Abstract
A considerable number of intraventricular hemorrhages (IVH) occur within the first hours of life (HOL). Temporality between IVH and its antecedents as well as a consistent definition of “early IVH” is lacking in a large and growing body of literature. We performed a systematic review of prospective studies that reported onset of IVH in preterm neonates within the first HOL and afterwards. The English literature was searched using three databases up to March 2013. Four timing periods of IVH can be compared in 16 identified studies: 0-6; 7-12; 13-24; after 24 HOL. The 0-6 and after 24 HOL were the major modes of IVH timing. Pooled IVH proportions were estimated through a meta-analysis of studies that were conducted after antenatal steroid and surfactant era. In neonates weighing ≤1500 g at birth: 48% of IVH (95% CI: 42-58%, 5 studies, 279 IVH cases) occurred during 0-6 HOL and 38% (95% CI: 19-57%, 4 studies, 241 IVH cases) after 24 HOL. The 0-6 HOL is the shortest, most vulnerable period for IVH, thus, an early IVH is an IVH occurs in it. Such early IVH had prognostic, etiological/preventive and medicolegal implications. Accordingly, preterm neonates at risk of IVH should have their first routine screening head ultrasound at about 6 HOL. Future research exploring the antecedents of IVH should guaranty the temporality between these antecedents and IVH. Additional research will be required to determine whether the long term neurological outcomes of early and late IVH are the same.
Keywords: Early intraventricular hemorrhage, head ultrasound, intraventricular hemorrhage, preterm neonates, timing of intraventricular hemorrhage, very low birth weight
INTRODUCTION
Intraventricular hemorrhage (IVH) in preterm neonates is a devastating consequence of prematurity that has both perinatal and postnatal antecedents.[1] Knowing the timing of IVH is a prerequisite for identifying its antecedents and subsequently applying preventive measures.[2,3] Studies before and after the widespread use of antenatal steroid and surfactant therapy have shown that IVH may occur as early as the 1st min.[4,5,6,7,8] This observation suggests that IVH may occur in utero, intrapartum or during the early postnatal period.[4,5,6,7,8] A large body of evidence has shown that a considerable number of IVH cases occur during the first hours of life (HOL).[3,5,6,7,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24] Reports in the literature from the 1980s and 1990s established that IVH occurring within the first HOL and later-occurring IVH must be analyzed separately as their antecedents may be different.[25,26,27] However, a more recent large and growing body of literature has considered early and late IVH as a single entity and has neglected the fact that a significant number of IVH cases may have occurred prior to the investigator's study intervention or antecedents of IVH. Underrepresentation of the studies that have carefully reported the timing of IVH and inconsistency in defining the term “early IVH” may have contributed to this negligence. Therefore, the aim of this article is to systematically review and analyze numerous previous studies that evaluated or reported onset of IVH within the first HOL and afterwards. Based on this analysis, we will propose a definition for early IVH as well as present clinical and research implications. We hope this review will increase the mindfulness of early IVH in clinical practice and research.
BIBLIOGRAPHIC SEARCH
The bibliographic search of English-language literature was performed electronically using PubMed and EMBASE databases. The search was limited to prospective studies published until March 2013. The following text words were used: “early [title]”, “timing [title]”, “intraventricular”, “periventricular”, “peri-intraventricular”, “subependymal”, “germinal matrix”, “intracranial”, “cerebral”, “cerebroventricular”, “cranial” and “brain”. The following Mesh terms were used for Pubmed: “hemorrhage”, “ultrasonography” and “infant, newborn”. The following Emtree terms were used for EMBASE: “brain hemorrhage”, “ultrasound”, “echoencephalography” and “newborn”. Google scholar database and reference lists of the selected articles were searched to find other relevant articles.
DESCRIPTION OF STUDIES
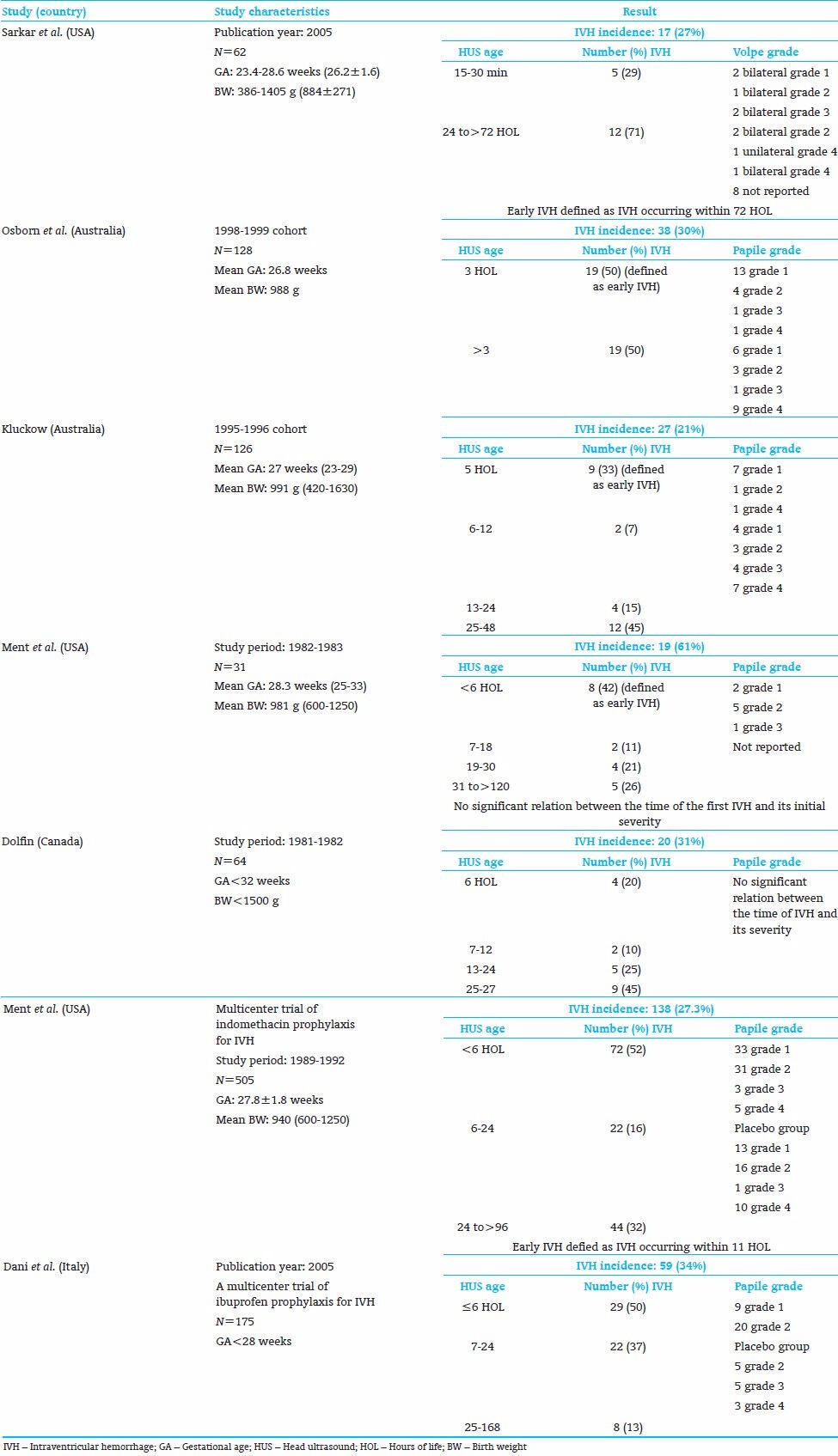
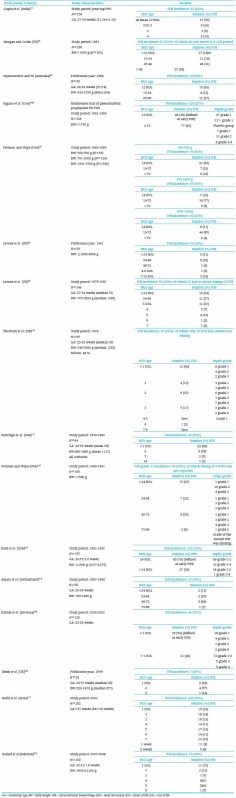
