Abstract
Purpose.
To develop a safe, noninvasive, noncontact, continuous in vivo method to measure the dehydration rate of the precorneal tear film and to compare the effectiveness of a viscoelastic agent in maintaining the precorneal tear film to that of a balanced salt solution.
Methods.
Software was designed to analyze the corneal reflection produced by the operating microscope's coaxial illumination. The software characterized the shape of the reflection, which became distorted as the precorneal tear film evaporated; characterization was accomplished by fitting an ellipse to the reflection and measuring its projected surface area. Balanced salt solution Plus (BSS+) and a 2% hydroxypropylmethylcellulose viscoelastic were used as the test agents. The tear film evaporation rate was characterized and compared over a period of 20 minutes in 20 eyes from 10 New Zealand white rabbits.
Results.
The ellipse axes ratio and surface area were found to decrease initially after each application of either viscoelastic or BSS+ and then to increase linearly as the tear film began to evaporate (P < 0.001) for eyes treated with BSS+ only. Eyes treated with BSS+ required 7.5 ± 2.7 applications to maintain sufficient corneal hydration during the 20-minute test period, whereas eyes treated with viscoelastic required 1.4 ± 0.5 applications. The rates of evaporation differed significantly (P < 0.043) between viscoelastic and BSS+.
Conclusions.
The shape and surface area of the corneal reflection are strongly correlated with the state of the tear film. Rabbits' corneas treated with viscoelastic remained hydrated significantly longer than corneas treated with BSS+.
Keywords: balanced salt solution, corneal hydration, evaporation, precorneal tear film stability, viscoelastic
The shape and surface area of the corneal reflection are strongly correlated with the state of the tear film. Rabbits' corneas treated with viscoelastic remain hydrated significantly longer than corneas treated with BSS+.
Introduction
Wolff1,2 first described the composition of precorneal tear film as a three-layered structure: a thin superficial lipid layer, an underlying thicker aqueous layer, and an innermost mucin layer. In the current description of tear film, instead of a boundary between the aqueous and mucin layer, there is a mucin gel and a concentration gradient in depth, with high concentrations of mucin near the epithelial cell surface and high concentrations of aqueous near the lipid layer.3 Functions of the tear film include lubricating the ocular surface; providing a smooth, regular optical surface for the eye; supplying nutrients to the ocular surface; and protecting the ocular surface against pathogens by means of antibacterial substances.4,5 Although this surface is relatively stable in healthy patients, the precorneal tear film will eventually break up if not resurfaced by the blinking eye lids.6 During intraocular surgical procedures, a transparent cornea is essential in order to allow the surgeon good visualization of the ocular structures located behind the cornea, in the anterior chamber or in the posterior segment of the eye. Thus, irrigation by wetting agents (e.g., balanced salt solution [BSS] or BSS with glutathione [BSS Plus {BSS+}]), performed by the surgeon or assistant, is required throughout the surgery to maintain corneal hydration and transparency. Several environmental and patient-related factors may influence the ocular surface and therefore, loss of corneal clarity during anterior segment as well as vitreoretinal surgery. These factors include: use of anesthetic and topical mydriatic agents, long surgery (e.g., vitreoretinal surgery), high temperature and low humidity in the operating room, intensity of the microscope illumination, and patients with a history of dry eye syndrome.7–13 In such cases, repeated instillations of wetting agents are required. However, excessive application of physiological solutions may harm the epithelium, stroma, and endothelium.10 Furthermore, Emre et al.10 suggested that fewer rewetting events are required when a viscoelastic fluid is applied over the corneal surface instead of BSS.
The aims of this study were to develop a safe, noninvasive, real-time, and noncontact approach for monitoring tear film stability in vivo and to compare the effectiveness of a viscoelastic fluid in maintaining a smooth ocular surface to that of BSS+. This study developed an objective, quantitative measure of tear film stability in an animal model (New Zealand White [NZW] rabbits) and assessed the efficacy of viscoelastic fluid to reduce the frequency of irrigation during ophthalmic surgery.
