Abstract
Abnormalities in bone turnover, mineralization, and volume represent one of the three components of chronic kidney disease–related mineral and bone disorder (CKD-MBD). The risk of hip fracture is considerably high, while the risk of spinal compression fracture may not be more elevated among CKD patients than in general population. The relationship between bone fracture and bone mineral density in CKD patients is more complex than in those without kidney disease. An increase in the rate of falls has been reported to be a major cause of high hip fracture risk among CKD patients; however, it certainly is not the only underlying mechanism. Abnormal parathyroid function is not likely to be a major cause of hip fracture among CKD patients. In experimental CKD animals, mechanical elasticity properties of long bones showed an inverse correlation with kidney function. The deterioration of bone elasticity showed a significant correlation with bone biochemical changes. Of note, administration of the oral absorbent AST-120 was capable of preventing both changes. These findings suggest that uremic toxins cause a deterioration of bone material properties, and changes in material properties disturb bone elasticity. This disease concept cannot be considered to be a direct consequence of CKD-MBD. We therefore would like to call it ‘uremic osteoporosis'. This entity may be a major cause of increased hip fracture risk among CKD patients.
Keywords: bone elastic mechanical properties, hip fracture, osteoporosis, uremic toxin
Although various abnormalities of bone metabolism are associated with chronic kidney disease (CKD), the pathophysiological background is not fully understood. Adherence to conventional concepts may have hindered our understanding of the mechanisms involved in the various types of skeletal disease. In the present paper, we review bone abnormalities in CKD patients from the perspective of fragility fracture prevention, and discuss a new bone disease concept named ‘uremic osteoporosis'.
CKD-RELATED MINERAL AND BONE DISORDER (CKD-MBD) AND BONE LESIONS ASSOCIATED WITH CKB-MBD
CKD-MBD is a systemic syndrome defined as ‘a systemic disorder of mineral metabolism that can lead to bone and cardiovascular abnormalities.' The syndrome consists of abnormalities in laboratory values, abnormal bone metabolism, and vascular calcification.1
Bone biopsy samples obtained from CKD patients demonstrate a wide spectrum of modified bone turnover and/or mineralization at the calcification front.2, 3 Histological examination is the most reliable method of assessing bone turnover and mineralization,4 and therefore bone biopsy is regarded as the gold standard in diagnosing bone disease in CKD.5, 6 However, whether bone turnover and mineralization, as assessed by histomorphometry, are truly the most important features to be assessed in evaluating the pathologic changes of bone metabolism observed in patients with CKD remains to be proven.
FRACTURE RISK IN PATIENTS WITH CKD
The risk of hip fracture among CKD patients is strikingly elevated.7, 8, 9, 10 The standard incidence ratio of hip fracture among dialysis patients was recently reported to be as high as 4.9–6.2.9 Considering the serious consequences of fractures from both clinical and social perspectives, the elevated risk of hip fracture and its treatment and prevention are major problem in patients with CKD.
On the other hand, the risk of spinal compression fracture may not be elevated among CKD patients.10, 11, 12 The situation looks quite different than that of hip fractures, which are obviously much more frequent in this patient population.7, 8, 9, 10
The relationship between fracture and bone mineral density in CKD patients is complex, and it remains controversial whether it is useful to assess bone mineral density in these patients on a regular basis.13, 14, 15, 16, 17 Regardless of the primary disease, bone mass is undoubtedly a major determining factor in bone mechanical strength;18 however, its contribution to bone strength is not necessarily a constant factor. Its relative contribution would be decreased under conditions where a higher number of factors or stronger factors are present, which determine bone strength other than bone mass. Considering several inconsistent reports on the relationship between bone mass and fracture risk, CKD is potentially such a condition.
BONE FRAGILITY OR ELEVATED FRACTURE RISK
In the majority of patients with CKD, hip fracture occurs as a consequence of a fall. CKD patients frequently fall,19, 20, 21 and this condition appears to be an important cause of increased hip fracture risk.
