, 1999; Ostrom, 2003; Ostrom & Ahn, 2009; Putnam, 1993). These effects may be less evident for self-rated health as the latter also reflects physical health, which may be less sensitive to the influence of social capital measures included in our study.
Although we did not find consistent effects of social capital on self-rated health, our results suggest that some forms of social capital may be particularly important for the development of cardiovascular risk (i.e. hypertension and diabetes). Results are suggestive of an effect of social capital on health that is not driven by subjective reporting bias. Previous studies have found a significant association between social capital and cardiovascular disease outcomes (Hyyppa et al., 2007; Kawachi et al., 1997; Lynch et al., 2001). Several mechanisms may account for this association. Social capital may exert an influence on health-related behavior. Indeed, previous evidence suggests that social capital is associated with the reduced prevalence of poor health habits, including substance abuse, unhealthy diet and smoking (Lindstrom, 2003; Poortinga, 2006; Weitzman & Chen, 2005; Weitzman & Kawachi, 2000). It is important to note that strong cohesion could be equally plausibly linked with bad behaviors (such as smoking), depending on the context. In other words, if the local norm is that the majority of people smoke, then an individual belonging to that group will be conforming to the social norm (as an expression of solidarity) by smoking. On the other hand, if local norms discourage smoking (or other substance abuse such as binge drinking) then strong social capital is likely to suppress such expressions of “deviant” behavior via informal social control. In contrast to the explanation based on social influence, our results could be equally consistent with the possibility of a direct psychobiological pathway between social capital and health, whereby social capital may moderate the effects of chronic stress and prevent the onset of hypertension or other stress-related pathways leading to enhanced cardiovascular risk (Steptoe et al., 2009; Steptoe & Feldman, 2001; Viswanath et al., 2006).
We found that the impact of social support on depression appears to be stronger and more consistent for woman than for men. Other studies have found results both in favor and against gender differences. For instance, while social support seems to have a stronger impact on well-being for women (Antonucci & Akiyama, 1987), social support has been found to be more strongly associated with self-reported health in men (Ferlander & Makinen, 2009). Our findings seem to confirm that social support has a larger impact in the psychological dimension for women. Two factors may explain this finding. First, evidence suggests that women depend more on family-based social capital (O’Neill & Gidengil, 2006), particularly emotional social support. Second, women usually have larger social networks and receive social support from multiple sources (Antonucci & Akiyama, 1987). The establishment of these networks requires a certain level of trust that, if unmet, will limit the potential sources from where individuals receive social support. This possibility is consistently supported by the social capital literature on trust and reciprocity (Ostrom, 2003).
We found that social capital has similar effects on depression at all ages, but effects on diabetes and hypertension are only evident at ages 45 and older. On the one hand, this pattern may reflect the increasing importance of reverse causality at older ages, as ill individuals may be more likely to report poorer social capital. On the other hand, the fact that effects for diabetes and hypertension remain significant in IV models, suggests that reverse causality is not the key explanation. Instead, these findings may reflect the fact that cardiovascular risk develops over long-periods of cumulative exposure, so that effects of social capital may only be evident at relatively old ages. While hypertension and diabetes below age 45 may be indicative of early cardiovascular risk, their occurrence at such young age may reflect more the influence of other biological factors rather than result from cumulative disadvantage associated with life-time exposure to low social capital. Our results therefore highlight the particular relevance of social capital for healthy ageing.
The results from the IV analyses provide some suggestive evidence of a causal relationship between social capital and health. IV estimates suggest that lower levels of social capital lead to higher probabilities of suffering from depression, diabetes and hypertension. A potential concern is that IV estimates are considerably larger than OLS estimates. This is not uncommon (Angrist & Pischke, 2009; Imberis & Angrist, 1994) and suggests that IV estimates may correspond to the Local Average Treatment Effect (LATE), i.e., the effect of individual social capital on the subpopulation affected by community social capital or crime victimization (the instruments), corresponding to those individuals whose effects of social capital on health are likely to be the largest. This may explain to some extent the differences in significance between the IV and stratified model results. Although the exogeneity assumption can never be fully tested, the F-test and Durbin-Wu-Hausman test confirm the applicability of the IVs method and the instruments validity. Nevertheless, it is not implausible that victimization has a direct impact on health and even though we argue that most of the effect will occur through the reduction of social capital future research based on other instruments is required to assess the extent to which associations between social capital and markers of cardiovascular disease are causal.
