Abstract
Purpose
Exacerbation is a critical event in asthma management. We investigated whether exacerbation of symptoms is associated with farming exposures among agricultural pesticide applicators with asthma.
Methods
Participants were pesticide applicators with active asthma (wheezing and breathing problems in past 12 months) who completed enrollment questionnaires for the Agricultural Health Study (AHS). Exacerbation of asthma was defined as having visited a hospital emergency room or doctor for an episode of wheezing or whistling in the past 12 months. Exposures of interest were using 36 specific pesticides in the past 12 months and conducting various agricultural activities. Adjusted odds ratios (ORs) were estimated by logistic regression while controlling for potential confounders.
Results
The 926 AHS adult pesticide applicators with active asthma included 202 (22%) with exacerbation. Inverse associations with exacerbation were observed for two herbicides (glyphosate, odds ratio (OR) = 0.5, 95% confidence interval (CI) 0.3–0.8, and paraquat, OR=0.3, 95% CI 0.1–0.9) and several agricultural activities (repairing engines, grinding metal, driving diesel tractors, and performing veterinary procedures). Only asthma cases with allergies (i.e., doctor-diagnosed hay fever or eczema, 46%) had positive exacerbation-pesticide associations, with OR=2.1 (95% CI 1.1–4.1) for the herbicide pendimethalin and OR=10.2 (95% CI 1.9–55) for the insecticide aldicarb.
Conclusions
The inverse associations with two pesticides and specific farm activities are consistent with the possibility that asthma cases prone to exacerbation may avoid exposures that trigger symptoms. Although limited by small sample size and a cross-sectional design, our study suggests that use of specific pesticides may contribute to exacerbation of asthma among individuals with allergies.
Keywords: Asthma, Asthma exacerbation, Work-related, Agriculture, Pesticides
Introduction
Work-related asthma comprises occupational asthma (OA) that is caused by conditions at work and work-exacerbated asthma (WEA) in which existing asthma is made worse by conditions at work (Tarlo et al. 2008). Work-related asthma is common, with work accounting for an average of 17% of all new adult-onset asthma cases (Toren and Blanc 2009), and with WEA detected in an estimated 22% of working adults with asthma (Henneberger et al. 2011). Work-related asthma is also associated with substantial costs and lost work time (Vandenplas and Henneberger 2007; Vandenplas et al. 2003). While both OA and WEA contribute to adverse health and socioeconomic outcomes, WEA receives less research and prevention effort (Tarlo et al. 2008).
Recent reports based on surveys conducted in the United States and Sweden suggest that work-related asthma is a problem among agricultural workers (Mazurek and Schleiff 2010; Rask-Andersen 2010). In addition to exposures to plant and animal allergens, farmer and commercial pesticide applicators are exposed to chemicals that may cause or exacerbate asthma and related symptoms (Fieten et al. 2009; Hernandez et al. 2011; Senthilselvan et al. 1992). The Agricultural Health Study (AHS) in the United States was initiated in the early 1990s to investigate the health effects of pesticide and other farming exposures among private pesticide applicators (who are mainly farmers), commercial pesticide applicators, and the spouses of the private applicators (Alavanja et al. 1996). Wheeze was associated with several pesticides among both farmer pesticide applicators (Hoppin et al. 2002a) and commercial pesticide applicators (Hoppin et al. 2006). Also, prevalent adult-onset asthma was associated with 12 specific pesticides among farmer applicators with a history of allergies and with 4 pesticides among farmer applicators without allergies (Hoppin et al. 2009). Finally, farmer pesticide applicators with wheeze had a greater odds of engaging in certain agricultural activities, including driving diesel tractors, driving combines, welding, repairing engines, grinding metal, painting, and using gasoline and other solvents (Hoppin et al. 2004).
Agricultural exposures could possibly exacerbate the symptoms of pesticide applicators with asthma, although detecting such associations might be challenging. Some people with asthma may avoid work-related exposures that trigger their symptoms by never entering certain jobs, leaving jobs with harmful exposures, or modifying their work environment to minimize exposures and remain active in that profession. These choices can result in a “healthy worker effect” in which asthma cases in unexposed jobs are less “healthy” and cases in exposed jobs are relatively “healthy” (Olivieri et al. 2010). This phenomenon is an example of reverse causality in which disease status can influence exposure (Le Moual et al. 2008), and has been observed in farmers (Mounchetrou et al. 2012). Under these circumstances, estimates of the association between exposure and disease might be flat or even inverse. For example, the healthy worker effect could possibly have contributed to some findings in the previous AHS study of wheeze among farmer pesticide applicators, in which asthmatic subjects who used certain pesticides had statistically significant lower odds of wheeze (Hoppin et al. 2002a).
The prior investigation of asthma in AHS participants focused on prevalent adult-onset asthma (Hoppin et al. 2009) among farmer pesticide applicators, excluding asthma cases with onset in childhood. For this analysis we utilized data on all agricultural pesticide applicators with asthma, regardless of age at diagnosis, to study the relationship of exacerbation of symptoms with farming exposures.
METHODS
Selection of participants
Details about enrollment in the AHS are published elsewhere (Alavanja et al. 1996). AHS participants, adults enrolled at pesticide licensing facilities during 1993–1997, included 52,394 private pesticide applicators from Iowa and North Carolina and 4916 commercial applicators from Iowa. All participants completed an enrollment questionnaire and some completed a take-home questionnaire that was given to all of them. We limited the current analysis to those who completed both questionnaires because the take-home questionnaire provided necessary information about respiratory health. A total of 25,291 pesticide applicators (22,916 farmer and 2375 commercial applicators) returned both questionnaires (Hoppin et al. 2009; Hoppin et al. 2006), representing 44% of those who were enrolled. Among farmer applicators, non-responders were as likely to report a diagnosis of asthma and handling pesticides as responders, but were less likely to have used several herbicides (i.e., 2–4D, alachlor, atrazine, dicamba, glyphosate, and imazethapyr) (Tarone et al. 1997). Questionnaires are available at www.aghealth.org/questionnaires.html.
