Abstract
Current therapies for acute kidney injury remain primarily supportive and have failed to reduce morbidity, mortality (>50%), and associated costs. This prompted our studies in which rats with bilateral ischemia/reperfusion-induced acute kidney injury were treated with bone marrow-derived, culture-expanded allogeneic mesenchymal stem cells. Their administration into the suprarenal aorta after reflow significantly protected renal function and hastened repair, mediated by complex antiapoptotic, mitogenic, anti-inflammatory, and immune modulating actions that were not elicited by isogeneic fibroblasts. Infused mesenchymal stem cells, recruited to renal sites of injury, did not significantly differentiate into target cells but rather disappeared from kidneys and other organs within 72 h. Furthermore, at 3 months, compared with vehicle-treated controls, renal function was well preserved and interstitial fibrosis was absent. These preclinical data served as the scientific basis for a recently completed Phase I Clinical Trial (http://www.clinicaltrials.gov; # NCT00733876), in which patients at high risk for cardiac surgery-associated AKI were treated with allogeneic mesenchymal stem cells. Until now, MSC therapy in the study subjects has been safe, and none of the patients has developed postoperative AKI or subsequent loss of renal function, suggesting that this novel form of therapy may have promise in this group of high-risk patients, which will be further investigated in a Phase II Trial.
Keywords: Bcl-2, cardiac surgery, chronic kidney disease, gene expression, paracrine actions, proinflammatory cytokines
Until now, no definitively effective treatment for the prevention of clinical acute renal failure or improved repair post-acute kidney injury (AKI) has been developed. Such effective therapy is, however, urgently needed because significant acute renal failure is associated with high morbidity and mortality rates, and substantial costs for required medical care.1 Importantly, even when renal function appears to fully recover after AKI, it is now recognized that a significant proportion of patients develop end-stage renal disease as a consequence of undiagnosed, incompletely resolved, or untreated AKI. This form of chronic kidney disease is characterized by continued inflammatory and fibrotic processes, and microvascular rarefaction.2 Consequently, those patients who seemingly recover from AKI frequently go on to develop chronic kidney disease, a significant percentage of these eventually requiring chronic hemodialysis or a renal transplant.2, 3
This continued therapeutic dilemma of AKI prompted us and others to investigate the potential therapeutic utility of adult bone marrow-derived mesenchymal stem cells, also termed multipotent stromal cells (MSCs).4, 5, 6, 7, 8, 9 Physiologically, these cells can differentiate into various mesenchymal cell types and support hematopoietic stem cells in the bone marrow niches. They are found in a pericyte location in all adult organs, as well as in adipose tissue and umbilical cord blood and tissue.10 MSCs can be readily obtained from the bone marrow and culture expanded. They differentiate into mesenchymal cell types (fat, bone, cartilage), do not express HLA-II (DR) and blood-group antigens, and secrete a large number of growth factors such as vascular endothelial growth factor, hepatocyte growth factor, insulin-like growth factor-I, and others.9, 11, 12, 13 Until now, MSCs have been safely and effectively used to treat children with osteogenesis imperfecta, patients with graft-versus-host disease, Crohn's disease, Hurler syndrome, poor bone marrow engraftment, poorly healing fractures, myocardial infarction, and other indications (http://www.clinicaltrials.org).14 In addition, a large number of preclinical studies have proven their therapeutic potential in models of the above diseases.
