Abstract
Intussusception is extremely rare in preterm neonates and is often confused with necrotizing enterocolitis leading to considerable delay in its diagnosis. We present a case report of a preterm with colo-colic intussusception, which was diagnosed preoperatively using ultrasound. We examine the pitfalls in diagnosing intussusception in preterm neonates. Intussusception, though rare, should be considered in the differential diagnosis while managing a preterm with abdominal symptomatology. Abdominal ultrasound is useful in diagnosing intussusception in neonates.
Keywords: Abdominal ultrasonography, intussusception, necrotizing enterocolitis, preterm neonate
INTRODUCTION
Intussusception is a rare diagnosis in neonates. It is extremely rare in preterms.[1] In preterm neonates, it is often missed, its presentation being confused with that of necrotizing enterocolitis.[2] Intussusception is often difficult to diagnose based only on clinical presentation and X-rays. Majority of the reported cases of intussusception were diagnosed intraoperatively.[1,3] Most of the cases reported involved the small bowel.[1] We report a case of intussusception (colocolic variety) in a preterm baby, which was diagnosed early using ultrasound.
CASE REPORT
A preterm neonate with gestational age 34 weeks was delivered by a cesarean section done due to non-reassuring CTG (cardiotocography). Apgar was 8, 9, 9 at 1, 5, 10 minutes, respectively. Birth weight was 2296 grams. Upon admission, baby had mild tachypnea with no grunting and no intercostal retractions. Abdomen was soft, no organomegaly or any mass were palpable, and anus was patent. Baby had normal male genitalia. Baby was managed conservatively with oxygen via oxyhood. Baby did not require intubation/ventilation.
Baby was kept NPO since admission and was given IV fluids. As per protocol, baby was started on IV Ampicillin and IV Amikacin. Baby was hemodynamically stable, maintaining euglycemia, maintain oxygen saturation. Baby passed meconium at 10 hours of age.
At the age of 40 hours, bloody stools were noticed in the pampers. Coagulation profile was normal. Sepsis work up was done, which was normal. Possibility of NEC was considered. IV Metronidazole was added. X-Ray thoracoabdomen was done [Figure 1a and b]. The radiograph showed no pathognomic features of NEC (e.g. pneumatosis intestinalis and portal venous gas) and no features of intestinal obstruction. Baby remained hemodynamically stable. Baby did not have any vomiting and did not have any abdominal distension. An orogastric tube was in situ, and the gastric aspirate was not bilious. No milk feeds were given to the baby since admission. Baby continued to pass bloody stools. Clinically, no mass was palpable per abdomen. An urgent abdominal ultrasound was arranged at the age of 68 hours of age. Abdominal ultrasound [Figure 2] showed classical ‘target sign’ in left lumbar region. A diagnosis of intussusception was made.
Figure 1.

(a and b) Thoracoabdomen X-ray AP and Cross Table Lateral View done at 48 hours of age. (a) (Left) – X-ray AP view, (b) (Right) - X-ray Cross-Table Lateral view. No abnormality was detected in the abdomen in both AP and Cross Table-Lateral Views. There were no dilated loops of bowel, no pneumatosis intestinalis, no portal gas shadows, no pneumoperitoneum
Figure 2.
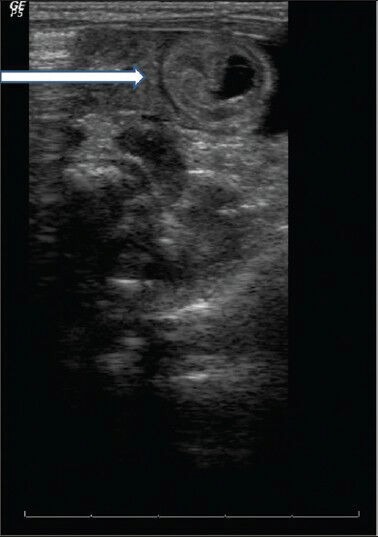
Ultrasound Abdomen (68 hours of life) - Left sided (lumbar) target sign (white arrow) as noted by invaginated bowel loop and recipient loop with minimal free fluid surrounding. Picture suggestive of intussusception
Baby was taken for urgent surgery. Laparotomy revealed colo-colic intussusception fixed in the splenic flexure region. Attempt at reduction failed. En bloc resection and primary end to end anastomosis was done. No lead point was identified. Post-operative course was uneventful. Baby was discharged 2 weeks later.
DISCUSSION
Though intussusception is common in infants 6 to 18 months of age;[3] however, in the NICU, it is a rare diagnosis.[2] Intussusception is extremely rare in preterms.[4] This often leads to an initial misdiagnosis causing a significant delay between the onset of symptoms and the establishment of a definitive treatment.[4] Its presentation closely mimics NEC, but management of intussusception is diametrically opposite to the conservative management, which preterms with NEC receive.[4,5]
The delay in the diagnosis of intussusceptions in neonates is considerable (reports include mean of 10 days[1] to 19 days[3]). This delay increases the risk of developing compromised bowel.[6] Intussusception was usually discovered during laparotomy.[4,6]
Preoperative diagnosis (either by contrast enema or by abdominal sonography) of intussusceptions in neonates is reported in only a few cases.[1,4,7] Our case is one of the handful of reported cases where diagnosis of intussusceptions was made early in the course, which led to early operative management.
The features in preterm neonates with intussusception mimic those of NEC[1,2,3,6](abdominal distension, feeding intolerance, vomiting, and bloody stools). Clinical features usually seen in older infants/toddlers like palpable abdominal mass, irritable crying indicative of colicky abdominal pain are rare in neonates.[2,5,6] In intussusception in preterm babies, symptoms are uniquely localized to the abdomen and the general condition does not deteriorate until perforation supervenes in contrast to NEC where abdominal signs go hand in hand with general deterioration.[2] In our case, other than bloody stools, baby was relatively stable.