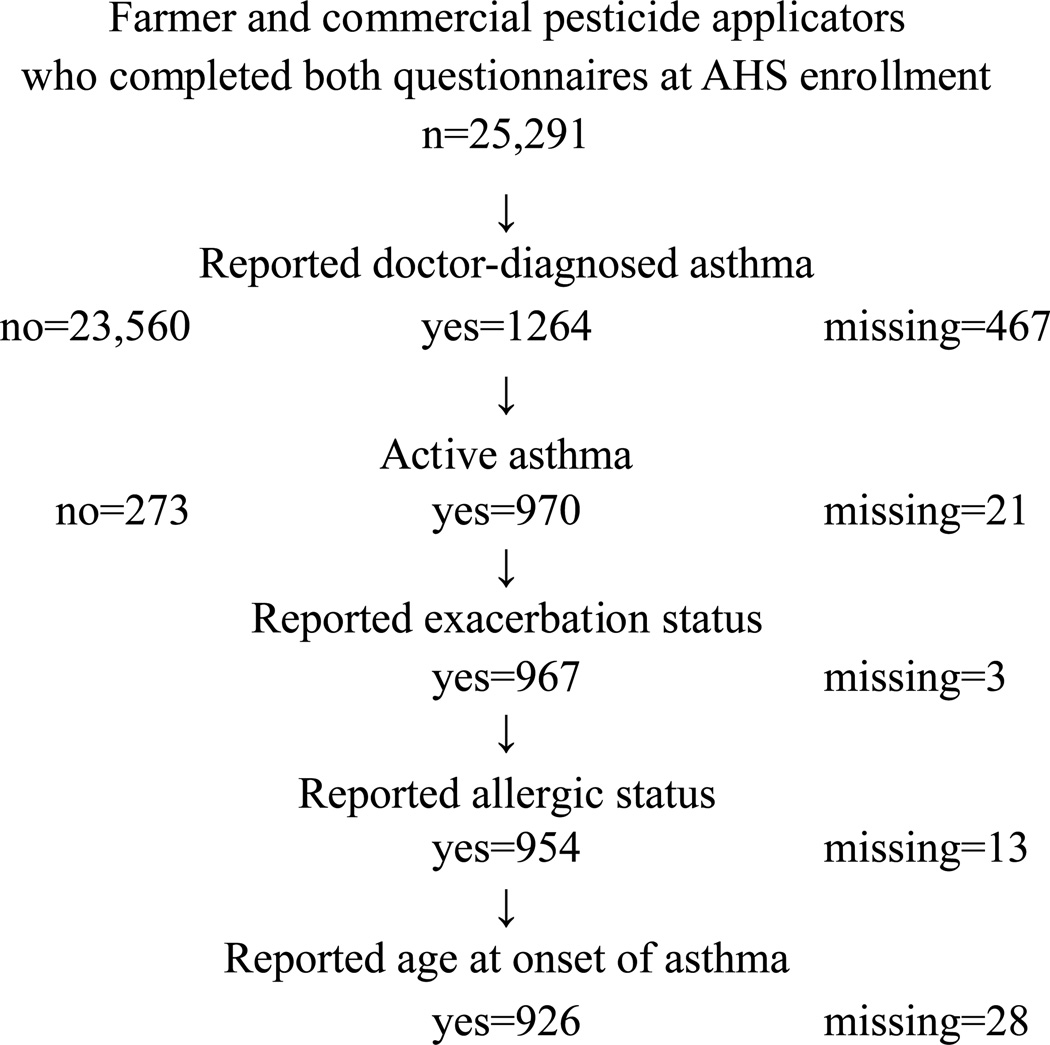
We applied several selection criteria, as illustrated in Figure 1. Of the five percent (i.e., 1264 of 25,291) who reported a doctor diagnosis of asthma, we selected only those with active asthma based on responses to two questions: having at least one episode of wheezing or whistling in the past 12 months and having breathing problems in the same time period. The remaining criteria were intended to ensure that participants had answered questions about asthma exacerbation, allergic status (i.e., history of doctor-diagnosed hay fever or eczema), and age at onset of asthma. The final study sample included 926 adult pesticide applicators with active asthma.
Fig. 1.
Selection of participants from the Agricultural Health Study (AHS) to investigate exacerbation among pesticide applicators with active asthma
Outcome of interest: Exacerbation of asthma
While all members of the study sample reported experiencing wheezing or whistling in the past year, only a subset fulfilled the criteria for exacerbation of asthma: a self-reported visit to a hospital emergency room or doctor for an episode of wheezing or whistling during the past 12 months. This definition is consistent with the criteria an expert panel recommended for use in observational studies of exacerbation (Fuhlbrigge et al. 2012).
Pesticide use and other agricultural activities
AHS participants were asked about their use of individual pesticides. We focused on the 36 pesticides used in the 12 months before enrollment (current exposure) by at least 10 applicators with at least two exacerbation cases. Our emphasis was the possible association of current exposure with exacerbation in the same time period (i.e., the past 12 months), but we wanted to ensure that former users (i.e., those who responded “yes” to ever use but “no” to current use), who might have persistent adverse effects of exposure, were excluded from the reference group. Consequently, we created a three level exposure variable (never, current, former) for each pesticide and assessed association by comparing current to never use while controlling for former exposure (Hoppin et al. 2002a; Hoppin et al. 2006; Slager et al. 2009). Participants who reported using a particular pesticide were also asked to indicate how many days they handled that pesticide in an average year when they had used it. Response categories for herbicides and insecticides were: <5, 5–9, 10–19, 20–39, 40–59, 60–150, and >150 days. Based on these responses and a report of current use, we created a three-level frequency-of-use variable: never, less frequent (1–9 days / year), and more frequent (≥10 days). Fungicides and fumigants are typically used fewer days per year than other pesticides, and we used a cutpoint of ≥5 days/year to define more frequent use and create a three-level frequency-of-use variable for these compounds. Participants were also asked to report use of personal protective equipment (PPE) while handling pesticides (14 covariates) and type of cab on the tractor used when applying pesticides (2 covariates).
