Abstract
Hypertension is the most common modifiable risk factor for cardiovascular disease, the leading cause of death in both men and women. The prevalence and severity of hypertension rise markedly with age, and blood pressure control becomes more difficult with aging in both genders, particularly in women. In addition, there are forms of hypertension that occur exclusively in women, e.g., hypertension related to menopause, oral contraceptive use, or pregnancy (e.g., chronic hypertension, gestational hypertension, pre-eclampsia or eclampsia). Randomized controlled trials show that antihypertensive therapy provides similar reductions in major cardiovascular events in men and women. Therefore, gender should not influence decisions on selection of blood pressure lowering therapies, except for consideration of gender-specific side effects or contraindications for use in women who are or may become pregnant. This article reviews the prevalence, awareness, treatment, and control of hypertension in women, as well as recent guidelines for management of hypertension in women.
Keywords: antihypertensive treatment, hypertension, oral contraceptives, preeclampsia, pregnancy-related hypertension, women
INTRODUCTION
The most recent data from the American Heart Association (AHA) show that 33% (78 million people) of US adults older than 20 years of age have hypertension, with nearly equal prevalence in men and women.1 Hypertension is more common in men than women among those younger than 45 years of age, but the situation is reversed in those 65 years and older. With the aging of the population, hypertension will become more common in women than in men in the near future.
Hypertension is a major risk factor for cardiovascular disease (CVD), and an elevated blood pressure (BP)>140/90 mm Hg has been demonstrated in approximately 69% of people who have a first heart attack, 77% of those who have a first stroke, and 74% of those who have heart failure.1 CVD is the leading cause of death among women in the US, and the adjusted population attributable fraction for CVD mortality for elevated BP is 41%, by far higher than other risk factors (e.g., 14% for smoking, 13% for poor diet quality, 12% for insufficient physical activity, and 9% for abnormal glucose levels).1 Life expectancy is approximately 5 years shorter for hypertensive women compared with normotensive women at 50 years of age. Post-menopausal women have the greatest population burden of sudden cardiac death, which accounts for 13% of all deaths and one-half of all coronary deaths. A report from the Women's Health Initiative (WHI) that included data from >160,000 postmenopausal women identified hypertension as a major independent risk factor for sudden cardiac death in this population.2
AWARENESS AND CONTROL
Appreciation of the importance of hypertension and associated CVD in women has led to multiple campaigns over the last decade to educate women about their risk. This effort appears to be paying off. Between 1997 and 2012, the rate of awareness of CVD as the leading cause of death among women in the US nearly doubled (56% vs. 30% P<0.001).3 Although awareness increased across all racial/ethnic subgroups, gaps persist between minorities compared with white women such that the level of awareness in black and Hispanic women in 2012 is similar to that of white women in 1997. This is consistent with recent data from AHA showing that 76% of Mexican American, 84% of non-Hispanic white, and 89% of non-Hispanic black women with hypertension are aware of their condition.1 Although hypertension control rates have improved over the years, only 42% of Mexican American, 54% of non-Hispanic white, and 53% of non-Hispanic black women with documented hypertension have their BP controlled to target levels.
