Abstract
Overweight/obese women are more likely to deliver newborns that also have a predisposition to store excessive amounts of fat since the early infancy period. Two evidence-based cycles are considered on the explanation of the maternal–child life-course approach for obesity prevention. The ‘maternal' cycle indicates that pre-pregnancy overweight primiparous women are more likely to gain excessive weight during gestation and to retain excessive weight postpartum. The ‘offspring' cycle indicates that newborns of pre-pregnancy overweight/obese women are more likely themselves to store excessive body fat starting very early on in life. The social ecological model (SEM) has been adopted as the framework needed to guide obesity prevention initiatives. The SEM considers the complex interrelationship among highly interconnected systems embedded within each other and having the individual on its inner most. Recommendations to women should include prevention of overweight/obesity prenatally, to attain adequate gestational weight and to lose the weight normally gained as part of the physiological response to pregnancy in the postpartum period. For the ‘offspring' the aims should be to promote optimal breastfeeding and complementary feeding practices, and to foster physical activity and adequate dietary habits. Well-coordinated inter-sectorial national obesity prevention programs built upon the life-course framework foundation requires in-depth early life systems analyses driven by the SEM.
Keywords: life-course, childhood, prevention, social ecological model
Introduction
Data from the USA National Health and Nutrition Examination Surveys show that among women of reproductive age, Latina and African American women are significantly more likely to be overweight or obese compared with their White counterparts.1 In addition, similar ethnic/racial obesity differentials among the offspring have been detected since infancy.2 The reasons for the similar ethnic/racial differentials in excessive obesity risk among women and their offspring deserve to be carefully considered, as this may have major public health implications for the design of obesity prevention programs. On the one hand, it is possible that these ‘coincidental' maternal–offspring trends are simply due to the fact that the dyads share a common environment. On the other hand, this may be due to the inheritance of genes that predispose both the mother and the offspring to become obese. Alternatively, it is possible that environmental exposures (for example, nutrient and endocrinological milieus) during pregnancy and infancy affect the expression of genes through epigenetic mechanisms, that is, environmental–genomic interactions.3 The empirical evidence offers overwhelming support for the later, as the most plausible explanation of the epidemiological finding that overweight/obese women are more likely to deliver newborns who also have a predisposition to store excessive amounts of fat since the early infancy period.4 This is the basis behind the life-course approach for childhood obesity prevention5 and the need for dramatically changing the environments and the quality of health promotion education and preventive health-care services offered to women and their children regardless of their social position.
Life-course approach for childhood obesity prevention
Pérez-Escamilla and Bermúdez described two evidence-based cycles that help explain the maternal–child life-course approach.5 These highly interrelated cycles are important to understand, as they can help guide the development of obesity prevention policies and programs from the local to the national and macro regional level in the context of the nutrition transition described by Kac and Pérez-Escamilla in this supplement issue.
In the obesogenic environments that characterize today's stages of the nutrition transition in most countries, pregnancy is indeed a major risk factor for maternal obesity. The first or ‘maternal' cycle indicates that primiparous women are more likely to gain excessive weight during gestation (in relation to the Institute of Medicine recommendation corresponding to their pre-pregnancy body mass index) and to retain excessive weight postpartum.6 As a result, women become more overweight or obese in subsequent pregnancies as the cycle repeats itself. This may explain at least in part why in the USA Latina and African–American mothers, who have higher fertility rates than their White counterparts, are more likely to be overweight or obese.5 The second or ‘offspring' cycle indicates that offspring born to women who were overweight or obese when they became pregnant are more likely themselves to store excessive body fat starting very early on in life. This risk gets compounded if the mother gains excessive weight during pregnancy and the infant is not breastfed exclusively for the first 6 months of life, and is introduced to obesogenic complementary foods and sugar sweetened beverages. This in turn increases the chance that the infant will accrue excessive weight during the first year of life, which is a significant risk factor for the subsequent development of obesity.5 If the child continues to be exposed to hyper-caloric unhealthy foods and suboptimal physical activity levels during the toddler and preschool periods, then there is a good chance that she/he will remain overweight/obese during the primary school and adolescent years. At this point, the chances that the youth will remain overweight/obese as an adult are very high. This implies that in the case of a girl born to an overweight or obese mother, it is very likely that she herself will enter her first pregnancy in the same overweight/obese state as her mother did and for the maternal and offspring cycles to repeat themselves facilitating the ‘transfer' of obesity to the next generation. Taveras et al.7 have shown in a cohort study conducted in Boston that ethnic/racial minority children are more likely to be exposed to prenatal, pregnancy, infancy and early childhood dietary (lack of breastfeeding, introduction to complementary foods by 4 months of life, consumption of sugar sweetened beverages and fast food), physical inactivity and other (for example, insufficient sleep time, maternal depression) obesogenic risk factors compared with their White counterparts.7 This may explain, at least in part, why minority children are more likely to accumulate excessive body fat since early infancy.