Methods
Procedure
Experiments were carried out in 10 NZW rabbits (age < 3 months; weight, 2.4 ± 0.4 kg). Rabbits were anesthetized by intramuscular injection. Each rabbit received 1 drop of a viscoelastic fluid (2% hydroxypropylmethylcellulose; Cornea Protect; Croma-Pharma GmbH, Leobendorf, Austria) on one eye and several drops of a BSS enriched with bicarbonate, dextrose, and glutathione (BSS Plus [BSS+] irrigating solution; Alcon, Inc., Fort Worth, TX, USA) on the contralateral eye. Experiments were performed in the following sequence for rabbit 1:
A lid speculum was inserted in the right eye without touching the cornea, and viscoelastic was applied to the center of the right eye.
While the left eye was covered with a patch to prevent dehydration, the right eye was monitored through the operating microscope (OPMI) for 20 minutes.
The lid speculum was removed, and the right eye was covered with a patch.
A lid speculum was inserted in the left eye, and BSS+ was applied to the center of the right eye.
While the right eye was covered with a patch, the left eye was monitored through the OPMI for 20 minutes.
The next animal received BSS+ on the right eye and viscoelastic on the left eye, where the order and side were alternated between experiments to eliminate bias. This procedure resulted in a total of 5 eyes with BSS+ on the right eye, 5 eyes with BSS+ on the left eye, 5 eyes with viscoelastic on the right eye, and 5 eyes with viscoelastic on the left eye, such that BSS+ experiments were carried out first in 5 rabbits and viscoelastic experiments were carried out first in the other 5 rabbits. The preservative-free viscoelastic comes in a sterile unidose package. BSS+ was used, as opposed to BSS, because it was found to be less harmful to the endothelial barrier than BSS.14 Room temperature was 19 ± 3°C, and relative humidity was 50 ± 5%. OPMI magnification was set at ×7 and sharply focused on the cornea by the surgeon. At the start of all cases, a video recording and a digital timer controlling a digital single-lens reflex camera were set up to produce a DVD as well as high resolution digital images (14 million pixels) every 5 seconds for the 20-minute duration. For each eye studied, our ophthalmic surgeon watched the corneal surface through the OPMI and decided, based on clinical impression, when it was necessary to apply either viscoelastic or BSS+. The same staff performed all experiments in the 20 eyes of the 10 animals in the exact same manner. All experiments were conducted in accordance with the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research and approved by the University of Miami Institutional Animal Care and Use Committee (IACUC).
Image and Data Analysis
Once a 20-minute test was completed, the recorded video was subjected to postprocessing operations consisting of specialized software using LabView (National Instruments Corp., Austin, TX, USA), designed to analyze the reflection cast by the coaxial illumination of the operating microscope. Using the particle image analysis feature, the software was able to characterize the shape of the corneal reflection that became distorted as the surface of the precorneal tear film evaporated (Fig. 1). For each data set (n = 20), a region of interest (ROI) was manually selected around the strongest reflection, to reduce the possibility of detecting multiple reflections (Fig. 2). The ROI was set based on the first image in the sequence, and none of the experiments involved motion significant enough to require movement of the ROI to track the reflection. Simple thresholding was used to segment the boundary of the reflection, which was then characterized as described below. The results of this characterization were not made known to the surgeon during the experiment, and the system did not include a visual or audible threshold detection signal. In other words, the software was not used in any way to guide or alter the behavior of the surgeon; it was used only to characterize the corneal reflection.
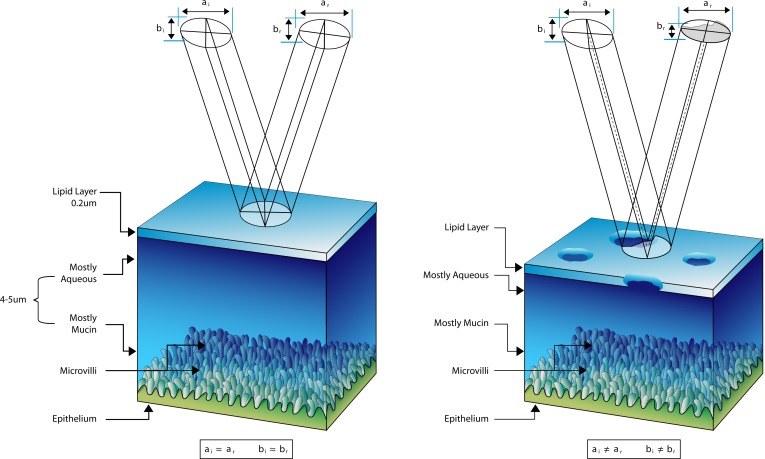
Figure 1.