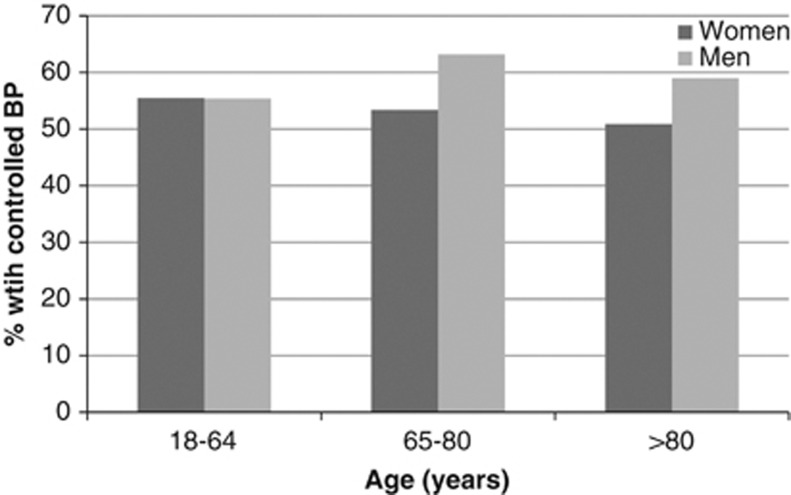
A US national survey of nonfederal ambulatory clinics and hospital outpatient clinics also revealed gender disparities in BP control and CVD care.4 In a cross-sectional analysis of >12,000 patient visits with primary care providers, women were less likely than men to have controlled hypertension (54.0% vs. 58.7% P<0.02, Figure 1). After adjustment for multiple covariates including insurance, race, and comorbidities, this gender disparity persisted for patients who were 65–80 years old (odds ratio for BP control for women vs. men 0.62 (95% CI 0.45–0.85)). There was no statistically significant difference in the number of antihypertensive medications used by gender, but women received an ACEI less frequently (20.9% vs. 28.7% P<0.001) and received diuretics more frequently (20.9% vs. 16.9% P=0.05) than men. These gender differences may be related to a lack of awareness among health care providers that women with hypertension are at increased CVD risk and need aggressive BP-lowering therapy, and to underestimation of CVD risk in women, leading to significant prescribing gaps. This finding is consistent with data from the Framingham Heart Study that showed a more pronounced age-related decline in BP control in women than in men.5 It remains unclear whether this age-related decrease in hypertension control in women is related to the inadequate intensity of BP treatment, non-adherence by patients, true treatment resistance, or other factors.
Figure 1.
Blood pressure control rates as a function of age and gender (data from Keyhani et al.4).
FORMS OF HYPERTENSION THAT OCCUR EXCLUSIVELY IN WOMEN
Post-menopausal hypertension
BP rises after menopause in most women, and it has been postulated that withdrawal of endogenous estrogen, a potent vasodilator, plays a key role in postmenopausal hypertension.6 Observational studies have shown that menopause is associated with an age-independent 4–5 mm Hg increase in systolic BP that may be related to increased salt sensitivity, decreased endothelial nitric oxide production, and upregulation of the angiotensin II subtype 1 (AT1) receptor. Estrogen appears to protect against salt-induced increases in BP, at least in part by increasing the sensitivity of the pressure–natriuresis relationship and augmenting renal excretion of sodium.
OCP-induced hypertension
Combined estrogen and progestin oral contraceptive pills (OCPs) are associated with small but significant increases in BP and risk of CV events, particularly stroke, in the general population of women. The etiology of the OCP-induced BP increase is likely related to a combination of increased arterial stiffness, renin–angiotensin system stimulation, and salt and water retention. While current users of OCPs have a significantly increased risk for hypertension compared with never-users, the absolute risk is small and decreases quickly with cessation of OCPs.7 The risk of developing OCP-induced hypertension increases significantly with age, cigarette smoking, duration of OCP use, and obesity. Guidelines suggest that contraceptive prescriptions be limited to 6 months to ensure regular monitoring of BP throughout contraceptive therapy, since OCPs can rarely precipitate severe or accelerated hypertension.8
Pregnancy-related hypertension
Hypertensive disorders in pregnancy include chronic hypertension, gestational hypertension, pre-eclampsia, and eclampsia. All of these have been associated with maternal, fetal, and neonatal morbidity and mortality. During pregnancy, the primary goal of treating chronic hypertension is to reduce maternal risk since there is no evidence that BP treatment improves perinatal outcomes, but the choice of antihypertensive agent should be largely driven by the safety of the fetus. Lifestyle modifications, particularly exercise and weight reduction, are first-line treatment for pregnancy-related hypertension, particularly when mild. The recent European Society of Hypertension/European Society of Cardiology guidelines for the management of arterial hypertension recommend drug treatment of severe hypertension in pregnancy (>160/110 mm Hg, Class I; Level of Evidence C) and consideration of drug treatment in pregnant women with persistent elevation of BP ⩾150/95 mm Hg and in those with BP ⩾140/90 in the presence of gestational hypertension (with or without pre-existing hypertension), asymptomatic organ damage, or symptoms at any time during pregnancy (Class IIb; Level of Evidence C).9 These guidelines recommend the use of labetalol, methyldopa, or nifedipine in pregnancy and caution when beta-blockers or diuretics are used. When BP has to be lowered emergently, as in pre-eclampsia, the guidelines recommend intravenous labetalol as the drug of choice and nitroprusside or nitroglycerin as other options (Class IIa; Level of Evidence B).
