Abstract
There has been a increasing interest in understanding emotion regulation deficits in social anxiety disorder (SAD; e.g., Hofmann, Sawyer, Fang, & Asnaani, 2012). However, much remains to be understood about the patterns of associations among regulation strategies in the repertoire. Doing so is important in light of the growing recognition that people’s ability to flexibly implement strategies is associated with better mental health (e.g., Kashdan et al., 2014). Based on previous work (Aldao & Nolen-Hoeksema, 2012), we examined whether putatively adaptive and maladaptive emotion regulation strategies interacted with each other in the prediction of social anxiety symptoms in a sample of 71 participants undergoing CBT for SAD. We found that strategies interacted with each other and that this interaction was qualified by a three-way interaction with a contextual factor, namely treatment study phase. Consequently, these findings underscore the importance of modeling contextual factors when seeking to understand emotion regulation deficits in SAD.
Keywords: Emotion regulation, Adaptive regulation strategies, Maladaptive regulation strategies, Social anxiety, Cognitive behavioral therapy
1. Background
In the past decade, there has been growing interest in understanding emotion regulation difficulties in social anxiety disorder (SAD; e.g., Hofmann, 2010; Hofmann et al., 2012; Kashdan et al., 2014; Kashdan & Steger, 2006; Moscovitch, Suvak, & Hofmann, 2010; Turk, Heimberg, Luterek, & Mennin, 2005). In non-clinical samples, symptoms of social anxiety have been associated with the use of the putatively maladaptive strategies of suppression (e.g., Kashdan & Breen, 2008; McLean, Miller, & Hope, 2007; Perini, Abbott, & Rapee, 2006), experiential avoidance (e.g., Santanello & Gardner, 2007), and rumination/post-event processing (e.g., Brozovich & Heimberg, 2008; Kashdan & Roberts, 2007; Perini et al., 2006). In clinical samples, participants diagnosed with SAD have tended to report making greater use of the putatively maladaptive strategies of expressive suppression, rumination, and experiential avoidance and lesser use of the putatively adaptive strategy of reappraisal than healthy controls (e.g., D’Avanzato, Joormann, Siemer, & Gotlib, 2013; Kashdan et al., 2013). Underscoring the clinical implications of studying the habitual use of emotion regulation strategies in SAD, Moscovitch et al. (2012) have found that patients who responded to CBT exhibited an increase in their habitual use of the putatively adaptive strategy of reappraisal from pre- to mid-treatment assessments (this was not the case for suppression). Similarly, Goldin et al. (2012) have found that, relative to patients with SAD in a wait list control condition, those who underwent CBT showed increased self-efficacy in the use of reappraisal.
Although these studies represent important initial steps in furthering our understanding of emotion regulation deficits in SAD, they are limited in that they have largely consisted of the examination of regulation strategies independently of one another. Consequently, much remains to be understood about the patterns of associations among strategies in the repertoire. Doing so is particularly important in light of a growing understanding that people’s ability to flexibility select and implement various strategies from their repertoires in response to varying contextual demands is associated with good mental health outcomes (e.g., Aldao, 2013; Bonanno & Burton, 2013; Kashdan & Rottenberg, 2010; Kashdan et al., 2014; Sheppes et al., 2014). Thus, in this investigation, we sought to conduct a broader examination of the repertoire of regulation strategies in SAD by comparing the magnitudes of their associations with symptoms and testing whether they interact with each other in the prediction of such symptoms in the context of CBT.
The framework for this investigation is a growing body of research on emotion regulation strategies and psychopathology that suggests that some emotion regulation strategies (e.g., avoidance, expressive suppression) are ineffective at modifying affect in experimental studies, and seem to be associated with greater levels of psychological symptoms. These strategies have been conceptualized as putatively maladaptive (e.g., Aldao, Nolen-Hoeksema, & Schweizer, 2010; Webb, Miles, & Sheeran, 2012). Conversely, other emotion regulation strategies (e.g., reappraisal, acceptance) are effective at modifying affect in laboratory settings, and seem to have negative associations with clinical symptoms. These strategies have been conceptualized as putatively adaptive (Aldao et al., 2010).
It has been widely assumed that both the presence of mal-adaptive strategies and the absence of adaptive strategies put a person at increased risk for psychopathology (e.g. Aldao et al., 2010; Gross & Jazaieri, 2014; Kring & Sloan, 2009). Initial work comparing the associations between symptoms of psychopathology and putatively adaptive and maladaptive strategies suggests these relationships might be of comparable magnitudes. For example, in the validation paper for the emotion regulation questionnaire, the correlation between depressive symptoms and the habitual use of expressive suppression was .25, and the correlation between depressive symptoms and habitual use of reappraisal was −.23 (Gross & John, 2003). Further, these putatively adaptive and maladaptive strategies did not interact with each other in the prediction of symptoms (Gross & John, 2003), suggesting that their effects might be additive.
However, two recent sets of findings call into question both of these assumptions. First, a meta-analytic review suggests that the habitual use of putatively adaptive strategies may have a weaker association with various symptoms of psychopathology (e.g., depression, anxiety, eating disorders, substance abuse) than the habitual use of putatively maladaptive strategies (d for adaptive = −.21; d for maladaptive = .40; Aldao et al., 2010). In other words, the relationship between strategies and mental health might be characterized by a substantial asymmetry, in which some strategies might play a larger role in the etiology, maintenance, and treatment of disorders.
Second, and more importantly, Aldao and Nolen-Hoeksema (2012) examined the relationship between emotion regulation strategies and mental health in a large community sample and found that the habitual use of putatively adaptive strategies (acceptance, positive reframing) interacted with the habitual use of putatively maladaptive strategies (behavioral disengagement, denial) in the prediction of a composite scores of symptoms of anxiety, depression, and alcohol abuse. Specifically, for participants who reported using high levels of putatively maladaptive strategies, the use of putatively adaptive strategies had the expected negative association with the composite score of symptoms. However, for participants who reported using low levels of putatively maladaptive strategies, the association between putatively adaptive strategies and psychopathology was non-significant. These findings lend support to the growing literature on emotion regulation flexibility, as they indicate that putatively adaptive strategies might be most beneficial when people are utilizing a wider range of strategies. More broadly, they suggest that modeling interactions among regulation strategies can be a very important avenue for furthering our understanding of the emotion regulation deficits that characterize mental disorders.
