Abstract
Cytokines have been found to be elevated in cancer patients and have been associated with worse prognosis in single tumour entities. We investigated the association of eight different cytokines with venous thromboembolism (VTE) and prognosis in cancer patients. The Vienna Cancer and Thrombosis Study (CATS), a prospective study, includes patients with newly diagnosed tumour or disease progression. Patients with an overt infection are excluded. Study end-points are VTE, death, loss to follow-up or study completion. Interleukin (IL) serum levels were measured using the xMAP technology developed by Luminex. Among 726 included patients, no associations between IL levels and VTE were found, with the exception of a trend for IL-1β and IL-6 in pancreatic cancer. Elevated levels of IL-6 [as continuous variable per double increase hazard ratio (HR) = 1·07, 95% confidence interval (CI) = 1·027–1·114, P = 0·001, IL-8 (HR = 1·12, 95% CI = 1·062–1·170, P < 0·001) and IL-11 (HR = 1·37, 95% CI = 1·103–1·709, P = 0·005] were associated with worse survival. In subgroup analyses based on tumour type, colon carcinoma patients, who had higher IL-6 levels, showed a shorter survival (HR = 2·405, 95% CI = 1·252–4·618, P = 0·008). A significant association of elevated IL-10 levels with a decrease in survival (HR = 1·824, 95% CI = 1·098–3·031, P = 0·020) was seen among patients with lung cancer. No correlation between VTE and IL levels was found, but higher IL-6, IL-8 and IL-11 levels were associated with worse survival in cancer patients. Further, elevated IL-6 levels might be a prognostic marker in colorectal cancer and elevated IL-10 levels in lung cancer patients.
Keywords: cancer, interleukin levels, survival, thrombosis
Introduction
Cancer is associated with the occurrence of venous thromboembolism (VTE) 1, which affects up to 20% of all cancer patients 2–4. However, the rate may even be underestimated because of asymptomatic VTE. The incidence of VTE differs widely between the various tumour types 1,5,6, with the highest risk of VTE observed in patients suffering from pancreatic, stomach, lung or colorectal cancer, as well as in patients with brain tumours 6–9. The occurrence of VTE negatively affects the prognosis of cancer patients and is among the most important causes of death in these patients 10–12. Many risk factors related to patient characteristics, tumour types and treatment influence the development of VTE in cancer patients 6. A number of biomarkers of haemostasis and inflammatory markers have been found to play the role of risk factors of VTE in patients with cancer 13–16.
There is evidence that elevated levels of interleukins (ILs) could be associated with VTE 17–19. Various ILs are elevated in cancer patients, dependent upon type and stage of the tumours 20,21. In particular, IL-6 and IL-8 play an important role in the process of inflammation and, therefore, also in the development and progression of cancer. IL-6 induces both T-lymphocyte proliferation and angiogenesis, which then influence growth, differentiation and migration of tumour cells. IL-8 is involved in stimulating neutrophils and angiogenesis 22. IL-10, which acts as an immunoinhibitory cytokine, is often elevated in patients with lung cancer, whereas in patients with colorectal cancer the levels of IL-6 are increased 19,21,23–25. Elevated levels of circulating IL-6 and IL-8 are often associated with poor survival rates, especially in patients suffering from lung cancer 24,26–30. The macrophage inflammatory protein-1α [CCL-3 (chemokine ligand 3)] is involved in acute inflammation via recruiting and activating leucocytes 31.
In the present study, we evaluated the associations between different ILs and the occurrence of VTE as well as overall survival in patients with cancer.
Materials and methods
Patients
This study included patients with cancer who were recruited into the Vienna Cancer and Thrombosis Study (CATS), an ongoing prospective and observational cohort study initiated in October 2003. The details of the study have been described previously 15,19. The study was approved by the ethics committee of the Medical University of Vienna. Each patient gave his/her written informed consent. CATS enrolled patients with cancer of the breast, lung, upper or lower gastrointestinal tract, pancreas, kidney, prostate or other sites and patients with haematological malignancies. Patients were divided into newly diagnosed cancer patients versus those with disease progression after complete or partial remission, and were observed for a period of up to 2 years. Patients with an overt bacterial or viral infection within the last 2 weeks or who had undergone surgery or radiotherapy within the last 2 weeks, as well as patients who had had chemotherapy or a venous or arterial thromboembolism within the last 3 months, were excluded from study entry. Patients treated with vitamin K antagonists or low-molecular-weight heparin (LMWH) for long-term anti-coagulation were also excluded. However, thromboprophylaxis while being hospitalized was not an exclusion criterion. At the time of inclusion, data on medical history, type and stage of tumour were collected. During the observation period, patients were contacted by postal mail or telephone approximately every 3 months in order to collect data on the clinical course of their disease, in particular concerning the occurrence of VTE and anti-cancer treatment.
Study end-points were the occurrence of VTE (which had to be confirmed objectively by means of duplex sonography, phlebography, computerized tomography or ventilation–perfusion lung scan), death due to any cause, loss to follow-up or completion of the 2-year study period.
Laboratory analysis
Venous blood samples were drawn by atraumatic and sterile vein puncture into vacuum tubes with serum clot activator (Vacuette, Greiner-Bio One, Kremsmuenster, Austria) on the day of study entry. All blood samples were collected at the same time of day, in the morning (9 a.m.–12 p.m.). The serum blood was then centrifuged at 3600 g for 10 min using the Rotanta/TRC centrifuge (Hettich, Tuttlingen, Germany).