RANDOMIZED CONTROLLED TRIALS OF BP LOWERING
Randomized controlled trials (RCTs) with CVD outcomes have provided the highest level of evidence that BP-lowering treatment is beneficial in hypertensive women, as well as men. A prospectively designed overview by the BP Lowering Treatment Trial Lists' Collaboration of 31 RCTs of antihypertensive treatment with CVD outcomes that included 87,349 women and 103,268 men tested whether there were important gender differences in the effects of different BP-lowering regimens.10 Separate overviews were carried out for trials comparing active agents with placebo, more intensive with less intensive regimens, and one active agent with another. In all cases, mean baseline BPs were slightly higher for women compared with men, but achieved BP reductions were comparable in both sexes. There was no difference in the effects of BP-lowering treatment regimens between women and men for any CVD outcome except stroke. There was some evidence, albeit of borderline (P=0.05) statistical significance, that women, but not men, derive greater benefit in stroke prevention from CCB-based regimens than ACEI-based regimens. In view of the large number (42) of subgroup analyses carried out in the study, the authors attributed this finding to chance. Overall, there was no evidence that women and men derive different outcome benefit from BP reduction or that different antihypertensive drug classes are more or less effective in women than in men. These observations led to the conclusion that a patient's gender should not influence decisions about the need for BP-lowering therapy, the magnitude of BP reduction to be sought, or the selection of drug classes.
Earlier overviews of aggregated data from RCTs that compared active treatment with placebo or less systematically treated controls and reported results by gender had concluded that the effects of BP-lowering treatment on morbidity and mortality did not differ between women and men.11 Absolute benefit of treatment did differ between genders for some outcomes (e.g., greater for coronary heart disease and mortality in men) but not others (e.g. stroke), but these gender differences in outcomes were entirely attributable to differences in underlying risk.
More recent outcome trials of BP treatment that reported results by gender have shown few differences between women and men in CVD endpoints. The placebo-controlled Systolic Hypertension in Europe (Syst-Eur) trial reported no interaction by gender for either stroke or cardiac outcomes in response to treatment with the CCB nitrendipine,12 and the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial13 reported no gender difference in the primary composite CVD outcome in the study as a whole, or between treatment arms (the CCB verapamil vs. beta-blocker or diuretic). A pre-specified subgroup analysis from the Valsartan Antihypertensive Long-term Use Evaluation (VALUE) trial found an excess of the primary composite CVD endpoint with treatment based on the ARB valsartan compared with the CCB amlodipine in women but not in men.14, 15 This outcome benefit, which was attributed to greater BP reduction with amlodipine, did not translate into greater overall cardiac protection with amlodipine-based versus valsartan-based treatment in women because it was counterbalanced by a significant reduction in heart failure in valsartan-treated men but not in women.
A post hoc analysis of the Losartan Intervention For Endpoint reduction in hypertension (LIFE) study evaluated the effects of treatment based on the ARB losartan versus the beta-blocker atenolol on the primary composite endpoint of CVD death, stroke, and myocardial infarction in 4963 women with hypertension and LVH based on ECG criteria.16 Fewer events occurred in women versus men overall, and women in the losartan arm had significant reductions in the primary endpoint, stroke, and new-onset diabetes versus the atenolol arm. These treatment effects occurred in the absence of major differences in BP control and were attributed to mechanisms other than BP lowering. There were no between-treatment differences for myocardial infarction, CVD mortality, or hospitalization for heart failure in women and no significant treatment by gender interactions for any endpoint studied, except hospitalization for angina, which was significantly more common among women in the losartan group.