We abstracted 16 prospective studies in which the time interval of IVH occurrence within the first HOL was reported or could be inferred. Nine of these 16 studies included low birth weight (LBW, ≤2000 g) preterm neonates.[5,7,12,14,15,16,17,19,22,28] All these nine studies were conducted before widespread of antenatal steroid and surfactant era. One of them had two reports; a primary report on all study neonates and a secondary report on the subgroup of neonates delivered by cesarean section only.[5,13] The study of Paneth et al. has the largest number of neonates and the narrowest intervals of censored times to IVH.[7] The other seven of the abstracted 16 studies included very low birth weight (VLBW, ≤1500 g) preterm neonates.[3,6,11,18,20,21] Five of them were conducted after widespread of antenatal steroid and surfactant era.[6,15,17,20,21] Table 1 depicts a summary of LBW studies and Table 2 depicts a summary of VLBW studies. The studies in both tables are ordered by the earliest reported time of head ultrasound (HUS).
Table 1.
Prospective studies evaluating or reporting onset of IVH during the interval censored in low birth weight neonates

Table 2.
Prospective studies evaluating or reporting onset of IVH during the interval censored in very low birth weight neonates
Another 16 studies reported IVH timing were abstracted but were excluded from this review as they did not report exact timing of IVH within the first HOL [Appendix].
TIMING OF IVH OCCURRENCE
The distribution of IVH occurrence in four different time intervals (0-6 HOL, 7-12 HOL, 13-24 HOL and after 24 HOL) can be compared in the included 17 reports listed in Tables 1 and 2.[3,5,6,7,10,11,12,13,14,15,16,17,18,19,20,21,22] Figures 1 and 2 depict the percentage of IVH cases in each report that occurred during these 4 time intervals in LBW and VLBW, respectively. These plots show that timing of IVH is bimodal in both LBW and VLBW neonates. These two modes are 0-6 and after 24 HOL intervals. The 0-6 HOL interval is the major mode in half of both LBW [Figure 1] and VLBW studies [Figure 2]. The 0-6 HOL interval includes ≥50% of the IVH cases in half of both LBW[5,12,14,15,22] and VLBE studies.[11,20,21] The “after 24” HOL interval includes ≥50% of the IVH cases in only two LBW[13,16] and one VLBW studies.[6]
Figure 1.
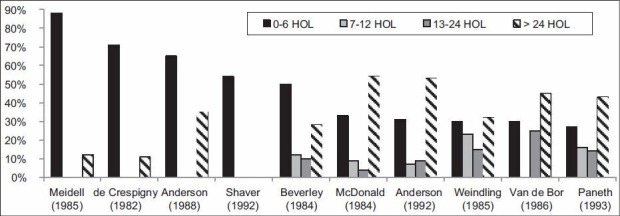
The percent of intraventricular hemorrhage cases that occurred during different hours of life periods in low birth weight neonates
Figure 2.
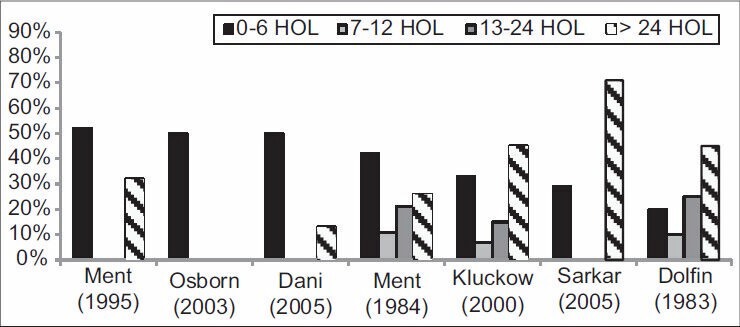
The percent of intraventricular hemorrhage cases that occurred during different hours of life periods in very low birth weight neonates
The discrepancies between some of these studies regarding the time period during which most IVH cases occur could be attributed to the methodological heterogeneity across these studies in terms of the exact timing of HUS and the study population. One of the LBW studies that reported ≥50% of the IVH cases occurring after 24 HOL was a secondary report on cesarean section deliveries.[13] The primary report, which included both vaginal and cesarean section deliveries, indicated that at least 54% of the IVH cases occurred within the first 6 HOL, whereas the secondary report indicated that only 31% of the IVH cases occurred within the first 6 HOL.[5,13] It appears that the timing of IVH is related to the maturation of neonates. Perlman and Volpe have demonstrated that the first 18 HOL include 62%, 18% and 11% of the IVH cases reported among neonates with birth weights of 500-700 g, 701-1000 g and 1001-1500 g, respectively.[32] It has been reported that neonates who developed IVH before 12 HOL were born on average 2 weeks earlier than those who developed IVH after 48 HOL (27.5 vs. 29.5 weeks).[33]
A meta-analysis of proportions was performed to estimate pooled IVH proportions through Open Meta-Analyst software, Tufts University, USA.[34] We included studies that were conducted after antenatal steroid and surfactant era pursuing methodological homogeneity across the studies and harmony with the present practice. Thus, only the five VLBW studies that were conducted after antenatal steroid and surfactant era were included in the meta-analysis.[6,15,17,20,21] Pooled IVH proportion occurred during 0-6 HOL interval was calculated using a fixed-effect model with inverse variance weighting [Figure 3]. Pooled IVH proportion in 0-6 HOL interval is 48% (95% confidence interval 42-53%). Insignificant heterogeneity was observed: Q test with 4 degrees of freedom = 6.48, I^2 = 38%, P = 0.17, 5 studies, 279 IVH cases).[35] Pooled IVH proportion occurred after 24 HOL was calculated using a DerSimonian and Laird random-effect model [Figure 4]. Osborn et al. study was excluded from the meta-analysis as the IVH proportion after 24 HOL cannot be abstracted [Table 2].[15] Pooled IVH proportion after 24 HOL was 38% (95% confidence interval 19-57%). Significant heterogeneity was observed: Tau^2 = 0.03, Q test with 3 degrees of freedom = 29.25, I^2 = 90%, P < 0.01, 4 studies, 241 IVH cases).[35] These observations suggest that the first 6 HOL is the shortest, most vulnerable period of time for a neonate with respect to IVH.