Serum aliquots were stored at −80°C until measurements were conducted in series. The samples of each individual patient were coded prior to laboratory analysis.
Assessment of cytokine serum levels was performed using the xMAP technology developed by Luminex (Riverside, CA, USA). This is a bead-based system for multiplex testing of cytokines, chemokines and growth factors. Specific anti-cytokine antibodies as well as recombinant cytokines were obtained from R&D Systems (Minneapolis, MN, USA). Measurements were performed using a Luminex analyser.
Statistical analysis
Continuous variables are described by the mean ± standard deviation or the median and the 25th–75th percentiles in case of non-normally distributed continuous data. Categorical variables are described by absolute numbers and percentages. The median follow-up time was calculated using the reverse Kaplan–Meier method. Survival probabilities were estimated by the Kaplan–Meier method. Spearman's correlation coefficient was used to describe the degree of correlation between the investigated IL serum levels.
Univariate and multivariable Cox regression analyses were used to evaluate the effect of the IL serum levels on the development of VTE and on survival. With respect to the outcome of VTE, the observation end-point was fatal or non-fatal VTE. Data were censored at death, end of observation period after 2 years or loss to follow-up. Considering the end-point death, data were censored at the end of the observational period after 2 years or loss to follow-up. Due to the large number of patients with IL serum levels equal to zero, each of the investigated IL parameters was represented by two prognostic factors within the Cox regression models: first, a binary variable discriminating between patients with IL serum levels equal to zero or greater than zero, and secondly a continuous variable comprising the log2-transformed IL serum level of patients with IL serum levels greater than zero. The log2-transformation was used to normalize the skewed distribution of IL serum levels greater than zero. The value of the continuous variable was set to zero in the case of patients with zero IL serum levels.
Two-sided P-values smaller than 0·05 were considered to indicate statistical significance. All analyses were performed with sas version 9·3.
Results
Study population
Overall, 726 cancer patients with a median age of 62·0 years were included between October 2003 and March 2009. Patient characteristics are listed in Table 1.
Table 1.
Patient characteristics (n = 726)
| Age at study entry, median (min.; max.), years | 62·0 (18; 88) |
| BMI, mean ± s.d., kg/m2 | 25·3 ± 4·5 |
| Gender | n (%) |
| Male | 382 (52·6) |
| Female | 344 (47·4) |
| Type of cancer | n (%) |
| Brain | 77 (10·6) |
| Breast | 129 (17·8) |
| Colon | 98 (13·5) |
| Kidney | 22 (3·0) |
| Lung | 109 (15·0) |
| Lymphoma | 70 (9·6) |
| Multiple myeloma | 15 (2·1) |
| Pancreas | 47 (6·5) |
| Prostate | 75 (10·3) |
| Stomach | 37 (5·1) |
| Others | 47 (6·5) |
| Treatment before study inclusion (ie. CHT, RT or surgery) | 311 (42·8) |
BMI = body mass index; CHT = chemotherapy; RT = radiotherapy; s.d. = standard deviation.
The tumour types consist of malignancies of the breast (n = 129), brain (n = 77), lung (n = 109), stomach (n = 37), colon (n = 98), pancreas (n = 47), kidney (n = 22), prostate (n = 75), multiple myeloma (n = 15) and lymphoma (n = 70). Other tumour entities, such as malignancies of the gynaecological system, sarcoma, cholangiocellular carcinoma and urothelial carcinoma, are combined in the ‘others’ group (n = 47).
Among solid tumours, localized tumours were found in 263 patients, whereas distant metastasis was present in 301 patients. There were 539 newly diagnosed patients, and 187 patients had suffered from disease progression following a complete or partial remission. The median follow-up time of the patients was 705 days (25th–75th percentiles: 262–731 days).
Outcome VTE
During the study period, 52 patients (7·2%) developed a VTE. Of these patients, 25 (48·1%) had a deep vein thrombosis (DVT), 19 (36·5%) a pulmonary embolism (PE), one of which had a fatal PE, two a combined DVT and PE (3·8%) and six (11·5%) other kinds of VTE (portal vein thrombosis, sinus vein thrombosis, brachial vein thrombosis, inferior vena cava thrombosis, jugular vein thrombosis).
In the total study population, none of the investigated cytokine levels (i.e. IL-1β, IL-3, IL-4, IL-6, IL-8, IL-10, IL-11, CCL-3) showed an association with the occurrence of VTE (see Table 2).
Table 2.