In contrast, smaller studies that enrolled fewer participants found no apparent benefit of the renin–angiotensin–aldosterone system blockade in preventing CVD events in women.17, 18 The Australian National Blood Pressure-2 (ANBP-2) trial showed a lack of benefit of ACEI (enalapril)-based treatment compared with diuretic-based treatment in women, but not in men.17 Only 524 events were observed in women, suggesting that the apparent lack of benefit of ACEI treatment may reflect inadequate power to detect a beneficial effect of ACEIs in treatment of hypertensive women because of low event rates. The Study on Cognition and Prognosis in the Elderly (SCOPE) compared an ARB (candesartan) with other antihypertensive treatment in older, higher-risk hypertensive patients. A prespecified subgroup analysis by gender found no significant outcome benefit of ARB treatment in women and no treatment–gender interaction.18 Interpretation of this finding is limited by design issues and the small number of events (273) experienced by the women, which limited the statistical power of the subgroup analysis.
The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), the largest RCT of antihypertensive treatment ever conducted, tested whether an ACEI (lisinopril) or a CCB (amlodipine) is superior to a diuretic (chlorthalidone) in preventing CVD outcomes in 15,638 women and 17,719 men with hypertension and other CVD risk factors.19 A prespecified subgroup analysis of ALLHAT results by gender showed slightly greater reductions in BP and in stroke in women randomized to amlodipine compared to lisinopril.20 Rates of heart failure, stroke, and combined CVD were also higher among women in the lisinopril arm compared to the chlorthalidone arm, and rates of heart failure were higher in the amlodipine arm than the chlorthalidone arm. There were no significant treatment–gender interactions. ALLHAT differs from most other RCTs of BP lowering in that it included a much higher percentage of blacks (35%) and Hispanics (19%) and thus its results may be more generalizable to the US population. Since rates of major CVD outcomes were not lower in the amlodipine or lisinopril groups than in the chlorthalidone group, and since chlorthalidone treatment resulted in the lowest rate of HF, the ALLHAT investigators concluded that other classes of antihypertensive drugs are not superior to thiazide-type diuretics for the initial treatment of hypertension in women, as well as in men.
ADVERSE EFFECTS OF BP-LOWERING THERAPY
While the benefits of antihypertensive treatment in reducing CVD outcomes are generally similar in women and men, important gender differences in adverse effect profiles often drive treatment choices. ACEIs and ARBs should absolutely be avoided in women who are or may become pregnant because of the risk of fetal developmental abnormalities. This caveat also applies to mineralocorticoid receptor antagonists and direct renin inhibitors. Some antihypertensive drugs have gender-specific adverse profiles that are unfavorable for women. For example, in the Treatment Of Mild Hypertension Study (TOMHS), in which 902 women and men received treatment with a drug chosen at random from each class of antihypertensive agent then available, women reported twice as many adverse effects as men.21 Biochemical responses to drugs may be gender dependent: men are more likely to develop gout and women are more likely to develop hyponatremia or hypokalemia associated with diuretic therapy.22 Women develop cough related to ACEI therapy 3 times more often than men and are more likely to complain of CCB-related peripheral edema and minoxidil-induced hirsutism.23 Further, sexual dysfunction related to antihypertensive therapy may be a problem in women as well as in men. This effect is most often associated with centrally acting agents, beta-blockers, and thiazide diuretics, while ARB therapy may improve these symptoms.24
GUIDELINES FOR MANAGEMENT OF HYPERTENSION IN WOMEN
The AHA Effectiveness-Based Guidelines for the Prevention of CVD in Women pointed out that, with few exceptions, the overwhelming majority of recommendations to prevent CVD are similar for women and men (Table 1).25 However, there may be real gender differences in the relative and absolute potential benefits and risks of preventive interventions. The guidelines adopted an optimal BP of <120/80 mm Hg, which should be encouraged through lifestyle approaches such as weight control, increased physical activity, alcohol moderation, sodium restriction, and increased consumption of fruits, vegetables, and low-fat dairy products (Class I; Level of Evidence B). Similar to JNC7, the document encourages the use of thiazide diuretics as part of the drug regimen for most patients unless contraindicated or if there are compelling indications for other agents in specific vascular diseases. Thiazide and thiazide-like diuretics are particularly attractive for use in elderly women because of decreased risk of hip fracture. Initial treatment of high-risk women with acute coronary syndrome or myocardial infarction should be with beta-blockers and/or ACEI/ARBs, with addition of other drugs such as thiazides as needed to achieve goal BP (Class I; Level of Evidence A).