The study design has several strengths. In particular, the analysis is based on a harmonized national cross-sectional survey that contains both reported and objective measurements of health for a nationally representative sample of the population. This study has extended previous analyses of outcomes such as depression, diabetes and hypertension to a more comprehensive sample of the population. Additionally, evaluating different health outcomes in the same study has reduced the reporting heterogeneity that has been extensively discussed in relation to self-reported health (Jurges, Avendano, & Mackenbach, 2008). Furthermore, while many studies using surveys have the problem of non-response, the high response rate of the survey used for this study significantly reduces the possible bias.
Despite these strengths, our study also has several limitations. First, it was based on a selected set of social capital indicators; findings may differ when using other measures of social capital. Second, it is based on cross-sectional data, making it impossible to fully assess the causal effect of social capital on health using a more dynamic approach. To our knowledge, this is the first study to assess links between social capital and early markers of cardiovascular disease in a middle-income country. However, Chile has experienced a major economic expansion and transformation of the welfare state during the last two decades, so the results for the Chilean population may not be generalizable to other middle-income countries. Nevertheless, the fact that we were able to reproduce some of the associations observed in high-income countries may add to evidence on the universality of the association between social capital and health. Further studies should nevertheless examine whether this association reflects a causal effect or whether it may be the result of selection of confounding mechanisms. Lastly, using victimization as an instrument is a limitation in the extent that its exogeneity with mental health may be questioned. We have argued throughout that the direct effect of victimization on mental health is mediated through social capital dimensions such as neighborhood and general trust. Nevertheless, this instrument does not allow us to disentangle to what extent we are capturing this effect and not the direct effect on mental health.
Conclusion
Results from this study suggest that there is an association between social capital and mental health, as well as between some measures of social capital and early markers of cardiovascular risk. If results in our IV approach are replicated in other studies, our findings may suggest that changes in social capital may lead to changes in mental and physical health outcomes. Social capital is an asset that individuals can access by participating in a network within an established set of norms, which in turn allows for efficient collective actions (Putnam, 1993). Our findings highlight the fact that collective actions that improve social capital may lead to significant population health improvements. Results indicate that this pattern is particularly strong for mental health, and to some extent for early markers of cardiovascular disease risk. Policies that increase social capital may thus benefit societies that are currently experiencing a rapid process of economic and social transition, as is the case in several Latin American countries that have only in the last decades started to expand their social protection systems.
Highlights.
This study evaluates the association of social capital with both self-rated and biologically assessed health outcomes.
Findings suggest that social capital has a causal effect on depression.
Evidence that social capital may be causally associated with early markers of cardiovascular risk.
Our finding highlight the potential role of social capital in the prevention of depression and early cardiovascular disease.
Acknowledgments
This study used information from the Chilean National Health Survey 2009–2010. The author thanks the Ministry of Health, intellectual owner of the survey, for allowing the use of the database. Mauricio Avendano was supported by a Starting Researcher grant from the European Research Council (ERC) (grant No 263684) and a grant from the National Institute of Ageing (R01AG037398). All the study results are the responsibility of the author and do not represent the opinion of the Ministry.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Altschuler A, Somkin CP, Adler NE. Local services and amenities, neighborhood social capital, and health. Social Science & Medicine. 2004;59:1219–1229. doi: 10.1016/j.socscimed.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Angrist JD, Pischke JS. Instrumental variables in action: sometimes you get what you need. In: Angrist JD, Pischke JS, editors. Mostly Harmless Econometrics: An Empiricists Companion. New Jersey: Princeton University Press; 2009. pp. 113–220. [Google Scholar]
