Abstract
Pakistan is a low-resource country with a population of 185 million where expenditure on health is 1.3% of the gross national product. The estimated incidence of end-stage renal disease (ESRD) is 100 per million of the population. The paucity and high costs of renal replacement therapy render more than 90% of the ESRD population disenfranchised from replacement therapy. Our center, which is a government sector organization, established as an integrated dialysis and living related renal transplant program in the 1980s, where all services were provided free of cost to all patients with life-long follow-up care including medications. The model was based on a concept of community/government partnership where the contributions to funds vary between 40% and 60% for each partner. The model has been self sustaining for 25 years, with an annual budget of $28 million in 2010. Presently, over 600 patients are dialyzed each day and each week, 7–10 patients have received live related transplants. The overall 1- and 5-year graft survival rate of 3150 transplants is 92% and 85%, respectively. Free dialysis and transplantation established our institute as a focus of transplantation in the country. This model therefore allowed the institute to have a vital role in the campaign against transplant tourism and in the promulgation of the transplant law. It shows that in low-resource countries, specialized centers in the government sector can, with community support, provide high-quality ESRD care to the disenfranchised population.
Keywords: developing country, model, transplant
INTRODUCTION
Pakistan is classified as a low-resource country according to the human development index (HDI).1 It has a population of 185 million with an HDI rank of 125 out of 169 countries. The gross national product (GNP) is $2335 per capita, literacy rate is 50%, access to safe water 90%, sanitation 59%, expenditure on education 2.9% of the gross domestic product and health 1.3% of GNP of which 1.8% is private healthcare.1 In terms of kidney diseases, the estimated incidence of end-stage renal disease (ESRD) is 100 per million population (pmp). Dialysis and transplantation is offered both in government and private sectors. There are 180 dialysis centers: 63 (35%) supported by government, 82 (46%) in private clinics, and 35 (19%) are supported by community. There are 30 transplant centers: 9 (30%) in government sector and the rest in the private sector.2 The estimated number of qualified nephrologists is 0.5 pmp and that of transplant surgeons 0.2 pmp. Dialysis and transplantation in the government sector, although free, has limited facilities; whereas in the private sector, dialysis costs $20–25 per session and transplant surgery between $600–10,000. This backdrop of economic deprivation and scarce facilities renders over 90% of the ESRD population disenfranchised from renal replacement where only 10% receive dialysis and <5% transplantation.3 Our institute, a public sector organization, became aware of this economic reality and established a model 25 years ago for free dialysis and transplantation for the disenfranchised.
A MODEL FOR DIALYSIS AND TRANSPLANT FOR LOW-RESOURCE COUNTRIES
A model was developed based on the concept of community/government partnership where dialysis and transplantation were integrated and all services were offered free of cost with life-long follow-up and medications.3 The institute's strict policy is to perform living related donor transplants, the only exceptions being spousal transplants and deceased donors. Recipients and donors have dedicated follow-up clinics where all treatment is provided free of cost including medicines.3, 4 Our transplant policy since inception in 1986 was based on the lines and spirit of the Istanbul Declaration of which we became a key supporter and signatory from its declaration in 2008. The government and community contribution for funds varies between 40% and 60%. The guiding principles of the model are equity, transparency, accountability to its supporting organizations, to remain at the cutting edge of technology, and to provide the best possible care to patients, where the follow-up is life-long, including investigations and medicines. Over the years, the institute has developed all of its facilities under one roof as the need arose to include urology, nephrology, gastrointestinal, and hepatobiliary, transplantation, laboratory medicine, radiology, social sciences and consulting services.