Cytokine levels in univariate Cox regression analyses in the study population
| VTE | Survival | |||||||
|---|---|---|---|---|---|---|---|---|
| Parameter | HR | 95% CI | P-value | HR | 95% CI | P-value | ||
| Age* | 0·99 | 0·97 | 1·01 | 0·323 | 1·01 | 1·00 | 1·02 | 0·004 |
| Gender† | 0·86 | 0·50 | 1·49 | 0·587 | 0·78 | 0·63 | 0·97 | 0·027 |
| M-stage‡ | 2·50 | 1·22 | 5·09 | 0·012 | 5·09 | 3·81 | 6·80 | < 0·001 |
| IL-1β§ | 0·98 | 0·80 | 1·20 | 0·792 | 1·02 | 0·94 | 1·11 | 0·5885 |
| IL-3§ | 0·99 | 0·84 | 1·18 | 0·549 | 1·03 | 0·96 | 1·10 | 0·4495 |
| IL-4§ | 1·11 | 0·86 | 1·42 | 0·708 | 0·10 | 0·90 | 1·11 | 0·9765 |
| IL-6§ | 1·08 | 0·98 | 1·20 | 0·118 | 1·07 | 1·03 | 1·11 | < 0·0015 |
| IL-8§ | 1·06 | 0·94 | 1·20 | 0·210 | 1·12 | 1·06 | 1·17 | < 0·0015 |
| IL-10§ | 1·01 | 0·83 | 1·22 | 0·302 | 1·05 | 0·97 | 1·14 | 0·1585 |
| IL-11§ | 0·90 | 0·76 | 1·06 | 0·349 | 0·97 | 0·91 | 1·04 | 0·0115 |
| CCL-3§ | 0·99 | 0·90 | 1·10 | 0·726 | 0·98 | 0·94 | 1·02 | 0·6045 |
P-value for the combination of the binary and continuous variable.
Per year of life;
female versus male;
for solid tumours only;
hazard ratio (HR) per double increase of the continuous interleukin (IL) serum levels. CCL-3 = chemokine ligand 3; VTE = venous thromboembolism; CI = confidence interval.
Separate analyses were performed regarding the different tumour entities. In these analyses, only tumour entities with a VTE rate of more than 5% (i.e. cancer of the brain, colon, lung, pancreas and stomach) were considered. Evaluating the effects of the binary prognostic factors (levels below versus levels above detection limit) only in patients with pancreatic cancer, IL-1β [hazard ratio (HR) = 7·16, 95% confidence interval (CI) = 1·906–30·895, P = 0·004) and IL-6 (H = 13·23, 95% CI = 1·656–1711·29, P = 0·01] were associated with an increased risk for VTE.
Outcome survival
Overall, 337 patients (46·4%) died within the study period. In univariate analyses, no correlation was found between the levels of IL-1β, IL-3, IL-4, IL-10 and CCL-3 and survival (see Table 2).
Both a twofold increase of IL-6 levels (HR per double increase = 1·07, 95% CI = 1·027–1·114, P = 0·001) and IL-8 levels (HR per double increase: 1·12, 95% CI = 1·062–1·170, P < 0·001) were associated with poor survival. IL-11 levels above zero also correlated negatively with the patients' survival (HR per double increase = 1·37, 95% CI = 1·103–1·709, P = 0·005). However, among the group of patients with IL-11 levels above zero, the extent of the IL-11 level seemed to have no further influence on survival (HR per double increase = 0·97, 95% CI = 0·908–1·037, P = 0·376).
In multivariable analyses, after adjustment for age and gender, the association of the levels of IL-1β (HR per double increase = 0·93, 95% CI = 0·838–1·040, P = 0·020), IL-6 (HR per double increase = 1·15, 95% CI, 1·089–1·211, P < 0·001), IL-8 (HR per double increase = 1·12, 95% CI = 1·051 −1·182, P < 0·001) and IL-11 (HR per double increase = 0·94, 95% CI = 0·865–1·014, P = 0·012) with risk of mortality remained statistically significant. Patients with increased CCL-3 levels showed a better survival outcome (HR per double increase = 0·93, 95% CI = 0·89–0·977, P = 0·004). For detailed results see Table 3. Furthermore, we performed multivariable analyses with adjustment for age, gender and tumour stage (localized tumour versus distant metastasis) by including only the solid tumours. For these analyses, we excluded patients with brain tumours as well as patients with multiple myeloma and lymphoma. From the remaining patients (n = 564), 276 (48·9%) died within the follow-up period (55% male). In these patients, IL-6 (HR per double increase = 1·173, 95% CI = 1·100–1·251, P < 0·001) and IL-8 (HR per double increase = 1·092, 95% CI = 1·023–1·166, P = 0·008) were associated with an increased risk of mortality (see Table 4).
Table 3.
Interleukin (IL) levels and survival in the study population: multivariable Cox regression analyses, including cytokine levels, age and gender-adjusted
| Parameter | HR | 95% CI | P-value | |
|---|---|---|---|---|
| Age* | 1·01 | 0·997 | 1·015 | 0·210 |
| Gender† | 0·85 | 0·680 | 1·061 | 0·151 |
| IL-1β‡ | 0·93 | 0·838 | 1·040 | 0·0204 |
| IL-3‡ | 0·95 | 0·879 | 1·032 | 0·4704 |
| IL-4‡ | 0·95 | 0·825 | 1·089 | 0·6924 |
| IL-6‡ | 1·15 | 1·089 | 1·211 | < 0·0014 |
| IL-8‡ | 1·12 | 1·051 | 1·182 | < 0·0014 |
| IL-10‡ | 1·07 | 0·952 | 1·194 | 0·5214 |
| IL-11‡ | 0·94 | 0·865 | 1·014 | 0·0124 |
| CCL-3‡ | 0·93 | 0·890 | 0·977 | 0·0044 |
P-value for the combination of the binary and continuous variable.