In the present investigation, we adopted a broader approach to the study of the emotion regulation repertoire in order to develop a more in-depth understanding of the patterns of emotion dysregulation in SAD. Participants were part of a randomized control trial of cognitive behavioral therapy for SAD (Hope, Heimberg, & Turk, 2006) and they provided weekly ratings of their use of regulation strategies and their experience of social anxiety symptoms. This afforded us the opportunity to examine the relationships between putatively adaptive/maladaptive strategies and symptoms at the state level, on a weekly basis. This is particularly important because emotions, their regulation, and symptoms of psychopathology fluctuate substantially over time (e.g., Aldao, 2013; Barrett, Gross, Christensen, & Benvenuto, 2001; Bylsma & Rottenberg, 2011; Ebner-Priemer & Trull, 2009; Robinson & Clore, 2002; Srivastava, Tamir, McGonigal, John, & Gross, 2009). In addition, because such assessments were obtained in the context of treatment, they reflected dynamic changes in participants’ symptoms and patterns of emotion regulation (e.g., Fentz et al., 2013; Kazdin, 2007)
It is noteworthy that the treatment study consisted of three distinct phases that varied in the extent to which participants were asked to regulate their social anxiety (see Gloster et al., 2013 for a similar approach to CBT for panic disorder). In the first 7 sessions, participants primarily received psychoeducation and learned cognitive restructuring. This constituted the cognitive phase, in which participants began to learn about more effective ways of regulating their emotions by practicing cognitive restructuring skills. In the next 9 sessions, participants continued practicing cognitive restructuring, but did so within the context of structured in-session and out of session behavioral exposures to social anxiety provoking situations (i.e., cognitive + behavioral exposure phase). Here, participants were required to actively confront feared situations and, thus, to frequently practice the new patterns of emotion regulation that they had been learning. After treatment was completed, participants were assessed every three months over the course of a year (i.e., follow-up phase). During this time, they were encouraged to utilize the skills they had acquired over the course of treatment. Given the heterogeneity in emotion regulation demands across the various study phases, we thought it unwise to assume that the associations between weekly emotion regulation and anxiety symptoms would be invariant across study phase. Consequently, we tested whether the associations between strategies and symptoms would be moderated by treatment study phase (e.g., Gloster et al., 2013)
Based on prior meta analytic work (e.g., Aldao et al., 2010), we hypothesized that the negative association between weekly social anxiety symptoms and use of putatively adaptive strategies would be weaker than the positive association between symptoms and putatively maladaptive strategies. In addition, we expected the weekly use of putatively adaptive and maladaptive strategies to interact with each other in the prediction of weekly social anxiety symptoms (e.g., Aldao & Nolen-Hoeksema, 2012). We did not formulate specific predictions regarding the magnitude or the direction of this interaction in each treatment study phase.
2. Method
2.1. Participants
As part of a larger neuroimaging study examining CBT for SAD, participants were recruited through referrals, community flyers, and web listings advertising a free treatment at Stanford University (see Goldin et al., 2014) for detailed methods. We screened 436 individuals over the telephone to obtain preliminary eligibility information based upon the study inclusion/exclusion criteria (described in detail in the next section). Individuals who met these criteria (N = 110) were invited to participate in an in-person clinical diagnostic interview (see CONSORT Supplemental Fig. 1). A total of 71 participants (see Table 1 for demographic and clinical variables) met diagnostic criteria for a principal diagnosis of generalized SAD according to the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994) and were invited to participate in a 16 sessions of individual CBT for generalized SAD. We randomly assigned them to either immediate CBT or to a wait list (WL) group using Efron’s biased coin randomization procedure (Efron, 1971), which results in approximately equal sample sizes throughout the duration of a clinical trial. Participants assigned to the WL group received treatment after 16 weeks, after which they had 4 week to complete all baseline assessments and start treatment. All participants received free treatment and they provided informed consent in accordance with the Institutional Review Board at Stanford University.
Table 1.
Participant characteristics.
| Variable | SAD n = 71 |
|---|---|
| Gender (Males, n, %) | 37 (52.1%) |
| Age (years, M ± SD) | 33.7 ± 8.94 |
| Years of Education (M ± SD) | 16.80 ± 2.38 |
| Ethnicity (n, % Caucasian) | 41 (57.7%) |
| Yearly income ($1000 s, M ± SD) | 66.56 ± 45.03 |
| Marital status (n, %) | |
| Single, never married | 49 (69%) |
| Married | 19 (26.8%) |
| Divorced or separated | 3 (4.2%) |
| Current Axis I comorbidity (n, %) | |
| Generalized anxiety disorder | 12 (16.9%) |
| Specific phobia | 5 (7%) |
| Panic disorder | 3 (4.2%) |
| Dysthymic disorder | 3 (4.2%) |
| Past Axis-I comorbidity (n, %) | |
| Major depressive disorder | 16 (22.5%) |
| Dysthymic disorder | 1 (1.4%) |
| Post-traumatic stress disorder | 1 (1.4%) |
| Panic disorder | 1 (1.4%) |
| Substance abuse disorder | 5 (7%) |
| Eating disorder | 1 (1.4%) |
| Obsessive-compulsive disorder | 1 (1.4%) |
| Past non-CBT Psychotherapy (n, %) | 36 (50.7%) |
| Past Pharmacotherapy (n, %) | 23 (32.4%) |
| Age at symptom onset (years, M ± SD) | 13.0 ± 7.25 |
| Years since symptom onset (M ± SD) | 20.84 ± 12.0 |
Note: SD = standard deviation.
We required that all participants be 21–55 years of age, speak fluent English, not be in treatment (psychotherapy or pharmacotherapy), and have no history of medical disorders. In addition, because this study was part of a larger investigation entailing fMRI data collection, we required that all participants be right-handed (as assessed by the Edinburgh Handedness Inventory; Oldfield, 1971), pass an MRI safety screen, and have no history of head trauma or neurological disorders. All participants had to meet DSM-IV criteria for a principal diagnosis of generalized SAD as assessed by the Anxiety Disorders Interview Schedule for the DSM-IV-Lifetime version (ADIS-IV-L; DiNardo, Brown, & Barlow, 1994). As noted in Table 1, generalized SAD participants were excluded for co-morbid psychiatric disorders other than secondary diagnoses of generalized anxiety disorder, specific phobia, panic disorder, and dysthymia.
2.2. Clinical intervention
We utilized the Managing Social Anxiety: A Cognitive-Behavioral Therapy Approach, which is a 16-session manualized treatment protocol which includes a therapist guide (Hope et al., 2006) and a client workbook (Hope, Heimberg, Juster, & Turk, 2000). The first treatment phase (sessions 1–7), consists primarily of psychoeducation about generalized SAD, orientation to the CBT model, and training in cognitive restructuring skills. In the second treatment phase (sessions 8–16), participants actively engage in gradual in vivo exposures to feared social situations, while continuing to use cognitive restructuring skills to examine and challenge their dysfunctional core beliefs. Participants engage in behavioral exposures both within the therapy session and outside of sessions, as homework. All treating therapists achieved proficiency in implementing CBT prior to treating study participants and met treatment adherence criteria (for details see Goldin et al., 2012)
2.3. Measures
2.3.1. Regulation strategies
At the beginning of each session (and every 3 months for a year following treatment), participants rated how often they had used specific emotion regulation strategies to manage the social anxiety they experienced in the past 7 days. They provided ratings of their use of each strategy via one-item measures ranging from 0% (not at all) to 100% (all the time) (see Robins, Hendin, & Trzesniewski, 2001 for information on utilizing one-item measures).
