Abstract
More than a quarter of human populations now suffer from hypertension paralleling the marked increase in the dietary intake of salt during the recent several decades. Despite overwhelming experimental and epidemiological evidence, some still debate the relation between salt and hypertension. Pointing to some conflicting data in a few flawed studies, they argue that policy interventions to reduce the dietary intake of salt are premature and maybe unsafe without further studies. A brief review of data relating salt intake to hypertension, along with an overview of the history of the introduction of salt to human diet on an historic and evolutionary time scale, should help dispel doubts on the effectiveness and safety of low-salt diet. The recorded history confirms how rare and inaccessible salt has been until recent times. Like all other terrestrial life forms, humans evolved in a salt-free environment under intense evolutionary pressure for the selection of salt-conserving genes. Hypertension is a prototypical evolutionary maladaptation disorder of the modern man—a species exquisitely well adapted to low salt conditions suddenly confronted with salt excess. The World Health Organization and many governments have finally taken action to reduce dietary intake of salt, which already has started to reduce the burden of hypertension and the associated cardiovascular morbidity and mortality. This brief review is to broadly look at the evidence linking salt to hypertension from a historic and evolutionary perspective as well as touching upon some of the epidemiological and experimental data.
Keywords: cardiovascular morbidity, evolutionary mismatch, hypertension, salt, selection pressure
During the recent several decades, the dietary intake of salt has steadily increased to up to 18 g per day worldwide, along with a marked increase in the prevalence of hypertension—more than 25% of adults aged ⩾25 years have hypertension globally. The World Health Organization has ranked hypertension as the leading cause of cardiovascular mortality, and citing the overwhelming evidence linking high salt intake to hypertension has urged member nations to take action to reduce dietary intake of salt to help decrease the number of deaths from heart disease and stroke (World Health Organization 2007).1, 2 Our understanding of the pathophysiology of hypertension clearly points to salt as a principal player in the genesis of hypertension, and there are abundant experimental and epidemiological data that confirm the beneficial effects of salt restriction on blood pressure. Despite the evidence, some in the academic and lay media dispute the benefits of salt restriction, pointing to inconsistent outcomes noted in some observational studies.3, 4 A broad review of the research data and the history of salt in human diet on historic and evolutionary time scales would help a better understanding of the strong link between salt and hypertension.
HISTORIC OVERVIEW
Salt played an important role in the recorded history of the world. The search for pure salt engaged humanity for millennia and influenced history in profound ways. Its preservative property allowed storage of food before refrigeration and had a momentous effect on history enabling transition from a hunter-gatherer to a settled lifestyle and established salt as a major economic commodity. Ancient Chinese texts describe two different methods to extract salt more than 2000 years ago, mention 40 different types of salt, and describe its uses in food preservation. The ancient Egyptians used it in mummification and preservation of food. Salt taxes were an important source of revenue for the ancient Chinese governments, and later many other governments around the world. Roman soldiers were issued their monthly pay as salt money, Latin salarium. In ancient Libya it was traded for equal weight of gold. Salt was taxed ruthlessly. The French salt tax, gabelle, may have incited the French revolution. It led to wars among nations, influenced the establishment of trade routes, such as the ancient Roman via salaria, which are the precursors of some of the modern highways in today's Italy. Many cities with salt mines derived their names from salt, for example, Salzburg, Hallstatt, Tuzla, and so on. Gandhi's 1930 Salt March in defiance of the British Salt Act was a pivotal moment in the Indian independence movement that ended the British rule in India. Thus, the recorded history documents that humans knew and valued, even revered salt, attaching sacred attributes to it for nearly 5000 years, because it was needed to preserve food, was extremely scarce, highly coveted, but out of the reach of ordinary people until recently.5, 6 The cheap purified table salt is a very recent and in many ways an unfortunate addition to human diet. It became widely available for less than two centuries only after modern geology helped identify abundant salt mines throughout the world and after it became possible to produce large quantities efficiently with the aid of modern technology.
EVOLUTIONARY BACKGROUND
The evolution of modern humans and our hominid ancestors took place in an environment virtually without any access to salt over a span of two million years.2, 6, 7 This is in fact true for most land-based animals stretching to several hundreds of millions of years in evolution.
