Abstract
Background:
To determine the adequacy of resources (human and material) for provision of maternal health services at the primary health care (PHC) level in Nnewi, Nigeria.
Materials and Methods:
A cross-sectional study of women utilising maternal health services in four public PHC facilities in Nnewi selected using multistage sampling technique was done. Data was collected using a mix of quantitative and qualitative methods. Quantitative data was analysed using statistical package for social sciences (SPSS) version 16, while qualitative data was reported verbatim, analysed thematically and necessary quotes presented.
Results:
Two hundred and eighty women were studied. The mean age of respondents was 29.2 ± 5.9 years, while 231 (82.5%) were married. Most of them (82.5%) and 184 (66.1%), had their blood pressure and body weight respectively measured, while 196 (70.0%) had tetanus toxoid vaccination. Less than half of the respondents (41.4%) had urine test for sugar, and protein, while 94 (33.8%) had blood test for anaemia. The four facilities studied had most of the equipment and drugs available but in insufficient quantities. In three out of the four facilities, the physical structures were mostly good. None of them is equipped to provide an essential obstetric care (EOC) services, while one medical doctor covered all the facilities studied.
Conclusions:
This study showed that none of the health facilities is equipped with the minimum equipment package, essential drugs nor staff complement required to enable them offer quality maternal health services. With advocacy, technical support and funding, strategies could be implemented to provide quality maternal health services.
Keywords: Adequacy, maternal health care services, primary health care level, resource provision
INTRODUCTION
There is demand as well as supply side of barriers to maternal health care services. When inadequacies exist, a balance may not be met between health services demand and supply. In most health facilities in developing countries health services are often not available. The service delivery point may not be open at the right time or supplies may not be adequate, as such, clients do not receive services of their choices when needed.1 Likewise, where health personnel are available they may not be in adequate proportion with the catchment population, not skilled or not trained and retrained on the necessary skills required to offer the needed quality services.2
An evaluation report on the primary health care (PHC) systems project in 10 local government areas (LGAs) in Katsina, Kebbi and Oyo states of Nigeria, shows that the performance of health systems is dependent on adequacy of resources and health infrastructure.3 Adeniyi et al.,4 in a 2001 study on the status of PHC in Nigeria and other authors have revealed inadequacies of staff, drugs and equipment at the first level health facilities.5,6 Olumide et al.,6 in a needs assessment survey carried out in Nigeria, by the National Primary Health Care Development Agency (NPHCDA) revealed that none of the sampled LGAs met the minimum standard of providing all the basic PHC services. Decline in health care quality and poor health development indicators have also been attributed to inadequacies such as rudimentary or absent managerial skill, shortage of staff, drugs, essential equipment, supplies and inadequacies in the contents of maternal health care services.3,7,8,9,10,11 The NPHCDA thus recommends a minimum staff, drugs, equipment and supplies complement for PHC centres.12
The fifth goal of the Millennium Declaration emphasises the need for the provision of quality maternal health services in order to reduce maternal mortality.13 In 1988, Nigeria adopted a National Health Policy aimed at achieving health for all Nigerians by the year 2000 and beyond using primary health care as the basis for development. The maternal mortality ratio in Nigeria remains one of the highest in the West African sub-region and yet the various efforts which have been made to reduce it have not yielded much fruit, as women are still dying from pregnancy related causes.6 There is need to assess the quality of maternal health care services at PHC level; to determine the adequacy of human and material resources for provision of these services in the PHC centres in Nnewi North LGA. It is expected that the findings of this study will guide recommendations and serve as a basis for further studies, policy formulation and putting in place appropriate intervention strategies towards the improvement of the quality of maternal health services in Nigeria.
MATERIALS AND METHODS
This was a cross-sectional descriptive study of women utilizing maternal health care services (at least three of the maternal health services viz., family planning, antenatal care, safe delivery services, postnatal care services and basic essential obstetric care) in public PHC facilities in Nnewi North local government area (LGA) in Eastern Nigeria, using a stratified (multistage) sampling technique.
Data collection technique
Data collection in this study employed a mix of quantitative (Client Exit Interviews and Observation Checklist) and qualitative (Focus Group Discussion and Key Informant Interview) methods.