Participants provided information about 20 other farming practices, including crop (n=6) and livestock (n=5) activities, farm maintenance tasks (n=6), and use of farm equipment (n=3). When a question asked participants to characterize their level of farm or farming work into one of several ordered categories, we typically recoded responses to “ever” versus “never.” We applied this recoding to the number of livestock and number of poultry last year, and to driving a combine, using natural and chemical fertilizers, and picking crops by hand last growing season. If a “never” category included very few participants, we chose a different cutpoint and dichotomized to “high” versus “low.” These variables were the number of acres planted last year (<200, ≥200), and the days tilled the soil (≤10, >10) and days planted (≤5, >5) last growing season. For activities with frequency categories of less than monthly to daily, we created variables where “low” was never or less than monthly, and “high” was at least every month.
Statistical analysis
For the crude analysis of categorical data, we used the continuity corrected chi square statistic or the Fisher’s exact test (if an expected cell count was less than 5) to test for statistical significance. For continuous data, we used the Student’s t-test.
We used logistic regression to model exacerbation and estimate odds ratios (ORs) for pesticide exposure and other farm activities while controlling for potential confounders. We fit a base regression model by determining which of the following variables were associated with exacerbation at p<0.15: age (continuous in years at enrollment), state (Iowa, North Carolina), type of pesticide applicator (private, commercial), cigarette smoking status (ever versus never), allergic status (no, yes) based on self-reports of doctor-diagnosed hay fever or eczema, adult onset of asthma (no, yes) based on onset at ≥20 years of age, and having spent at least half of their life on a farm before the age of 18 (no, yes). We explored both forward addition and backward elimination of the covariates to fit the base model. Each pesticide and agricultural activity was evaluated in a separate regression model by adding the appropriate variables to the base model. Because prior AHS studies of wheeze and prevalent adult-onset asthma suggested that applicators with a history of allergies might be susceptible to pesticides, we fit additional models with terms to represent the interaction of allergic status with current pesticide use and other agricultural activities.
Statistical tests were two-sided and considered significant if p≤0.05 and borderline significant if 0.05<p≤0.10. All analyses were completed using SAS® software version 9.2 (SAS Institute Inc., Cary, NC).
Human subjects approval
The protocol for AHS was approved by the institutional review boards of the National Institutes for Health and its contractors. Informed consent was implied when the participant returned a completed questionnaire.
Results
The 926 pesticide applicators with active asthma ranged in age from 16 to 83 years with a mean of 48.5 (SD=13.9) and a median of 48 years. Seventy-one percent (n=658) lived in Iowa and 90% (n=832) were private pesticide applicators. Approximately half had ever smoked, with 36% (n=325) former and 11% (n=102) current smokers. A history of allergies was common (n=423, 46%), and the sample was equally divided between asthma onset in adulthood (n=460, 50%) and in childhood (n=466, 50%). Nearly all participants (n=804, 87%) had grown up on farms, and most of the private applicators (n=622, 75%) had lived or worked more than 30 years on a farm. The distribution of the 926 participants by the number of pesticides they had mixed or applied in the past year was: 0 pesticides 23% (n=215); 1–2 pesticides 24% (n=225); 3–5 pesticides 25% (n=233); and 6 to 20 pesticides 27% (n=253). The sample was overwhelmingly male with only 4% (n=33) female, and 97% (n=894) of participants were white.
A total of 202 (22%) of the 926 pesticide applicators with active asthma fulfilled the criteria for exacerbation in the past 12 months. Exacerbation was positively associated with residence in North Carolina rather than Iowa, ever smoking, and onset of asthma in adulthood (Table 1). Those with exacerbation were somewhat older (p=0.15) and less likely to be in the highest quartile of the number of pesticides used in the past year. Participants with and without exacerbation varied little by type of pesticide applicator, allergic status, whether they had grown up on a farm, and duration of living or working on a farm.
Table 1.
Demographic and medical characteristics by exacerbation status for 926 pesticide applicators with active asthma
| With exacerbation |
Without exacerbation |
|||
|---|---|---|---|---|
| Characteristics | Categories | n=202 | n=724 | Pa |
| Age (years) | Mean (SEM) | 49.7 (1.0) | 48.1 (0.5) | 0.15 |
| Range, median | 16 – 79, 51 | 18 – 83, 47 | ||
| State | Iowa | 63% | 73% | 0.005 |
| North Carolina | 37% | 27% | ||
| Type of pesticide | Private | 93% | 89% | 0.19 |
| Applicator | Commercial | 7% | 11% | |
| Cigarette smoking | Never | 45% | 54% | 0.02 |
| Ever | 55% | 46% | ||
| Allergic statusb | Yes | 45% | 46% | 0.90 |
| Asthma onset ≥20 years age | Yes | 70% | 44% | <0.0001 |
| Spent 1/2 life on farm before age 18 | Yes | 88% | 87% | 0.99 |
| Years lived or worked on farmc | 1–30 years | 26% | 23% | 0.49 |
| > 30 years | 74% | 77% | ||
| No. of pesticides used last year | 0 | 27% | 22% | Reference |
| 1–2 | 26% | 24% | 0.70 | |
| 3–5 | 26% | 25% | 0.48 | |
| 6–20 | 21% | 29% | 0.02 |
SEM standard error of the mean
p value based on Student’s t-test for age and continuity corrected chi square for categorical variables
Allergic status defined as a self-report of doctor-diagnosed hay fever or eczema
Information asked only of private applicators, and findings exclude 94 commercial pesticide applicators and 13 private applicators with missing data
In fitting the base regression model, both forward addition and backward elimination of candidate covariates yielded the same model with the five covariates of age, state, ever smoked, allergic status, and adult onset of asthma. Allergic status had an inverse association with adult onset of asthma, which had a strong positive association with exacerbation (Table 1). A positive association between allergic status and exacerbation was not seen in the crude data analysis (Table 1), but appeared in the base regression model after controlling for the effect of adult onset of asthma.