Figure 3.

Forest plot of intraventricular hemorrhage proportion occurred during 0-6 h of life interval in very low birth weight neonates
Figure 4.
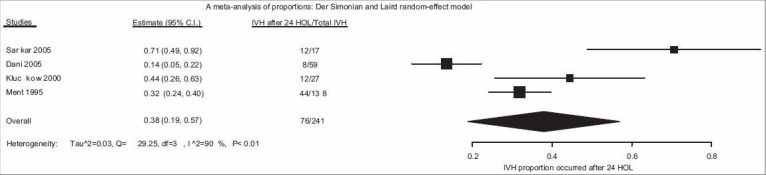
Forest plot of intraventricular hemorrhage proportion occurred after 24 h of life interval in very low birth weight neonates
WHY DOES DOCUMENTATION OF THE IVH STATUS WITHIN THE FIRST HOLMATTER?
Documentation of the IVH status within the first HOL is important due to its prognostic, etiological/preventive and medicolegal implications.[36]
The prognostic implications
The severity
The available evidence is inconclusive regarding whether the IVHs occurring within the first HOL are more severe initially than the later-occurring IVHs. According to some LBW [Table 1][5] and VLBW studies [Table 2],[3,6,18] both the IVHs occurring within the first HOL and the later-occurring IVHs had the same proportion of IVH grade 3-4 IVH cases. On the contrary, in other studies, the IVHs occurring within the first HOL had a significant less proportion of grade 3-4 IVH cases than the later-occurring IVHs in both LBW [Table 1][15,17] and VLBW population [Table 2].[20,21]
The progression to a higher grade
The risk of IVH progression is inversely related to the timing of the IVH occurrence in both LBW and VLBW preterm neonates. It has been demonstrated that a significant portion of the grade 1 or grade 2 IVH cases occurring within the first HOL progress to a higher grade.[5,8,14,15,17,18,21,22,24,37] This may account for the greater observed mortality risk associated with IVH that occurs within the first HOL.[18,22,37]
A small study on LBW preterm neonates from 1984 reported that progressed cases of IVH occurred at an earlier median HOL compared with non-progressed cases of IVH (35 vs. 48 HOL).[38] Another old report on LBW preterm neonates concluded that the majority of 20 IVH cases that were identified within the first 8 HOL progressed to a higher grade.[22] The exact number of IVH cases that progressed was not provided in this report. Meidell et al. found that in LBW preterm neonates 60% (9/15) of the IVH grade 1 cases identified at a mean of 2 HOL progressed to a higher grade by 3 DOL.[14] Shaver et al. found that in LBW preterm neonates 48% (13/27) of the IVH grade 1 identified at ≤1 HOL progressed to grade 2-3 versus 20% (3/15) of the same IVH grade identified at >1 HOL progressed to grade 2-3 (P = 0.07).[5] They found that 75% (12/16) of the IVH grade 2 identified at ≤1 HOL progressed to a higher grade, whereas only 31% (9/29) of the same IVH grade identified at >1 HOL progressed (P = 0.005).[5]
A report on VLBW neonates from 1984 concluded that cases of grade 1 IVH identified at a median of 12 HOL were more likely to progress than those identified at a median of 42 HOL.[24] The exact number of IVH cases that progressed was not provided in this report. One trial involving the use of indomethacin prophylaxis as an IVH prevention in VLBW neonates found that 63% (10/16) of the grade 1 IVH cases in the placebo group that were identified at 6 HOL progressed to grade 2 in five, grade 3 in four and grade 4 in one case.[8] Another trial involving the use of ibuprofen prophylaxis as an IVH prevention in VLBW neonates found that 44% (4/9) of the grade 1 IVH cases identified within 6 HOL progressed to a higher grade; three progressed to grade 2 and one case to grade 3.[21] Another study demonstrated that 5 of 6 (83%) IVH cases identified within the first 6 HOL in VLBW neonates and had repeated HUS progressed, in which three of them progressed to IVH grade 4, whereas none of the 11 IVH cases identified after 6 HOL progressed.[18] This study showed that IVH cases identified within the first 6 HOL had a significantly higher mortality rate than IVH cases identified after 6 HOL (6/8 [75%] vs. 2/11 [18%], P = 0.04).[18] A considerable number of IVH that were identified among two different cohorts of Australian VLBW preterm neonates at 5 (1995-1996 cohort) and 3 (1998-1999 cohort) HOL progressed to higher grades.[15,17] The total rate of IVH progression was 30% (3/9) among the 1995-1996 cohorts. Two of the seven (28%) of IVH grade1 progressed to grade 2 and the IVH grade 2 case progressed to grade 3 among the 1995-1996 cohorts.[17] The total rate of IVH progression was 37% (7/19) among the 1998-1999 cohorts.[15] Thirty eight percent (5/13) of IVH grade 1 progressed to a higher grade among the 1998-1999 cohorts. The proportion of IVH grade 3-4 among the IVH cases identified at 3 HOL was 11% (2/19) then subsequently increased to 37% (7/19).[15] Cerebral hypoperfusion may have contributed to the observed IVH progression as the superior vena cava flow was low in all three progressed IVH cases and normal in all the 6 non-progressed IVH cases in the 1995-1996 cohort.[17] The superior vena cava flow was low in 4 of the 7 progressed IVH cases in the 1998-1999 cohort.[15] Ment et al. in their study have reported that the proportion of IVH grade 3-4 among IVH cases identified during the first 5-11 HOL increased from 9% (4/43) to 28% (12/43) at 21 DOL in a preliminary report on 229 of 505 neonates enrolled in a multicenter trial investigated the use of indomethacin prophylaxis to prevent IVH.[37]
The neurological outcomes
A secondary report from the above-mentioned trial of Ment et al. is the only report that we are aware of that has addressed the long-term neurological outcomes of IVH occurring within the first 5-11 HOL.[39] The study included 29 neonates with IVH identified at 5-11 HOL and the controls were a combination of 32 neonates with IVH identified after 11 HOL and 217 neonates with no IVH. The report demonstrated that the neurological outcomes at 3 years corrected for age for patients with IVH were worse than those observed in the controls. This result is axiomatic as 87% (217/249) of controls had no IVH at any time. Unfortunately, the small numbers of early and late IVH cases preclude a meaningful comparison of the neurological outcomes of these IVH cases.