CKD induces muscle wasting22, 23, 24 and limitation of joint motion.25 The two of them probably contribute to the increase in risk of falls. As abnormal vitamin D metabolism is one among the possible causes of muscle wasting in CKD,26 bone fracture due to muscle weakness could also be regarded as a fraction of CKD-MBD.
The increased occurrence of falls almost certainly is a major cause of elevated hip fracture risk among CKD patients; however, it seems unlikely to be the only one. First, falls may induce compression fractures as well as hip fractures. If increased falls are a critical cause of increased hip fracture risk, the risk of spinal compression fracture would also be increased. Second, the risk of hip fracture among CKD patients is elevated even among those in their 20s.9 A simple fall rarely causes hip fracture among patients in their 20s unless bone fragility is increased. For instance, the administration of native vitamin D prevents hip fracture through decreasing the risk of falls, however, such an effect is observed among those younger than 65 years of age.27
Thus, an increase in fall rates does not seem to be the only cause of increased hip fracture risk among CKD patients. Increased bone fragility probably contributes as well, and this may be another important factor in the uremic state.
HIP FRACTURE AND CKD-MBD
The recent Kidney Disease Improving Global Outcomes (KDIGO) guideline for CKD-MBD advocates prevention of bone fracture as a major treatment objective.1 As mentioned above, the hip joint is the most frequent fracture site among CKD patients. Therefore, the KDIGO treatment recommendation above could be replaced by ‘prevention of hip fracture as a major treatment objective in CKD-MBD.' In this scenario, CKD-MBD would be assumed to be the major cause of hip fracture, but is this really the case?
Treatment success of CKD-MBD is generally assessed based on improved control of circulating Ca, P, and parathyroid hormone (PTH) levels. The optimal ranges of these biochemical parameters have been defined by KDIGO and other national/regional clinical practice guidelines.28, 29, 30 Among these parameters, several reports dealt with a possible relationship between hip fracture and serum PTH levels.10, 31, 32, 33 Some of them reported an association with extremely elevated levels of PTH and an increase in hip fracture risk, whereas others failed to find such a relationship, and others focused on an increased risk among those with extremely low PTH levels. However, it is probably not clinically meaningful to consider the generally small increase of fracture risk in presence of extreme PTH values as an important cause of hip fracture among CKD patients, in whom the risk is several times greater than that of the general population.8, 9 In fact, it has so far proven impossible to identify an optimal PTH range, which would be associated with a decrease in the risk of hip fracture in a satisfactory way. Although different PTH levels are associated with different bone histology features,34, 35, 36 the association with bone fracture rates is thus far from being established. These findings strongly suggest that conventional bone histomorphometry classification contributes little to the identification of optimal treatment and prevention approach with respect to fragility fractures.
CHANGES IN BONE MATERIAL PROPERTIES IN THE UREMIC STATE
On the one hand, spinal compression fracture is caused by forces applied in parallel to the surface of cortical bone. Bone mass and cancellous bone microstructure critically affects the process involved in the development of this type of fracture. On the other hand, long bone fractures are generally caused by forces applied in vertical direction relative to cortical bone. In the development of this type of fracture, bone elasticity has a major role in addition to cortical bone mass. If the mechanical properties of bone elasticity were deteriorated above all in CKD patients, this would reasonably well explain why hip fracture risk, but not spinal compression fracture risk, is considerably elevated.
Although it is practically impossible to assess the mechanical properties of long bone elasticity in CKD patients directly, suggestive findings on this issue have been provided by in vivo experimental studies. In animals with CKD, the mechanical properties of elasticity in femoral bones showed a clear inverse correlation with creatinine clearance, indicating that uremia deteriorates long bone elasticity (Figure 1). Interestingly, the deterioration of bone elasticity showed significant correlations with bone biochemical changes as assessed by spectroscopic analyses.37 Moreover, administering the oral absorbent AST-120 prevented both bone biochemical changes and bone elasticity deterioration.38
Figure 1.