For life forms that have originated in briny waters to free themselves from marine environment and transition to land environment, ability to carry ‘the sea within us' was critical.7 Thus, in the environment where humans and our distant ancestors evolved (the environment of adaptedness), there was intense and unrelenting selection pressure for genes and mechanisms that could preserve the very small quantities of salt available in natural diet—barely 0.25 g salt per day. Indeed, all genes identified to date with a link to blood pressure are associated with sodium transport.8 Without an efficient mechanism to preserve salt, its loss in bodily secretions would have fatal consequences as salt is an essential ingredient of our plasma volume. Owing to a physiology that has evolved over millions of years, all terrestrial animal life forms are exquisitely well adapted to salt scarcity and can survive without regular access to salt supplements unless faced with excessive salt losses, such as diarrhea or vomiting. All these life forms still exist successfully without access to added salt in their diet. Only humans have discovered salt as a dietary additive, and when thrust into salt surfeit conditions, as in the modern diet that contains 10–18 g or even more salt per day (50- to 70-fold higher than our natural Paleolithic diet), the consequences are high blood pressure, kidney failure, strokes, and heart disease.9, 10
Worldwide, the prevalence of hypertension has now reached 26% in parallel with the increased salt consumption in the modern diet. There is also evidence linking high-salt diet to higher risk of obesity through greater consumption of sugared drinks, stomach cancer, kidney stones, and osteoporosis.11 High salt intake is clearly linked to increased salt and water retention, increased glomerular filtration, and a blunted pressure natriuresis response—physiologic processes that favor hypertension. This is what evolutionary medicine characterizes as evolutionary mismatch, and hypertension a prototypical maladaptation disorder.9, 10
Observations in contemporary no-salt societies confirm not only the relation between salt and hypertension but also provide evidence of successful adaptation to salt-free environment during the evolution of the human species. For example, the Australian aborigines, the African Bushmen, or the Amazonian Yanomami had no access to salt in their diet until recently. Their total salt intake was found no more than what they could obtain from natural sources—based on the typical hunter–gatherer diet, which is only around 0.25 g per day. Hypertension is simply non-existent in such societies.12 Yet, when such communities are urbanized and exposed to the salty modern diet, they do suffer from hypertension and its complications, in some cases at disproportionately higher rates than the rest of the population.6, 12
EXPERIMENTAL EVIDENCE
The extraordinary experiments conducted in 1995 by Derek Denton in chimpanzees, our closest living evolutionary relatives, showed markedly that the chimpanzees placed on high-salt diet (12 g per day) developed hypertension, which reversed when they resumed their usual low-salt (0.25–0.5 g per day) diet.13 Numerous animal experiments confirm the role of salt in hypertension and some studies also suggest that excess salt may have harmful effects on cardiovascular health independent of hypertension. For example, one such study showed that in normotensive Wistar–Kyoto rats high salt intake resulted in deposition of fibrous tissue in the heart and kidneys despite only modest rises in their blood pressure, almost to the same extent seen in their hypertensive counterparts, spontaneously hypertensive rats.14
In the 1940s when there were no drugs available to treat hypertension, Walter Kempner treated hundreds of severely hypertensive patients on a strict low-salt (0.25 g per day) diet based on rice, fruit juices, and vitamins (Kempner's rice diet) for many weeks, some more than a year making this one of the longest salt restriction studies in the medical literature. Meticulous records kept by Dr Kempner document that the diet markedly improved blood pressure, reversed heart enlargement, improved kidney function, and also reversed the hypertensive changes in the retinal vasculature in these patients.15