Nevertheless, the comparisons between the severity, progression and the short- and long-term outcomes of the IVH cases that were identified within the first HOL and those that were identified later were not the primary objective of the above cited studies.
The etiological/preventive implications
Early and late IVH may have both common and different antecedents.[15,17,18,25,27,40,41] A growing body of literature has shown that certain perinatal antecedents are related to IVH occurring within the first HOL but not to IVH occurring later on.[15,18,22,28,42,43,44] Several reports suggest that early IVH is associated with a longer duration of the active phase and total labor compared with late IVH.[5,12,14,26] A study by Meidell et al. found that a total labor duration of more than 12 h is inevitably associated with IVH identified at a mean of 2 HOL.[14] Other researchers have shown that grade 1 IVH identified within the first 12 HOL is associated with active labor.[26] Similarly, another group of researchers found that the occurrence of IVH during the first 1 HOL was increased in neonates of women who went through the active phase of labor.[5,12] Unexpectedly, these same investigators did not observe this association in a secondary report that included neonates delivered by caesarian section only; however, they did observe that the active phase of labor is associated with the progression of the hemorrhage.[13] Based on a multivariable analysis this group of researchers proposed that cesarian section or forceps delivery may attenuate the effect of active-phase labor.[5]
Similarly, four additional reports suggested that cesarean section is protective against IVH identified in the first 1-11 HOL.[12,15,17,20] Using a multivariable analysis, three of these reports concluded that cesarean section was independently associated with a lower risk of such IVH.[15,17,20] One of these reports included two different cohorts of Australian preterm neonates and found no association between the mode of delivery and IVH occurring after 5 HOL in either cohort.[15] Two small studies found no association between the mode of delivery and IVH occurring in the first HOL.[14,41] Together, these observations support the notion that the protective effect of a cesarean section may be strongest for IVH occurring within the first HOL rather than later on.[45]
Medicolegal implications
The IVH occurring within the first 12 HOL is more strongly associated with perinatal hypoxic-ischemic events than the later onset IVH.[1,25,26,41] Perhaps documentation of the IVH status within the first HOL is a surrogate for perinatal hypoxic-ischemic events in preterm labors as these events are difficult to diagnosis based on intrapartum fetal monitoring, cord pH, Apgar score, or clinical findings.[46,47,48,49]
PROPOSED DEFINITION OF EARLY ONSET IVH
There has been inconsistency in defining the term “early IVH” in the literature [Tables 1 and 2]. The term “early IVH” has been used to refer to IVH occurring as early as the first HOL and as late as the first 10 DOL.[4,50,51,52] We propose that early IVH is an IVH that occurs within the first 6 HOL for three reasons. First, this period is the earliest mode of the bimodal distribution of IVH timing. Second, it is the shortest, most vulnerable period of time for IVH because it includes about 50% of the IVH cases [Figures 1–3]. Third, it is less vulnerable to postnatal intervention bias.[53,54]
GUIDELINES FOR CLINICAL PRACTICE
A high percentage of IVH is clinically silent.[1,3,23] Thus, there is universal consensus that all preterm neonates born at <30 weeks gestation or a birth weight of <1500 g should have a routine screening HUS. However, the timing of the first routine screening HUS varies widely ranging from the first 6-12 HOL[36,55,56] to the 2nd week of life.[50,57,58,59,60,61,62,63,64] Given the important prognostic and medicolegal aspect of early IVH and the fact that about 50% of IVH cases occur within the first 6 HOL, we recommend that the first routine screening HUS to be performed at about 6 HOL. A portable user-friendly ultrasound machine that can be operated by physicians is affordable and has been proven to be reliable.[6,65] Japanese researchers were able to perform continuous HUS monitoring 25 years ago.[2,66] Continuous HUS monitoring can be accomplished by using a hands-free ultrasound system, including ultrasound probe holders.
IMPLICATIONS FOR RESEARCH
According to Hill, when trying to determine the cause and effect, temporality plays a key role.[67,68,69] Thus, temporal intervals used in a study are critical; “the shorter the temporal and spatial interval, the less room for confounders to interfere”.[69] Therefore, linking perinatal antecedents such as the mode of delivery to the cases of IVH that occurred after the first 6 HOL is not sensible because multiple confounders may have interfered. Similarly, logic dictates that temporality cannot be assumed for the postnatal antecedents in studies where the first HUSs were performed after the first 6 HOL because about 50% of IVH cases occur within the first 6 HOL [Figures 1–3]. Therefore, future research using a continuous HUS monitoring or shorter temporal interval is required to explore the antecedents of IVH. Analyzing early IVH separately from late IVH will reduce the observed inconsistency and more effectively delineate additional antecedents of IVH.[15,45] Future research is required to elucidate whether the long-term neurological outcomes of early and late IVH are the same. A large-scale study is required to elucidate whether the severity of early and late IVH are the same. A more precise assessment of the severity can be accomplished by using an IVH severity score.[70]
SUMMARY
The 0-6 and after 24 HOL were the major modes of IVH timing. The first 6 HOL is the shortest, most vulnerable period of time for a neonate with respect to IVH. We propose that early IVH is an IVH that occurs within the first 6 HOL. Documentation of the early IVH status has important prognostic and medicolegal implications. Thus, we recommend that the first routine screening HUS to be performed at about 6 HOL for all preterm neonates at risk of IVH. Future research exploring the antecedents of IVH should guaranty the temporality between these antecedents and IVH. Additional research will be required to determine whether the long-term neurological outcomes of early and late IVH are the same.
