Abstract
In the past 25 years the International Society of Nephrology has sponsored 545 physicians from 83 developing countries to undertake nephrology training in renal units in the developed world. Data collected biennially from past fellows have demonstrated a very positive impact of the program on individual trainees and their home institutions. Many of the trainees have gone on to leadership positions in their home institutions, countries, and regions. Increasingly, fellowships are undertaken in selected developed centers within the fellow's own region, which increases the relevance and utility of the training to the fellow and the fellow's home institution, and lessens the risk of ‘brain drain'.
Keywords: clinical training, developing countries, fellowship, nephrology training
ISN GLOBAL OUTREACH PROGRAMS
The mission of the International Society of Nephrology (ISN) is to advance the diagnosis, treatment, and prevention of kidney disease in both the developed and the developing worlds. Around 20 years after its founding, ISN introduced a series of new programs to enhance its services to developing countries, where needs go beyond the traditional member benefits of journal subscriptions and reduced registration fees at meetings. Over time these programs, originally under the umbrella of the Commission on the Global Advancement of Nephrology (COMGAN), have evolved into what are now called the ISN Global Outreach programs (ISN GO). GO programs target all countries in the developing world. Within ISN GO are several discreet programs—Fellowship, Sister Renal Center, Continuing Medical Education, Educational Ambassador and Research and Prevention. ISN commits ∼30% of its budget to these GO programs, the single largest cost item in the annual budget after administration of the society itself. Previous publications have provided details of each of those programs,1 but have not focused on formal assessment of their impacts.
ISN'S FELLOWSHIP PROGRAM
ISN's Fellowship Program was established in 1985 and specifically designed to enhance renal care by training more physicians to practice nephrology in less developed countries, many of which had no trained nephrologists at all.2 In its first 25 years, this program has trained 545 fellows from 83 developing countries. Applications have also been received from four other countries (Cuba, Sudan, Iran, and Myanmar) but could not be funded because these countries are embargoed by the US Office of Foreign Assets Control (OFAC). As ISN is registered in the United States, these candidates must await a change in OFAC rulings. ISN fellows undertook short- (2–6 months) or long-term (6–12 months) training in host institutions from 24 developed countries (Tables 1 and 2). Each fellow can apply to extend their fellowship by up to 12 months. Applicants typically have at least a year's experience in nephrology in their home institution and are aged 30–40 years, although some exceptions have been made to seed nephrology in the countries where no trained nephrologist currently exists. They can apply to the program in one of two rounds annually, and an international panel of nephrologists assesses their applications competitively. Approximately 70% of applications are successful. Among a range of assessment criteria are the specific needs of the home institution and its match to the proposed training available in the host unit. The importance of properly targeted fellowships with clear objectives has also been stressed for other fellowships, including those of the World Health Organization.3 National nephrology societies affiliated with the ISN, and ISN's own regional committees, are invited to solicit individual applications from within their regions and to comment on their national relevance to assist the committee in its evaluations. At the end of the fellowship fellows and their host mentors must submit reports by which their progress and achievements are assessed.
Table 1. Number of fellows by home and host region.
| |
Host region |
||||||
|---|---|---|---|---|---|---|---|
| Home region | Total | Africa | East Asia | Europe | Latin America | North America | OSEA |
| Africa | 114 | 33 | 1 | 57 | 0 | 22 | 1 |
| East Asia | 67 | 0 | 10 | 22 | 0 | 27 | 8 |
| Eastern and Central Europe | 66 | 0 | 0 | 33 | 0 | 31 | 2 |
| Latin America | 107 | 0 | 0 | 49 | 6 | 51 | 1 |
| Middle East | 20 | 5 | 0 | 9 | 0 | 6 | 0 |
| OSEA | 57 | 0 | 2 | 6 | 0 | 32 | 17 |
| Russia and CIS | 33 | 1 | 0 | 10 | 0 | 22 | 0 |
| South Asia | 81 | 1 | 1 | 27 | 0 | 32 | 20 |
| Total | 545 | 40 | 14 | 213 | 6 | 223 | 49 |
Abbreviations: CIS, Commonwealth of Independent States; OSEA, Oceania and South East Asia.