- Antonucci TC, Akiyama H. An examination of sex-differences in social support among older men and women. Sex Roles. 1987;17:737–749. [Google Scholar]
- Aye M, Champagne F, Contandriopoulos AP. Economic role of solidarity and social capital in accessing modern health care services in the Ivory Coast. Social Science & Medicine. 2002;55:1929–1946. doi: 10.1016/s0277-9536(01)00322-7. [DOI] [PubMed] [Google Scholar]
- Becker G, Murphy K, editors. Social economics: Market behaviour in a social environment. Cambridge: Belknap Press; 2000. [Google Scholar]
- Blakely T, Atkinson J, Ivory V, Collings S, Wilton J, Howden-Chapman P. No association of neighbourhood volunteerism with mortality in New Zealand: a national multilevel cohort study. International Journal of Epidemiology. 2006;35:981–989. doi: 10.1093/ije/dyl088. [DOI] [PubMed] [Google Scholar]
- Bourdieu P. The forms of capital. In: Richardson J, editor. Handbook of Theory and Research in the Sociology of Education. New York: Greenwood Press; 1986. pp. 241–258. [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Archives Internal Medicine. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Chobanian A, Bakris G, Black H, Cushman W, Green L, Izzo J, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Coleman A, Freeman P, Steel S, Shennan A. Validation of the Omron MX3 Plus oscillometric blood pressure monitoring device according to the European Society of hypertension international protocol. Blood Press Monit. 2005;10:165–168. doi: 10.1097/00126097-200506000-00009. [DOI] [PubMed] [Google Scholar]
- Drukker M, Gunther N, Feron FJM, van Os J. Social capital and mental health: objective measures of health in the Netherlands. British Journal of Psychiatry. 2003;183:174–174. doi: 10.1192/bjp.183.2.174. [DOI] [PubMed] [Google Scholar]
- Ewig C, Palmucci GA. Inequality and the politics of social policy implementation: gender, age and Chile’s 2004 health reforms. World Development. 2012;40:2490–2504. [Google Scholar]
- Ferlander S, Makinen IH. Social capital, gender and self-rated health. Evidence from the Moscow Health Survey 2004. Social Science & Medicine. 2009;69:1323–1332. doi: 10.1016/j.socscimed.2009.08.009. [DOI] [PubMed] [Google Scholar]
- Franzini L. Self-rated health and trust in low-income Mexican-origin individuals in Texas. Social Science & Medicine. 2008;67:1959–1969. doi: 10.1016/j.socscimed.2008.09.030. [DOI] [PubMed] [Google Scholar]
- Fujiwara T, Kawachi I. Social capital and health: a study of adult twins in the U.S. American Journal of Preventive Medicine. 2008;35:139–144. doi: 10.1016/j.amepre.2008.04.015. [DOI] [PubMed] [Google Scholar]
- Gfk. Informe Mensual. Santiago: ADIMARK; 2012. Encuesta: evaluacion gestion del gobierno. [Google Scholar]
- Glaeser E, Laibson D, Sacerdote B. The economic approach to social capital. Economic Journal. 2002;112:437–458. [Google Scholar]
- Gold M, Franks P, Erickson P. Assessing the health of the nation - The predictive validity of a preference-based measure and self-rated health. Medical Care. 1996;34:163–177. doi: 10.1097/00005650-199602000-00008. [DOI] [PubMed] [Google Scholar]
- Harpham T. The measurement of community social capital through surveys. In: Kawachi I, Subramanian SV, Kim D, editors. Social Capital and Health. New York: Springer; 2008. pp. 51–62. [Google Scholar]
- Harpham T, Grant E, Rodriguez C. Mental health and social capital in Cali, Colombia. Social Science & Medicine. 2004;58:2267–2277. doi: 10.1016/j.socscimed.2003.08.013. [DOI] [PubMed] [Google Scholar]
- Holtgrave DR, Crosby R. Is social capital a protective factor against obesity and diabetes? Findings from an exploratory study. Annals of Epidemiology. 2006;16:406–408. doi: 10.1016/j.annepidem.2005.04.017. [DOI] [PubMed] [Google Scholar]
- Hurtado D, Kawachi I, Sudarsky J. Social capital and self-rated health in Colombia: The good, the bad and the ugly. Social Science & Medicine. 2011;72:584–590. doi: 10.1016/j.socscimed.2010.11.023. [DOI] [PubMed] [Google Scholar]
- Hyyppa MT, Maki J, Impivaara O, Aromaa A. Individual-level measures of social capital as predictors of all-cause and cardiovascular mortality: a population-based prospective study of men and women in Finland. European Journal of Epidemiology. 2007;22:589–597. doi: 10.1007/s10654-007-9153-y. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Imberis G, Angrist JD. Identification and estimation of local average treatment effects. Econometrica. 1994;62:467–475. [Google Scholar]