The odds ratios for current use of specific pesticides were generally close to or less than one, with two that were statistically significant (i.e., p≤0.05) (Table 2). Asthma exacerbation was inversely associated with current use of the herbicides glyphosate (OR=0.5, 95% CI 0.3, 0.8) and paraquat (OR=0.3, 95% CI 0.1, 0.9). The herbicide butylate (OR=2.9, 95% CI 0.9, 9.4) and insecticide aldicarb (OR=2.3, 95% CI 0.9, 6.2) had positive associations with exacerbation that were of borderline significance (0.05<p≤0.10).
Table 2.
Frequency of current exposure to 36 pesticides by exacerbation status, and adjusted odds ratios among 926 pesticide applicators with active asthma
| With exacerbation |
Without exacerbation |
Adjusted odds ratio for current exposure (95% confidence interval)b |
|||
|---|---|---|---|---|---|
| Pesticides | Na | % currently exposed |
Na | % currently exposed |
|
| Herbicides | |||||
| 2 4-D | 97 | 56 | 380 | 65 | 0.8 (0.5, 1.3) |
| Alachlor W | 101 | 16 | 377 | 22 | 0.7 (0.4, 1.3) |
| Atrazine W | 115 | 39 | 403 | 54 | 0.7 (0.4, 1.0) |
| Butylate WA | 151 | 3 | 491 | 2 | 2.9 (0.9, 9.4) |
| Chlorimuron-ethyl W | 155 | 13 | 557 | 17 | 0.8 (0.5, 1.4) |
| Cyanazine | 124 | 14 | 423 | 18 | 0.8 (0.4, 1.4) |
| Dicamba | 125 | 31 | 438 | 37 | 1.0 (0.6, 1.6) |
| EPTC AA,W | 141 | 4 | 517 | 6 | 0.7 (0.3, 2.0) |
| Glyphosate WI | 117 | 57 | 441 | 68 | 0.5* (0.3, 0.8) |
| Imazethapyr | 150 | 27 | 570 | 35 | 0.8 (0.5, 1.3) |
| Metolachlor | 132 | 26 | 470 | 26 | 1.1 (0.7, 1.8) |
| Metribuzin | 143 | 6 | 453 | 10 | 0.7 (0.3, 1.5) |
| Paraquat AA,W,WI | 166 | 2 | 602 | 4 | 0.3* (0.1, 0.9) |
| Pendimethalin | 151 | 18 | 532 | 19 | 1.0 (0.6, 1.7) |
| Petroleum Oil AN,W | 167 | 10 | 566 | 14 | 0.7 (0.4, 1.3) |
| Trifluralin W | 123 | 24 | 437 | 30 | 0.9 (0.5, 1.4) |
| Insecticides | |||||
| Pyrethroids | |||||
| Permethrin (animals) W,WI | 172 | 3 | 599 | 4 | 0.8 (0.3, 2.0) |
| Permethrin (crops) | 166 | 6 | 580 | 7 | 0.7 (0.3, 1.5) |
| Organophosphates | |||||
| Chlorpyrifos W | 144 | 23 | 504 | 20 | 1.2 (0.7, 1.9) |
| Coumaphos AA,WI | 173 | 3 | 606 | 5 | 0.6 (0.2, 1.5) |
| Diazinon AA | 163 | 10 | 572 | 10 | 0.7 (0.4, 1.3) |
| Dichlorvos (DDVP) | 170 | 2 | 591 | 3 | 0.8 (0.3, 2.6) |
| Fonofos WA | 143 | 4 | 508 | 6 | 0.6 (0.2, 1.7) |
| Malathion AN,W | 87 | 33 | 359 | 37 | 0.8 (0.4, 1.3) |
| Phorate AN | 150 | 2 | 481 | 5 | 0.5 (0.1, 1.7) |
| Terbufos | 140 | 15 | 481 | 16 | 0.9 (0.5, 1.6) |
| Organochlorines | |||||
| Lindane AA | 175 | 1 | 606 | 1 | 0.7 (0.1, 3.5) |
| Carbamates | |||||
| Aldicarb | 192 | 4 | 669 | 2 | 2.3 (0.9, 6.2) |
| Carbaryl | 136 | 18 | 465 | 20 | 0.6 (0.4, 1.1) |
| Carbofuran | 137 | 3 | 478 | 3 | 0.9 (0.3, 2.9) |
| Fungicides | |||||
| Benomyl WI | 185 | 2 | 663 | 2 | 1.1 (0.3, 4.3) |
| Captan AA | 168 | 7 | 619 | 8 | 0.8 (0.4, 1.7) |
| Chlorothalonil | 188 | 4 | 662 | 3 | 1.3 (0.6, 3.2) |
| Maneb/Mancozeb | 184 | 2 | 659 | 3 | 0.4 (0.1, 1.3) |
| Metalaxyl W | 175 | 9 | 613 | 7 | 0.9 (0.4, 1.7) |
| Fumigants | |||||
| Methyl Bromide (Brom-O-Gas) | 170 | 3 | 638 | 4 | 0.6 (0.2, 1.9) |
The study population of 926 included 202 with and 724 without exacerbation. The entry for N represents the total of never and current users (without former users) and, consequently, is smaller than the corresponding total for the column.