APPENDIX: EXCLUDED STUDIES
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Volpe JJ. Germinal matrix-intraventricular hemorrhage. In: Volpe JJ, editor. Neurology of the Newborn. 5th ed. Philadelphia, PA: Saunders Elsevier; 2008. pp. 517–88. [Google Scholar]
- 2.Funato M, Tamai H, Noma K, Kurita T, Kajimoto Y, Yoshioka Y, et al. Clinical events in association with timing of intraventricular hemorrhage in preterm infants. J Pediatr. 1992;121:614–9. doi: 10.1016/s0022-3476(05)81157-6. [DOI] [PubMed] [Google Scholar]
- 3.Dolfin T, Skidmore MB, Fong KW, Hoskins EM, Shennan AT. Incidence, severity, and timing of subependymal and intraventricular hemorrhages in preterm infants born in a perinatal unit as detected by serial real-time ultrasound. Pediatrics. 1983;71:541–6. [PubMed] [Google Scholar]
- 4.Bejar R, Curbelo V, Coen RW, Leopold G, James H, Gluck L. Diagnosis and follow-up of intraventricular and intracerebral hemorrhages by ultrasound studies of infant's brain through the fontanelles and sutures. Pediatrics. 1980;66:661–73. [PubMed] [Google Scholar]
- 5.Shaver DC, Bada HS, Korones SB, Anderson GD, Wong SP, Arheart KL. Early and late intraventricular hemorrhage: The role of obstetric factors. Obstet Gynecol. 1992;80:831–7. [PubMed] [Google Scholar]
- 6.Sarkar S, Kaplan C, Wiswell TE, Spitzer AR. Histological chorioamnionitis and the risk of early intraventricular hemorrhage in infants born < or = 28 weeks gestation. J Perinatol. 2005;25:749–52. doi: 10.1038/sj.jp.7211399. [DOI] [PubMed] [Google Scholar]
- 7.Paneth N, Pinto-Martin J, Gardiner J, Wallenstein S, Katsikiotis V, Hegyi T, et al. Incidence and timing of germinal matrix/intraventricular hemorrhage in low birth weight infants. Am J Epidemiol. 1993;137:1167–76. doi: 10.1093/oxfordjournals.aje.a116619. [DOI] [PubMed] [Google Scholar]
- 8.Bada HS, Green RS, Pourcyrous M, Leffler CW, Korones SB, Magill HL, et al. Indomethacin reduces the risks of severe intraventricular hemorrhage. J Pediatr. 1989;115:631–7. doi: 10.1016/s0022-3476(89)80300-2. [DOI] [PubMed] [Google Scholar]
- 9.Emerson P, Fujimura M, Howat P, Howes D, Keeling J, Robinson RO, et al. Timing of intraventricular haemorrhage. Arch Dis Child. 1977;52:183–7. doi: 10.1136/adc.52.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van de Bor M, Janssen JW, Van Bel F, Ruys JH. Serum creatine kinase BB as predictor of periventricular haemorrhage in preterm infants. Early Hum Dev. 1988;17:165–74. doi: 10.1016/0378-3782(88)90005-9. [DOI] [PubMed] [Google Scholar]
- 11.de Crespigny LC, Mackay R, Murton LJ, Roy RN, Robinson PH. Timing of neonatal cerebroventricular haemorrhage with ultrasound. Arch Dis Child. 1982;57:231–3. doi: 10.1136/adc.57.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson GD, Bada HS, Sibai BM, Harvey C, Korones SB, Magill HL, et al. The relationship between labor and route of delivery in the preterm infant. Am J Obstet Gynecol. 1988;158:1382–90. doi: 10.1016/0002-9378(88)90371-7. [DOI] [PubMed] [Google Scholar]
- 13.Anderson GD, Bada HS, Shaver DC, Harvey CJ, Korones SB, Wong SP, et al. The effect of cesarean section on intraventricular hemorrhage in the preterm infant. Am J Obstet Gynecol. 1992;166:1091–9. doi: 10.1016/s0002-9378(11)90594-8. [DOI] [PubMed] [Google Scholar]
- 14.Meidell R, Marinelli P, Pettett G. Perinatal factors associated with early-onset intracranial hemorrhage in premature infants. A prospective study. Am J Dis Child. 1985;139:160–3. doi: 10.1001/archpedi.1985.02140040058028. [DOI] [PubMed] [Google Scholar]
- 15.Osborn DA, Evans N, Kluckow M. Hemodynamic and antecedent risk factors of early and late periventricular/intraventricular hemorrhage in premature infants. Pediatrics. 2003;112:33–9. doi: 10.1542/peds.112.1.33. [DOI] [PubMed] [Google Scholar]
- 16.McDonald MM, Koops BL, Johnson ML, Guggenheim MA, Rumack CM, Mitchell SA, et al. Timing and antecedents of intracranial hemorrhage in the newborn. Pediatrics. 1984;74:32–6. [PubMed] [Google Scholar]
- 17.Kluckow M, Evans N. Low superior vena cava flow and intraventricular haemorrhage in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2000;82:F188–94. doi: 10.1136/fn.82.3.F188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ment LR, Duncan CC, Ehrenkranz RA, Lange RC, Taylor KJ, Kleinman CS, et al. Intraventricular hemorrhage in the preterm neonate: Timing and cerebral blood flow changes. J Pediatr. 1984;104:419–25. doi: 10.1016/s0022-3476(84)81109-9. [DOI] [PubMed] [Google Scholar]
- 19.Weindling AM, Wilkinson AR, Cook J, Calvert SA, Fok TF, Rochefort MJ. Perinatal events which precede periventricular haemorrhage and leukomalacia in the newborn. Br J Obstet Gynaecol. 1985;92:1218–23. doi: 10.1111/j.1471-0528.1985.tb04865.x. [DOI] [PubMed] [Google Scholar]
- 20.Ment LR, Oh W, Ehrenkranz RA, Philip AG, Duncan CC, Makuch RW. Antenatal steroids, delivery mode, and intraventricular hemorrhage in preterm infants. Am J Obstet Gynecol. 1995;172:795–800. doi: 10.1016/0002-9378(95)90001-2. [DOI] [PubMed] [Google Scholar]
- 21.Dani C, Bertini G, Pezzati M, Poggi C, Guerrini P, Martano C, et al. Prophylactic ibuprofen for the prevention of intraventricular hemorrhage among preterm infants: A multicenter, randomized study. Pediatrics. 2005;115:1529–35. doi: 10.1542/peds.2004-1178. [DOI] [PubMed] [Google Scholar]
