Chapter 5.1: Timing of renal replacement therapy in AKI
Whether or not to provide RRT, and when to start, are two of the fundamental questions facing nephrologists and intensive-care practitioners in most cases of severe AKI. In recent publications, the timing of initiation of RRT was listed as one of the top priorities in research on AKI.524 However, this dimension has not been included as a factor in any of the large RCTs in this area. The optimal timing of dialysis for AKI is not defined. In current practice, the decision to start RRT is based most often on clinical features of volume overload and biochemical features of solute imbalance (azotemia, hyperkalemia, severe acidosis). However, in the absence of these factors there is generally a tendency to avoid dialysis as long as possible, a thought process that reflects the decisions made for patients with CKD Stage 5.
Clinicians tend to delay RRT when they suspect that patients may recover on their own, and because of concern for the well-known risks associated with the RRT procedure, including hypotension, arrhythmia, membrane bioincompatibility, and complications of vascular access and anticoagulant administration. There is also some concern that RRT may compromise recovery of renal function, and increase the progression of CKD.525 Whether these risks outweigh the potential benefits of earlier initiation of RRT is still unclear.
5.1.1: Initiate RRT emergently when life-threatening changes in fluid, electrolyte, and acid-base balance exist. (Not Graded)
5.1.2: Consider the broader clinical context, the presence of conditions that can be modified with RRT, and trends of laboratory tests—rather than single BUN and creatinine thresholds alone—when making the decision to start RRT. (Not Graded)
RATIONALE
While no RCTs exist for dialysis for life-threatening indications, it is widely accepted that patients with severe hyperkalemia, severe acidosis, pulmonary edema, and uremic complications should be dialyzed emergently. In the absence of kidney function, and when therapeutic measures that promote the intracellular shift of potassium (such as correction of acidosis with bicarbonate, glucose and insulin infusion, and beta-2 agonists) are exhausted, an excess of potassium can only be eliminated with RRT. On the other hand, when intermittent dialysis is used after these therapeutic interventions, the extracorporeal removal of potassium will be reduced and the post-treatment rebound of serum potassium will be more pronounced.526
Metabolic acidosis is a frequent clinical problem in patients with severe AKI. Although the discussion as to when metabolic acidosis in critically ill patients should be corrected is outside the scope of this guideline, metabolic acidosis associated with AKI can usually be corrected with bicarbonate and should rarely require urgent dialysis if not accompanied by volume overload or uremia.527 As the pH and bicarbonate values to initiate dialysis for metabolic acidosis are not supported by evidence, no standard criteria for initiating dialysis for acidosis exist. A variety of poisons, drug overdoses, and toxic compounds (e.g., salicylates, ethylene glycol, methanol, metformin) can contribute to acid-base problems and also lead to AKI. In these circumstances, RRT may also facilitate removal of the offending drug.528, 529, 530
Only one RCT has evaluated the effect of timing of initiation of RRT on outcome. Bouman et al.531 randomized 106 critically ill patients with AKI to early vs. late initiation of RRT. The early initiation group started RRT within 12 hours of oliguria (<30 ml/h for 6 hours, not responding to diuretics or hemodynamic optimization), or CrCl <20 ml/min. The late-initiation group started RRT when classic indications were met. The study did not find differences in ICU or hospital mortality, or in renal recovery among survivors, but was clearly too small to allow for definitive conclusions (Suppl Table 30).
The remaining data come from observational studies. The association of early initiation of dialysis with survival benefit was first suggested by case series with historical controls conducted in the 1960 s and 1970 s.532, 533, 534, 535 In these studies, levels of blood urea or BUN were used to distinguish early vs. late start of dialysis. However, these studies mostly combined early start with more-intensive dialysis and late start with less-intensive dialysis. More recent studies have continued the trend focusing on BUN as a biomarker for starting RRT. Single-center observational studies that were restricted to AKI after trauma536 and coronary artery bypass surgery537, 538 suggested a benefit to RRT initiation at lower BUN concentrations. A prospective multicenter observational cohort study performed by the Program to Improve Care in Acute Renal Disease (PICARD) analyzed dialysis initiation—as inferred by BUN concentration—in 243 patients from five geographically and ethnically diverse clinical sites. Adjusting for age, hepatic failure, sepsis, thrombocytopenia, and SCr, and stratified by site and initial dialysis modality, initiation of RRT at higher BUN (>76 mg/dl [blood urea>27.1 mmol/l]) was associated with an increased risk of death (RR 1.85; 95% CI 1.16–2.96).539 In a prospective multicenter observational study conducted at 54 ICUs in 23 countries, timing of RRT was stratified into “early” or “late” by median urea at the time RRT started (24.2 mmol/l [BUN 67.8 mg/dl]), and also categorized temporally from ICU admission into early (less than 2 days), delayed (between 2–5 days), or late (more than 5 days). Timing by serum urea showed no significant difference in mortality. However, when timing was analyzed in relation to ICU admission, late RRT was associated with greater crude mortality (72.8% late vs. 62.3% delayed vs. 59% early, P=0.001) and covariate-adjusted mortality (OR 1.95; 95% CI 1.30–2.92; P=0.001). Overall, late RRT was associated with a longer duration of RRT and stay in hospital, and greater dialysis dependence.540 It is, however, not clear whether AKI occurring later in the course of ICU stay has the same pathophysiology and prognosis than AKI present on or early after admission. The most recent study on this subject is the analysis of surgical ICU patients with AKI, showing that late initiation of RRT (defined as RIFLE-I or -F) was an independent predictor of mortality (HR 1.846; CI 1.07–3.18).541
Traditional indications for RRT, developed for patients with advanced CKD, are not necessarily valid in the context of AKI. For instance, massive volume overload resulting from volume resuscitation may be an indication for RRT even in the absence of significant elevations in BUN or SCr. In this instance, it may be more appropriate to consider dialytic intervention in the ICU patient as a form of renal support rather than renal replacement. Indeed, some of the traditional indications for dialysis (e.g., uremic pericarditis, pleuritis, encephalopathy, coagulopathy) would be considered “complications” of AKI rather than indications for RRT. Additionally, the decision to start RRT should recognize the goals of therapy, keeping in mind the therapeutic potential of dialysis in general, and each dialysis modality in particular. The treatment of AKI with RRT has the following goals: i) to maintain fluid and electrolyte, acid-base, and solute homeostasis; ii) to prevent further insults to the kidney; iii) to permit renal recovery; and iv) to allow other supportive measures (e.g., antibiotics, nutrition support) to proceed without limitation or complication. Ideally, therapeutic interventions should be designed to achieve the above goals and a systematic assessment of all these factors is key to determining the optimal timing for initiating dialysis (Table 17).
Table 17. Potential applications for RRT.
| Applications | Comments |
|---|---|
| Renal replacement | This is the traditional, prevailing approach based on utilization of RRT when there is little or no residual kidney function. |
| Life-threatening indications | No trials to validate these criteria. |
| Hyperkalemia | Dialysis for hyperkalemia is effective in removing potassium; however, it requires frequent monitoring of potassium levels and adjustment of concurrent medical management to prevent relapses. |
| Acidemia | Metabolic acidosis due to AKI is often aggravated by the underlying condition. Correction of metabolic acidosis with RRT in these conditions depends on the underlying disease process. |
| Pulmonary edema | RRT is often utilized to prevent the need for ventilatory support; however, it is equally important to manage pulmonary edema in ventilated patients. |
| Uremic complications (pericarditis, bleeding, etc.) | In contemporary practice it is rare to wait to initiate RRT in AKI patients until there are uremic complications. |
| Nonemergent indications | |
| Solute control | BUN reflects factors not directly associated with kidney function, such as catabolic rate and volume status. |
| SCr is influenced by age, race, muscle mass, and catabolic rate, and by changes in its volume of distribution due to fluid administration or withdrawal. | |
| Fluid removal | Fluid overload is an important determinant of the timing of RRT initiation. |
| Correction of acid-base abnormalities | No standard criteria for initiating dialysis exist. |
| Renal support | This approach is based on the utilization of RRT techniques as an adjunct to enhance kidney function, modify fluid balance, and control solute levels. |
| Volume control | Fluid overload is emerging as an important factor associated with, and possibly contributing to, adverse outcomes in AKI. |
| Recent studies have shown potential benefits from extracorporeal fluid removal in CHF. | |
| Intraoperative fluid removal using modified ultrafiltration has been shown to improve outcomes in pediatric cardiac surgery patients. | |
| Nutrition | Restricting volume administration in the setting of oliguric AKI may result in limited nutritional support and RRT allows better nutritional supplementation. |
| Drug delivery | RRT support can enhances the ability to administer drugs without concerns about concurrent fluid accumulation. |
| Regulation of acid-base and electrolyte status | Permissive hypercapnic acidosis in patients with lung injury can be corrected with RRT, without inducing fluid overload and hypernatremia. |
| Solute modulation | Changes in solute burden should be anticipated (e.g., tumor lysis syndrome). Although current evidence is unclear, studies are ongoing to assess the efficacy of RRT for cytokine manipulation in sepsis. |
AKI, acute kidney injury; BUN, blood urea nitrogen; CHF, congestive heart failure; SCr, serum creatinine; RRT, renal replacement therapy.
There is increasing evidence that fluid overload in critical illness and AKI is associated with adverse outcomes, especially in the pediatric setting.83, 84, 542, 543, 544, 545, 546, 547, 548, 549 Whether this is a causal relationship remains to be proven, although a randomized trial in hemodynamically stable patients with acute respiratory distress syndrome seems to suggest that it is.549 Randomizing patients according to RRT initiation on the basis of fluid status would allow this question to be answered. A secondary analysis of a randomized trial comparing IHD to CRRT showed that patients receiving RRT predominantly for solute control experienced better outcomes than those predominantly treated for volume overload. Patients dialyzed for control of both azotemia and volume overload experienced the worst outcome.550 Analysis of a multicenter observational cohort showed that mean daily fluid balance in AKI patients was significantly more positive among nonsurvivors than survivors.84 Data from the PICARD group examining 396 ICU patients with AKI requiring RRT further supports these findings. Survivors had lower fluid accumulation at dialysis initiation compared to nonsurvivors (8.8% vs. 14.2% of baseline body weight; P=0.01 adjusted for dialysis modality and severity score). The adjusted OR for death associated with fluid overload at dialysis initiation was 2.07 (95% CI 1.27–3.37).83 These data suggest that fluid overload should be further evaluated as parameter to guide the initiation of RRT (see also Pediatric Considerations).
Other factors that might influence the decision of when to start RRT are the severity of the underlying disease (affecting the likelihood of recovery of kidney function), the degree of dysfunction in other organs (affecting the tolerance to e.g., fluid overload), the prevalent or expected solute burden (e.g., in tumor lysis syndrome), and the need for fluid input related to nutrition or drug therapy (Table 17). Early detection and accurate prediction of patients that ultimately will require RRT may allow earlier initiation in those who need it and, at the same time, prevent harm in those who do not. Recent evidence suggests a potential role for biomarkers in this field. Plasma neutrophil gelatinase-associated lipocalin was shown to have an area under the receiver operating characteristic curve of 0.82 for the prediction of RRT requirement.551
Pediatric considerations
Provision of acute RRT to children requires special considerations. Pediatric and adolescent patients range in age from the premature neonate to 25 years of age, with a size range of 1.5–200 kg. In addition, the epidemiology of the pediatric AKI has changed from primary kidney disease in the 1980 s to injury resulting from another systemic illness or its treatment (e.g., sepsis and nephrotoxic medications).552, 553 Newborns with inborn errors of metabolism who do not respond to dietary and pharmacologic management require expeditious dialytic removal of ammonia to decrease the risk of death and long-term neurologic dysfunction,554 and infants who receive surgical correction of congenital heart disease, often receive PD early after cardiopulmonary bypass to prevent fluid overload and/or minimize the proinflammatory response. Finally, children develop multiorgan dysfunction very rapidly in their ICU course, with the maximal organ dysfunction occurring with 72 hours and mortality occurring within 7 days of ICU admission, respectively.555, 556 Thus, the issue of timing of dialysis initiation is critically important in children.
Both recommendations in this section of the guideline are applicable to pediatric patients. A detailed discussion of the specific pediatric clinical situations is beyond the scope of this guideline, and the reader is referred to in-depth reviews.557, 558
Importantly, fluid overload has emerged as a significant factor associated with mortality in children with AKI requiring CRRT (Table 18), although the physiological link between increasing percent volume overload and mortality is not completely clear.543, 544, 545, 546, 547, 548, 559 The largest trial to assess this relationship in children is a multicenter prospective study showing that the percentage fluid accumulation at CRRT initiation is significantly lower in survivors vs. non-survivors (14.2 ± 15.9% vs. 25.4 ± 32.9% P<0.03) even after adjustment for severity of illness. This study also found a significantly higher mortality in patient with >20% fluid overload (58%) vs. <20% fluid overload (40%) at CRRT initiation.546 One retrospective study, in pediatric patients who received stem-cell transplantation and developed AKI, suggested that survival may be improved by an aggressive use of diuretics and early initiation of RRT. All survivors (n=11) maintained or remained with percentage fluid accumulation <10%, with diuretics and RRT. Among the 15 nonsurvivors, only 6 (40%) had percentage fluid accumulation <10% at the time of death.559 The latest analysis on this issue confirmed increased mortality with increasing fluid overload in 297 children treated with RRT: 29.6% mortality with less than 10% fluid overload, 43.1% with 10–20% fluid overload, and 65.6% with >20% fluid overload.548 However, strong evidence to suggest that preventing this fluid overload with earlier RRT will improve outcome remains absent.
Table 18. Fluid overload and outcome in critically ill children with AKI.
| Author | Cohort (N) | Outcome | P |
|---|---|---|---|
| Goldstein 2001545 | Single-center (22) | Survivors 16% FO Nonsurvivors 34% FO | 0.03 |
| Gillespie 2004544 | Single-center (77) | % FO >10% with OR death 3.02 | 0.002 |
| Foland 2004543 | Single-center (113) | 3 organ MODS patients Survivors 9% FO Nonsurvivors 16% FO 1.78 OR death for each 10% FO increase | 0.01 |
| Goldstein 2005546 | Multicenter (116) | 2+ organ MODS patients Survivors 14% FO Nonsurvivors 25% FO <20% FO: 58% survival >20% FO: 40% survival | 0.002 |
| Hayes 2009547 | Single-center (76) | Survivors 7% FO Nonsurvivors 22% FO OR death 6.1 for >20% FO | 0.001 |
| Sutherland 2010548 | Multicenter (297) | <10% FO: 70% survival 10–20% FO: 57% survival >20% FO: 34% survival OR 1.03 (1.01–1.05) per % FO | 0.001 |
AKI, acute kidney injury; FO, fluid overload; MODS, multiple-organ dysfunction syndrome; OR, odds ratio.
Reprinted from Goldstein SL. Advances in pediatric renal replacement therapy for acute kidney injury. Semin Dial 2011; 24:
187–191 with permission from John Wiley and Sons560; accessed http://onlinelibrary.wiley.com/doi/10.1111/j.1525-139X.2011.00834.x/full
RESEARCH RECOMMENDATIONS
Determine reproducible criteria (e.g., fluid overload, biomarker level, severity score) to inform the decision to start RRT in adult and pediatric AKI patients. Such criteria may also permit the identification of patients who will ultimately require RRT and hence limit uncertainty around whether to begin therapy.
Determine whether early vs. late start of RRT, based on the above-mentioned criteria, results in improved clinical outcomes (e.g., mortality, evolution to CKD Stage 5) of AKI patients.
Chapter 5.2: Criteria for stopping renal replacement therapy in AKI
Although many patients with AKI recover kidney function sufficiently to be independent of RRT, discontinuation of RRT in AKI has received little attention in the literature. The decision whether or when to stop RRT in a patient with AKI needs to consider an improvement in kidney function adequate to meet demand, an improvement in the disorder that prompted kidney support or futility. It is evident that each of these events is influenced by the initial indication for starting RRT and is subject to individual variation. The strategy for stopping RRT requires consideration of additional factors and often involves a modality transition.
5.2.1: Discontinue RRT when it is no longer required, either because intrinsic kidney function has recovered to the point that it is adequate to meet patient needs, or because RRT is no longer consistent with the goals of care. (Not Graded)
RATIONALE
Many, but not all, patients requiring RRT will recover enough function not to require long-term RRT. 21, 394, 561 The mean duration of RRT in two recent large RCTs was 12–13 days.562, 563 Thus, daily assessment of both intrinsic kidney function and the ongoing appropriateness of RRT consistent with the goals of therapy for the patient are required. More than 50% of patients with severe AKI will not improve, despite appropriate therapy. The incidence of withdrawal of life-support treatments in critically ill patients with multiorgan failure has increased over the last decade.564 In addition to vasoactive medication, mechanical ventilation, and artificial nutrition, RRT is one of the therapies most likely to be discontinued during withdrawal of life support. In general, decisions to withdraw therapy occur in 10% of all patients from general ICUs, and are responsible for roughly 40% of all deaths. Analysis of a database of 383 AKI patients shows withdrawal of life support in 72% of deaths.565 In another single-center retrospective study involving 179 AKI patients requiring RRT, therapy was withheld or withdrawn in 21.2%.566 A posthoc analysis of the BEST KIDNEY database showed that CRRT was withdrawn in 13% of the patients, representing 29% of those who died while on CRRT and 21% of all nonsurvivors.196
Assessment of kidney function during RRT is not easy and will depend on the modality used. In IHD, the fluctuations of solute levels prevent achieving a steady state and thus exclude the use of clearance measurements. Native kidney function can only be assessed during the interdialytic period by evaluating urine volume, urinary excretion of creatinine, and changes in SCr and/or BUN values. However, one must realize that intermittent treatment will be associated with post-treatment rebound in solute levels, and that changes in BUN and creatinine levels can also be modified by nonrenal factors, such as volume status and catabolic rate. In CRRT, continuous solute clearance of 25–35 ml/min will stabilize serum markers after 48 hours. This allows more reliable measurements of CrCl by the native kidneys during CRRT.
Very few investigators have looked at urine CrCl values as a guide for CRRT withdrawal. One small retrospective study (published as abstract) demonstrated that a CrCl (measured over 24 hours) >15 ml/min was associated with successful termination of CRRT, defined as the absence of CRRT requirement for at least 14 days following cessation.567 Further prospective trials will be needed to support these findings. A large prospective observational study showed that, in 529 patients who survived the initial period of CRRT, 313 were successfully removed from RRT, whereas 216 patients needed “repeat CRRT” within 7 days of discontinuation. Multivariate logistic regression identified urine output as the most significant predictor of successful termination (OR 1.078 per 100 ml/d). Not surprisingly, the predictive ability of urine output was negatively affected by the use of diuretics.196 Another retrospective observational analysis showed that, of a total of 304 patients with postoperative AKI requiring RRT (IHD), 31% could be weaned for more than 5 days and 21% were successfully weaned for at least 30 days. Independent predictors for restarting RRT within 30 days were longer duration of RRT, a higher Sequential Organ Failure Assessment score, oliguria, and age >65 years.568 In other words, urine output seems to be a very important predictor of successful discontinuation of RRT. Whether too-early discontinuation of RRT, requiring reinstitution, is by itself harmful has not been properly investigated. The above-mentioned observational studies found a higher mortality in patients who needed to be retreated with RRT (42.7% vs. 28.5%196 and 79.7% vs. 40%568). It is, however, not clear whether failure to wean is simply a marker of illness severity or contributed by itself to the adverse outcome.
The process of stopping RRT may consist of simple discontinuation of RRT, or may include a change in the modality, frequency, or duration of RRT. For example, switching from CRRT to IHD, or decreasing the frequency of IHD from daily to every other day, represents different methods of testing the ability of the patient's own kidney to take over. No specific guidance can be provided for how to manage the transition of RRT from continuous to intermittent. Evidence from large observational studies suggests that large variation in practice exists.196
5.2.2: We suggest not using diuretics to enhance kidney function recovery, or to reduce the duration or frequency of RRT. (2B)
RATIONALE
The role of diuretics in the prevention and treatment of AKI has already been discussed in Chapter 3.4. Only one RCT has evaluated the potential role of diuretics in resolving AKI in patients receiving RRT. After the end of the CVVH session, the urine of the first 4 hours was collected for measuring CrCl. Seventy one patients were subsequently randomized to receive furosemide (0.5 mg/kg/h) or placebo by continuous infusion, continued until CrCl reached 30 ml/min. Urinary fluid losses were compensated by i.v. infusion. The primary end-point was renal recovery (CrCl >30 ml/min or stable SCr without RRT) in the ICU and in the hospital. CVVH was restarted based on predefined criteria. Patients treated with furosemide (n=36) had a significantly increased urinary volume and greater sodium excretion compared to placebo-treated patients (n=35). However, there were no differences in need for repeated CVVH, or renal recovery during ICU or hospital stay.195 An observational study of discontinuation of RRT also found no difference in diuretic use between patents with successful or unsuccessful discontinuation of IHD.568 In summary, diuretics may improve urine volume after RRT, but do not appear to have any significant benefit in reducing the need for RRT or promoting renal recovery from AKI.