A separate logistic regression model was fit to estimate the effect of each pesticide. The model included covariates to control for age (years), state, ever smoked, allergic status, and adult onset of asthma, as well as separate indicator variables for current and former exposure.
p<0.05
Footnotes for Column 1, Pesticides:
Pesticide previously reported as positively associated with prevalent adult-onset asthma in allergic participants (Hoppin et al. 2009)
Pesticide previously reported as positively associated with prevalent adult-onset asthma in non-allergic participants (Hoppin et al. 2009)
Pesticide previously reported as positively associated with wheeze (Hoppin et al. 2002)
Pesticide previously reported as positively associated with wheeze among those with allergic diseases (Hoppin et al. 2002)
Pesticide previously reported as inversely associated with wheeze among those with asthma (Hoppin et al. 2002)
We fit an additional regression model for each pesticide in Table 2 to explore possible interactions with allergic status. Three pesticides had statistically significant (i.e., p≤0.05) interactions between allergic status and current use (Table 3). Among the applicators with asthma who reported having allergies, the herbicide pendimethalin (OR=2.1, 95% CI 1.1, 4.1) and the carbamate insecticide aldicarb (OR=10.2, 95% CI 1.9, 55) were positively associated with exacerbation. The herbicide metribuzin also had a positive interaction with allergic status; it was inversely associated with exacerbation (OR=0.2, 95% CI 0.1, 0.9) among the non-allergic, but did not have an elevated OR among those with allergies.
Table 3.
Odds ratios (OR) and 95% confidence intervals (95% CI) for exacerbation of asthma among applicators with and without an allergy history, for pesticides with statistically significant interactions with allergic statusa
| Not Allergic |
Allergic |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| With exacerbation |
Without exacerbation |
With exacerbation |
Without exacerbation |
|||||||||
| Pesticides | Nb | % current exposure |
Nb | % current exposure |
OR (95% CI) |
Nb | % current exposure |
Nb | % current exposure |
OR (95% CI) |
P interaction |
|
| Herbicides | ||||||||||||
| Metribuzin | 75 | 3 | 253 | 12 | 0.2* (0.1, 0.9) | 68 | 10 | 200 | 7 | 1.9 (0.7, 5.1) | 0.02 | |
| Pendimethalin | 84 | 12 | 290 | 19 | 0.5 (0.2, 1.1) | 67 | 25 | 242 | 18 | 2.1* (1.1, 4.1) | 0.005 | |
| Insecticide, carbamate | ||||||||||||
| Aldicarb | 106 | 2 | 366 | 3 | 0.7 (0.1, 3.5) | 86 | 7 | 303 | 0.7 | 10.2* (1.9, 55) | 0.02 | |
The regression models included covariates for allergic status and interaction terms for current pesticide use and allergic status, as well as covariates to control for age (years), state, ever smoked, adult onset of asthma, and former exposure to the pesticide.
N is the total of never and current users, without former users
p≤0.05
When we compared less frequent and more frequent users of specific pesticides to never users, two herbicides had an inverse association with exacerbation after controlling for potential confounders. These results include statistically significant ORs for more frequent use of cyanazine (OR=0.3, 95% CI 0.1–0.8, p=0.02) and both less and more frequent use of glyphosate (OR=0.5, 95% CI 0.3–0.9, p=0.01, and OR=0.4, 95% CI 0.2–0.8, p=0.01, respectively).
Applicators with exacerbation tended to be underrepresented in certain crop production activities. Specifically, those with exacerbation were less likely to repair engines (OR=0.6, 95% CI 0.4–0.9), grind metal (OR=0.6, 95% CI 0.4–0.9), drive diesel tractors (OR=0.5, 95% CI 0.3–0.8), and perform veterinary procedures (OR=0.7, 95% CI 0.5–1.0) than those without exacerbation. An OR less than one was observed for painting (OR=0.7, 95% CI 0.5–1.1), but was of borderline statistical significance. The frequency of other activities (i.e., grinding feed, milking cows, using gasoline or solvents to clean hands or equipment, welding, and driving gasoline tractors) varied little by exacerbation status (data not shown). Similarly, several farm activities performed last year (i.e., planting 200 or more acres or raising livestock or poultry) or in the last growing season (i.e., more frequent tilling or planting, applying chemical or natural fertilizer, driving a combine, or picking crops by hand) were not associated with exacerbation (data not shown).
Exacerbation was not related to using a tractor with an enclosed cab or a cab with a charcoal filter when applying pesticides. Also, the use of PPE when handling pesticides did not differ substantially by exacerbation status among all applicators. However, two PPE variables had statistically significant interactions with allergic status. Among applicators with allergies, those with exacerbation were more likely to report using PPE when handling insecticides (OR=1.8, 95% CI 1.1, 3.0), while the findings for non-allergic applicators were inverse and not statistically significant (OR=0.8, 95% CI 0.5, 1.3). Use of goggles when handling pesticides also had a statistically significant positive interaction with allergic status, but neither of the allergy-specific ORs was significant (data not shown). The association of exacerbation with other agricultural activities did not vary by allergic status (i.e., p>0.05 for interaction).
Especially with an older study sample, it may be difficult to differentiate asthma from chronic obstructive pulmonary disease (COPD) based on questionnaires, and the two conditions may co-exist. Thus, our outcome that is based on symptoms (i.e., wheezing or whistling) may not be uniquely representing exacerbation of asthma. Self-reported doctor-diagnosed chronic bronchitis (n=209, 22.6%) and emphysema (n=70, 7.6%) were both positively associated with exacerbation (data not shown). However, when we added a covariate for the presence of either disease (n=243, 26.2%) to the regression models already described, the results for pesticides and agricultural activities were unchanged (data not shown).