Table 2. Income category (World Bank list of economies, 2010) of fellows and home countries by home region.
|
Income category |
||||||
|---|---|---|---|---|---|---|
| Home region | Total | Low | Lower middle | Upper middle | High non OECD | High OECD |
| Africa | 114/22a | 39/11 | 64/7 | 11/4 | — | — |
| East Asia | 67/2 | — | 67/2 | — | — | — |
| Eastern and Central Europe | 66/15 | — | 2/1 | 40/8 | 9/2 | 15/4 |
| Latin America | 107/17 | — | 25/6 | 82/11 | — | — |
| Middle Eastb | 20/7 | — | 12/4 | 7/2 | — | — |
| OSEA | 57/9 | 16/4 | 35/4 | 6/1 | — | — |
| Russia and CIS | 33/6 | — | 12/4 | 21/2 | — | — |
| South Asia | 81/5 | 14/2 | 67/3 | |||
| Total | 545/83 | 69/17 | 284/31 | 167/28 | 9/2 | 15/4 |
Abbreviations: CIS, Commonwealth of Independent States; OECD, Organisation for Economic Co-operation and Development; OSEA, Oceania and South East Asia.
Number of fellows/countries.
Palestinian authority was not considered by OECD table.
Fellows from the developing world have usually been trained in centers in North America, Europe, or Australia. In the past decade an increasing number of fellows from emerging countries have trained instead in host centers within their own region of the world (Table 1). There are several potential advantages to these intraregional fellowships (discussed below), which can usually provide training that is more relevant to the needs of the home institution and region. In the past 10 years, just over 25% of fellows trained in their own region, and their number is still increasing.
ASSESSING IMPACT
But does this Fellowship Program really accomplish its goals by making a difference to the fellow and to the practice of nephrology in his or her home unit and home country? Assessment of the impact of the Fellowship Program is essential, but difficult to perform. The definition of objective outcomes is not straightforward and the data from emerging countries often difficult to collect.
In an effort to steer the future development of the Fellowship Program and to evaluate the impact and benefits of the program on the career of ISN Fellows, a fellowship survey is conducted every 2 years. The most recent survey in 2010 was sent to 329 fellows from the past 10 years. Of these 226 (69%) returned the questionnaire, although not all of them answered all of the questions. In an attempt to increase the response rate of the answers, the survey was anonymous. The results of the 2010 survey are presented below.
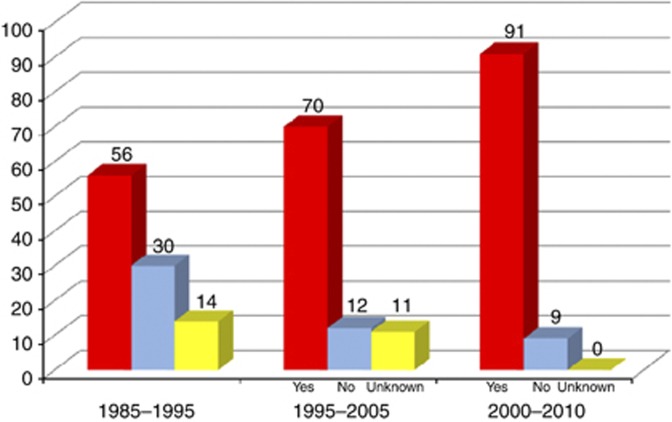
A major concern of any programs that require trainees to leave their home countries for training is that migration of physicians can lead to critical medical workforce shortages in developing countries if the trainees do not return.4, 5 To avoid ‘brain drain' and to ensure that the fellowship is of value to the home unit and country, and not just the fellow, it is a requirement of the ISN program that positions be guaranteed for them at home and that fellows return to their home unit within a few months of completing the fellowship. The fellowship stipend must be refunded and other benefits do not flow if fellows do not comply. These policies, and improving economic conditions in several countries, have led to a steady improvement in the number of fellows returning to their home units, from 56% in the first decade of the program to 70% in the second decade (1995–2005) and 91% in the past 10 years (Figure 1). Of the fellows who trained outside Europe or North America, 100% returned home. After returning, fellows are expected to remain in their home unit for at least 3 years. In the last survey of fellows trained in the period 2000–2010, 76% were still working in their home institution at the end of the survey period.
Figure 1.
Percentage of fellows re-employed by their home institution.