Per year of life;
female versus male;
hazard ratio (HR) per double increase of the continuous IL serum levels. CI = confidence interval; CCL-3 = chemokine ligand 3.
Table 4.
Interleukin (IL) levels and survival in patients with solid tumours: multivariable Cox regression analyses, including cytokine levels, age, gender and tumour stage
| Parameter | HR | 95% CI | P-value | |
|---|---|---|---|---|
| Age* | 1·01 | 0·994 | 1·017 | 0·338 |
| Gender† | 0·89 | 0·692 | 1·141 | 0·353 |
| M-stage‡ | 4·63 | 3·435 | 6·237 | < 0·001 |
| IL-1β§ | 0·92 | 0·813 | 1·039 | 0·0245 |
| IL-3§ | 0·97 | 0·884 | 1·062 | 0·710 |
| IL-4§ | 0·96 | 0·818 | 1·129 | 0·1445 |
| IL-6§ | 1·17 | 1·101 | 1·251 | < 0·0015 |
| IL-8§ | 1·10 | 1·030 | 1·173 | 0·0145 |
| IL-10§ | 1·05 | 0·918 | 1·204 | 0·1285 |
| IL-11§ | 0·98 | 0·894 | 1·068 | 0·6325 |
| CCL-3§ | 0·96 | 0·911 | 1·010 | 0·0885 |
P-value for the combination of the binary and continuous variable.
Per year of life;
female versus male;
distant versus no distant metastasis;
hazard ratio (HR) per double increase of the continuous IL serum levels. CI = confidence interval; CCL-3 = chemokine ligand 3.
An additional consideration of the previous anti-tumour treatments within the multivariable models had no relevant impact on the results.
Additional multivariate analyses were conducted in the total study population after adjusting for age, body mass index (BMI) and tumour stage, which presented comparable results (data not shown).
There was a strong correlation between IL-4 and IL-1β (r = 0·650, P < 0·001) and between IL-1β and IL-6 (r = 0·537, P < 0·001), respectively.
In the subgroups, which were made depending on the tumour type, no significance was found between either IL levels and survival in breast cancer, or prostate cancer or brain tumours, whereas in patients with colon carcinoma higher IL-6 levels correlated significantly with decreased survival (HR per double increase = 2·27, 95% CI = 1·227–4·371, P = 0·009); see Table 5a. Patients with lung cancer showed a significant association of elevated IL-10 levels with a decrease in survival (HR per double increase = 1·82, 95% CI = 1·097–2·927, P = 0·021); see Table 5b.
Table 5.
Tumour types – subanalysis (multivariable Cox regression analyses)
| (a) Colorectal cancer | ||||
|---|---|---|---|---|
| Survival | ||||
| Parameter | HR | 95% CI | P-value | |
| Age* | 1·02 | 0·990 | 1·045 | 0·216 |
| Gender† | 1·22 | 0·635 | 2·267 | 0·547 |
| M-stage‡ | 6·00 | 2·613 | 16·783 | < 0·001 |
| IL-64 | 2·27 | 1·227 | 4·371 | 0·0095 |
| (b) Lung cancer | ||||
|---|---|---|---|---|
| Parameter | Survival | |||
| HR | 95% CI | P-value | ||
| Age* | 1·02 | 0·997 | 1·047 | 0·084 |
| Gender† | 0·66 | 0·425 | 1·009 | 0·055 |
| M-stage‡ | 2·53 | 1·416 | 4·911 | 0·001 |
| IL-10§ | 1·82 | 1·097 | 2·927 | 0·0215 |
P-value for the combination of binary and continuous variables.
Per year of life;
female versus male;
distant versus no distant metastasis;
hazard ratio (HR) per double increase of the continuous interleukin (IL) serum levels. CI = confidence interval.
The Kaplan–Meier curves (see Fig. 1) illustrate the survival rates in our cancer patients according to the IL-6, IL-8, IL-10 and IL-11 levels, discriminating between patients with IL serum levels equal to zero or greater than zero, respectively.
Fig. 1.
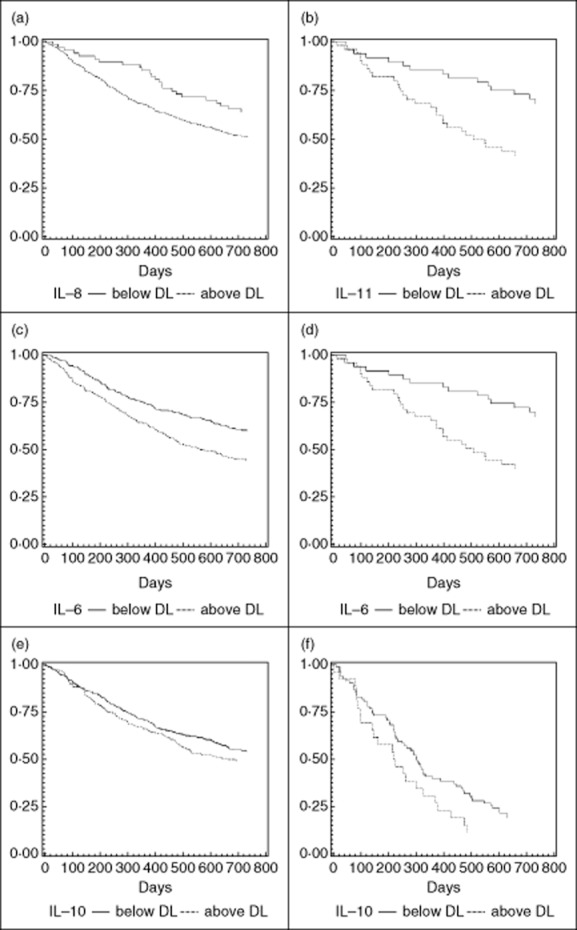
Kaplan–Meier curves discriminating between patients with interleukin (IL) serum levels equal to or greater than zero. (a) Probability of survival in patients with IL-8 levels below and above detection limit (DL) (log-rank: P = 0·030). (b) Probability of survival in patients with IL-11 levels below and above DL (log-rank: P = 0·004). (c) Probability of survival in patients with IL-6 levels below and above DL (log-rank: P < 0·001). (d) Probability of survival in colorectal cancer patients with IL-6 levels below and above DL (log-rank: P = 0·004). (e) Probability of survival in patients with IL-10 levels below and above DL (log-rank: P = 0·160). (f) Probability of survival in lung cancer patients with IL-10 levels below and above DL (log-rank: P = 0·130); x-axis: survival time in days; y-axis: survival distribution function.