Sampling technique
Stage I: A simple random sampling technique applying balloting system was used to select one health facility from each of these four administrative zones of the LGA.
Stage II: Then the sample size determined was proportionately allotted to the 4 health centres based on the average number of clients that presented for antenatal care at this facility within the period of the study.
Stage III: Based on the average for the 3 months preceding the month of the study, the total monthly antenatal attendance for the four facilities was 300. The total number of clients that was interviewed for each health facility was calculated thus:
Stage IV: Then, eligible and consenting respondents utilising maternal health services were recruited consecutively by systematic sampling technique at the point of exit from the health facilities until the required number allotted to each selected facility has been obtained.
Data management and analysis
Quantitative data was analysed using statistical package for social sciences (SPSS) version 16.
Ethical consideration
Approval to conduct the study was obtained from the Ethical Committee, while permission was obtained from the State Ministry of Health.
Limitations of the study
The client exit interviews questionnaires were interviewer administered and this might have influenced the responses from the participants. However, in the training of research assistants it was ensured that efforts were made by these research assistants to assure respondents of confidentiality of their responses. Qualitative data and results of the observation checklist were also used to cross-check the quantitative results obtained from the questionnaires. The findings of the study may not be generalised to give a comprehensive perspective of quality in the LGA as it is a public facility based. However, the study was designed to gauge government's preparedness to meet the MDG5.
RESULTS
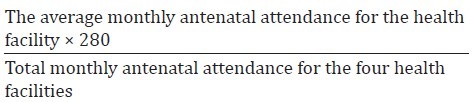
Table 1 summarises the socio- demographic characteristics of respondents. A total of 280 women were interviewed. The mean age of the respondents was 29.2 ± 5.9 years. Majority of the respondents, 231 (82.5%) were married while most of them, 216 (77.2%) attained at least secondary level of education, only 7 (2.5%) did not have any formal education.
Table 1.
Socio-demographic characteristics of the respondents studied
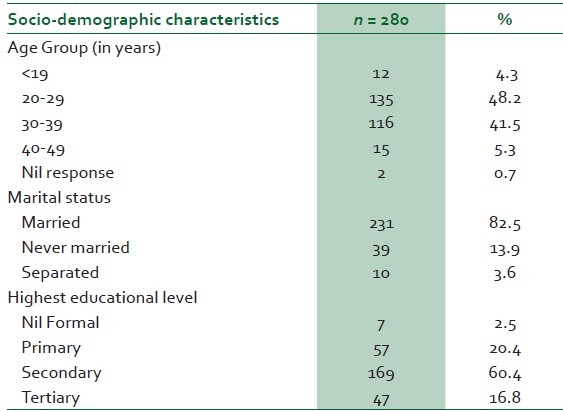
Table 2 summarises the components of maternal health services received by the respondents. Most of them (82.5%) and (66.1%), had their blood pressure and body weight, respectively, measured, while (77.9%) received advice on drugs/supplements, (70.0%) had tetanus toxoid vaccination, (65.8%), received health education on nutrition and (61.1%) had malaria prophylaxis. Less than half of the respondents (41.4%) had urine test for sugar, and protein, while (33.8%) had blood test for anaemia. The only components of EOC observed at the facilities studied are parenteral administration of oxytocics; parenteral administration of antibiotics and manual removal of placenta.
Table 2.
Components of maternal health care services provided to clients
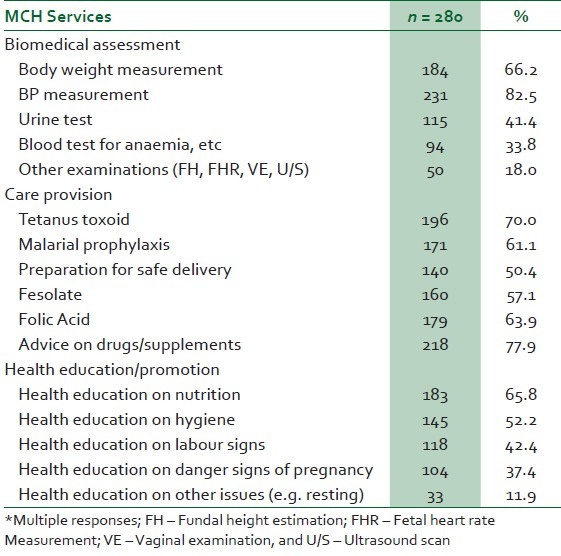
Table 3 summarises the availability of equipment for the provision of maternal health services in the facilities studied. All the four health centres had most of the equipment except for the following; none of them had a mackintosh screen, one out of the four facilities had a dressing trolley, half of the four facilities had beds with mackintosh, while three out of the four facilities had weighing scale both bathroom and infant and shakir's strip.