FUNDING THE PROGRAM
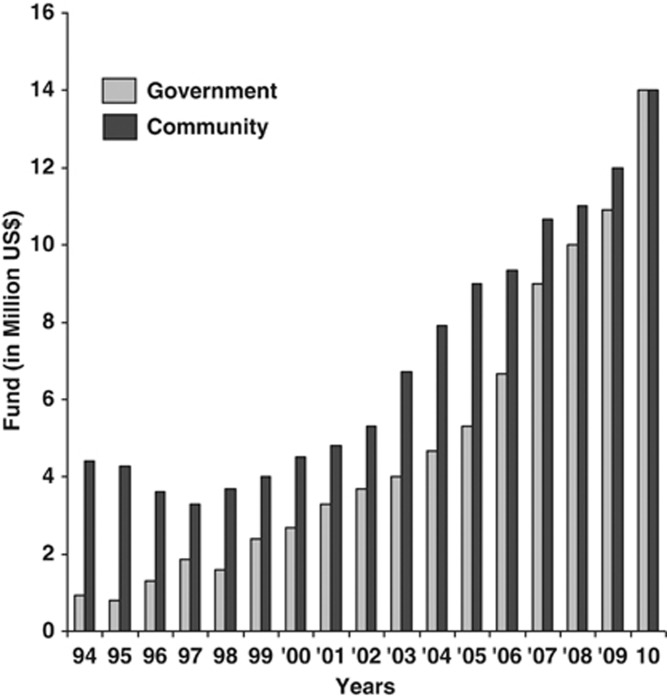
The development of the partnership was gradual. Initially, the government provided the infrastructure, e.g., building, utilities, equipment, and staff salaries. The community was asked to donate in kind or cash to support functioning of the services. Increasing patient volumes required more funds for medicines and other essentials for dialysis and transplantation. To raise funds, a number of community-based schemes were launched, e.g., support a patient scheme for dialysis or transplant, sponsor an equipment scheme, e.g., a dialysis machine or a CT scan, and sponsor a unit scheme, e.g., a 20 machine dialysis center for hepatitis B-antigen positive patients, a six-storey dialysis and transplant center worth $5 million.3 In the last 10 years, these schemes have generated a total sum of $28 million with $3 million from patient schemes, $12 million from equipment scheme and $13 million from unit schemes. The government has also increased its share from $0.5 million in 1992 to $14 million in 2010, constituting 50% of the annual budget of $28 million.3 The contribution of government and community funding is shown in Figure 1.
Figure 1.
Community government partnership.
IMPACT OF THE MODEL ON PATIENT SERVICES
The institute offers comprehensive urology, nephrology, dialysis, gastrointestinal and hepatobiliary and renal transplantation services. The growth of services in the last 10 years is shown in Table 1. The causes of ESRD remain unknown in 50% of the patients. Major known causes are chronic glomerulonephritis in 16%, hypertension in 9%, stone disease in 8.9%, diabetic nephropathy in 1.5%, reflux nephropathy in 2% and congenital abnormalities of kidney and urinary tract in 3%. The number of patients on dialysis and the number of renal transplants have increased over the years (Figure 2). Presently, over 600 patients are dialyzed each day, whereas 544 transplants were performed in 2009 and 358 in 2010. The number of transplants fell in 2010 due to the increasing number of patients on dialysis who either were or became untransplantable. Of the total of 1268 patients on regular dialysis, 244 (19%) were Hepatitis C virus positive and undergoing variable periods of time on interferon treatment, 312 (25%) had medical and surgical comorbidities, and 190 (15%) either had no donors in the family or were too old to undergo transplantation. To increase the capacity of dialysis beyond 600 patients per day, two new centers were opened in 2010. A 16-bedded dialysis center in the city of Sukkur 500 km from Karachi and a satellite unit of 16 machines within the city of Karachi. Patients who cannot be transplanted are being transferred to these new centers to accommodate new transplantable patients. Of the 3150 transplants performed up until 2010, 426 (13.5%) were pediatric transplants.
Table 1. Growth of services at SIUT (1998–2010).
| Parameters | 1998 | 2010 |
|---|---|---|
| No. of patients | 136,000 | 691,010 |
| Outpatients | 49,033 | 189,660 |
| Inpatients | 5378 | 34,065 |
| Emergency | 13,451 | 89,064 |
| Minor and major surgical procedures | 17,881 | 60,910 |
| Lithotripsy sessions | 2508 | 4138 |
| Dialysis sessions | 42,470 | 163,915 |
| Transplants | 99 | 358 |
| Radiology tests | 15,416 | 180,567 |
| Laboratory investigations | 500,000 | 5,594,513 |
| Medical expenditure | $1.4 million | $11 million |
| Total staff | 634 | 1351 |
Figure 2.
Increasing dialysis and transplant activity at the Institute.
Recipient demographic and follow-up
The mean age of the recipients was 29.5±10.36 years with a male-to-female ratio of 3.1:1. Recipients after discharge are seen weekly for the first month, monthly for the next 6 months and thereafter 3 months or yearly depending on their place of residence. On an average, 70–80 patients are seen daily in the clinic. Immunosuppression is achieved by a triple drug regimen of Cyclosporine, Steroid and Azathioprine. Poorly matched (<2 antigens or mismatched at DR) transplants are given Tacrolimus, Steroid and Mycophenolate Mofetil. These patients and children (<13 years) are given induction therapy using Anti-thymocyte globulin (ATG) or an Interlukin 2 antagonist (IL-2). Anti-rejection therapy comprises steroid bolus or ATG. All graft dysfunction episodes are evaluated by drug levels, color Doppler sonography and graft biopsy. The overall 1- and 5-year graft survival rates are 92% and 85% and patient survival rates are 96% and 90%, respectively. Overall, 1- and 5-year pediatric graft survival rates are 93% and 78% and patient survival are 97% and 88%, respectively. The overall acute rejection rate is 14%.
