Abstract
Circadian clocks maintain periodicity in internal cycles of behavior, physiology, and metabolism, enabling organisms to anticipate the 24-h rotation of the Earth. In mammals, circadian integration of metabolic systems optimizes energy harvesting and utilization across the light/dark cycle. Disruption of clock genes has recently been linked to sleep disorders and to the development of cardiometabolic disease. Conversely, aberrant nutrient signaling affects circadian rhythms of behavior. This chapter reviews the emerging relationship between the molecular clock and metabolic systems and examines evidence that circadian disruption exerts deleterious consequences on human health.
Keywords: Circadian clock, Metabolism, Energy homeostasis, Metabolic disease, Nutrient sensing
1 Introduction
The daily order of temporal life is so innate as to slip from consciousness on most days. So it should not be surprising that a conceptual framework for studies of biological timing remains outside of the realm of modern medical practice. Yet with a transformation in our understanding of the molecular mechanism encoding circadian systems over the past 20 years, new studies have begun to bridge the gap from molecular clocks to human biology. Insight into circadian clocks and metabolism stems directly from the discovery that biological rhythms are sustained by a genetically encoded transcription network that functions as a molecular oscillator with near 24-h precision in most cell types, maintaining phase alignment in a range of behavioral, physiological, and biochemical processes with the environmental light cycle. The impact of circadian timing on human health has begun to emerge through observational population studies in individuals subjected to sleep restriction, shift work, and jet travel, in addition to experimental studies that reveal broad pathophysiologic consequences of circadian disruption on cognitive function, psychiatric disorders, cancer, metabolic syndrome, and inflammation (Bechtold et al. 2010; Reppert and Weaver 2002; Albrecht 2013). In this chapter, we focus on the growing body of evidence indicating a critical role of the clock network in metabolic homeostasis and highlight the cross talk between circadian and metabolic systems as a framework to understand effects of biological timing on physiology and disease states.
2 Clocks, Metabolism, and Disease
2.1 Rhythmicity of Metabolic Processes
While the most overt outputs of the mammalian clock are the sleep/wake and fasting/feeding cycles, the circadian clock also influences homeostasis across a broad range of behavioral and physiological processes, including glucose and lipid metabolism, body temperature, endocrine hormone secretion, and cardiovascular health (Fig. 1) (Panda et al. 2002b; Reppert and Weaver 2002). An evolutionary advantage of the circadian clock may be that it enhances energetic efficiency through temporal separation of anabolic and catabolic reactions (such as gluconeogenesis and glycolysis). An additional function of the clock is to maintain proper alignment of internal metabolic cycles relative to the sleep/wake cycle, enabling organisms to anticipate changes in the daily energetic environment tied to the rising and setting of the sun. In humans, circadian control over physiology has been well established through epidemiological research. For example, myocardial infarction, pulmonary edema, and hypertensive crises all have a tendency to peak at particular times during the day (Maron et al. 1994; Staels 2006). Circadian control of glucose metabolism has also been well documented, though the precise molecular mechanisms are not yet well understood. Glucose tolerance and insulin action are known to vary throughout the day, as oral glucose tolerance is impaired in the evening compared to morning hours due to combined effects of reduced insulin sensitivity and diminished insulin secretion in the nighttime. Glucose levels per se also display circadian oscillations and peak before the start of the active period (Arslanian et al. 1990; Bolli et al. 1984). Evidence from SCN-ablated rats and degeneration of autonomic tracts linking SCN to liver further points toward a direct role for the circadian clock in glucose homeostasis, as these rats display loss of 24-h glucose rhythms (Cailotto et al. 2005; la Fleur et al. 2001). Of note, studies in both rodents and humans suggest that loss of circadian rhythmicity of glucose metabolism may even contribute to the development of metabolic disorders such as type 2 diabetes, as rhythms of insulin secretion, glucose tolerance, and corticosterone release are diminished in streptozotocin-induced diabetic rats and in patients with type 2 diabetes (Oster et al. 1988; Shimomura et al. 1990; Van Cauter et al. 1997). Gaining a better understanding of the molecular mechanisms underlying circadian control of glucose homeostasis and other physiological processes will therefore be critical for enabling temporal evaluation in the diagnosis and treatment of metabolic disorders.
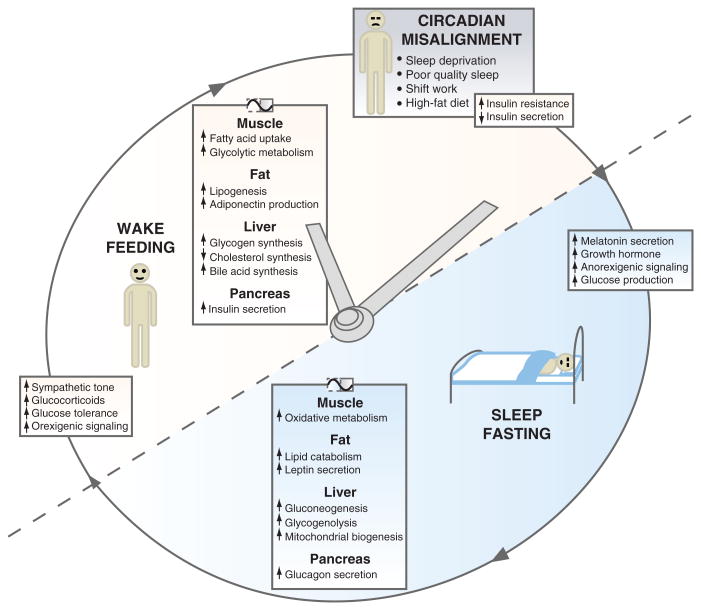
Fig. 1.
Rhythmicity of metabolic processes according to time of day. The clock coordinates appropriate metabolic responses with the light/dark cycle and enhances energetic efficiency through temporal separation of anabolic and catabolic reactions in peripheral tissues. Circadian misalignment, which occurs during sleep disruption, shift work, and dietary alterations, disrupts the integration of circadian and metabolic systems, leading to adverse metabolic health effects [Figure modified from Bass and Takahashi (2010)]
2.2 CNS Circuits Integrating Circadian and Metabolic Processes
Circadian and metabolic processes interact at both the neuroanatomic and neuroendocrine levels to regulate overall metabolic homeostasis. In order to better appreciate how the circadian clock network within brain regulates whole body metabolism, it is important to understand the anatomic connections between brain centers essential for circadian rhythmicity and those that control appetite and energy expenditure (Fig. 2) (reviewed in Horvath 2005; Horvath and Gao 2005; Saper et al. 2005; Slat et al. 2013; Kalsbeek and Fliers 2013). Classical lesioning studies performed in the 1970s first determined that the “master pacemaker” neurons are localized to the suprachiasmatic nuclei (SCN), which consist of bilateral nuclei within the anterior hypothalamus that receive environmental light input via the retinohypothalamic tract (RHT). SCN ablation abolishes 24-h rhythms of locomotor activity, feeding, drinking, and sleep. Subsequent studies in the 1990s revealed that transplantation of a short-period (tau) mutant SCN into an SCN-lesioned wild-type hamster results in the wild-type hamster having a period length identical to that of the tau mutant donor SCN (Ralph et al. 1990). However, 24-h rhythms of glucocorticoid and melatonin oscillations were not restored. These experiments established that direct neuronal projections, in addition to secreted factors, are necessary for SCN regulation of behavioral and metabolic homeostasis (Cheng et al. 2002; Kramer et al. 2001; Meyer-Bernstein et al. 1999; Silver et al. 1996). Elegant tracing studies have revealed that neurons from the SCN predominantly synapse directly on cell bodies within the ventral and dorsal subparaventricular zones (vSPZ and dSPZ, respectively) and the dorsomedial hypothalamus (DMH). vSPZ neurons are involved in regulation of sleep/wake and activity cycles, but not body temperature cycles, while neurons within the dSPZ control temperature rhythms and have minimal impact on sleep and activity cycles (Lu et al. 2001). The SPZ also projects to the DMH, a brain region important for rhythms of the sleep/wake cycle, locomotor activity, body temperature, food intake, and corticosteroid secretion (Chou et al. 2003). Projections from neurons within the DMH target neuronal centers involved in the regulation of sleep/wake cycle (ventrolateral preoptic nucleus—VLPO), corticosteroid release (paraventricular nucleus—PVN), and feeding and wakefulness (lateral hypothalamus—LHA). As such, the DMH acts as a relay center, amplifying circadian signals from the SCN to multiple regions of the brain involved in regulation of sleep, activity, and feeding.
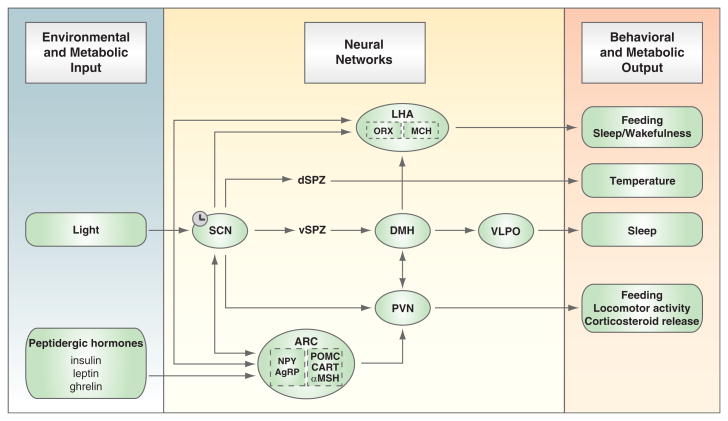
Fig. 2.
Neural circuits linking hypothalamic regions important in circadian and energetic control. Signals from the exogenous environment (i.e., light) and endogenous metabolism (i.e., hormones and metabolites) are integrated in a network of hypothalamic neuronal centers (see text for details), which in turn impart rhythmicity on behavioral and metabolic outputs, including sleep, feeding and activity behavior, thermogenesis, and hormone secretion [Figure modified from Huang et al. (2011)]
The DMH and LHA also receive input from the arcuate nucleus (ARC), which plays a well-characterized role in the regulation of feeding and appetite. The ARC contains orexigenic neurons that express neuropeptide Y (NPY) and the agouti-related protein (AgRP), as well as neurons expressing anorexigenic peptides including pro-opiomelanocortin (POMC) and cocaine- and amphetamine-regulated transcript (CART). Because the choroid plexus allows passage through the blood–brain barrier, the ARC is uniquely positioned to integrate humoral signals from the periphery with neuronal signals within the hypothalamus. For example, leptin, a hormone secreted in proportion to fat mass by adipose tissue, stimulates production of α-melanocyte-stimulating hormone (α-MSH) from POMC/CART neurons while simultaneously inhibiting NPY/AgRP production within the ARC (Cowley et al. 2001; Frederich et al. 1995). This in turn decreases production of the orexigenic peptides orexin (ORX) and melanin-concentrating hormone (MCH) within the LHA and suppresses appetite and food intake. When leptin levels are low, the orexigenic neurons in the ARC produce NPY and AgRP, which stimulate hunger and decrease energy expenditure via signaling to the LHA. Interestingly, in addition to regulation by nutrient status, leptin also displays a circadian pattern of expression. While our knowledge of circadian regulation of circulating hormones from the periphery is still quite incomplete, it will ultimately be important to identify how signals regulated by the nutritional status of the organism communicate with and co-regulate brain centers involved in control of activity, feeding, sleep, and metabolism. In this regard it is of note that NPY, AgRP, and orexin display circadian patterns of expression within the hypothalamus, with peaks around the beginning of the active period, while α-MSH levels are highest at the beginning of the inactive period (Kalra et al. 1999; Lu et al. 2002). Thus, understanding the neural networks integrating centers involved in regulation of circadian rhythms, sleep, and energy homeostasis may shed light on the interplay between anticipatory and adaptive behaviors involved in long-term energy constancy.
2.3 Peripheral Oscillators and Circadian Regulation of Metabolic Transcription Networks
Prior to the discovery of molecular clock genes, a prevailing model held that circadian rhythms represent a unique property of pacemaker neurons. However, seminal experiments performed in the 1990s established the presence of cell-autonomous circadian gene rhythmic expression in cultured fibroblasts, demonstrating the ubiquity of circadian transcriptional oscillators throughout all cells (Balsalobre et al. 1998). Subsequent molecular analyses have revealed that the clock network is indeed expressed not only in the SCN, but in most mammalian tissues, including those essential for cardiometabolic function, such as liver, pancreas, muscle, and heart (Davidson et al. 2005; Marcheva et al. 2010; Wilsbacher et al. 2002; Yamazaki et al. 2000; Yoo et al. 2004; reviewed in Brown and Azzi 2013). Because the phase of peripheral clocks is delayed compared to that of the SCN, and since ablation of the SCN abolishes synchrony of peripheral oscillators, it is believed that the SCN functions as a master pacemaker maintaining phase alignment of autonomous cellular clocks throughout all peripheral tissues (Balsalobre et al. 1998; Sakamoto et al. 1998).