Table 3.
Availability of equipment
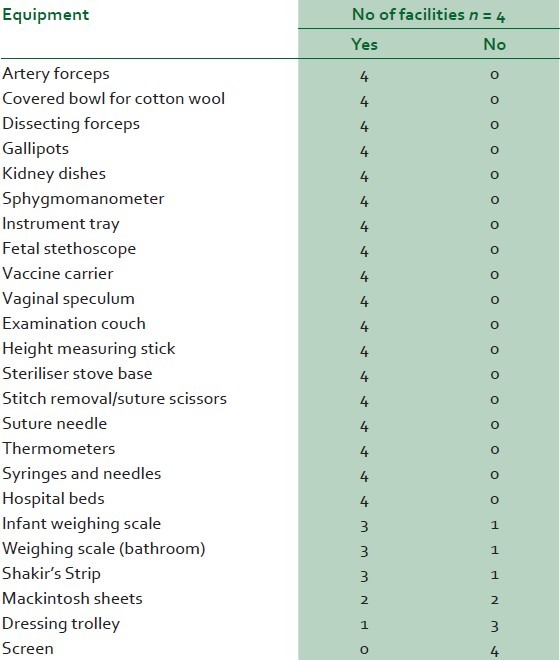
Table 4 summarises the availability of essential drugs in the facilities studied. Most of the drugs were available but in insufficient quantities except for ergometrine injection, gentian violet solution and oral rehydration salt. All the health care facilities assessed had consumables, which included needles and syringes, cotton wool, latex gloves, antiseptic lotion and sutures.
Table 4.
Availability of essential drugs
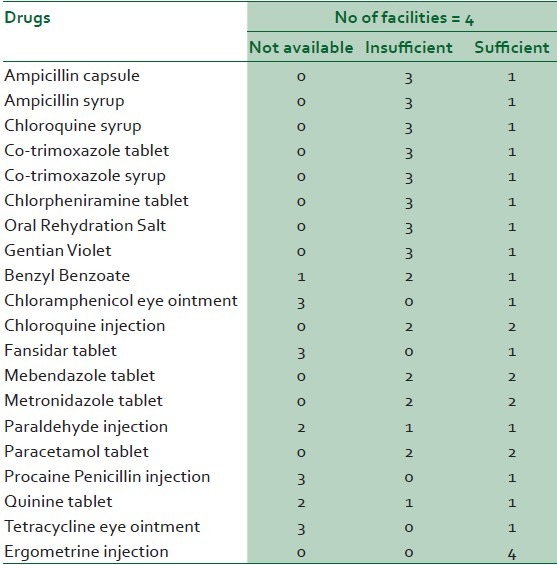
Table 5 summarises the physical infrastructure in the health facilities studied. In most of the health facilities their physical structures were mostly good or acceptable on observation according to the established guideline. Also, room size and furniture were good in three out of the four facilities; however, only two had adequate ventilation and chairs.
Table 5.