- 22.Beverley DW, Chance GW, Coates CF. Intraventricular haemorrhage - Timing of occurrence and relationship to perinatal events. Br J Obstet Gynaecol. 1984;91:1007–13. doi: 10.1111/j.1471-0528.1984.tb03679.x. [DOI] [PubMed] [Google Scholar]
- 23.Gupta AK, Anand NK, Lamba IM. Ultrasonic evaluation of neonatal subependymal-intraventricular hemorrhage and its complications. Indian J Pediatr. 1993;60:11–8. doi: 10.1007/BF02860497. [DOI] [PubMed] [Google Scholar]
- 24.Szymonowicz W, Yu VY. Timing and evolution of periventricular haemorrhage in infants weighing 1250 g or less at birth. Arch Dis Child. 1984;59:7–12. doi: 10.1136/adc.59.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leviton A, Pagano M, Kuban KC. Etiologic heterogeneity of intracranial hemorrhages in preterm newborns. Pediatr Neurol. 1988;4:274–8. doi: 10.1016/0887-8994(88)90065-3. [DOI] [PubMed] [Google Scholar]
- 26.Pagano M, Leviton A, Kuban K. Early and late germinal matrix hemorrhage may have different antecedents. Eur J Obstet Gynecol Reprod Biol. 1990;37:47–54. doi: 10.1016/0028-2243(90)90094-h. [DOI] [PubMed] [Google Scholar]
- 27.Wells JT, Ment LR. Prevention of intraventricular hemorrhage in preterm infants. Early Hum Dev. 1995;42:209–33. doi: 10.1016/0378-3782(95)01651-i. [DOI] [PubMed] [Google Scholar]
- 28.Van de Bor M, Van Bel F, Lineman R, Ruys JH. Perinatal factors and periventricular-intraventricular hemorrhage in preterm infants. Am J Dis Child. 1986;140:1125–30. doi: 10.1001/archpedi.1986.02140250051035. [DOI] [PubMed] [Google Scholar]
- 29.Rumack CM, Manco-Johnson ML, Manco-Johnson MJ, Koops BL, Hathaway WE, Appareti K. Timing and course of neonatal intracranial hemorrhage using real-time ultrasound. Radiology. 1985;154:101–5. doi: 10.1148/radiology.154.1.3880600. [DOI] [PubMed] [Google Scholar]
- 30.Ment LR. Intraventricular hemorrhage of the preterm infant. In: McMillan JA, McMillan JA, Feigin RD, DeAngelis C, Jones MD, editors. Oski's Pediatrics: Principles and Practice. Philadelphia PA USA: Lippincott Williams and Wilkins A Wolters Kluwer Business; 2006. pp. 271–8. [Google Scholar]
- 31.Ment LR, Oh W, Ehrenkranz RA, Philip AG, Vohr B, Allan W, et al. Low-dose indomethacin and prevention of intraventricular hemorrhage: A multicenter randomized trial. Pediatrics. 1994;93:543–50. [PubMed] [Google Scholar]
- 32.Perlman JM, Volpe JJ. Intraventricular hemorrhage in extremely small premature infants. Am J Dis Child. 1986;140:1122–4. doi: 10.1001/archpedi.1986.02140250048034. [DOI] [PubMed] [Google Scholar]
- 33.Morgan ME, Cooke RW. Timing of neonatal cerebroventricular haemorrhage with ultrasound. Arch Dis Child. 1982;57:811. doi: 10.1136/adc.57.10.811-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wallace BC, Schmid CH, Lau J, Trikalinos TA. Meta-analyst: Software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol. 2009;9:80. doi: 10.1186/1471-2288-9-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, West Sussex, England: John Wiley and Sons Ltd; 2008. [Google Scholar]
- 36.Dyet LE, Rennie JM. Preterm cerebral haemorrhage. In: Rennie JM, editor. Rennie and Roberton's Textbook of Neonatology. 5th ed. China: Churchill Livingstone/Elsevier; 2012. pp. 1156–81. [Google Scholar]
- 37.Ment LR, Oh W, Philip AG, Ehrenkranz RA, Duncan CC, Allan W, et al. Risk factors for early intraventricular hemorrhage in low birth weight infants. J Pediatr. 1992;121:776–83. doi: 10.1016/s0022-3476(05)81915-8. [DOI] [PubMed] [Google Scholar]
- 38.Levene MI, de Vries L. Extension of neonatal intraventricular haemorrhage. Arch Dis Child. 1984;59:631–6. doi: 10.1136/adc.59.7.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vohr B, Allan WC, Scott DT, Katz KH, Schneider KC, Makuch RW, et al. Early-onset intraventricular hemorrhage in preterm neonates: Incidence of neurodevelopmental handicap. Semin Perinatol. 1999;23:212–7. doi: 10.1016/s0146-0005(99)80065-2. [DOI] [PubMed] [Google Scholar]
- 40.Miletin J, Dempsey EM. Low superior vena cava flow on day 1 and adverse outcome in the very low birthweight infant. Arch Dis Child Fetal Neonatal Ed. 2008;93:F368–71. doi: 10.1136/adc.2007.129304. [DOI] [PubMed] [Google Scholar]
- 41.Leviton A, Pagano M, Kuban KC, Krishnamoorthy KS, Sullivan KF, Allred EN. The epidemiology of germinal matrix hemorrhage during the first half-day of life. Dev Med Child Neurol. 1991;33:138–45. doi: 10.1111/j.1469-8749.1991.tb05092.x. [DOI] [PubMed] [Google Scholar]
- 42.Babnik J, Stucin-Gantar I, Kornhauser-Cerar L, Sinkovec J, Wraber B, Derganc M. Intrauterine inflammation and the onset of peri-intraventricular hemorrhage in premature infants. Biol Neonate. 2006;90:113–21. doi: 10.1159/000092070. [DOI] [PubMed] [Google Scholar]
- 43.Szymonowicz W, Yu VY, Wilson FE. Antecedents of periventricular haemorrhage in infants weighing 1250 g or less at birth. Arch Dis Child. 1984;59:13–7. doi: 10.1136/adc.59.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bada HS, Korones SB, Anderson GD, Magill HL, Wong SP. Obstetric factors and relative risk of neonatal germinal layer/intraventricular hemorrhage. Am J Obstet Gynecol. 1984;148:798–804. doi: 10.1016/0002-9378(84)90571-4. [DOI] [PubMed] [Google Scholar]