DONOR DEMOGRAPHICS AND FOLLOW-UP
The mean age of donors was 34.9±10.6 years with a male-to-female ratio of 1.25:1.0. Of the total 3150 donors, 266 (8.4%) were spousal, 30 (0.95%) were deceased donors, 1692 (54%) were siblings, 189 (6%) were child-to-parent, 861 (27%) were parent-to-child, and others 112 (3.5%) were close blood relatives. All donors are selected by an Evaluation Committee comprising physicians, surgeons, immunologists, medical social workers and two distinguished citizens. The relationship is established by National Identity Card, birth and marriage certificates and tissue typing for Class I and II and where needed extended typing for HLA-DQ and microsatellite analysis. Tissue typing for Class I antigen is performed by 120 antisera trays from Collaborative Transplant Study (CTS) and by PCR using sequence-specific primers for both class I and II (CTS). For HLA-A 24 primers and HLA-B 48 primers, HLA-DR 24 primers and HLA-DQ 48 primer from CTS. HLA antibody screen includes serological cross match and panel-reactive antibody. Flow cross match for T and B cells and Elisa for Class I, II and Mica antibodies by Luminex.
In low-resource settings, where transplant activity is low and the society is not committed to transplantation, living donor well-being is of extreme importance, especially when deceased donation is not established. This fact made it necessary to follow-up each donor on a long-term basis. The large number of donors in regular follow-up led to the initiation of a donor clinic in 2000.4 All donors are followed up at 3 and 6 months and thereafter yearly. At each visit, tests are undertaken for renal function, lipids, diabetes, and 24-h urine collection for protein and creatinine clearance. Intervention is undertaken wherever needed and any necessary drugs are provided. There are 2750 donors in regular follow-up with a mean creatinine clearance (ml/min) of 84±22 and 82±024 at 5 and 10 years and 24-h protein excretion (mg/24 h) of 138±304 and 158±443 at 5 and 10 years. One donor who went into renal failure 12 years after donation later received a live related transplant.
Many of the recipients and donors come from other cities for follow-up. Patients in remote areas and other cities have designated physicians who look after them with medical and laboratory follow-up. In emergency situations, military hospitals provide logistic support. For patients who cannot afford to pay for their care, arrangements are made within the city to accommodate them and those in need are provided travel expenses. The most important aspect is that all post transplant drugs including immunosuppressants are provided to the patients for as long as they need them. In this modern era, all recipients from far-off areas are in contact via mobile phones and in many situations phones are also provided to the patients.
REHABILITATION PROGRAM
The institute runs a rehabilitation center for transplant recipients. A vocational training program is run for patients, which is open to all who wish to avail themselves of the facility. In special cases where they cannot return to their professions, e.g., sanitary workers, heavy-duty work etc., the institute provides vocational training or financial support. Female patients are given training in tailoring, dress designing, and beautician courses, whereas male patients are given training in tailoring and computing. Financial support is given on both merit and needs basis especially to those who have lost their jobs. Financial support is given to establish small businesses, e.g., home beauty parlors, tailor shops, vegetable and fruit stalls. Recipients and donors are given employment in the institute whenever possible. Offers are made on merit to those who fulfill the criteria for any vacant position. Presently, over 250 recipients and donors are involved in this scheme. To highlight physical rehabilitation, the institute sends teams to the transplant games internationally and organizes its own local version of the games. Pediatric patients are helped to go back to school and provided support to catch up on lost studies in private tuition centers. Children are helped with purchase of books, uniforms, and in some cases, the tuition fees of school.