Physical infrastructure
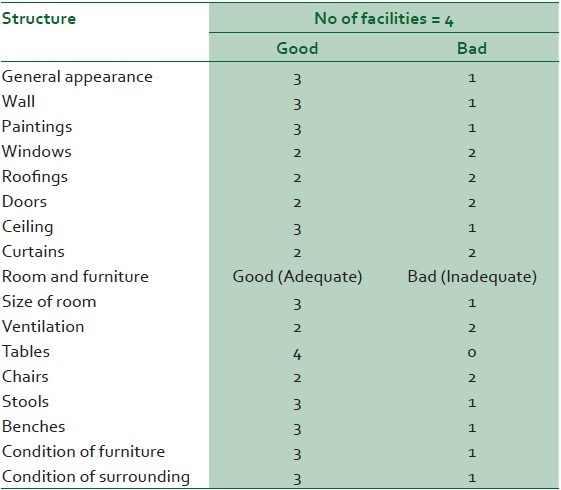
Figure 1 shows the amenities available and the level of sanitation in the facilities studied. Water closet was the common form of sewage disposal, primary source of water was borehole most of which are far from the facility. Power supply is via the national grid; however, in about half of them regularity of power supply was bad. The refuse disposal system in most of the facilities surveyed was bad.
Figure 1.
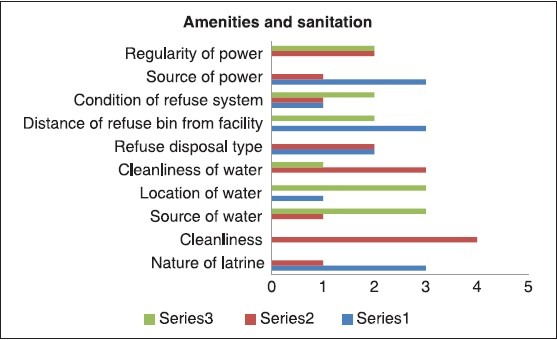
A bar chart showing the amenities and sanitation
Figure 2 shows that all the health facilities had a community health officer (CHO), two had staff nurse midwives, and one medical doctor covered all the primary health care facilities studied, while one had senior community health extension workers (CHEW), junior CHEW and administrative officers. None of the health centres had a pharmacy technician, laboratory technologists, medical records officer and environmental health officers.
Figure 2.
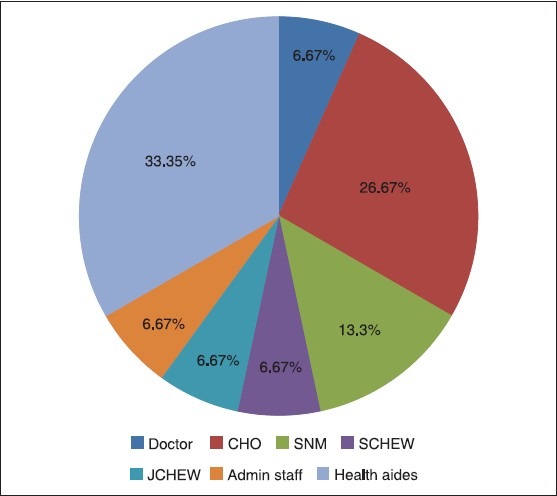
Pie chart showing the distribution of health care workersby cadres
Most of the discussants said that the facilities were clean, had good appearance, but do not have enough seats. According to a 35-year-old civil servant, “They need to have modern comfortable chairs, but here they make use of old benches.” Generally, the facility buildings were described as insufficient, with a few bed spaces and there were no security personnel to man the gates. In one of the health centres, the discussants complained about the walls which they said needed to be plastered and painted. A young mother of two had this to say: “Accommodation for women who delivered is poor in this facility. When I delivered my first baby, I was not supposed to be discharged but another woman made us four, and since there were only three beds, the matron pleaded with me to go home.” According to a 29-year-old nursery school teacher, “You know the time for labour is not planned, if a woman comes in labour at night, there will be no security man to open the gate for her.”
Most of the discussants said that personnel, equipment and supplies were fairly adequate. They mentioned equipment such as weighing scales, thermometers and added that the services of at least a doctor and a laboratory technologist are needed per health facility. A 31-year-old mother of two said: “Imagine that we pay for laboratory tests but these tests are done outside this health centre. Even if it is an emergency, you still have to wait until the results are brought back and only God knows for how long. At times it takes several days.”
The heads of facility were of the opinion that the facilities were in fair condition. They said the walls have cracks, were in need of renovation and that the facilities need boreholes or an extension of the public pipe-borne water supply since they buy water from vendors. One of the heads of the facilities studied mentioned that there is no residential accommodation for workers, and that toilet facility was inadequate and as such they share toilets with the clients.