2.3.1.1. Maladaptive strategies
We adapted four items corresponding to four phases of the process model of emotion regulation to capture the patterns of maladaptive avoidance that characterize SAD (Werner & Gross, 2010). Specifically, we assessed situational avoidance (“how often did you try to avoid social situations or aspects of the situations”), situation modification (“how often did you try to modify the social situations”), attentional deployment (“how often did you try to distract yourself?”), and expressive suppression (“how often did you try to hide all visible signs of your anxiety”). We averaged these four strategies into a composite score called “maladaptive avoidance strategies” (α = .69). Exploratory factor analysis provides evidence for a unitary construct (eigenvalue = 2.13, 53% variance explained; each variable had a factor loading > .605).4
2.3.1.2. Adaptive strategies
We assessed participants’ utilization of cognitive reappraisal (“how often did you try to change the way you were thinking about the situation you were in?”) and acceptance (“how often did you try to just accept your anxiety and not change it in any way?”). We averaged these two strategies into a composite “adaptive engagement strategies” score (r = .22, p < .01; α cannot be calculated with only 2 items) on the basis of conceptual and methodological grounds. First, the conceptual boundaries between acceptance and reappraisal might be blurrier than it is frequently assumed (see Hayes, 2008; Hofmann, 2008; Hofmann & Asmundson, 2008; Hofmann et al., 2012; but also see, Farb, Anderson, Irving, & Segal, 2014; McRae, Ciesielski, & Gross, 2012; Werner & Gross, 2010). Second, the empirical evidence supporting a functional differentiation between these strategies is promising, yet equivocal. This is particularly clear upon closer inspection of their effects across emotional modalities (subjective feelings, physiological arousal), which reveals that they sometimes have comparable effects and at other times they do not (e.g., Aldao & Mennin, 2012; Hofmann, Heering, Sawyer, & Asnaani, 2009; Szasz, Szentogotai, & Hofmann, 2011; Wolgast, Lundh, & Viborg, 2011). In addition, the focus of this investigation to understand their associations with symptoms of psychopathology. In this respect, it is appropriate to combine reappraisal and acceptance, since they have shown comparable adaptive associations with symptoms. In the meta-analysis by Aldao et al. (2010), acceptance had a mean effect size of −.19 and reappraisal had a mean effect size of −.14. Their confidence intervals overlapped (acceptance: −.40 to .05; reappraisal: −.20 to −.07), thus suggesting that these effect sizes are not statistically significant from each other.
2.3.2. Social anxiety
Each week during treatment (and every 3 months for a year following treatment), participants provided ratings of their social anxiety symptoms over the past 7 days. They rated 6 facets of social anxiety, including anticipatory anxiety (“how often have you gone over and over in your mind things that you think might go wrong before you entered social situations?”), in-the-moment anxiety (“how often have you been preoccupied by your anxiety while you were in social situations?”), post-event anxiety (“how often have you gone over and over social interactions in your mind after they have finished?”), anxiety intensity (“how intense has your social anxiety been?”), distress caused by the anxiety (“how distressed have you been by your social anxiety?”), and impairment caused by the anxiety (“how much has your social anxiety interfered with your life as a whole?”). We averaged these items into a composite “social anxiety” score (α = .91).
2.4. Overview of analyses
We used generalized estimating equations (GEE), which is an extension of the general linear model (GLM) that assumes correlated observations of dependent variables and are fairly robust to missing data and to misspecifications of the covariance matrix (e.g., Ghisletta & Spini, 2004; Liang & Zeger, 1986). The repeated measure component was session number. We specified an autoregressive (AR1) covariance structure because we expected observations to be correlated over time within each participant. We broke down significant interactions using simple slope analyses (Aiken & West, 1991). All the predictor variables were centered (mean equal zero) in order to facilitate interpretation (Tabachnick & Fidell, 2006).
3. Results
3.1. Preliminary analyses
Before conducting our main analyses, we examined how the measures of interest changed over time by running 3 GEE models, predicting weekly changes in social anxiety symptoms, use of maladaptive avoidance strategies, or use of adaptive engagement strategies by treatment study phase (N = 71 participants, n = 1088 observations). We found a significant two-way interaction between study phase and weekly changes in social anxiety symptoms, Wald’s χ2 = 9.11, p < .001, b = .39, SE (.13), CI (.14; .65), the use of mal-adaptive avoidance strategies, Wald’s χ2 = 11.03, p < .001, b = .45, SE (.13), (CI .18; .71), and the use of adaptive engagement strategies, Wald’s χ2 = 16.49, p < .001, b = −.71, SE (.17), CI (−1.05; −.37). Consequently, we examined weekly changes in the experience of social anxiety symptoms and the use of maladaptive avoidance and adaptive engagement strategies separately for each treatment study phase.
During the cognitive phase (N = 71, participants, n = 477 observations), the experience of social anxiety symptoms and the use of maladaptive avoidance strategies declined significantly every week, Wald’s χ2 = 48.78, p < .001, b = −2.09, SE (.30), CI (−2.67; − 1.50), Wald’s χ2 = 12.73, p < .001, b = −.90, SE (.25), CI (−1.39; −.40), respectively. The use of adaptive engagement strategies increased every week, Wald’s χ2 = 18.90 p < .001, b = 1.57, SE (.36), CI (.86; 2.28). We observed a similar pattern during the cognitive + behavioral exposures phase (N = 60 participants, n = 436 observations), Wald’s χ2 = 35.88, p < .001, b = −1.85, SE (.31), CI (−2.45; −1.24), Wald’s χ2 = 31.37, p < .001, b = −1.44, SE (.26), CI (−1.95; −.94), Wald’s χ2 = 4.98, p < .03, b = .69, SE (.31), CI (.08; 1.29), respectively.
On the other hand, during the follow-up phase (N = 53 participants, n = 175 observations), there were no changes in the experience of social anxiety symptoms or in the use of maladaptive avoidance or adaptive engagement strategies, Wald’s χ2 = .57, ns, b = .66, SE (.87), CI (−1.05; 2.37), Wald’s χ2 = 1.17, ns, b = .85, SE (.79), CI (−.69; 2.39), Wald’s χ2 = .03, ns, b = .13, SE (.81), CI (−1.46; 1.71), respectively. This suggests that the changes in the experience of social anxiety symptoms and in the use regulation strategies that took place during treatment were maintained during the 1-year follow-up. Table 2 contains the means and standard deviations for the average social anxiety symptoms and use of adaptive engagement and maladaptive avoidance strategies in each treatment study phase.
Table 2.
Means and standard deviations for anxiety and regulation strategies in each phase of treatment.
| Phase | Social anxiety symptoms | Maladaptive strategies | Adaptive strategies |
|---|---|---|---|
| Cognitive | 59.01 (17.41)** | 47.90 (17.03)** | 33.22 (19.69)** |
| Cognitive + behavioral exposures | 46.82 (16.62)** | 38.42 (16.90)** | 43.99 (16.84)** |
| Follow-up | 42.24 (21.68) | 37.89 (19.90) | 42.91 (20.84) |
p < .01 for changes in each variable over time within that phase.