- 45.Heuchan AM, Evans N, Henderson Smart DJ, Simpson JM. Perinatal risk factors for major intraventricular haemorrhage in the Australian and New Zealand Neonatal Network, 1995-97. Arch Dis Child Fetal Neonatal Ed. 2002;86:F86–90. doi: 10.1136/fn.86.2.F86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Afors K, Chandraharan E. Use of continuous electronic fetal monitoring in a preterm fetus: Clinical dilemmas and recommendations for practice. J Pregnancy. 2011;2011:848794. doi: 10.1155/2011/848794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chan SS, To WW. Correlation between intrapartum cardiotocogram findings and cord blood pH in term and preterm labours. Hong Kong J Gynaecol Obstet Midwifery. 2009;9:36–42. [Google Scholar]
- 48.MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: International consensus statement. BMJ. 1999;319:1054–9. doi: 10.1136/bmj.319.7216.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Corcoran JD, Hamilton A, Halliday HL. Antenatal intraventricular haemorrhage. Ir Med J. 1994;87:185–6. [PubMed] [Google Scholar]
- 50.Vela-Huerta MM, Amador-Licona M, Medina-Ovando N, Aldana-Valenzuela C. Factors associated with early severe intraventricular haemorrhage in very low birth weight infants. Neuropediatrics. 2009;40:224–7. doi: 10.1055/s-0030-1248249. [DOI] [PubMed] [Google Scholar]
- 51.Horsch S, Kutz P, Roll C. Late germinal matrix hemorrhage-like lesions in very preterm infants. J Child Neurol. 2010;25:809–14. doi: 10.1177/0883073809346849. [DOI] [PubMed] [Google Scholar]
- 52.Kallankari H, Kaukola T, Ojaniemi M, Herva R, Perhomaa M, Vuolteenaho R, et al. Chemokine CCL18 predicts intraventricular hemorrhage in very preterm infants. Ann Med. 2010;42:416–25. doi: 10.3109/07853890.2010.481085. [DOI] [PubMed] [Google Scholar]
- 53.Dorling JS, Field DJ, Manktelow B. Neonatal disease severity scoring systems. Arch Dis Child Fetal Neonatal Ed. 2005;90:F11–6. doi: 10.1136/adc.2003.048488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Richardson DK, Corcoran JD, Escobar GJ, Lee SK. SNAP-II and SNAPPE-II: Simplified newborn illness severity and mortality risk scores. J Pediatr. 2001;138:92–100. doi: 10.1067/mpd.2001.109608. [DOI] [PubMed] [Google Scholar]
- 55.Dani C, Poggi C, Bertini G, Pratesi S, Di Tommaso M, Scarselli G, et al. Method of delivery and intraventricular haemorrhage in extremely preterm infants. J Matern Fetal Neonatal Med. 2010;23:1419–23. doi: 10.3109/14767051003678218. [DOI] [PubMed] [Google Scholar]
- 56.Brouwer A, Groenendaal F, van Haastert IL, Rademaker K, Hanlo P, de Vries L. Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J Pediatr. 2008;152:648–54. doi: 10.1016/j.jpeds.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 57.North Trent Neonatal Network: Cranial Ultrasound Guideline: North Trent Neonatal Network. 2009. [Last accessed on 2013 Feb 24]. Available from: http://www.northtrentneonatal.nhs.uk/uploaded_files/-1Cranial_Ultrasound_Policy_-Revised_October_2009.pdf .
- 58.NHS Forth Valley: Cranial Ultrasound Scan Guideline. 2011. [Last accessed on 2013 Feb 24]. Available from: http://www.nhsforthvalley.com/__documents/qi/CE_Guideline_WCDNeonatal/CranialUSS.pdf .
- 59.von Lindern JS, Hulzebos CV, Bos AF, Brand A, Walther FJ, Lopriore E. Thrombocytopaenia and intraventricular haemorrhage in very premature infants: A tale of two cities. Arch Dis Child Fetal Neonatal Ed. 2012;97:F348–52. doi: 10.1136/fetalneonatal-2011-300763. [DOI] [PubMed] [Google Scholar]
- 60.Obladen M, Metze B, Henrich W, Aktas A, Czernik C, Schulz-Baldes A. Interdisciplinary surveillance of intraventricular haemorrhage associated conditions in infants < 1000 g. Acta Paediatr. 2008;97:731–7. doi: 10.1111/j.1651-2227.2008.00812.x. [DOI] [PubMed] [Google Scholar]
- 61.Lee JY, Kim HS, Jung E, Kim ES, Shim GH, Lee HJ, et al. Risk factors for periventricular-intraventricular hemorrhage in premature infants. J Korean Med Sci. 2010;25:418–24. doi: 10.3346/jkms.2010.25.3.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lim WH, Lien R, Chiang MC, Fu RH, Lin JJ, Chu SM, et al. Hypernatremia and grade III/IV intraventricular hemorrhage among extremely low birth weight infants. J Perinatol. 2011;31:193–8. doi: 10.1038/jp.2010.86. [DOI] [PubMed] [Google Scholar]
- 63.Audeh S, Smolkin T, Bental Y, Haramati Z, Blazer S, Litig E, et al. Does admission hypothermia predispose to intraventricular hemorrhage in very-low-birth-weight infants? Neonatology. 2011;100:373–9. doi: 10.1159/000327370. [DOI] [PubMed] [Google Scholar]
- 64.Ment LR, Bada HS, Barnes P, Grant PE, Hirtz D, Papile LA, et al. Practice parameter: Neuroimaging of the neonate: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2002;58:1726–38. doi: 10.1212/wnl.58.12.1726. [DOI] [PubMed] [Google Scholar]
- 65.Burdjalov V, Srinivasan P, Baumgart S, Spitzer AR. Handheld, portable ultrasound in the neonatal intensive care nursery: A new, inexpensive tool for the rapid diagnosis of common neonatal problems. J Perinatol. 2002;22:478–83. doi: 10.1038/sj.jp.7210782. [DOI] [PubMed] [Google Scholar]