On the basis of this background, we hypothesized that the delivery of MSCs to rat kidneys with ischemia/reperfusion-induced AKI would favorably alter the subsequent outcome through their potential ability to differentiate into and replace destroyed renal cells. Our data demonstrated, however, that administered MSCs only temporarily reside in the injured kidneys, and that they function renoprotectively through paracrine antiapoptotic, mitogenic, anti-inflammatory, and immune modulating effects.6 We used the consistently positive results with this form of cell therapy as the scientific justification for a recently completed Phase I Clinical Trial in patients at particularly high risk for the development of AKI following on-pump cardiac surgery; that is, patients with underlying renal disease, diabetes mellitus, older age, congestive heart failure, hypertension, and chronic obstructive pulmonary disease.15, 16, 17
PRECLINICAL STUDIES: TREATMENT OF AKI WITH ALLOGENEIC MSCs
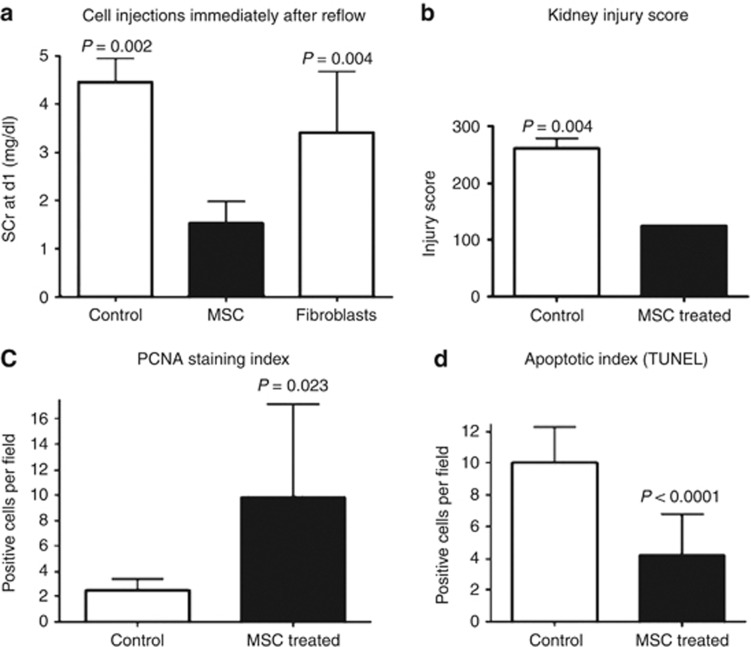
On the basis reports by several other investigators, the administration of MSCs, hematopoietic stem cells, or a bone marrow transplant, following myeloablation, to rodents with glycerol-, cis-platinum-, or ischemia/reperfusion-induced AKI, protected renal function and improved recovery, mediated, as was concluded, by significant engraftment of stem cells that had differentiated into tubular cells.4, 5, 18, 19 However, as differentiation of MSCs into renal cells requires several days, we questioned whether the prompt renoprotective effects of these cells, clearly observed by 12–24 h post-infusion and ischemic injury, was indeed the result of cell differentiation and engraftment. To investigate this issue further, we conducted a series of preclinical studies that are summarized in the following, and that formed the basis for a now completed Phase I Clinical Trial (http://www.clinicaltrials.gov; # NCT00733876). We tested whether the immediate or delayed administration, by 24 h, of syngeneic or allogeneic MSCs to rats with ischemia/reperfusion-induced AKI was safe and exerted significant renoprotective and repair-stimulating actions. The infusion of MSCs into the suprarenal aorta following induction of AKI was not associated with immediate adverse effects such as respiratory distress, deterioration in renal function, or animal death. Instead, as shown in Figure 1, MSC administration to rats with severe AKI significantly protected renal function at 24 h post-AKI and hastened functional recovery, whereas vehicle or isogeneic fibroblast infusion had no beneficial effects on outcomes.6, 7, 9 The fate of administered MSCs from male rats, rats transgenic for human placental alkaline phosphatase, MSCs loaded with various vital dyes, or iron sucrose microparticles in kidneys, was monitored in all major organs and the bone marrow using reverse transcriptase-polymerase chain reaction, in vivo two-photon laser confocal microscopy (O'Brien Center, University of Indiana), magnetic imaging resonance (University of Hamburg, Germany), immunohistochemistry, and in vivo tracking by bioluminescence detection of firefly luciferase-transfected MSCs.20, 21 Together, these studies clearly demonstrated that the organ-protective actions of infused MSCs were not mediated by early differentiation and subsequent engraftment in the injured kidney. Significantly, by 72 h post-AKI and MSC infusion, a time point when renal function was approaching baseline, although renal function in vehicle- or fibroblast-treated animals continued to deteriorate, no MSCs were detectable in kidneys and other organs. Very rarely, however, MSCs, transgenic for human placental alkaline phosphatase, had by day 7 intrarenally engrafted in an endothelial cell location, and an occasional human placental alkaline phosphatase transgenic MSC was detected by reverse transcriptase-polymerase chain reaction in the bone marrow.8, 9 The significance of these low-level intrarenal engraftments regarding recovery of renal function or fate in the bone marrow is not known. Of importance, however, is our observation that compared with vehicle-treated rats, at 1–3 months post-treatment of ischemia/reperfusion-induced AKI with MSCs, renal function remained normal, interstitial fibrosis was absent, and was associated with low expression levels of profibrotic genes (plasminogen activator inhibitor type I complexes, tissue inhibitors of metalloproteinase-1, transforming growth factor-β, connective tissue growth factor). In addition, MSC therapy prevented rarefaction of the microvascular density in the kidney that was seen in vehicle-treated animals. In these, there was progressive deterioration of renal function, associated with microvascular rarefaction, increased interstitial fibrosis, and upregulation of profibrotic genes.9, 13 MSCs delivered to and transiently present in the injured kidney, are located primarily in glomerular and in lesser numbers in peritubular capillaries. Adhesion in the microvasculature is mediated by upregulation of integrins and vascular cellular adhesion molecule-1 on both endothelial cells and MSCs.22 In addition, a fraction of MSCs is able to attach via their CXCR4 receptors to upregulated stromal-derived factor-1 in the injured kidney23 (see Togel et al., in this issue). When MSCs are administered into the suprarenal aorta, as was done in all our preclinical studies and in our Phase I Clinical Trial, no ectopic differentiation of MSCs into adipocytes or other mesenchymal cell types in the kidney or oncogenic transformation of administered cells is observed24 (see Kunter et al., in this issue).