Discussion
The current investigation of 926 well-characterized agricultural pesticide applicators with active asthma revealed both positive and inverse associations. First, asthma exacerbation was positively associated with use of two pesticides, but only among applicators with a history of allergies. Second, exacerbation was inversely associated with using other pesticides and engaging in selected agricultural activities. These seemingly contradictory results may be due to the cross-sectional nature of the analysis or the potential for those with problematic asthma to modify their exposures.
Exacerbation was inversely associated with the number of different pesticides used (Table 1). We also observed inverse associations between exacerbation and the pesticides glyphosate and paraquat among all 926 applicators with asthma (Table 2). An earlier analysis of AHS data reported similar findings, with wheeze inversely associated with these same pesticides among the farmer applicators who had asthma (Hoppin et al. 2002a). The authors commented that it was unclear whether people with asthma simply reacted less to these chemicals or that sensitive asthma cases avoided these exposures and “healthier” cases remained exposed and did not respond. Other herbicides were inversely associated with exacerbation for subsets of the current study sample: metribuzin for non-allergic applicators and cyanazine if used more frequently. These two were not previously identified as having a positive relationship with wheeze (Hoppin et al. 2002a) among all the farmer applicators.
Our results indicated that the herbicide pendimethalin and the carbamate insecticide aldicarb may contribute to exacerbation of asthma, but only among asthma cases with a history of allergic disease (Table 3). These relatively strong modifications of the pesticide-exacerbation association by allergic status parallel an observation in the AHS investigation of prevalent cases of adult-onset asthma among farmer pesticide applicators (i.e., a subset of the current cohort), in which positive asthma-pesticide associations were more common among those with allergic diseases (Hoppin et al. 2009). However, the two pesticides related to exacerbation were associated with neither asthma (Hoppin et al. 2009) nor wheeze (Hoppin et al. 2002a) among farmer pesticide applicators in the AHS. These pesticides differ in both their agricultural use and chemical class. The dinitroaniline herbicide pendimethalin is used on a variety of field crops to control annual grasses and broadleaf weeds (Extoxnet 1996). The carbamate insecticide aldicarb is commonly used on field crops to control insects and nematodes (Extoxnet. 1996). However, each pesticide has been associated with adverse respiratory responses, so could plausibly contribute to the exacerbation of asthma. Inhalation of pendimethalin can be mildly to moderately irritating to the upper airways and lungs (Extoxnet 1996; Reigart and Roberts 1999), and inhalation of aldicarb has been reported to aggravate chronic respiratory problems such as asthma (BayerCropScience 2002). Why these specific pesticides were associated with severe exacerbation of asthma rather than other pesticides that have also been reported to have respiratory effects remains unclear.
Several findings for agricultural activities suggest that asthmatic pesticide applicators with exacerbation avoided certain activities. For example, we saw statistically significant ORs less than one for repairing engines, grinding metal, driving diesel tractors, and performing veterinary procedures. In an earlier analysis of AHS data, the first three activities were positively associated with reports of wheeze among all farmer pesticide applicators (Hoppin et al. 2004). A possible interpretation of this contrast in findings is that asthmatic farmers with exacerbation avoided performing these tasks because they were perceived to trigger respiratory symptoms. Also, applicators with a history of allergies had an elevated OR for using PPE when handling insecticides, suggesting that this subset of participants with exacerbation might have been more attentive to limiting exposures to pesticides.
The healthy worker effect among agricultural and food production workers has been reported elsewhere. Agricultural work routinely involves exposure to a variety of chemicals and allergens that might exacerbate asthma. People with onset of asthma in childhood may avoid agricultural work entirely because of the perceived risk of symptom triggers. For example, a study in Sweden found that farm children with asthma were unlikely to later have jobs with a high probability of exposure to airway-irritating agents (Wiebert et al. 2008). A cohort of pig farmers in the Netherlands had a lower frequency of childhood asthma than non-farming neighborhood controls, a difference the researchers attributed to adults with a history of childhood asthma avoiding worksites perceived as troublesome (Vogelzang et al. 1999).
Individuals with asthma may leave a job in agriculture or food production once it is found to involve conditions that cause respiratory symptoms. Workers at a potato processing plant in the Netherlands were more likely to have asthma if they had worked for no more than 5 years (Zock et al. 1998). The investigators attributed this pattern to workers with asthma leaving these jobs after a few years. From a study conducted in France, having asthma was associated with early cessation of dairy farming, especially among women (Mounchetrou et al. 2012).
The current cross-sectional analysis of asthmatic mainly middle-aged farmers (mean age of 48.5 years) could have missed the most sensitive individuals in the population at large as they may have stopped farming earlier in life and thus never enrolled in the AHS. Typical of many agricultural workers, most AHS participants began this type of work in childhood. Future studies that followed farm children prospectively could possibly clarify the sequence of exposure and asthma outcomes, and document self-selection of those with asthma away from troublesome occupational exposures, including the departure from agricultural work entirely.
Although the AHS cohort is very large, the current investigation focused only on the 926 pesticide applicators with active asthma, which meant there was limited power to detect differences by pesticide use and other farm activities, particularly for less common exposures. Another limitation of the current investigation is its cross-sectional design, which restricted our ability to discern the temporal sequence of exposure and exacerbation of asthma. Both events occurred in the same 12 month period, but we cannot be certain that ORs less than 1.0 were due to asthma cases avoiding certain exposures or ORs greater than 1.0 were characterized by exposure preceding exacerbation. Because our cohort includes mostly middle-aged pesticide applicators, it is possible that farmers with asthma are underrepresented in our cohort and this self-selection could limit generalizability of some findings. Also, we tested numerous exposure covariates and it is possible that some findings were due to chance. With these limitations in mind, the current results must be interpreted with some caution, and further studies are needed to confirm them.