RELEVANCE OF FELLOWSHIP TO HOME INSTITUTION
In the 2010 survey 90% of fellows rated their training as having high or good relevance to the needs of their home institution or country, and 85% as having a high level or good impact on their home institution and home country (Figure 2). The ratings were similar in the previous 10-year survey.
Figure 2.
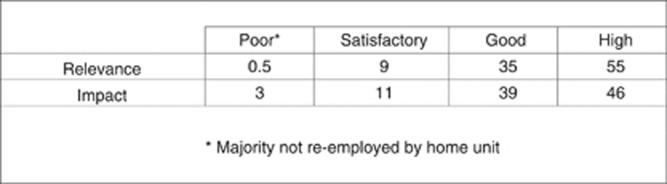
Self-reported outcomes (percentage) of fellowship on home institution/country (2000–2010).
Such a satisfactory outcome, albeit from a self-reported and incomplete survey, is somewhat surprising when looking at the activities undertaken during the training. The primary training activity in the last survey was laboratory research in 28% and clinical service as an observer only in 22%. Training activities which could be considered of more relevance included clinical service with direct patient contact in 23%, epidemiological research in 7%, and other clinical research in 10%. However, the discipline and some of the skills learned in laboratory research can be invaluable in clinical practice and clinical research. Moreover, in some developing countries at the cusp of becoming a developed country, training in laboratory research by one or two fellows was pivotal in establishing a relevant national or local basic research program. With an increase in intraregional fellowships (see below and Table 3), there is a greater opportunity for clinical service with direct patient contact rather than just an observership, where the host country shares the same language, religion and culture, and similar medical education system. Among fellows training in their own region, 49% undertook clinical service with direct patient contact, compared with 16% for those training outside their region (P<0.001 by chi-squared test).
Table 3. Comparison of fellowships undertaken within versus outside home region of the worlda.
| Easier visa application |
| More hands-on clinical training |
| Fewer publications, and none of high impact |
| Greater relevance and impact on home unit |
| Less ‘brain drain' |
Based on 2000–2010 survey.
Another valuable benefit of the fellowship is the continued interaction between the fellow and the host unit, which facilitates an ongoing clinical and/or research relationship after the fellowship has been completed. The importance of cementing what has been learned in the host institute by the fellow returning to a supervised home environment, where the skills can be applied, has been recognized in other training programs.6 Fellowships may be specifically designed to meet the future clinical needs of the home unit rather than just the individual fellow. For example, a home unit with no expertise in renal pathology may benefit from a fellowship structured to focus on the processing and interpretation of renal biopsy specimens.
POST-FELLOWSHIP ACCOMPLISHMENTS
In the past 10-year survey the fellows' substantive positions on returning home included clinical duties in 84%, teaching 75%, research 51%, and administration 19%. However, the full breadth of fellows' current activities was greater and included patient care in 89%, clinical research 80%, patient education and information 63%, renal disease registry 46%, epidemiology 42%, laboratory research 36%, and health planning 23%.
Of particular interest are data showing that within 10 years of completing their fellowship, 60% of responding fellows occupied a leadership position within their department or hospital, 28% within their country, and 7% at an international level. In all, 30% of fellows had been invited to deliver lectures overseas, particularly at national events and congresses; 34% had received national or international awards, mainly for conduct or presentation of clinical or basic research; 50% were involved in social contributions to renal health in medicine, including health awareness programs, interviews with media and setting up dialysis in rural areas; 72% of respondents maintained their ISN membership long term and 12% were involved in ISN committees within 10 years of completion of their fellowship. It has become apparent, as ISN continues to involve more members from developing world countries in its programs, that this decade's leaders in both internal medicine and nephrology are often past decade's ISN fellows, an important impact of the program that can be unappreciated from most survey data.
Of the 226 respondents in the latest survey, 152 answered questions about publications. Together there had been 395 publications directly related to the fellowship training and 2135 not directly related to the fellowship training, 54% of which were original articles. Of 188 articles directly related to the fellowship training, one-third were in journals ranked in the first six among the more than 60 kidney and urology journals, or top-rung general clinical or science journals. The mean rate per fellow of publications directly related to the fellowship was twice as high and all high impact publications arose, when fellowships were undertaken outside rather than within the fellow's home region.