Relationship between kidney function and bone elasticity in chronic kidney disease (CKD) rats. The femoral bone elastic mechanical properties assessed by dynamic mechanical analysis (DMA) method showed a clear sigmoid curve relationship with the creatinine clearance (CCr) levels in partial nephrectomized rats with chronic kidney insufficiency. In other words, bone elasticity decreases along with deterioration of the kidney function, which causes increased risk of fracture against mechanical load from the vertical direction to the cortical bone surface.37
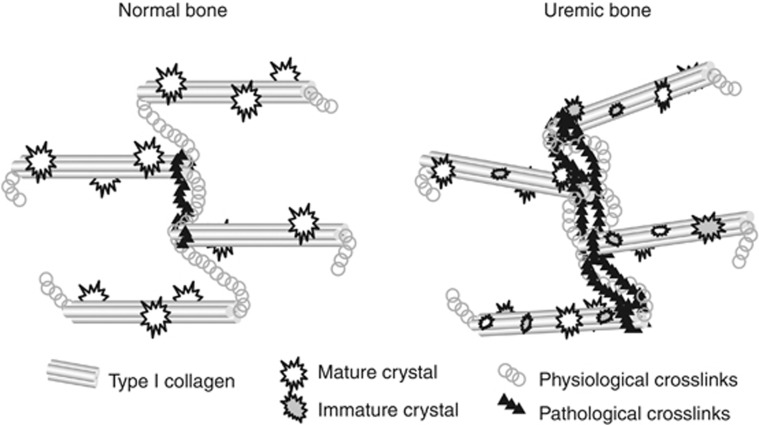
AST-120 is an oral adsorbent of low molecular uremic toxins such as indoxyl sulfate and p-cresyl sulfate.39 The administration of AST-120 did not improve kidney function or systemic mineral metabolism. Nevertheless, it prevented bone biochemical changes that are specifically promoted in uremic condition, and bone elasticity was preserved. These findings strongly suggest that uremic toxins adsorbed to AST-120 caused alterations in bone chemical properties or bone cell activities.40 This in turn could affect bone matrix proteins and/or mineral crystals causing deterioration of bone material properties, and consequently disturbances of the mechanical properties of bone elasticity (Figure 2).
Figure 2.
Changes in bone material properties in uremic condition. Bone matrix has a structure in which type-I collagen fibers connected with crosslinks fibers form the main framework to which matrix protein and mineral crystals attach. In uremic condition, it was revealed that both physiological and pathological crosslinks increase, the orientation of collagen fibers is disturbed, and the mineral crystal remains immature. These changes in material property cause deteriorated bone elasticity in theory, and in fact these changes are closely correlated with mechanical properties of bone elasticity in experimental CKD animals. However, it is difficult to obtain any information about these material changes from biopsied bone histological findings.38
CKD-MBD AND UREMIC OSTEOPOROSIS
Bone has two major functions in vertebrates, securing body firmness and buffering minerals in extracellular fluid. Fracture causes failure of the former function, and failure of the latter function leads to the disturbances of systemic mineral metabolism.
Osteoporosis is defined as ‘a skeletal disorder characterized by compromised bone strength predisposing to an increased risk of fracture'.41 In other words, osteoporosis is any condition with increased bone fragility. Osteopenia is one of the indicators for increased bone fragility, but not a compulsory aspect for osteoporosis.
CKD-MBD is defined as ‘a systemic disorder of mineral metabolism that can lead to bone and cardiovascular abnormalities', as mentioned above.1 Concerning the bone abnormalities of CKD-MBD, the underlying causes must be CKD and/or CKD-related systemic mineral metabolic disturbances, whereas the modalities of bone dysfunction have not been specifically designated. However, as this disease concept is the consequence of disturbances in systemic mineral metabolism, one would naturally assume that changes in the function of ‘buffering minerals in extracellular fluid' would represent the main disturbance (Table 1).