Tear film immediately after resurfacing by the eye lids (left) and after surface evaporation (right). The elliptical projection represents the specular component of the coaxial illumination of the operation microscope, where the major and minor axes of the ellipse are given by a and b, respectively, upon incidence (subscript i) and reflection (subscript r). After surface evaporation, the shape of the reflection becomes distorted, such that ai ≠ ar and bi ≠ br.
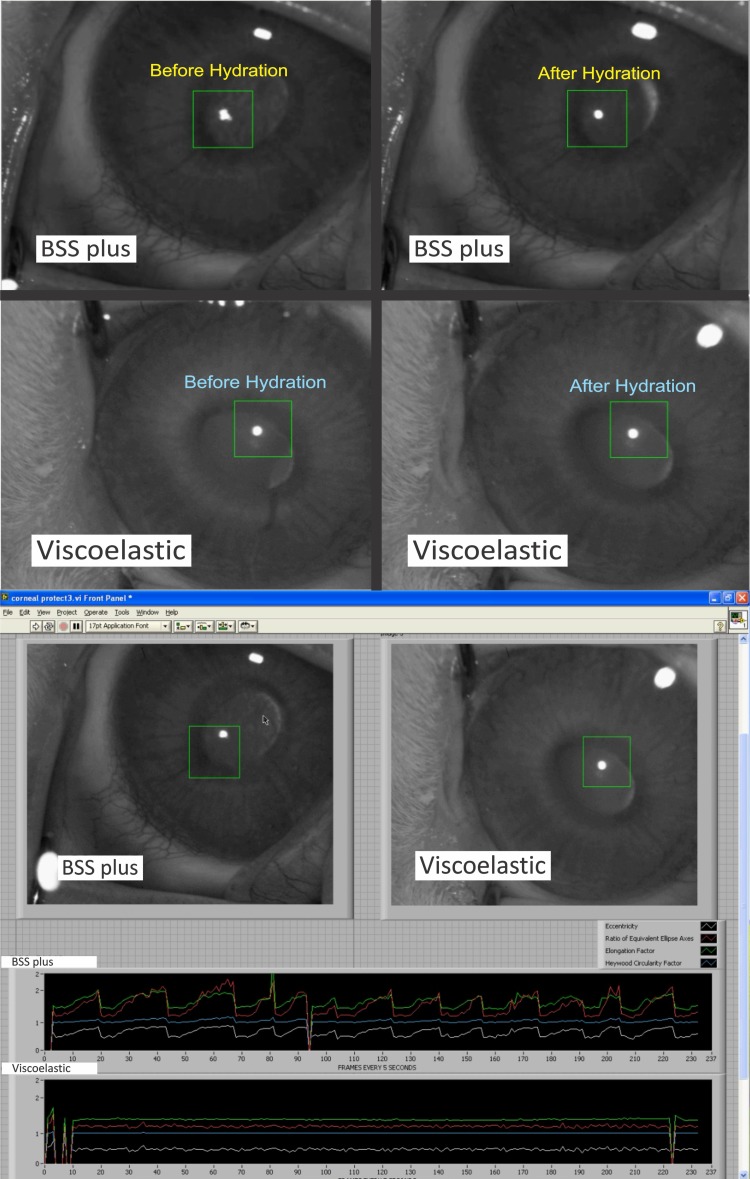
Figure 2.
Image series showing the effect of tear film evaporation on the shape of the corneal reflection (top). The LabView graphic user interface shows a rabbit treated with BSS+ and viscoelastic along with the corresponding reflection metrics (bottom).
Initially, four parameters were identified as potential candidates for quantification of the distortion of the reflection: Heywood circularity factor, eccentricity, ratio of equivalent ellipse axes, and elongation factor. A preliminary analysis indicated that the ellipse axes ratio parameter provided the best compromise between sensitivity and response amplitude, so that parameter was used for the final comparison of the evaporation dynamics of BSS+ and viscoelastic. The ellipse axes ratio was defined by an equivalent ellipse. The equivalent ellipse was obtained by fitting an ellipse to the reflection contour by using standard least square regression techniques to minimize the error of the fit. In particular, the area of the ellipse was set to match the area of the reflection, and the major and minor axes and the position and angular orientation of the ellipse were adjusted iteratively until the error of the fit was minimized and the equivalent ellipse was obtained. The ratio of equivalent ellipse axes was the ratio of major axis to minor axis, where a ratio of unity corresponded to a perfectly circular reflection.