Pediatric considerations
The medical indications guiding discontinuation of RRT in children do not differ from adults, except in those instances where RRT is initiated for pediatric-specific disease, such as inborn errors of metabolism to treat hyperammonemia557 or immediately after surgical correction of congenital heart disease to maintain euvolemia, and/or possibly mitigate the postbypass proinflammatory response.558
Prognosis in children who survive an AKI episode is significantly better than in adults, and many children may have several decades of life expectancy. Askenazi demonstrated nearly 80% 3- to 5-year survival for children discharged after an AKI episode from a tertiary center,569 yet two-thirds of deaths occurred in the first 2 years after discharge, suggesting a high probability of greater life expectancy after that period. In addition, no data exist to define a maximal RRT duration; even data from the Prospective Pediatric CRRT Registry show 35% survival in children receiving CRRT for >28 days.570 Finally, since pediatric AKI now results more often as a secondary phenomenon from another systemic illness or its treatment,552, 553 determination of the overall goals of therapy for children, as in for adults, must take into consideration local standards, patient and family wishes, as well as the probability of recovery of the underlying illness leading to AKI and the need for RRT.
RESEARCH RECOMMENDATIONS
Determine clinical parameters (e.g., parameters of kidney function, fluid overload, hypercatabolism) that predict successful discontinuation of RRT in AKI patients.
Determine biomarkers that may indicate renal recovery, and whether their levels can be used to guide discontinuation of RRT.
Determine more reliable predictors of long-term outcomes (e.g., mortality, quality of life) in AKI patients (including clinical severity scores, biomarkers, machine learning techniques, or combinations of these), that—after validation in large cohorts—could be helpful adjuncts in the decision to withdraw treatment.
Chapter 5.3: Anticoagulation
In patients with AKI requiring RRT, the contact of blood with the foreign surface of the extracorporeal circuit results in activation of both the intrinsic and the extrinsic pathway of plasmatic coagulation and activation of platelets.571 Prevention of dialyzer/hemofilter clotting often requires some form of anticoagulation, which may represent a particular challenge in patients with AKI. The need for continuous anticoagulation represents a potential drawback of CRRT.
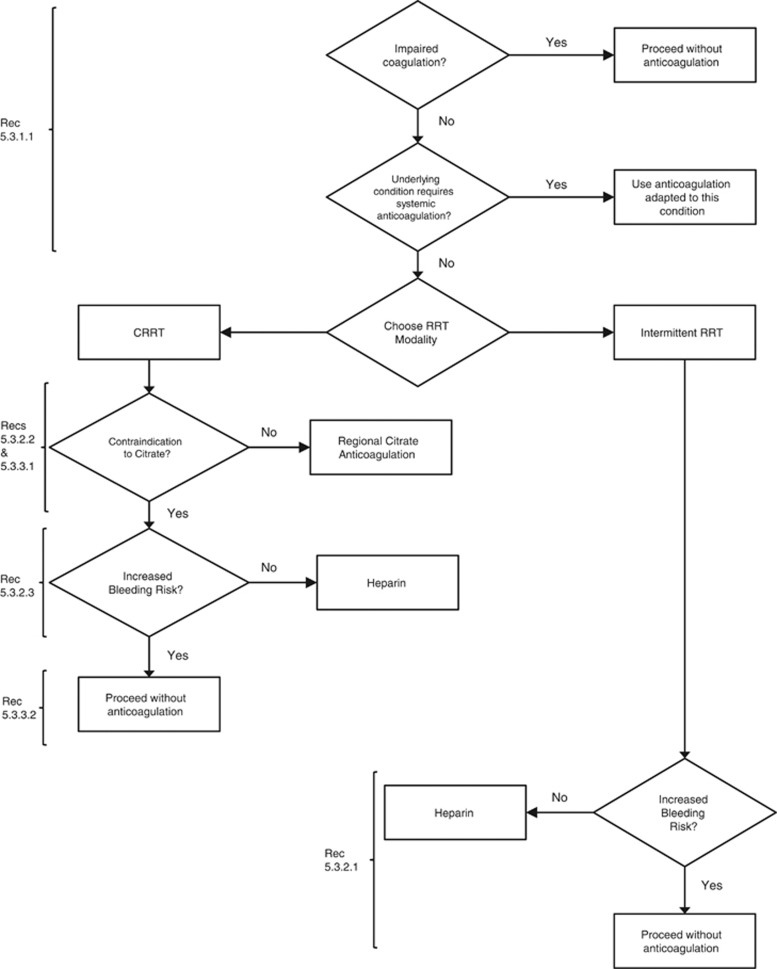
- 5.3.1: In a patient with AKI requiring RRT, base the decision to use anticoagulation for RRT on assessment of the patient's potential risks and benefits from anticoagulation (see Figure 17). (Not Graded)
- 5.3.1.1: We recommend using anticoagulation during RRT in AKI if a patient does not have an increased bleeding risk or impaired coagulation and is not already receiving systemic anticoagulation. (1B)
Figure 17.
Flow-chart summary of recommendations. Heparin includes low-molecular-weight or unfractionated heparin. CRRT, continuous renal replacement therapy; RRT, renal replacement therapy.
RATIONALE
The goal of anticoagulation with RRT is to prevent clotting of the filter and/or reduction in membrane permeability, and thus to achieve adequate RRT and to prevent blood loss in the clotted filter. These benefits have to be weighed against the risk of bleeding, and economic issues, such as workload and costs.
Patients with impaired coagulation (e.g., thrombocytopenia, or prolonged prothrombin time or activated partial thromboplastin time [aPTT]), due to underlying diseases such as liver failure or dilution coagulopathy, may not benefit from additional anticoagulation for RRT. In two recent large trials 50–60% of AKI patients requiring RRT were treated without anticoagulant.562, 563 While filter performance was not assessed, adequate CRRT filter survival without anticoagulation has mostly been described in patients with coagulopathies.572, 573, 574, 575 However, no specific cut-off points have been determined for platelet count, aPTT, International Normalized Ratio, fibrinogen, or other coagulation factors that would indicate the possibility to perform RRT without anticoagulation. On the other hand, prolonged clotting times can also point to a consumptive coagulopathy based on the presence of an activated coagulation. In these patients, frequent filter clotting will occur and necessitate a switch to some form of anticoagulation.576
In patients that are treated without anticoagulation, special attention is required to non-anticoagulant strategies to prolong filter survival. These include a good functioning vascular access, the reduction of blood viscosity and hemoconcentration by saline flushes, predilution, high blood flow rates, diffusive treatment, the reduction of blood-air contact in the bubble trap, and assuring prompt reaction to alarms.577, 578
Many patients with AKI require systemic anticoagulation for their underlying diseases (e.g., artificial heart valve, acute coronary syndrome, atrial fibrillation). It is evident that, in most instances, these patients will not require additional anticoagulation for RRT; however, this should be assessed on a case-by-case basis.
- 5.3.2: For patients without an increased bleeding risk or impaired coagulation and not already receiving effective systemic anticoagulation, we suggest the following:
- 5.3.2.1: For anticoagulation in intermittent RRT, we recommend using either unfractionated or low-molecular-weight heparin, rather than other anticoagulants. (1C)
- 5.3.2.2: For anticoagulation in CRRT, we suggest using regional citrate anticoagulation rather than heparin in patients who do not have contraindications for citrate. (2B)
- 5.3.2.3: For anticoagulation during CRRT in patients who have contraindications for citrate, we suggest using either unfractionated or low-molecular-weight heparin, rather than other anticoagulants. (2C)
RATIONALE
Worldwide, unfractionated heparin is still the most widely used anticoagulant. Many European centers, however, have switched from unfractionated to low-molecular-weight heparin for routine anticoagulation during IHD.579 Advantages and disadvantages of each type of heparin are summarized in Table 19.
Table 19. Overview of the advantages and disadvantages of different anticoagulants in AKI patients.
| Anticoagulant | Advantage | Disadvantage | References |
|---|---|---|---|
| Heparin (unfractionated) | Wide availability | Narrow therapeutic index – risk of bleeding | 580, 581 |
| Large experience | Unpredictable kinetics – monitoring required | ||
| Short half-life | HIT | ||
| Antagonist available | Heparin resistance | ||
| Monitoring with routine tests (aPTT or ACT) | |||
| Low costs | |||
| Low-molecular-weight heparin | More predictable kinetics – Weight-based dosing possible | Risk of accumulation in kidney failure | 580, 582, 583, 584 |
| More reliable anticoagulant response – No monitoring required | Monitoring requires nonroutine test (anti–Factor Xa) | ||
| Single predialysis dose may be sufficient in IHD | Different drugs not interchangeable | ||
| Reduced risk of HIT | Incomplete reversal by protamine | ||
| In most countries more expensive than unfractionated heparin | |||
| Citrate | Strict regional anticoagulation – reduced bleeding risk | Risk of accidental overdose with potentially fatal consequences | 585 |
| Insufficient citrate metabolism in patients with reduced liver function and shock states resulting in accumulation with metabolic acidosis and hypocalcemia | |||
| Other metabolic complication (acidosis, alkalosis, hypernatremia, hypocalcemia, hypercalcemia) | |||
| Increased complexity | |||
| Requires strict protocol |
aPTT, activated partial thromboplastin time; ACT, activated clotting time; HIT, heparin-induced thrombocytopenia; IHD, intermittent hemodialysis
A recent meta-analysis of 11 RCTs comparing unfractionated to low-molecular-weight heparin in chronic IHD concluded that both are equally safe in terms of bleeding complications (RR 0.96; CI 0.27–3.43) and as effective in preventing extracorporeal thrombosis (RR 1.15; CI 0.7–1.91).586 Mainly because of the convenience of using a single bolus injection at the start of IHD, the reduced risk of heparin-induced thrombocytopenia (HIT), and of long-term side-effects such as abnormal serum lipids, osteoporosis, and hypoaldosteronism, the European practice guideline for prevention of dialyzer clotting suggests using low-molecular-weight rather than unfractionated heparin in chronic dialysis patients.587 Many European centers have extrapolated this to IHD for AKI, although studies in this setting are lacking. In patients with AKI, the dose of heparin for IHD and the target aPTT should be individualized according to the presence or absence of coagulation abnormalities and/or risk of bleeding.588, 589 Monitoring should also include platelet count, allowing timely detection of HIT.581 Since low-molecular-weight heparins rely on the kidney as primary route of elimination, patients with kidney injury are at risk of accumulation and bleeding complications, depending on the degree of kidney injury, and the dose and type of low-molecular-weight heparin.590 The American College of Chest Physicians (ACCP) guidelines for antithrombotic and thrombolytic therapy therefore suggest using unfractionated instead of low-molecular-weight heparin in patients with severe renal insufficiency (CrCl <30 ml/min) who require therapeutic anticoagulation, or to reduce the dose of low-molecular-weight heparin by 50%.580 The doses of low-molecular-weight heparin that are required for IHD are lower than those required for therapeutic anticoagulation. The doses of low-molecular-weight heparin, as provided by the manufacturers, should be adapted to the bleeding risk of the individual patient. Dose reduction may also be required in patients receiving daily dialysis, which increases the risk of accumulation. Since many patients with AKI require prophylaxis for deep-vein thrombosis, scheduling this prophylactic (or a slightly higher) dose at the beginning of the dialysis session may serve the two purposes. Periodic measurement of anti–Factor Xa levels may be useful with prolonged use.
Alternative anticoagulants for IHD include protease inhibitors such as nafamostate and platelet inhibitors such as prostacyclin or its analogues. Randomized trials comparing these anticoagulants/antiaggregants with heparin in the setting of IHD for AKI are not available, and their use in clinical practice is limited. Nafamostat is a protease inhibitor that is mainly used in Japan and not available in the USA or Europe. Small observational trials in chronic dialysis patients with increased bleeding risk suggest a reduced bleeding incidence.591, 592, 593 Concerns with nafamostat include the absence of an antidote, and side-effects such as anaphylaxis, hyperkalemia, and bone marrow suppression.594, 595, 596 Crossover comparisons of prostacyclin with low-molecular-weight heparin in chronic dialysis patients show reduced efficiency.597 A small trial showed reduced bleeding complications compared to low-dose heparin; however, at the expense of slightly more premature terminations.598 Additional drawbacks are systemic hypotension and the high costs. Therefore, the routine use of alternative anticoagulants can not be recommended in patients with AKI.
The anticoagulant effect of sodium citrate relies on forming a complex with ionized calcium, thus removing an essential component of the coagulation cascade. Part of the citrate is removed in the extracorporeal circuit. Citrate reaching the systemic circulation is rapidly metabolized in the liver, muscle, and kidney, liberating the calcium and producing bicarbonate. The buffering effect of sodium citrate is proportional to the sodium ions it contains: a mole of trisodium citrate produces the same buffering effect as 3 moles of sodium bicarbonate; whereas preparations of citrate, including hydrogen citrate, have proportionally less buffering effect. Extracorporeal losses of calcium have to be compensated by an exogenous infusion. Additional complications of citrate are summarized in Table 19. Regional citrate anticoagulation requires a strict protocol, adapted to the local treatment modality and flow settings. The protocol should include instructions for the infusion of citrate and calcium, for the composition of the dialysate/replacement fluid, and for intensive metabolic monitoring, including acid-base status, sodium, and total and ionized calcium levels.
Five randomized trials have compared citrate to heparins during CRRT (Suppl Tables 31 and 32). For ethical reasons, these trials were performed in patients without increased bleeding risk. The first trial by Monchi et al. used a crossover design to compare anticoagulation with unfractionated heparin or citrate in 20 patients treated with postdilution CVVH. Patients with high bleeding risk, liver cirrhosis, and sensitivity to heparin were excluded. Forty-nine filters were evaluated. Citrate was titrated to achieve a postfilter ionized calcium level below 1.20 mg/dl (0.3 mmol/l). The dosing regimen of heparin consisted of a bolus of 2000 to 5000 U, followed by a continuous infusion of 500–2000 U/h, aiming at an aPTT of 60–80 seconds. Despite this rather high heparin dose, the citrate group had a longer filter lifetime and less spontaneous filter failure. Fewer patients in the citrate group required transfusion, and the number of transfused units was also lower. One patient in the heparin group experienced bleeding and one patient in the citrate group had metabolic alkalosis.599
The second trial randomized 30 patients with AKI undergoing predilution continuous venovenous hemodiafiltration (CVVHDF) to anticoagulation with citrate or unfractionated heparin. Patients with contra-indications to one of the two anticoagulants (mainly high bleeding risk/severe coagulopathy or metabolic problems that might be aggravated by citrate) or who required systemic anticoagulation for medical reasons were excluded. Heparin was titrated to achieve an aPTT of 45–65 seconds. Citrate was titrated to a postfilter ionized calcium between 1.0–1.40 mg/dl (0.25–0.35 mmol/l). Two patients in each group crossed over to the other anticoagulant and these filters were not included in the analysis. The trial was stopped early after 79 filters because of an advantage using citrate, which resulted in a significantly improved filter survival (124.5 hours vs. 38.3 hours; P<0.001). In addition, significantly less citrate-anticoagulated filters were terminated for clotting (16.7% vs. 53.5%). The incidence of bleeding also tended to be lower with citrate (RR 0.17; CI 0.03–1.04; P=0.06), but transfusion requirement was not significantly different. Three patients in the citrate group had metabolic alkalosis and two had hypocalcemia.600
The third trial randomized 48 patients with AKI, treated with CVVH, to citrate or unfractionated heparin. Patients requiring systemic anticoagulation for medical reasons and patients with high bleeding risk, severe coagulopathy, circulatory failure, liver failure, or hypocalcemia were excluded (n=12). A total of 142 circuits was analyzed. Heparin was administered as a bolus of 3000–5000 U followed by a continuous infusion of 1500 U/h adjusted to achieve an aPTT of 50–70 seconds. Citrate (500 mmol/l) was titrated to a postfilter ionized calcium between 1.0–1.20 mg/dl (0.25–0.30 mmol/l). Neither circuit survival nor the reasons for disconnecting the CVVH circuit differed significantly between the two groups. However, the number of major bleedings and the need for transfusion was significantly greater in the heparin group. Two cases of metabolic alkalosis were noted in the heparin group and two episodes of hypocalcemia in the citrate group.601 Findings from two studies published after the cut-off date for our literature review are consistent with recommendation 5.3.2.2.601a, 601b
A small randomized crossover study compared citrate anticoagulation to regional heparinization in 10 CVVH patients. Both treatment arms had a relatively short filter life (13 hours for regional heparinization and 17 hours for citrate) that did not differ significantly. No bleeding occurred in either group.602
In the largest and most recent randomized trial, 200 patients treated with postdilution CVVH were randomized to citrate or the low-molecular-weight heparin, nadroparin. Again, patients with bleeding risk or liver cirrhosis were excluded. Nadroparin was started with a bolus of 2850 U followed by 380 U/h without further monitoring. Citrate (500 mmol/l) was administered at a dose of 3 mmol per liter blood flow, without monitoring of postfilter ionized calcium. The primary outcomes were safety, defined as the absence of adverse events necessitating discontinuation of the study anticoagulant, and efficacy, defined as circuit survival. Safety was significantly better in the citrate group with only two patients requiring a change in anticoagulation regimen vs. 20 patients in the nadroparin group (P>0.001). Adverse events were citrate accumulation (n=1) and early clotting due to protocol violation (n=1) in the citrate group, and bleeding (n=16) or severe thrombocytopenia (n=4) in the nadroparin group. Circuit survival did not significantly differ. A computer-driven combination of buffered and nonbuffered replacement fluids was used in the citrate group, explaining why metabolic alkalosis occurred more frequently in the nadroparin group. Rather surprisingly, the authors also found an improved renal recovery and an improved hospital survival in the citrate group. This could not be attributed to differences in severity of illness, nor in bleeding or transfusion requirement, and requires further investigation.603
Metabolic complications were infrequent in these randomized trials. In observational trials, the most frequent metabolic complication is metabolic alkalosis, occurring in up to 50% of the patients.604, 605, 606 In recently published surveys or large clinical trials, the use of regional citrate anticoagulation is still limited to 0–20% of the patients/treatments.562, 563, 607
A major contra-indication for the use of citrate anticoagulation is severely impaired liver function or shock with muscle hypoperfusion, both representing a risk of citrate accumulation. Markedly reduced citrate clearances and lower ionized calcium levels have been found in patients with acute liver failure or with severe liver cirrhosis.608, 609, 610 These patients were excluded in all the randomized trials. In patients at risk, intensified monitoring is recommendable. The ratio of total to ionized calcium appears to be the best parameter to detect citrate accumulation611, 612 with an optimal cutoff at 2.1.613 Another important drawback of citrate anticoagulation, that might influence the decision to implement it in routine clinical practice, is the increased complexity of the procedure, with risk of metabolic complications and the need for a strict protocol adapted to the local RRT modality. We, therefore, only recommend the use of citrate for anticoagulation during CRRT in patients that do not have shock or severe liver failure, and in centers that have an established protocol for citrate anticoagulation.
Unfractionated heparin still remains the most widely used anticoagulant during CRRT,562, 563, 607 mostly administered as a prefilter infusion, with large variability in the administered doses. When choosing a dose of heparin, the clinician should realize that the relationship among heparin dose, aPTT, filter survival, and bleeding complications is not straightforward,574, 614, 615, 616, 617, 618, 619 but it is common practice to measure aPTT for safety reasons and to adapt the target to the bleeding risk of the patient.
Only two small prospective RCTs have compared unfractionated to low-molecular-weight heparin for anticoagulation during CRRT in patients with AKI and, thus, no firm recommendations can be made. The first trial randomized 47 patients with AKI or systemic inflammatory response syndrome undergoing CVVHDF to heparin, starting with a bolus of 2000–5000 U followed by an infusion of 10 U/kg/h titrated to an aPTT of 70–80 seconds, or to dalteparin administered as bolus of 20 U/kg followed by an infusion of 10 U/kg/h. The mean aPTT in the heparin group was 79 seconds. The mean anti–Factor Xa level, determined in six patients in the dalteparin group, was 0.49 U/ml. Only 37 of the 82 tested filters were stopped for coagulation. There was no difference in filter survival (with electively discontinued filters being censored). The mean time to filter failure was 46.8 hours in the dalteparin group and 51.7 hours in the heparin group (NS). Three patients in each group had bleeding, with no difference in transfusion requirement between the two groups. Daily costs, including the coagulation assays, were 10% higher with dalteparin.620
The second trial used a crossover design in 40 patients with normal coagulation parameters undergoing predilution CVVH. Patients treated with unfractionated heparin received a bolus of 30 U/kg followed by a continuous infusion of 7 U/kg/h titrated to achieve an aPTT of 40–45 seconds. Enoxaparin was given as an initial bolus of 0.15 mg/kg followed by a continuous infusion of 0.05 mg/kg/h, adjusted to an anti–Factor Xa level of 0.25–0.30 U/ml. In the 37 patients that completed both treatment arms, mean filter life was 21.7 hours with heparin and 30.6 hours with enoxaparin (P=0.017). A similar difference was found in the per-protocol analysis. The incidence of bleeding was low and not different between the two anticoagulants. Filter life did not correlate with aPTT or anti–Factor Xa level. Costs were similar in the two groups.616 Interestingly, these clinical studies did not find a correlation between anti–Factor Xa levels and filter life, questioning the value of anti–Factor Xa monitoring with regard to efficacy.616, 621 However, if used for more than a few days, monitoring might be useful to detect accumulation.