Table 1. Bone has two major physiological functions, namely ‘securing body firmness' and ‘buffering minerals in extracellular fluid'.
| Pathogenesis | Impaired bone function | |
|---|---|---|
| Osteoporosis | Not specified | Securing body firmness |
| Abnormal bone metabolism in CKD-MBD | CKD-related disorders of systemic mineral metabolism | Predominantly mineral buffering |
Abbreviation: CKD-MBD, chronic kidney disease-related mineral and bone disorder. Osteoporosis is a disease in which bone fails to secure body firmness, but the causative factors are unclear. Bone abnormalities in CKD-MBD occur because of CKD and/or disturbance in systemic mineral metabolism associated with CKD. However, either bone function could be disturbed as a consequence. Thus, when bone fragility is increased in CKD patents, a diagnosis of osteoporosis can be made. CKD-MBD may be a cause of osteoporosis.
Consequently, the disease concepts of osteoporosis and bone abnormalities in CKD-MBD are totally different. Bone fragility is not a condition required for CKD-MBD. If CKD patients show bone fragility, the diagnosis of osteoporosis can be made. However, CKD-MBD could be the cause or one of the causes of the osteoporotic condition.
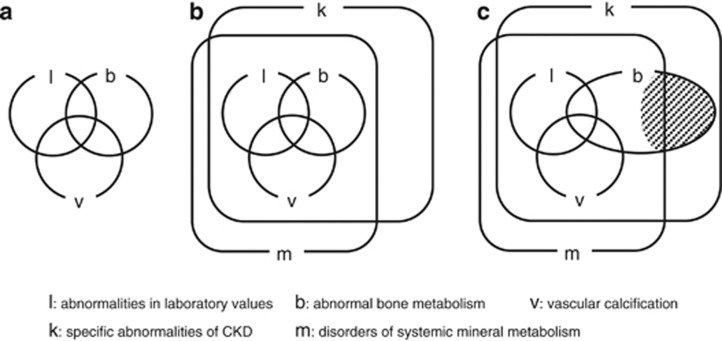
KDIGO has proposed a conceptual figure for CKD-MBD (Figure 3a).1 This figure is unfortunately incomplete in expressing the disease definition precisely. In order to express the definition of CKD-MBD mentioned above more precisely, the set shown in Figure 3a must be within the subset of two larger sets of ‘specific abnormalities of CKD' and ‘disorders of systemic mineral metabolism' (Figure 3b). However, ‘abnormalities of bone metabolism' as a subset of ‘specific abnormalities in CKD' is not necessarily always a subset of ‘disorders of systemic mineral metabolism.' For instance, if uremic toxin-induced deterioration of bone elastic mechanical properties causes bone fragility, it is one of the ‘specific abnormalities in CKD' and ‘abnormalities of bone metabolism' but not the consequence of ‘disorders of systemic mineral metabolism.' Hypogonadism is frequently found in CKD patients, which potentially promotes bone fragility independent from abnormal systemic mineral metabolism, especially in women.42 These conditions cannot be considered as factors of CKD-MBD, but are located within the shaded area in Figure 3c. We would like to term the disease condition located in this shaded area as ‘uremic osteoporosis'. Uremic osteoporosis may be a major cause of increased hip fracture risk observed among CKD patients. Further studies are clearly needed to validate this hypothesis.
Figure 3.
Chronic kidney disease-related mineral and bone disorder (CKD-MBD) and uremic osteoporosis. The Kidney Disease Improving Global Outcomes (KDIGO) advocates a figure for understanding the concept of CKD-MBD (a). However, the concept of CKD-MBD should be expressed as shown in (b) according to the disease definition strictly. However, bone abnormalities specific to CKD condition are not always a consequence of systemic abnormalities in mineral metabolism, and therefore the shaded area in c indicates such disease condition. This concept is termed uremic osteoporosis, which may be the main cause of increased risk of hip fracture among CKD patients. b, abnormal bone metabolism; l, abnormalities in laboratory values; k, specific abnormalities of CKD; m, disorders of systemic mineral metabolism; v, vascular calcification.