The metrics for exacerbation and pesticide exposure used in this study offer some advantages. Exacerbation of asthma as defined by a visit to a hospital emergency room or doctor for an episode of wheezing or whistling should be relatively easy to recall, especially because it is in the time frame of only the past 12 months. This definition of exacerbation is more specific and less sensitive than some other definitions, such as an episode of wheezing or whistling that required additional medication like oral steroids. Also, the characterization of pesticide exposure using self-reports is reliable and has been used successfully in several previous analyses of AHS data (Blair et al. 2002; Hoppin et al. 2002b).
This investigation differed in many ways from prior analyses of AHS data. The sample for the current investigation was limited to those with asthma, and the data analyses focused on potential risk factors for the unique outcome of exacerbation of asthma, rather than risk factors for asthma as explored in earlier analyses (Hoppin et al. 2009). Also, while the prior AHS study of prevalent asthma included only cases with onset in adulthood, the current study included both childhood and adult-onset asthma patients.
In conclusion, the findings from this study suggest that use of selected pesticides might be risk factors for exacerbation of symptoms among adult pesticide applicators with active allergic asthma. The fact that applicators with exacerbation of asthma were less likely to use certain pesticides and engage in selected farming activities might be evidence for a healthy worker effect. Future work should focus on prospective analyses, especially of children living on farms or young adult farmers, so that the correct temporal order of exposure and disease state can be assessed.
Acknowledgments
The authors thank the Agricultural Health Study participants, the staff of the Iowa and North Carolina field stations (Ellen Heywood, Margaret Hayslip) and the Agricultural Health Study coordinating center (Ben Laimon, Marsha Dunn, Kate Torres, Stanley Legum). This work was supported by the National Institute for Occupational Safety and Health and the Intramural Research Program of the National Institutes of Health, National Institute of Environmental Health Sciences (Z01-ES049030) and the National Institutes of Health, National Cancer Institute (Z01-CP010119).
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
Contributor Information
Paul K. Henneberger, Division of Respiratory Disease Studies, National Institute for Occupational Safety and Health, MS 2800, 1095 Willowdale Road, Morgantown, West Virginia 26505, United States, pkh0@cdc.gov, Telephone: +1 304 285 6161; Fax: +1 304 285 5820
Xiaoming Liang, Division of Respiratory Disease Studies, National Institute for Occupational Safety and Health, MS 2800, 1095 Willowdale Road, Morgantown, West Virginia 26505, United States.
Stephanie J. London, Epidemiology Branch, National Institute of Environmental Health Sciences (NIEHS), National Institutes of Health (NIH), Research Triangle Park, North Carolina, United States
David M. Umbach, Biostatistics Branch, NIEHS, NIH, Research Triangle Park, North Carolina, United States
Dale P. Sandler, Epidemiology Branch, National Institute of Environmental Health Sciences (NIEHS), National Institutes of Health (NIH), Research Triangle Park, North Carolina, United States
Jane A. Hoppin, Epidemiology Branch, National Institute of Environmental Health Sciences (NIEHS), National Institutes of Health (NIH), Research Triangle Park, North Carolina, United States
References
- Alavanja MCR, et al. The Agricultural Health Study. Environmental Health Perspectives. 1996;104(4):362–369. doi: 10.1289/ehp.96104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BayerCropScience. [Accessed October 11, 2012];MSDS 212: Temik Brand 15G Lock and Load Aldicarb Pesticide. 2002 http://www.cdms.net/ldat/mp840004.pdf.
- Blair A, et al. Reliability of reporting on life-style and agricultural factors by a sample of participants in the Agricultural Health Study from Iowa. Epidemiology. 2002;13(1):94–99. doi: 10.1097/00001648-200201000-00015. [DOI] [PubMed] [Google Scholar]
- Extoxnet. Pesticide Information Profiles. Extension Toxicology Network; 1996. [Accessed July 11, 2012]. Pendimethalin. http://extoxnet.orst.edu/pips/pendimet.htm. [Google Scholar]
- Extoxnet. Pesticide Information Profiles. Extension Toxicology Network; 1996. [Accessed July 11, 2012]. Aldicarb. http://extoxnet.orst.edu/pips/aldicarb.htm. [Google Scholar]
- Fieten KB, Kromhout H, Heederik D, de Joode BV. Pesticide Exposure and Respiratory Health of Indigenous Women in Costa Rica. American Journal of Epidemiology. 2009;169(12):1500–1506. doi: 10.1093/aje/kwp060. [DOI] [PubMed] [Google Scholar]
- Fuhlbrigge A, et al. Asthma outcomes: Exacerbations. Journal of Allergy and Clinical Immunology. 2012;129(3):S34–S48. doi: 10.1016/j.jaci.2011.12.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henneberger PK, et al. An official American Thoracic Society Statement: Work-exacerbated asthma. American Journal of Respiratory and Critical Care Medicine. 2011;184(3):368–378. doi: 10.1164/rccm.812011ST. [DOI] [PubMed] [Google Scholar]
- Hernandez AF, Parron T, Alarcon R. Pesticides and asthma. Current Opinion in Allergy and Clinical Immunology. 2011;11(2):90–96. doi: 10.1097/ACI.0b013e3283445939. [DOI] [PubMed] [Google Scholar]