Alternative anticoagulants for use during CRRT include the protease inhibitor nafamostate and the platelet inhibitors, prostacyclin and analogues. Both have a short half-life and a low MW, with the theoretical advantage of extracorporeal elimination and reduced systemic anticoagulation. Nafamostat is not available in the USA and Europe; there is no antidote and several side-effects (agranulocytosis, hyperkalemia, anaphylactoid reactions) have been described.594, 595, 596 A few small trials showed improved filter survival during CRRT when adding prostaglandins to heparin compared to heparin alone.622, 623, 624 However, prostaglandins appear to have a limited efficacy when used alone, induce systemic hypotension,625, 626 and are expensive. Their use during CRRT can therefore not be recommended.
- 5.3.3: For patients with increased bleeding risk who are not receiving anticoagulation, we suggest the following for anticoagulation during RRT:
- 5.3.3.1: We suggest using regional citrate anticoagulation, rather than no anticoagulation, during CRRT in a patient without contraindications for citrate. (2C)
- 5.3.3.2: We suggest avoiding regional heparinization during CRRT in a patient with increased risk of bleeding. (2C)
RATIONALE
The risk of bleeding is considered high in patients with recent (within 7 days) or active bleeding, with recent trauma or surgery (especially in head trauma and neurosurgery), recent stroke, intracranial arteriovenous malformation or aneurysm, retinal hemorrhage, uncontrolled hypertension, or presence of an epidural catheter. In these patients, the benefit of anticoagulation may not outweigh the risk of bleeding, and they should (at least initially) be treated without anticoagulation, or with CRRT with regional citrate anticoagulation.
We suggest performing RRT without anticoagulation in patients with increased bleeding risk. A possible exception can be made for patients who do not have contraindications for citrate. Randomized trials comparing citrate with heparins have been performed in patients without increased bleeding risk. However, since citrate results in strictly regional anticoagulation, it seems reasonable to also suggest its use during CRRT in AKI patients with increased bleeding risk.
Another approach to achieve regional anticoagulation is regional heparinization combining a prefilter dose of heparin, aiming at a prolongation of the extracorporeal aPTT, with postfilter neutralization with protamine, aiming at normalizing the systemic aPTT. This procedure has been described in chronic dialysis and CRRT,572, 573, 624, 627, 628 but has not been studied with much scrutiny. It is cumbersome and difficult to titrate because heparin has a much longer half-life than protamine, inducing a risk of rebound. In addition, it exposes the patient to the side-effects of both heparin (mainly the risk of HIT) and protamine (mainly anaphylaxis, platelet dysfunction, hypotension, and pulmonary vasoconstriction with right ventricular failure)629 and is therefore not recommended.
- 5.3.4: In a patient with heparin-induced thrombocytopenia (HIT), all heparin must be stopped and we recommend using direct thrombin inhibitors (such as argatroban) or Factor Xa inhibitors (such as danaparoid or fondaparinux) rather than other or no anticoagulation during RRT. (1A)
- 5.3.4.1: In a patient with HIT who does not have severe liver failure, we suggest using argatroban rather than other thrombin or Factor Xa inhibitors during RRT. (2C)
RATIONALE
Immune-mediated HIT results from antibodies directed against the complex of heparin and platelet factor 4, and occurs in 1–3% of heparin-exposed patients. Its main clinical complication is the development of thrombocytopenia with or without thrombosis.581 In patients with AKI undergoing CRRT, the diagnosis should therefore also be suspected in patients with repeated premature filter clotting.630 The likelihood of having HIT can be predicted by the so-called 4 T score, that includes the degree of thrombocytopenia, the timing of onset of the fall in platelet count, the presence of thrombosis or acute systemic symptoms, and the presence of other etiologies of thrombocytopenia.631 If HIT is likely, all heparins have to be stopped, including any “heparin lock” solutions for dialysis or other catheters.
With regard to the diagnosis and management of HIT, we refer to the recent guideline of the ACCP581 and the European best practice guideline on chronic dialysis.587 These guidelines recommend the use of therapeutic doses of an alternative nonheparin anticoagulant in patients with strong suspicion of HIT. Candidates are the direct thrombin inhibitors lepirudin, argatroban, or bivaluridin, or the antithrombin-dependent Factor Xa inhibitors, danaparoid or fondaparinix. Pharmacokinetic data and dosing guidelines for these alternative anticoagulants have been published for IHD588, 632 and CRRT.633
Argatroban is a direct thrombin inhibitor, is eliminated by the liver, has a short half-life, and can be monitored with aPTT.634 A recent observational study on the use of argatroban for anticoagulation during continuous dialysis in 30 patients with AKI and HIT derived a dosing equation, based on illness severity scores or by use of indocyanine green plasma clearance.635 Regional citrate anticoagulation has been used along with reduced doses of argatroban or other nonheparin anticoagulants in cases where bleeding occurs. However, there are no published reports on this practice.
Pediatric considerations
Standardized protocols have been well established for both heparin and regional citrate anticoagulation in children receiving dialysis. The ppCRRT Registry Group has shown that heparin- and citrate-based anticoagulation protocols have been shown to confer equitable filter survival in pediatric CRRT, and the use of either is clearly supported over the use of no anticoagulation schemes.636 The main advantage of citrate anticoagulation was the prevention of systemic pharmacological anticoagulation of the patient, which can be an issue in patients with multiorgan failure and sepsis. Calcium is a requisite cofactor in both the intrinsic and extrinsic coagulation cascades. Citrate functions by binding free calcium, thereby inhibiting coagulation in both the intrinsic and extrinsic coagulation pathways. The most frequently studied pediatric citrate protocol636, 637, 638 uses Anticoagulant Dextrose solution A (ACD-A, Baxter Healthcare, USA), prescribed based on the blood flow rate:
ACD-A is infused via a stopcock at the catheter-CRRT circuit connection leading to the CRRT machine. Since our prescribed blood pump flow is 200 ml/min, the resulting ACD-A rate would be 300 ml/h. The second aspect of the citrate protocol provides prevention of citrate-induced systemic hypocalcemia by providing a calcium chloride continuous infusion (8 g calcium chloride per liter normal saline) to the patient via a central line. The calcium chloride rate is also based on the blood pump rate:
The goals of regional citrate anticoagulation are to maintain the circuit ionized calcium between 0.8 and 1.6 mg/dl (0.2 and 0.4 mmol/l), and the patient's systemic ionized calcium in the normal physiologic range 4.4–5.2 mg/dl (1.1–1.3 mmol/l). The circuit ionized calcium concentration is managed by adjustment of the citrate rate, while the patient's systemic ionized calcium concentration is managed by adjustment of the calcium chloride rate.
RESEARCH RECOMMENDATIONS
Randomized trials should compare unfractionated to low-molecular-weight heparin during IHD in patients with AKI.
Randomized trials should compare unfractionated to low-molecular-weight heparin during CRRT in patients with AKI.
Randomized trials should compare citrate to unfractionated to low-molecular-weight heparin during CRRT in patients with AKI.
Future trials should compare a strategy without anticoagulation against one of anticoagulation during CRRT.
Outcomes of interest for trials testing different anticoagulation strategies with RRT in AKI are clinical end-points, including bleeding, renal recovery, mortality, incidence of HIT, and surrogates such as circuit survival and efficiency of dialysis, metabolic complications, and effects on the coagulation system.
Chapter 5.4: Vascular access for renal replacement therapy in AKI
Functional vascular access is essential for adequate RRT. Basic requirements are to ensure adequate and regular flow with low morbidity. Most studies on indwelling tunneled dialysis catheters have been performed in chronic dialysis patients. For individuals requiring acute dialysis, the evidence on dialysis catheters is more limited, but there is a body of literature on nondialysis central venous catheters (CVC) in intensive-care patients. Many of the recommendations for patients requiring acute dialysis are, therefore, based on extrapolation of evidence from tunneled dialysis catheters or from nondialysis nontunneled CVC.
5.4.1: We suggest initiating RRT in patients with AKI via an uncuffed nontunneled dialysis catheter, rather than a tunneled catheter. (2D)
RATIONALE
Since most early catheter-related infections have a cutaneous origin, tunneling the catheter under the skin together with a subcutaneous anchoring system, may reduce the risk of infection. Tunneling also increases mechanical stability of the catheter. On the other hand, the insertion of a tunneled cuffed catheter (TCC) is a cumbersome procedure that requires expertise (mostly performed by surgeons or interventional radiologists), time, and effort (mostly performed in the operating room or radiology department), thus potentially delaying initiation of RRT. The removal of TCCs is also technically more difficult.
A randomized trial compared the initial use of tunneled vs. nontunneled femoral catheters in 34 patients with AKI. Failure to insert the TCC occurred in four patients (12%) that were excluded from the final analysis. In the remaining 30 patients, those with tunneled catheters had an increased insertion time and more femoral hematomas, but also less dysfunction, fewer infectious and thrombotic complications, and a significantly better catheter survival.639 The small size of this study and the absence of an intention-to-treat analysis preclude firm conclusions (Suppl Table 33). In addition, the use of tunneled catheters for starting acute dialysis is not widespread practice.
Both the Centers for Disease Control (CDC) guidelines for prevention of catheter-related infections and the KDOQI guideline for vascular access in chronic dialysis patients recommend using a cuffed catheter for dialysis if a prolonged (e.g., >1–3 weeks) period of temporary access is anticipated.640, 641 In two recent large randomized trials, the mean duration of RRT for AKI was 12–13 days.562, 563 This probably does not justify the burden of an initial tunneled catheter in all patients with AKI receiving RRT. Rather, selected use of tunneled catheters in patients who require prolonged RRT is warranted.
No recommendation can be given regarding the optimal timing to change the nontunneled-uncuffed catheter to a more permanent access. It seems reasonable to create a more permanent access when recovery of kidney function is unlikely. The optimal timing should take into account the increased risk of infection with untunneled catheters, but also the practical issues related to the insertion of a tunneled catheter.
Several configurations of dialysis catheter lumen and tip have emerged over the years with no proven advantage of one design over another. The outer diameter varies between 11 and 14 French and it is self-evident that larger sizes decrease the risk of inadequate blood flow. In order to provide an adequate blood flow and reduce the risk of recirculation, the tip of the catheter should be in a large vein (see Recommendation 5.4.2). This means that the optimal length is 12–15 cm for the right internal jugular vein, 15–20 cm for the left internal jugular vein, and 19–24 cm for the femoral vein.642, 643, 644
In PD, the Tenckhoff catheter, a soft, silicone rubber catheter with a polyester cuff, reduced early complications such as bowel perforation, massive bleeding, or leakage, and has become the standard for PD. Further modifications, including the use of swan-neck catheters, T-fluted catheters, curled intraperitoneal portions, dual cuffs, and insertion through the rectus muscle instead of the midline, have been made to reduce remaining complications such as peritonitis, exit/tunnel infection, cuff extrusion, obstruction, and dialysate leaks.645, 646 Blind placement has been largely replaced by surgical placement or placement guided by ultrasound/fluoroscopy, laparoscopy, or peritoneoscopy.647, 648, 649 Continuous-flow PD dictates the need for an efficient dual-lumen catheter or two separate catheters with ports separated maximally.646 Outside the pediatric setting, no investigations have specifically looked at peritoneal catheters in the setting of AKI.
- 5.4.2: When choosing a vein for insertion of a dialysis catheter in patients with AKI, consider these preferences (Not Graded):
- First choice: right jugular vein;
- Second choice: femoral vein;
- Third choice: left jugular vein;
- Last choice: subclavian vein with preference for the dominant side.
RATIONALE
Although generally associated with the lowest rate of infectious complications, the CDC guideline as well as the KDOQI guideline recommend avoiding the subclavian vein for RRT access,640, 641 because this may lead to central vein stenosis and jeopardize subsequent permanent access. This recommendation is mainly derived from observational data in ESRD patients showing a higher incidence of central vein stenosis with subclavian than with jugular dialysis catheters.650, 651 On the other hand, central vein stenosis has also been described after jugular catheterization.652, 653 Contact of the catheter with the vessel wall is considered a primary initiating event for catheter-related thrombosis and stenosis. Catheters in the right internal jugular vein have a straight course into the right brachiocephalic vein and superior vena cava, and, therefore, the least contact with the vessel wall. A catheter inserted through the subclavian or the left jugular vein has one or more angulations. explaining the higher risk of vessel contact and thrombosis/stenosis with subclavian compared to jugular catheters,650, 651 and with left-sided compared to right-sided jugular catheters.654, 655, 656 The subclavian vein should, therefore, be considered the last choice for insertion of a dialysis catheter in patients with AKI, especially when the risk of nonrecovery of kidney function is substantial. Whether this recommendation should be extended to the left jugular vein remains unclear. In patients where the subclavian vein remains the only available option, preference should be given to the dominant side in order to spare the nondominant side for eventual future permanent access.
Because the subclavian vein should be avoided, the remaining options are the jugular and femoral veins. The use of femoral catheters is thought to be associated with the highest risk of infection, and avoidance of femoral lines is part of many “central line bundles” that intend to reduce the incidence of catheter-related bloodstream infection.657 This dogma was questioned in a concealed, randomized, multicenter, evaluator-blinded, parallel-group trial of 750 AKI patients, comparing the femoral with the jugular site for first catheter insertion for RRT. Ultrasound was seldom used, probably explaining the somewhat higher rate of failure on one side and crossover in the jugular group. The rate of hematoma formation was also higher in the jugular group. In both groups, 20% of the catheters were antiseptic-impregnated. Mean duration of catheterization was 6.2 days for the femoral and 6.9 days for the jugular group. The major reasons for catheter removal were death or “no longer required”. The incidence of catheter colonization at removal (the primary end-point) was not significantly different between the femoral and jugular group. When stratified according to body mass index (BMI), those within the lowest BMI tertile had a higher incidence of colonization with the jugular site, whereas those within the highest BMI tertile had the highest colonization rate with femoral catheters. Bloodstream infection did not differ between the groups (2.3 per 1000 catheter-days for jugular and 1.5 per 1000 catheter-days for femoral) but the study was not powered for this end-point. This was also the case for thrombotic complications (Suppl Table 34).658
Malfunction is another issue that needs to be considered when choosing between a jugular and femoral vascular access. Observational trials show more malfunctioning and a shorter actuarial survival for femoral than for jugular dialysis catheters],659, 660, 661 and more malfunction with left-sided jugular catheters compared to right-sided.662 Recirculation has been shown to be more frequent in femoral than subclavian or jugular dialysis catheters, especially with shorter femoral catheters.642, 643 A secondary analysis of the French multicenter trial did not find a difference in catheter dysfunction between jugular and femoral catheters in the intention-to-treat analysis. However, a separate analysis of the right and left jugular catheters showed a trend toward more dysfunction with femoral than with right jugular catheters, but significantly more dysfunction with left jugular compared to femoral catheters.663
Another point to consider is that any patient who has the option of undergoing a kidney transplantation should not have a femoral catheter placed to avoid stenosis of the iliac vein, to which the transplanted kidney's vein is anatomized.640 The presence of a femoral catheter also reduces the patient's mobilization, especially when the RRT is continuous.
In summary, the right jugular vein appears to be the best option for insertion of a dialysis catheter. Femoral catheters are preferred over left jugular catheters because of reduced malfunction, and the subclavian vein should only be considered a rescue option. It is evident that individual patient characteristics may require deviations from this order of preferences. Catheter insertion should be performed with strict adherence to infection-control policies, including maximal sterile barrier precautions (mask, sterile gown, sterile gloves, large sterile drapes) and chlorhexidine 2% skin antisepsis.641, 664, 665
5.4.3: We recommend using ultrasound guidance for dialysis catheter insertion. (1A)
RATIONALE
For several decades, techniques involving the use of anatomic landmarks have been the traditional mainstay of accessing the central venous system. Using the “blind” landmark technique is not without significant morbidity and mortality. Complications of central venous catheterization include arterial puncture (0.5–6%), hematoma (0.1–4.4%), hemothorax (0.4–0.6%), pneumothorax (0.1–3.1%), and up to 10–20% of insertion attempts are not successful.666, 667 In view of their large size, the risk of complications of dialysis catheters is expected to be even higher. Two meta-analyses have addressed the role of real-time two-dimensional ultrasound for central vein cannulation, and concluded that, compared to the landmark method, ultrasound-guided venous access increases the probability of successful catheter placement and reduces the risk of complications, the need for multiple catheter placement attempts, and the time required for the procedure. The advantage appears most pronounced for the jugular vein, whereas the evidence is scarce for the subclavian and femoral vein.668, 669 Subsequent large randomized trials have confirmed the superiority of ultrasound guidance.670, 671 Trials evaluating the placement of dialysis catheters in ESRD patients, mostly with observational design, yield a similar conclusion.672, 673, 674, 675, 676, 677, 678 The KDOQI guideline for vascular access also recommends using ultrasound-assisted insertion.640
5.4.4: We recommend obtaining a chest radiograph promptly after placement and before first use of an internal jugular or subclavian dialysis catheter. (1B)
RATIONALE
Uncuffed, nontunneled dialysis catheters are semirigid. Their tip should not be in the heart, because of the risk of atrial perforation and pericardial tamponade. On the other hand, a position too high in the brachiocephalic vein, especially with subclavian and left-sided catheters, should also be avoided, because it allows a narrow contact between the catheter tip and the vessel wall, which may result in improper catheter function and vessel thrombosis.655, 679, 680 The correct position of the tip of a semirigid dialysis catheter is at the junction of the superior vena cava and the right atrium, allowing the catheter to run in parallel with the long axis of the superior vena cava.679 Tunneled catheters are usually softer and can be positioned into the right atrium, thus allowing a higher blood flow.680
To confirm the correct position and to assess for potential complications, a postprocedural chest radiograph is conventionally performed. Although this procedure has been debated after uneventful placement of a CVC, the high blood flows used during RRT and the administration of anticoagulants necessitate confirming the correct position before initiating dialysis therapy.640 It should, however, be remembered that none of the radiographic landmarks (carina, right tracheobronchial angle, etc) that are used to exclude intra-atrial tip position are 100% reliable.679, 680 Echocardiography might be another tool to confirm the correct position of the catheter.681
5.4.5: We suggest not using topical antibiotics over the skin insertion site of a nontunneled dialysis catheter in ICU patients with AKI requiring RRT. (2C)
RATIONALE
The incidence of catheter-related bloodstream infection can be reduced by implementing education-based programs and so-called central-line bundles, that emphasize the importance of hand hygiene, maximal barrier precautions upon insertion, chlorhexidine skin antisepsis, optimal catheter site selection, and daily review of line necessity.657 For detailed instructions on catheter care, the reader is referred to published guidelines.640, 641, 664, 665 These guidelines also recommend not using dialysis catheters for applications other than RRT, except under emergency circumstances.641
A recent meta-analysis of five RCTs confirmed that topical antibiotics (mainly mupirocin) reduce the risk of bacteremia, exit-site infection, need for catheter removal, and hospitalization for infection in ESRD patients.682 The majority of the catheters in the included studies were tunneled. However, the CDC, National Health Service, and Infectious Diseases Society of America guidelines strongly recommend against topical antibiotic ointment for the care of CVC, because of their potential to promote fungal infections and antimicrobial resistance.641, 664, 665 For patients with AKI that are treated in an ICU, it seems reasonable to follow this last recommendation. No recommendations can be given for AKI patients that are treated outside an ICU.
5.4.6: We suggest not using antibiotic locks for prevention of catheter-related infections of nontunneled dialysis catheters in AKI requiring RRT. (2C)
RATIONALE
Four meta-analyses have evaluated the efficacy of various antibiotic lock solutions in chronic dialysis patients, and conclude that they significantly reduce catheter-related bloodstream infection. Drawbacks are the overall moderate trial quality and the short follow-up that does not allow excluding the development of resistance.682, 683, 684, 685 However, the CDC, National Health Service, and Infectious Diseases Society of America guidelines strongly recommend against routinely using antibiotic lock solutions in CVC, because of their potential to promote fungal infections, antimicrobial resistance, and systemic toxicity.641, 664, 665 Mentioned exceptions are long-term cuffed and tunneled catheters with history of multiple catheter-related bloodstream infections despite maximal adherence to aseptic technique,641, 665 patients with limited venous access and history of recurrent catheter-related bloodstream infection, or patients with heightened risk of severe sequelae from a catheter-related bloodstream infection.664
Pediatric considerations
Most of the guidelines for adults are applicable to children. Functional CRRT circuit survival in children is favored by larger catheter size686 that should be adapted to patient size (Table 20).687 Recent data from the Prospective Pediatric CRRT Registry group shows that internal jugular catheters may be associated with longer functional CRRT circuit survival, compared to femoral and subclavian access.686 In addition, the Prospective Pediatric CRRT Registry group showed extremely poor circuit survival with two single-lumen 5 F catheters; these catheters should therefore be avoided. Future permanent access in the form of an arteriovenous graft or fistula for patients who develop CKD may be compromised if acute access is placed in a subclavian vein. Clinicians must therefore consider the potential long-term vascular needs of patients who may be expected to develop CKD, especially children who have demonstrated excellent long-term survival with CKD and ESRD.688
Table 20. Catheter and patient sizes.
| Patient size | Catheter size | Site of insertion |
|---|---|---|
| Neonate | Double-lumen 7F | Femoral artery or vein |
| 3–6 kg | Double- or triple-lumen 7F | Jugular, subclavian, or femoral |
| 6–30 kg | Double-lumen 8F | Jugular, subclavian, or femoral |
| >15 kg | Double-lumen 9F | Jugular, subclavian, or femoral |
| >30 kg | Double-lumen 10F or triple-lumen 12F | Jugular, subclavian, or femoral |
Reprinted from Bunchman TE, Brophy PD, Goldstein SL. Technical considerations for renal replacement therapy in children.