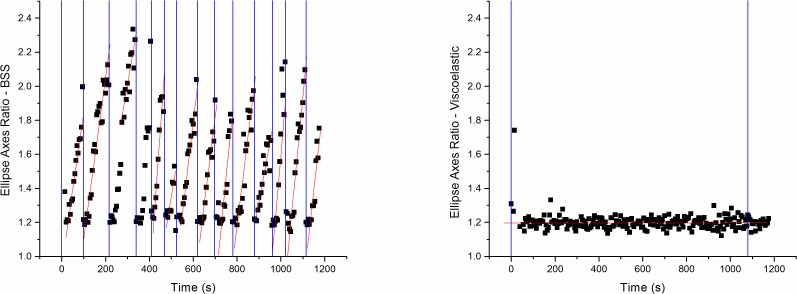
Each frame of the 20-minute time series was processed and the data stored. Data were segmented into epochs representing each application of either viscoelastic or BSS+. The rate of tear film evaporation was calculated with Origin 7 software (Origin Lab, Northampton, MA, USA); a linear fit was obtained through least squares regression for each dose, where the slope of the line was an indication of the rate at which the tear film evaporated after each application of either viscoelastic or BSS+. Because the ellipse axes ratio was unitless, the slope of this ratio as a function of time was given by units of inverse seconds. Figure 3 shows the typical changes observed after application for one rabbit.
Figure 3.
Both graphs show the ellipse axes ratio as a function of time, where the blue vertical lines indicate the application of either BSS+ (left) or viscoelastic (right), and the red lines indicate the best fit line for that particular evaporation event. Applications of viscoelastic or BSS+ that yielded a negative slope, or in cases where the image data contained artifacts, were treated as null events and were not used for the analysis.
Results