The heads of facilities complained about the insufficiency of personnel and equipment. Such equipment as weighing scales, sphygmomanometer were mentioned. One head of facility said: “For the past 5 years that I have been heading this facility, they have never changed our sphygmomanometers and stethoscopes. We are just patching, using them as they are. Sometimes, they do not give us accurate results.”
DISCUSSION
This study revealed that the maternal health services commonly assessed by the clients in the facilities include: ANC, child welfare services, delivery care and postpartum care services. This study also found out that none of the health facilities studied had the capacity to deliver even the full range of basic EOC. This agrees with the findings of a countrywide Nigerian study in 1998, the 2003 Nigerian National Demographic Health Survey (NDHS) and a study in Peru in 2006, that the met need for EOC is still low.1,15,16 It also conforms with the finding of a 2003 study, where only 42% of public PHC facilities in Nigeria met internationally accepted standards for EOC.17 Essential obstetric care is one of the four pillars of safe motherhood, and has been identified as the main intervention strategy with the highest impact on maternal health.18,19 It ensures that essential care for high-risk pregnancies and complications is provided to all women who need it. Perhaps, this low met need for EOC as has been reported by several studies is a major contributory factor to the unacceptably high maternal mortality rates in the country.
Laboratory services are important support services to maternal health care. Despite this, our study showed that none of the health facilities had a laboratory technologist. Also, essential laboratory facilities for obstetric care was lacking in three out of the four facilities. This would explain why some of the needed laboratory investigations were not carried out. This agrees with the finding in Zimbabwe; where poor quality of care provided by the health centre staff was attributed to limited availability of equipment coupled with poor know how by the available health personnel.7 Although a few of the clients paid for laboratory services, FGD analysis showed that most of these investigations were done in laboratories outside the health facilities studied. The quality of the laboratory investigations done outside these facilities may be questionable except there is quality assurance assessment prior to using them.
Most respondents said that the health facilities had good appearance, and were in fair condition. This differed from the findings of an evaluation of primary health care in Nigeria where many of the PHC facilities were dilapidated with little or no evidence of maintenance or repair.17 This difference may be as a result of perceived philanthropic gestures of the indigenes of the town in complementing governments' developmental efforts. Some of the respondents however made observations on the need for more buildings to serve as residential accommodation for the health workers, and for security personnel. These according to them will enable 24-hour provision of services at the health facilities. The primary sources of water were borehole, most of which are far from the health facilities assessed. Respondents also complained about lack of constant water supply as in other studies where water supply was found to be inadequate in PHC facilities.6,11,20 Refuse disposal was found to be inadequate in half of the health facilities. This was similar to the findings of a Nigerian study by Olumide et al., where about half of the primary health care facilities surveyed had inadequate refuse disposal.6
Equipment, drugs and supplies form an essential part of structure in quality of care. Three out of the four facilities studies had weighing scale (both bathroom and infant); and shakir's strip, two had plastic bowl for tepid sponging. None had a screen or tongue depressor. This finding was similar to those of other studies where none of the health facilities had the entire minimum equipment package available.4,5,20 Even where the facilities had other equipment for the provision of maternal health services, the providers complained that some such as weighing scales, sphygmomanometer and stethoscopes were not functional. This scenario was said to have contributed to long waiting time during consultation. None of the facilities surveyed operated a drug revolving fund scheme, and none had essential drugs list. Also, none had all the essential drugs recommended for a PHC. Even where the facilities had most of the drugs available, they were insufficient. This was similar to findings by other studies carried out on essential drugs availability at the PHC level.4,8,9,10,11 Findings of this study showed that all the facilities had such consumables as latex gloves, sutures, antiseptic lotion, soaps, syringes and cotton wool available, and was in contrast with the findings from Pakistan where these basic supplies were not available at the primary and secondary facilities.21