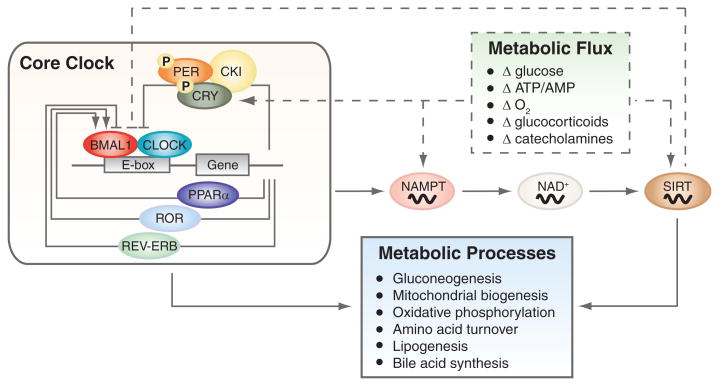
Emerging genomic studies have illuminated the multifaceted function of peripheral circadian oscillators at the cellular level (Fig. 3). For instance, transcriptional profiling studies have revealed that ∼10 % of all mammalian genes across multiple tissues exhibit 24-h variations in mRNA levels (Miller et al. 2007; Oishi et al. 2003; Panda et al. 2002a; Rey et al. 2011; Rudic et al. 2005; Storch et al. 2002; Zvonic et al. 2006). Importantly, gene ontogeny analyses have shown that many of these rhythmic genes cluster within classes regulating intermediary metabolism, including processes such as mitochondrial oxidative phosphorylation, carbohydrate metabolism and transport, lipid biosynthesis, adipocyte differentiation, and cholesterol synthesis and degradation (Bass and Takahashi 2010; Delaunay and Laudet 2002; Doherty and Kay 2010; Panda et al. 2002a; Yang et al. 2006). While only a small subset of these oscillating metabolic genes is a direct target of the molecular clock, many encode transcription factors, transcription or translation modulators, or rate-limiting enzymes, which in turn impart rhythmicity on downstream metabolic genes and processes (Noshiro et al. 2007; Panda et al. 2002a; Ripperger and Schibler 2006). Interestingly, the phase of oscillation and the level of expression of each metabolic gene vary across different tissues, suggesting that the circadian system responds to both local and systemic cues to control diverse metabolic processes in a physiologically meaningful manner (Delaunay and Laudet 2002; Kornmann et al. 2007). Not surprisingly, mutation of the core molecular clock disrupts the rhythmic expression of numerous key metabolic genes (Lamia et al. 2008; McCarthy et al. 2007; Oishi et al. 2003; Panda et al. 2002a). Whether rhythmicity of these metabolic genes is secondary to the feeding rhythm or arises due to intrinsic clock expression within the periphery has been a long-standing question. Only recently, studies involving tissue-specific circadian gene mutant mice have indicated that molecular clocks in the periphery play a crucial role in imparting rhythmicity to metabolic gene oscillation (Lamia et al. 2008; Marcheva et al. 2010; Sadacca et al. 2010).
Fig. 3.
Cross talk between the core clock mechanism and metabolic pathways. The core clock consists of a series of transcription/translation feedback loops that either directly or indirectly synchronize diverse metabolic processes. The clock also receives reciprocal input from nutrient signaling pathways (including NAD+-dependent sirtuins), which function as rheostats to coordinate metabolic processes with daily cycles of sleep/wakefulness and fasting/feeding [Figure modified from Bass and Takahashi (2010)]
Although the mammalian core clock genes are well defined, the precise role of both central and peripheral oscillators in the maintenance of energy balance and metabolic homeostasis is still not well understood. Research aiming to elucidate the molecular pathways linking the circadian clock with metabolic sensors remains an active area of investigation.
3 Circadian Disruption and Disease
3.1 Metabolic Phenotypes of Circadian Mutant Mice
Mouse models have been invaluable in defining the roles of individual core clock genes in the generation and maintenance of circadian rhythmicity and have recently begun to provide insight into the metabolic functions of the circadian clock. The first genetic link between circadian rhythmicity and metabolism was discovered in mice carrying the ClockΔ19/Δ19 mutation. While initial studies found that these animals become arrhythmic when subjected to total darkness, it was subsequently observed that they also display attenuated diurnal feeding rhythms, hyperphagia, hyperlipidemia, hyperleptinemia, hepatic steatosis, and hyperglycemic hypoinsulinemia due to impaired insulin secretion and islet proliferation (Marcheva et al. 2010; Turek et al. 2005). In addition, ClockΔ19/Δ19 animals exhibit loss of rhythmic expression of key metabolic and proliferative genes in liver, muscle, and pancreas, which undoubtedly contributes to the extensive disruption of glucose and lipid homeostasis (Marcheva et al. 2010; McCarthy et al. 2007; Miller et al. 2007; Panda et al. 2002a). Knockout of Clock also compromises renal sodium reabsorption and reduces arterial blood pressure (Zuber et al. 2009). Furthermore, overexpression of the ClockΔ19 allele in cardiomyocytes alters heart rate variability, contractility, and responsiveness to changes in afterload, revealing a role of the peripheral circadian gene network in the control of cardiac fuel handling (Bray et al. 2008).
Studies in mice mutant for BMAL1, the heterodimeric partner of CLOCK, have revealed that, in addition to causing arrhythmic behavior, loss of BMAL1 also impairs adipogenesis, adipocyte differentiation, and hepatic carbohydrate metabolism (Lamia et al. 2008; Rudic et al. 2004; Shimba et al. 2005). Mutation of Bmal1 also leads to disruption of circadian variation in blood pressure and heart rate, to increased susceptibility to vascular injury, and to skeletal muscle pathologies (Anea et al. 2009; Curtis et al. 2007; McCarthy et al. 2007). Various peripheral tissue-specific Bmal1 knockout mouse models, which exhibit normal circadian activity and feeding rhythms, have provided further insight into the role of the cell-autonomous clock in metabolism and energy balance. For example, pancreas-specific Bmal1 disruption leads to hyperglycemia, impaired glucose tolerance, and decreased insulin response due to impaired β-cell proliferation and insulin granule exocytosis, while liver-specific Bmal1 deletion leads to loss of oscillation of key hepatic metabolic genes, impaired gluconeogenesis, exaggerated glucose clearance, and hypoglycemia during the resting phase (Lamia et al. 2008; Marcheva et al. 2010; Sadacca et al. 2010). Thus, tissue-specific circadian clocks have distinct roles within pancreatic islets and liver, affecting opposing metabolic processes and thereby contributing to glucose constancy across periods of feeding and fasting.
Genetic loss of core clock genes downstream of the CLOCK/BMAL1 heterodimer also leads to metabolic abnormalities. Disruption of both Cry1 and Cry2 in mice results in glucose intolerance, elevated corticosterone levels, increased glucocorticoid transactivation in liver, altered lipogenic and steroidogenic pathways, and impaired body growth and liver regeneration (Bur et al. 2009; Lamia et al. 2011; Matsuo et al. 2003; Okamura et al. 2011). Knockdown of Cry1 and Cry2 was also found to increase expression of gluconeogenic genes and to augment hepatic glucose production (Zhang et al. 2010). These observations are consistent with findings that adenoviral overexpression of CRY1 decreases fasting glucose levels and improves insulin sensitivity in insulin-resistant Leprdb/db mice, while overexpression of mutant CRY1 results in polydipsia, polyuria, and hyperglycemia, all symptoms of diabetes mellitus (Okano et al. 2009; Zhang et al. 2010). Deficiency of PER2, another member of the core circadian feedback loop, abolishes glucocorticoid rhythmicity and protects mice from development of glucose intolerance in response to glucocorticoids (So et al. 2009; Yang et al. 2009). Finally, disruption of the ability of the circadian kinase CK1ε to phosphorylate its PER and CRY protein targets (tau mutation of the Syrian hamsters) is also associated with reduced growth and elevated metabolic rate (Lucas et al. 2000; Oklejewicz et al. 1997).
Mice carrying mutations of nuclear hormone receptors (NHRs) that participate in circadian transcription feedback loops also display alterations in metabolic function. For example, in addition to a shorter circadian period in constant darkness, mice lacking the Bmal1 repressor REV-ERBα exhibit altered lipid and bile metabolism (Le Martelot et al. 2009; Preitner et al. 2002). Conditional liver-specific overexpression of Rev-erbα induces changes in expression of genes involved in xenobiotic detoxification, carbohydrate and energy metabolism, and lipid and sterol homeostasis (Kornmann et al. 2007). Deficiency of the Bmal1 activator RORα in staggerer mice leads to predisposition to age-related phenotypes such as atherosclerosis (Akashi and Takumi 2005; Mamontova et al. 1998; Sato et al. 2004). Similarly, vascular deletion of Pparγ, a stimulator of Bmal1 expression, causes a significant reduction of the daily fluctuation in heart rate and blood pressure, modifies the diurnal variation in sympathetic nerve activity, and alters the expression of vascular adrenoceptors (Berger 2005; Wang et al. 2008). Additionally, ablation of Pgc-1α, a rhythmically expressed metabolic regulator and coactivator of the RAR-related orphan receptor (ROR) family of orphan nuclear receptors, leads to abnormal rhythms of locomotor activity, body temperature, and metabolic rate in mice (Liu et al. 2007).
Finally, disruption in the expression of clock-controlled genes downstream of the core circadian network also impacts metabolism. For instance, mice mutant for the circadian poly(A) deadenylase Nocturnin, which is involved in posttranscriptional regulation of rhythmic gene expression, exhibit alterations in glucose tolerance and peripheral tissue insulin sensitivity. They are also resistant to diet-induced obesity and hepatic steatosis due to defective lipid absorption in the small intestine (Douris et al. 2011; Green et al. 2007). Similarly, disruption of the estrogen-related receptor-α (ERR-α), another orphan nuclear receptor, has been implicated in resistance to high-fat diet and metabolic dysregulation, including reduced peripheral fat deposits, hypoglycemia, and time-dependent hypoinsulinemia (Dufour et al. 2011). Of note, ablation of ERR-α also modifies locomotor activity rhythms and the expression patterns of the core clock genes, suggesting a function of ERR-α as a potential regulator of the circadian clock (Dufour et al. 2011). Collectively, these animal model studies have unveiled the importance of both central and peripheral circadian clocks for the maintenance of energy homeostasis.
3.2 Circadian Gene Polymorphisms and Metabolic Phenotypes in Humans
In addition to the recent findings in animal models, mounting evidence suggests that genetic variation in circadian genes also influences metabolic parameters in humans. A number of genome-wide association studies (GWAS) have uncovered links between polymorphisms in CLOCK and susceptibility to hypertension, obesity, and metabolic syndrome (Garaulet et al. 2009; Sookoian et al. 2008, 2010). Single-nucleotide polymorphisms (SNPs) in CLOCK are also associated with high plasma ghrelin concentrations, short sleep duration, and altered eating behaviors, leading to higher total energy intake, decreased compliance with prescribed diet plans, and, ultimately, resistance to weight loss (Garaulet et al. 2010b, 2011). Case–control studies have further revealed a correlation between common genetic variations of CLOCK and the incidence and severity of nonalcoholic fatty liver disease (NAFLD), one of the most common disorders observed in obese persons (Sookoian et al. 2007).
Genetic variants in BMAL1 have also been linked with the development of hypertension and type 2 diabetes, and SNPs in loci in or near CRY2 have been associated with fasting glucose concentrations (Dupuis et al. 2010; Woon et al. 2007). PER2 polymorphisms have also been linked with hyperglycemia, abdominal obesity, and unhealthy feeding behavior phenotypes, while expression of PER2 mRNA may also correlate with metabolic markers in humans (Ando et al. 2010; Englund et al. 2009; Garaulet et al. 2010a; Gomez-Abellan et al. 2008). Conversely, a rare variant of NAMPT1, a gene involved in a clock negative feedback loop, is associated with protection from obesity (Blakemore et al. 2009).
GWAS studies have also recently indicated that MTNR1A and MTNR1B, G-protein-coupled receptors for melatonin, a circadianly regulated circulating hormone implicated in the regulation of sleep and glucose homeostasis, are associated with high fasting plasma glucose levels (Dubocovich et al. 2003; Li et al. 2011; Ling et al. 2011; Peschke and Muhlbauer 2010; Ronn et al. 2009; Takeuchi et al. 2010; Tam et al. 2010). Genetic variants in and near MTNR1B are further associated with impaired insulin secretion and increased risk of developing type 2 and gestational diabetes mellitus, while the SNP rs2119882 in the MTNR1A gene is linked to insulin resistance and susceptibility to polycystic ovary syndrome, a hormonal disorder in women often associated with obesity, type 2 diabetes, and heart disease (Kim et al. 2011; Kwak et al. 2012; Li et al. 2011; Lyssenko et al. 2009; Staiger et al. 2008).
While most GWAS analyses do not take into account the added complexity of gene–gene interactions, one study demonstrated the existence of a synergistic effect of specific polymorphisms in PER2, PER3, CLOCK, and BMAL1 that accounts for morning or evening activity preference in humans (Pedrazzoli et al. 2010). The extensive cross talk between circadian and metabolic networks further adds to the complexity of analysis of human genetic studies. For instance, environmental dysregulation of metabolic homeostasis, such as overnutrition with western diet, may reciprocally feedback to impair circadian homeostasis (Kohsaka et al. 2007). Further, carriers of the CLOCK SNP rs4580704 display lower glucose levels and improved insulin sensitivity only when on a diet high in monounsaturated fatty acids, while an association between the CLOCK SNP rs1801260 and increased waist circumference is evident only in the presence of saturated fatty acids (Garaulet et al. 2009). A complete understanding of circadian gene function in humans will ultimately require consideration of both genetic and nutritional variables. As new evidence for interactions between clocks and metabolism emerges from epidemiologic and association studies, it underscores the clinical importance of rhythmicity for the maintenance of metabolic homeostasis and emphasizes the significance and implications of a better understanding of the interconnections between the two systems.