More recent studies, although of shorter durations, confirmed that low-salt diet lowers blood pressure both in individuals with normal blood pressure and in patients with hypertension. Perhaps, the best known is the Dietary Approaches to Stop Hypertension (DASH) diet trial. This 12-week controlled trial showed that reducing dietary intake of salt from the ‘normal' (8 g per day) to intermediate (6 g), and low (4 g) lowered blood pressure among both hypertensive and normotensive individuals.16
EPIDEMIOLOGICAL STUDIES
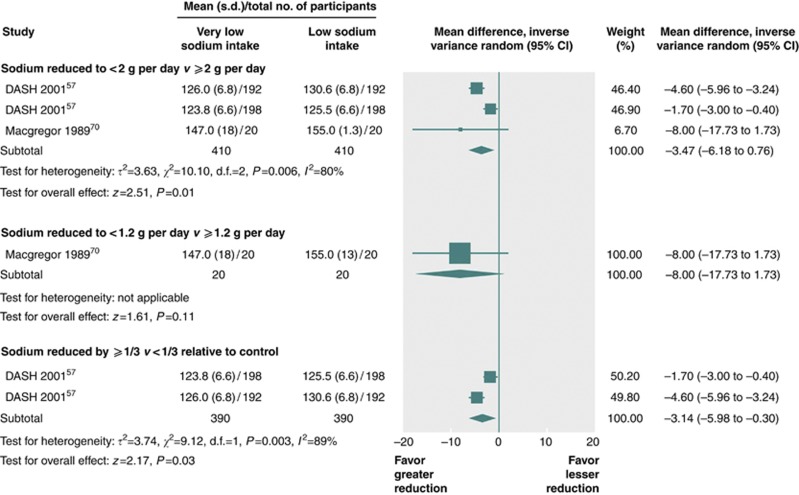
The recent Cochrane review17 and a comprehensive meta-analysis of data on the health effects of salt restriction documents convincingly the beneficial effects of salt in non-acutely ill adults, and also highlights the efficacy and safety of very-low–salt diet (Figure 1).18 This systematic review conducted by scientist from the World Health Organization's Nutrition Policy and Scientific Advice Unit concluded that, ‘evidence in non-acutely ill adults shows that reduced sodium intake reduces blood pressure and has no adverse effect on blood lipids, catecholamine levels, or renal function.'18 Lower sodium intake was also associated with a reduced risk of stroke and fatal coronary heart disease in adults. In this study, the totality of the evidence suggested that most people would benefit from reducing sodium intake.18 Consensus has now emerged among most hypertension experts that the beneficial effect of salt reduction starts at daily intake levels of 5 g or less, and the relatively high potassium content of low-salt diets may have additional beneficial effects on blood pressure.11, 18, 19 Evidence also suggests that for maximum benefit, salt reduction might need to be started early in life, and some of the cardiovascular effects of sustained high salt intake may be irreversible.2, 9
Figure 1.
Direct comparisons of effect of sodium intake of <2 versus >2 g per day, <1.2 versus >1.2 g per day, and a reduction by one-third or more versus less than one-third relative to control on systolic blood pressure in adults. The meta-analysis of three comparisons showed a significant decrease in systolic blood pressure by 3.47 mm Hg (0.76–6.18 mm Hg) and diastolic blood pressure by1.81 mm Hg (0.54–3.08 mm Hg) when sodium intake was <2 g per day compared with ⩾2 g per day. There was only one comparison of <1.2 versus ⩾1.2 g per day and it reported a nonsignificant decrease in systolic blood pressure of 8.00 mm Hg (−1.73 to 17.73 mm Hg) and diastolic blood pressure of 4.00 mm Hg (−1.58 to 9.58 mm Hg). When the relative reduction in sodium intake was one-third or more of control compared with less than one-third of control, the meta-analysis of two comparisons detected a significant decrease in systolic blood pressure by 3.14 mm Hg (0.30–5.98 mm Hg) and diastolic blood pressure by 1.70 mm Hg (0.33–3.07 mm Hg). Reproduced from ref. 18 Effect of lower sodium intake on health: systematic review and meta-analyses.346: f1326. ©2013 with permission from BMJ Publishing Group.
THE CONTROVERSY
Why then there is still a controversy and caution that reducing dietary intake may have unforeseen health hazards, and additional evidence is sought? The findings in some observational studies that show adverse cardiovascular outcomes in very low salt intake groups have been highlighted as an argument against recommending reduced salt intake to very low levels.3, 4 For example, the report by Stolarz-Skrzypek et al.20 attracted much attention for their finding of ‘a weak but consistent inverse association between cardiovascular mortality and the 24-h urinary sodium excretion at baseline.' The authors nevertheless noted that ‘systolic but not diastolic pressure change in parallel with urinary sodium excretion.' However, this observational study had too many limitations. First, long-term salt intake was estimated from a single 24-h urine collection for the duration of the study. Second, all patients with known hypertension and cardiovascular disease were excluded from the analysis, potentially biasing the conclusions in favor of the high salt intake tertiles, known to be associated with higher incidence of hypertension and cardiovascular disease. And thirdly, the finding of a cohort ingesting unusually low quantities of salt (107 mmol, or 6.3 g salt per 24 h) in a high-salt culture is not sufficiently explained.