3.2. Predicting weekly social anxiety symptoms with regulation strategies
We first ran an omnibus GEE model, in which we predicted weekly social anxiety symptoms with the weekly use of maladaptive avoidance and adaptive engagement strategies as well as with treatment study phase (N = 71 participants; n = 1088 observations). This analysis yielded a three-way interaction between treatment study phase, maladaptive avoidance, and adaptive engagement strategies, Wald’s χ2 = 17.15, p < .001, b = −.007, SE (.002), CI (−.01; −.003). Consequently, we examined the association between strategies and social anxiety symptoms separately in each treatment study phase.
3.2.1. Cognitive phase
We predicted weekly social anxiety symptoms with the weekly use of maladaptive avoidance and adaptive engagement strategies and their interaction (N = 71 participants; n = 477 observations). The weekly use of maladaptive avoidance strategies was positively associated with weekly social anxiety symptoms, Wald’s χ2 = 68.99, p < .001, b = .49, SE (.06), CI (.37; .60) and the weekly use of adaptive engagement strategies was marginally associated with lower weekly social anxiety symptoms, Wald’s χ2 = 2.93, p = .09, b = −.09, SE (.05), CI (−.20; .01). We compared the magnitude of the coefficients for adaptive engagement and maladaptive avoidance strategies by examining whether their confidence intervals overlapped. Because these coefficients were in opposite directions, we re-ran the model with a reversed coefficient for adaptive engagement strategies. Its confidence interval then became (−.01; .20). Given that the confidence intervals for maladaptive avoidance (.37; .60) and reversed adaptive engagement strategies (−.01; .20) did not overlap, we can conclude that the coefficients significantly differed from each other.
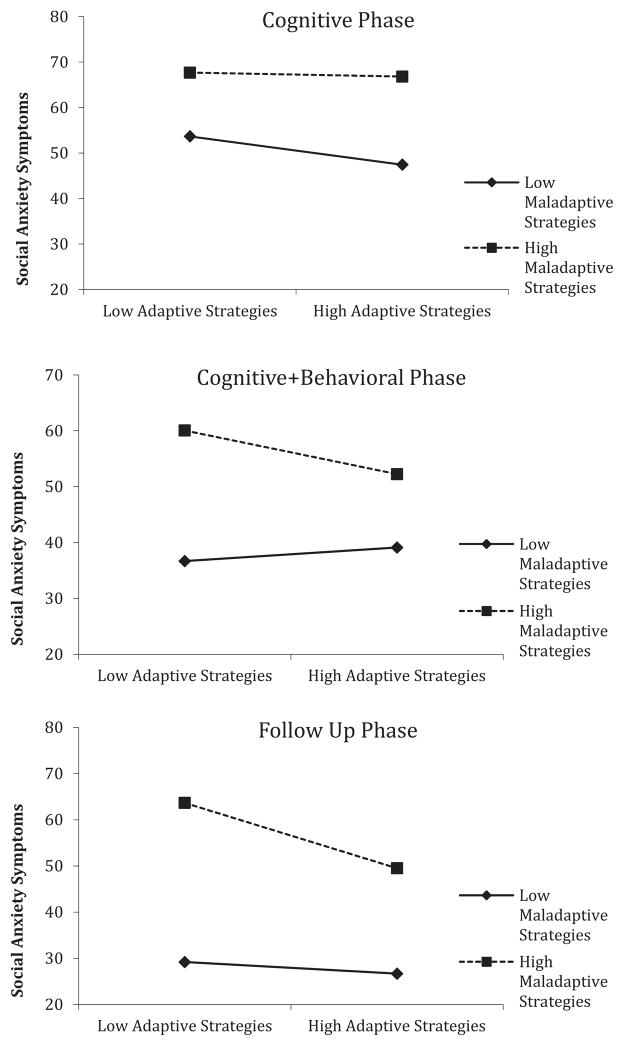
Importantly, the interaction between the weekly use of adaptive engagement and maladaptive avoidance strategies was significant, Wald’s χ2 = 4.90, p < .03, b = .004, SE (.002), CI (.001; .008). We probed this interaction with simple slope analyses. Results revealed that, on weeks when participants used maladaptive avoidance strategies with low frequency (1 SD below the mean), adaptive engagement strategies were associated with lower weekly social anxiety symptoms, Wald’s χ2 = 5.37, p < .02, b = −.16, SE (.07), CI (−.30; −.03). Conversely, on weeks when participants utilized maladaptive avoidance strategies with greater frequency (1 SD above the mean), the use of adaptive engagement strategies was not associated with weekly social anxiety symptoms, Wald’s χ2 = .21, ns, b = −.03, SE (.05), CI (−.13; .08). See Fig. 1.
Fig. 1.
Predicting social anxiety symptoms with adaptive and maladaptive strategies in each phase.
3.2.2. Cognitive + behavioral exposures phase
We predicted weekly social anxiety symptoms with the weekly use of maladaptive avoidance and adaptive engagement strategies and their interaction (N = 60 participants; n = 436 observations). The weekly use of maladaptive avoidance strategies was positively associated with weekly social anxiety symptoms, Wald’s χ2 = 58.39, p < .001, b = .54, SE (.07), CI (.40; .68), but the use of adaptive engagement strategies was not associated with weekly social anxiety symptoms, Wald’s χ2 = .92, ns, b = −.08, SE (.09), CI (−.25; .09). Given that the confidence intervals for maladaptive avoidance (.40; .68) and reversed adaptive engagement strategies (−.09; .25) did not overlap, we can conclude that the coefficients significantly differed from each other.
Importantly, the interaction between the use of maladaptive avoidance and adaptive strategies was significant, Wald’s χ2 = 7.71, p < .005, b = −.009, SE (.003), CI (−.015; −.003). We probed this interaction with simple slope analyses. Results reveal that, on weeks when participants used maladaptive avoidance strategies with low frequency (1 SD below the mean), adaptive engagement strategies were not associated with weekly social anxiety symptoms, Wald’s χ2 = .43, ns, b = .07, SE (.11), CI (−.14; .28). Conversely, on weeks when participants utilized maladaptive avoidance strategies with greater frequency (1 SD above the mean), the use of adaptive engagement strategies had the expected negative association with weekly social anxiety symptoms, Wald’s χ2 = 5.89, p < .02, b = −.24, SE (.10), CI (−.43; −.05). See Fig. 1.