Semin Nephrol 2008; 28: 488–492 687, copyright 2008, with permission from Elsevier; accessed http://www.seminarsinnephrology.org/article/S0270-9295(08)00117-4/fulltext
Analysis of a pediatric database (1989–1999) showed that surgically placed Tenckhoff catheters for PD induce less complications than more stiff percutaneously placed catheters.689 A more recent retrospective analysis with historical controls reports that, compared to the surgically placed Tenckhoff catheter, using a more flexible catheter for percutaneous insertion may achieve a comparable catheter survival and complication rate.690
RESEARCH RECOMMENDATIONS
Determine whether the initial use of a tunneled vs. nontunneled catheter for RRT in AKI patients results in a beneficial effect on catheter function and catheter-related complications, including infections and number of additional access procedures.
Develop better means of predicting the need for long-term access and better methods to select access site in individual patients by balancing various risks and benefits.
Chapter 5.5: Dialyzer membranes for renal replacement therapy in AKI
Semipermeable hollow-fiber dialyzers are used as standard of care for both solute clearance and ultrafiltration in IHD and CRRT circuits. Membrane composition and clearance characteristics vary among the commercially available dialyzers. While no RCTs exist to provide definitive recommendations for a particular dialyzer type, the characteristics and potential side-effects of each dialyzer type require consideration.
5.5.1: We suggest to use dialyzers with a biocompatible membrane for IHD and CRRT in patients with AKI. (2C)
RATIONALE
Semipermeable hollow-fiber dialyzers currently represent the standard of care for IHD or CRRT for patients with AKI. All dialyzer membranes induce some degree of activation of blood components, a phenomenon called bioincompatibility.691 Earlier-generation dialyzer membranes composed of cuprophane or unmodified cellulose were more bioincompatible and had the potential to cause a “dialyzer membrane reaction”, mediated by complement activation, release of proinflammatory markers, and oxidative stress, and manifested clinically by acute hypotension, vasodilatation, leucopenia, hypoxia and fever.692, 693, 694, 695, 696, 697 More recently, modified cellulosic membranes (with substitution of the hydroxyl groups) and synthetic membranes composed of polyacylnitrile, polysulfone, or poly(methyl methacrylate) have been developed. These “biocompatible membranes” (or less bioincompatible membranes) produce less complement and cytokine activation, and decrease oxidative stress.697, 698 Recent studies suggest that platelet activation might also be involved in the bioincompatibility phenomenon.698, 699, 700, 701 Another membrane characteristic that might have clinical importance is the flux property, with membranes generally being divided in low-flux and high-flux, the latter having larger pores and thus the potential to clear larger solutes. The question of whether membrane bioincompatibility or flux has clinical relevance in the setting of AKI has been the subject of many clinical trials. A recent meta-analysis of 10 randomized or quasi-randomized controlled trials in 1100 patients could not establish any advantage for biocompatible or high-flux membranes.702 Of note, the authors chose to include modified cellulose membranes in the bioincompatible group, although other investigators consider modified cellulosic membranes to be biocompatible. When comparing the synthetic membranes to cuprophane, there was a trend towards reduced mortality with the synthetic membranes. This meta-analysis also did not assess the side-effects of different membrane compositions on more proximal, temporal associations, such as acute hypotension or fever. As a result, we agree with the authors' conclusion that the use of either a biocompatible or modified cellulose acetate membrane appears to be appropriate.
Recent observations reveal specific potential side-effects when using certain dialyzer membranes. Bradykinin release syndrome has been observed at the start of CRRT with uncoated AN-69 membranes.703 Bradykinin release syndrome is characterized by acute hypotension and pulmonary vascular congestion. The syndrome is usually self-limited and is pH-dependent, and therefore more pronounced in patients with severe acidosis. Also, priming of the circuit with banked blood (that is acidotic and contains a large amount of citrate, inducing hypocalcemia) may evoke bradykinin release syndrome. Numerous measures have been published to prevent or mitigate this syndrome, including zero-balance HF to normalize the banked blood pH and calcium,704 or a bypass maneuver in which the blood prime is given to the patient instead of the circuit, while the patient is bled on to the circuit with the saline prime discarded.705 Finally, a form of bradykinin release syndrome has been reported in patients receiving ACE-I and IHD with AN-69 membranes,706, 707, 708 since ACE-I prevent the conversion of bradykinin and thereby prolong the hypotensive response when acidic blood comes in contact with the AN-69 membrane. However, others have disputed this interaction.704, 705 Nevertheless, clinicians should be aware of the potential for bradykinin release syndrome if an uncoated AN-69 membrane is employed for RRT, especially in acidotic patients or in those receiving ACE-I. Neutralizing the electronegativity of the AN-69 membrane by coating with polyethyleneimine significantly reduces bradykinin generation.709
Whether conventional dialysis membranes are able to affect clinical outcomes in sepsis by removal of inflammatory mediators remains highly controversial. Until further evidence becomes available, the use of RRT to treat sepsis should be considered experimental.
RESEARCH RECOMMENDATIONS
Future research should assess the impact of middle-molecule clearance by high-flux membranes and/or membrane adsorption on patient outcome in sepsis. The comparator group should be patients with sepsis that do not receive extracorporeal treatment (if no AKI) or conventional RRT (if AKI).
The potential impact of dialyzer membrane composition (material, flux, etc.) on outcomes in patients with AKI remains unsettled, due to the relatively small size of trials. It would be useful to conduct larger trials comparing different membranes and examining patient-centered outcomes include survival, renal recovery, and resource utilization.
Chapter 5.6: Modality of renal replacement therapy for patients with AKI
Controversy exists as to which is the optimal RRT modality for patients with AKI. In current clinical practice, the choice of the initial modality for RRT is primarily based on the availability of, and experience with, a specific treatment and on the patient's hemodynamic status. Transitions between CRRT and IHD are also frequent, mostly determined by the hemodynamic status of the patient or coagulation problems. Experience with PD in AKI is limited, except in the pediatric setting and in regions with limited resources.
5.6.1: Use continuous and intermittent RRT as complementary therapies in AKI patients. (Not Graded)
RATIONALE
Current modalities of RRT for AKI include IHD, CRRT, and PD. An overview of the different modalities of RRT and their commonly used settings is given in Table 21.
Table 21. Typical setting of different RRT modalities for AKI (for 70-kg patient).
| SCUF | CVVH | CVVHD | CVVHDF | PD | SLED | IHD | |
|---|---|---|---|---|---|---|---|
| Blood flow (ml/min) | 100–200 | 150–250 | 150–250 | 150–250 | N/A | 100–300 | 200–300 |
| Predominant solute transport principle | convection | convection | diffusion | diffusion+convection | diffusion | diffusion | diffusion |
| Ultrafiltrate (ml/h) | 100–300 | 1500–2000 | variable | 1000–1500 | variable | variable | variable |
| Dialysate flow (ml/h) | 0 | 0 | 1500–2000 | 1000–1500 | 1–2 l per exchange | 100–300 ml/min | 300–500 ml/min |
| Effluent volume (l/d) | 2–8 | 36–48 | 36–48 | 36–72 | 24–48 | N/A | N/A |
| Replacement fluid for zero balance (ml/h) | 0 | 1500–2000 | 0 | 1000–1500 | 0 | 0 | 0 |
| Urea clearance (ml/min) | 1–5 | 25–33 | 25–33 | 25–33 | variable | 80–90 | variable |
CVVH, continuous venovenous hemofiltration; CVVHD, continuous venovenous hemodialysis, CVVHDF, continuous venovenous hemodialfiltration; IHD, intermittent hemodialysis; N/A, not applicable; PD, peritoneal dialysis; SCUF, slow continuous ultrafiltration; SLED, slow low-efficiency dialysis.
Since the introduction of CRRT into clinical practice in the early 1980 s, its use in critically ill patients with AKI has increased steadily.710, 711, 712 The theoretical advantages of CRRT over IHD are the slower fluid removal, resulting in more hemodynamic stability and better control of fluid balance, the slower control of solute concentration, avoiding large fluctuations and fluid shifts (including a reduced risk [worsening] of cerebral edema), the great flexibility (allowing adaptation of the treatment to the patient's need at any time), and the ability to perform the treatment with relatively simple and user-friendly machines (allowing ICU nurses to monitor the treatment). Disadvantages include the need for immobilization, the use of continuous anticoagulation, the risk of hypothermia and, in some settings, higher costs. Major advantages of IHD over CRRT are the fast removal of toxins and the restricted treatment period, allowing down-time for diagnostic and therapeutic interventions. IHD may, therefore, be the preferred treatment in patients where immediate removal of small solutes is required, such as severe hyperkalemia, some cases of poisoning, and tumor lysis syndrome. Hybrid treatments, such as SLED, may share some of the advantages of both IHD and CRRT without having their disadvantages (Table 22).
Table 22. Theoretical advantages and disadvantages of CRRT, IHD, SLED, and PD.
| Modality | Potential setting in AKI | Advantages | Disadvantages |
|---|---|---|---|
| IHD | Hemodynamically stable | Rapid removal of toxins and low-molecular-weight substances Allows for “down time” for diagnostic and therapeutic procedures Reduced exposure to anticoagulation Lower costs than CRRT | Hypotension with rapid fluid removal Dialysis disequilibrium with risk of cerebral edema Technically more complex and demanding |
| CRRT | Hemodynamically unstable Patients at risk of increased intracranial pressure | Continuous removal of toxins Hemodynamic stability Easy control of fluid balance No treatment-induced increase of intracranial pressure User-friendly machines | Slower clearance of toxins Need for prolonged anticoagulation Patient immobilization Hypothermia Increased costs |
| SLED | Hemodynamically unstable | Slower volume and solute removal Hemodynamic stability Allows for “down time” for diagnostic and therapeutic procedures Reduced exposure to anticoagulation | Slower clearance of toxins Technically more complex and demanding |
| PD | Hemodynamically unstable Coagulopathy Difficult access Patients at risk of increased intracranial pressure Under-resourced region | Technically simple Hemodynamic stability No anticoagulation No need for vascular access Lower cost Gradual removal of toxins | Poor clearance in hypercatabolic patients Protein loss No control of rate of fluid removal Risk of peritonitis Hyperglycemia Requires intact peritoneal cavity Impairs diaphragmatic movement, potential for respiratory problems |
CRRT, continuous renal replacement therapy; IHD, intermittent hemodialysis; PD, peritoneal dialysis; SLED, sustained low-efficiency dialysis.
Several RCTs have compared CRRT to IHD in AKI patients. The most inclusive meta-analysis was performed by the Cochrane Collaboration, analyzing 15 RCTs in 1550 AKI patients. This analysis concluded that outcomes were similar in critically ill AKI patients treated with CRRT and IHD for hospital mortality (RR 1.01; 95% CI 0.92–1.12; n=1245), ICU mortality (RR 1.06; 95% CI 0.90–1.26; n=515), length of hospitalization (mean deviation −6.1; 95% CI −26.45 to −14.25; n=25), and renal recovery (free of dialysis on discharge) in survivors (RR 0.99; 95% CI 0.92–1.07; n=161).713 Comparable results have been reported by other meta-analyses.714, 715 Individual studies used different definitions of AKI and were underpowered. Most of the trials excluded patients with hypotension or maximized efforts to improve the hemodynamic tolerance of IHD. The high rate of crossover between the treatment modalities also complicates the interpretation of the results. In addition, in some of the trials, IHD patients were treated with bioincompatible membranes and studies were not standardized for treatment dose. A subsequent RCT not included in the Cochrane meta-analyses reported similar outcomes.716 Two recent studies, confined to single geographic regions, showed reduced costs with IHD compared to CRRT.717, 718 However, an analysis of cost ranges from a multicenter, multinational observational study found considerable heterogeneity in costs related to IHD and CRRT, and concluded that either therapy might be more or less costly depending on local practices, especially staffing.719
Some large observational studies, including all patients receiving RRT, suggest that CRRT is an independent predictor of renal recovery among survivors.720, 721, 722 This evidence, however, is insufficient to fully elucidate the impact of choice of therapy on this outcome. Appropriately planned prospective trials will be required to address this issue.
In conclusion, no RRT is ideal for all patients with AKI. Clinicians should be aware of the pros and cons of different RRTs, and tailor RRT on the basis of the individual and potentially changing needs of their patients. Besides the individual patient's characteristics, the available expertise and resources may also be an important determinant of the ultimate choice.
5.6.2: We suggest using CRRT, rather than standard intermittent RRT, for hemodynamically unstable patients. (2B)
RATIONALE
Many clinicians prefer CRRT in critically ill AKI patients with severe hemodynamic instability, because of better hemodynamic tolerance due to the slower fluid removal and the absence of fluid shifts induced by rapid solute removal. The Cochrane meta-analysis could not establish a difference in the number of patients with (however poorly defined) hemodynamic instability (RR 0.48; 95% CI 0.10–2.28; n=205) nor with (variably defined) hypotension (RR 0.92; 95% CI 0.72–1.16; n=514). On the other hand, the mean arterial pressure at the end of the treatment was significantly higher with CRRT than with IHD (mean deviation 5.35; 95% CI 1.41–9.29; n=112) and the number of patients requiring escalation of vasopressor therapy was significantly lower with CRRT compared to IHD (RR 0.49; 95% CI 0.27–0.87; n=149).713 In general, the number of patients included in these analyses of the hemodynamic tolerance of RRT remains limited, and none of the RCTs has specifically looked at the effect of different modalities of RRT in patients with shock.
SLED has been proposed as an alternative to other forms of RRT and is used in many centers worldwide for logistical reasons. A recent review723 summarizes the results obtained with SLED in several studies and discusses in detail the technical aspects of this dialysis method. However, randomized trials comparing IHD with SLED have not been performed. Also, clinical experience is far more limited with SLED compared to CRRT, and very few randomized studies have compared SLED to CRRT. A first small trial in 39 AKI patients did not find any difference in hemodynamics, and less need for anticoagulation with SLED compared to CRRT.724 An (even smaller) Australian study showed similar control of urea, creatinine, and electrolytes, but a better control of acidosis and less hypotension during the first hours of the treatment with CRRT.725, 726 A recent retrospective analysis examined the mortality data from three general ICUs in different countries that have switched their predominant therapeutic dialysis approach from CRRT to SLED. This change was not associated with a change in mortality.727 In addition, Fieghen et al.728 examined the relative hemodynamic tolerability of SLED and CRRT in critically ill patients with AKI. This study also compared the feasibility of SLED administration with that of CRRT and IHD. Relatively small cohorts of critically ill AKI patients in four critical-care units included 30 patients treated with CRRT, 13 patients with SLED, and 34 patients with IHD. Hemodynamic instability occurred during 22 (56.4%) SLED and 43 (50.0%) CRRT sessions (P=0.51). In a multivariable analysis that accounted for clustering of multiple sessions within the same patient, the OR for hemodynamic instability with SLED was 1.20 (95% CI 0.58–2.47) compared to CRRT. Significant session interruptions occurred in 16 (16.3%), 30 (34.9%), and 11 (28.2%) of IHD, CRRT, and SLED therapies, respectively. This study concluded that, in critically ill patients with AKI, the administration of SLED is feasible and provides hemodynamic control comparable to CRRT.
In conclusion, in the presence of hemodynamic instability in patients with AKI, CRRT is preferable to standard IHD. SLED may also be tolerated in hemodynamically unstable patients with AKI in settings where other forms of CRRT are not available, but data on comparative efficacy and harm are limited. Once hemodynamic stability is achieved, treatment may be switched to standard IHD.
5.6.3: We suggest using CRRT, rather than intermittent RRT, for AKI patients with acute brain injury or other causes of increased intracranial pressure or generalized brain edema. (2B)
RATIONALE
In a patient with acute brain injury, IHD may worsen neurological status by compromising cerebral perfusion pressure. This may be the result of a decrease of mean arterial pressure (dialysis-induced hypotension) or an increase of cerebral edema and intracranial pressure (dialysis disequilibrium), and may jeopardize the potential for neurologic recovery. Dialysis disequilibrium results from the rapid removal of solutes, resulting in intracellular fluid shifts. Both hypotension and disequilibrium can be avoided by the slow progressive removal of fluids and solutes that occurs during CRRT.729 Small observational trials and case reports in patients with intracranial pressure monitoring indeed reported increases in intracranial pressure with IHD.730, 731 Using CT scans to measure brain density, Ronco et al.732 showed an increase of brain water content after IHD, whereas no such changes were observed after CRRT.
Protocols for decreasing hemodynamic instability with intermittent RRT
Intradialytic hypotension is a major problem during RRT in AKI patients, limiting its efficacy and causing morbidity. Surprisingly, there are only a few studies assessing this highly relevant clinical problem. Paganini et al.733 performed a small-sample (10 subjects) randomized crossover controlled trial in AKI patients. They evaluated two different RRT protocols: fixed dialysate sodium (140 mEq) and fixed ultrafiltration rate vs. variable dialysate sodium (160 to 140 mEq) and variable ultrafiltration rate (50% in first third of the treatment and 50% in the last two-thirds of the treatment). The variable sodium and ultrafiltration rate protocol achieved better hemodynamic stability, needed fewer interventions, and induced lesser relative blood volume changes, despite higher ultrafiltration rates.
Schortgen et al.734 evaluated the effects of implementing specific guidelines aiming to improve IHD hemodynamic tolerance. The clinical practice algorithm included priming the dialysis circuit with isotonic saline, setting dialysate sodium concentration at 145 mEq/l, discontinuing vasodilator therapy, and setting dialysate temperature to below 37 °C. A total of 289 RRT sessions were performed in 76 patients and compared to a historical series of 248 sessions in 45 patients. Hemodynamic tolerance was better in the guideline patients. They developed less systolic drop at and during RRT. They also had less hypotensive episodes and the need for therapeutic interventions was less frequent. The adoption of guidelines did not influence ICU mortality, but death rate was significantly lower than predicted from illness severity in the guideline patients, but not in the historical series subjects. Length of ICU stay was also reduced for survivors in the protocol-oriented group, as compared to the historical series of patients.
Peritoneal dialysis
In the developing world, the development of CRRT techniques has resulted in a substantial decline in the expertise with, and use of, PD for treatment of AKI. The use of PD in AKI is mainly confined to pediatrics and in regions with limited resources, because of its ease of use, low cost, and minimal requirements on infrastructure. Other advantages include the lack of a need for vascular access and anticoagulation, the absence of a disequilibrium syndrome and the relatively good hemodynamic tolerance compared to IHD. Disadvantages are the overall lower effectiveness (especially in patients with splanchnic hypoperfusion or who are on vasopressors), the risk of protein loss, the unpredictability of solute and fluid removal, the need for an intact peritoneal cavity, risk of peritonitis, diaphragmatic splinting leading to ventilatory compromise and fluctuating blood glucose levels. Recent developments in the technique of PD (use of flexible and cuffed catheters, automatic cycling, and continuous flow PD) have increased its potential to become an acceptable alternative to other forms of RRT in AKI,735, 736, 737 but direct comparative effectiveness trials are extremely limited. Earlier reports on PD in AKI are mainly uncontrolled observations. Only two relatively recent randomized trials have compared PD to other modalities of RRT in AKI. Phu randomized 70 patients with septic AKI to PD or continuous venovenous hemofiltration (CVVH) and found a better survival with CVVH. However, the PD treatment appeared not to be “up to date” with use of a rigid catheter, manual exchanges with open drainage and acetate buffering.738 The second trial compared daily IHD to high-volume PD (with Tenckhoff catheter and automated cycler) and showed no difference in survival or recovery of kidney function. The duration of RRT was significantly shorter in the PD group (Suppl Table 35).739 However, this trial has not been published in a peer-reviewed journal and the randomization process is unclear. Currently indications for PD in patients with AKI may include bleeding diathesis, hemodynamic instability and difficulty in obtaining a vascular access. Extremely high catabolism, severe respiratory failure, severe ileus, intra-abdominal hypertension, recent abdominal surgery and diaphragmatic peritoneum-pleura connections are contraindications to PD.
Pediatric considerations
RRT modality choice for children with AKI is guided by many of the same principles used for adult patients. However, since severe AKI is relatively rare in children compared to adults, occurring in less than 1% of hospitalized children740 and only 4.5% of children admitted to an intensive care unit,741 the impact of local expertise and resource restrictions may be greater for pediatric acute RRT modality decisions. As noted below, each modality of acute RRT can be successfully provided to pediatric patients of all sizes. Thus, with rare exception driven by medical indication or contraindication, no form of acute RRT can be recommended above another at the present time. Each program should evaluate which modality is provided most optimally and feasibly in its particular setting.