Discussion
In the present prospective cohort study, we investigated the association between levels of IL/CCL-3 and the occurrence of VTE in cancer patients. While we did not observe a significant correlation between cytokine levels and the occurrence of VTE in the total study population, we found a correlation between levels of IL-1β and IL-6 and VTE in pancreatic cancer patients. However, these data are hampered by the very low patient number (only 47 pancreatic cancer patients). In order to evaluate this thoroughly, further studies with higher patient numbers would be of interest.
Regarding mortality, a correlation between IL-6, IL-8 and IL-11 and mortality was observed. We were able to define elevated levels of IL-6 and IL-10 as risk factors for increased mortality in patients with colorectal cancer and patients with lung cancer, respectively.
Associations of cytokine levels and VTE have not been studied previously in cancer patients, with the exception of IL-6. A recent study conducted by Malaponte et al. 32 found that IL-6 plasma levels were higher in cancer patients with a DVT compared to cancer patients without DVT as well as healthy individuals. Further, two case–control studies with discrepant results have been reported for non-cancer patients. In patients without cancer, Christiansen et al. 33 found no correlation between elevated levels of IL-6, IL-8, IL-10 and IL-1β and incidence of venous thromboembolic events. Van Aken et al. 34 reported that increased IL-8 levels (>90th percentile) were associated with a 1·9-fold increased risk for thrombosis. In patients with recurrent venous thrombosis, van Aken et al. also found an association between increased levels of IL-6 and IL-8 and the recurrence of venous thrombosis. Regarding the prognostic quality of the investigated cytokines, the underlying molecular mechanisms and the exact cellular sources of these immunomodulatory signal molecules are currently widely unknown and warrant further investigation. Enhanced levels of the multi-functional, proinflammatory cytokine IL-6 might be derived from either infiltrating immune cells, stromal cells or the cancer cell itself 35,36. The less-investigated IL-6 family member IL-11 can be produced by myeloid cells, but also by cancer-associated fibroblasts or cancer cells 37. IL-6 is known to directly promote tumour growth, but also facilitates immune invasion by several signalling pathways, in particular the signal transducer and transcription activator 3 36. Moreover, IL-6 might not only be induced by chemotherapy, but also mediate therapy resistance, which could add to the worse prognosis of patients with high circulating IL-6 levels 38. Interestingly, in a former study by our group, enhanced levels of C-reactive protein (CRP), an acute-phase protein known to be induced strongly by IL-6, indicated a worse prognosis of cancer patients not associated with VTE frequency 13. These observations suggest that a direct tumour-promoting effect might underlie the negative prognostic impact of IL-6. Accordingly, another proinflammatory cytokine connected to worse prognosis is the CXC chemokine IL-8, frequently produced by cancer cells. Interestingly, both IL-6 and IL-8 are stimulated by macrophage migration inhibitory factor 1 (MIF) expressed by multiple immune cells in the cancer tissues, sustaining macrophage survival 39. These observations support the hypothesis that the persistence of a proinflammatory tumour environment also drives disease progression within the investigated mixed patient cohort. However, in lung cancer, the usually immunosuppressive cytokines such as IL-10, acting primarily on macrophages and dentritic cells 40, also correlate with a worse prognosis. This indicates that the prognostic quality of these cytokines might generally reflect the consequences of the immunoediting process and the avoidance of immune destruction known as one of the hallmarks of cancer 41. As our CATS cohort includes patients with diverse cancer types, these data support the recently developed concept that such cytokine patterns are potentially a manifestation of an underlying systemic ‘paraneoplastic’ immune response that seems to be a consistent characteristic of patients suffering from diverse forms of cancer 42.
Previous studies have already shown that elevated levels of IL-6 correlated with lower survival rates 30,43 of cancer patients, including those of metastatic breast cancer 44, gastrointestinal cancer 28, metastatic renal cell carcinoma 29 prostate cancer 45 and lung cancer 46,47.
IL-8 levels were reported to be higher in patients with non-small-cell lung cancer than in healthy controls. Elevated levels correlated with shorter overall survival, but were not shown to be an independent prognostic factor 20.