3.2.3. Follow-up phase
We predicted weekly social anxiety symptoms with the weekly (i.e., past week at months 3, 6, 9, and 12) use of maladaptive avoidance and adaptive engagement strategies and their interaction (N = 51 participants; n = 175 observations). The weekly use of maladaptive avoidance strategies was positively associated with weekly social anxiety symptoms, Wald’s χ2 = 84.50, p < .001, b = .72, SE (.08), CI (.57; .88) and the use of adaptive engagement strategies was associated with lower weekly social anxiety symptoms, Wald’s χ2 = 8.12, p < .004, b = −.20, SE (.07), CI (−.34; −.06). Given that the confidence intervals for maladaptive avoidance (.57; .88) and reversed adaptive engagement strategies (.06; .34) did not overlap, we can conclude that the coefficients significantly differed from each other.
Importantly, the interaction between the use of maladaptive avoidance and adaptive strategies was significant, Wald’s χ2 = 5.78, p < .02, b = −.007, SE (.003), CI (−.013; −.001). We probed this interaction with simple slope analyses. Results reveal that, on weeks when participants used maladaptive avoidance strategies with low frequency (1 SD below the mean), adaptive engagement strategies were not associated with weekly social anxiety symptoms, Wald’s χ2 = .34, ns, b = −.05, SE (.09), CI (−.24; .13). Conversely, on weeks when participants utilized maladaptive avoidance strategies with greater frequency (1 SD above the mean), the use of adaptive engagement strategies had the expected negative association with weekly social anxiety symptoms, Wald’s χ2 = 13.49, p < .001, b = −.35, SE (.10), CI (−.54; −.16). See Fig. 1.5
4. Discussion
In this study, we sought to expand upon the growing literature on emotion regulation deficits in SAD by adopting a contextual framework emphasizing the examination of interactions among strategies in the repertoire (e.g., Aldao & Nolen-Hoeksema, 2012). First, we found support for the presence of an asymmetry in the relationship between social anxiety symptoms and the use of adaptive engagement/maladaptive avoidance strategies, whereby the use of adaptive engagement strategies had a weaker association with symptoms than did the use of maladaptive avoidance strategies (Aldao et al., 2010). Second, this asymmetry was qualified by an interaction between the use of adaptive engagement and maladaptive avoidance strategies (Aldao & Nolen-Hoeksema, 2012). Interestingly, the direction of this interaction varied as a function of treatment study phase (i.e., cognitive, cognitive + behavioral exposures, follow-up).
4.1. Implications for emotion regulation and psychopathology
This study extends the literature on emotion regulation and SAD in two important ways. First, it suggests that the interaction between adaptive engagement and maladaptive avoidance strategies found in an unselected community sample (i.e., adaptive engagement strategies had a negative association with symptoms only when participants endorsed high levels of maladaptive avoidance strategies; Aldao & Nolen-Hoeksema, 2012) might also describe patterns of affective functioning in adults diagnosed with this condition. Second, because participants were asked to complete 21 weekly assessments, we were able to obtain a more nuanced understanding of the temporal patterns of associations between strategies and symptoms relative to earlier work (e.g., Aldao & Nolen-Hoeksema, 2012; Aldao et al., 2010). To our knowledge, this is the first published report examining weekly changes in the use of emotion regulation strategies in a sample of participants seeking treatment for generalized SAD (e.g., Moscovitch et al., 2012 assessed regulation strategies at pre, mid, and post-treatment). The value of such an approach is particularly illustrated by the interactions we found between treatment study phase and the experience of social anxiety symptoms as well as the use of regulation strategies (see Gloster et al., 2013 for looking at treatment study phase within the context of CBT for panic disorder). In this respect, we found that both, social anxiety symptoms and the use of maladaptive avoidance strategies decreased during the cognitive and cognitive + behavioral exposures phases, but they reached a plateau during the follow-up phase. We observed a similar pattern for the increases in the use of adaptive engagement strategies.
We also found that the interaction between the use of maladaptive avoidance and adaptive engagement strategies took a different shape in the cognitive phase than in the cognitive + behavioral exposures and follow-up phases. Whereas in the cognitive phase, the use of adaptive engagement strategies had negative associations with social anxiety symptoms when the use of maladaptive avoidance strategies was low, in the cognitive + behavioral exposures and follow-up phases, their use had negative associations with symptoms when the use of maladaptive avoidance strategies was high. Interestingly, this second pattern of interactions (i.e., when patients were less symptomatic) is akin to the one found by Aldao and Nolen-Hoeksema (2012) in a community sample of relatively healthy participants. This further underscores the importance of expanding upon the extant literature on the trait use of emotion regulation strategies by examining the use of strategies at the state level in order to better understand patterns of emotion dysregulation in mental disorders.
One possible interpretation for this modulation of the interaction between strategies by treatment study phase hinges on changes in the mean levels of strategies and social anxiety in each phase. As the reader might recall, we broke down interactions by examining what happened at 1 standard deviation above and below the mean of maladaptive avoidance strategies. Thus, the interpretation of high versus low use of maladaptive avoidance strategies as a moderator ought to incorporate the mean value for these strategies.
In the cognitive phase, the use of maladaptive avoidance strategies was higher than the use of adaptive engagement strategies. Over the course of sessions (in the cognitive and cognitive + behavioral exposures phases), the use of maladaptive avoidance strategies declined and that of adaptive engagement strategies increased (see Table 2). If the use of adaptive engagement strategies had a significant association with symptoms when (1) the elevated maladaptive avoidance strategies were 1 standard deviation below the mean, and (2) the reduced maladaptive avoidance strategies were 1 standard deviation above the mean, this suggests that the optimal effects of adaptive engagement strategies might be seen when their use is relatively similar to that of maladaptive avoidance strategies. In other words, when participants are using relatively equal levels of strategies, adaptive engagement strategies might exert their most beneficial effects. This might reflect that participants are “shopping around” for strategies, until they find the one that works best. Such an interpretation is in line with current work underscoring the importance of regulating one’s emotions with flexibility (e.g., Bonanno & Burton, 2013; Kashdan & Rottenberg, 2010). In this respect, it will be essential for future investigations to utilize laboratory-based and experience sampling paradigms that will allow researchers to test such causal associations. In addition, it will be useful to examine the order with which people try to implement strategies in response to a given situation. More broadly, these findings speak to the importance of systematically assessing contextual factors when seeking to understand the role that emotion regulation strategies play in mental health and well-being (Aldao, 2013; Troy, Shallcross, & Mauss, 2013).
The findings from this investigation highlight the value of conducting weekly assessments of the use of strategies over the course of several weeks. These weekly assessments are quite prevalent in the treatment outcome literature, given that patients usually meet with their therapist on a weekly basis and provide reports of the past week (e.g., Fentz et al., 2013; Kazdin, 2007). Yet, their administration in basic research has been virtually non-existent. Rather, most of the longitudinal work on emotion regulation tends to assess the use of strategies a few times over a long period of time (e.g., prospective studies, 2–3 times over the course of a year or two, e.g., Aldao & Nolen-Hoeksema, 2012) or multiple times over the course of a few weeks (e.g., ecological momentary assessment (EMA) studies, 4 times/day over the course of 2 weeks; Kashdan & Collins, 2010). As this investigation suggests, capturing regulation patterns on a weekly basis might be particularly useful for developing a nuanced understanding of how people regulate their emotions in everyday life and consequently, for tailoring psychosocial interventions in order to target person-specific patterns of emotion dysfunction. In this respect, we consider that it will be of utmost importance for future work to empirically determine which units of time might be most optimal for reliably capturing meaningful patterns of variation in the process of emotion regulation.