Provision of RRT as IHD, PD, or CRRT is now a mainstay of treatment for the child with severe AKI. The widely varying size range of pediatric patients imparts technical considerations in selection of a modality. Given their small size and associated low blood volume, PD may provide the least technically challenging option for infants and small children. However, technological advances aimed at providing accurate ultrafiltration with volumetric control incorporated into IHD and CRRT equipment, and disposable lines, circuits, and dialyzers sized for the entire pediatric weight spectrum have made IHD and CRRT safer and feasible for children of all ages and sizes.570, 742, 743, 744 Transition from the use of adaptive CRRT equipment to production of high-flow machines with volumetric control allowing for accurate ultrafiltration flows has likewise lead to a change in pediatric RRT modality prevalence patterns in the USA. Accurate ultrafiltration and blood flow rates are crucial for pediatric RRT, since the extracorporeal circuit volume can comprise more than 15% of a small pediatric patient's total blood volume, and small ultrafiltration inaccuracies may represent a large percentage of a small pediatric patient's total body water. Polls of USA pediatric nephrologists demonstrate increased CRRT use over PD as the preferred modality for treating pediatric ARF. In 1995, 45% of pediatric centers ranked PD and 18% ranked CRRT as the most common modality used for initial ARF treatment. In 1999, 31% of centers chose PD vs. 36% of centers reported CRRT as their primary initial modality for ARF treatment.745
In the 1990 s, survival rates stratified by RRT modality were better for children receiving IHD (73–89%) than those receiving PD (49–64%) or CRRT (34–42%).545, 746 However, this analysis did not correct for illness severity. More recent data demonstrate much improved survival in children receiving CRRT,543, 544, 546, 570 with survival rates ranging from 50–70% for children with multiple-organ dysfunction who receive CRRT. While no RCT exists to assess the impact of CRRT modality on survival, convective modalities were associated with increased survival in children with stem-cell transplants in a prospective cohort study (59% vs. 27%, P<0.05).747
RESEARCH RECOMMENDATIONS
Large RCTs should compare SLED against other forms of RRT in patients with AKI. These trials should be standardized for treatment dose, buffer, membrane, anticoagulant, and timing of treatment.
The effects of different modalities of RRT on the long-term need for chronic dialysis, along with mortality, should be evaluated in prospective randomized trials.
Chapter 5.7: Buffer solutions for renal replacement therapy in patients with AKI
One goal of CRRT is to maintain normal or near-normal acid-base balance, thus preventing detrimental effects of acidosis on cardiovascular performance and hormonal response. Options for correction of metabolic acidosis include the use of acetate-, lactate-, and bicarbonate-containing replacement solutions or dialysate. Some centers use citrate anticoagulation, and the citrate load provides an adequate supply of anionic base to control metabolic acidosis. Dialysate solutions for IHD are produced on-line by the dialysis machine, by mixing specially treated municipal water with electrolytes. Dialysate or replacement solutions for CRRT are produced commercially or locally in hospital pharmacies.
5.7.1: We suggest using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI. (2C)
5.7.2: We recommend using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI and circulatory shock. (1B)
5.7.3: We suggest using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI and liver failure and/or lactic acidemia. (2B)
RATIONALE
Options for correction of metabolic acidosis in patients with AKI include acetate, lactate, bicarbonate, and citrate. The use of acetate has been largely abandoned in view of the associated hemodynamic instability and weight loss, probably related to excessive nitric oxide production and cytokine synthesis.748 Citrate, used for regional anticoagulation of the extracorporeal circuit, is alkalinizing, and most patients receiving citrate anticoagulation do not need an additional buffer in the dialysate or replacement fluid.
Original HF solutions contained lactate as a buffer. Under normal circumstances, this lactate is metabolized, resulting in adequate correction of acidosis in most patients. A survey in 34 Australian ICUs concluded that 55% of the ICU patients with AKI were treated with lactate-based solutions710 that, in most countries, are less expensive than bicarbonate solutions. In addition, bicarbonate solutions have a higher risk of bacterial contamination and the solution is unstable in the presence of calcium and magnesium. However, in recent years, bicarbonate has gained popularity because of concerns that lactate may not be rapidly metabolized in the setting of multiple-organ failure.749 Since lactate is a strong anion, insufficient lactate conversion will result in worsening acidosis, especially since bicarbonate losses are ongoing in the extracorporeal circuit. Hyperlactatemia has also been linked to impaired cellular function and catabolism due to lowering of the cellular redox state and phosphorylation potential.750 In addition, iatrogenic increases in lactate levels may lead to misinterpretation of the clinical situation. The risk of “lactate intolerance” is highest in patients with liver failure (impaired lactate clearance) or circulatory shock (increased endogenous lactate production).
Few adequately designed trials have compared different buffers during RRT in AKI patients, and most of them have been performed during CRRT. Barenbrock et al.751 randomized 117 AKI patients to CVVH with lactate or bicarbonate replacement fluid. The use of bicarbonate resulted in better correction of acidosis and lower lactate levels. Also, the incidence of hypotension and other cardiovascular events was lower with bicarbonate. In the subgroup of patients with cardiac failure, mortality tended to be lower with bicarbonate, whereas in the subgroup of septic patents no difference in outcome was found (Suppl Table 36). A nonrandomized crossover study in 54 patients with multiple-organ dysfunction undergoing CVVHDF confirmed the superior control of acidosis and better hemodynamic tolerance with bicarbonate.752 However, another RCT in 40 patients treated with CVVH could not find a difference in hemodynamic tolerance, despite the higher lactate levels in the lactate-buffered group.753 Differences in the case-mix may explain these different results.
Two small prospective randomized crossover comparisons of bicarbonate- and lactate-buffered solutions in AKI patients treated with CVVH or CVVHDF found elevated serum lactate levels with lactate, an effect that was more pronounced in patients with hepatic insufficiency.754, 755 An observational trial in 27 patients found a compromised lactate tolerance in patients with coincidental liver disease, those on inotropic support, and in patients with initial blood lactate measurements of >90.1 mg/dl (>10 mmol/l) and large base deficits.756
In conclusion, the use of bicarbonate as a buffer in the dialysate or replacement fluid of AKI patients results in better correction of acidosis, lower lactate levels, and improved hemodynamic tolerance. This effect is most pronounced in patients with circulatory problems and in those with liver dysfunction.
5.7.4: We recommend that dialysis fluids and replacement fluids in patients with AKI, at a minimum, comply with American Association of Medical Instrumentation (AAMI) standards regarding contamination with bacteria and endotoxins. (1B)
RATIONALE
Replacement fluids for HF or HDF are infused directly into the patient's circulation and should be sterile. A potential major step forward in acute RRT, reducing the costs and the need for storage of fluids, is the on-line production of replacement fluids, which is achieved by passing water and/or dialysate through two or three ultrafilters before being infused.757, 758 On-line production of replacement fluids has not yet been approved by the FDA or by some regulatory authorities in Europe.
Conventional IHD uses nonsterile dialysate, as there is no direct contact between blood and dialysate. However, with the use of high-permeability membranes, the lower blood side pressures at the end of the dialyzer filter may allow back-filtration of dialysate to the blood,759 raising the possibility of endotoxin or other contaminant exposure. Two studies confirmed microbial contamination of (locally prepared and commercial) fluids and circuitry during CRRT.760, 761 Dialysate for CRRT should preferably be ultrapure, and should at least comply with quality standards for dialysis water and dialysis fluids that may differ worldwide (Table 23).762
Table 23. Microbiological quality standards of different regulatory agencies.
| ANSI/AAMI/ISO763, 764, 765 | ERA-EDTA guidelines765a | |
|---|---|---|
| Water for dialysis | ||
| Bacteria (CFU/ml) | <100 (action level at 50) | <100 |
| Endotoxin (EU/ml) | <0.5 | <0.25 |
| Dialysate | ||
| Bacteria (CFU/ml) | <100 (action level at 50) | <100 |
| Endotoxin (EU/ml) | <0.5 | <0.25 |
| Ultrapure dialysate | ||
| Bacteria (CFU/ml) | <0.1 | <0.1 |
| Endotoxin (EU/ml) | <0.03 | <0.03 |
| Substitution fluid for infusion | ||
| Bacteria (CFU/ml) | Sterile | <10−6 |
| Endotoxin (EU/ml) | Undetectable | <0.03 |
AAMI, Association for the Advancement of Medical Instrumentation; ANSI, American National Standards Institute; CFU, colony-forming units; ERA-EDTA, European Renal Association—European Dialysis and Transplant Asssociation; EU, endotoxin units; ISO, International Organization for Standardization.
Finally, an international quality standard for dialysis fluid is in preparation by the International Society for Standardization. Until international standards are in place, we recommend that dialysis fluids and replacement fluids in patients with AKI, at a minimum, comply with AAMI standards for bacteria and endotoxins. When local standards exceed AAMI standards, local standards should be followed (Table 23).
RESEARCH RECOMMENDATION
Further studies are required to explore the impact of on-line preparation of replacement fluid for HDF on clinical outcomes (incidence of sepsis, renal recovery, mortality) in AKI patients requiring RRT.
Chapter 5.8: Dose of renal replacement therapy in AKI
The first report of RRT in AKI was published in 1965.766 Despite more than six decades of clinical experience and research, controversy remains about the best way to measure and what constitutes optimal dose of RRT for patients with AKI. Indeed, three of the top five questions considered most relevant by an international expert's panel on RRT delivery in AKI were about dose.767
The methods used for RRT dose quantification in AKI have several limitations, and have not been fully validated in this specific population. Earlier single-center trials assessing the effects of RRT dose in AKI provided conflicting results.531, 768, 769, 770, 771, 772 Considering the complexity of AKI patients, RRT dose, by itself, may have less impact on mortality both in patients with very high or very low chance of surviving, but may be most important in patients with intermediate scores of disease severity.773 In addition, it is possible that dose and timing are closely linked factors, i.e., a high RRT dose may not work adequately if provided late, or an early RRT starting may not be able to change outcomes if the dose is not optimized. Currently, only one small RCT considered both variables at the same time.531
5.8.1: The dose of RRT to be delivered should be prescribed before starting each session of RRT. (Not Graded) We recommend frequent assessment of the actual delivered dose in order to adjust the prescription. (1B)
5.8.2: Provide RRT to achieve the goals of electrolyte, acid-base, solute, and fluid balance that will meet the patient's needs. (Not Graded)
RATIONALE
The judgment and awareness of how much of a particular therapeutic procedure should be, and actually it is, delivered is essential for a good medical practice. However, recent surveys have shown a disappointingly low number of physicians that report being aware of, or calculating, RRT dose in AKI.774
Although widely used for evaluation of RRT in CKD, Kt/V urea has important limitations as a tool for RRT dosing in AKI. AKI patients are metabolically unstable, with variations in urea generation. In addition, their urea volume of distribution appears to exceed the patient's total body-water volume.775 Different ways to measure Kt/V obtained significantly different results in AKI patients.776 In the same way, the selection of a target serum urea level as an indicator of dialysis dose is highly arbitrary, as serum urea is influenced by several extrarenal factors, such as ethnicity, age, gender, nutrition, presence of liver disease, sepsis, muscle injury, drugs, etc.
Several clinical investigations have shown that the actual delivered dose of RRT in AKI patients is frequently smaller than the prescribed dose, and even smaller than the recommended minimum for CKD patients.771, 773, 776, 777, 778 Impediments to adequate dose delivery were hemodynamic instability, patient size, access problems, technical problems, need for patient transportation, and early filter clotting.
Trials studying dose in CRRT have used the amount of effluent volume normalized by the patient's weight and procedure time as a parameter for dose evaluation. However, the actual effluent flow will be influenced by interruptions of CRRT, and effluent flow will exceed actual dose with use of predilution or with reductions in membrane permeability during the treatment. In summary, it is essential to check very carefully if the prescribed RRT dose is really being delivered to AKI patients. Increasing filter size, dialysis time, blood flow rate, dialysate flow rate, and/or effluent flow rate should be considered in case of dose inadequacy.
In determining a prescription of RRT it is mandatory to consider parameters other than small-solute clearance, such as patients' fluid balance, acid-base and electrolyte homeostasis, and nutrition, among others, as possible components of an optimal RRT dose. In fact, positive fluid balance appears to be an independent risk factor for mortality in AKI patients.83
5.8.3: We recommend delivering a Kt/V of 3.9 per week when using intermittent or extended RRT in AKI. (1A)
5.8.4: We recommend delivering an effluent volume of 20–25 ml/kg/h for CRRT in AKI (1A). This will usually require a higher prescription of effluent volume. (Not Graded)
RATIONALE
Three RCTs evaluated the dose of IHD in AKI (Suppl Tables 37 and 38). Schiffl et al.771 compared daily to alternate-day IHD in 146 ICU patients with AKI. RRT was started with rather high values of SCr (over 4.5 mg/dl [398 μmol/l]) and BUN (around 90 mg/dl [32.1 mmol/l urea]). The daily arm received a weekly Kt/V approximately two times higher than the alternate-day arm (5.8 ± 0.6 vs. 3 ± 0.6, respectively). Daily IHD resulted in lower mortality (28% vs. 46%, P=0.01) and faster recovery of kidney function (9 ± 2 vs. 16 ± 6 days, P=0.001). Major limitations of this study were inadequate randomization, a “very low dose” in the control group (actually less than that recommended for CKD). Also overall mortality in the study (34%) was lower than in other studies in this population, suggesting that the results may not generalize. Moreover, alternate-day IHD was associated with significant differences in fluid removal and dialysis-associated hypotension, suggesting that aspects other than solute control might modify patient outcomes.
The Veterans Affairs/National Institutes of Health Acute Renal Failure Trial Network (ARFTN) study563 was a RCT assessing the effects of intensive compared to less-intensive RRT in 1124 ICU patients with AKI in 27 Veterans Affairs– and university-affiliated North-American centers. Within each randomization arm patients were switched between IHD and CRRT or SLED, based on their hemodynamic status, reflecting average clinical practice in the USA. Intermittent treatments were prescribed at a Kt/V of 1.4, with a delivered Kt/V averaging 1.3, and were performed three (less-intensive arm) or six (more-intensive arm) times per week. Consequently, the weekly Kt/V was approximately 6.5 in the intensive and 3.9 in the less-intensive arm. Mortality at 60 days was similar in both groups (53.6% and 51.5%) as was the percentage of patients recovering kidney function (15.4% and 18.4%). Limitations of this study include the predominance of males, and the nonstandardized timing for initiating RRT. In addition, a significantly higher frequency of hypotension and electrolyte disturbances were seen in the more-intensive arm. Similar to what has been reported in chronic dialysis, acute IHD results in under-dosing when Kt/V is not measured. In the ARFTN study, the first session of IHD had an average delivery of 1.1 Kt/V, while the prescribed dose was 1.4.
The Hannover Dialysis Outcome Study768 randomized 148 ICU patients with AKI to two different doses of SLED: a standard-dialysis arm dosed to maintain plasma urea levels between 120–150 mg/dl (20–25 mmol/l), or an intensified-dialysis arm dosed to maintain plasma urea levels <90 mg/dl (<15 mmol/l). Patients were included with SCr around 3 mg/dl (265 μmol/l) and plasma urea around 60 mg/dl (10 mmol/l). The mean plasma urea was kept at 68 ± 24 mg/dl (11.3 ± 4 mmol/l) in the intensified and 114 ± 36 mg/dl (19 ± 6 mmol/l) in the standard group. Mortality at 28 days was not statistically different between groups (38.7% and 44.4%) and the frequency of survivors recovering kidney function at day 28 was very similar (63% and 60%).
In CKD, the analysis by Gotch and Sargent779 of the National Cooperative Dialysis Study showed that survival could be increased by increasing Kt/V to 1.0–1.2. Analysis of a large database of 2311 Medicare IHD patients also showed a strong association between the delivered IHD dose and mortality, with a decreased mortality risk of 7% for each 0.1 higher level of delivered Kt/V in CKD patients. However, above a Kt/V of 1.3, no further decrease in mortality was noted.780 The HEMO study, a large RCT comparing two different dialysis doses in CKD, also could not demonstrate a further reduction of mortality with equilibrated Kt/V of 1.43 compared to 1.16.781 If we assume that AKI patients should receive at least the same dose as CKD patients, it seems reasonable to recommend a thrice-weekly Kt/V of 1.3 or a weekly Kt/V of 3.9 (assuming at least thrice-weekly treatment), which also represents the lowest dose in the largest randomized trial in AKI (ARFTN study). Whether specific subgroups of AKI patients, such as those with hypercatabolism, may benefit from higher doses will require further investigation.
In conclusion, there are only two adequately designed and executed RCTs testing intermittent or extended RRT dose in AKI. Neither study showed improvement in mortality or renal recovery when the dialysis dose was increased, either by increasing Kt/V above 3.9 weekly or by achieving a plasma urea target below 90 mg/dl (15 mmol/l) in AKI patients. However, consistent with the data on dose of IHD in CKD, and consistent with the lower-dose arm in the ARFTN study, we recommend thrice-weekly Kt/V of 1.3 or a weekly Kt/V of 3.9 for IHD in AKI.
Seven RCTs have investigated the role of CRRT dose in AKI (Suppl Tables 37 and 38).531, 562, 563, 768, 769, 770, 772 While earlier single-center trials showed mixed results, two large multicenter trials have reached remarkably consistent conclusions concerning the dose of CRRT that should be provided to critically ill patients with AKI.
The ARFTN study563 compared standard-intensity predilution CVVHDF with a prescribed effluent flow of 20 ml/kg/h to high-intensity CVVHDF at 35 ml/kg/h. As discussed in Recommendation 5.8.3 rationale, there were no differences in outcomes between the two study arms. Importantly, more than 95% of the prescribed dose of CRRT was delivered in the less-intensive group. This represents a considerably greater intensity of delivered dose than is typically seen in clinical practice. As in chronic dialysis, studies in CRRT have shown that delivery usually falls substantially short of the prescribed dose.782 Thus, it will usually be necessary to prescribe a high dose of CRRT in order to achieve a specific target. For example, in order to achieve a delivered dose of 20–25 ml/kg/h, it is likely that the prescription will need to be in the range of 25–30 ml/kg/h. The Randomized Evaluation of Normal vs. Augmented Level of RRT study was conducted in 35 centers in Australia and New Zealand.562 It compared the effects of postdilution CVVHDF at doses of 25 and 40 ml/kg/h on 28- and 90-day mortality rates in 1464 AKI patients. The delivered dose was 88% and 84% of prescribed in the low- and high-dose groups, respectively. As in the ARFTN study, there was no difference in 28- or 90-day mortality between the two groups. Apart from a higher incidence of hypophosphatemia in the high-dose group, the complication rate was similar.562
In conclusion, there are now consistent data from two large multicenter trials showing no benefits of increasing CRRT doses in AKI patients above effluent flows of 20–25 ml/kg/h. In clinical practice, in order to achieve a delivered dose of 20–25 ml/kg/h, it is generally necessary to prescribe in the range of 25–30 ml/kg/h, and to minimize interruptions in CRRT.
Additional considerations
In patients who do not achieve the target dose of RRT, despite optimization of the initial modality, a switch to another modality or the combination of different modalities should be considered.
Although there are insufficient data supporting a recommendation for elevated RRT doses in patients with AKI and septic shock, limited data suggest that a higher dose might be beneficial in some patients. A small single-center RCT was conducted in 20 patients with septic shock and AKI. Patients were randomized to either high-volume (effluent flow of 65 ml/kg/h) or low-volume CVVH (effluent flow of 35 ml/kg/h). The primary end-point was vasopressor dose required to maintain mean arterial pressure at 65 mm Hg. Mean norepinephrine dose decreased more rapidly after 24 hours of high-volume as compared to low-volume CVVH treatment. Survival on day 28 was not affected.783
RESEARCH RECOMMENDATIONS
Determine the optimal dose parameter that should be used in future trials comparing different intensities of dialysis in AKI patients. Some possible methods to explore are on-line Kt/V urea, urea reduction ratios, or application of the concept of corrected equivalent renal urea clearance for solute removal measurement and ultrafiltration effluent volume, or substitution fluid volume normalized by body weight and time for CRRT. Other aspects of intensity should also be studied, e.g., fluid control and acid-base and electrolyte balance. The comparators might be the standard ways to measure dose as Kt/V or prescribed effluent volume. Suggested outcome parameters are 60- to 90-day mortality, ICU and hospital LOS, and recovery of kidney function.
Determine the optimal dose of RRT in AKI in homogeneous subpopulations, such as cardiac surgery or sepsis patients, and separately in ICU and non-ICU patients. Future RCTs should be controlled for timing of RRT initiation and, perhaps, for general care of patients (antibiotics, nutrition, kind and indication for vasoactive drugs, mode of mechanical ventilation). Studies should also assess the efficiency of RRT (since dose does not necessarily mean efficiency), assessing control of BUN, creatinine, fluid balance, and acid-base and electrolyte status. The comparators might be different efficiency targets. The suggested outcomes are 60- to 90-day mortality, need for vasopressor drugs, time on mechanical ventilation, ICU and hospital stay, and renal recovery.
SPONSORSHIP
KDIGO gratefully acknowledges the following sponsors that make our initiatives possible: Abbott, Amgen, Belo Foundation, Coca-Cola Company, Dole Food Company, Genzyme, Hoffmann-LaRoche, JC Penney, NATCO—The Organization for Transplant Professionals, NKF—Board of Directors, Novartis, Robert and Jane Cizik Foundation, Shire, Transwestern Commercial Services, and Wyeth. KDIGO is supported by a consortium of sponsors and no funding is accepted for the development of specific guidelines.