The following section describes the multilevel and multi-sectorial approach needed for addressing childhood obesity prevention based on the life-course framework.
Multilevel and multi-sectorial life-course approach for preventing childhood obesity
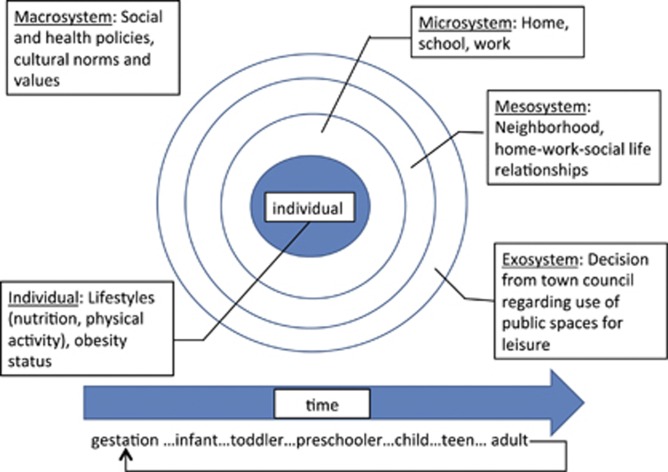
The social ecological model (SEM), based on the conceptualization of human development by Bronfenbrenner,8 has been widely adopted as the framework needed to guide obesity prevention initiatives in the Unites States and other countries.9 Analogous to a set of Russian dolls, the SEM posits that the lifestyle choices that individuals make are the result of the complex interrelationship among highly interconnected systems embedded within each other: (a) the immediate micro system surrounding the individual (for example, home, school, work), (b) the meso-system (for example, neighborhood characteristics, relationship between home, work and social life) surrounding the micro-system, (c) the exo-system (for example, decision from town council regarding use of public spaces for physical activity) surrounding the meso-system and d) the macro-system (for example, social and health policies, cultural norms and values) surrounding the lower order exo-, meso- and micro-systems (Figure 1).
Figure 1.
The multilevel components of the social-ecological model depicting how macro-, exo-, meso- and micro-systems shape lifestyle behaviors and maternal–child obesity risks. The time dimension depicts the life-course framework for understanding change in environments/exposures across the life-course and the parental–offspring ‘transmission' of obesity risk. Diagram developed for manuscript based on concepts from Pérez-Escamilla and Bermúdez5 and Bronfenbrenner8.
Nader et al.4 conducted an early life systems analysis to better understand effective policies and specific actions to prevent childhood obesity in the United States that is consistent with the SEM. Consistent with the ‘maternal' life-course cycle,5 Nader et al.4 specifically recommend to support women to prevent overweight/obesity prenatally, attain adequate gestational weight and to lose the needed pregnancy-related weight in the postpartum period. Consistent with the ‘offspring' cycle,5 they recommend addressing breastfeeding, complementary feeding and other factors during infancy, as well as fostering physical activity, adequate dietary habits and limiting screen time during the toddler period. In terms of strategies they call for policy, professional, and educational approaches to reach out to women and their offspring before the obesity problem develops. As documented in this workshop, education and counseling are necessary for ultimately nudging women and young infants toward healthy lifestyles capable of preventing the onset of obesity. However, for women and children to be able to apply the knowledge gained, major environmental changes are needed as suggested by Nader et al.4
The following section briefly describes a case study involving how a local community–academic partnership led to the development of sound maternal–child health and nutrition education following the life-course approach.