4.2. Limitations and future directions
Although the utilization of an existing sample of treatment-seeking participants provided us with the opportunity to answer important questions about emotion regulation strategies and symptoms over time, it also resulted in certain constraints. For example, because participants completed assessments at the beginning of each therapy session for a period of 16 weeks (four months), such assessments needed to be relatively short. Consequently, participants reported on their use of a limited subset of emotion regulation strategies (i.e., avoidance-based maladaptive strategies). It will be important for future investigations to conduct more comprehensive assessments of the broader repertoire of emotion regulation strategies (e.g., Aldao & Dixon-Gordon, 2014). In addition, it will be critical to test interactions among individual strategies. Such an approach might result, for example, in a more precise understanding of the complex relationship between the strategies of acceptance and reappraisal (see Hofmann, 2010; McRae et al., 2012; Werner & Gross, 2010).
In addition, participants completed single-item measures of strategies, which can be problematic because such measures might not capture the complexity of psychological processes. This is particularly noteworthy in light of growing evidence suggesting that a given emotion regulation strategy can be implemented in more than one way (e.g., McRae et al., 2012). Given that completing existing questionnaires for each strategy would be quite time consuming, we consider that it will be essential for the continuous growth of the translational work on emotion regulation that investigators conduct psychometric work to develop shorter versions of existing measures (e.g., Berle et al., 2011 recently developed a 3-item measure of the Penn State Worry Questionnaire).
Another important consideration for future work is that participants in this study received one form of therapy, namely individual CBT for generalized SAD (Hope et al., 2006). In the past decade, there has been a growing enthusiasm for developing emotion-focused interventions that explicitly target different aspects of emotion dysregulation to varying degrees (e.g., Barlow, Allen, & Choate, 2004; Hayes, Strosahl, & Wilson, 1999; Linehan, 1993; Mennin & Fresco, 2014; Roemer, Orsillo, & Salters-Pedneault, 2008; Segal, Williams, & Teasdale, 2002). Thus, it will be essential for future investigations to examine changes in the use of regulation strategies (and their relationship to symptoms) in the context of different emotion-focused psychosocial interventions. A final limitation stems from the fact that during the follow-up phase, we collected data from 51 out of the original 71 participants. Thus, it is possible that we might have observed different patterns in changes in symptoms and strategies (and their relationships) if we had been able to assess the full sample of participants. In all, these limitations highlight the many exciting opportunities for future work in this area.
Overall, this study constitutes an important initial step in our understanding the dynamic changes that the repertoire of emotion regulation strategies that take place when people suffering from social anxiety undergo CBT treatment. We hope that this work motivates additional research to systematically examine the processes by which individuals suffering from psychopathology can learn to modify their patterns of emotion regulation over time.
Acknowledgments
Funding
This research was supported by a National Institute of Mental Health Grant R01 MH076074 awarded to James J. Gross.
Footnotes
We have re-run this factor analysis for each of the 21 measurement points and we have found converging evidence of a unitary factor. The only exception out of the 21 sessions was session 7, for which there were 2 factors. Factor 1 consisted of situational avoidance, behavioral avoidance, and mental avoidance (loadings > .76). It had an eigenvalue of 1.89 and it accounted for 47% of the variance. Factor 2 consisted of expressive suppression (loading = .96). It an eigenvalue of 1.02 and it accounted for 25% of the variance. Of note, an eigenvalue of 1.02 is barely above Kaiser criterion of 1 (Tabachnick & Fidell, 2012). Thus, we can be quite confident that these 4 items reflect an unitary construct. We have included a mention of this in the revised manuscript[0].
We have re-run our main analyses predicting weekly social anxiety symptoms with the weekly use of regulation strategies and completer status and have found a non-significant main effect of completer status as well as non-significant of interactions between completer status and the strategies (all p’s > .34.
Authorship note
A. A., H. J., and J.G. developed the study concept. H. J., P. G., and J. G. contributed to the study design and data collection. A. A. conducted data analysis. All four authors wrote the manuscript and approved the final version for submission.
Contributor Information
Amelia Aldao, Email: amealdao@gmail.com, aldao.1@osu.edu.
Hooria Jazaieri, Email: hooria@berkeley.edu.
Philippe R. Goldin, Email: pgoldin@stanford.edu.
James J. Gross, Email: gross@stanford.edu.
References
- Aiken LS, West SG. Multiple regression: testing and interpreting interactions. Newbury Park. London: Sage; 1991. [Google Scholar]
- Aldao A. The future of emotion regulation research: capturing context. Perspectives on Psychological Science. 2013;8:155–172. doi: 10.1177/1745691612459518. http://dx.doi.org/10.1177/1745691612459518. [DOI] [PubMed] [Google Scholar]
- Aldao A, Dixon-Gordon K. Broadening the scope of research on emotion regulation strategies and psychopathology. Cognitive Behaviour Therapy. 2014 doi: 10.1080/16506073.2013.816769. http://dx.doi.org/10.1080/16506073.2013.816769 (in press) [DOI] [PubMed]
- Aldao A, Mennin DS. Paradoxical cardiovascular effects of implementing adaptive emotion regulation strategies in generalized anxiety disorder. Behaviour Research & Therapy. 2012;50:122–130. doi: 10.1016/j.brat.2011.12.004. http://dx.doi.org/10.1016/j.brat.2011.12.004. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S. When are adaptive strategies most predictive of psychopathology? Journal of Abnormal Psychology. 2012;121:276–281. doi: 10.1037/a0023598. http://dx.doi.org/10.1037/a0023598. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. http://dx.doi.org/10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. http://dx.doi.org/10.1016/s0005-7894(04)80036-4. [DOI] [PubMed] [Google Scholar]
- Barrett LF, Gross J, Christensen TC, Benvenuto M. Knowing what you’re feeling and knowing what to do about it: mapping the relation between emotion differentiation and emotion regulation. Cognition & Emotion. 2001;15:713–724. http://dx.doi.org/10.1080/02699930143000239. [Google Scholar]