The main risk is attributed to the expected activation of the renin–angiotensin–aldosterone system along with increased sympathetic nervous system activity,3 which are in fact activated to conserve sodium and prevent further sodium losses. These hormonal mechanisms are the precise tools that have emerged during the evolution of terrestrial life forms under pressure to conserve the miniscule quantities of salt intake that they had access to through their natural diet. This level of salt intake is compatible with normal physiology in animals as well as humans. Although controversial, the evidence suggests that increased renin–angiotensin–aldosterone system activity or sympathetic activity in the absence of high salt intake do not lead to adverse cardiac effects in healthy individuals, as has been observed in no-salt populations and similar to hypertensive patients on diuretics.12, 17 The danger is when these hormones cannot be shut off in patients who are on high salt intake, or have impaired salt balance because of heart, liver, or kidney disease. The adverse outcomes generally derive from unhealthy individuals who are salt-avid, such as patients with heart failure, who usually have very low sodium concentrations in urine, which are taken erroneously as representative of their salt intake.
The argument for caution on lowering salt intake further fails as these patients with impaired salt balance are often treated with natriuretic agents, that is, diuretics, for the explicit purpose of reducing their total body sodium. Although not openly stated, what these critics seem to suggest is that lowering total body sodium by using a diuretic drug is safer than reducing their salt intake! Worse outcomes in salt-avid populations cannot be explained by low dietary intake of salt, but are much more likely related to the seriousness of their pathophysiology that makes them salt-avid.
The meta-analysis by Aburto et al.18 is particularly valuable, because they restricted their analysis to high-quality studies that did not include sick patients, and showed that lowering salt intake below 1200 mg per day is beneficial and safe (Figure 1). Of note, the characterization of 1200 mg sodium (3 g salt) intake as very low is arbitrary and relative to the current conditions. Until approximately 150–200 years ago, the majority of the world's population did not have access to even this much salt in their diet. In no-salt populations, the average salt intake is barely 250–500 mg per day, and such populations can survive in good cardiovascular health without hypertension, and also without hypotension or hypovolemia.12 This is because the human kidney can conserve sodium very efficiently and the average urine sodium in such populations is usually very low (1–2 mmol per day). The relation between salt and hypertension should no longer be disputed. Both interventional and observational studies in non-acutely ill populations clearly show this.2, 17, 18, 19, 21 Our understanding of renal and cardiovascular physiology and its evolution in a salt-free environment are also sufficient evidence.
CONCLUSION
World governments faced with the economic burden caused by the ravages of hypertension and the associated cardiovascular morbidity have now started to take action. A worldwide campaign to reduce dietary salt intake to ∼5 g per day has been undertaken.11, 21 Finland and England have already reduced the amount of salt being consumed by a combined policy of getting the food industry to decrease the amount of salt added to foods, labeling the sodium content on food products, and increasing public awareness of the harmful effects of salt on health. A global approach is required to extend these measures to developing countries where approximately 80% of the world's hypertension-related disease burden exists. Experience has shown that even a modest reduction in salt intake can result in major improvements in public health and lead to cost reduction in health-care expenditures. A worldwide coalition, World Action on Salt and Health (WASH), has been launched recently (http://www.worldactiononsalt.c om), encouraging other countries and health-care professionals interested in hypertension, kidney, and heart diseases to join in this effort.21
Millions of years of the successful existence of ours and related species in a salt-free environment is sufficient proof that a low-salt diet is man's original and natural diet, is compatible with normal physiology, and is safe. The modern man while well adapted to low-salt diet is poorly equipped to cope with the salt surfeit imposed on him in recent times. The experimental data on the role of salt in hypertension are multifaceted and incontrovertible. The unnaturally high salt intake, an artifact of recent times, contributes to hypertension and to the increased cardiovascular morbidity and mortality caused by hypertension. Reducing daily salt intake to approximately 5 g per day (2 g sodium) or less helps lower blood pressure significantly and reduces the complications of hypertension. This is essentially a cost-free intervention that can help cut health-care expenditure and save millions of lives worldwide.2, 11, 22
Acknowledgments
This work was supported in part by the Dialysis Clinic, and Huberwald endowed chair.