CONCLUSION
If one accepts the concept of ‘uremic osteoporosis' described above, this implies that one has to abandon the conventional agreement that bone remodeling frequency and mineralizing speed at the calcification front are the main, if not the most crucially important factors determining fracture propensity in CKD, because the relationships between these factors and bone chemical properties are unknown. Consequently, the general consensus that bone biopsy remains the gold standard for the diagnosis of changes in bone structure and function in patients with CKD may become outdated. A paradigm shift is approaching.
Acknowledgments
This supplement was supported by a grant from the 58th Annual Meeting of the Japanese Society for Dialysis Therapy.
JJK and YI have received grant support from the Japanese Society of the Promotion of Science. JJK and MF have received consulting and lecture fees from Kyowa-Hakko Kirin, Chugai, Bayer Japan, and Astellas. MF has also received consulting fees from Novartis, JT, Abbvie, and grant support from Kyowa-Hakko Kirin and Chugai.
References
- Moe S, Drueke T, Cunningham J, et al. Kidney Disease: Improving Global Outcomes (KDIGO): definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2006;69:1945–1953. doi: 10.1038/sj.ki.5000414. [DOI] [PubMed] [Google Scholar]
- Sherrard DJ, Hercz G, Pei Y, et al. The spectrum of bone disease in end-stage renal failure—an evolving disorder. Kidney Int. 1993;43:436–442. doi: 10.1038/ki.1993.64. [DOI] [PubMed] [Google Scholar]
- Malluche HH, Mawad HW, Monier-Faugere MC. Renal osteodystrophy in the first decade of the new millennium: analysis of 630 bone biopsies in black and white patients. J Bone Miner Res. 2011;26:1368–1376. doi: 10.1002/jbmr.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott SM. Histomorphometric measurements of bone turnover, mineralization, and volume. Clin J Am Soc Nephrol. 2008;3 (Suppl 3:S151–S156. doi: 10.2215/CJN.04301206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malluche HH, Langub MC, Monier-Faugere MC. The role of bone biopsy in clinical practice and research. Kidney Int. 1999. pp. S20–S25. [DOI] [PubMed]
- Ott SM. Bone histomorphometry in renal osteodystrophy. Semin Nephrol. 2009;29:122–132. doi: 10.1016/j.semnephrol.2009.01.005. [DOI] [PubMed] [Google Scholar]
- Maravic M, Ostertag A, Torres PU, et al. Incidence and risk factors for hip fractures in dialysis patients Osteoporos Int(in press). [DOI] [PubMed]
- Alem AM, Sherrard DJ, Gillen DL, et al. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int. 2000;58:396–399. doi: 10.1046/j.1523-1755.2000.00178.x. [DOI] [PubMed] [Google Scholar]
- Wakasugi M, Kazama JJ, Taniguchi M, et al. Increased risk of hip fracture among Japanese hemodialysis patients. J Bone Miner Metab. 2013;31:315–321. doi: 10.1007/s00774-012-0411-z. [DOI] [PubMed] [Google Scholar]
- Jadoul M, Albert JM, Akiba T, et al. Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2006;70:1358–1366. doi: 10.1038/sj.ki.5001754. [DOI] [PubMed] [Google Scholar]
- Fusaro M, D'Angelo A, Scalzo G, et al. Vertebral fractures in dialysis: endocrinological disruption of the bone-kidney axis. Endocrinol Invest. 2010;33:347–352. doi: 10.1007/BF03346598. [DOI] [PubMed] [Google Scholar]