Table 1. Clinical recommendations for high blood pressure in women.
| • Encourage an optimal blood pressure of <120/80 mm Hg through lifestyle approaches |
| • Pharmacotherapy is indicated when blood pressure is ⩾140/90 mm Hg |
| • Women generally respond to antihypertensive drugs similarly to men but there are special considerations: |
| ACEIs, ARBs, direct renin inhibitors, and mineralocorticoid antagonists are contraindicated for women who are or intend to become pregnant |
| Diuretics useful in some elderly women at risk because of a decreased risk of hip fracture |
| However, women are more likely to develop diuretic-induced hyponatremia and hypokalemia |
| ACEI-induced cough is three times as common in women as in men |
| Women more likely to complain of CCB-related peripheral edema and minoxidil-induced hirsutism |
FGH has received grant support from the American Heart Association and a US Department Veterans Affairs Merit Award. SO has received research support from Duke University (Sponsor: AstraZeneca AB), Daiichi Sankyo, Medtronic, Merck & Co., National Institutes of Health/National Heart, Lung, and Blood Institute (NHLBI), Novartis AG, Takeda Global Research & Development, UAB Comprehensive Cardiovascular Center, and Vivus, and has served as PI or Co-PI for clinical trials with Duke University, Merck & Co., Novartis, and Takeda Global Research & Development. SO received honoraria in her capacity as Faculty Presenter for the American Society of Hypertension sponsored by Daiichi Sankyo, and served as advisor for Bayer, Daiichi Sankyo, Novartis, Pfizer, and Takeda. Publication costs for this article were supported by the Turkish Society of Hypertension and Renal Diseases, a nonprofit national organization in Turkey.
References
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2013 update: a report from the American heart association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertoia ML, Allison MA, Manson JE, et al. Risk factors for sudden cardiac death in post-menopausal women. J Am Coll Cardiol. 2012;60:2674–2682. doi: 10.1016/j.jacc.2012.09.031. [DOI] [PubMed] [Google Scholar]
- Mosca L, Hammond G, Mochari-Greenberger H, et al. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey Circulation 20131271254–1263., e1251–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyhani S, Scobie JV, Hebert PL, et al. Gender disparities in blood pressure control and cardiovascular care in a national sample of ambulatory care visits. Hypertension. 2008;51:1149–1155. doi: 10.1161/HYPERTENSIONAHA.107.107342. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–472. doi: 10.1001/jama.294.4.466. [DOI] [PubMed] [Google Scholar]
- Bowling M, Oparil S, Hage FG, et al. Sex hormones and vascular functionIn: Dubey RK (ed).Sex Hormones InTech: Rijeka, Croatia; 2012(ISBN: 978-953-307-856-4). [Google Scholar]
- Chasan-Taber L, Willett WC, Manson JE, et al. Prospective study of oral contraceptives and hypertension among women in the United States. Circulation. 1996;94:483–489. doi: 10.1161/01.cir.94.3.483. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- Turnbull F, Woodward M, Neal B, et al. Do men and women respond differently to blood pressure-lowering treatment? Results of prospectively designed overviews of randomized trials. Eur Heart J. 2008;29:2669–2680. doi: 10.1093/eurheartj/ehn427. [DOI] [PubMed] [Google Scholar]