VB is a recipient of a grant from the Paul Teschan Research Fund. Publication costs for this article were supported by the Turkish Society of Hypertension and Renal Diseases, a nonprofit national organization in Turkey. The contents of this article do not represent the views of the Department of Veterans Affairs or the United States Government.
References
- Cutler JA. Prevention of hypertension. Curr Opin Nephrol Hypertens. 1993;2:404–414. doi: 10.1097/00041552-199305000-00008. [DOI] [PubMed] [Google Scholar]
- He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009;23:363–384. doi: 10.1038/jhh.2008.144. [DOI] [PubMed] [Google Scholar]
- Alderman MH. Reducing dietary sodium: the case for caution. JAMA. 2010;303:448–449. doi: 10.1001/jama.2010.69. [DOI] [PubMed] [Google Scholar]
- Kolata G. No benefit seen in sharp limits on salt in diet. The New York Times. 14 May 2013.
- Kurlansky M. Salt: A World History. Penguin: New York, NY; 2003. [Google Scholar]
- MacGregor GA, de Wardener HE. Salt, Diet and Health. Neptune's Poisoned Chalice: The Origins of High Blood Pressure. Cambridge University Press: Cambridge, UK; 1998. [Google Scholar]
- Smith WH. From Fish To Philosopher. Little, Brown and Company: Boston, MA; 1953. [Google Scholar]
- Lifton RP, Gharavi AG, Geller DS. Molecular mechanisms of human hypertension. Cell. 2001;104:545–556. doi: 10.1016/s0092-8674(01)00241-0. [DOI] [PubMed] [Google Scholar]
- Tekol Y. Irreversible and reversible components in the genesis of hypertension by sodium chloride (salt) Med Hypotheses. 2008;70:255–259. doi: 10.1016/j.mehy.2007.06.007. [DOI] [PubMed] [Google Scholar]
- Kurokawa K, Okuda T. Genetic and non-genetic basis of essential hypertension: maladaptation of human civilization to high salt intake. Hypertens Res. 1998;21:67–71. doi: 10.1291/hypres.21.67. [DOI] [PubMed] [Google Scholar]
- Cappuccio FP.Cardiovascular and other effects of salt consumption Kidney inter Suppl 2013(this issue). [DOI] [PMC free article] [PubMed]
- Oliver WJ, Cohen EL, Neel JV. Blood pressure, sodium intake, and sodium related hormones in the Yanomamo Indians, a ‘no-salt' culture. Circulation. 1975;52:146–151. doi: 10.1161/01.cir.52.1.146. [DOI] [PubMed] [Google Scholar]
- Denton D, Weisinger R, Mundy NI, et al. The effect of increased salt intake on blood pressure of chimpanzees. Nat Med. 1995;1:1009–1016. doi: 10.1038/nm1095-1009. [DOI] [PubMed] [Google Scholar]
- Yu HC, Burrel LM, Black MJ, et al. Salt induces myocardial and renal fibrosis in normotensive and hypertensive rats. Circulation. 1998;98:2621–2628. doi: 10.1161/01.cir.98.23.2621. [DOI] [PubMed] [Google Scholar]
- Kempner W. Treatment of hypertensive vascular disease with rice diet. Arch Intern Med. 1974;133:758–790. [PubMed] [Google Scholar]
- Sacks FM, Svetkey LP, Vollmer WM, et al. DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. doi: 10.1136/bmj.f1325. [DOI] [PubMed] [Google Scholar]
- Aburto NJ, Ziolkovska A, Hooper L, et al. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. doi: 10.1136/bmj.f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio FP, Capewell S, Lincoln P, et al. Policy options to reduce population salt intake. BMJ. 2011;343:d4995. doi: 10.1136/bmj.d4995. [DOI] [PubMed] [Google Scholar]
- Stolarz-Skrzypek K, Kuznetsova T, Thijs L, et al. European Project on Genes in Hypertension (EPOGH) Investigators. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305:1777–1785. doi: 10.1001/jama.2011.574. [DOI] [PubMed] [Google Scholar]
- He FJ, Jenner KH, Macgregor GA. WASH—world action on salt and health. Kidney Int. 2010;78:745–753. doi: 10.1038/ki.2010.280. [DOI] [PubMed] [Google Scholar]
- Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362:590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]