- Berle D, Starcevic V, Moses K, Hannan A, Milicevic D, Sammut P. Preliminary validation of an ultra-brief version of the Penn State Worry Questionnaire. Clinical Psychology & Psychotherapy. 2011;18:339–346. doi: 10.1002/cpp.724. http://dx.doi.org/10.1002/cpp.724. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Burton CL. Regulatory flexibility: an individual differences perspective on coping and emotion regulation. Perspectives on Psychological Science. 2013;8:591–612. doi: 10.1177/1745691613504116. http://dx.doi.org/10.1177/1745691613504116. [DOI] [PubMed] [Google Scholar]
- Brozovich F, Heimberg RG. An analysis of post-event processing in social anxiety disorder. Clinical Psychology Review. 2008;28:891–903. doi: 10.1016/j.cpr.2008.01.002. http://dx.doi.org/10.1016/j.cpr.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Bylsma LM, Rottenberg J. Uncovering the dynamics of emotion regulation and dysfunction in daily life with ecological momentary assessment. In: Nyklicek I, Vingerhoets AJJM, Zeelenberg M, editors. Emotion regulation and well-being. New York: Springer; 2011. pp. 225–244. [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety disorders interview schedule for DSM-IV (ADIS-IV) New York: Graywind; 1994. [Google Scholar]
- D’Avanzato C, Joormann J, Siemer M, Gotlib IH. Emotion regulation in depression and anxiety: examining diagnostic specificity and stability of strategy use. Cognitive Therapy and Research. 2013;37:968–980. http://dx.doi.org/10.1007/s10608-013-9537-0. [Google Scholar]
- Ebner-Priemer UW, Trull TJ. Ecological momentary assessment of mood disorders and mood dysregulation. Psychological Assessment. 2009;21:463–475. doi: 10.1037/a0017075. http://dx.doi.org/10.1037/a0017075. [DOI] [PubMed] [Google Scholar]
- Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403. http://dx.doi.org/10.1093/biomet/58.3.403. [PubMed] [Google Scholar]
- Farb NA, Anderson AK, Irving JA, Segal ZV. Mindfulness interventions and emotion regulation. In: Gross JJ, editor. Handbook of emotion regulation. Guilford Press; New York: 2014. [Google Scholar]
- Fentz HN, Hoffart A, Jensen MB, Arendt M, O’Toole M, Rosenberg NK, Hougaard E. Mechanisms of change in cognitive behaviour therapy for panic disorder: the role of panic self-efficacy and catastrophic misinterpretations. Behaviour Research and Therapy. 2013;51:579–589. doi: 10.1016/j.brat.2013.06.002. http://dx.doi.org/10.1016/j.brat.2013.06.002. [DOI] [PubMed] [Google Scholar]
- Ghisletta P, Spini D. An introduction to generalized estimating equations and an application to assess selectivity effects in a longitudinal study on very old individuals. Journal of Educational and Behavioral Statistics. 2004;2:9. http://dx.doi.org/10.3102/1076998602900442. [Google Scholar]
- Gloster AT, Klotsche J, Gerlach AL, Hamm A, Ströhle A, Gauggel S, Wittchen H. Timing matters: change depends on the stage of treatment in cognitive behavioral therapy for panic disorder with agoraphobia. Journal of Consulting and Clinical Psychology. 2013 doi: 10.1037/a0034555. http://dx.doi.org/10.1037/a0034555 [E-pub ahead of print] [DOI] [PubMed]
- Goldin PR, Lee IA, Ziv M, Jazaieri H, Heimberg RG, Gross JJ. Trajectories of change in emotion regulation and social anxiety during cognitive-behavioral therapy for social anxiety disorder. Behaviour Research and Therapy. 2014 doi: 10.1016/j.brat.2014.02.005. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Ziv M, Jazaieri H, Werner K, Kraemer H, Heimberg RG, Gross JJ. Cognitive reappraisal self-efficacy mediates the effects of individual cognitive-behavioral therapy for social anxiety disorder. Journal of Consulting and Clinical Psychology. 2012;80:1034–1040. doi: 10.1037/a0028555. http://dx.doi.org/10.1037/a0028555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ, Jazaieri H. Emotion regulation and psychopathology: an affective science perspective. Clinical Psychological Science. 2014 (in press) [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well being. Journal of Personality and Social Psychology. 2003;85:248–362. doi: 10.1037/0022-3514.85.2.348. http://dx.doi.org/10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Hayes SC. Climbing our hills: a beginning conversation on the comparison of acceptance and commitment therapy and traditional cognitive behavioral therapy. Clinical Psychology: Science & Practice. 2008;15:286–295. http://dx.doi.org/10.1111/j.1468-2850.2008.00139.x. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson K. Acceptance and commitment therapy: an experiential approach to behavior change. New York: The Guilford Press; 1999. [Google Scholar]
- Hofmann SG. Acceptance and commitment therapy: new wave or Morita therapy? Clinical Psychology: Science & Practice. 2008;15:280–285. http://dx.doi.org/10.1111/j.1468-2850.2008.00139.x. [Google Scholar]
- Hofmann SG. Advances in the research of social anxiety and its disorder (Special section) Anxiety, Stress, & Coping. 2010;23:239–242. doi: 10.1080/10615801003612014. http://dx.doi.org/10.1080/10615801003612014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Asmundson GJG. Acceptance and mindfulness-based therapy: new wave or old hat? Clinical Psychology Review. 2008;28:1–16. doi: 10.1016/j.cpr.2007.09.003. http://dx.doi.org/10.1016/j.cpr.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Heering S, Sawyer AT, Asnaani A. How to handle anxiety: the effects of reappraisal, acceptance, and suppression strategies on anxious arousal. Behaviour Research & Therapy. 2009;47:389–394. doi: 10.1016/j.brat.2009.02.010. http://dx.doi.org/10.1016/j.brat.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A, Asnaani A. Emotion dysregulation model of mood and anxiety disorders. Depression & Anxiety. 2012;29:409–416. doi: 10.1002/da.21888. http://dx.doi.org/10.1002/da.21888. [DOI] [PubMed] [Google Scholar]
- Hope DA, Heimberg RG, Juster HR, Turk CL. Managing social anxiety: a cognitive-behavioral approach. San Antonio. TX: The Psychological Corp; 2000. [Google Scholar]
- Hope DA, Heimberg RG, Turk CL. Therapist guide for managing social anxiety: a cognitive-behavioral therapy approach. New York: Oxford University Press; 2006. [Google Scholar]