- Gueyffier F, Boutitie F, Boissel JP, et al. Effect of antihypertensive drug treatment on cardiovascular outcomes in women and men. A meta-analysis of individual patient data from randomized, controlled trials. The INDANA Investigators. Ann Intern Med. 1997;126:761–767. doi: 10.7326/0003-4819-126-10-199705150-00002. [DOI] [PubMed] [Google Scholar]
- Staessen JA, Thijs L, Celis H, et al. Dihydropyridine calcium-channel blockers for antihypertensive treatment in older patients—evidence from the Systolic Hypertension in Europe Trial. S Afr Med J. 2001;91:1060–1068. [PubMed] [Google Scholar]
- Black HR, Elliott WJ, Grandits G, et al. Principal results of the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial. JAMA. 2003;289:2073–2082. doi: 10.1001/jama.289.16.2073. [DOI] [PubMed] [Google Scholar]
- Zanchetti A, Julius S, Kjeldsen S, et al. Outcomes in subgroups of hypertensive patients treated with regimens based on valsartan and amlodipine: an analysis of findings from the VALUE trial. J Hypertens. 2006;24:2163–2168. doi: 10.1097/01.hjh.0000249692.96488.46. [DOI] [PubMed] [Google Scholar]
- Julius S, Kjeldsen SE, Weber M, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet. 2004;363:2022–2031. doi: 10.1016/S0140-6736(04)16451-9. [DOI] [PubMed] [Google Scholar]
- Os I, Franco V, Kjeldsen SE, et al. Effects of losartan in women with hypertension and left ventricular hypertrophy: results from the losartan intervention for endpoint reduction in hypertension study. Hypertension. 2008;51:1103–1108. doi: 10.1161/HYPERTENSIONAHA.107.105296. [DOI] [PubMed] [Google Scholar]
- Wing LM, Reid CM, Ryan P, et al. A comparison of outcomes with angiotensin-converting—enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med. 2003;348:583–592. doi: 10.1056/NEJMoa021716. [DOI] [PubMed] [Google Scholar]
- Trenkwalder P, Elmfeldt D, Hofman A, et al. The Study on COgnition and Prognosis in the Elderly (SCOPE) - major CV events and stroke in subgroups of patients. Blood Press. 2005;14:31–37. doi: 10.1080/08037050510008823. [DOI] [PubMed] [Google Scholar]
- Officers A, Coordinators for the ACRGTA, Lipid-Lowering Treatment to Prevent Heart Attack T Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002;288:2981–2997. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]
- Oparil S, Davis BR, Cushman WC, et al. Mortality and morbidity during and after antihypertensive and lipid-lowering treatment to prevent heart attack trial: results by sex. Hypertension. 2013;61:977–986. doi: 10.1161/HYPERTENSIONAHA.111.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neaton JD, Grimm RH, Jr., Prineas RJ, et al. Treatment of Mild Hypertension Study. Final results. Treatment of Mild Hypertension Study Research Group. JAMA. 1993;270:713–724. [PubMed] [Google Scholar]
- August P, Oparil S.Hypertension in womenIn: Oparil S, Weber M (eds).Hypertension: A Companion to Brenner and Rector's the Kidney W. B. Saunders Company: Philadelphia, PA; 1999546–550. [Google Scholar]
- Os I, Oparil S, Gerdts E, et al. Essential hypertension in women. Blood Press. 2004;13:272–278. doi: 10.1080/08037050410024330. [DOI] [PubMed] [Google Scholar]
- Grimm RH, Jr., Grandits GA, Prineas RJ, et al. Long-term effects on sexual function of five antihypertensive drugs and nutritional hygienic treatment in hypertensive men and women. Treatment of Mild Hypertension Study (TOMHS) Hypertension. 1997;29:8–14. doi: 10.1161/01.hyp.29.1.8. [DOI] [PubMed] [Google Scholar]
- Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011;57:1404–1423. doi: 10.1016/j.jacc.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]