In another study in previously untreated patients with non-small-cell lung cancer, IL-10 levels were elevated compared to healthy controls. IL-10 levels were decreased in patients who responded to chemotherapy, but were not affected in those with disease progression. Patients with IL-10 levels >19·6 pg/ml showed increased mortality compared to those with values ≤19·6 pg/ml 48. Thus, these findings are consistent with those of our study.
Moreover, Kaminska et al. showed that a rise of IL-6 and IL-10 concentrations in lung cancer patients was related significantly to the tumour size. In addition, patients with squamous cell carcinoma of the lung had higher circulating IL-6 levels compared to patients with adenocarcinomas. With regard to survival, Kaminska et al. did not find an association between the above-mentioned IL levels and survival 47.
It has already been reported by Baune et al. that an increase of IL-6 levels is related to higher mortality 49, which resembles our results.
A strength of our study is that we included a large number of patients with various tumour entities and investigated seven different ILs.
One limitation of our study is that we observed only 52 patients with VTE in our study population, despite the large number of patients with many different tumour entities enrolled into our study. IL levels were determined only at the time of inclusion prior to any anti-cancer therapy. However, a longitudinal determination of IL levels during the cytostatic treatment would be of further interest.
In conclusion, we did not find an association between different IL-levels and the occurrence of VTE, with the exception of a trend for IL-1β and IL-6 in pancreatic cancer patients. Our results indicate that IL-6, IL-8 and IL-11 are associated with increased mortality in cancer patients. IL-6 and IL-10 are associated with patients' prognosis in colorectal and lung cancer, respectively. In the future, more extensive studies are needed in order to evaluate the role of these ILs as relevant biomarkers in cancer patients regarding their survival.
Acknowledgments
We would like to thank University Professor Dr Walter Berger (Institute of Cancer Research) for his input regarding tumour immunology. The CATS project was supported by a grant from the Jubilaeumsfonds of the Austrian National Bank (project numbers 10935 and 12739).
Disclosures
All authors state that they have no conflicts of interest.
Author contributions
C. A., I. P., E.-M. R. carried out the study concept and design. C. A., A. K., I. P., E.-M. R. analysed and interpreted the data. C. A., I. P., E-M. R. drafted the manuscript. C. A., A. K., I. P., R. P., E.-M. R., C. Z., G. Z. critically revised the manuscript for important intellectual content. A. K. conducted the statistical analysis. I. P. was the study supervisor.
References
- 1.Cronin CG, Lohan DG, Keane M, Roche C, Murphy JM. Prevalence and significance of asymptomatic venous thromboembolic disease found on oncologic staging CT. Am J Roentgenol. 2007;189:162–170. doi: 10.2214/AJR.07.2067. [DOI] [PubMed] [Google Scholar]
- 2.Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost. 2007;5:632–634. doi: 10.1111/j.1538-7836.2007.02374.x. [DOI] [PubMed] [Google Scholar]
- 3.Lyman GH, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25:5490–5505. doi: 10.1200/JCO.2007.14.1283. [DOI] [PubMed] [Google Scholar]
- 4.Gao S, Escalante C. Venous thromboembolism and malignancy. Exp Rev Anticancer Ther. 2004;4:303–320. doi: 10.1586/14737140.4.2.303. [DOI] [PubMed] [Google Scholar]
- 5.Rollins KE, Peters CJ, Safranek PM, Ford H, Baglin TP, Hardwick RH. Venous thromboembolism in oesophago-gastric carcinoma: incidence of symptomatic and asymptomatic events following chemotherapy and surgery. Eur J Surg Oncol. 2011;37:1072–1077. doi: 10.1016/j.ejso.2011.08.140. [DOI] [PubMed] [Google Scholar]
- 6.Lyman GH. Venous thromboembolism in the patient with cancer: focus on burden of disease and benefits of thromboprophylaxis. Cancer. 2011;117:1334–1349. doi: 10.1002/cncr.25714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martin LK, Bekaii-Saab T. Management of venous thromboembolism in patients with advanced gastrointestinal cancers: what is the role of novel oral anticoagulants? Thrombosis. 2012;2012:758385. doi: 10.1155/2012/758385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah MA, Capanu M, Soff G, Asmis T, Kelsen DP. Risk factors for developing a new venous thromboembolism in ambulatory patients with non-hematologic malignancies and impact on survival for gastroesophageal malignancies. J Thromb Haemost. 2010;8:1702–1709. doi: 10.1111/j.1538-7836.2010.03948.x. [DOI] [PubMed] [Google Scholar]