- Kashdan TB, Breen WE. Social anxiety and positive emotions: a prospective examination of a self-regulatory model with tendencies to suppress or express emotions as a moderating variable. Behavior Therapy. 2008;39:1–12. doi: 10.1016/j.beth.2007.02.003. http://dx.doi.org/10.1016/j.beth.2007.02.003. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Collins RL. Social anxiety and the experience of positive emotion and anger in everyday life: an ecological momentary assessment approach. Anxiety Stress Coping. 2010;23:259–272. doi: 10.1080/10615800802641950. http://dx.doi.org/10.1080/10615800802641950. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Farmer AS, Adams LM, Ferssizidis P, McKnight PE, Nezlek JB. Distinguishing healthy adults from people with social anxiety disorder: evidence for the value of experiential avoidance and positive emotions in everyday social interactions. Journal of Abnormal Psychology. 2013;122:645–655. doi: 10.1037/a0032733. http://dx.doi.org/10.1037/a0032733. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Goodman FR, Machell KA, Kleiman EM, Monfort SS, Ciarrochi J, Nezlek JB. A contextual approach to experiential avoidance and social anxiety: evidence from an experimental interaction and daily interactions of people with social anxiety disorder. Emotion. 2014 doi: 10.1037/a0035935. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, Roberts JE. Social anxiety, depressive symptoms, and post-event rumination: Affective consequences and social contextual influences. Journal of Anxiety Disorders. 2007;21:285–301. doi: 10.1016/j.janxdis.2006.05.009. http://dx.doi.org/10.1016/j.janxdis.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30:865–878. doi: 10.1016/j.cpr.2010.03.001. http://dx.doi.org/10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, Steger MF. Expanding the topography of social anxiety: an experience-sampling assessment of positive emotions, positive events, and emotion suppression. Psychological Science. 2006;17:120–128. doi: 10.1111/j.1467-9280.2006.01674.x. http://dx.doi.org/10.1111/j.1467-9280.2006.01674.x. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. http://dx.doi.org/10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kring AM, Sloan DS. Emotion regulation and psychopathology. New York. NY: Guilford Press; 2009. [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. http://dx.doi.org/10.2307/2336267. [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford; 1993. [Google Scholar]
- McLean CP, Miller NA, Hope DA. Mediating social anxiety and disordered eating: the role of expressive suppression. Eating Disorders. 2007;15:41–54. doi: 10.1080/10640260601044485. http://dx.doi.org/10.1080/10640260601044485. [DOI] [PubMed] [Google Scholar]
- McRae K, Ciesielski B, Gross JJ. Unpacking cognitive reappraisal: goals, tactics, and outcomes. Emotion. 2012;12:250–253. doi: 10.1037/a0026351. http://dx.doi.org/10.1037/a0026351. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM. Emotion regulation therapy. In: Gross JJ, editor. Handbook of emotion regulation. New York: Guildford Press; 2014. (in press) [Google Scholar]
- Moscovitch DA, Gavric DL, Senn JM, Santesso DL, Miskovic V, Schmidt LA, Antony MM. Changes in judgment biases and use of emotion regulation strategies during cognitive-behavioral therapy for social anxiety disorder: distinguishing treatment responders from nonresponders. Cognitive Therapy and Research. 2012;36:261–271. http://dx.doi.org/10.1007/s10608-011-9371-1. [Google Scholar]
- Moscovitch DA, Suvak MK, Hofmann SG. Emotional response patterns during social threat in individuals with generalized social anxiety disorder and non-anxious controls. Journal of Anxiety Disorders. 2010;24:785–791. doi: 10.1016/j.janxdis.2010.05.013. http://dx.doi.org/10.1016/j.janxdis.2010.05.013. [DOI] [PubMed] [Google Scholar]
- Oldfield RC. The assessment and analysis of handedness: the Edin-burgh inventory. Neuropsychologia. 1971;9:97–113. doi: 10.1016/0028-3932(71)90067-4. http://dx.doi.org/10.1016/0028-3932(71)90067-4. [DOI] [PubMed] [Google Scholar]
- Perini SJ, Abbott MJ, Rapee RM. Perception of performance as a mediator in the relationship between social anxiety and negative post-event rumination. Cognitive Therapy & Research. 2006;30:645–659. http://dx.doi.org/10.1007/s10608-006-9023-z. [Google Scholar]
- Robins RW, Hendin HM, Trzesniewski KH. Measuring global self-esteem: construct validation of a single-item measure and the rosenberg self-esteem scale. Personality and Social Psychology Bulletin. 2001;27:151–161. http://dx.doi.org/10.1177/0146167201272002. [Google Scholar]
- Robinson MD, Clore GL. Episodic and semantic knowledge in emotional self-report. Evidence for Two Judgment Processes. 2002;83:198–215. http://dx.doi.org/10.1037/0022-3514.83.1.198. [PubMed] [Google Scholar]
- Roemer L, Orsillo SM, Salters-Pedneault K. Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: evaluation in a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2008;76:1083–1089. doi: 10.1037/a0012720. http://dx.doi.org/10.1037/a0012720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santanello AW, Gardner FL. The role of experiential avoidance in the relationship between maladaptive perfectionism and worry. Cognitive Therapy & Research. 2007;30:319–332. doi: 10.1007/s10608-006-9000-6. [DOI] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale J. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press; 2002. [Google Scholar]
- Sheppes G, Scheibe S, Suri G, Radu P, Blecert J, Gross JJ. Emotion regulation choice: a conceptual framework and supporting evidence. Journal of Experimental Psychology: General. 2014;143:163–181. doi: 10.1037/a0030831. http://dx.doi.org/10.1037/a0030831. [DOI] [PubMed] [Google Scholar]
- Srivastava S, Tamir M, McGonigal KM, John OP, Gross JJ. The social costs of emotional suppression: a prospective study of the transition to college. Journal of Personality and Social Psychology. 2009;96:883–897. doi: 10.1037/a0014755. http://dx.doi.org/10.1037/a0014755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szasz PL, Szentagotai A, Hofmann SG. The effect of emotion regulation strategies on anger. Behaviour Research & Therapy. 2011;49:114–119. doi: 10.1016/j.brat.2010.11.011. http://dx.doi.org/10.1016/j.brat.2010.11.011. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. Boston: Allyn & Bacon; 2006. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5. Boston: Allyn & Bacon; 2012. [Google Scholar]
- Turk CL, Heimberg RG, Luterek JA, Mennin DS, Fresco DM. Emotion dysregulation in generalized anxiety disorder: a comparison with social anxiety disorder. Cognitive Therapy & Research. 2005;29:89–106. http://dx.doi.org/10.1007/s10608-005-1651-1. [Google Scholar]
- Troy AS, Shallcross AJ, Mauss IB. A person-by-situation approach to emotion regulation cognitive reappraisal can either help or hurt, depending on the context. Psychological Science. 2013 doi: 10.1177/0956797613496434. http://dx.doi.org/10.1177/0956797613496434 [E-pub ahead of print] [DOI] [PubMed]
- Webb TL, Miles E, Sheeran P. Dealing with feeling: a meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychological Bulletin. 2012;138:775–808. doi: 10.1037/a0027600. http://dx.doi.org/10.1037/a0027600. [DOI] [PubMed] [Google Scholar]
- Werner K, Gross JJ. Emotion regulation and psychopathology: a conceptual framework. In: Kring AM, Sloan DM, editors. Emotion regulation in psychopathology. Guilford Press; New York: 2010. [Google Scholar]
- Wolgast M, Lundh LG, Viborg G. Cognitive reappraisal and acceptance: an experimental comparison of two emotion regulation strategies. Behaviour Research & Therapy. 2011;49:858–866. doi: 10.1016/j.brat.2011.09.011. http://dx.doi.org/10.1016/j.brat.2011.09.011. [DOI] [PubMed] [Google Scholar]