The majority of reported cases in preterms involve the small bowel.[1,4,8] Our case of colocolic intussusception in a preterm baby is very rare. AL-Jahdali et al.[9] have reported a colocolic intussusception in a preterm baby associated with malrotation (Waugh syndrome) with an identifiable lead point (intestinal lymphangioma). In our case, there was no malrotation and no lead-point was identified. Unlike in full-term neonates where an underlying pathological lesion may be seen, in majority of the preterm infants, no anatomical abnormalities are found on surgery.[6] Etiology of intussusception in preterms remains unclear.[6,7,8]
Neonatal intussusception does not have any classical radiological signs. The most common imaging findings in preterms with intussusception are signs of ileus such as dilation of bowel loops[1] and occasionally gas-fluid levels.[6] This is in contrast to the hallmark of NEC i.e. pneumatosis with generalized bowel distension. However, in our case, the X-ray was generally unremarkable. Moreover, only about half the cases of NEC have Pneumatosis intestinalis and/or portal venous gas in the X-ray.[1,8]
Using contrast enema also does not help in reaching a diagnosis.[1,3] Though Barium enema is helpful in diagnosing intussusception with colonic component (as is seen in term neonates), it often misses the diagnosis in preterm neonates with intussusception.[2,8] This is because majority of intussusception in preterms is usually enteric without colonic component[3] and does not have complete intestinal obstruction. Moreover, contrast enemas may even be harmful because frequently the bowel is already compromised at the time of investigation, increasing the risk of perforation.[6]
The diagnosis in our case was made using abdominal ultrasound. There are numerous reports[1,2,4,6,7] showing its role in diagnosing intussusception in neonates. Its use in pediatric intussusception has been well established. Furthermore, ultrasound has numerous advantages including the ability to document ileo-ileal intussusception, the absence of ionizing radiation to the neonate, and identification of lead points.[4] Shad et al.[10] in their case report (ileo-cecal intussusception in a preterm) could not detect intussusception using abdominal ultrasound. They believe that a superficial right lying sigmoid colon along with dilated small bowel loops could have obscured the visualization of the cecum.
CONCLUSION
Successful management of intussusception in preterms requires a timely and accurate diagnosis.[8] Not all preterms with bowel symptomatology have NEC. The possibility of intussusception should be suspected in the baby who is diagnosed presumptively with NEC but who has a more stable course than would normally be expected.[2] Abdominal ultrasound is useful in making a diagnosis of intussusception in neonates and should be considered early in the work-up of a neonate with abdominal symptomatology.[1,3]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Avansino JR, Bjerke S, Hendrickson M, Stelzner M, Sawin R. Clinical features and treatment outcome of intussusception in premature neonates. J Pediatr Surg. 2003;38:1818–21. doi: 10.1016/j.jpedsurg.2003.08.048. [DOI] [PubMed] [Google Scholar]
- 2.Wang NL, Yeh ML, Chang PY, Sheu JC, Chen CC, Lee HC, et al. Prenatal and neonatal intussusception. Pediatr Surg Int. 1998;13:232–6. doi: 10.1007/s003830050305. [DOI] [PubMed] [Google Scholar]
- 3.Mooney DP, Steinthorsson G, Shorter NA. Perinatal intussusception in premature infants. J Pediatr Surg. 1996;31:695–7. doi: 10.1016/s0022-3468(96)90676-4. [DOI] [PubMed] [Google Scholar]
- 4.Martínez Biarge M, García-Alix A, Luisa del Hoyo M, Alarcón A, Sáenz de Pipaón M, Hernández F, et al. Intussusception in a preterm neonate; a very rare, major intestinal problem-systematic review of cases. J Perinat Med. 2004;32:190–4. doi: 10.1515/JPM.2004.036. [DOI] [PubMed] [Google Scholar]
- 5.Yoo RP, Touloukian RJ. Intussusception in the newborn: A unique clinical entity. J Pediatr Surg. 1974;9:495–8. doi: 10.1016/s0022-3468(74)80012-6. [DOI] [PubMed] [Google Scholar]
- 6.Görgen-Pauly U, Schultz C, Kohl M, Sigge W, Möller J, Gortner L. Intussusception in preterm infants: Case report and literature review. Eur J Pediatr. 1999;158:830–2. doi: 10.1007/s004310051216. [DOI] [PubMed] [Google Scholar]
- 7.Ueki I, Nakashima E, Kumagai M, Tananari Y, Kimura A, Fukuda S, et al. Intussusception in neonates: Analysis of 14 Japanese patients. J Paediatr Child Health. 2004;40:388–91. doi: 10.1111/j.1440-1754.2004.00408.x. [DOI] [PubMed] [Google Scholar]
- 8.Loukas I, Baltogiannis N, Plataras C, Skiathitou A-V, Siahanidou S, Geroulanos G. Intussusception in a premature neonate: A rare often misdiagnosed cause of intestinal obstruction. Case Rep Med. 2009;2009:607989. doi: 10.1155/2009/607989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Jahdali A, Lees GM, Gay DP, Al-Sairafi R. Colocolic intussusception in a preterm infant with intestinal malrotation. J Pediatr Surg. 2009;44:e17–8. doi: 10.1016/j.jpedsurg.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 10.Shad J, Biswas R. Ileo-colic intussusception in premature neonate. BMJ Case Rep. 2011 doi: 10.1136/bcr.11.2011.5109. [DOI] [PMC free article] [PubMed] [Google Scholar]