- EVOLVE Trial Investigators Chertow GM, Block GA, Correa-Rotter R, et al. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med. 2012;367:2482–2494. doi: 10.1056/NEJMoa1205624. [DOI] [PubMed] [Google Scholar]
- Jamal SA, West SL, Miller PD. Fracture risk assessment in patients with chronic kidney disease. Osteoporos Int. 2012;23:1191–1198. doi: 10.1007/s00198-011-1781-0. [DOI] [PubMed] [Google Scholar]
- Nickolas TL, Stein E, Cohen A, et al. Bone mass and microarchitecture in CKD patients with fracture. J Am Soc Nephrol. 2010;21:1371–1380. doi: 10.1681/ASN.2009121208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yenchek RH, Ix JH, Shlipak MG, et al. Bone mineral density and fracture risk in older individuals with CKD. Clin J Am Soc Nephrol. 2012;7:1130–1136. doi: 10.2215/CJN.12871211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal SA, Hayden JA, Beyene J. Low bone mineral density and fractures in long-term hemodialysis patients: a meta-analysis. Am J Kidney Dis. 2007;49:674–681. doi: 10.1053/j.ajkd.2007.02.264. [DOI] [PubMed] [Google Scholar]
- Jamal S, Cheung AM, West S, et al. Bone mineral density by DXA and HR pQCT can discriminate fracture status in men and women with stages 3 to 5 chronic kidney disease. Osteoporos Int. 2012;23:2805–2813. doi: 10.1007/s00198-012-1908-y. [DOI] [PubMed] [Google Scholar]
- Ritchie RO. How does human bone resist fracture. Ann N Y Acad Sci. 2010;1192:72–80. doi: 10.1111/j.1749-6632.2009.05232.x. [DOI] [PubMed] [Google Scholar]
- Cook WL, Tomlinson G, Donaldson M, et al. Falls and fall-related injuries in older dialysis patients. Clin J Am Soc Nephrol. 2006;1:1197–1204. doi: 10.2215/CJN.01650506. [DOI] [PubMed] [Google Scholar]
- Desmet C, Beguin C, Swine C, Université Catholique de Louvain Collaborative Group et al. Falls in hemodialysis patients: prospective study of incidence, risk factors, and complications. Am J Kidney Dis. 2005;45:148–153. doi: 10.1053/j.ajkd.2004.09.027. [DOI] [PubMed] [Google Scholar]
- Rossier A, Pruijm M, Hannane D, et al. Incidence, complications and risk factors for severe falls in patients on maintenance haemodialysis. Nephrol Dial Transplant. 2012;27:352–357. doi: 10.1093/ndt/gfr326. [DOI] [PubMed] [Google Scholar]
- Xu J, Li R, Workeneh B, et al. Transcription factor FoxO1, the dominant mediator of muscle wasting in chronic kidney disease, is inhibited by microRNA-486. Kidney Int. 2012;82:401–411. doi: 10.1038/ki.2012.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Workeneh BT, Mitch WE. Review of muscle wasting associated with chronic kidney disease. Am J Clin Nutr. 2010;91:1128S–1132S. doi: 10.3945/ajcn.2010.28608B. [DOI] [PubMed] [Google Scholar]
- Thomas SS, Dong Y, Zhang L, et al. Signal regulatory protein-α interacts with the insulin receptor contributing to muscle wasting in chronic kidney disease. Kidney Int. 2013;84:308–316. doi: 10.1038/ki.2013.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazama JJ, Yamamoto S, Takahashi N, et al. Abeta-2M-amyloidosis and related bone diseases. J Bone Miner Metab. 2006;24:182–184. doi: 10.1007/s00774-005-0669-5. [DOI] [PubMed] [Google Scholar]
- Boudville N, Inderjeeth C, Elder GJ, et al. Association between 25-hydroxyvitamin D, somatic muscle weakness and falls risk in end-stage renal failure. Clin Endocrinol (Oxf) 2010;73:299–230. doi: 10.1111/j.1365-2265.2010.03821.x. [DOI] [PubMed] [Google Scholar]