Health personnel were unevenly distributed in all the facilities studied, while manpower was less than the minimum staff complement recommended.6,22 There was shortage of medical officers and public health nurses as were the findings of other studies.4,6,22 It was also revealed that there were no laboratory technologists nor pharmacy technicians in the entire PHC facilities. Also only one medical doctor covered all the health facilities studied, while these facilities were manned by community health officers. Even where other resources are available, human resources were needed for proper management of these resources. Little wonder, none of the facilities is an EOC facility, as there were no personnel with the necessary skills needed to address the major causes of maternal mortality.23,24 This agrees with the finding that shortage of health professionals reduce the number of facilities equipped to offer EOC 24 hrs a day and are significantly related to the quality of care and maternal mortality rates.25 This finding is also in keeping with the Nigeria Reproductive Health Resources and Service Survey, which reported paucity of skilled birth attendants and the effect of same on health workers capacity to offer effective and efficient maternal health services.26 Several studies have attributed high maternal mortality ratios to such inadequacies as rudimentary or absent managerial skills shortage of staff, drugs, equipment and supplies.8,9,10,11 It then suffices that the type and quality of care provided to women often determine their survival through the processes of pregnancy, labour and puerperium.1
Other key elements of the quality of service with respect to inadequacies include; the number of visits and the component of services such as ANC. Majority of the women we studied had their blood pressure and body weight, respectively, measured, received advice on drugs/ supplement, had tetanus toxoid and received health education on nutrition. Few, had urine test for sugar and protein, blood test for anaemia. These findings differed from the report of the study by Trinh et al.,27 where 9% of women reported receiving items on biomedical assessment, 8.6% in care provision/health promotion. The results of ANC content were similar to those of other studies in the developing world in that more clinical assessments than laboratory tests were reported27 This has been linked to lack of equipment and skilled personnel in these countries and confirms that ANC services in the aforementioned countries still focus on the traditional approach,where more priority is given to clinical assessments than to health promotion/education.
CONCLUSIONS
This study concludes that the facilities available for the provision of maternal health services in Nnewi had most of the equipment, drugs and supplies available though they were inadequate. None of the facilities surveyed operated a drug revolving fund scheme, nor had essential drugs list.
Also the structures that house some of the facilities were not large enough to accommodate all the clients and providers. Water supply, power supply and refuse disposal system were not adequate.
None of the health facilities had the capacity for even basic EOC. There were no laboratory technicians, no pharmacy technicians, only one of the facilities has a laboratory, while only one doctor covered the entire LG PHCs.
ACKNOWLEDGMENTS
This work was part of a dissertation submitted to the National Postgraduate Medical College of Nigeria in part fulfillment of the requirements for the award of the Fellowship of the College in Public Health.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Physicians for human rights. Deadly delays. Maternal mortality in Peru. A rights - based approach to safe motherhood. Physicians for human rights.org [Google Scholar]
- 2.Parent F, Fromageot A, Coppieters Y, Lejeune C, Lemenu D, Garant M, et al. Analysis of adequacy levels for human resources improvement within primary health care framework in Africa. Health Res Policy Syst. 2005;3:8. doi: 10.1186/1478-4505-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hodges A. Children's and women's right in Nigeria, wake-up call: Situation assessment and analysis, Nigeria, Abuja. National Planning Commission and United Nations Children's Fund. 2001:2–10. [Google Scholar]
- 4.Adeniyi JD, Ejembi CL, Igbineosun P, Mohammed D. The status of primary health care in Nigeria. Report of a needs assessment survey. The National Primary Health Care Development Agency (NPHCDA) 2001:1–100. [Google Scholar]
- 5.Musa EO, Ejembi CL. Reasons and routine of paediatric referrals from first level health of facilities in Sabon Gari Zaria. Northwest Niger J Community Med Prim Health Care. 2004;16:10–15. [Google Scholar]
- 6.Olumide EA, Obionu CN, Mako IV. An assessment of quality of primary health care in Nigeria. Report of a survey commissioned by the National Primary Health Care Development Agency (NPHCDA) Published by the NPHCDA Abuja, Nigeria. 2000 Mar [Google Scholar]
- 7.Sikosana PL. An evaluation of the quality of antenatal care at rural health centres in Matebaleland North Province. Cent Afr Med. 1994;40:268–72. [PubMed] [Google Scholar]
- 8.Chapman RR. Endangering safe motherhood in Mozambique: Prenatal care as pregnancy risk. Soc Sci Med. 2003;57:355–74. doi: 10.1016/s0277-9536(02)00363-5. [DOI] [PubMed] [Google Scholar]
- 9.Thaddeus S, Maine D. Too far to walk: Maternal mortality in context. Soc Sci Med. 1994;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 10.Kale OO. Management capacity and institutional reform in Better Health in Africa. The Nigeria Perspective Chestrad. 1996:12–17. [Google Scholar]
- 11.Oyesola R, Shehu D, Ikeh AT, Maru I. Improving emergency obstetric care at a state referral hospital, Kebbi State, Nigeria. International Journal of Gynaecology and Obstetrics, 1997;59(Suppl 2):S75–81. doi: 10.1016/s0020-7292(97)00150-1. [DOI] [PubMed] [Google Scholar]
- 12.United Nations Geneva. Millennium Development Goal (MDG) 2000 [Google Scholar]
- 13.Nnewi facts and figures. The profile of Nnewi North Local Government Area. 2008. pp. 1–2. Available from: http//www.nac.uk.org.factfile.Htm .