DISCLAIMER
While every effort is made by the publishers, editorial board, and ISN to see that no inaccurate or misleading data, opinion or statement appears in this Journal, they wish to make it clear that the data and opinions appearing in the articles and advertisements herein are the responsibility of the contributor, copyright holder, or advertiser concerned. Accordingly, the publishers and the ISN, the editorial board and their respective employers, office and agents accept no liability whatsoever for the consequences of any such inaccurate or misleading data, opinion or statement. While every effort is made to ensure that drug doses and other quantities are presented accurately, readers are advised that new methods and techniques involving drug usage, and described within this Journal, should only be followed in conjunction with the drug manufacturer's own published literature.
Footnotes
SUPPLEMENTARY MATERIAL
Supplementary Table 30: Summary table of RCTs examining the effect of early vs. late CVVH in the treatment of AKI.
SUPPLEMENTARY MATERIAL
Supplementary Table 31: Evidence profile of RCTs examining the effect of citrate vs. heparin/nadroparin in CRRT for AKI.
Supplementary Table 32: Summary table of RCTs examining the effect of citrate vs. heparin/nadroparin in CRRT for AKI.
SUPPLEMENTARY MATERIAL
Supplementary Table 33: Summary table of RCTs examining the effect of access placement with tunneled versus non-tunneled catheters on AKI.
Supplementary Table 34: Summary table of RCTs examining the effect of jugular vs. femoral access placement on AKI.
SUPPLEMENTARY MATERIAL
Supplementary Table 35: Summary table of RCTs examining the effect of dialysis modality (continuous vs. intermittent RRT) in AKI.
SUPPLEMENTARY MATERIAL
Supplementary Table 36: Summary table of RCTs examining the effect of bicarbonate vs. lactate as buffer for CVVH replacement fluid on acidosis in AKI.
SUPPLEMENTARY MATERIAL
Supplementary Table 37: Evidence profile of RCTs examining the effect of dose of continuous and intermittent RRT on AKI.
Supplementary Table 38: Summary table of RCTs examining the effect of dose of continuous and intermittent RRT on AKI.
Supplementary material is linked to the online version of the paper at http://www.kdigo.org/clinical_practice_guidelines/AKI.php
References
- Liano F, Pascual J. Epidemiology of acute renal failure: a prospective, multicenter, community-based study. Madrid Acute Renal Failure Study Group. Kidney Int. 1996;50:811–818. doi: 10.1038/ki.1996.380. [DOI] [PubMed] [Google Scholar]
- Bouchard J, Soroko SB, Chertow GM, et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76:422 –427. doi: 10.1038/ki.2009.159. [DOI] [PubMed] [Google Scholar]
- Payen D, de Pont AC, Sakr Y, et al. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care. 2008;12:R74 . doi: 10.1186/cc6916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Voort PH, Boerma EC, Koopmans M, et al. Furosemide does not improve renal recovery after hemofiltration for acute renal failure in critically ill patients: a double blind randomized controlled trial. Crit Care Med. 2009;37:533 –538. doi: 10.1097/CCM.0b013e318195424d. [DOI] [PubMed] [Google Scholar]
- Uchino S, Bellomo R, Morimatsu H, et al. Discontinuation of continuous renal replacement therapy: a post hoc analysis of a prospective multicenter observational study. Crit Care Med. 2009;37:2576 –2582. doi: 10.1097/CCM.0b013e3181a38241. [DOI] [PubMed] [Google Scholar]
- Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930 –936. doi: 10.1053/ajkd.2002.32766. [DOI] [PubMed] [Google Scholar]
- Kellum JA, Mehta RL, Levin A, et al. Development of a clinical research agenda for acute kidney injury using an international, interdisciplinary, three-step modified Delphi process. Clin J Am Soc Nephrol. 2008;3:887 –894. doi: 10.2215/CJN.04891107. [DOI] [PubMed] [Google Scholar]
- Palevsky PM, Baldwin I, Davenport A, et al. Renal replacement therapy and the kidney: minimizing the impact of renal replacement therapy on recovery of acute renal failure. Curr Opin Crit Care. 2005;11:548 –554. doi: 10.1097/01.ccx.0000179936.21895.a3. [DOI] [PubMed] [Google Scholar]
- Allon M, Shanklin N. Effect of albuterol treatment on subsequent dialytic potassium removal. Am J Kidney Dis. 1995;26:607 –613. doi: 10.1016/0272-6386(95)90597-9. [DOI] [PubMed] [Google Scholar]
- Gauthier PM, Szerlip HM. Metabolic acidosis in the intensive care unit. Crit Care Clin. 2002;18:289 –308. doi: 10.1016/s0749-0704(01)00012-4. [DOI] [PubMed] [Google Scholar]
- Kraut JA, Kurtz I. Toxic alcohol ingestions: clinical features, diagnosis, and management. Clin J Am Soc Nephrol. 2008;3:208 –225. doi: 10.2215/CJN.03220807. [DOI] [PubMed] [Google Scholar]
- Pearlman BL, Gambhir R. Salicylate intoxicati on: a clinical review. Postgrad Med. 2009;121:162 –168. doi: 10.3810/pgm.2009.07.2041. [DOI] [PubMed] [Google Scholar]
- Tyagi PK, Winchester JF, Feinfeld DA. Extracorporeal removal of toxins. Kidney Int. 2008;74:1231 –1233. doi: 10.1038/ki.2008.476. [DOI] [PubMed] [Google Scholar]
- Bouman CS, Oudemans-Van Straaten HM, Tijssen JG, et al. Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: a prospective, randomized trial. Crit Care Med. 2002;30:2205 –2211. doi: 10.1097/00003246-200210000-00005. [DOI] [PubMed] [Google Scholar]
- Conger JD. A controlled evaluation of prophylactic dialysis in post-traumatic acute renal failure. J Trauma. 1975;15:1056 –1063. doi: 10.1097/00005373-197512000-00003. [DOI] [PubMed] [Google Scholar]
- Fischer RP, Griffen WO, Jr, Reiser M, et al. Early dialysis in the treatment of acute renal failure. Surg Gynecol Obstet. 1966;123:1019 –1023. [PubMed] [Google Scholar]
- Kleinknecht D, Jungers P, Chanard J, et al. Uremic and non-uremic complicat ions in acute renal failure: Evaluation of early and frequent dialysis on prognosis. Kidney Int. 1972;1:190 –196. doi: 10.1038/ki.1972.26. [DOI] [PubMed] [Google Scholar]
- Parsons FM, Hobson SM, Blagg CR, et al. Optimum time for dialysis in acute reversible renal failure. Description and value of an improved dialyser with large surface area. Lancet. 1961;1:129 –134. doi: 10.1016/s0140-6736(61)91309-5. [DOI] [PubMed] [Google Scholar]
- Gettings LG, Reynolds HN, Scalea T. Outcome in post-traumatic acute renal failure when continuous renal replacement therapy is applied early vs. late. Intensive Care Med. 1999;25:805 –813. doi: 10.1007/s001340050956. [DOI] [PubMed] [Google Scholar]
- Demirkilic U, Kuralay E, Yenicesu M, et al. Timing of replacement therapy for acute renal failure after cardiac surgery. J Card Surg. 2004;19:17 –20. doi: 10.1111/j.0886-0440.2004.04004.x. [DOI] [PubMed] [Google Scholar]
- Elahi MM, Lim MY, Joseph RN, et al. Early hemofiltrati on improves survival in post-cardiotomy patients with acute renal failure. Eur J Cardiothorac Surg. 2004;26:1027 –1031. doi: 10.1016/j.ejcts.2004.07.039. [DOI] [PubMed] [Google Scholar]
- Liu KD, Himmelfarb J, Paganini E, et al. Timing of initiation of dialysis in critically ill patients with acute kidney injury. Clin J Am Soc Nephrol. 2006;1:915 –919. doi: 10.2215/CJN.01430406. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Uchino S, Bellomo R, et al. Timing of renal replacement therapy and clinical outcomes in critically ill patients with severe acute kidney injury. J Crit Care. 2009;24:129 –140. doi: 10.1016/j.jcrc.2007.12.017. [DOI] [PubMed] [Google Scholar]
- Shiao CC, Wu VC, Li WY, et al. Late initiation of renal replacement therapy is associated with worse outcomes in acute kidney injury after major abdominal surgery. Crit Care. 2009;13:R171 . doi: 10.1186/cc8147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandstrup B, Tonnesen H, Beier-Holgersen R, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238:641 –648. doi: 10.1097/01.sla.0000094387.50865.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foland JA, Fortenberry JD, Warshaw BL, et al. Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit Care Med. 2004;32:1771 –1776. doi: 10.1097/01.ccm.0000132897.52737.49. [DOI] [PubMed] [Google Scholar]
- Gillespie RS, Seidel K, Symons JM. Effect of fluid overload and dose of replacement fluid on survival in hemofiltration. Pediatr Nephrol. 2004;19:1394 –1399. doi: 10.1007/s00467-004-1655-1. [DOI] [PubMed] [Google Scholar]
- Goldstein SL, Currier H, Graf C, et al. Outcome in children receiving continuous venovenous hemofiltration. Pediatrics. 2001;107:1309 –1312. doi: 10.1542/peds.107.6.1309. [DOI] [PubMed] [Google Scholar]
- Goldstein SL, Somers MJ, Baum MA, et al. Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int. 2005;67:653 –658. doi: 10.1111/j.1523-1755.2005.67121.x. [DOI] [PubMed] [Google Scholar]
- Hayes LW, Oster RA, Tofil NM, et al. Outcomes of critically ill children requiring continuous renal replacement therapy. J Crit Care. 2009;24:394 –400. doi: 10.1016/j.jcrc.2008.12.017. [DOI] [PubMed] [Google Scholar]
- Sutherland SM, Zappitelli M, Alexander SR, et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis. 2010;55:316 –325. doi: 10.1053/j.ajkd.2009.10.048. [DOI] [PubMed] [Google Scholar]
- Wiedemann HP, Wheeler AP, Bernard GR, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564 –2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- Mehta RL, McDonald B, Pahl M, et al. Continuous vs. intermittent dialysis for acute renal failure in the ICU: Results from a randomized multicenter trial (abstract) J Am Soc Nephrol. 1996;7:1456 . [Google Scholar]
- Cruz DN, de Cal M, Garzotto F, et al. Plasma neutrophil gelatinase-associated lipocalin is an early biomarker for acute kidney injury in an adult ICU population. Intensive Care Med. 2010;36:444 –451. doi: 10.1007/s00134-009-1711-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui-Stickle S, Brewer ED, Goldstein SL. Pediatric ARF epidemiology at a tertiary care center from 1999 to 2001. Am J Kidney Dis. 2005;45:96 –101. doi: 10.1053/j.ajkd.2004.09.028. [DOI] [PubMed] [Google Scholar]
- Williams DM, Sreedhar SS, Mickell JJ, et al. Acute kidney failure: a pediatric experience over 20 years. Arch Pediatr Adolesc Med. 2002;156:893 –900. doi: 10.1001/archpedi.156.9.893. [DOI] [PubMed] [Google Scholar]
- Picca S, Dionisi-Vici C, Abeni D, et al. Extracorporeal dialysis in neonatal hyperammonemia: modalities and prognostic indicators. Pediatr Nephrol. 2001;16:862 –867. doi: 10.1007/s004670100702. [DOI] [PubMed] [Google Scholar]
- Proulx F, Fayon M, Farrell CA, et al. Epidemiology of sepsis and multiple organ dysfunction syndrome in children. Chest. 1996;109:1033 –1037. doi: 10.1378/chest.109.4.1033. [DOI] [PubMed] [Google Scholar]
- Proulx F, Gauthier M, Nadeau D, et al. Timing and predictors of death in pediatric patients with multiple organ system failure. Crit Care Med. 1994;22:1025 –1031. doi: 10.1097/00003246-199406000-00023. [DOI] [PubMed] [Google Scholar]
- Picca S, Bartuli A, Dionisi-Vici C. Medical management and dialysis therapy for the infant with an inborn error of metabolism. Semin Nephrol. 2008;28:477 –480. doi: 10.1016/j.semnephrol.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Picca S, Ricci Z, Picardo S. Acute kidney injury in an infant after cardiopulmonary bypass. Semin Nephrol. 2008;28:470 –476. doi: 10.1016/j.semnephrol.2008.05.006. [DOI] [PubMed] [Google Scholar]
- Michael M, Kuehnle I, Goldstein SL. Fluid overload and acute renal failure in pediatric stem cell transplant patients. Pediatr Nephrol. 2004;19:91 –95. doi: 10.1007/s00467-003-1313-z. [DOI] [PubMed] [Google Scholar]
- Goldstein SL. Advances in pediatric renal replacement therapy for acute kidney injury. Semin Dial. 2011;24:187 –191. doi: 10.1111/j.1525-139X.2011.00834.x. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Mortis G, Godinez-Luna T, et al. Renal recovery after severe acute renal failure. Int J Artif Organs. 2006;29:1023 –1030. doi: 10.1177/039139880602901102. [DOI] [PubMed] [Google Scholar]
- Bellomo R, Cass A, Cole L, et al. Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med. 2009;361:1627 –1638. doi: 10.1056/NEJMoa0902413. [DOI] [PubMed] [Google Scholar]
- Palevsky PM, Zhang JH, O’Connor TZ, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359:7 –20. doi: 10.1056/NEJMoa0802639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast TJ, Luce JM. Increasing incidence of withholding and withdrawal of life support from the critically ill. Am J Respir Crit Care Med. 1997;155:15 –20. doi: 10.1164/ajrccm.155.1.9001282. [DOI] [PubMed] [Google Scholar]
- Swartz R, Perry E, Daley J. The frequency of withdrawal from acute care is impacted by severe acute renal failure. J Palliat Med. 2004;7:676 –682. doi: 10.1089/jpm.2004.7.676. [DOI] [PubMed] [Google Scholar]
- Ho KM, Liang J, Hughes T, et al. Withholding and withdrawal of therapy in patients with acute renal injury: a retrospective cohort study. Anaesth Intensive Care. 2003;31:509 –513. doi: 10.1177/0310057X0303100503. [DOI] [PubMed] [Google Scholar]
- Shealy CB, Campbell RC, Hey JC, et al. 24-hr creatinine clearance as a guide for CRRT withdrawal: a retrospective study (abstr) Blood Purif. 2003;21:192 . [Google Scholar]
- Wu VC, Ko WJ, Chang HW, et al. Risk factors of early redialysis after weaning from postoperative acute renal replacement therapy. Intensive Care Med. 2008;34:101 –108. doi: 10.1007/s00134-007-0813-x. [DOI] [PubMed] [Google Scholar]
- Askenazi DJ, Feig DI, Graham NM, et al. 3–5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int. 2006;69:184 –189. doi: 10.1038/sj.ki.5000032. [DOI] [PubMed] [Google Scholar]
- Symons JM, Chua AN, Somers MJ, et al. Demographic characteristics of pediatric continuous renal replacement therapy: a report of the prospective pediatric continuous renal replacement therapy registry. Clin J Am Soc Nephrol. 2007;2:732 –738. doi: 10.2215/CJN.03200906. [DOI] [PubMed] [Google Scholar]
- Schetz M. Anticoagulation in continuous renal replacement therapy. Contrib Nephrol. 2001;132:283 –303. doi: 10.1159/000060097. [DOI] [PubMed] [Google Scholar]
- Bellomo R, Parkin G, Love J, et al. Use of continuous haemodiafiltration: an approach to the management of acute renal failure in the critically ill. Am J Nephrol. 1992;12:240 –245. doi: 10.1159/000168452. [DOI] [PubMed] [Google Scholar]
- Morabito S, Guzzo I, Solazzo A, et al. Continuous renal replacement therapies: anticoagulation in the critically ill at high risk of bleeding. J Nephrol. 2003;16:566 –571. [PubMed] [Google Scholar]
- Tan HK, Baldwin I, Bellomo R. Continuous veno-venous hemofiltration without anticoagulation in high-risk patients. Intensive Care Med. 2000;26:1652 –1657. doi: 10.1007/s001340000691. [DOI] [PubMed] [Google Scholar]
- Uchino S, Fealy N, Baldwin I, et al. Continuous venovenous hemofiltration without anticoagulation. ASAIO J. 2004;50:76 –80. doi: 10.1097/01.mat.0000104822.30759.a7. [DOI] [PubMed] [Google Scholar]
- Agarwal B, Shaw S, Hari MS, et al. Continuous renal replacement therapy (CRRT) in patients with liver disease: is circuit life different. J Hepatol. 2009;51:504 –509. doi: 10.1016/j.jhep.2009.05.028. [DOI] [PubMed] [Google Scholar]
- Davies H, Leslie G. Maintaining the CRRT circuit: non-anticoagulant alternatives. Aust Crit Care. 2006;19:133 –138. doi: 10.1016/s1036-7314(06)80026-3. [DOI] [PubMed] [Google Scholar]
- Joannidis M, Oudemans-van Straaten HM. Clinical review: Patency of the circuit in continuous renal replacement therapy. Crit Care. 2007;11:218 . doi: 10.1186/cc5937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- davenport A. Review article: Low-molecular-weight heparin as an alternative anticoagulant to unfractionated heparin for routine outpatient haemodialysis treatments. Nephrology (Carlton) 2009;14:455 –461. doi: 10.1111/j.1440-1797.2009.01135.x. [DOI] [PubMed] [Google Scholar]
- Hirsh J, Bauer KA, Donati MB, et al. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133:141S –159S. doi: 10.1378/chest.08-0689. [DOI] [PubMed] [Google Scholar]
- Warkent in TE, Greinacher A, Koster A, et al. Treatment and prevention of heparin-induced thrombocytopenia: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133:340S –380S. doi: 10.1378/chest.08-0677. [DOI] [PubMed] [Google Scholar]
- Baglin T, Barrowcliffe TW, Cohen A, et al. Guidelines on the use and monitoring of heparin. Br J Haematol. 2006;133:19 –34. doi: 10.1111/j.1365-2141.2005.05953.x. [DOI] [PubMed] [Google Scholar]
- Gray E, Mulloy B, Barrowcliffe TW. Heparin and low-molecular-weight heparin. Thromb Haemost. 2008;99:807 –818. doi: 10.1160/TH08-01-0032. [DOI] [PubMed] [Google Scholar]
- Martel N, Lee J, Wells PS. Risk for heparin-induced thrombocytopenia with unfraction ated and low-molecular-weight heparin thromboprophylaxis: a meta-analysis. Blood. 2005;106:2710 –2715. doi: 10.1182/blood-2005-04-1546. [DOI] [PubMed] [Google Scholar]
- Davenport A, Tolwani A. Citrate anticoagulation for continuous renal replacement therapy (CRRT) in patients with acute kidney injury admitted to the intensive care unit. NDT Plus. 2009;2:439 –447. doi: 10.1093/ndtplus/sfp136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim W, Cook DJ, Crowther MA. Safety and efficacy of low molecular weight heparins for hemodialysis in patients with end-stage renal failure: a meta-analysis of randomized trials. J Am Soc Nephrol. 2004;15:3192 –3206. doi: 10.1097/01.ASN.0000145014.80714.35. [DOI] [PubMed] [Google Scholar]
- European Best Practice Guidelines for Haemodialysis (Part 1). V. Chronic intermittent haemodialysis and prevention of clotting in the extracorporal system. 2002;17 (Suppl 7) :63 –71. doi: 10.1093/ndt/17.suppl_7.63. [DOI] [PubMed] [Google Scholar]
- Fi scher KG. Essentials of anticoagulation in hemodialysis. Hemodial Int. 2007;11:178 –189. doi: 10.1111/j.1542-4758.2007.00166.x. [DOI] [PubMed] [Google Scholar]
- Ouseph R, Ward RA. Anticoagulation for intermittent hemodialysis. Semin Dial. 2000;13:181 –187. doi: 10.1046/j.1525-139x.2000.00052.x. [DOI] [PubMed] [Google Scholar]
- Lim W, Dentali F, Eikelboom JW, et al. Meta-analysis: low-molecular-weight heparin and bleeding in patients with severe renal insufficiency. Ann Intern Med. 2006;144:673 –684. doi: 10.7326/0003-4819-144-9-200605020-00011. [DOI] [PubMed] [Google Scholar]
- Akizawa T, Koshikawa S, Ota K, et al. Nafamostat mesilate: a regional anticoagulant for hemodialysis in patients at high risk for bleeding. Nephron. 1993;64:376 –381. doi: 10.1159/000187357. [DOI] [PubMed] [Google Scholar]
- Matsuo T, Kario K, Nakao K, et al. Anticoagulation with nafamostat mesilate, a synthetic protease inhibitor, in hemodialysis patients with a bleeding risk. Haemostasis. 1993;23:135 –141. doi: 10.1159/000216866. [DOI] [PubMed] [Google Scholar]