The 10 eyes treated with BSS+ required 7.5 ± 2.7 applications to maintain the precorneal tear film during the 20-minute test period, giving a mean dose duration time of 2.4 ± 0.9 minutes. The 10 eyes treated with viscoelastic required 1.4 ± 0.5 applications, with a mean dose duration time of 16 ± 5.1 minutes (Fig. 4). The wetting frequency was significantly reduced in eyes treated with viscoelastic, such that the mean dose duration time was significantly longer (P < 0.001).
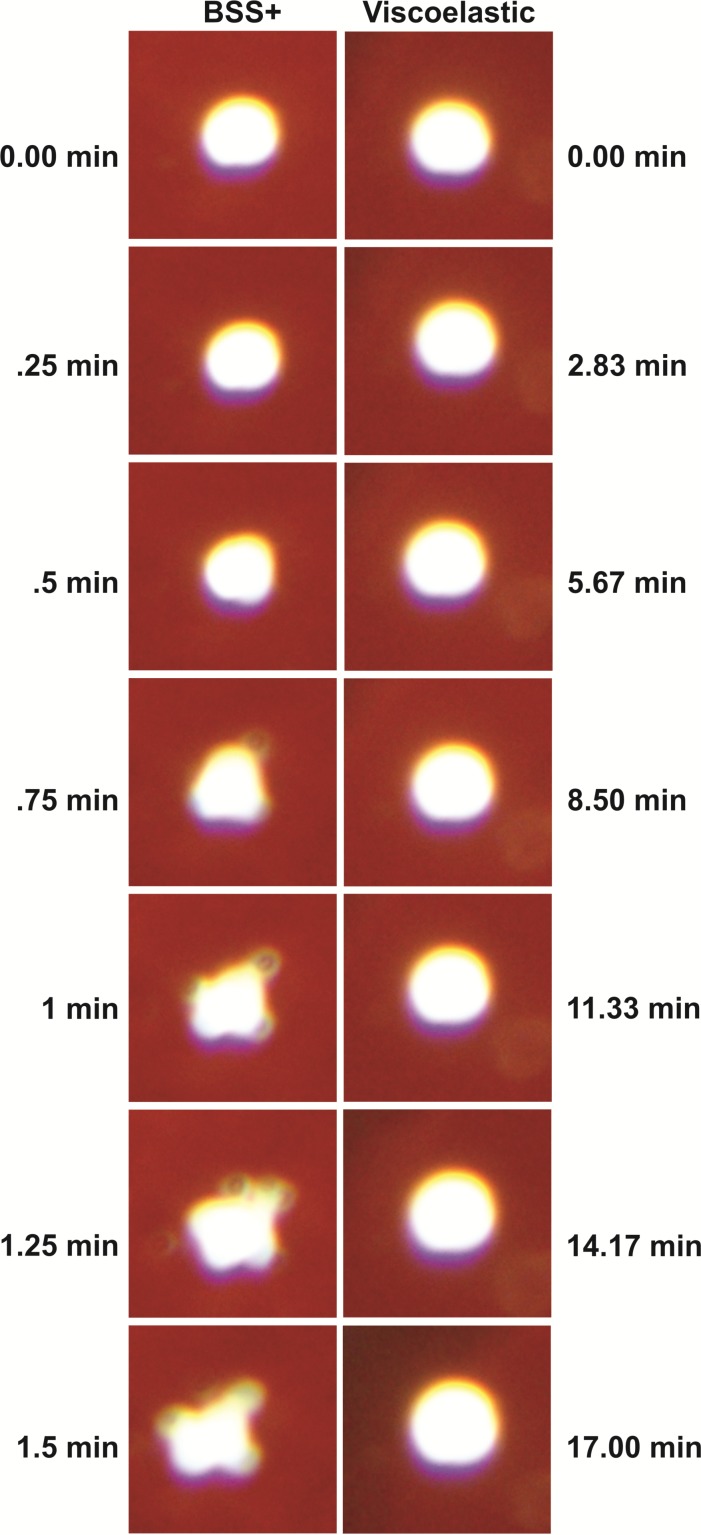
Figure 4.
Image series shows an enlarged view of the corneal reflection in contrast against the red background of the rabbit retina for both BSS+ and viscoelastic for the same rabbit. Clearly, the shape of the reflection is much more rapidly distorted with BSS+. It is notable that some motion of the corneal reflection was observed, but the edges of the reflection remain within the region of interest.
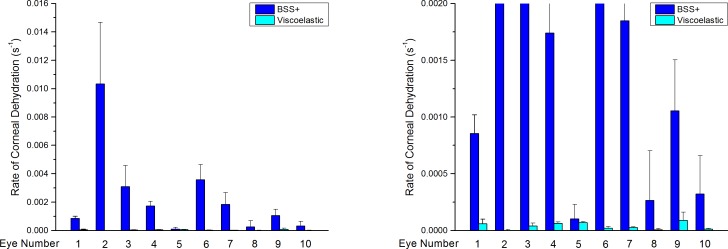
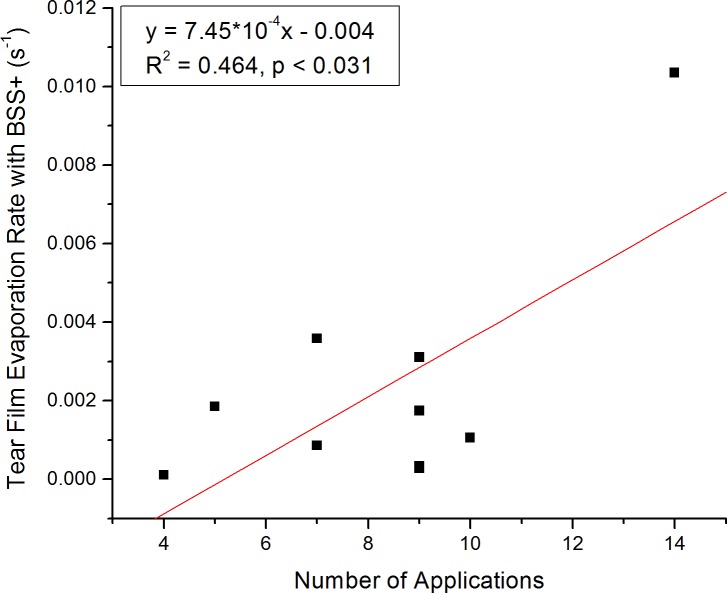
Despite significant variations among animals (coefficient of variation = 0.87), the rate of tear film evaporation differed significantly (P < 0.043) between viscoelastic ([39 ± 9.6] · 10−6 s−1) and BSS+ ([2321 ± 966] · 10−6 s−1) (Fig. 5), and in the case of BSS+, the rate of evaporation was correlated (P < 0.031) with the number of applications that were required to maintain the tear film (Fig. 6).