SUSTAINABILITY OF MODEL
The model has been operative for the last 25 years with the increasing support of the community government and society at large. The most important achievement is that society has taken up the ownership of the model, such that transparency of services, equity in treatment and state-of-the-art facilities have made the institute the premier transplant center of the country. One of the strategies employed for sustainability is that of cost reduction without compromising patient care. In dialysis, the use of simple machines, dialyzer reuse, in-house preparation of dialysis fluid and operation of machines round the clock has led to economies of scale with resultant savings of over $2.0 million/year. Use of generic immunosuppressants reduces the costs by up to 35% with an annual saving of over $1.8 million.5 In recent years, with the promulgation of a national transplant law, which prohibits unrelated commercial transplants, overall activity was reduced in the country. The increasing burden of dialysis together with patients coming to our center from all over Pakistan necessitated an increase of transplant activity at our center. The transplant rate increased from 2–3/week to 10–12/week in 2007. Economies of scale reduced transplant costs with immunosuppressive drugs for 1 year from $7876 to $5245 with annual savings in excess of $1.5 million.3
IMPACT OF THE MODEL ON TRANSPLANTATION ACTIVITY IN PAKISTAN
The institute has helped establish transplantation as a successful mode of therapy in the country. The donor follow-up clinic had a vital role in establishing donor well–being, which has resulted in a reduction of refusal rates within families from 60% in the early period to <15% in 2010. International recognition of the institute and its free services led to the first deceased donor transplantation in 1994, when one kidney was gifted by the Euro transplant Foundation.6 This brought about awareness of deceased organ donation in the country and to date 26 kidneys have been received from the Euro transplant Foundation. The first local deceased donor transplants were performed at the institute in 1998 and up until 2010, five deceased donations have taken place in the country.
One of the important roles of the institute has been its efforts to prohibit unrelated commercial transplants and ‘transplant tourism'. The institute held several conferences in the country in collaboration with the World Health Organization and The Transplantation Society to highlight the problem of transplant tourism and the sale of kidneys. It helped frame the transplant law and struggled in the parliament and courts till finally in 2007 the Transplantation of Tissue and Organ Ordinance was promulgated and the bill became law in 2010, where it was passed unanimously by the two houses of Parliament.7 Institute teams undertook studies on vendors in the province of Punjab and published findings on their poor socio-economic status and compromised renal function.8, 9 Post law, the institute also helped to maintain transplant activity in the country by increasing its transplant rate by 2–3/week to 10–12/week thereby performing over 1000 transplants in the 2008 and 2009 period.
Transplantation with regular follow-up of recipients and donors has provided opportunities for clinical and also basic science research. The institute has regularly published its experiences in transplantation.10, 11, 12 A number of research projects are in progress including; noninvasive markers for rejection;13 genetic markers for rejection; urinary markers of rejection by evaluation of the urine from the donor kidney just before devascularization, at nephrectomy, and after reanastomosis in the recipient at different time intervals; donor follow-up with special emphasis on intervention; the role of post-transplant HLA antibodies in chronic rejection, and post-transplant tuberculosis.14
CONCLUSIONS
In low-resource settings, for transplantation to be accepted as a successful mode of therapy, it has to be made available to the common man. The model has been sustained for over 25 years and the numbers of those who have benefitted continue to grow. Our graft outcomes for living donors are comparable to or better than other regional centers in Asia where overall graft survival rates range from 96% to 91% at 1 year and 87% to 68% at 5 years.15, 16, 17, 18, 19 The main reasons for our better outcomes are integrated dialysis and transplantation, presence of all facilities under one roof, optimal immunosuppression treatment, the ability to diagnose and treat graft dysfunction and above all, ‘free of cost' treatment with life-long follow-up for recipients and donors. We conclude that in our setting, it is important to develop specialized centers in the government sector, where the community can become involved in the support and care of ESRD patients.
Acknowledgments
We are grateful for the active cooperation and support of the SIUT team who have made this program possible for the last 25 years, and the generous support by the Pakistani community, which has sustained this model of free healthcare delivery. Publication of this article was supported in part by the National Health and Medical Research Council of Australia through an Australia Fellowship Award (no. 511081: theme Chronic Disease in High Risk Populations) to Dr Wendy Hoy, School of Medicine, the University of Queensland, and the National Institutes of Health – NIDDK DK079709, NCRR RR026138, and NIMHD MD000182.
All the authors declared no competing interests.