Figure 1.
Treatment of severe acute renal failure (ARF) with syngeneic multipotent stromal cells (MSCs) or fibroblasts. (a) MSC administration immediately after reflow to animals with severe ARF (Fisher 344 rats) significantly improves renal function at 24 h after clamping, whereas vehicle- and fibroblast-treated animals show no such response. P=0.002, vehicle- versus MSC-treated animals; P=0.04, fibroblast- versus MSC-treated animals; P=0.05, vehicle- versus fibroblast-treated animals. (b) MSC administration significantly lowered cortical and outer medullary injury scores. (c) MSC-treated rats showed significantly higher numbers of proliferating cells, whereas it simultaneously reduced the number of apoptotic cells compared with controls. (d) PCNA, proliferating cell nuclear antigen; SCr, serum creatinine; TUNEL, terminal transferase-mediated dUTP nick-end labeling. Reproduced from Togel et al.,6 with permission from the American Physiological Society.
Further investigation into the renoprotective- and regeneration-enhancing mediator mechanisms elicited by MSCs in AKI showed that MSCs do not improve the early decrease in renal blood flow, but that they exert powerful antiapoptotic and mitogenic effects in the kidney, associated with robust downregulation of proinflammatory cytokines (interleukin-1β, tumor necrosis factor-α, interferon-γ) and upregulation of anti-inflammatory interleukin10 in renal cells. Associated with these actions is upregulation of antiapoptotic Bcl-2 and various growth factors such as basic fibroblast growth factor, transforming growth factor-α, hepatocyte growth factor, vascular endothelial growth factor, and others, all known to mediate renoprotection and organ repair.6, 13 Comparison of gene expression profiles between renoprotective MSCs and ineffective fibroblasts suggested that the mix of growth factors delivered by MSCs into the kidney was characterized by high expression levels of hepatocyte growth factor, insulin-like growth factor-I, vascular endothelial growth factor, stromal-derived factor-1, and other factors.11, 13 The individual importance of insulin-like growth factor-I in AKI therapy with MSCs was demonstrated by Imberti and colleagues,12 and see Imberti et al., in this issue. We have similarly shown that treatment of AKI with MSCs in which vascular endothelial growth factor was knocked down, using small interfering RNA technology, resulted in increased post-AKI mortality compared with treatment with wild-type MSCs, and resulted in significant rarefaction of the renal microvasculature.9, 13 Of additional importance in the use of allogeneic MSCs in animal models, as well as in clinical trials, is the fact that MSCs are hypoimmunogenic, suppress T-cell responses, and exert broad based immune modulating effects.11 These unique characteristics are due to the fact that MSCs do not express blood group and major histocompatibility complex-II antigens, as well as costimulatory factors, together making the use of allogeneic MSCs in humans safe, as has been shown in numerous ongoing clinical trials (http://www.clinicaltrials.gov; see Lange et al., in this issue).
In summary, the treatment of AKI in animals with isogeneic or allogeneic MSCs provides for a safe and highly effective intervention that is mediated by complex paracrine and endocrine mechanisms that can, in part, be reproduced by the intraperitoneal administration of MSC-conditioned media.25 Together, the body of these preclinical data formed the basis for our Phase I Clinical Trial, in which allogeneic MSCs were administered to patients who were at high risk for open-heart surgery-associated AKI.