Figure 5.
Rate of tear film evaporation for all 10 eyes is shown in dark blue for BSS+ and in cyan for viscoelastic (left) applications. The graph (right) shows the same data but with the y-axis adjusted so that the rate of tear film evaporation with viscoelastic can be put into perspective at the cost of clipping some of the BSS data (right).
Figure 6.
Tear film evaporation rate with BSS+ as a function of the number of applications of BSS+, showing a positive correlation between the two parameters.
Discussion
In this experimental study, we investigated the effectiveness of a viscoelastic at preventing tear film evaporation and compared its performance to that of BSS+, with the aim of examining the potential to reduce the need for frequent irrigations to maintain a hydrated cornea during surgery. Our findings indicate that the prevention of corneal dehydration due to surface evaporation can be controlled more effectively with a viscoelastic than with BSS+ in the rabbit, and this may hold similar implications for the human cornea. In fact, we are 95% confident that NZW rabbit corneas treated with BSS+ dehydrate at least 9 times more rapidly than those treated with viscoelastic.
The limitations to this study include the extrapolation used to estimate the duration of the dose of viscoelastic required to maintain optimal corneal hydration. The cornea irrigation data indicate that BSS+ lasts 2.4 ± 0.9 minutes and that viscoelastic lasts 16 ± 5.1 minutes. Using the surgically obtained BSS+ duration as a gauge for the measured rate of evaporation, we obtained a value of 77 ± 38 minutes for the duration of viscoelastic. The subjective nature guiding the application of the cornea wetting agent during the experiment is likely responsible for the inconsistency between the two measures of viscoelastic duration. The disparity between these two results suggests that the surgeon may have over-applied viscoelastic. A follow-up investigation could use the reflection analysis software in real-time mode, with established cutoff values for the corneal hydration parameter to indicate when the cornea is too dry and requires another dose of wetting agent, thus eliminating the surgeon's subjective judgment from the study. Also, the surgeon and staff were not masked to the nature of the wetting agent, as the significant differences in the shape of the containers and the viscosity of the two wetting agents were immediately apparent during application. In addition, a comparable study should be performed in human corneas to verify that the results hold for humans.
Similarly, Arshinoff et al.15 describes an elastoviscous hylan surgical shield (HsS, 0.45%; Biomatrix Medical Canada, Inc., Pointe-Claire, Quebec, Canada) which showed a retention time 10.7 times greater than that of BSS, and Wessels et al.16 showed that Healon (Pharmacia-AMO, Abott Park, IL, USA) has a retention time that is 9 times greater than BSS. Chen et al.17 compared the corneal wetting properties of BSS+ to those of Cornea Protect during cataract surgery. They found that BSS+ was applied 10 times more frequently than the viscoelastic and that optical clarity was superior with the viscoelastic. Kalyanasundaram and Hasan18 found a reduction in the frequency of corneal irrigation applications when anesthetic lignocaine jelly was used instead of topical lidocaine. Overall, the results in the literature roughly match our findings with the viscoelastic; we observed a more than 9-fold increase in retention time with viscoelastic, while others found a 9- to 11-fold increase when comparing various viscoelastic fluids to BSS. In this context, it seems that the benefit of longer lasting corneal hydration is due to the high viscosity of the substance used in these studies.
In conclusion, the shape and surface area of the corneal reflection are strongly correlated with the state of the precorneal tear film. Also, the shape of the corneal reflection can be automatically detected and quantified, thus providing an unbiased means of assessing tear film stability in a noninvasive manner. Corneas treated with viscoelastic present a tear film that is stable significantly longer than corneas treated with BSS (P < 0.043). The viscoelastic maintained a stable tear film more than 9 times longer than BSS+, on average. Therefore, viscoelastic is better at preventing corneal tear film evaporation than BSS+ in a rabbit model. Further prospective randomized studies performed in humans are needed to confirm these findings.
Acknowledgments
The authors thank Eleut Hernandez, LAT, for technical support.
Presented in part at the annual meeting of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, Florida, United States, May 2012.
Supported by Croma-Pharma GmbH, Center Grant P30EY14801, Florida Lions Eye Bank, an unrestricted grant from Research to Prevent Blindness, and the Henri and Flore Lesieur Foundation (JMAP).