3.3 Impact of Circadian Misalignment in Humans
Since the introduction of artificial light and nighttime work, serious health consequences have been reported for those who sleep less and/or routinely disconnect their working time from the light/dark cycle. Reduced sleep duration (both acute and chronic) and poor-quality sleep are linked with impaired glucose tolerance, reduced insulin responsiveness following glucose challenge, increased body mass index, decreased levels of leptin, and increased levels of ghrelin (Donga et al. 2010; Gottlieb et al. 2005; Knutson and Van Cauter 2008; Megirian et al. 1998; Nilsson et al. 2004; Spiegel et al. 2009; Taheri et al. 2004). Association studies have further revealed that shift workers have increased risk of obesity, metabolic dysfunction, cardiovascular disease, cancer, and ischemic stroke (Di Lorenzo et al. 2003; Ellingsen et al. 2007; Karlsson et al. 2001, 2003). Social jetlag, the discrepancy between the circadian and social clock resulting in chronic sleep loss, has also been linked to increased BMI (Roenneberg et al. 2012). One of the most compelling clinical studies to examine the role of circadian alignment on metabolic physiology comes from an experimental paradigm in which healthy volunteers were placed on a 28-h “day” and scheduled to sleep at different phases throughout the circadian cycle. When the subjects were shifted 12 h from their normal sleep/wake cycle, they exhibited decreased leptin, increased glucose, and elevated blood pressure. In addition, their post-meal glucose response was similar to that seen in prediabetic patients (Scheer et al. 2009). Together, these studies highlight the detrimental health effects of disruption of the circadian system and the importance of synchronization of physiological systems with the light/dark cycle for maintenance of overall health.
4 Clocks and Nutrient Sensing
4.1 Impact of Diet Composition and Feeding Time
The aforementioned trend in modern society to disrupt the traditional sleep/wake cycle is coupled with a tendency to eat at irregular times. However, high-energy food intake in the evening and fasting in the morning have both been associated with the development of obesity, and skipping breakfast has also been shown to impair postprandial insulin sensitivity and fasting lipid levels in humans (Ekmekcioglu and Touitou 2011; Farshchi et al. 2005). Further, mice fed a high-fat diet (HFD) have increased daytime activity, lengthened period of locomotor activity rhythms, and altered expression of clock and clock-controlled genes involved in fuel utilization (Kohsaka et al. 2007). Interestingly, these mice consume nearly all of their extra calories during the 12-h light phase, suggesting that feeding at the incorrect time in the light/dark cycle (i.e., their rest period) exacerbates the obesogenic effects of high caloric intake due to desynchronization of various behavioral, hormonal, and molecular rhythms involved in maintaining energy balance (Kohsaka et al. 2007). In agreement with these observations, food restriction to the active (dark) phase in genetically obese mice with disrupted diurnal feeding patterns leads to improvement of their obesity and metabolic disorders, while HFD consumption exclusively during the rest (light) phase in wild-type mice significantly contributes to weight gain (Arble et al. 2009; Masaki et al. 2004). Together, these data suggest that the normal alignment of feeding and activity with the environmental light cycle is critical for the maintenance of energy homeostasis, though further studies will be necessary to understand the precise mechanisms of how the timing of food intake impacts energy constancy.
Restricted feeding (RF) (i.e., limiting food availability to the normal rest period) in rodents also induces a burst of food anticipatory activity (FAA), or an increase in locomotor activity prior to mealtime. On a molecular level, RF entrains circadian oscillations in peripheral tissues, such as liver and kidney, without affecting the clock rhythms in the central pacemaker in the SCN, thereby uncoupling the phase of peripheral clocks from that of the SCN (Damiola et al. 2000; Stokkan et al. 2001). However, the involvement of circadian oscillators in FAA remains controversial because while lesioning of the dorsomedial nucleus alters FAA, food anticipatory behavior persists in Bmal1 nullizygous mice (Fulton et al. 2006; Mieda et al. 2006). It is possible that the FAA constitutes a metabolic oscillator responsive to peripheral, neural, or circulating signals elicited by food ingestion. Resolution of the precise stimuli and neural pathways involved in FAA and understanding the effect of these nutrient signaling pathways on core properties of the SCN pacemaker remain important avenues for further investigation.
In addition to timing of food availability affecting the circadian outputs of the clock, caloric restriction (i.e., restriction of the total number of calories consumed without malnutrition) induces phase advances in rat behavioral and physiological circadian rhythms and alters expression of clock genes and neuropeptides in the mouse SCN (for review, Challet 2010). Prolonged fasting also advances the phase of free-running rhythms of locomotor activity and temperature (Challet et al. 1997). Together, these studies demonstrate that feeding behavior plays an essential role in coordinating the circadian rhythms of metabolism, though the precise identity of the signals that are able to reset the clock remains obscure.
4.2 Circadian Control of NAD+ Biosynthesis and Sirtuin/PARP Activity
One potential molecule that has been implicated as a mediator between circadian and metabolic pathways is nicotinamide adenine dinucleotide NAD+, a key cofactor involved in cellular redox reactions. The molecular clock directly regulates transcription of nicotinamide phosphoribosyltransferase (NAMPT), a key rate-limiting enzyme in the NAD+ salvage pathway (Nakahata et al. 2009; Ramsey et al. 2009). Consistent with circadian regulation of NAMPT, NAD+ levels also oscillate in peripheral tissues such as liver and adipose tissue, even when animals are maintained in constant darkness (Ramsey et al. 2009; Sahar et al. 2011). Importantly, mice with mutations in the activator genes Clock and Bmal1 exhibit constitutively low NAD+ levels, while those deficient in the clock repressor genes Cry1 and Cry2 have elevated NAD+, indicating direct regulation of NAD+ by the clock (Ramsey et al. 2009).
In addition to its role in redox reactions, NAD+ also acts as a cofactor for several enzymatic reactions, including NAD+-dependent deacetylation and ADP-ribosylation. The circadian clock was recently shown to modulate the activity of the metabolic enzyme, SIRT1, a class III protein deacetylase and a member of the sirtuin family of NAD+-dependent deacetylases. SIRT1 resides primarily in the nucleus and targets several transcription factors involved in the maintenance of nutrient flux, including Peroxisome Proliferator-Activated Receptor Gamma Coactivator 1-alpha (PGC-1α), Forkhead Box Protein O1 (FOXO1), Transducer of Regulated CREB Protein 2 (TORC2), Sterol Regulatory Element-Binding Protein 1c (SREBP-1c), and Signal Transducer and Activator of Transcription 3 (STAT3) (Haigis and Sinclair 2010; Rodgers et al. 2005; Sahar et al. 2011; Saunders and Verdin 2007). SIRT1 is a critical regulator of metabolic processes such as gluconeogenesis, lipid metabolism, and insulin sensitivity, as well as lifespan (Haigis and Sinclair 2010; Sahar et al. 2011; Saunders and Verdin 2007). Through rhythmic NAD+ biosynthesis, the circadian clock modulates SIRT1 activity, which then coordinates the daily transitions between the periods of fasting and feeding. Of note, SIRT1 also modulates CLOCK/BMAL1 activity, generating a negative feedback loop in which circadian control of NAD+-mediated sirtuin activity in turn regulates the clock itself through interaction with PER2, CLOCK, and BMAL1 (Asher et al. 2008; Grimaldi et al. 2009; Nakahata et al. 2008). Thus, the cross talk between the biological clock and the NAMPT/NAD+/SIRT1 pathway provides a nexus linking the circadian system and nutrient-sensing pathways.
It will be of great interest to determine whether circadian control of NAD+ biosynthesis affects other NAD+-dependent metabolic enzymes, including the six other mammalian sirtuin homologs (SIRT2–7) or the poly (ADP-ribose) polymerase (PARP-1). SIRT3–5 are primarily localized to mitochondria and have recently been characterized as important regulators of oxidative (fasting) metabolic pathways, including fatty acid oxidation, TCA cycle, ketogenesis, urea cycle, and oxidative phosphorylation (Haigis et al. 2006; Hallows et al. 2006, 2011; Hirschey et al. 2010; Huang et al. 2010; Nakagawa and Guarente 2009; Schwer et al. 2006; Shimazu et al. 2010; Someya et al. 2010). While little is known about circadian rhythms of NAD+ in mitochondria, it is intriguing to speculate that the circadian clock may influence mitochondrial sirtuins. PARP-1, which also plays an important role in the response to metabolic stress, has recently been identified as a regulator of clock gene expression through direct ADP-ribosylation of CLOCK and inhibition of CLOCK/BMAL1 DNA-binding activity (Asher et al. 2010). Interestingly, PARP-1 activity in mice is rhythmic, suggesting circadian control of ADP-ribosylation (Asher et al. 2010; Kumar and Takahashi 2010). However, at present, there is no evidence to suggest that these oscillations are mediated by clock-dependent control of NAD+ biosynthesis.
4.3 A Role of Redox in Circadian Rhythms
Prior to the discovery that the molecular clock directly regulates rhythms of NAD+, in vitro studies by McKnight and coworkers revealed that cellular redox status affects the circadian clock. Increased levels of oxidized cofactors (NAD+ or NADP+) decrease the ability of CLOCK/BMAL1 and NPAS2/BMAL1 to bind to DNA in purified systems, suggesting that cellular redox changes may be sufficient to entrain clocks (Rutter et al. 2001).
Interestingly, recent studies have further identified ∼24-h rhythms in the cellular redox state, which control circadian oscillations of the oxidation state of the peroxiredoxin family of antioxidant enzymes (Kil et al. 2012; O'Neill and Reddy 2011; O'Neill et al. 2011; Vogel 2011). Oscillating peroxiredoxin redox state affects its antioxidant activity, generating self-sustained rhythms of cellular redox status even in the absence of transcriptional control of circadian gene expression (both in anucleate human red blood cells and in single-celled alga Ostreococcus tauri treated with inhibitors of transcription and translation) (O'Neill and Reddy 2011; O'Neill et al. 2011). More recent studies have revealed that rhythms of peroxiredoxin oxidation exist in all domains of life and that these rhythms persist even in the presence of genetic clock disruption in mammalian cells, fungi and flies (Edgar et al. 2012; O'Neill and Reddy 2011). These studies raise the possibility that oscillations in cellular redox state may be an integral mechanism by which circadian rhythms of metabolic processes are controlled and that these rhythms may be maintained independently from the molecular clock transcriptional feedback loop.
4.4 A Link Between Circadian Rhythms and Nuclear Hormone Receptor Pathways
Several recent studies have focused on the role of nuclear hormone receptors as potential nutrient-sensing factors linking metabolic and circadian pathways. NHRs comprise a large family of proteins, containing both DNA- and ligand-binding domains that regulate their activities as transcriptional activators and/or repressors. Known NHR ligands include a wide range of molecules (e.g., steroid hormones, fatty acids, heme, sterols), though many NHRs are still classified as “orphan” since their endogenous ligands have not yet been identified (Sonoda et al. 2008). Interestingly, more than half of the ∼50 known NHRs display rhythmic expression patterns in peripheral tissues and are thus attractive candidates as integrators of circadian and nutrient-sensing pathways (Asher and Schibler 2011; Teboul et al. 2009; Yang et al. 2006, 2007).
Some NHRs, such as members of the REV-ERB and ROR families, are both transcriptional targets of the CLOCK/BMAL1 complex as well as transcriptional regulators of clock genes themselves. In the SCN and most metabolic tissues, REV-ERBs repress and RORs activate Bmal1 transcription, generating a short negative feedback loop (Akashi and Takumi 2005; Duez and Staels 2009; Preitner et al. 2002; Sato et al. 2004) (refer also to Sect. 3.1). As sensors of metabolites including heme, fatty acids, and sterols, REV-ERBα/β and RORα integrate nutrient signals with transcriptional regulation of the clock (Jetten 2009; Kallen et al. 2004; Yin et al. 2007). REV-ERBs and RORs also directly interact with other important metabolic factors, including the transcriptional regulator PGC-1α, which coactivates Bmal1 with RORα and β and also plays a key role in regulation of mitochondrial oxidative metabolism (Grimaldi and Sassone-Corsi 2007; Liu et al. 2007). Interestingly, activity of PGC-1α is regulated by SIRT1-mediated NAD+-dependent deacetylation, suggesting that circadian regulation of NAD+ may represent yet another metabolic feedback loop involving PGC-1α (Rodgers et al. 2005).
In addition to REV-ERBs and RORs, other NHRs are important for the coordination of molecular clocks and nutrient-sensing pathways. For example, members of the PPAR family of NHRs are also regulators of clock gene expression. PPARα activates both Bmal1 and Rev-erbα in liver (Li and Lin 2009; Schmutz et al. 2010; Yang et al. 2007). Conversely, several proteins, including PPARα, γ, and δ, are transcriptionally regulated by the circadian clock (Li and Lin 2009). Ligands for PPARs include various types of lipids, including the circulating gut metabolite oleylethanolamide (OEA), which is generated and released from the small intestine and suppresses food intake during the rest period in a PPARα-dependent manner (Fu et al. 2003; Rodriguez de Fonseca et al. 2001). In addition, PPARγ maintains daily rhythms of blood pressure and heart rate in blood vessels via regulation of Bmal1 expression (Wang et al. 2008). Further studies will be necessary to determine the importance of other lipid-derived PPAR ligands as effectors of the molecular clock.
The glucocorticoid receptor (GR) is another important NHR involved in the cross talk between central and peripheral circadian clocks. GR is expressed in many metabolic tissues, including liver, skeletal muscle, heart, and kidney, and activates several metabolic pathways including lipid metabolism and gluconeogenesis (Dickmeis and Foulkes 2011). GR is activated by glucocorticoid (GC) steroid hormones, which are produced and secreted in a circadian manner from the adrenal cortex. Timed release of GC from the adrenal cortex is generated through relays from the SCN to the hypothalamic-pituitary-adrenal axis (HPA). As such, GC rhythms are entrained by light and peak in the early morning in humans (Chung et al. 2011; Oster et al. 2006). Rhythmic GC release affects GR activity in peripheral tissues and thereby acts to synchronize peripheral clocks with the SCN (Teboul et al. 2009). Indeed, liver-specific GR knockout mice display accelerated clock phase-shifting in response to daytime food restriction, suggesting a lack of entrainment by the central clock (Le Minh et al. 2001). Furthermore, pharmacological activation of GR by dexamethasone resets the peripheral clock in liver, heart, and kidney, presumably by direct GR regulation of Rev-erbα and Per1 expression (Balsalobre et al. 2000; Torra et al. 2000; Yamamoto et al. 2005). While detailed mechanisms underlying clock resetting by GR have not been fully defined, GR appears to be a key entrainment signal of peripheral clock rhythms, allowing for the coupling of food- and SCN-derived resetting cues.