- Yang JW, Han BG, Kim BR, et al. Superior outcome of nafamostat mesilate as an anticoagulant in patients undergoing maintenance hemodialysis with intracerebral hemorrhage. Ren Fail. 2009;31:668 –675. doi: 10.3109/08860220903180616. [DOI] [PubMed] [Google Scholar]
- Maruyama H, Miyakawa Y, Gejyo F, et al. Anaphylactoid reaction induced by nafamostat mesilate in a hemodialysis patient. Nephron. 1996;74:468 –469. doi: 10.1159/000189371. [DOI] [PubMed] [Google Scholar]
- Muto S, Imai M, Asano Y. Mechanisms of hyperkalemia caused by nafamostat mesilate. Gen Pharmacol. 1995;26:1627 –1632. doi: 10.1016/0306-3623(95)00072-0. [DOI] [PubMed] [Google Scholar]
- Okada H, Suzuki H, Deguchi N, et al. Agranulocytosis in a haemodialysed patient induced by a proteinase inhibitor, nafamostate mesilate. Nephrol Dial Transplant. 1992;7:980 . doi: 10.1093/ndt/7.9.980a. [DOI] [PubMed] [Google Scholar]
- Novacek G, Kapiotis S, Jilma B, et al. Enhanced blood coagulation and enhanced fibrinolysis during hemodialysis with prostacyclin. Thromb Res. 1997;88:283 –290. doi: 10.1016/s0049-3848(97)00255-7. [DOI] [PubMed] [Google Scholar]
- Swartz RD, Flamenbaum W, Dubrow A, et al. Epoprostenol (PGI2, prostacyclin) during high-risk hemodialysis: preventing further bleeding complications. J Clin Pharmacol. 1988;28:818 –825. doi: 10.1002/j.1552-4604.1988.tb03222.x. [DOI] [PubMed] [Google Scholar]
- Monchi M, Berghmans D, Ledoux D, et al. Citrate vs. heparin for anticoagulation in continuous venovenous hemofiltration: a prospective randomized study. Intensive Care Med. 2004;30:260 –265. doi: 10.1007/s00134-003-2047-x. [DOI] [PubMed] [Google Scholar]
- Kutsogiannis DJ, Gibney RT, Stollery D, et al. Regional citrate versus systemic heparin anticoagulation for continuous renal replacement in critically ill patients. Kidney Int. 2005;67:2361 –2367. doi: 10.1111/j.1523-1755.2005.00342.x. [DOI] [PubMed] [Google Scholar]
- Betjes MG, van Oosterom D, van Agteren M, et al. Regional citrate versus heparin anticoagulation during venovenous hemofiltration in patients at low risk for bleeding: similar hemofilter survival but significantly less bleeding. J Nephrol. 2007;20:602 –608. [PubMed] [Google Scholar]
- Hetzel GR, Schmitz, Wissing H, et al. Regional citrate versus systemic heparin for anticoagulation in critically ill patients on continuous venovenous haemofiltration: a prospective randomized multicentre trial. Nephrol Dial Transplant. 2011;26:232 –239. doi: 10.1093/ndt/gfq575. [DOI] [PubMed] [Google Scholar]
- Park JS, Kim GH, Kang CM, et al. Regional anticoagulation with citrate is superior to systemic anticoagulation with heparin in critically ill patients undergoin g continuous venovenous hemodiafiltration. Korean J Intern Med. 2011;26:68 –75. doi: 10.3904/kjim.2011.26.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fealy N, Baldwin I, Johnstone M, et al. A pilot randomized controlled crossover study comparing regional heparinization to regional citrate anticoagulation for continuous venovenous hemofiltration. Int J Artif Organs. 2007;30:301 –307. doi: 10.1177/039139880703000404. [DOI] [PubMed] [Google Scholar]
- Oudemans-van Straaten HM, Bosman RJ, Koopmans M, et al. Citrate anticoagulation for continuous venovenous hemofiltration. Crit Care Med. 2009;37:545 –552. doi: 10.1097/CCM.0b013e3181953c5e. [DOI] [PubMed] [Google Scholar]
- Mehta RL, McDonald BR, Aguilar MM, et al. Regional citrate anticoagulation for continuous arteriovenous hemodialysis in critically ill patients. Kidney Int. 1990;38:976 –981. doi: 10.1038/ki.1990.300. [DOI] [PubMed] [Google Scholar]
- Morgera S, Scholle C, Voss G, et al. Metabolic complications during regional citrate anticoagulation in continuous venovenous hemodialysis: single-center experience. Nephron Clin Pract. 2004;97:c131 –c136. doi: 10.1159/000079171. [DOI] [PubMed] [Google Scholar]
- Thoenen M, Schmid ER, Binswanger U, et al. Regional citrate anticoagulation using a citrate-based substitution solution for continuous venovenous hemofiltration in cardiac surgery patients. Wien Klin Wochenschr. 2002;114:108 –114. [PubMed] [Google Scholar]
- Uchino S, Bellomo R, Morimatsu H, et al. Continuous renal replacement therapy: a worldwide practice survey. The beginning and ending supportive therapy for the kidney (B .E.S.T. kidney) investigators. Intensive Care Med. 2007;33:1563 –1570. doi: 10.1007/s00134-007-0754-4. [DOI] [PubMed] [Google Scholar]
- Apsner R, Schwarzenhofer M, Derfler K, et al. Impairment of citrate metabolism in acute hepatic failure. Wien Klin Wochenschr. 1997;109:123 –127. [PubMed] [Google Scholar]
- Durao MS, Monte JC, Batista MC, et al. The use of regional citrate anticoagulation for continuous venovenous hemodiafiltration in acute kidney injury. Crit Care Med. 2008;36:3024 –3029. doi: 10.1097/CCM.0b013e31818b9100. [DOI] [PubMed] [Google Scholar]
- Kramer L, Bauer E, Joukhadar C, et al. Citrate pharmacoki netics and metabolism in cirrhotic and noncirrhotic critically ill patients. Crit Care Med. 2003;31:2450 –2455. doi: 10.1097/01.CCM.0000084871.76568.E6. [DOI] [PubMed] [Google Scholar]
- Hetzel GR, Taskaya G, Sucker C, et al. Citrate plasma levels in patients under regional anticoagulation in continuous venovenous hemofiltration. Am J Kidney Dis. 2006;48:806 –811. doi: 10.1053/j.ajkd.2006.07.016. [DOI] [PubMed] [Google Scholar]
- Meier-Kriesche HU, Gitomer J, Finkel K, et al. Increased total to ionized calcium ratio during continuous venovenous hemodialysis with regional citrate anticoagulati on. Crit Care Med. 2001;29:748 –752. doi: 10.1097/00003246-200104000-00010. [DOI] [PubMed] [Google Scholar]
- Bakker AJ, Boerma EC, Keidel H, et al. Detection of citrate overdose in critically ill patients on citrate-anticoagulated venovenous haemofiltration: use of ionised and total/ionised calcium. Clin Chem Lab Med. 2006;44:962 –966. doi: 10.1515/CCLM.2006.164. [DOI] [PubMed] [Google Scholar]
- Davies HT, Leslie G, Pereira SM, et al. A randomized comparative crossover study to assess the affect on circuit life of varying pre-dilution volume associated with CVVH and CVVHDF. Int J Artif Organs. 2008;31:221 –227. doi: 10.1177/039139880803100305. [DOI] [PubMed] [Google Scholar]
- Holt AW, Bierer P, Bersten AD, et al. Continuous renal replacement therapy in critically ill patients: monitoring circuit function. Anaesth Intensive Care. 1996;24:423 –429. doi: 10.1177/0310057X9602400402. [DOI] [PubMed] [Google Scholar]
- Joannidis M, Kountchev J, Rauchenzauner M, et al. Enoxaparin vs. unfractionated heparin for anticoagulation during continuous veno-venous hemofiltration: a randomized controlled crossover study. Intensive Care Med. 2007;33:1571 –1579. doi: 10.1007/s00134-007-0719-7. [DOI] [PubMed] [Google Scholar]
- Stefanidis I, Hagel J, Frank D, et al. Hemostatic alterations during continuous venovenous hemofiltration in acute renal failure. Clin Nephrol. 1996;46:199 –205. [PubMed] [Google Scholar]
- van de Wetering J, Westendorp RG, van der Hoeven JG, et al. Heparin use in continuous renal replacement procedures: the struggle between filter coagulation and patient hemorrhage. J Am Soc Nephrol. 1996;7:145 –150. doi: 10.1681/ASN.V71145. [DOI] [PubMed] [Google Scholar]
- Yang RL, Liu DW. Clinical evaluation of hemofiltration without anticoagulation in critically ill patients at high risk of bleeding] Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2007;29:651 –655. [PubMed] [Google Scholar]
- Reeves JH, Cumming AR, Gallagher L, et al. A controlled trial of low-molecular-weight heparin (dalteparin) versus unfractionated heparin as anticoagulant during continuous venovenous hemodialysis with filtration. Crit Care Med. 1999;27:2224 –2228. doi: 10.1097/00003246-199910000-00026. [DOI] [PubMed] [Google Scholar]
- de Pont AC, Oudemans-van Straaten HM, Roozendaal KJ, et al. Nadroparin versus dalteparin anticoagulation in high-volume, continuous venovenous hemofiltration: a double-blind, randomized, crossover study. Crit Care Med. 2000;28:421 –425. doi: 10.1097/00003246-200002000-00022. [DOI] [PubMed] [Google Scholar]
- Birnbaum J, Spies CD, Klotz E, et al. Iloprost for additional anticoagulation in continuous renal replacement therapy--a pilot study. Ren Fail. 2007;29:271 –277. doi: 10.1080/08860220601166222. [DOI] [PubMed] [Google Scholar]
- Kozek-Langenecker SA, Spiss CK, Gamsjager T, et al. Anticoagulation with prostaglandins and unfractionated heparin during continuous venovenous haemofiltration: a randomized controlled trial. Wien Klin Wochenschr. 2002;114:96 –101. [PubMed] [Google Scholar]
- Fabbri LP, Nucera M, Al Malyan M, et al. Regional anticoagulation and antiaggregation for CVVH in critically ill patients: a prospective, randomized, controlled pilot study. Acta Anaesthesiol Scand. 2010;54:92 –97. doi: 10.1111/j.1399-6576.2009.02031.x. [DOI] [PubMed] [Google Scholar]
- Fiaccadori E, Maggiore U, Rotelli C, et al. Continuous haemofiltration in acute renal failure with prostacyclin as the sole anti-haemostatic agent. Intensive Care Med. 2002;28:586 –593. doi: 10.1007/s00134-002-1249-y. [DOI] [PubMed] [Google Scholar]
- Langenecker SA, Felfernig M, Werba A, et al. Anticoagulation with prostacyclin and heparin during continuous venovenous hemofiltration. Crit Care Med. 1994;22:1774 –1781. [PubMed] [Google Scholar]
- Biancofi ore G, Esposito M, Bindi L, et al. Regional filter heparinizati on for continuous veno-venous hemofiltration in liver transplant recipients Minerva Anestesiol 200369527 –534.534–528. [PubMed] [Google Scholar]
- Kaplan AA, Petrillo R. Regional heparinizati on for continuous arterio-venous hemofiltration (CAVH) ASAIO Trans. 1987;33:312 –315. [PubMed] [Google Scholar]
- Carr JA, Silverman N. The heparin-protamine interaction. A review. J Cardiovasc Surg (Torino) 1999;40:659 –666. [PubMed] [Google Scholar]
- Lasocki S, Piednoir P, Ajzenberg N, et al. Anti-PF4/heparin antibodies associated with repeated hemofiltration-filter clotting: a retrospective study. Crit Care. 2008;12:R84 . doi: 10.1186/cc6937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo GK, Juhl D, Warkentin TE, et al. Evaluation of pretest clinical score (4 T's) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost. 2006;4:759 –765. doi: 10.1111/j.1538-7836.2006.01787.x. [DOI] [PubMed] [Google Scholar]
- O’Shea SI, Ortel TL, Kovalik EC. Alternative methods of anticoagulation for dialysis-dependent patients with heparin-induced thrombocytopenia. Semin Dial. 2003;16:61 –67. doi: 10.1046/j.1525-139x.2003.03014.x. [DOI] [PubMed] [Google Scholar]
- Davenport A. Anticoagulation options for patients with heparin-induced thrombocytopenia requiring renal support in the intensive care unit. Contrib Nephrol. 2007;156:259 –266. doi: 10.1159/000102110. [DOI] [PubMed] [Google Scholar]
- Hursting MJ, Murray PT. Argatroban anticoagulati on in renal dysfunction: a literature analysis. Nephron Clin Pract. 2008;109:c80 –c94. doi: 10.1159/000139993. [DOI] [PubMed] [Google Scholar]
- Link A, Girndt M, Selejan S, et al. Argatroban for anticoagulation in continuous renal replacement therapy. Crit Care Med. 2009;37:105 –110. doi: 10.1097/CCM.0b013e3181932394. [DOI] [PubMed] [Google Scholar]
- Brophy PD, Somers MJ, Baum MA, et al. Multi-centre evaluation of anticoagulation in patients receiving continuous renal replacement therapy (CRRT) Nephrol Dial Transplant. 2005;20:1416 –1421. doi: 10.1093/ndt/gfh817. [DOI] [PubMed] [Google Scholar]
- Bunchman TE, Maxvold NJ, Barnett J, et al. Pediatric hemofiltration: Normocarb dialysate solution with citrate anticoagulation. Pediatr Nephrol. 2002;17:150 –154. doi: 10.1007/s00467-001-0791-0. [DOI] [PubMed] [Google Scholar]
- Bunchman TE, Maxvold NJ, Brophy PD. Pediatric convective hemofiltration: Normocarb replacement fluid and citrate anticoagulation. Am J Kidney Dis. 2003;42:1248 –1252. doi: 10.1053/j.ajkd.2003.08.026. [DOI] [PubMed] [Google Scholar]
- Klouche K, Amigues L, Deleuze S, et al. Complications, effects on dialysis dose, and survival of tunneled femoral dialysis catheters in acute renal failure. Am J Kidney Dis. 2007;49:99 –108. doi: 10.1053/j.ajkd.2006.09.014. [DOI] [PubMed] [Google Scholar]
- National Kidney Foundation KDOQI clinical practice guidelines and clinical practice recommen dations for 2006 updates: vascular access. Am J Kidney Dis. 2006;48:S176 –S307. doi: 10.1053/j.ajkd.2006.04.029. [DOI] [PubMed] [Google Scholar]
- O’Grady NP, Alexander M, Dellinger EP, et al. Guidelines for the prevention of intravascular catheter-related infections. Infect Control Hosp Epidemiol. 2002;23:759 –769. doi: 10.1086/502007. [DOI] [PubMed] [Google Scholar]
- Leblanc M, Fedak S, Mokris G, et al. Blood recirculat ion in temporary central catheters for acute hemodialysis. Clin Nephrol. 1996;45:315 –319. [PubMed] [Google Scholar]
- Little MA, Conlon PJ, Walshe JJ. Access recirculation in temporary hemodialysis catheters as measured by the saline dilution technique. Am J Kidney Dis. 2000;36:1135 –1139. doi: 10.1053/ajkd.2000.19821. [DOI] [PubMed] [Google Scholar]
- Oliver MJ. Acute dialysis catheters. Semin Dial. 2001;14:432 –435. doi: 10.1046/j.1525-139x.2001.00107.x. [DOI] [PubMed] [Google Scholar]
- Twardowski ZJ. History of peritoneal access development. Int J Artif Organs. 2006;29:2 –40. doi: 10.1177/039139880602900102. [DOI] [PubMed] [Google Scholar]
- Ronco C, Dell’Aquila R.Peritoneal access for acute peritoneal dialysisIn: Ronco C, Bellomo R, Kellum J (eds).Critical Care Nephrology2nd Edn.Saunders Elsevier: Philadelphia, PA; 20091467–1471. [Google Scholar]
- Asif A, Byers P, Vieira CF, et al. Peritoneoscopic placement of peritoneal dialysis catheter and bowel perforation: experience of an interventional nephrology program. Am J Kidney Dis. 2003;42:1270 –1274. doi: 10.1053/j.ajkd.2003.08.029. [DOI] [PubMed] [Google Scholar]
- Maya ID. Ultrasound/fluoroscopy-assisted placement of peritoneal dialysis catheters. Semin Dial. 2007;20:611 –615. doi: 10.1111/j.1525-139X.2007.00371.x. [DOI] [PubMed] [Google Scholar]
- Schmidt SC, Pohle C, Langrehr JM, et al. Laparoscopic-assisted placement of peritoneal dialysis catheters: implantation technique and results. J Laparoendosc Adv Surg Tech A. 2007;17:596 –599. doi: 10.1089/lap.2006.0162. [DOI] [PubMed] [Google Scholar]
- Cimochowski GE, Worley E, Rutherford WE, et al. Superiority of the internal jugular over the subclavian access for temporary dialysis. Nephron. 1990;54:154 –161. doi: 10.1159/000185837. [DOI] [PubMed] [Google Scholar]
- Schillinger F, Schillinger D, Montagnac R, et al. Post catheterisation vein stenosis in haemodialysis: comparative angiographic study of 50 subclavi an and 50 internal jugular accesses. Nephrol Dial Transplant. 1991;6:722 –724. doi: 10.1093/ndt/6.10.722. [DOI] [PubMed] [Google Scholar]
- Oguzkurt L, Tercan F, Torun D, et al. Impact of short-term hemodialysi s catheters on the central veins: a catheter venographic study. Eur J Radiol. 2004;52:293 –299. doi: 10.1016/j.ejrad.2003.12.004. [DOI] [PubMed] [Google Scholar]
- Taal MW, Chesterton LJ, McIntyre CW. Venography at insertion of tunnelled internal jugular vein dialysis catheters reveals significant occult stenosis. Nephrol Dial Transplant. 2004;19:1542 –1545. doi: 10.1093/ndt/gfh216. [DOI] [PubMed] [Google Scholar]
- Agarwal AK, Patel BM, Haddad NJ. Central vein stenosis: a nephrologist's perspective. Semin Dial. 2007;20:53 –62. doi: 10.1111/j.1525-139X.2007.00242.x. [DOI] [PubMed] [Google Scholar]
- Puel V, Caudry M, Le Metayer P, et al. Superior vena cava thrombosis related to catheter malposition in cancer chemotherapy given through implanted ports. Cancer. 1993;72:2248 –2252. doi: 10.1002/1097-0142(19931001)72:7<2248::aid-cncr2820720731>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Yevzlin AS. Hemodialysis catheter-associated central venous stenosis. Semin Dial. 2008;21:522 –527. doi: 10.1111/j.1525-139X.2008.00496.x. [DOI] [PubMed] [Google Scholar]
- Pronovost P. Interventions to decrease catheter-related bloodstream infections in the ICU: the Keystone Intensive Care Unit Project. Am J Infect Control. 2008;36:S171 e171–S171 e175. doi: 10.1016/j.ajic.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Parienti JJ, Thirion M, Megarbane B, et al. Femoral vs jugular venous catheterization and risk of nosocomial events in adults requiring acute renal replacement therapy: a randomized controlled trial. JAMA. 2008;299:2413 –2422. doi: 10.1001/jama.299.20.2413. [DOI] [PubMed] [Google Scholar]
- Hryszko T, Brzosko S, Mazerska M, et al. Risk factors of nontunneled noncuffed hemodialysis catheter malfunction. A prospective study. Nephron Clin Pract. 2004;96:c43 –c47. doi: 10.1159/000076398. [DOI] [PubMed] [Google Scholar]
- Liangos O, Rao M, Ruthazer R, et al. Factors associated with urea reduction ratio in acute renal failure. Artif Organs. 2004;28:1076 –1081. doi: 10.1111/j.1525-1594.2004.00023.x. [DOI] [PubMed] [Google Scholar]
- Naumovic RT, Jovanovic DB, Djukanovic LJ. Temporary vascular catheters for hemodialysis: a 3-year prospective study. Int J Artif Organs. 2004;27:848 –854. doi: 10.1177/039139880402701006. [DOI] [PubMed] [Google Scholar]
- Oliver MJ, Edwards LJ, Treleaven DJ, et al. Randomized study of temporary hemodialysis catheters. Int J Artif Organs. 2002;25:40 –44. doi: 10.1177/039139880202500107. [DOI] [PubMed] [Google Scholar]
- Parienti JJ, Megarbane B, Fischer MO, et al. Catheter dysfunction and dialysis performance according to vascular access among 736 critically ill adults requiring renal replacement therapy: a randomized controlled study. Crit Care Med. 2010;38:1118 –1125. doi: 10.1097/CCM.0b013e3181d454b3. [DOI] [PubMed] [Google Scholar]
- Marschall J, Mermel LA, Classen D, et al. Strategies to prevent central line-associ ated bloodstream infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29 (Suppl 1) :S22 –S30. doi: 10.1086/591059. [DOI] [PubMed] [Google Scholar]
- Pratt RJ, Pellowe CM, Wilson JA, et al. epic2: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2007;65 (Suppl 1) :S1 –64. doi: 10.1016/S0195-6701(07)60002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusminsky RE. Complications of central venous catheterization. J Am Coll Surg. 2007;204:681 –696. doi: 10.1016/j.jamcollsurg.2007.01.039. [DOI] [PubMed] [Google Scholar]
- McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348:1123 –1133. doi: 10.1056/NEJMra011883. [DOI] [PubMed] [Google Scholar]
- Hind D, Calvert N, McWilliams R, et al. Ultrason ic locating devices for central venous cannulation: meta-analysis. BMJ. 2003;327:361 . doi: 10.1136/bmj.327.7411.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randolph AG, Cook DJ, Gonzales CA, et al. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996;24:2053 –2058. doi: 10.1097/00003246-199612000-00020. [DOI] [PubMed] [Google Scholar]