Life-course community-based education and support: the Hispanic Family Nutrition Program
The ongoing Hispanic Family Nutrition Program was co-founded in 1995 in Hartford, Connecticut, by the Hispanic Health Council and the University of Connecticut, with funding from the education department of the Supplemental Nutrition Assistance Program (formerly known as the Food Stamp Program). Since its inception, its goal was to provide informational and instrumental education to Supplemental Nutrition Assistance Program recipient families with young children. Consistent with the life-course framework, this evidence-based program has delivered the following education initiatives to minority women and their children: (a) social marketing campaigns targeting increased fruit and vegetable consumption, (b) prenatal nutrition guide including gestational weight gain recommendations, (c) breastfeeding peer counseling, (d) complementary feeding guide, (e) a series of six food and nutrition puppet shows delivered through public school to low-income children enrolled from preschool through fourth grade.10 An important gap in this and several other community-based programs is that a comprehensive collective evaluation of these initiatives at influencing childhood obesity outcomes still needs to be conducted.
Conclusions
Empirical evidence strongly supports the adequacy of following the life-course framework for obesity prevention in order to slow down the epidemic. Waiting until children start school to initiate intervening may be too late for many of them who, through epigenetic mechanisms, are already strongly ‘programmed' to become obese. The life-course framework provides policy makers and program leaders with a pragmatic and useful approach to guide childhood obesity prevention programs from the local (as illustrated through the Hispanic Family Nutrition Program) to the national or even macro regional level. As this supplement illustrates in countries such as Mexico (see Latnovic and Cabrera (in this supplement issue)) and Brazil (see Silva and coworkers (in this supplement issue)) several of the life-course framework initiatives needed for childhood obesity prevention are in place but others are missing or need to be strengthened substantially, especially those related to the pre-conceptional, pregnancy and postpartum period. Designing, implementing and evaluating the impact of well-coordinated inter-sectorial national obesity prevention programs built upon the life-course framework foundation requires in-depth early life systems analyses driven by the SEM.
As the focus of this paper was on the consequences of maternal–child obesity, we did not include a discussion on the obesogenic consequences for the offspring when the mother does not gain enough during pregnancy and as a result the newborn has low birth weight known as Barker's hypothesis.11 However, we fully recognize that maternal undernutrition also has major implications for the childhood obesity epidemic.
Acknowledgments
RP-E has received grant support from National Institutes of Health and the Centers for Disease Control and Prevention. GK is a research fellow from the Brazilian National Council for Scientific and Technological Development (CNPq). The publication was supported in part by the Government of Aruba, the Obetech Obesity Research Center, the Pan American Health Organization and the Pan American Health and Education Foundation. This paper is derived from the workshop ‘Education for childhood obesity prevention: A life-course approach', co-organized by the Panamerican Health Organization (PAHO) and the Panamerican Health and Education Foundation (PAHEF), and held on 14 June 2012 in Aruba, as part of the II Pan-American Conference on Childhood Obesity (http://www.paco.aw/).
The authors declare no conflict of interest.
References
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 2012; 307: 491–497. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012; 307: 483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IOM (Institute of Medicine). Weight Gain during Pregnancy: Reexamining the Guidelines. The National Academies Press: Washington, DC, USA. [PubMed] [Google Scholar]
- Nader PR, Huang TT, Gahagan S, Kumanyika S, Hammond RA, Christoffel KK. Next steps in obesity prevention: altering early life systems to support healthy parents, infants, and toddlers. Child Obes 2012; 8: 195–204. [DOI] [PubMed] [Google Scholar]
- Pérez-Escamilla R, Bermúdez O. Early life nutrition disparities: where the problem begins? Adv Nutr 2012; 3: 71–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kac G, Benício MH, Velásquez-Meléndez G, Valente JG, Struchiner CJ. Gestational weight gain and pre-pregnancy weight influence postpartum weight retention in a cohort of Brazilian women. J Nutr 2004; 134: 661–666. [DOI] [PubMed] [Google Scholar]
- Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics 2010; 125: 686–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. The Ecology of Human Development. Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Story M, Kaphingst KM, Robinson-O′Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health 2008; 29: 253–272. [DOI] [PubMed] [Google Scholar]
- Pérez-Escamilla R, Damio G, Himmelgreen D, González A, Segura-Pérez S, Bermúdez-Millán A. Translating knowledge into community nutrition programs: lessons learned from the Connecticut Family Nutrition Program for Infants, Toddlers, and Children. Recent Res Dev Nutr 2002; 5: 69–90. [Google Scholar]
- Vaag AA, Grunnet LG, Arora GP, Brøns C. The thrifty phenotype hypothesis revisited. Diabetologia 2012; 55: 2085–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]