4.5 Circadian Control of Metabolic Peptide Hormones
Several metabolic hormones also display circadian oscillations and likely integrate circadian rhythms with feeding responses (reviewed in Kalsbeek and Fliers 2013). Diurnal oscillations of leptin and ghrelin, two hormones produced by the adipocytes and stomach, respectively, are important for delivering nutritional cues to the brain and establishing feeding behavior (Ahima et al. 1998; Huang et al. 2011; Kalra et al. 2003; Kalsbeek et al. 2001; Mistlberger 2011; Yildiz et al. 2004). Leptin levels in humans peak at night and are responsible for nocturnal appetite suppression mediated by hypothalamic neurons (Sinha et al. 1996). Conversely, ghrelin increases before meal times and facilitates food anticipatory behavior (Cummings et al. 2001). Although the mechanisms controlling the rhythmic release of leptin and ghrelin from peripheral tissues remain unclear, it is known that their effects modulate the hypothalamic clock. Thus, these hormones counterbalance the GC/GR pathway, providing information from peripheral food-responsive clocks to the central pacemaker within the SCN.
Recent studies have also uncovered a role for the pancreatic β-cell clock in normal islet insulin exocytosis (Marcheva et al. 2010, 2011). As insulin is a primary regulator of blood glucose levels, these findings highlight the critical importance of the circadian system for the maintenance of energy homeostasis. Clock-dependent insulin levels may also have a broad impact on various nutrient-sensing pathways such as signaling through AMPK or sirtuins in other tissues. Interestingly, insulin, which is able to reach the brain via a transporter across the blood–brain barrier, is in turn able to modulate circadian feeding behavior (Gerozissis 2003). Thus, this feedback loop adds another layer to the intricate interplay between the circadian and metabolic systems that ultimately increases the organism's adaptability and chances for survival.
5 Perspectives on Timing in Animal and Human Studies
5.1 Importance of Timing and Environmental Light in Experimental Design
As compelling evidence for the vast effect of the biological clock on metabolic processes continues to mount, the importance of understanding the effect of circadian rhythmicity in the treatment and design of animal and clinical studies is becoming increasingly clear. Since a vast number of metabolic genes display diurnal tissue-specific variations in expression, comprehensive analysis of metabolic processes and pathways in animals should involve studies at several different time points over a 24-h period (Lamia et al. 2008; Marcheva et al. 2010; Sadacca et al. 2010). Phase delay between the timing of transcription and translation should also be considered, since processes such as pre-mRNA splicing, polyadenylation, and RNA decay may influence the activity and function of enzymes involved in metabolic homeostasis (reviewed in Staiger and Koster 2011; O'Neill et al. 2013). For instance, in liver, rhythmic transcription of the mitochondrial succinate dehydrogenase (Sdh1) is phase-advanced compared to its translation, while the inhibitor of serine protease Serpina1d exhibits a nonrhythmic mRNA pattern, but an oscillating protein profile (Reddy et al. 2006). Finally, circadian regulation of posttranslational modification, such as protein phosphorylation and ubiquitinylation, may also affect metabolic function (Eide et al. 2005; Lamia et al. 2009; Lee et al. 2001, 2008).
Temporal factors in the environment can also influence reproducibility of research results. Light is a powerful synchronizer of circadian rhythms, and thus, animal facility lighting intensity and photoperiod can affect behavioral activity and metabolic homeostasis (Menaker 1976; Reiter 1991). For example, exposure to constant light affects catecholamine, ACTH, and progesterone levels, while constant darkness shifts the peaks of blood glucose and nonesterified fatty acids and alters the expression of catabolic enzymes (Ivanisevic-Milovanovic et al. 1995; Zhang et al. 2006). Even small changes to the normal light/dark cycles, such as a switch to daylight savings time or a brief light pulse during the dark phase, can cause temporary misalignment of behavioral and metabolic rhythmicity, potentially increasing variability in experimental results (Clough 1982). Further, contamination of light at night in animal facilities, from translucent observation door windows, poorly insulated doorframes, and in-room lighted equipment, should be minimized, as studies have reported that as little as 0.2 lux light exposure during the dark cycle can disrupt the circadian rhythms of gene expression, shift the timing of food consumption, increase body mass, reduce glucose tolerance, alter melatonin rhythms, and increase oncogenicity (Dauchy et al. 1999; Fonken et al. 2010; Minneman et al. 1974). These observations underscore the importance of taking circadian timing and environmental light cycles into consideration in the design and interpretation of metabolic studies.
5.2 Clinical Aspects of Timing
As scientists continue to uncover links between the circadian network and metabolism at the molecular level, many of these findings have made their way into the clinical realm in both the diagnosis and treatment of various metabolic disorders. For example, cortisol, an adrenal hormone essential for lipid and glucose metabolism, and ACTH, the pituitary hormone that regulates cortisol secretion from the adrenal gland, exhibit robust circadian rhythms in man (Orth et al. 1979; Orth and Island 1969; Szafarczyk et al. 1979). Therefore, proper diagnosis of Cushing's disease (characterized by cortisol excess) necessitates measurement of saliva cortisol in the late evening hours when the levels of this hormone are typically low, while adrenal insufficiency is more appropriately diagnosed when cortisol is measured in the morning hours when it is at its peak. Further, glucocorticoid therapy for patients with adrenal insufficiency aims to mimic the endogenous rhythms of cortisol, as short-acting synthetic glucocorticoids are usually given 2–3 times a day in tapering doses such that the largest amount is taken in the morning and the smallest in the early evening (Arlt 2009).
Melatonin, a natural hormone important for the initiation and maintenance of sleep, is another example where timing of drug delivery is critical in the treatment of daytime sleepiness following shift work or jetlag. Physiologic doses of melatonin during the day (when melatonin is normally low) result in daytime sleepiness, while treatment during the dark phase (coinciding with the endogenous increase in melatonin secretion) improves sleep latency and helps achieve continuous sleep (Brzezinski et al. 2005). Further, melatonin administration several hours prior to the normal onset of secretion causes a phase advance in the endogenous melatonin rhythm, which is particularly useful for treatment of eastbound jetlag. Conversely, melatonin treatment following the endogenous onset of secretion is often useful to improve westbound jetlag (Herxheimer and Petrie 2002).
As our knowledge of the complexity of the circadian and metabolic interacting networks deepens, we can also begin to rationally develop new treatments for disorders affected by circadian misalignment. For example, unbiased drug discovery screens have identified several compounds that can shift the phase of the endogenous clock. Indeed, treatment of human U20S cells stably expressing a Bmal1-Luc reporter construct with more than 120,000 potential drugs uncovered numerous compounds that either shorten or lengthen the period, including various inhibitors of CKIδ, CKIε, and GSK-3 (Hirota and Kay 2009; Hirota et al. 2008). This novel approach provides a means to pharmacologically control the circadian cycle, which may be useful in the treatment of circadian disorders and metabolic disturbances with a circadian component (reviewed in Antoch and Kondratov 2013). It also offers new insight into the interaction of previously unsuspected pathways with the circadian system.
6 Conclusion
The circadian clock is an evolutionarily conserved internal timekeeping mechanism that synchronizes endogenous systems with daily environmental cycles. The clock network is present in almost all mammalian tissues and governs a remarkable variety of biochemical, physiological, and behavioral processes. A growing body of evidence indicates that proper function of central and peripheral clocks is crucial for the well-being of the organism. Disruption of circadian rhythmicity has been implicated in the pathogenesis of several diseases, including metabolic disorders. Therefore, a deeper understanding of the role of the molecular clock in regulation of daily physiological processes will enable development of new treatments, more efficient therapeutic delivery, and better preventative strategies for management of diabetes, obesity, and other metabolic disorders.
Acknowledgments
C.B. Peek, A. Affinati and B. Marcheva are supported by NIH grants F32 DK092034-01, 1F30DK085936-01A1, and T32 DK007169, respectively. J. Bass is supported by NIH grants R01 HL097817-01, R01 DK090625-01A1, and P01 AG011412, the American Diabetes Association, the Chicago Biomedical Consortium Searle Funds, and the University of Chicago Diabetes Research and Training Center (grant P60 DK020595).
Footnotes
Disclosures: J. Bass is a member of the scientific advisory board of ReSet Therapeutics Inc.
References
- Ahima RS, Prabakaran D, Flier JS. Postnatal leptin surge and regulation of circadian rhythm of leptin by feeding. Implications for energy homeostasis and neuroendocrine function. J Clin Invest. 1998;101:1020–1027. doi: 10.1172/JCI1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akashi M, Takumi T. The orphan nuclear receptor RORalpha regulates circadian transcription of the mammalian core-clock Bmal1. Nat Struct Mol Biol. 2005;12:441–448. doi: 10.1038/nsmb925. [DOI] [PubMed] [Google Scholar]
- Albrecht U. Circadian clocks and mood-related behaviors. In: Kramer A, Merrow M, editors. Circadian clocks, vol 217, Handbook of experimental pharmacology. Springer; Heidelberg: 2013. [DOI] [PubMed] [Google Scholar]
- Ando H, Ushijima K, Kumazaki M, Eto T, Takamura T, Irie S, Kaneko S, Fujimura A. Associations of metabolic parameters and ethanol consumption with messenger RNA expression of clock genes in healthy men. Chronobiol Int. 2010;27:194–203. doi: 10.3109/07420520903398617. [DOI] [PubMed] [Google Scholar]
- Anea CB, Zhang M, Stepp DW, Simkins GB, Reed G, Fulton DJ, Rudic RD. Vascular disease in mice with a dysfunctional circadian clock. Circulation. 2009;119:1510–1517. doi: 10.1161/CIRCULATIONAHA.108.827477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoch MP, Kondratov RV. Pharmacological modulators of the circadian clock as potential therapeutic drugs: focus on genotoxic/anticancer therapy. In: Kramer A, Merrow M, editors. Circadian clocks, vol 217, Handbook of experimental pharmacology. Springer; Heidelberg: 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW. Circadian timing of food intake contributes to weight gain. Obesity. 2009;17:2100–2102. doi: 10.1038/oby.2009.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arlt W. The approach to the adult with newly diagnosed adrenal insufficiency. J Clin Endocrinol Metab. 2009;94:1059–1067. doi: 10.1210/jc.2009-0032. [DOI] [PubMed] [Google Scholar]
- Arslanian S, Ohki Y, Becker DJ, Drash AL. Demonstration of a dawn phenomenon in normal adolescents. Horm Res. 1990;34:27–32. doi: 10.1159/000181791. [DOI] [PubMed] [Google Scholar]
- Asher G, Schibler U. Crosstalk between components of circadian and metabolic cycles in mammals. Cell Metab. 2011;13:125–137. doi: 10.1016/j.cmet.2011.01.006. [DOI] [PubMed] [Google Scholar]
- Asher G, Gatfield D, Stratmann M, Reinke H, Dibner C, Kreppel F, Mostoslavsky R, Alt FW, Schibler U. SIRT1 regulates circadian clock gene expression through PER2 deacetylation. Cell. 2008;134:317–328. doi: 10.1016/j.cell.2008.06.050. [DOI] [PubMed] [Google Scholar]
- Asher G, Reinke H, Altmeyer M, Gutierrez-Arcelus M, Hottiger MO, Schibler U. Poly (ADP-ribose) polymerase 1 participates in the phase entrainment of circadian clocks to feeding. Cell. 2010;142:943–953. doi: 10.1016/j.cell.2010.08.016. [DOI] [PubMed] [Google Scholar]
- Balsalobre A, Damiola F, Schibler U. A serum shock induces circadian gene expression in mammalian tissue culture cells. Cell. 1998;93:929–937. doi: 10.1016/s0092-8674(00)81199-x. [DOI] [PubMed] [Google Scholar]