FELLOWSHIP INFRASTRUCTURE
The largest single infrastructure problem, identified by 11% of 119 respondents, was difficulties arranging a visa. This reflects enhanced security concerns in the post 9/11 world and is another benefit of intraregional fellowship training. Although individual stipends, which were based on the socioeconomic level of the host country, were relatively modest, 78% of 122 respondents claimed that they had sufficient funds from the fellowship alone to cover basic living expenses. Practical information regarding the host country and unit was passed on to subsequent fellows.
LESSONS LEARNED
The ISN GO Fellowship program is the largest and oldest international subspecialty program in internal medicine dedicated to training physicians from developing countries to practice, and sometimes initiate, nephrology in emerging countries. Data collected from 25 years of the program indicate it has had a very positive impact on trainees, on host training institutions, and on home nephrology programs. Several lessons have been learned as the program has evolved and adapted to the current era. The role of local and regional committees in identifying both individual applicants and countries where fellowship training could have a major impact is essential to ensure effective regional allocation of resources when a single, centrally administered program serves countries in eight developing regions of the world. Stringent program requirements as well as changing economic conditions have largely resolved the problem of trainees not returning home and prevented the program from facilitating a ‘brain drain'. Increasing restrictions that preclude effective ‘hands on' clinical training in traditionally prominent training sites have been overcome by the initiation of intraregional training programs that allow training to occur in selected well-developed centers in the fellow's own region of the world. In addition to enabling more clinical training, these programs have also made training more relevant to the needs and cultural aspects of developing countries. Although the program initially emphasized basic research training, the focus has evolved to include more training in the skills of clinical research and facilitated the conduct of clinical research in emerging centers that often have access to large numbers of patients that can be enrolled in clinical studies. There is increasing appreciation of the benefit international fellows bring to host institutions, particularly when close contact is maintained between the fellow and the host center after training is completed, thus enhancing global health initiatives in many developed centers. The program has also had the unanticipated effect of identifying and training individuals who have later become leaders in both nephrology and internal medicine in their own institutions, countries, and regions, thus leveraging the training to have a positive impact beyond just subspecialty clinical service. Finally, it is clear that the success of the ISN fellowship program is due, in significant part, to the fact that the program does not exist in isolation but is closely linked to other outreach programs of the sponsoring society that offer opportunities for continuing educational enhancement and involvement after training utilizing other outreach programs such as the Sister Renal Centers, Research and Prevention grants, Continuing Medical Education events, and the Educational Ambassador program.
DCHH has received consulting fees from Amgen Australia. DCHH is also Chair of the ISN Publications and the ISN Education Committees. SD is Manager of ISN's Global Outreach programs and WGC is Chair of ISN's Global Outreach programs. JF is President of ISN.
Footnotes
TO CITE THIS ARTICLE: Harris DCH, Dupuis S, Couser WG et al. Training nephrologists from developing countries: does it have a positive impact? Kidney inter., Suppl. 2012; 2: 275–278.
References
- Couser WG, Feehally J, Rodriguez-Iturbe B. The International Society of Nephrology: what does ‘philanthropic' mean for members. Kidney Int. 2009;76:239–242. doi: 10.1038/ki.2009.228. [DOI] [PubMed] [Google Scholar]
- Weening JJ, Brenner BM, Dirks JH, et al. Toward global advancement of medicine: the International Society of Nephrology experience. Kidney Int. 1998;54:1017–1021. doi: 10.1046/j.1523-1755.1998.00057.x. [DOI] [PubMed] [Google Scholar]
- Godlee F. WHO fellowships—what do they achieve. Brit Med J. 1995;310:110–112. doi: 10.1136/bmj.310.6972.110a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdick WP, Morahan PS, Norcini JJ. Slowing the brain drain: FAIMER education programs. Med Teach. 2006;28:63104. doi: 10.1080/01421590600922883. [DOI] [PubMed] [Google Scholar]
- Senewiratne B. The emigration of doctors. A problem for the developing and the developed countries. Part II Brit Med J. 1975;1:669–671. doi: 10.1136/bmj.1.5959.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam F, Damji KF, Kiage D, et al. The Sandwich fellowship, a subspecialty training model for the developing world. Acad Med. 2009;84:1152–1160. doi: 10.1097/ACM.0b013e3181acf95c. [DOI] [PubMed] [Google Scholar]