- Bischoff-Ferrari HA, Willett WC, Orav EJ, et al. A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med. 2012;367:40–49. doi: 10.1056/NEJMoa1109617. [DOI] [PubMed] [Google Scholar]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder(CKD-MBD) Kidney Int. 2009. pp. S1–S130. [DOI] [PubMed]
- National Kidney Foundation K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2004;42 (Suppl 3:S1–S202. [PubMed] [Google Scholar]
- Fukagawa M, Yokoyama K, Koiwa F, et al. CKD-MBD guideline working group; Japanese Society for Dialysis Therapy. Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Ther Apher Dial. 2013;17:247–288. doi: 10.1111/1744-9987.12058. [DOI] [PubMed] [Google Scholar]
- Nakai S, Suzuki K, Masakane I, et al. Overview of regular dialysis treatment in Japan (as of 31 December 2008) Ther Apher Dial. 2010;14:505–540. doi: 10.1111/j.1744-9987.2010.00893.x. [DOI] [PubMed] [Google Scholar]
- Coco M, Rush H. Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis. 2000;36:1115–1121. doi: 10.1053/ajkd.2000.19812. [DOI] [PubMed] [Google Scholar]
- Danese MD, Kim J, Doan QV, et al. PTH and the risks for hip, vertebral, and pelvic fractures among patients on dialysis. Am J Kidney Dis. 2006;47:149–156. doi: 10.1053/j.ajkd.2005.09.024. [DOI] [PubMed] [Google Scholar]
- Qi Q, Monier-Faugere MC, Geng Z, et al. Predictive value of serum parathyroid hormone levels for bone turnover in patients on chronic maintenance dialysis. Am J Kidney Dis. 1995;26:622–631. doi: 10.1016/0272-6386(95)90599-5. [DOI] [PubMed] [Google Scholar]
- Gal-Moscovici A, Popovtzer MM. New worldwide trends in presentation of renal osteodystrophy and its relationship to parathyroid hormone levels. Clin Nephrol. 2005;63:284–289. doi: 10.5414/cnp63284. [DOI] [PubMed] [Google Scholar]
- Morishita T, Nomura M, Hanaoka M, et al. Anew assay method that detects only intact osteocalcin. Two-step non-invasive diagnosis to predict adynamic bone disease in haemodialysed patients. Nephrol Dial Transplant. 2000;15:659–667. doi: 10.1093/ndt/15.5.659. [DOI] [PubMed] [Google Scholar]
- Iwasaki Y, Kazama JJ, Yamato H, et al. Changes in chemical composition of cortical bone associated with bone fragility in rat model with chronic kidney disease. Bone. 2011;48:1260–1267. doi: 10.1016/j.bone.2011.03.672. [DOI] [PubMed] [Google Scholar]
- Iwasaki Y, Kazama JJ, Yamato H, et al. Accumulated uremic toxins attenuate bone mechanical properties in rats with chronic kidney disease Bone(in press). [DOI] [PubMed]
- Akiyama Y, Takeuchi Y, Kikuchi K, et al. A metabolomic approach to clarifying the effect of AST-120 on 5/6 nephrectomized rats by capillary electrophoresis with mass spectrometry (CE-MS) Toxins (Basel) 2012;4:1309–1322. doi: 10.3390/toxins4111309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka H, Iwasaki Y, Yamato H, et al. p-Cresyl sulfate induces osteoblast dysfunction through activating JNK and p38 MAPK pathways. Bone. 2013;56:347–354. doi: 10.1016/j.bone.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Osteoporosis prevention, diagnosis, and therapy. NIH Consensus Statement. 2000;17:1–45. [PubMed] [Google Scholar]
- Doumouchtsis KK, Perrea DN, Doumouchtsis SK. The impact of sex hormone changes on bone mineral deficit in chronic renal failure. Endocr Res. 2009;34:90–99. doi: 10.1080/07435800903127598. [DOI] [PubMed] [Google Scholar]