- Balsalobre A, Brown SA, Marcacci L, Tronche F, Kellendonk C, Reichardt HM, Schutz G, Schibler U. Resetting of circadian time in peripheral tissues by glucocorticoid signaling. Science. 2000;289:2344–2347. doi: 10.1126/science.289.5488.2344. [DOI] [PubMed] [Google Scholar]
- Bass J, Takahashi JS. Circadian integration of metabolism and energetics. Science. 2010;330:1349–1354. doi: 10.1126/science.1195027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechtold DA, Gibbs JE, Loudon AS. Circadian dysfunction in disease. Trends Pharmacol Sci. 2010;31:191–198. doi: 10.1016/j.tips.2010.01.002. [DOI] [PubMed] [Google Scholar]
- Berger JP. Role of PPARgamma, transcriptional cofactors, and adiponectin in the regulation of nutrient metabolism, adipogenesis and insulin action: view from the chair. Int J Obes. 2005;29(Suppl 1):S3–S4. doi: 10.1038/sj.ijo.0802904. [DOI] [PubMed] [Google Scholar]
- Blakemore AI, Meyre D, Delplanque J, Vatin V, Lecoeur C, Marre M, Tichet J, Balkau B, Froguel P, Walley AJ. A rare variant in the visfatin gene (NAMPT/PBEF1) is associated with protection from obesity. Obesity. 2009;17:1549–1553. doi: 10.1038/oby.2009.75. [DOI] [PubMed] [Google Scholar]
- Bolli GB, De Feo P, De Cosmo S, Perriello G, Ventura MM, Calcinaro F, Lolli C, Campbell P, Brunetti P, Gerich JE. Demonstration of a dawn phenomenon in normal human volunteers. Diabetes. 1984;33:1150–1153. doi: 10.2337/diab.33.12.1150. [DOI] [PubMed] [Google Scholar]
- Bray MS, Shaw CA, Moore MW, Garcia RA, Zanquetta MM, Durgan DJ, Jeong WJ, Tsai JY, Bugger H, Zhang D, et al. Disruption of the circadian clock within the cardiomyocyte influences myocardial contractile function, metabolism, and gene expression. Am J Physiol Heart Circ Physiol. 2008;294:H1036–H1047. doi: 10.1152/ajpheart.01291.2007. [DOI] [PubMed] [Google Scholar]
- Brown SA, Azzi A. Peripheral circadian oscillators in mammals. In: Kramer A, Merrow M, editors. Circadian clocks, vol 217, Handbook of experimental pharmacology. Springer; Heidelberg: 2013. [DOI] [PubMed] [Google Scholar]
- Brzezinski A, Vangel MG, Wurtman RJ, Norrie G, Zhdanova I, Ben-Shushan A, Ford I. Effects of exogenous melatonin on sleep: a meta-analysis. Sleep Med Rev. 2005;9:41–50. doi: 10.1016/j.smrv.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Bur IM, Cohen-Solal AM, Carmignac D, Abecassis PY, Chauvet N, Martin AO, van der Horst GT, Robinson IC, Maurel P, Mollard P, et al. The circadian clock components CRY1 and CRY2 are necessary to sustain sex dimorphism in mouse liver metabolism. J Biol Chem. 2009;284:9066–9073. doi: 10.1074/jbc.M808360200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cailotto C, La Fleur SE, Van Heijningen C, Wortel J, Kalsbeek A, Feenstra M, Pevet P, Buijs RM. The suprachiasmatic nucleus controls the daily variation of plasma glucose via the autonomic output to the liver: are the clock genes involved? Eur J Neurosci. 2005;22:2531–2540. doi: 10.1111/j.1460-9568.2005.04439.x. [DOI] [PubMed] [Google Scholar]
- Challet E. Interactions between light, mealtime and calorie restriction to control daily timing in mammals. J Comp Physiol B. 2010;180:631–644. doi: 10.1007/s00360-010-0451-4. [DOI] [PubMed] [Google Scholar]
- Challet E, Pevet P, Lakhdar-Ghazal N, Malan A. Ventromedial nuclei of the hypothalamus are involved in the phase advance of temperature and activity rhythms in food-restricted rats fed during daytime. Brain Res Bull. 1997;43:209–218. doi: 10.1016/s0361-9230(96)00439-x. [DOI] [PubMed] [Google Scholar]
- Cheng MY, Bullock CM, Li C, Lee AG, Bermak JC, Belluzzi J, Weaver DR, Leslie FM, Zhou QY. Prokineticin 2 transmits the behavioural circadian rhythm of the suprachiasmatic nucleus. Nature. 2002;417:405–410. doi: 10.1038/417405a. [DOI] [PubMed] [Google Scholar]
- Chou TC, Scammell TE, Gooley JJ, Gaus SE, Saper CB, Lu J. Critical role of dorsomedial hypothalamic nucleus in a wide range of behavioral circadian rhythms. J Neurosci. 2003;23:10691–10702. doi: 10.1523/JNEUROSCI.23-33-10691.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung S, Son GH, Kim K. Adrenal peripheral oscillator in generating the circadian glucocorticoid rhythm. Ann NY Acad Sci. 2011;1220:71–81. doi: 10.1111/j.1749-6632.2010.05923.x. [DOI] [PubMed] [Google Scholar]
- Clough G. Environmental effects on animals used in biomedical research. Biol Rev Camb Philos Soc. 1982;57:487–523. doi: 10.1111/j.1469-185x.1982.tb00705.x. [DOI] [PubMed] [Google Scholar]
- Cowley MA, Smart JL, Rubinstein M, Cerdan MG, Diano S, Horvath TL, Cone RD, Low MJ. Leptin activates anorexigenic POMC neurons through a neural network in the arcuate nucleus. Nature. 2001;411:480–484. doi: 10.1038/35078085. [DOI] [PubMed] [Google Scholar]
- Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, Weigle DS. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes. 2001;50:1714–1719. doi: 10.2337/diabetes.50.8.1714. [DOI] [PubMed] [Google Scholar]
- Curtis AM, Cheng Y, Kapoor S, Reilly D, Price TS, Fitzgerald GA. Circadian variation of blood pressure and the vascular response to asynchronous stress. Proc Natl Acad Sci USA. 2007;104:3450–3455. doi: 10.1073/pnas.0611680104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damiola F, Le Minh N, Preitner N, Kornmann B, Fleury-Olela F, Schibler U. Restricted feeding uncouples circadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus. Genes Dev. 2000;14:2950–2961. doi: 10.1101/gad.183500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauchy RT, Blask DE, Sauer LA, Brainard GC, Krause JA. Dim light during darkness stimulates tumor progression by enhancing tumor fatty acid uptake and metabolism. Cancer Lett. 1999;144:131–136. doi: 10.1016/s0304-3835(99)00207-4. [DOI] [PubMed] [Google Scholar]
- Davidson AJ, London B, Block GD, Menaker M. Cardiovascular tissues contain independent circadian clocks. Clin Exp Hypertens. 2005;27:307–311. [PubMed] [Google Scholar]
- Delaunay F, Laudet V. Circadian clock and microarrays: mammalian genome gets rhythm. Trends Genet. 2002;18:595–597. doi: 10.1016/s0168-9525(02)02794-4. [DOI] [PubMed] [Google Scholar]
- Di Lorenzo L, De Pergola G, Zocchetti C, L'Abbate N, Basso A, Pannacciulli N, Cignarelli M, Giorgino R, Soleo L. Effect of shift work on body mass index: results of a study performed in 319 glucose-tolerant men working in a Southern Italian industry. Int J Obes Relat Metab Disord. 2003;27:1353–1358. doi: 10.1038/sj.ijo.0802419. [DOI] [PubMed] [Google Scholar]
- Dickmeis T, Foulkes NS. Glucocorticoids and circadian clock control of cell proliferation: at the interface between three dynamic systems. Mol Cell Endocrinol. 2011;331:11–22. doi: 10.1016/j.mce.2010.09.001. [DOI] [PubMed] [Google Scholar]
- Doherty CJ, Kay SA. Circadian control of global gene expression patterns. Annu Rev Genet. 2010;44:419–444. doi: 10.1146/annurev-genet-102209-163432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donga E, van Dijk M, van Dijk JG, Biermasz NR, Lammers GJ, van Kralingen KW, Corssmit EP, Romijn JA. A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J Clin Endocrinol Metab. 2010;95:2963–2968. doi: 10.1210/jc.2009-2430. [DOI] [PubMed] [Google Scholar]
- Douris N, Kojima S, Pan X, Lerch-Gaggl AF, Duong SQ, Hussain MM, Green CB. Nocturnin regulates circadian trafficking of dietary lipid in intestinal enterocytes. Curr Biol. 2011;21:1347–1355. doi: 10.1016/j.cub.2011.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubocovich ML, Rivera-Bermudez MA, Gerdin MJ, Masana MI. Molecular pharmacology, regulation and function of mammalian melatonin receptors. Front Biosci. 2003;8:d1093–d1108. doi: 10.2741/1089. [DOI] [PubMed] [Google Scholar]
- Duez H, Staels B. Rev-erb-alpha: an integrator of circadian rhythms and metabolism. J Appl Physiol. 2009;107:1972–1980. doi: 10.1152/japplphysiol.00570.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dufour CR, Levasseur MP, Pham NH, Eichner LJ, Wilson BJ, Charest-Marcotte A, Duguay D, Poirier-Heon JF, Cermakian N, Giguere V. Genomic convergence among ERRalpha, PROX1, and BMAL1 in the control of metabolic clock outputs. PLoS Genet. 2011;7:e1002143. doi: 10.1371/journal.pgen.1002143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupuis J, Langenberg C, Prokopenko I, Saxena R, Soranzo N, Jackson AU, Wheeler E, Glazer NL, Bouatia-Naji N, Gloyn AL, et al. New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet. 2010;42:105–116. doi: 10.1038/ng.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar RS, Green EW, Zhao Y, van Ooijen G, Olmedo M, Qin X, Xu Y, Pan M, Valekunja UK, Feeney KA, et al. Peroxiredoxins are conserved markers of circadian rhythms. Nature. 2012;485:459–464. doi: 10.1038/nature11088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eide EJ, Woolf MF, Kang H, Woolf P, Hurst W, Camacho F, Vielhaber EL, Giovanni A, Virshup DM. Control of mammalian circadian rhythm by CKIepsilon-regulated proteasome-mediated PER2 degradation. Mol Cell Biol. 2005;25:2795–2807. doi: 10.1128/MCB.25.7.2795-2807.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekmekcioglu C, Touitou Y. Chronobiological aspects of food intake and metabolism and their relevance on energy balance and weight regulation. Obes Rev. 2011;12:14–25. doi: 10.1111/j.1467-789X.2010.00716.x. [DOI] [PubMed] [Google Scholar]
- Ellingsen T, Bener A, Gehani AA. Study of shift work and risk of coronary events. J R Soc Promot Health. 2007;127:265–267. doi: 10.1177/1466424007083702. [DOI] [PubMed] [Google Scholar]
- Englund A, Kovanen L, Saarikoski ST, Haukka J, Reunanen A, Aromaa A, Lonnqvist J, Partonen T. NPAS2 and PER2 are linked to risk factors of the metabolic syndrome. J Circadian Rhythms. 2009;7:5. doi: 10.1186/1740-3391-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farshchi HR, Taylor MA, Macdonald IA. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr. 2005;81:388–396. doi: 10.1093/ajcn.81.2.388. [DOI] [PubMed] [Google Scholar]
- Fonken LK, Workman JL, Walton JC, Weil ZM, Morris JS, Haim A, Nelson RJ. Light at night increases body mass by shifting the time of food intake. Proc Natl Acad Sci USA. 2010;107:18664–18669. doi: 10.1073/pnas.1008734107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frederich RC, Hamann A, Anderson S, Lollmann B, Lowell BB, Flier JS. Leptin levels reflect body lipid content in mice: evidence for diet-induced resistance to leptin action. Nat Med. 1995;1:1311–1314. doi: 10.1038/nm1295-1311. [DOI] [PubMed] [Google Scholar]
- Fu J, Gaetani S, Oveisi F, Lo Verme J, Serrano A, Rodriguez De Fonseca F, Rosengarth A, Luecke H, Di Giacomo B, Tarzia G, et al. Oleylethanolamide regulates feeding and body weight through activation of the nuclear receptor PPAR-alpha. Nature. 2003;425:90–93. doi: 10.1038/nature01921. [DOI] [PubMed] [Google Scholar]
- Fulton S, Pissios P, Manchon RP, Stiles L, Frank L, Pothos EN, Maratos-Flier E, Flier JS. Leptin regulation of the mesoaccumbens dopamine pathway. Neuron. 2006;51:811–822. doi: 10.1016/j.neuron.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Garaulet M, Lee YC, Shen J, Parnell LD, Arnett DK, Tsai MY, Lai CQ, Ordovas JM. CLOCK genetic variation and metabolic syndrome risk: modulation by monounsaturated fatty acids. Am J Clin Nutr. 2009;90:1466–1475. doi: 10.3945/ajcn.2009.27536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garaulet M, Corbalan-Tutau MD, Madrid JA, Baraza JC, Parnell LD, Lee YC, Ordovas JM. PERIOD2 variants are associated with abdominal obesity, psycho-behavioral factors, and attrition in the dietary treatment of obesity. J Am Diet Assoc. 2010a;110:917–921. doi: 10.1016/j.jada.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garaulet M, Lee YC, Shen J, Parnell LD, Arnett DK, Tsai MY, Lai CQ, Ordovas JM. Genetic variants in human CLOCK associate with total energy intake and cytokine sleep factors in overweight subjects (GOLDN population) Eur J Hum Genet. 2010b;18:364–369. doi: 10.1038/ejhg.2009.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garaulet M, Sanchez-Moreno C, Smith CE, Lee YC, Nicolas F, Ordovas JM. Ghrelin, sleep reduction and evening preference: relationships to CLOCK 3111 T/C SNP and weight loss. PLoS One. 2011;6:e17435. doi: 10.1371/journal.pone.0017435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerozissis K. Brain insulin: regulation, mechanisms of action and functions. Cell Mol Neurobiol. 2003;23:1–25. doi: 10.1023/A:1022598900246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez-Abellan P, Hernandez-Morante JJ, Lujan JA, Madrid JA, Garaulet M. Clock genes are implicated in the human metabolic syndrome. Int J Obes. 2008;32:121–128. doi: 10.1038/sj.ijo.0803689. [DOI] [PubMed] [Google Scholar]
- Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM, Nieto FJ. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165:863–867. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- Green CB, Douris N, Kojima S, Strayer CA, Fogerty J, Lourim D, Keller SR, Besharse JC. Loss of Nocturnin, a circadian deadenylase, confers resistance to hepatic steatosis and diet-induced obesity. Proc Natl Acad Sci USA. 2007;104:9888–9893. doi: 10.1073/pnas.0702448104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimaldi B, Sassone-Corsi P. Circadian rhythms: metabolic clockwork. Nature. 2007;447:386–387. doi: 10.1038/447386a. [DOI] [PubMed] [Google Scholar]
- Grimaldi B, Nakahata Y, Kaluzova M, Masubuchi S, Sassone-Corsi P. Chromatin remodeling, metabolism and circadian clocks: the interplay of CLOCK and SIRT1. Int J Biochem Cell Biol. 2009;41:81–86. doi: 10.1016/j.biocel.2008.08.035. [DOI] [PubMed] [Google Scholar]
- Haigis MC, Sinclair DA. Mammalian sirtuins: biological insights and disease relevance. Annu Rev Pathol. 2010;5:253–295. doi: 10.1146/annurev.pathol.4.110807.092250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haigis MC, Mostoslavsky R, Haigis KM, Fahie K, Christodoulou DC, Murphy AJ, Valenzuela DM, Yancopoulos GD, Karow M, Blander G, et al. SIRT4 inhibits glutamate dehydrogenase and opposes the effects of calorie restriction in pancreatic beta cells. Cell. 2006;126:941–954. doi: 10.1016/j.cell.2006.06.057. [DOI] [PubMed] [Google Scholar]
- Hallows WC, Lee S, Denu JM. Sirtuins deacetylate and activate mammalian acetyl-CoA synthetases. Proc Natl Acad Sci USA. 2006;103:10230–10235. doi: 10.1073/pnas.0604392103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallows WC, Yu W, Smith BC, Devries MK, Ellinger JJ, Someya S, Shortreed MR, Prolla T, Markley JL, Smith LM, et al. Sirt3 promotes the urea cycle and fatty acid oxidation during dietary restriction. Mol Cell. 2011;41:139–149. doi: 10.1016/j.molcel.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herxheimer A, Petrie KJ. Melatonin for the prevention and treatment of jet lag. Cochrane Database Syst Rev. 2002:CD001520. doi: 10.1002/14651858.CD001520. [DOI] [PubMed] [Google Scholar]
- Hirota T, Kay SA. High-throughput screening and chemical biology: new approaches for understanding circadian clock mechanisms. Chem Biol. 2009;16:921–927. doi: 10.1016/j.chembiol.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirota T, Lewis WG, Liu AC, Lee JW, Schultz PG, Kay SA. A chemical biology approach reveals period shortening of the mammalian circadian clock by specific inhibition of GSK-3beta. Proc Natl Acad Sci USA. 2008;105:20746–20751. doi: 10.1073/pnas.0811410106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschey MD, Shimazu T, Goetzman E, Jing E, Schwer B, Lombard DB, Grueter CA, Harris C, Biddinger S, Ilkayeva OR, et al. SIRT3 regulates mitochondrial fatty-acid oxidation by reversible enzyme deacetylation. Nature. 2010;464:121–125. doi: 10.1038/nature08778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath TL. The hardship of obesity: a soft-wired hypothalamus. Nat Neurosci. 2005;8:561–565. doi: 10.1038/nn1453. [DOI] [PubMed] [Google Scholar]
- Horvath TL, Gao XB. Input organization and plasticity of hypocretin neurons: possible clues to obesity's association with insomnia. Cell Metab. 2005;1:279–286. doi: 10.1016/j.cmet.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Huang JY, Hirschey MD, Shimazu T, Ho L, Verdin E. Mitochondrial sirtuins. Biochim Biophys Acta. 2010;1804:1645–1651. doi: 10.1016/j.bbapap.2009.12.021. [DOI] [PubMed] [Google Scholar]
- Huang W, Ramsey KM, Marcheva B, Bass J. Circadian rhythms, sleep, and metabolism. J Clin Invest. 2011;121:2133–2141. doi: 10.1172/JCI46043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanisevic-Milovanovic OK, Demajo M, Karakasevic A, Pantic V. The effect of constant light on the concentration of catecholamines of the hypothalamus and adrenal glands, circulatory hadrenocorticotropin hormone and progesterone. J Endocrinol Invest. 1995;18:378–383. doi: 10.1007/BF03347842. [DOI] [PubMed] [Google Scholar]
- Jetten AM. Retinoid-related orphan receptors (RORs): critical roles in development, immunity, circadian rhythm, and cellular metabolism. Nucl Recept Signal. 2009;7:e003. doi: 10.1621/nrs.07003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kallen J, Schlaeppi JM, Bitsch F, Delhon I, Fournier B. Crystal structure of the human RORalpha Ligand binding domain in complex with cholesterol sulfate at 2.2 A. J Biol Chem. 2004;279:14033–14038. doi: 10.1074/jbc.M400302200. [DOI] [PubMed] [Google Scholar]
- Kalra SP, Dube MG, Pu S, Xu B, Horvath TL, Kalra PS. Interacting appetite-regulating pathways in the hypothalamic regulation of body weight. Endocr Rev. 1999;20:68–100. doi: 10.1210/edrv.20.1.0357. [DOI] [PubMed] [Google Scholar]
- Kalra SP, Bagnasco M, Otukonyong EE, Dube MG, Kalra PS. Rhythmic, reciprocal ghrelin and leptin signaling: new insight in the development of obesity. Regul Pept. 2003;111:1–11. doi: 10.1016/s0167-0115(02)00305-1. [DOI] [PubMed] [Google Scholar]
- Kalsbeek A, Fliers E. Daily regulation of hormone profiles. In: Kramer A, Merrow M, editors. Circadian clocks, vol 217, Handbook of experimental pharmacology. Springer; Heidelberg: 2013. [DOI] [PubMed] [Google Scholar]
- Kalsbeek A, Fliers E, Romijn JA, La Fleur SE, Wortel J, Bakker O, Endert E, Buijs RM. The suprachiasmatic nucleus generates the diurnal changes in plasma leptin levels. Endocrinology. 2001;142:2677–2685. doi: 10.1210/endo.142.6.8197. [DOI] [PubMed] [Google Scholar]
- Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people. Occup Environ Med. 2001;58:747–752. doi: 10.1136/oem.58.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson BH, Knutsson AK, Lindahl BO, Alfredsson LS. Metabolic disturbances in male workers with rotating three-shift work. Results of the WOLF study. Int Arch Occup Environ Health. 2003;76:424–430. doi: 10.1007/s00420-003-0440-y. [DOI] [PubMed] [Google Scholar]
- Kil IS, Lee SK, Ryu KW, Woo HA, Hu MC, Bae SH, Rhee SG. Feedback control of adrenal steroidogenesis via H2O2-dependent, reversible inactivation of peroxiredoxin III in mitochondria. Mol Cell. 2012;46:584–594. doi: 10.1016/j.molcel.2012.05.030. [DOI] [PubMed] [Google Scholar]
- Kim JY, Cheong HS, Park BL, Baik SH, Park S, Lee SW, Kim MH, Chung JH, Choi JS, Kim MY, et al. Melatonin receptor 1 B polymorphisms associated with the risk of gestational diabetes mellitus. BMC Med Genet. 2011;12:82. doi: 10.1186/1471-2350-12-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann NY Acad Sci. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohsaka A, Laposky AD, Ramsey KM, Estrada C, Joshu C, Kobayashi Y, Turek FW, Bass J. High-fat diet disrupts behavioral and molecular circadian rhythms in mice. Cell Metab. 2007;6:414–421. doi: 10.1016/j.cmet.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Kornmann B, Schaad O, Bujard H, Takahashi JS, Schibler U. System-driven and oscillator-dependent circadian transcription in mice with a conditionally active liver clock. PLoS Biol. 2007;5:e34. doi: 10.1371/journal.pbio.0050034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer A, Yang FC, Snodgrass P, Li X, Scammell TE, Davis FC, Weitz CJ. Regulation of daily locomotor activity and sleep by hypothalamic EGF receptor signaling. Science. 2001;294:2511–2515. doi: 10.1126/science.1067716. [DOI] [PubMed] [Google Scholar]
- Kumar V, Takahashi JS. PARP around the clock. Cell. 2010;142:841–843. doi: 10.1016/j.cell.2010.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwak SH, Kim SH, Cho YM, Go MJ, Cho YS, Choi SH, Moon MK, Jung HS, Shin HD, Kang HM, et al. A genome-wide association study of gestational diabetes mellitus in Korean women. Diabetes. 2012;61:531–541. doi: 10.2337/db11-1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- la Fleur SE, Kalsbeek A, Wortel J, Fekkes ML, Buijs RM. A daily rhythm in glucose tolerance: a role for the suprachiasmatic nucleus. Diabetes. 2001;50:1237–1243. doi: 10.2337/diabetes.50.6.1237. [DOI] [PubMed] [Google Scholar]
- Lamia KA, Storch KF, Weitz CJ. Physiological significance of a peripheral tissue circadian clock. Proc Natl Acad Sci USA. 2008;105:15172–15177. doi: 10.1073/pnas.0806717105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamia KA, Sachdeva UM, DiTacchio L, Williams EC, Alvarez JG, Egan DF, Vasquez DS, Juguilon H, Panda S, Shaw RJ, et al. AMPK regulates the circadian clock by cryptochrome phosphorylation and degradation. Science. 2009;326:437–440. doi: 10.1126/science.1172156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamia KA, Papp SJ, Yu RT, Barish GD, Uhlenhaut NH, Jonker JW, Downes M, Evans RM. Cryptochromes mediate rhythmic repression of the glucocorticoid receptor. Nature. 2011;480:552–556. doi: 10.1038/nature10700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Martelot G, Claudel T, Gatfield D, Schaad O, Kornmann B, Sasso GL, Moschetta A, Schibler U. REV-ERBalpha participates in circadian SREBP signaling and bile acid homeostasis. PLoS Biol. 2009;7:e1000181. doi: 10.1371/journal.pbio.1000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Minh N, Damiola F, Tronche F, Schutz G, Schibler U. Glucocorticoid hormones inhibit food-induced phase-shifting of peripheral circadian oscillators. EMBO J. 2001;20:7128–7136. doi: 10.1093/emboj/20.24.7128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C, Etchegaray JP, Cagampang FR, Loudon AS, Reppert SM. Posttranslational mechanisms regulate the mammalian circadian clock. Cell. 2001;107:855–867. doi: 10.1016/s0092-8674(01)00610-9. [DOI] [PubMed] [Google Scholar]
- Lee J, Lee Y, Lee MJ, Park E, Kang SH, Chung CH, Lee KH, Kim K. Dual modification of BMAL1 by SUMO2/3 and ubiquitin promotes circadian activation of the CLOCK/BMAL1 complex. Mol Cell Biol. 2008;28:6056–6065. doi: 10.1128/MCB.00583-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S, Lin JD. Molecular control of circadian metabolic rhythms. J Appl Physiol. 2009;107:1959–1964. doi: 10.1152/japplphysiol.00467.2009. [DOI] [PubMed] [Google Scholar]
- Li C, Shi Y, You L, Wang L, Chen ZJ. Melatonin receptor 1A gene polymorphism associated with polycystic ovary syndrome. Gynecol Obstet Invest. 2011;72:130–134. doi: 10.1159/000323542. [DOI] [PubMed] [Google Scholar]
- Ling Y, Li X, Gu Q, Chen H, Lu D, Gao X. A common polymorphism rs3781637 in MTNR1B is associated with type 2 diabetes and lipids levels in Han Chinese individuals. Cardiovasc Diabetol. 2011;10:27. doi: 10.1186/1475-2840-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C, Li S, Liu T, Borjigin J, Lin JD. Transcriptional coactivator PGC-1alpha integrates the mammalian clock and energy metabolism. Nature. 2007;447:477–481. doi: 10.1038/nature05767. [DOI] [PubMed] [Google Scholar]
- Lu J, Zhang YH, Chou TC, Gaus SE, Elmquist JK, Shiromani P, Saper CB. Contrasting effects of ibotenate lesions of the paraventricular nucleus and subparaventricular zone on sleep-wake cycle and temperature regulation. J Neurosci. 2001;21:4864–4874. doi: 10.1523/JNEUROSCI.21-13-04864.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu XY, Shieh KR, Kabbaj M, Barsh GS, Akil H, Watson SJ. Diurnal rhythm of agouti-related protein and its relation to corticosterone and food intake. Endocrinology. 2002;143:3905–3915. doi: 10.1210/en.2002-220150. [DOI] [PubMed] [Google Scholar]
- Lucas RJ, Stirland JA, Mohammad YN, Loudon AS. Postnatal growth rate and gonadal development in circadian tau mutant hamsters reared in constant dim red light. J Reprod Fertil. 2000;118:327–330. doi: 10.1530/jrf.0.1180327. [DOI] [PubMed] [Google Scholar]
- Lyssenko V, Nagorny CL, Erdos MR, Wierup N, Jonsson A, Spegel P, Bugliani M, Saxena R, Fex M, Pulizzi N, et al. Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat Genet. 2009;41:82–88. doi: 10.1038/ng.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamontova A, Seguret-Mace S, Esposito B, Chaniale C, Bouly M, Delhaye-Bouchaud N, Luc G, Staels B, Duverger N, Mariani J, et al. Severe atherosclerosis and hypoalphalipoproteinemia in the staggerer mouse, a mutant of the nuclear receptor RORalpha. Circulation. 1998;98:2738–2743. doi: 10.1161/01.cir.98.24.2738. [DOI] [PubMed] [Google Scholar]