- 14.Araoye MO. Research methodology with statistics for health and social sciences. Nathadex Publications, saw-mill, Ilorin. (2nd ed) 2008:115–22. [Google Scholar]
- 15.National Population Commission (Nigeria) and ICF Macro Nigeria, Nigeria Demographic and Health Survey 2008. Calverton, Maryland: National Population Commission and ICF/Macro. 2009 [Google Scholar]
- 16.National Population Commission (Nigeria), Nigeria Demographic and Health Survey 1999. Calverton, Maryland: National Population Commission and ORC/Macro. 2000 [Google Scholar]
- 17.Fatusi A, Ijadunola K. National Study on essential obstetric care facilities in Nigeria. Abuja: Federal Ministry of Health and United Nations Populations Fund; 2003. [Google Scholar]
- 18.AVSC/COPE for child health; A process and tools for improving the quality of maternal and child health services in Southeast Nigeria. East Afr Med J. 2004;8:293–99. doi: 10.4314/eamj.v81i6.9178. [DOI] [PubMed] [Google Scholar]
- 19.Maxwell RJ. In World Health Organization. A review of determinants of hospital performance. WHO/SHs/DHS/94. 1994;5:8–11. [Google Scholar]
- 20.Sambo MN, Lewis I, Sabitu K. Quality of record system in primary health centres of Tafa LGA, North Central Nigeria. Ann Niger Med. 2005;1:155. [Google Scholar]
- 21.Fikree FF, Mir AM, Haq IU. She may reach a facility but will still die! An analysis of quality of public sector maternal health services, District Multan, Pakistan. J Pak Med Assoc. 2006;56:156–63. [PubMed] [Google Scholar]
- 22.National Primary Health Care Development Agency (NPHCDA), Health manpower in primary health care report, NPHCDA. 2002:10–1. [Google Scholar]
- 23.Rafei UM. A paper presented at the World Health Organization, South-East Asia regional consultation on improvement of quality of maternal health services through implementation of reviews on maternal death; 13-15 January 2003; New Delhi. [Google Scholar]
- 24.Annelies WS. Current status of essential obstetric care activities internationally. A literature review. Trop Doc. 2003;33:135–38. doi: 10.1177/004947550303300305. [DOI] [PubMed] [Google Scholar]
- 25.Raikkonen O, Perälä M, Kahanpää A. Staffing adequacy, supervisory support and quality of care in long-term care settings: Staff perceptions. J Adv Nurs. 2007;60:615–26. doi: 10.1111/j.1365-2648.2007.04443.x. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization/Federal Ministry of Health, Abuja, Nigeria reproductive health resources and service survey at the primary health care level of government facilities. 2002 [Google Scholar]
- 27.Trinh LT, Dibley MJ, Byles J. Antenatal care adequacy in three provinces of Vietnam. Public Health Rep. 2006;121:408–75. doi: 10.1177/003335490612100417. [DOI] [PMC free article] [PubMed] [Google Scholar]