- 9.Horsted F, West J, Grainge MJ. Risk of venous thromboembolism in patients with cancer: a systematic review and meta-analysis. PLOS Med. 2012;9:e1001275. doi: 10.1371/journal.pmed.1001275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heit JA, Silverstein MD, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ., III Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case–control study. Arch Intern Med. 2000;160:809–815. doi: 10.1001/archinte.160.6.809. [DOI] [PubMed] [Google Scholar]
- 11.Sousou T, Khorana A. Identifying cancer patients at risk for venous thromboembolism. Hamostaseologie. 2009;29:121–124. [PubMed] [Google Scholar]
- 12.Blom JW, Doggen CJ, Osanto S, Rosendaal FR. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293:715–722. doi: 10.1001/jama.293.6.715. [DOI] [PubMed] [Google Scholar]
- 13.Kanz R, Vukovich T, Vormittag R, et al. Thrombosis risk and survival in cancer patients with elevated C-reactive protein. J Thromb Haemost. 2011;9:57–63. doi: 10.1111/j.1538-7836.2010.04069.x. [DOI] [PubMed] [Google Scholar]
- 14.Vormittag R, Simanek R, Ay C, et al. High factor VIII levels independently predict venous thromboembolism in cancer patients: the cancer and thrombosis study. Arterioscler Thromb Vasc Biol. 2009;29:2176–2181. doi: 10.1161/ATVBAHA.109.190827. [DOI] [PubMed] [Google Scholar]
- 15.Ay C, Simanek R, Vormittag R, et al. High plasma levels of soluble P-selectin are predictive of venous thromboembolism in cancer patients: results from the Vienna Cancer and Thrombosis Study (CATS) Blood. 2008;112:2703–2708. doi: 10.1182/blood-2008-02-142422. [DOI] [PubMed] [Google Scholar]
- 16.Ay C, Pabinger I. Predictive potential of haemostatic biomarkers for venous thromboembolism in cancer patients. Thromb Res. 2012;129(Suppl. 1):S6–S9. doi: 10.1016/S0049-3848(12)70008-7. [DOI] [PubMed] [Google Scholar]
- 17.Noble S, Pasi J. Epidemiology and pathophysiology of cancer-associated thrombosis. Br J Cancer. 2010;102(Suppl. 1):S2–S9. doi: 10.1038/sj.bjc.6605599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller GJ, Bauer KA, Howarth DJ, Cooper JA, Humphries SE, Rosenberg RD. Increased incidence of neoplasia of the digestive tract in men with persistent activation of the coagulant pathway. J Thromb Haemost. 2004;2:2107–2114. doi: 10.1111/j.1538-7836.2004.01011.x. [DOI] [PubMed] [Google Scholar]
- 19.Vormittag R, Hsieh K, Kaider A, et al. Interleukin-6 and interleukin-6 promoter polymorphism (-174) G > C in patients with spontaneous venous thromboembolism. Thromb Haemost. 2006;95:802–806. [PubMed] [Google Scholar]
- 20.Guthrie GJ, Roxburgh CS, Horgan PG, McMillan DC. Does interleukin-6 link explain the link between tumour necrosis, local and systemic inflammatory responses and outcome in patients with colorectal cancer? Cancer Treat Rev. 2013;39:89–96. doi: 10.1016/j.ctrv.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Orditura M, De VF, Catalano G, et al. Elevated serum levels of interleukin-8 in advanced non-small cell lung cancer patients: relationship with prognosis. J Interferon Cytokine Res. 2002;22:1129–1135. doi: 10.1089/10799900260442557. [DOI] [PubMed] [Google Scholar]
- 22.Kaminska J, Kowalska MM, Nowacki MP, Chwalinski MG, Rysinska A, Fuksiewicz M. CRP, TNF-alpha, IL-1ra, IL-6, IL-8 and IL-10 in blood serum of colorectal cancer patients. Pathol Oncol Res. 2000;6:38–41. doi: 10.1007/BF03032656. [DOI] [PubMed] [Google Scholar]
- 23.Wang YC, Sung WW, Wu TC, et al. Interleukin-10 haplotype may predict survival and relapse in resected non-small cell lung cancer. PLOS ONE. 2012;7:e39525. doi: 10.1371/journal.pone.0039525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yanagawa H, Sone S, Takahashi Y, et al. Serum levels of interleukin 6 in patients with lung cancer. Br J Cancer. 1995;71:1095–1098. doi: 10.1038/bjc.1995.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heikkila K, Harris R, Lowe G, et al. Associations of circulating C-reactive protein and interleukin-6 with cancer risk: findings from two prospective cohorts and a meta-analysis. Cancer Causes Control. 2009;20:15–26. doi: 10.1007/s10552-008-9212-z. [DOI] [PubMed] [Google Scholar]
- 26.Songur N, Kuru B, Kalkan F, Ozdilekcan C, Cakmak H, Hizel N. Serum interleukin-6 levels correlate with malnutrition and survival in patients with advanced non-small cell lung cancer. Tumori. 2004;90:196–200. doi: 10.1177/030089160409000207. [DOI] [PubMed] [Google Scholar]
- 27.De VF, Orditura M, Auriemma A, Infusino S, Roscigno A, Catalano G. Serum levels of interleukin-6 as a prognostic factor in advanced non-small cell lung cancer. Oncol Rep. 1998;5:649–652. [PubMed] [Google Scholar]
- 28.De VF, Romano C, Orditura M, et al. Interleukin-6 serum level correlates with survival in advanced gastrointestinal cancer patients but is not an independent prognostic indicator. J Interferon Cytokine Res. 2001;21:45–52. doi: 10.1089/107999001459150. [DOI] [PubMed] [Google Scholar]