- Marcheva B, Ramsey KM, Buhr ED, Kobayashi Y, Su H, Ko CH, Ivanova G, Omura C, Mo S, Vitaterna MH, et al. Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature. 2010;466:627–631. doi: 10.1038/nature09253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcheva B, Ramsey KM, Bass J. Circadian genes and insulin exocytosis. Cell Logist. 2011;1:32–36. doi: 10.4161/cl.1.1.14426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maron BJ, Kogan J, Proschan MA, Hecht GM, Roberts WC. Circadian variability in the occurrence of sudden cardiac death in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 1994;23:1405–1409. doi: 10.1016/0735-1097(94)90384-0. [DOI] [PubMed] [Google Scholar]
- Masaki T, Chiba S, Yasuda T, Noguchi H, Kakuma T, Watanabe T, Sakata T, Yoshimatsu H. Involvement of hypothalamic histamine H1 receptor in the regulation of feeding rhythm and obesity. Diabetes. 2004;53:2250–2260. doi: 10.2337/diabetes.53.9.2250. [DOI] [PubMed] [Google Scholar]
- Matsuo T, Yamaguchi S, Mitsui S, Emi A, Shimoda F, Okamura H. Control mechanism of the circadian clock for timing of cell division in vivo. Science. 2003;302:255–259. doi: 10.1126/science.1086271. [DOI] [PubMed] [Google Scholar]
- McCarthy JJ, Andrews JL, McDearmon EL, Campbell KS, Barber BK, Miller BH, Walker JR, Hogenesch JB, Takahashi JS, Esser KA. Identification of the circadian transcriptome in adult mouse skeletal muscle. Physiol Genomics. 2007;31:86–95. doi: 10.1152/physiolgenomics.00066.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megirian D, Dmochowski J, Farkas GA. Mechanism controlling sleep organization of the obese Zucker rats. J Appl Physiol. 1998;84:253–256. doi: 10.1152/jappl.1998.84.1.253. [DOI] [PubMed] [Google Scholar]
- Menaker M. Physiological and biochemical aspects of circadian rhythms. Fed Proc. 1976;35:2325. [PubMed] [Google Scholar]
- Meyer-Bernstein EL, Jetton AE, Matsumoto SI, Markuns JF, Lehman MN, Bittman EL. Effects of suprachiasmatic transplants on circadian rhythms of neuroendocrine function in golden hamsters. Endocrinology. 1999;140:207–218. doi: 10.1210/endo.140.1.6428. [DOI] [PubMed] [Google Scholar]
- Mieda M, Williams SC, Richardson JA, Tanaka K, Yanagisawa M. The dorsomedial hypothalamic nucleus as a putative food-entrainable circadian pacemaker. Proc Natl Acad Sci USA. 2006;103:12150–12155. doi: 10.1073/pnas.0604189103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BH, McDearmon EL, Panda S, Hayes KR, Zhang J, Andrews JL, Antoch MP, Walker JR, Esser KA, Hogenesch JB, et al. Circadian and CLOCK-controlled regulation of the mouse transcriptome and cell proliferation. Proc Natl Acad Sci USA. 2007;104:3342–3347. doi: 10.1073/pnas.0611724104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minneman KP, Lynch H, Wurtman RJ. Relationship between environmental light intensity and retina-mediated suppression of rat pineal serotonin-N-acetyl-transferase. Life Sci. 1974;15:1791–1796. doi: 10.1016/0024-3205(74)90180-5. [DOI] [PubMed] [Google Scholar]
- Mistlberger RE. Neurobiology of food anticipatory circadian rhythms. Physiol Behav. 2011;104:535–545. doi: 10.1016/j.physbeh.2011.04.015. [DOI] [PubMed] [Google Scholar]
- Nakagawa T, Guarente L. Urea cycle regulation by mitochondrial sirtuin, SIRT5. Aging. 2009;1:578–581. doi: 10.18632/aging.100062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakahata Y, Kaluzova M, Grimaldi B, Sahar S, Hirayama J, Chen D, Guarente LP, Sassone-Corsi P. The NAD+-dependent deacetylase SIRT1 modulates CLOCK-mediated chromatin remodeling and circadian control. Cell. 2008;134:329–340. doi: 10.1016/j.cell.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakahata Y, Sahar S, Astarita G, Kaluzova M, Sassone-Corsi P. Circadian control of the NAD+ salvage pathway by CLOCK-SIRT1. Science. 2009;324:654–657. doi: 10.1126/science.1170803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson PM, Roost M, Engstrom G, Hedblad B, Berglund G. Incidence of diabetes in middle-aged men is related to sleep disturbances. Diabetes Care. 2004;27:2464–2469. doi: 10.2337/diacare.27.10.2464. [DOI] [PubMed] [Google Scholar]
- Noshiro M, Usui E, Kawamoto T, Kubo H, Fujimoto K, Furukawa M, Honma S, Makishima M, Honma K, Kato Y. Multiple mechanisms regulate circadian expression of the gene for cholesterol 7alpha-hydroxylase (Cyp7a), a key enzyme in hepatic bile acid biosynthesis. J Biol Rhythms. 2007;22:299–311. doi: 10.1177/0748730407302461. [DOI] [PubMed] [Google Scholar]
- O'Neill J, Maywood L, Hastings M. Cellular mechanisms of circadian pacemaking: beyond transcriptional loops. In: Kramer A, Merrow M, editors. Circadian clocks, vol 217, Handbook of experimental pharmacology. Springer; Heidelberg: 2013. [DOI] [PubMed] [Google Scholar]
- Oishi K, Miyazaki K, Kadota K, Kikuno R, Nagase T, Atsumi G, Ohkura N, Azama T, Mesaki M, Yukimasa S, et al. Genome-wide expression analysis of mouse liver reveals CLOCK-regulated circadian output genes. J Biol Chem. 2003;278:41519–41527. doi: 10.1074/jbc.M304564200. [DOI] [PubMed] [Google Scholar]
- Okamura H, Doi M, Yamaguchi Y, Fustin JM. Hypertension due to loss of clock: novel insight from the molecular analysis of Cry1/Cry2-deleted mice. Curr Hypertens Rep. 2011;13:103–108. doi: 10.1007/s11906-011-0181-3. [DOI] [PubMed] [Google Scholar]
- Okano S, Akashi M, Hayasaka K, Nakajima O. Unusual circadian locomotor activity and pathophysiology in mutant CRY1 transgenic mice. Neurosci Lett. 2009;451:246–251. doi: 10.1016/j.neulet.2009.01.014. [DOI] [PubMed] [Google Scholar]
- Oklejewicz M, Hut RA, Daan S, Loudon AS, Stirland AJ. Metabolic rate changes proportionally to circadian frequency in tau mutant Syrian hamsters. J Biol Rhythms. 1997;12:413–422. doi: 10.1177/074873049701200503. [DOI] [PubMed] [Google Scholar]
- O'Neill JS, Reddy AB. Circadian clocks in human red blood cells. Nature. 2011;469:498–503. doi: 10.1038/nature09702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill JS, van Ooijen G, Dixon LE, Troein C, Corellou F, Bouget FY, Reddy AB, Millar AJ. Circadian rhythms persist without transcription in a eukaryote. Nature. 2011;469:554–558. doi: 10.1038/nature09654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orth DN, Island DP. Light synchronization of the circadian rhythm in plasma cortisol (17-OHCS) concentration in man. J Clin Endocrinol Metab. 1969;29:479–486. doi: 10.1210/jcem-29-4-479. [DOI] [PubMed] [Google Scholar]
- Orth DN, Besser GM, King PH, Nicholson WE. Free-running circadian plasma cortisol rhythm in a blind human subject. Clin Endocrinol. 1979;10:603–617. doi: 10.1111/j.1365-2265.1979.tb02120.x. [DOI] [PubMed] [Google Scholar]
- Oster MH, Castonguay TW, Keen CL, Stern JS. Circadian rhythm of corticosterone in diabetic rats. Life Sci. 1988;43:1643–1645. doi: 10.1016/0024-3205(88)90536-x. [DOI] [PubMed] [Google Scholar]
- Oster H, Damerow S, Kiessling S, Jakubcakova V, Abraham D, Tian J, Hoffmann MW, Eichele G. The circadian rhythm of glucocorticoids is regulated by a gating mechanism residing in the adrenal cortical clock. Cell Metab. 2006;4:163–173. doi: 10.1016/j.cmet.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Panda S, Antoch MP, Miller BH, Su AI, Schook AB, Straume M, Schultz PG, Kay SA, Takahashi JS, Hogenesch JB. Coordinated transcription of key pathways in the mouse by the circadian clock. Cell. 2002a;109:307–320. doi: 10.1016/s0092-8674(02)00722-5. [DOI] [PubMed] [Google Scholar]
- Panda S, Hogenesch JB, Kay SA. Circadian rhythms from flies to human. Nature. 2002b;417:329–335. doi: 10.1038/417329a. [DOI] [PubMed] [Google Scholar]
- Pedrazzoli M, Secolin R, Esteves LO, Pereira DS, Koike Bdel V, Louzada FM, Lopes-Cendes I, Tufik S. Interactions of polymorphisms in different clock genes associated with circadian phenotypes in humans. Genet Mol Biol. 2010;33:627–632. doi: 10.1590/S1415-47572010005000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peschke E, Muhlbauer E. New evidence for a role of melatonin in glucose regulation. Best Pract Res Clin Endocrinol Metab. 2010;24:829–841. doi: 10.1016/j.beem.2010.09.001. [DOI] [PubMed] [Google Scholar]
- Preitner N, Damiola F, Lopez-Molina L, Zakany J, Duboule D, Albrecht U, Schibler U. The orphan nuclear receptor REV-ERBalpha controls circadian transcription within the positive limb of the mammalian circadian oscillator. Cell. 2002;110:251–260. doi: 10.1016/s0092-8674(02)00825-5. [DOI] [PubMed] [Google Scholar]
- Ralph MR, Foster RG, Davis FC, Menaker M. Transplanted suprachiasmatic nucleus determines circadian period. Science. 1990;247:975–978. doi: 10.1126/science.2305266. [DOI] [PubMed] [Google Scholar]
- Ramsey KM, Yoshino J, Brace CS, Abrassart D, Kobayashi Y, Marcheva B, Hong HK, Chong JL, Buhr ED, Lee C, et al. Circadian clock feedback cycle through NAMPT-mediated NAD+ biosynthesis. Science. 2009;324:1638–1646. doi: 10.1126/science.1171641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy AB, Karp NA, Maywood ES, Sage EA, Deery M, O'Neill JS, Wong GK, Chesham J, Odell M, Lilley KS, et al. Circadian orchestration of the hepatic proteome. Curr Biol. 2006;16:1107–1115. doi: 10.1016/j.cub.2006.04.026. [DOI] [PubMed] [Google Scholar]
- Reiter RJ. Pineal gland interface between the photoperiodic environment and the endocrine system. Trends Endocrinol Metab. 1991;2:13–19. doi: 10.1016/1043-2760(91)90055-r. [DOI] [PubMed] [Google Scholar]
- Reppert SM, Weaver DR. Coordination of circadian timing in mammals. Nature. 2002;418:935–941. doi: 10.1038/nature00965. [DOI] [PubMed] [Google Scholar]
- Rey G, Cesbron F, Rougemont J, Reinke H, Brunner M, Naef F. Genome-wide and phase-specific DNA-binding rhythms of BMAL1 control circadian output functions in mouse liver. PLoS Biol. 2011;9:e1000595. doi: 10.1371/journal.pbio.1000595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ripperger JA, Schibler U. Rhythmic CLOCK-BMAL1 binding to multiple E-box motifs drives circadian Dbp transcription and chromatin transitions. Nat Genet. 2006;38:369–374. doi: 10.1038/ng1738. [DOI] [PubMed] [Google Scholar]
- Rodgers JT, Lerin C, Haas W, Gygi SP, Spiegelman BM, Puigserver P. Nutrient control of glucose homeostasis through a complex of PGC-1alpha and SIRT1. Nature. 2005;434:113–118. doi: 10.1038/nature03354. [DOI] [PubMed] [Google Scholar]
- Rodriguez de Fonseca F, Navarro M, Gomez R, Escuredo L, Nava F, Fu J, Murillo-Rodriguez E, Giuffrida A, LoVerme J, Gaetani S, et al. An anorexic lipid mediator regulated by feeding. Nature. 2001;414:209–212. doi: 10.1038/35102582. [DOI] [PubMed] [Google Scholar]
- Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22:939–943. doi: 10.1016/j.cub.2012.03.038. [DOI] [PubMed] [Google Scholar]
- Ronn T, Wen J, Yang Z, Lu B, Du Y, Groop L, Hu R, Ling C. A common variant in MTNR1B, encoding melatonin receptor 1B, is associated with type 2 diabetes and fasting plasma glucose in Han Chinese individuals. Diabetologia. 2009;52:830–833. doi: 10.1007/s00125-009-1297-8. [DOI] [PubMed] [Google Scholar]
- Rudic RD, McNamara P, Curtis AM, Boston RC, Panda S, Hogenesch JB, Fitzgerald GA. BMAL1 and CLOCK, two essential components of the circadian clock, are involved in glucose homeostasis. PLoS Biol. 2004;2:e377. doi: 10.1371/journal.pbio.0020377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudic RD, McNamara P, Reilly D, Grosser T, Curtis AM, Price TS, Panda S, Hogenesch JB, FitzGerald GA. Bioinformatic analysis of circadian gene oscillation in mouse aorta. Circulation. 2005;112:2716–2724. doi: 10.1161/CIRCULATIONAHA.105.568626. [DOI] [PubMed] [Google Scholar]
- Rutter J, Reick M, Wu LC, McKnight SL. Regulation of clock and NPAS2 DNA binding by the redox state of NAD cofactors. Science. 2001;293:510–514. doi: 10.1126/science.1060698. [DOI] [PubMed] [Google Scholar]
- Sadacca LA, Lamia KA, Delemos AS, Blum B, Weitz CJ. An intrinsic circadian clock of the pancreas is required for normal insulin release and glucose homeostasis in mice. Diabetologia. 2010;54:120–124. doi: 10.1007/s00125-010-1920-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahar S, Nin V, Barbosa MT, Chini EN, Sassone-Corsi P. Altered behavioral and metabolic circadian rhythms in mice with disrupted NAD+ oscillation. Aging. 2011;3:794–802. doi: 10.18632/aging.100368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakamoto K, Nagase T, Fukui H, Horikawa K, Okada T, Tanaka H, Sato K, Miyake Y, Ohara O, Kako K, Ishida N. Multitissue circadian expression of rat period homolog (rPer2) mRNA is governed by the mammalian circadian clock, the suprachiasmatic nucleus in the brain. J Biol Chem. 1998;273:27039–27042. doi: 10.1074/jbc.273.42.27039. [DOI] [PubMed] [Google Scholar]