- 66.Funato M, Tamai H, Kodaka R, Taki H, Yoshioka Y, Shimada S. The moment of intraventricular hemorrhage. Brain Dev. 1988;10:325–7. doi: 10.1016/s0387-7604(88)80064-0. [DOI] [PubMed] [Google Scholar]
- 67.Hill AB. The environment and disease: Association or causation? Proc R Soc Med. 1965;58:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Goodman KJ, Phillips CV. Encyclopedia of Statistics in Behavioral Science. London, UK: John Wiley and Sons, Ltd; 2005. Hill's Criteria of Causation. [Google Scholar]
- 69.Howick J, Glasziou P, Aronson JK. The evolution of evidence hierarchies: What can Bradford Hill's ‘guidelines for causation’ contribute? J R Soc Med. 2009;102:186–94. doi: 10.1258/jrsm.2009.090020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Al-Abdi SY. A severity score for intraventricular hemorrhage in preterm neonates. Saudi Med J. 2011;32:1313–4. [PubMed] [Google Scholar]
REFERENCES: EXCLUDED STUDIES
- 1.Gupta AK, Anand NK, Lamba IM. Ultrasonic evaluation of neonatal subependymal-intraventricular hemorrhage and its complications. Indian J Pediatr. 1993;60:11–8. doi: 10.1007/BF02860497. [DOI] [PubMed] [Google Scholar]
- 2.Morgan ME, Cooke RW. Timing of neonatal cerebroventricular haemorrhage with ultrasound. Arch Dis Child. 1982;57:811. doi: 10.1136/adc.57.10.811-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Szymonowicz W, Yu VY. Timing and evolution of periventricular haemorrhage in infants weighing 1250 g or less at birth. Arch Dis Child. 1984;59:7–12. doi: 10.1136/adc.59.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuban KC, Leviton A, Krishnamoorthy KS, Brown ER, Teele RL, Baglivo JA, et al. Neonatal intracranial hemorrhage and phenobarbital. Pediatrics. 1986;77:443–50. [PubMed] [Google Scholar]
- 5.Pagano M, Leviton A, Kuban K. Early and late germinal matrix hemorrhage may have different antecedents. Eur J Obstet Gynecol Reprod Biol. 1990;37:47–54. doi: 10.1016/0028-2243(90)90094-h. [DOI] [PubMed] [Google Scholar]
- 6.Leviton A, Pagano M, Kuban KC, Krishnamoorthy KS, Sullivan KF, Allred EN. The epidemiology of germinal matrix hemorrhage during the first half-day of life. Dev Med Child Neurol. 1991;33:138–45. doi: 10.1111/j.1469-8749.1991.tb05092.x. [DOI] [PubMed] [Google Scholar]
- 7.Perlman JM, Volpe JJ. Intraventricular hemorrhage in extremely small premature infants. Am J Dis Child. 1986;140:1122–4. doi: 10.1001/archpedi.1986.02140250048034. [DOI] [PubMed] [Google Scholar]
- 8.Levene MI, Wigglesworth JS, Dubowitz V. Cerebral structure and intraventricular haemorrhage in the neonate: A real time ultrasound study. Am J Dis Child. 1981;56:416–24. doi: 10.1136/adc.56.6.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levene MI, Fawer CL, Lamont RF. Risk factors in the development of intraventricular haemorrhage in the preterm neonate. Am J Dis Child. 1982;57:410–7. doi: 10.1136/adc.57.6.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thorburn RJ, Lipscomb AP, Stewart AL, Reynolds EO, Hope PL. Timing and antecedents of periventricular haemorrhage and of cerebral atrophy in very preterm infants. Early Hum Dev. 1982;7:221–38. doi: 10.1016/0378-3782(82)90085-8. [DOI] [PubMed] [Google Scholar]
- 11.Partridge JC, Babcock DS, Steichen JJ, Han BK. Optimal timing for diagnostic cranial ultrasound in low birth weight infants: Detection of intracranial hemorrhage and ventricular dilation. J Pediatr. 1982;102:281–7. doi: 10.1016/s0022-3476(83)80544-7. [DOI] [PubMed] [Google Scholar]
- 12.Perlman JM, Volpe JJ. Cerebral blood flow velocity in relation to intraventricular hemorrhage in the premature newborn infant. J Pediatr. 1982;100:956–9. doi: 10.1016/s0022-3476(82)80527-1. [DOI] [PubMed] [Google Scholar]
- 13.Bada HS, Korones SB, Anderson GD, Magill HL, Wong SP. Obstetric factors and relative risk of neonatal germinal layer/intraventricular hemorrhage. Am J Obstet Gynecol. 1984;148:798–804. doi: 10.1016/0002-9378(84)90571-4. [DOI] [PubMed] [Google Scholar]
- 14.Amato M, Hüppi P, Gambon R, Schneider H. Biochemical timing of peri intraventricular hemorrhage assessed by perinatal CPK BB isoenzyme measurements. J Perinat Med. 1989;17:447–52. doi: 10.1515/jpme.1989.17.6.447. [DOI] [PubMed] [Google Scholar]
- 15.Babnik J, Stucin Gantar I, Kornhauser Cerar L, Sinkovec J, Wraber B, Derganc M. Intrauterine inflammation and the onset of peri intraventricular hemorrhage in premature infants. Biol Neonate. 2006;90:113–21. doi: 10.1159/000092070. [DOI] [PubMed] [Google Scholar]
- 16.Meek JH, Tyszczuk L, Elwell CE, Wyatt JS. Low cerebral blood flow is a risk factor for severe intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed. 1999;81:F15–8. doi: 10.1136/fn.81.1.f15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kadri H, Mawla AA, Kazah J. The incidence, timing, and predisposing factors of germinal matrix and intraventricular hemorrhage (GMH/IVH) in preterm neonates. Childs Nerv Syst. 2006;22:1086–90. doi: 10.1007/s00381-006-0050-6. [DOI] [PubMed] [Google Scholar]
- 18.Rashid J, Shahid M, Anwar S, Sharaf D, Bhatti MT. Frequency of intraventricular haemorrhage in preterm neonates. Pak J Med Health Sci. 2010;4:515–9. [Google Scholar]