- 29.Ljungberg B, Grankvist K, Rasmuson T. Serum interleukin-6 in relation to acute-phase reactants and survival in patients with renal cell carcinoma. Eur J Cancer. 1997;33:1794–1798. doi: 10.1016/s0959-8049(97)00179-2. [DOI] [PubMed] [Google Scholar]
- 30.Chang CH, Hsiao CF, Yeh YM, et al. Circulating interleukin-6 level is a prognostic marker for survival in advanced non-small cell lung cancer patients treated with chemotherapy. Int J Cancer. 2013;132:1977–1985. doi: 10.1002/ijc.27892. [DOI] [PubMed] [Google Scholar]
- 31.Guan E, Wang J, Norcross MA. Identification of human macrophage inflammatory proteins 1alpha and 1beta as a native secreted heterodimer. J Biol Chem. 2001;276:12404–12409. doi: 10.1074/jbc.M006327200. [DOI] [PubMed] [Google Scholar]
- 32.Malaponte G, Polesel J, Candido S, et al. IL-6–174 G > C and MMP-9-1562 C > T polymorphisms are associated with increased risk of deep vein thrombosis in cancer patients. Cytokine. 2013;62:64–69. doi: 10.1016/j.cyto.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 33.Christiansen SC, Naess IA, Cannegieter SC, Hammerstrom J, Rosendaal FR, Reitsma PH. Inflammatory cytokines as risk factors for a first venous thrombosis: a prospective population-based study. PLOS Med. 2006;3:e334. doi: 10.1371/journal.pmed.0030334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Aken BE, Reitsma PH, Rosendaal FR. Interleukin 8 and venous thrombosis: evidence for a role of inflammation in thrombosis. Br J Haematol. 2002;116:173–177. doi: 10.1046/j.1365-2141.2002.03245.x. [DOI] [PubMed] [Google Scholar]
- 35.Schafer ZT, Brugge JS. IL-6 involvement in epithelial cancers. J Clin Invest. 2007;117:3660–3663. doi: 10.1172/JCI34237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guo Y, Xu F, Lu T, Duan Z, Zhang Z. Interleukin-6 signaling pathway in targeted therapy for cancer. Cancer Treat Rev. 2012;38:904–910. doi: 10.1016/j.ctrv.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 37.Putoczki T, Ernst M. More than a sidekick: the IL-6 family cytokine IL-11 links inflammation to cancer. J Leukoc Biol. 2010;88:1109–1117. doi: 10.1189/jlb.0410226. [DOI] [PubMed] [Google Scholar]
- 38.Chang CH, Hsiao CF, Yeh YM, et al. Circulating interleukin-6 level is a prognostic marker for survival in advanced nonsmall cell lung cancer patients treated with chemotherapy. Int J Cancer. 2013;132:1977–1985. doi: 10.1002/ijc.27892. [DOI] [PubMed] [Google Scholar]
- 39.Calandra T, Roger T. Macrophage migration inhibitory factor: a regulator of innate immunity. Nat Rev Immunol. 2003;3:791–800. doi: 10.1038/nri1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mosser DM, Zhang X. Interleukin-10: new perspectives on an old cytokine. Immunol Rev. 2008;226:205–218. doi: 10.1111/j.1600-065X.2008.00706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 42.Lippitz BE. Cytokine patterns in patients with cancer: a systematic review. Lancet Oncol. 2013;14:e218–e228. doi: 10.1016/S1470-2045(12)70582-X. [DOI] [PubMed] [Google Scholar]
- 43.Galizia G, Orditura M, Romano C, et al. Prognostic significance of circulating IL-10 and IL-6 serum levels in colon cancer patients undergoing surgery. Clin Immunol. 2002;102:169–178. doi: 10.1006/clim.2001.5163. [DOI] [PubMed] [Google Scholar]
- 44.Salgado R, Junius S, Benoy I, et al. Circulating interleukin-6 predicts survival in patients with metastatic breast cancer. Int J Cancer. 2003;103:642–646. doi: 10.1002/ijc.10833. [DOI] [PubMed] [Google Scholar]
- 45.Nakashima J, Tachibana M, Horiguchi Y, et al. Serum interleukin 6 as a prognostic factor in patients with prostate cancer. Clin Cancer Res. 2000;6:2702–2706. [PubMed] [Google Scholar]
- 46.Martin F, Santolaria F, Batista N, et al. Cytokine levels (IL-6 and IFN-gamma), acute phase response and nutritional status as prognostic factors in lung cancer. Cytokine. 1999;11:80–86. doi: 10.1006/cyto.1998.0398. [DOI] [PubMed] [Google Scholar]
- 47.Kaminska J, Kowalska M, Kotowicz B, et al. Pretreatment serum levels of cytokines and cytokine receptors in patients with non-small cell lung cancer, and correlations with clinicopathological features and prognosis. Oncology. 2006;70:115–125. doi: 10.1159/000093002. [DOI] [PubMed] [Google Scholar]
- 48.De VF, Orditura M, Galizia G, et al. Serum interleukin-10 levels as a prognostic factor in advanced non-small cell lung cancer patients. Chest. 2000;117:365–373. doi: 10.1378/chest.117.2.365. [DOI] [PubMed] [Google Scholar]
- 49.Baune BT, Rothermundt M, Ladwig KH, Meisinger C, Berger K. Systemic inflammation (interleukin 6) predicts all-cause mortality in men: results from a 9-year follow-up of the MEMO Study. Age (Dordr) 2011;33:209–217. doi: 10.1007/s11357-010-9165-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