- Hoppin JA, Umbach DM, London SJ, Alavanja MCR, Sandler DP. Chemical predictors of wheeze among farmer pesticide applicators in the Agricultural Health Study. American Journal of Respiratory and Critical Care Medicine. 2002a;165(5):683–689. doi: 10.1164/ajrccm.165.5.2106074. [DOI] [PubMed] [Google Scholar]
- Hoppin JA, Umbach DM, London SJ, Alavanja MCR, Sandler DP. Diesel exhaust, solvents, and other occupational exposures as risk factors for wheeze among farmers. American Journal of Respiratory and Critical Care Medicine. 2004;169(12):1308–1313. doi: 10.1164/rccm.200309-1228OC. [DOI] [PubMed] [Google Scholar]
- Hoppin JA, et al. Pesticide use and adult-onset asthma among male farmers in the Agricultural Health Study. European Respiratory Journal. 2009;34(6):1296–1303. doi: 10.1183/09031936.00005509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoppin JA, Umbach DM, London SJ, Lynch CF, Alavanja MCR, Sandler DP. Pesticides associated with wheeze among commercial pesticide applicators in the Agricultural Health Study. American Journal of Epidemiology. 2006;163(12):1129–1137. doi: 10.1093/aje/kwj138. [DOI] [PubMed] [Google Scholar]
- Hoppin JA, Yucel F, Dosemeci M, Sandler DP. Accuracy of self-reported pesticide use duration information from licensed pesticide applicators in the Agricultural Health Study. Journal of Exposure Analysis and Environmental Epidemiology. 2002b;12(5):313–318. doi: 10.1038/sj.jea.7500232. [DOI] [PubMed] [Google Scholar]
- Le Moual N, Kauffmann F, Eisen EA, Kennedy SM. The healthy worker effect in asthma - Work may cause asthma, but asthma may also influence work. American Journal of Respiratory and Critical Care Medicine. 2008;177(1):4–10. doi: 10.1164/rccm.200703-415PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurek JM, Schleiff PL. Physician recognition of work-related asthma among US farm operators. Family Medicine. 2010;42(6):408–413. [PubMed] [Google Scholar]
- Mounchetrou IN, Monnet E, Laplante J-J, Dalphin J-C, Thaon I. Predictors of early cessation of dairy farming in the French Doubs province: 12-year follow-up. American Journal of Industrial Medicine. 2012;55(2):136–142. doi: 10.1002/ajim.21031. [DOI] [PubMed] [Google Scholar]
- Olivieri M, et al. Healthy hire effect, job selection and inhalation exposure among young adults with asthma. European Respiratory Journal. 2010;36(3):517–523. doi: 10.1183/09031936.00125709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rask-Andersen A. Asthma increase among farmers: a 12-year follow-up. Upsala Journal of Medical Sciences. 2010:1–12. doi: 10.3109/03009734.2010.503287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reigart JR, Roberts JR. Recognition and management of pesticide poisonings. 5th edn. Washington, DC: U.S. EPA; 1999. [Google Scholar]
- Senthilselvan A, McDuffie HH, Dosman JA. Association of asthma with use of pesticides: Results of a cross-sectional survey of farmers. Am Rev Respir Dis. 1992;146:884–887. doi: 10.1164/ajrccm/146.4.884. [DOI] [PubMed] [Google Scholar]
- Slager RE, Poole JA, LeVan TD, Sandler DP, Alavanja MCR, Hoppin JA. Rhinitis associated with pesticide exposure among commercial pesticide applicators in the Agricultural Health Study. Occupational and Environmental Medicine. 2009;66(11):718–724. doi: 10.1136/oem.2008.041798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarlo SM, et al. Diagnosis and management of work-related asthma: American College Of Chest Physicians Consensus Statement. Chest. 2008;134(3 Suppl):1S–41S. doi: 10.1378/chest.08-0201. [DOI] [PubMed] [Google Scholar]
- Tarone RE, et al. The Agricultural Health Study: Factors affecting completion and return of self-administered questionnaires in a large prospective cohort study of pesticide applicators. American Journal of Industrial Medicine. 1997;31(2):233–242. doi: 10.1002/(sici)1097-0274(199702)31:2<233::aid-ajim13>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Toren K, Blanc PD. Asthma caused by occupational exposures is common - a systematic analysis of estimates of the population-attributable fraction. BMC Pulm Med. 2009;9:7. doi: 10.1186/1471-2466-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenplas O, Henneberger PK. Socioeconomic outcomes in work-exacerbated asthma. Current Opinion in Allergy and Clinical Immunology. 2007;7(3):236–241. doi: 10.1097/ACI.0b013e3280b10d68. [DOI] [PubMed] [Google Scholar]
- Vandenplas O, Toren K, Blanc PD. Health and socioeconomic impact of work-related asthma. European Respiratory Journal. 2003;22(4):689–697. doi: 10.1183/09031936.03.00053203. [DOI] [PubMed] [Google Scholar]
- Vogelzang PFJ, van der Gulden JWJ, Tielen MJM, Folgering H, van Schayck CP. Health-based selection for asthma, but not for chronic bronchitis, in pig farmers: an evidence-based hypothesis. European Respiratory Journal. 1999;13(1):187–189. doi: 10.1034/j.1399-3003.1999.13a34.x. [DOI] [PubMed] [Google Scholar]
- Wiebert P, Svartengren M, Lindberg M, Hemmingsson T, Lundberg I, Nise G. Mortality, morbidity and occupational exposure to airway-irritating agents among men with a respiratory diagnosis in adolescence. Occupational and Environmental Medicine. 2008;65(2):120–125. doi: 10.1136/oem.2006.032441. [DOI] [PubMed] [Google Scholar]
- Zock JP, Heederik D, Doekes G. Evaluation of chronic respiratory effects in the potato processing industry: indications of a healthy worker effect? Occupational and Environmental Medicine. 1998;55(12):823–827. doi: 10.1136/oem.55.12.823. [DOI] [PMC free article] [PubMed] [Google Scholar]