References
- Human development Report 2010 The Real Wealth of Nations: Pathways to Human Development United Nations Development Programme. UN Plaza, New York, USA; p199 [Google Scholar]
- Naqvi SAJ. Renal diseases in Pakistan – ‘Time to act'. J Nephrol Renal Transplant. 2009;2:133–135. [Google Scholar]
- Rizvi SAH, Naqvi SAA, Zafar MN, et al. A renal transplantation model for developing countries. Am J Transplant. 2011;11:2302–2307. doi: 10.1111/j.1600-6143.2011.03712.x. [DOI] [PubMed] [Google Scholar]
- Rizvi SAH, Naqiv SAA, Jawad F, et al. Living kidney donor follow-up in a dedicated clinic. Transplantation. 2005;79:1247–1251. doi: 10.1097/01.tp.0000161666.05236.97. [DOI] [PubMed] [Google Scholar]
- Rizvi SAH, Naqvi SAA, Zafar MN, et al. Living related renal transplants with lifelong follow-up. A model for the developing world. Clin Nephrology. 2010;74 (Suppl 1:S142–S149. doi: 10.5414/cnp74s142. [DOI] [PubMed] [Google Scholar]
- Naqvi A, Zafar N, Hashmi A, et al. Two cadaveric renal transplants in Pakistan from non-heart beating donors from Maastricht. Lancet. 1996;347:477–478. doi: 10.1016/s0140-6736(96)90059-8. [DOI] [PubMed] [Google Scholar]
- Bile KM, Qureshi JARH, Rizvi SAH, et al. Human organ and tissue transplantation in Pakistan: when a regulation makes a difference. East Med Health J. 2010;16 (Suppl:S159–S166. [PubMed] [Google Scholar]
- Naqvi SAA, Ali B, Mazhar F, et al. A socio-economic survey of kidney vendors in Pakistan. Transplant Int. 2007;20:934. doi: 10.1111/j.1432-2277.2007.00529.x. [DOI] [PubMed] [Google Scholar]
- Naqvi SAA, Rizvi SAH, Zafar MN, et al. Health status and renal function evaluation of kidney vendors. A report from Pakistan. Am J Transplant. 2008;8:1444. doi: 10.1111/j.1600-6143.2008.02265.x. [DOI] [PubMed] [Google Scholar]
- Rizvi SAH, Naqvi SAA, Zafar MN.Renal transplantation in PakistanIn: Cecka MJ and Terasaki PI (eds)Clinical Transplants UCLA Immonogenetics Center: Los Angels, USA; 2002191–200. [PubMed] [Google Scholar]
- Rizvi SAH, Naqvi SAA, Hussain Z, et al. Renal Transplantation in developing countries. Kidney Int. 2003;83 (Suppl:S96–100. doi: 10.1046/j.1523-1755.63.s83.20.x. [DOI] [PubMed] [Google Scholar]
- Rizvi SAH, Naqiv SAA, Zafar MN, et al. Pakistan abolishes kidney market and ushers in a new era of ethical transplantation. Int J Org Transplant Med. 2010;1:193–197. [PMC free article] [PubMed] [Google Scholar]
- Naqvi R, Jafri SB, Imani Z, et al. Urine immune profiling by measurement of multiple cytokine/chemokine mRNA levels in renal allograft dysfunction. Open J Immunol. 2011;1:87–96. [Google Scholar]
- Naqvi R, Naqvi A, Akhtar S, et al. Use of Isoniazid chemophylaxis in renal transplant recipients. Nephrol Dial Transplant. 2010;25:634–637. doi: 10.1093/ndt/gfp489. [DOI] [PubMed] [Google Scholar]
- Hashiani AA, Rajaeefard AR, Hassanzade J, et al. Graft survival rate of renal transplantation: a single center experience, (1999-2009) Iran Red Crescent Med J. 2011;13:392–397. [PMC free article] [PubMed] [Google Scholar]
- Torkaman M, Zadeh ZKM, Farahani MA, et al. Outcome of living kidney transplant: pediatric in comparison to adults. Transplant Proc. 2007;39:1088–1090. doi: 10.1016/j.transproceed.2007.03.090. [DOI] [PubMed] [Google Scholar]
- Chelluri LK, Vasantha A, Ratnakar KS. Impact of ethnicity, donor status and HLA matching on renal allograft survival: a single center study. Saudi J Kidney Dis Transpl. 2009;20:995–997. [PubMed] [Google Scholar]
- Shahbazian H, Hajiani E, Ehsanpour A. Patient and graft survival of kidney allograft recipients with minimal Hepatitis C virus infection: a case-control study. Urol J. 2008;5:178–183. [PubMed] [Google Scholar]
- Ali AAM, Abraham G, Khanna P, et al. Renal transplantation in the elderly: South Indian experience. Int Urol Nephrol. 2011;43:265–271. doi: 10.1007/s11255-010-9887-4. [DOI] [PubMed] [Google Scholar]