- Saper CB, Lu J, Chou TC, Gooley J. The hypothalamic integrator for circadian rhythms. Trends Neurosci. 2005;28:152–157. doi: 10.1016/j.tins.2004.12.009. [DOI] [PubMed] [Google Scholar]
- Sato TK, Panda S, Miraglia LJ, Reyes TM, Rudic RD, McNamara P, Naik KA, FitzGerald GA, Kay SA, Hogenesch JB. A functional genomics strategy reveals Rora as a component of the mammalian circadian clock. Neuron. 2004;43:527–537. doi: 10.1016/j.neuron.2004.07.018. [DOI] [PubMed] [Google Scholar]
- Saunders LR, Verdin E. Sirtuins: critical regulators at the crossroads between cancer and aging. Oncogene. 2007;26:5489–5504. doi: 10.1038/sj.onc.1210616. [DOI] [PubMed] [Google Scholar]
- Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA. 2009;106:4453–4458. doi: 10.1073/pnas.0808180106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmutz I, Ripperger JA, Baeriswyl-Aebischer S, Albrecht U. The mammalian clock component PERIOD2 coordinates circadian output by interaction with nuclear receptors. Genes Dev. 2010;24:345–357. doi: 10.1101/gad.564110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwer B, Bunkenborg J, Verdin RO, Andersen JS, Verdin E. Reversible lysine acetylation controls the activity of the mitochondrial enzyme acetyl-CoA synthetase 2. Proc Natl Acad Sci USA. 2006;103:10224–10229. doi: 10.1073/pnas.0603968103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimazu T, Hirschey MD, Hua L, Dittenhafer-Reed KE, Schwer B, Lombard DB, Li Y, Bunkenborg J, Alt FW, Denu JM, et al. SIRT3 deacetylates mitochondrial 3-hydroxy-3-methylglutaryl CoA synthase 2 and regulates ketone body production. Cell Metab. 2010;12:654–661. doi: 10.1016/j.cmet.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimba S, Ishii N, Ohta Y, Ohno T, Watabe Y, Hayashi M, Wada T, Aoyagi T, Tezuka M. Brain and muscle Arnt-like protein-1 (BMAL1), a component of the molecular clock, regulates adipogenesis. Proc Natl Acad Sci USA. 2005;102:12071–12076. doi: 10.1073/pnas.0502383102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimomura Y, Takahashi M, Shimizu H, Sato N, Uehara Y, Negishi M, Inukai T, Kobayashi I, Kobayashi S. Abnormal feeding behavior and insulin replacement in STZ-induced diabetic rats. Physiol Behav. 1990;47:731–734. doi: 10.1016/0031-9384(90)90086-j. [DOI] [PubMed] [Google Scholar]
- Silver R, LeSauter J, Tresco PA, Lehman MN. A diffusible coupling signal from the transplanted suprachiasmatic nucleus controlling circadian locomotor rhythms. Nature. 1996;382:810–813. doi: 10.1038/382810a0. [DOI] [PubMed] [Google Scholar]
- Sinha MK, Ohannesian JP, Heiman ML, Kriauciunas A, Stephens TW, Magosin S, Marco C, Caro JF. Nocturnal rise of leptin in lean, obese, and non-insulin-dependent diabetes mellitus subjects. J Clin Invest. 1996;97:1344–1347. doi: 10.1172/JCI118551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slat E, Freeman GM, Jr, Herzog ED. The clock in the brain: neurons, glia and networks in daily rhythms. In: Kramer A, Merrow M, editors. Circadian clocks, vol 217, Handbook of experimental pharmacology. Springer; Heidelberg: 2013. [DOI] [PubMed] [Google Scholar]
- So AY, Bernal TU, Pillsbury ML, Yamamoto KR, Feldman BJ. Glucocorticoid regulation of the circadian clock modulates glucose homeostasis. Proc Natl Acad Sci USA. 2009;106:17582–17587. doi: 10.1073/pnas.0909733106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Someya S, Yu W, Hallows WC, Xu J, Vann JM, Leeuwenburgh C, Tanokura M, Denu JM, Prolla TA. Sirt3 mediates reduction of oxidative damage and prevention of age-related hearing loss under caloric restriction. Cell. 2010;143:802–812. doi: 10.1016/j.cell.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonoda J, Pei L, Evans RM. Nuclear receptors: decoding metabolic disease. FEBS Lett. 2008;582:2–9. doi: 10.1016/j.febslet.2007.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sookoian S, Castano G, Gemma C, Gianotti TF, Pirola CJ. Common genetic variations in CLOCK transcription factor are associated with nonalcoholic fatty liver disease. World J Gastroenterol. 2007;13:4242–4248. doi: 10.3748/wjg.v13.i31.4242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sookoian S, Gemma C, Gianotti TF, Burgueno A, Castano G, Pirola CJ. Genetic variants of Clock transcription factor are associated with individual susceptibility to obesity. Am J Clin Nutr. 2008;87:1606–1615. doi: 10.1093/ajcn/87.6.1606. [DOI] [PubMed] [Google Scholar]
- Sookoian S, Gianotti TF, Burgueno A, Pirola CJ. Gene-gene interaction between serotonin transporter (SLC6A4) and CLOCK modulates the risk of metabolic syndrome in rotating shiftworkers. Chronobiol Int. 2010;27:1202–1218. doi: 10.3109/07420528.2010.496913. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Tasali E, Leproult R, Van Cauter E. Effects of poor and short sleep on glucose metabolism and obesity risk. Nat Rev Endocrinol. 2009;5:253–261. doi: 10.1038/nrendo.2009.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staels B. When the Clock stops ticking, metabolic syndrome explodes. Nat Med. 2006;12:54–55. doi: 10.1038/nm0106-54. discussion 55. [DOI] [PubMed] [Google Scholar]
- Staiger D, Koster T. Spotlight on post-transcriptional control in the circadian system. Cell Mol Life Sci. 2011;68:71–83. doi: 10.1007/s00018-010-0513-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staiger H, Machicao F, Schafer SA, Kirchhoff K, Kantartzis K, Guthoff M, Silbernagel G, Stefan N, Haring HU, Fritsche A. Polymorphisms within the novel type 2 diabetes risk locus MTNR1B determine beta-cell function. PLoS One. 2008;3:e3962. doi: 10.1371/journal.pone.0003962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokkan KA, Yamazaki S, Tei H, Sakaki Y, Menaker M. Entrainment of the circadian clock in the liver by feeding. Science. 2001;291:490–493. doi: 10.1126/science.291.5503.490. [DOI] [PubMed] [Google Scholar]
- Storch KF, Lipan O, Leykin I, Viswanathan N, Davis FC, Wong WH, Weitz CJ. Extensive and divergent circadian gene expression in liver and heart. Nature. 2002;417:78–83. doi: 10.1038/nature744. [DOI] [PubMed] [Google Scholar]
- Szafarczyk A, Ixart G, Malaval F, Nouguier-Soule J, Assenmacher I. Effects of lesions of the suprachiasmatic nuclei and of p-chlorophenylalanine on the circadian rhythms of adrenocorticotrophic hormone and corticosterone in the plasma, and on locomotor activity of rats. J Endocrinol. 1979;83:1–16. doi: 10.1677/joe.0.0830001. [DOI] [PubMed] [Google Scholar]
- Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi F, Katsuya T, Chakrewarthy S, Yamamoto K, Fujioka A, Serizawa M, Fujisawa T, Nakashima E, Ohnaka K, Ikegami H, et al. Common variants at the GCK, GCKR, G6PC2-ABCB11 and MTNR1B loci are associated with fasting glucose in two Asian populations. Diabetologia. 2010;53:299–308. doi: 10.1007/s00125-009-1595-1. [DOI] [PubMed] [Google Scholar]
- Tam CH, Ho JS, Wang Y, Lee HM, Lam VK, Germer S, Martin M, So WY, Ma RC, Chan JC, et al. Common polymorphisms in MTNR1B, G6PC2 and GCK are associated with increased fasting plasma glucose and impaired beta-cell function in Chinese subjects. PLoS One. 2010;5:e11428. doi: 10.1371/journal.pone.0011428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teboul M, Grechez-Cassiau A, Guillaumond F, Delaunay F. How nuclear receptors tell time. J Appl Physiol. 2009;107:1965–1971. doi: 10.1152/japplphysiol.00515.2009. [DOI] [PubMed] [Google Scholar]
- Torra IP, Tsibulsky V, Delaunay F, Saladin R, Laudet V, Fruchart JC, Kosykh V, Staels B. Circadian and glucocorticoid regulation of Rev-erbalpha expression in liver. Endocrinology. 2000;141:3799–3806. doi: 10.1210/endo.141.10.7708. [DOI] [PubMed] [Google Scholar]
- Turek FW, Joshu C, Kohsaka A, Lin E, Ivanova G, McDearmon E, Laposky A, Losee-Olson S, Easton A, Jensen DR, et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science. 2005;308:1043–1045. doi: 10.1126/science.1108750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Cauter E, Polonsky KS, Scheen AJ. Roles of circadian rhythmicity and sleep in human glucose regulation. Endocr Rev. 1997;18:716–738. doi: 10.1210/edrv.18.5.0317. [DOI] [PubMed] [Google Scholar]
- Vogel G. Cell biology. Telling time without turning on genes. Science. 2011;331:391. doi: 10.1126/science.331.6016.391. [DOI] [PubMed] [Google Scholar]
- Wang N, Yang G, Jia Z, Zhang H, Aoyagi T, Soodvilai S, Symons JD, Schnermann JB, Gonzalez FJ, Litwin SE, Yang T. Vascular PPARgamma controls circadian variation in blood pressure and heart rate through Bmal1. Cell Metab. 2008;8:482–491. doi: 10.1016/j.cmet.2008.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsbacher LD, Yamazaki S, Herzog ED, Song EJ, Radcliffe LA, Abe M, Block G, Spitznagel E, Menaker M, Takahashi JS. Photic and circadian expression of luciferase in mPeriod1-luc transgenic mice invivo. Proc Natl Acad Sci USA. 2002;99:489–494. doi: 10.1073/pnas.012248599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woon PY, Kaisaki PJ, Braganca J, Bihoreau MT, Levy JC, Farrall M, Gauguier D. Aryl hydrocarbon receptor nuclear translocator-like (BMAL1) is associated with susceptibility to hypertension and type 2 diabetes. Proc Natl Acad Sci USA. 2007;104:14412–14417. doi: 10.1073/pnas.0703247104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto T, Nakahata Y, Tanaka M, Yoshida M, Soma H, Shinohara K, Yasuda A, Mamine T, Takumi T. Acute physical stress elevates mouse period1 mRNA expression in mouse peripheral tissues via a glucocorticoid-responsive element. J Biol Chem. 2005;280:42036–42043. doi: 10.1074/jbc.M509600200. [DOI] [PubMed] [Google Scholar]
- Yamazaki S, Numano R, Abe M, Hida A, Takahashi R, Ueda M, Block GD, Sakaki Y, Menaker M, Tei H. Resetting central and peripheral circadian oscillators in transgenic rats. Science. 2000;288:682–685. doi: 10.1126/science.288.5466.682. [DOI] [PubMed] [Google Scholar]
- Yang X, Downes M, Yu RT, Bookout AL, He W, Straume M, Mangelsdorf DJ, Evans RM. Nuclear receptor expression links the circadian clock to metabolism. Cell. 2006;126:801–810. doi: 10.1016/j.cell.2006.06.050. [DOI] [PubMed] [Google Scholar]
- Yang X, Lamia KA, Evans RM. Nuclear receptors, metabolism, and the circadian clock. Cold Spring Harb Symp Quant Biol. 2007;72:387–394. doi: 10.1101/sqb.2007.72.058. [DOI] [PubMed] [Google Scholar]
- Yang S, Liu A, Weidenhammer A, Cooksey RC, McClain D, Kim MK, Aguilera G, Abel ED, Chung JH. The role of mPer2 clock gene in glucocorticoid and feeding rhythms. Endocrinology. 2009;150:2153–2160. doi: 10.1210/en.2008-0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildiz BO, Suchard MA, Wong ML, McCann SM, Licinio J. Alterations in the dynamics of circulating ghrelin, adiponectin, and leptin in human obesity. Proc Natl Acad Sci USA. 2004;101:10434–10439. doi: 10.1073/pnas.0403465101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin L, Wu N, Curtin JC, Qatanani M, Szwergold NR, Reid RA, Waitt GM, Parks DJ, Pearce KH, Wisely GB, Lazar MA. Rev-erbalpha, a heme sensor that coordinates metabolic and circadian pathways. Science. 2007;318:1786–1789. doi: 10.1126/science.1150179. [DOI] [PubMed] [Google Scholar]
- Yoo SH, Yamazaki S, Lowrey PL, Shimomura K, Ko CH, Buhr ED, Siepka SM, Hong HK, Oh WJ, Yoo OJ, et al. PERIOD2::LUCIFERASE real-time reporting of circadian dynamics reveals persistent circadian oscillations in mouse peripheral tissues. Proc Natl Acad Sci USA. 2004;101:5339–5346. doi: 10.1073/pnas.0308709101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Kaasik K, Blackburn MR, Lee CC. Constant darkness is a circadian metabolic signal in mammals. Nature. 2006;439:340–343. doi: 10.1038/nature04368. [DOI] [PubMed] [Google Scholar]
- Zhang EE, Liu Y, Dentin R, Pongsawakul PY, Liu AC, Hirota T, Nusinow DA, Sun X, Landais S, Kodama Y, et al. Cryptochrome mediates circadian regulation of cAMP signaling and hepatic gluconeogenesis. Nat Med. 2010;16:1152–1156. doi: 10.1038/nm.2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuber AM, Centeno G, Pradervand S, Nikolaeva S, Maquelin L, Cardinaux L, Bonny O, Firsov D. Molecular clock is involved in predictive circadian adjustment of renal function. Proc Natl Acad Sci USA. 2009;106:16523–16528. doi: 10.1073/pnas.0904890106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvonic S, Ptitsyn AA, Conrad SA, Scott LK, Floyd ZE, Kilroy G, Wu X, Goh BC, Mynatt RL, Gimble JM. Characterization of peripheral circadian clocks in adipose tissues. Diabetes. 2006;55:962–970. doi: 10.2337/diabetes.55.04.06.db05-0873. [DOI] [PubMed] [Google Scholar]