Disclosure: D. Nankivil, None; A. Gonzalez, None; E. Arrieta, None; C. Rowaan, None; M.C. Aguilar, None; K. Sotolongo, None; F.A. Cabot, None; S.H. Yoo, None; J.M.A. Parel, Croma-Pharma GmbH (F)
References
- 1. Wolff E. The muco-cutaneous function of the lid margin and the distribution of the tear fluid. Trans Ophthalmol Soc UK. 1946; 66: 291–308 [Google Scholar]
- 2. Wolff E. The Anatomy of the Eye and Orbit. 4th ed. London: HK Lewis and Co.; 1954; 49 [Google Scholar]
- 3. International Dry Eye WorkShop. Report of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5( 2); 65–204 [DOI] [PubMed] [Google Scholar]
- 4. Ohashi Y, Dogru M, Tsubota K. Laboratory findings in tear fluid analysis. Clin Chim Acta. 2006; 369: 17–28 [DOI] [PubMed] [Google Scholar]
- 5. Montes-Mico R. Role of the tear film in the optical quality of the human eye. J Cataract Refract Surg. 2007; 33: 1631–1635 [DOI] [PubMed] [Google Scholar]
- 6. Norn MS. Desiccation of the precorneal tear film: corneal wetting time. Acta Ophthalmol. 1969; 47: 865–880 [DOI] [PubMed] [Google Scholar]
- 7. Edelhauser HF, Van Horn DL, Hyndiuk RA, Schultz RO. Intraocular irrigating solutions. Their effect on the corneal endothelium. Arch Ophthalmol. 1975; 93: 648–657 [DOI] [PubMed] [Google Scholar]
- 8. Edelhauser HF, Hine JE, Pederson H, et al. The effect of phenylephrine on the cornea. Arch Ophthalmol. 1979; 97: 937–947 [DOI] [PubMed] [Google Scholar]
- 9. de Souza IR, de Souza AP, de Queiroz AP, Figueiredo P, Jesus RS, Kara-José N. Influence of temperature and humidity on laser in situ keratomileusis outcomes. J Refract Surg. 2001; 17( suppl 2); S202–204 [DOI] [PubMed] [Google Scholar]
- 10. Emre S, Akkin C, Afrashi F, Yagci A. Effect of corneal wetting solutions on corneal thickness during ophthalmic surgery. J Cataract Refract Surg. 2002; 28: 149–151 [DOI] [PubMed] [Google Scholar]
- 11. Asensio I, Rahhal SM, Alonso L, et al. Corneal thickness values before and after oxybuprocaine 0.4% eye drops. Cornea. 2003; 22: 527–532 [DOI] [PubMed] [Google Scholar]
- 12. Gao L, Fan H, Cheng AC, Wang Z, Lam DS. The effects of eye drops on corneal thickness in adult myopia. Cornea. 2006; 25: 404–407 [DOI] [PubMed] [Google Scholar]
- 13. Hwang HB1, Kim HS. Phototoxic effects of an operating microscope on the ocular surface and tear film. Cornea. 2014; 33: 82–90 [DOI] [PubMed] [Google Scholar]
- 14. Li J, Akiyama R, Kuang K, Fischbarg J. Effects of BSS and BSS+ irrigation solutions on rabbit corneal transendothelial electrical potential difference. Cornea. 1993; 12: 199–203 [DOI] [PubMed] [Google Scholar]
- 15. Arshinoff SA, Khoury E. HsS vs BSS as a corneal wetting agent during routine cataract extraction and lens implantation. J Cataract Refract Surg. 1997; 23: 1221–1225 [DOI] [PubMed] [Google Scholar]
- 16. Wessels IF, DeBarge R, Wessels DA. Salvaged viscoelastic reduces irrigation frequency during cataract surgery. Ophthalmic Surg Lasers. 1998; 29: 688–691 [PubMed] [Google Scholar]
- 17. Chen Y-A, Hirnschall N, Findl O. Comparison of corneal wetting properties of viscous eye lubricant and balanced salt solution to maintain optical clarity during cataract surgery. J Cataract Refract Surg. 2011; 37: 1806–1808 [DOI] [PubMed] [Google Scholar]
- 18. Kalyanasundaram TS, Hasan M. Corneal-wetting property of lignocaine 2% jelly. J Cataract Refract Surg. 2002; 28: 1444–1445 [DOI] [PubMed] [Google Scholar]