PHASE I CLINICAL TRIAL: PREVENTION AND TREATMENT OF AKI WITH ALLOGENEIC MSCs
In this safety and feasibility trial, adult subjects who have undergone on-pump coronary artery bypass graft and/or cardiac valve surgery were infused via the suprarenal aorta with allogeneic MSCs, using a dose-escalating protocol. All studied subjects presented with the following risk factors for post-cardiac surgery-associated AKI: underlying chronic kidney disease-1 to 4, congestive heart failure, diabetes mellitus, hypertension, chronic obstructive pulmonary disease, and age >65 years.15, 16, 17, 26 Preliminary analysis of the outcomes in this cohort of study subjects showed that the suprarenal, postoperative administration of allogeneic MSCs is feasible and safe, as it has not resulted in adverse or serious adverse events, and preliminary efficacy data appear promising, showing, compared with well-matched historical case controls from the same institution, that MSC therapy prevented postoperative deterioration in renal function (∼20% AKI incidence in case controls), reduced length of stay (by ∼40%), need for readmission (by ∼40%), and prevented late deterioration in renal function, outcomes that closely parallel those obtained in our preclinical studies. Of note is the fact that these initial clinical observations provide post hoc validation of the relevance of the experimental models we used in our preclinical studies. After the completion of this Phase I trial, and if late safety is documented in all studied subjects, a double-blind, controlled, multicenter Phase II efficacy trial will be conducted.
In conclusion, the hypoimmunogenic and immune modulating characteristics make the safe, off-the-shelf use of allogeneic MSCs in patients possible and safe. The very short time that MSCs remain in the acutely injured kidney and other major organs, their paracrine and endocrine modes of action, and the absence of their ectopic differentiation and oncogenic transformation further underscore the safety of this novel from of therapy. Although only limited or no published data are currently available, Phase I/II clinical trails in which MSCs are to be administered to kidney recipients from living, unrelated donors, to patients with chronic allograft nephropathy, and individuals with lupus nephritis, are currently being conducted at the Organ Transplant Institute of China, Fuzhou General Hospital. In addition, MSCs are tested for the treatment of kidney transplant rejection at Leiden University, The Netherlands (http://www.clinicaltrials.com).
Acknowledgments
This work was in part supported by funds from the VA Central Office Merit Review Program, the National Kidney Foundation (UT, ID), the American Heart Association (Western Affiliate), the National Institutes of Health, the Western Institute of Biomedical Research, and Allocure.
CW served as consultant to Allocure, which provided support for the Phase I Clinical Trial discussed in this paper. FET declared no competing interests.
Footnotes
TO CITE THIS ARTICLE: Westenfelder C, Togel FE. Protective actions of administered mesenchymal stem cells in acute kidney injury: relevance to clinical trials. Kidney inter., Suppl. 2011; 1: 103–106.
References
- Chertow GM, Burdick E, Honour M, et al. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16:3365–3370. doi: 10.1681/ASN.2004090740. [DOI] [PubMed] [Google Scholar]
- Goldberg R, Dennen P. Long-term outcomes of acute kidney injury. Adv Chronic Kidney Dis. 2008;15:297–307. doi: 10.1053/j.ackd.2008.04.009. [DOI] [PubMed] [Google Scholar]
- Okusa MD, Chertow GM, Portilla D. The nexus of acute kidney injury, chronic kidney disease, and World Kidney Day 2009. Clin J Am Soc Nephrol. 2009;4:520–522. doi: 10.2215/CJN.06711208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morigi M, Imberti B, Zoja C, et al. Mesenchymal stem cells are renotropic, helping to repair the kidney and improve function in acute renal failure. J Am Soc Nephrol. 2004;15:1794–1804. doi: 10.1097/01.asn.0000128974.07460.34. [DOI] [PubMed] [Google Scholar]
- Herrera MB, Bussolati B, Bruno S, et al. Mesenchymal stem cells contribute to the renal repair of acute tubular epithelial injury. Int J Mol Med. 2004;14:1035–1041. [PubMed] [Google Scholar]
- Togel F, Hu Z, Weiss K, et al. Administered mesenchymal stem cells protect against ischemic acute renal failure through differentiation-independent mechanisms. Am J Physiol Renal Physiol. 2005;289:F31–F42. doi: 10.1152/ajprenal.00007.2005. [DOI] [PubMed] [Google Scholar]