- Islam MK, Merlo J, Kawachi I, Lindstrom M, Burstrom K, Gerdtham UG. Does it really matter where you live? A panel data multilevel analysis of Swedish municipality-level social capital on individual health-related quality of life. Health Economics, Policy and Law. 2006;1:209–235. doi: 10.1017/S174413310600301X. [DOI] [PubMed] [Google Scholar]
- Kawachi I. Social capital and community effects on population and individual health. Socioeconomic Status and Health in Industrial Nations. 1999;896:120–130. doi: 10.1111/j.1749-6632.1999.tb08110.x. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Berkman L. Social cohesion, social capital, and health. Social Epidemiology. 2000:170–190. [Google Scholar]
- Kawachi I, Kennedy BP, Glass R. Social capital and self-rated health: a contextual analysis. American Journal of Public Health. 1999;89:1187–1193. doi: 10.2105/ajph.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Kennedy BP, Lochner KA, Prothrowstith D. Social capital, income inequality, and mortality. American Journal of Public Health. 1997;87:1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy BP, Kawachi I, Brainerd E. The role of social capital in the Russian mortality crisis. World Development. 1998;26:2029–2043. [Google Scholar]
- Kennelly B, O’Shea E, Garvey E. Social capital, life expectancy and mortality: a cross-national examination. Social Science & Medicine. 2003;56:2367–2377. doi: 10.1016/s0277-9536(02)00241-1. [DOI] [PubMed] [Google Scholar]
- Kessler R, Andrew G, Mroczek D, Ustun T, Wittchen H. Composite international diagnostic interview short form. International Journal of Methods in Psychiatric Research. 1998;7:171–185. [Google Scholar]
- Kim D, Baum CF, Ganz ML, Subramanian SV, Kawachi I. The contextual effects of social capital on health: A cross-national instrumental variable analysis. Social Science & Medicine. 2011;73:1689–1697. doi: 10.1016/j.socscimed.2011.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Subramanian SV, Gortmaker SL, Kawachi I. US state- and county-level social capital in relation to obesity and physical inactivity: A multilevel, multivariable analysis. Social Science & Medicine. 2006;63:1045–1059. doi: 10.1016/j.socscimed.2006.02.017. [DOI] [PubMed] [Google Scholar]
- Kim D, Subramanian SV, Kawachi I. Social Capital and physical health: A systematic review of the literature. In: Kawachi I, Subramanian SV, Kim D, editors. Social Capital and Health. New York: Springer; 2008. pp. 139–190. [Google Scholar]
- Kumar S, Calvo R, Avendano M, Sivaramakrishnan K, Berkman LF. Social support, volunteering and health around the world: cross-national evidence from 139 countries. Social Science & Medicine. 2012;74:696–706. doi: 10.1016/j.socscimed.2011.11.017. [DOI] [PubMed] [Google Scholar]
- Lindstrom M. Social capital and the miniaturization of community among daily and intermittent smokers: a population-based study. Preventive Medicine. 2003;36:177–184. doi: 10.1016/s0091-7435(02)00049-x. [DOI] [PubMed] [Google Scholar]
- Lindstrom M, Axen E, Lindstrom C, Beckman A, Moghaddassi M, Merlo J. Social capital and administrative contextual determinants of lack of access to a regular doctor: a multilevel analysis in southern Sweden. Health Policy. 2006;79:153–164. doi: 10.1016/j.healthpol.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Lochner, Kawachi, Brennan, Buka Social capital and neighborhood mortality rates in Chicago. Social Science & Medicine. 2003;56:1797–1805. doi: 10.1016/s0277-9536(02)00177-6. [DOI] [PubMed] [Google Scholar]
- Lopez R, Miller SJ. Chile: The unbearable burden of inequality. World Development. 2008;36:2679–2695. [Google Scholar]
- Lynch J, Smith GD, Hillemeier M, Shaw M, Raghunathan T, Kaplan G. Income inequality, the psychosocial environment, and health: comparisons of wealthy nations. Lancet. 2001;358:194–200. doi: 10.1016/S0140-6736(01)05407-1. [DOI] [PubMed] [Google Scholar]
- Mesa-Lago C. Social security in Latin America - Pension and health care reforms in the last quarter century. Latin American Research Review. 2007;42:181–201. [Google Scholar]
- Salud MD, editor. MINSAL. Informe ENS 2009. Santiago: 2009. [Google Scholar]
- Mohseni M, Lindstrom M. Social capital, trust in the health-care system and self-rated health: the role of access to health care in a population-based study. Social Science & Medicine. 2007;64:1373–1383. doi: 10.1016/j.socscimed.2006.11.023. [DOI] [PubMed] [Google Scholar]