- Lange C, Togel F, Ittrich H, et al. Administered mesenchymal stem cells enhance recovery from ischemia/reperfusion-induced acute renal failure in rats. Kidney Int. 2005;68:1613–1617. doi: 10.1111/j.1523-1755.2005.00573.x. [DOI] [PubMed] [Google Scholar]
- Togel F, Weiss K, Yang Y, et al. Vasculotropic, paracrine actions of infused mesenchymal stem cells are important to the recovery from acute kidney injury. Am J Physiol Renal Physiol. 2007;292:F1626–F1635. doi: 10.1152/ajprenal.00339.2006. [DOI] [PubMed] [Google Scholar]
- Togel F, Cohen A, Zhang P, et al. Autologous and allogeneic marrow stromal cells are safe and effective for the treatment of acute kidney injury. Stem Cells Dev. 2009;18:475–485. doi: 10.1089/scd.2008.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- Humphreys BD, Bonventre JV. Mesenchymal stem cells in acute kidney injury. Annu Rev Med. 2008;59:311–325. doi: 10.1146/annurev.med.59.061506.154239. [DOI] [PubMed] [Google Scholar]
- Imberti B, Morigi M, Tomasoni S, et al. Insulin-like growth factor-1 sustains stem cell mediated renal repair. J Am Soc Nephrol. 2007;18:2921–2928. doi: 10.1681/ASN.2006121318. [DOI] [PubMed] [Google Scholar]
- Togel F, Zhang P, Hu Z, et al. VEGF is a mediator of the renoprotective effects of multipotent marrow stromal cells in acute kidney injury. J Cell Mol Med. 2009;13:2109–2114. doi: 10.1111/j.1582-4934.2008.00641.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Togel F, Westenfelder C. Adult bone marrow-derived stem cells for organ regeneration and repair. Dev Dyn. 2007;236:3321–3331. doi: 10.1002/dvdy.21258. [DOI] [PubMed] [Google Scholar]
- Lassnigg A, Schmidlin D, Mouhieddine M, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol. 2004;15:1597–1605. doi: 10.1097/01.asn.0000130340.93930.dd. [DOI] [PubMed] [Google Scholar]
- Loef BG, Epema AH, Smilde TD, et al. Immediate postoperative renal function deterioration in cardiac surgical patients predicts in-hospital mortality and long-term survival. J Am Soc Nephrol. 2005;16:195–200. doi: 10.1681/ASN.2003100875. [DOI] [PubMed] [Google Scholar]
- Rosner MH, Portilla D, Okusa MD. Cardiac surgery as a cause of acute kidney injury: pathogenesis and potential therapies. J Intensive Care Med. 2008;23:3–18. doi: 10.1177/0885066607309998. [DOI] [PubMed] [Google Scholar]
- Kale S, Karihaloo A, Clark PR, et al. Bone marrow stem cells contribute to repair of the ischemically injured renal tubule. J Clin Invest. 2003;112:42–49. doi: 10.1172/JCI17856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin F, Cordes K, Li L, et al. Hematopoietic stem cells contribute to the regeneration of renal tubules after renal ischemia-reperfusion injury in mice. J Am Soc Nephrol. 2003;14:1188–1199. doi: 10.1097/01.asn.0000061595.28546.a0. [DOI] [PubMed] [Google Scholar]
- Ittrich H, Lange C, Togel F, et al. In vivo magnetic resonance imaging of iron oxide-labeled, arterially-injected mesenchymal stem cells in kidneys of rats with acute ischemic kidney injury: detection and monitoring at 3T. J Magn Reson Imaging. 2007;25:1179–1191. doi: 10.1002/jmri.20925. [DOI] [PubMed] [Google Scholar]
- Togel F, Yang Y, Zhang P, et al. Bioluminescence imaging to monitor the in vivo distribution of administered mesenchymal stem cells in acute kidney injury. Am J Physiol Renal Physiol. 2008;295:F315–F321. doi: 10.1152/ajprenal.00098.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooke G, Tong H, Levesque JP, et al. Molecular trafficking mechanisms of multipotent mesenchymal stem cells derived from human bone marrow and placenta. Stem Cells Dev. 2008;17:929–940. doi: 10.1089/scd.2007.0156. [DOI] [PubMed] [Google Scholar]
- Togel F, Isaac J, Hu Z, et al. Renal SDF-1 signals mobilization and homing of CXCR4-positive cells to the kidney after ischemic injury. Kidney Int. 2005;67:1772–1784. doi: 10.1111/j.1523-1755.2005.00275.x. [DOI] [PubMed] [Google Scholar]
- Kunter U, Rong S, Boor P, et al. Mesenchymal stem cells prevent progressive experimental renal failure but maldifferentiate into glomerular adipocytes. J Am Soc Nephrol. 2007;18:1754–1764. doi: 10.1681/ASN.2007010044. [DOI] [PubMed] [Google Scholar]
- Bi B, Schmitt R, Israilova M, et al. Stromal cells protect against acute tubular injury via an endocrine effect. J Am Soc Nephrol. 2007;18:2486–2496. doi: 10.1681/ASN.2007020140. [DOI] [PubMed] [Google Scholar]
- Lassnigg A, Schmid ER, Hiesmayr M, et al. Impact of minimal increases in serum creatinine on outcome in patients after cardiothoracic surgery: do we have to revise current definitions of acute renal failure. Crit Care Med. 2008;36:1129–1137. doi: 10.1097/CCM.0b013e318169181a. [DOI] [PubMed] [Google Scholar]