- Mulvaney-Day NE, Alegria M, Sribney W. Social cohesion, social support, and health among Latinos in the United States. Social Science & Medicine. 2007;64:477–495. doi: 10.1016/j.socscimed.2006.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ. 2001;322:531–536. doi: 10.1136/bmj.322.7285.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill BL, Gidengil E. Gender and social capital. New York: Routledge; 2006. [Google Scholar]
- Ostrom E. Toward a behavioral theory linking trust, reciprocity, and reputation. Trust and Reciprocity. 2003;6:19–79. [Google Scholar]
- Ostrom E, Ahn TK. The meaning of social capital and its link to collective action. In: Tinggaard G, Lind Hasse G, editors. Handbook of Social Capital: The Troika of Sociology, Political Science and Economics. Cheltenham: Edward Elgar Publishing Limited; 2009. pp. 17–35. [Google Scholar]
- Poortinga W. Do health behaviors mediate the association between social capital and health? Preventive Medicine. 2006;43:488–493. doi: 10.1016/j.ypmed.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Putnam RD. Making democracy work : civic traditions in modern Italy. Princeton, N.J: Princeton University Press; 1993. [Google Scholar]
- Rioseco P, Saldivia S, Kohn R, Torres S. Chilean study on the prevalence of psychiatric disorders (DSM-III-R/CIDI) (ECPP) Revista Medica de Chile. 2002;130:527–536. [PubMed] [Google Scholar]
- Rocco L, Suhrcke M. Is social capital good for health? A European perspective. Copenhaguen: WHO Regional Office for Europe; 2012. [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sapag JC, Aracena M, Villarroel L, Poblete F, Berrocal C, Hoyos R, et al. Social capital and self-rated health in urban low income neighbourhoods in Chile. Journal of Epidemiology and Community Health. 2008;62:790–792. doi: 10.1136/jech.2006.052993. [DOI] [PubMed] [Google Scholar]
- Siahpush M, Singh GK. Social integration and mortality in Australia. Australian and New Zealand Journal of Public Health. 1999;23:571–577. doi: 10.1111/j.1467-842x.1999.tb01539.x. [DOI] [PubMed] [Google Scholar]
- Sirven N, Debrand T. Social participation and healthy ageing: An international comparison using SHARE data. Social Science & Medicine. 2008;67:2017–2026. doi: 10.1016/j.socscimed.2008.09.056. [DOI] [PubMed] [Google Scholar]
- Sirven N, Debrand T. Social Capital and health of older europeans: Individual Pathways to Health Inequalities. Gerontologist. 2011;51:217–217. doi: 10.1016/j.socscimed.2012.05.009. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Dockray S, Wardle J. Positive affect and psychobiological processes relevant to health. Journal of Personality. 2009;77:1747–1776. doi: 10.1111/j.1467-6494.2009.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23:177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Kawachi I, Kennedy BP. Does the state you live in make a difference? Multilevel analysis of self-rated health in the US. Social Science & Medicine. 2001;53:9–19. doi: 10.1016/s0277-9536(00)00309-9. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Lochner KA, Kawachi I. Neighborhood differences in social capital: a compositional artifact or a contextual construct? Health & Place. 2003;9:33–44. doi: 10.1016/s1353-8292(02)00028-x. [DOI] [PubMed] [Google Scholar]
- Takagi D, Ikeda K, Kawachi I. Neighborhood social capital and crime victimization: Comparison of spatial regression analysis and hierarchical regression analysis. Social Science & Medicine. 2012;75:1895–1902. doi: 10.1016/j.socscimed.2012.07.039. [DOI] [PubMed] [Google Scholar]
- van Ginneken W, editor. Social security for the excluded majority: Case studies of developing countries. Geneva: International Labour Office; 1999. [Google Scholar]
- Viswanath K, Steele WR, Finnegan JR. Social capital and health: Civic engagement, community size, and recall of health messages. American Journal of Public Health. 2006;96:1456–1461. doi: 10.2105/AJPH.2003.029793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman ER, Chen YY. Risk modifying effect of social capital on measures of heavy alcohol consumption, alcohol abuse, harms, and secondhand effects: national survey findings. Journal of Epidemiology and Community Health. 2005;59:303–309. doi: 10.1136/jech.2004.024711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman ER, Kawachi I. Giving means receiving: The protective effect of social capital on binge drinking on college campuses. American Journal of Public Health. 2000;90:1936–1939. doi: 10.2105/ajph.90.12.1936. [DOI] [PMC free article] [PubMed] [Google Scholar]