- Karakitsos D, Labropoulos N, De Groot E, et al. Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10:R162 . doi: 10.1186/cc5101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung J, Duffy M, Finckh A. Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complication s: a randomized, prospective study. Ann Emerg Med. 2006;48:540 –547. doi: 10.1016/j.annemergmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Bansal R, Agarwal SK, Tiwari SC, et al. A prospective randomized study to compare ultrasound-guided with nonultrasound-guided double lumen internal jugular catheter insertion as a temporary hemodialysis access. Ren Fail. 2005;27:561 –564. doi: 10.1080/08860220500199084. [DOI] [PubMed] [Google Scholar]
- Farrell J, Gellens M. Ultrasound-guided cannulation versus the landmark-guided technique for acute haemodialysis access. Nephrol Dial Transplant. 1997;12:1234 –1237. doi: 10.1093/ndt/12.6.1234. [DOI] [PubMed] [Google Scholar]
- Gallieni M. Central vein catheterization of dialysis patients with real time ultrasound guidance. J Vasc Access. 2000;1:10 –14. doi: 10.1177/112972980000100104. [DOI] [PubMed] [Google Scholar]
- Kwon TH, Kim YL, Cho DK. Ultrasound-guided cannulation of the femoral vein for acute haemodialysis access. Nephrol Dial Transplant. 1997;12:1009 –1012. doi: 10.1093/ndt/12.5.1009. [DOI] [PubMed] [Google Scholar]
- Lin BS, Huang TP, Tang GJ, et al. Ultrasound-guided cannulation of the internal jugular vein for dialysis vascular access in uremic patients. Nephron. 1998;78:423 –428. doi: 10.1159/000044971. [DOI] [PubMed] [Google Scholar]
- Nadig C, Leidig M, Schmiedeke T, et al. The use of ultrasound for the placement of dialysis catheters. Nephrol Dial Transplant. 1998;13:978 –981. doi: 10.1093/ndt/13.4.978. [DOI] [PubMed] [Google Scholar]
- Zollo A, Cavatorta F, Galli S. Ultrasound-guided cannulation of the femoral vein for acute hemodialysis access with silicone catheters. J Vasc Access. 2001;2:56 –59. doi: 10.1177/112972980100200206. [DOI] [PubMed] [Google Scholar]
- Schummer W, Sakr Y, Schummer C.Towards optimal central venous catheter tip positionIn: Vincent J-L (ed).Intensive Care Medicine Springer Verlag: Berlin, Germany; 2008581–590. [Google Scholar]
- Vesely TM. Central venous catheter tip position: a continui ng controversy. J Vasc Interv Radiol. 2003;14:527 –534. doi: 10.1097/01.rvi.0000071097.76348.72. [DOI] [PubMed] [Google Scholar]
- Hsu JH, Wang CK, Chu KS, et al. Comparison of radiographic landmarks and the echocardiographic SVC/RA junction in the positioning of long-term central venous catheters. Acta Anaesthesiol Scand. 2006;50:731 –735. doi: 10.1111/j.1399-6576.2006.01025.x. [DOI] [PubMed] [Google Scholar]
- James MT, Conley J, Tonelli M, et al. Meta-analysis: antibiotics for prophylaxis against hemodialysis catheter-related infections. Ann Intern Med. 2008;148:596 –605. doi: 10.7326/0003-4819-148-8-200804150-00004. [DOI] [PubMed] [Google Scholar]
- Jaffer Y, Selby NM, Taal MW, et al. A meta-analysis of hemodialysis catheter locking solutions in the prevention of catheter-related infection. Am J Kidney Dis. 2008;51:233 –241. doi: 10.1053/j.ajkd.2007.10.038. [DOI] [PubMed] [Google Scholar]
- Labriola L, Crott R, Jadoul M. Preventing haemodialysis catheter-related bacteraemia with an antimicrobial lock solution: a meta-analysis of prospective randomized trials. Nephrol Dial Transplant. 2008;23:1666 –1672. doi: 10.1093/ndt/gfm847. [DOI] [PubMed] [Google Scholar]
- Yahav D, Rozen-Zvi B, Gafter-Gvili A, et al. Antimicrobial lock solutions for the prevention of infections associated with intravascular catheters in patients undergoing hemodialysis: systematic review and meta-analysis of randomized, controlled trials. Clin Infect Dis. 2008;47:83 –93. doi: 10.1086/588667. [DOI] [PubMed] [Google Scholar]
- Hackbarth R, Bunchman TE, Chua AN, et al. The effect of vascular access location and size on circuit survival in pediatric continuous renal replacement therapy: a report from the PPCRRt registry. Int J Artif Organs. 2007;30:1116 –1121. doi: 10.1177/039139880703001212. [DOI] [PubMed] [Google Scholar]
- Bunchman TE, Brophy PD, Goldstein SL. Technical considerations for renal replacement therapy in children. Semin Nephrol. 2008;28:488 –492. doi: 10.1016/j.semnephrol.2008.05.009. [DOI] [PubMed] [Google Scholar]
- McDon ald SP, Craig JC. Long-term survival of children with end-stage renal disease. N Engl J Med. 2004;350:2654 –2662. doi: 10.1056/NEJMoa031643. [DOI] [PubMed] [Google Scholar]
- Chadha V, Warady BA, Blowey DL, et al. Tenckhoff catheters prove superior to cook catheters in pediatric acute peritoneal dialysis. Am J Kidney Dis. 2000;35:1111 –1116. doi: 10.1016/s0272-6386(00)70048-5. [DOI] [PubMed] [Google Scholar]
- Auron A, Warady BA, Simon S, et al. Use of the multipurpose drainage catheter for the provision of acute peritoneal dialysis in infants and children. Am J Kidney Dis. 2007;49:650 –655. doi: 10.1053/j.ajkd.2007.02.274. [DOI] [PubMed] [Google Scholar]
- Modi GK, Pereira BJ, Jaber BL. Hemodialysis in acute renal failure: does the membrane matter. Semin Dial. 2001;14:318 –321. doi: 10.1046/j.1525-139x.2001.00078.x. [DOI] [PubMed] [Google Scholar]
- Canivet E, Lavaud S, Wong T, et al. Cuprophane but not synthetic membrane induces increases in serum tumor necrosis factor-alpha levels during hemodialysis. Am J Kidney Dis. 1994;23:41 –46. doi: 10.1016/s0272-6386(12)80810-9. [DOI] [PubMed] [Google Scholar]
- Marchant A, Tielemans C, Husson C, et al. Cuprophane haemodialysis induces upregulation of LPS receptor (CD14) on monocytes: role of complement activation. Nephrol Dial Transplant. 1996;11:657 –662. doi: 10.1093/oxfordjournals.ndt.a027355. [DOI] [PubMed] [Google Scholar]
- Patarca R, Perez G, Gonzalez A, et al. Comprehensive evaluation of acute immunological changes induced by cuprophane and polysulfone membranes in a patient on chronic hemodialysis. Am J Nephrol. 1992;12:274 –278. doi: 10.1159/000168459. [DOI] [PubMed] [Google Scholar]
- Puentes F, Pons H, Rodriguez-Iturbe B. Hemodialysis with cuprophane membranes is associated with a reduction in peripheral blood mononuclear cells expressing VLA-4 cell adhesion molecule. Clin Nephrol. 1994;42:278 –279. [PubMed] [Google Scholar]
- Schaefer RM, Huber L, Gilge U, et al. Clinical evaluation of a new high-flux cellulose acetate membrane. Int J Artif Organs. 1989;12:85 –90. [PubMed] [Google Scholar]
- Walker RJ, Sutherland WH, De Jong SA. Effect of changing from a cellulose acetate to a polysulphone dialysis membrane on protein oxidation and inflammation markers. Clin Nephrol. 2004;61:198 –206. doi: 10.5414/cnp61198. [DOI] [PubMed] [Google Scholar]
- Itoh S, Susuki C, Tsuji T. Platelet activation through interaction with hemodialysis membranes induces neutrophils to produce reactive oxygen species. J Biomed Mater Res A. 2006;77:294 –303. doi: 10.1002/jbm.a.30608. [DOI] [PubMed] [Google Scholar]
- Hakim RM, Schafer AI. Hemodialysis-associated platelet activation and thrombocytopenia. Am J Med. 1985;78:575 –580. doi: 10.1016/0002-9343(85)90398-5. [DOI] [PubMed] [Google Scholar]
- Sirolli V, Strizzi L, Di Stante S, et al. Platelet activation and platelet-erythrocyte aggregates in end-stage renal disease patients on hemodialysis. Thromb Haemost. 2001;86:834 –839. [PubMed] [Google Scholar]
- Takeshita K, Susuki C, Itoh S, et al. Preventive effect of alpha-tocopherol and glycyrrhizin against platelet -neutrophil complex formation induced by hemodialysis membranes. Int J Artif Organs. 2009;32:282 –290. doi: 10.1177/039139880903200505. [DOI] [PubMed] [Google Scholar]
- Alonso A, Lau J, Jaber BL. Biocompatible hemodialysis membranes for acute renal failure. Cochrane Database Syst Rev. 2008. p. CD005283. [DOI] [PMC free article] [PubMed]
- Brophy PD, Mottes TA, Kudelka TL, et al. AN-69 membrane reactions are pH-dependent and preventable. Am J Kidney Dis. 2001;38:173 –178. doi: 10.1053/ajkd.2001.25212. [DOI] [PubMed] [Google Scholar]
- Hackbarth RM, Eding D, Gianoli Smith C, et al. Zero balance ultrafiltration (Z-BUF) in blood-primed CRRT circuits achieves electrolyte and acid-base homeostasis prior to patient connection. Pediatr Nephrol. 2005;20:1328 –1333. doi: 10.1007/s00467-005-1970-1. [DOI] [PubMed] [Google Scholar]
- Pasko DA, Mottes TA, Mueller BA. Pre dialysis of blood prime in continuous hemodialysis normalizes pH and electrolytes. Pediatr Nephrol. 2003;18:1177 –1183. doi: 10.1007/s00467-003-1258-2. [DOI] [PubMed] [Google Scholar]
- Perez-Garcia R, Galan A, Garcia Vinuesa M, et al. Anaphylactoid reactions during hemodialysis on AN69 membranes: role of ACE inhibitors and back-filtration. Nephron. 1992;61:123 . doi: 10.1159/000186855. [DOI] [PubMed] [Google Scholar]
- Petrie JJ, Campbell Y, Hawley CM, et al. Anaphylactoid reactions in patients on hemodiafiltration with AN69 membranes whilst receiving ACE inhibitors. Clin Nephrol. 1991;36:264 –265. [PubMed] [Google Scholar]
- Tielemans C, Madhoun P, Lenaers M, et al. Anaphylactoid reactions during hemodialysi s on AN69 membranes in patients receiving ACE inhibitors. Kidney Int. 1990;38:982 –984. doi: 10.1038/ki.1990.301. [DOI] [PubMed] [Google Scholar]
- Desormeaux A, Moreau ME, Lepage Y, et al. The effect of electronegativity and angiotensin-converting enzyme inhibition on the kinin-forming capacity of polyacrylonitrile dialysis membranes. Biomaterials. 2008;29:1139 –1146. doi: 10.1016/j.biomaterials.2007.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RENAL Study Investigators Renal replacement therapy for acute kidney injury in Australian and New Zealand intensive care units: a practice survey. Crit Care Resusc. 2008;10:225 –230. [PubMed] [Google Scholar]
- Gatward JJ, Gibbon GJ, Wrathall G, et al. Renal replacement therapy for acute renal failure: a survey of practice in adult intensive care units in the United Kingdom. Anaesthesia. 2008;63:959 –966. doi: 10.1111/j.1365-2044.2008.05514.x. [DOI] [PubMed] [Google Scholar]
- Langford S, Slivar S, Tucker SM, et al. Exploring CRRT practices in ICU: a survey of Canadian hospitals. Dynamics. 2008;19:18 –23. [PubMed] [Google Scholar]
- Rabindranath K, Adams J, Macleod AM, et al. Intermittent versus continuous renal replacement therapy for acute renal failure in adults. Cochrane Database Syst Rev. 2007. p. CD003773. [DOI] [PubMed]
- Bagshaw SM, Berthiaume LR, Delaney A, et al. Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: a meta-analysis. Crit Care Med. 2008;36:610 –617. doi: 10.1097/01.CCM.0B013E3181611F552. [DOI] [PubMed] [Google Scholar]
- Pan nu N, Klarenbach S, Wiebe N, et al. Renal replacement therapy in patients with acute renal failure: a systematic review. JAMA. 2008;299:793 –805. doi: 10.1001/jama.299.7.793. [DOI] [PubMed] [Google Scholar]
- Lins RL, Elseviers MM, Van der Niepen P, et al. Intermittent versus continuous renal replacement therapy for acute kidney injury patients admitted to the intensive care unit: results of a randomized clinical trial. Nephrol Dial Transplant. 2009;24:512 –518. doi: 10.1093/ndt/gfn560. [DOI] [PubMed] [Google Scholar]
- Farese S, Jakob SM, Kalicki R, et al. Treatment of acute renal failure in the intensive care unit: lower costs by intermittent dialysis than continuous venovenous hemodiafiltration. Artif Organs. 2009;33:634 –640. doi: 10.1111/j.1525-1594.2009.00794.x. [DOI] [PubMed] [Google Scholar]
- Klarenbach S, Manns B, Pannu N, et al. Economic evaluation of continuous renal replacement therapy in acute renal failure. Int J Technol Assess Health Care. 2009;25:331 –338. doi: 10.1017/S0266462309990134. [DOI] [PubMed] [Google Scholar]
- Srisawat N, Lawsin L, Uchino S, et al. Cost of acute renal replacement therapy in the intensive care unit: results from The Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) study. Crit Care. 2010;14:R46 . doi: 10.1186/cc8933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell M, Granath F, Schon S, et al. Continuous renal replacement therapy is associated with less chronic renal failure than intermittent haemodialysis after acute renal failure. Intensive Care Med. 2007;33:773 –780. doi: 10.1007/s00134-007-0590-6. [DOI] [PubMed] [Google Scholar]
- Jacka MJ, Ivancinova X, Gibney RT. Continuous renal replacement therapy improves renal recovery from acute renal failure. Can J Anaesth. 2005;52:327 –332. doi: 10.1007/BF03016071. [DOI] [PubMed] [Google Scholar]
- Uchino S, Bellomo R, Kellum JA, et al. Patient and kidney survival by dialysis modality in critically ill patients with acute kidney injury. Int J Artif Organs. 2007;30:281 –292. doi: 10.1177/039139880703000402. [DOI] [PubMed] [Google Scholar]
- Kielstein JT, Schiffer M, Hafer C. Back to the future: extended dialysis for treatment of acute kidney injury in the intensive care unit. J Nephrol. 2010;23:494 –501. [PubMed] [Google Scholar]
- Kielstein JT, Kretschmer U, Ernst T, et al. Efficacy and cardiovascular tolerability of extended dialysis in critically ill patients: a randomized controlled study. Am J Kidney Dis. 2004;43:342 –349. doi: 10.1053/j.ajkd.2003.10.021. [DOI] [PubMed] [Google Scholar]
- Baldwin I, Bellomo R, Naka T, et al. A pilot randomized controlled comparison of extended daily dialysis with filtration and continuous veno-venous hemofiltration: fluid removal and hemodynamics. Int J Artif Organs. 2007;30:1083 –1089. doi: 10.1177/039139880703001208. [DOI] [PubMed] [Google Scholar]
- Baldwin I, Naka T, Koch B, et al. A pilot randomised controlled comparison of continuous veno-venous haemofiltration and extended daily dialysis with filtration: effect on small solutes and acid-base balance. Intensive Care Med. 2007;33:830 –835. doi: 10.1007/s00134-007-0596-0. [DOI] [PubMed] [Google Scholar]
- Marshall MR, Creamer JM, Foster M, et al. Mortality rate comparison after switching from continuous to prolonged intermittent renal replacement for acute kidney injury in three intensive care units from different countries. Nephrol Dial Transplant. 2011;26:2169 –2175. doi: 10.1093/ndt/gfq694. [DOI] [PubMed] [Google Scholar]
- Fieghen HE, Friedrich JO, Burns KE, et al. The hemodynamic tolerability and feasibility of sustained low efficiency dialysis in the management of critically ill patients with acute kidney injury. BMC Nephrol. 2010;11:32 . doi: 10.1186/1471-2369-11-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport A. Continuous renal replacement therapies in patients with acute neurological injury. Semin Dial. 2009;22:165 –168. doi: 10.1111/j.1525-139X.2008.00548.x. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Peets AD, Hameed M, et al. Dialysis Disequilibrium Syndrome: brain death following hemodialysis for metabolic acidosis and acute renal failure--a case report. BMC Nephrol. 2004;5:9 . doi: 10.1186/1471-2369-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CM, Lin JW, Tsai JT, et al. Intracran ial pressure fluctuation during hemodialysis in renal failure patients with intracranial hemorrhage. Acta Neurochir Suppl. 2008;101:141 –144. doi: 10.1007/978-3-211-78205-7_24. [DOI] [PubMed] [Google Scholar]
- Ronco C, Bellomo R, Brendolan A, et al. Brain density changes during renal replacement in critically ill patients with acute renal failure. Continuous hemofiltration versus intermittent hemodialysis. J Nephrol. 1999;12:173 –178. [PubMed] [Google Scholar]
- Paganini EP, Sandy D, Moreno L, et al. The effect of sodium and ultrafiltration modelling on plasma volume changes and haemodynamic stability in intensive care patients receiving haemodialysis for acute renal failure: a prospective, stratified, ra ndomized, cross-over study. Nephrol Dial Transplant. 1996;11 (Suppl 8) :32 –37. doi: 10.1093/ndt/11.supp8.32. [DOI] [PubMed] [Google Scholar]
- Schortgen F, Soubrier N, Delclaux C, et al. Hemodynamic tolerance of intermittent hemodialysis in critically ill patients: usefulness of practice guidelines. Am J Respir Crit Care Med. 2000;162:197 –202. doi: 10.1164/ajrccm.162.1.9907098. [DOI] [PubMed] [Google Scholar]
- Bargman JM. New technologies in peritoneal dialysis. Clin J Am Soc Nephrol. 2007;2:576 –580. doi: 10.2215/CJN.03331006. [DOI] [PubMed] [Google Scholar]
- Chionh CY, Soni S, Cruz DN, et al. Peritoneal dialysis for acute kidney injury: techniques and dose. Contrib Nephrol. 2009;163:278 –284. doi: 10.1159/000223811. [DOI] [PubMed] [Google Scholar]
- Ronco C, Amerling R. Continuous flow peritoneal dialysis: current state-of-the-art and obstacles to further development. Contrib Nephrol. 2006;150:310 –320. doi: 10.1159/000093625. [DOI] [PubMed] [Google Scholar]
- Phu NH, Hien TT, Mai NT, et al. Hemofiltration and peritoneal dialysis in infection-associated acute renal failure in Vietnam. N Engl J Med. 2002;347:895 –902. doi: 10.1056/NEJMoa020074. [DOI] [PubMed] [Google Scholar]
- Gabriel DP, Caramori JT, Martim LC, et al. High volume peritoneal dialysis vs daily hemodialysis: a randomized, controlled trial in patients with acute kidney injury. Kidney Int Suppl. 2008. pp. S87–S93. [DOI] [PubMed]
- Vachvanichsanong P, Dissaneewate P, Lim A, et al. Childhood acute renal failure: 22-year experience in a university hospital in southern Thailand. Pediatrics. 2006;118:e786 –e791. doi: 10.1542/peds.2006-0557. [DOI] [PubMed] [Google Scholar]
- Bailey D, Phan V, Litalien C, et al. Risk factors of acute renal failure in critically ill children: A prospective descriptive epidemiological study. Pediatr Crit Care Med. 2007;8:29 –35. doi: 10.1097/01.pcc.0000256612.40265.67. [DOI] [PubMed] [Google Scholar]
- Bunchman TE, Maxvold NJ, Kershaw DB, et al. Continuous venovenous hemodiafiltration in infants and children. Am J Kidney Dis. 1995;25:17 –21. doi: 10.1016/0272-6386(95)90618-5. [DOI] [PubMed] [Google Scholar]
- Sadowski RH, Harmon WE, Jabs K. Acute hemodialysis of infants weighing less than five kilograms. Kidney Int. 1994;45:903 –906. doi: 10.1038/ki.1994.119. [DOI] [PubMed] [Google Scholar]
- Symons JM, Brophy PD, Gregory MJ, et al. Continuous renal replacement therapy in children up to 10 kg. Am J Kidney Dis. 2003;41:984 –989. doi: 10.1016/s0272-6386(03)00195-1. [DOI] [PubMed] [Google Scholar]
- Warady BA, Bunchman T. Dialysis therapy for children with acute renal failure: survey results. Pediatr Nephrol. 2000;15:11 –13. doi: 10.1007/s004670000420. [DOI] [PubMed] [Google Scholar]
- Bunchman TE, McBryde KD, Mottes TE, et al. Pediatric acute renal failure: outcome by modality and disease. Pediatr Nephrol. 2001;16:1067 –1071. doi: 10.1007/s004670100029. [DOI] [PubMed] [Google Scholar]
- Flores FX, Brophy PD, Symons JM, et al. Continuous renal replacement therapy (CRRT) after stem cell transplantation. A report from the prospective pediatric CRRT Registry Group. Pediatr Nephrol. 2008;23:625 –630. doi: 10.1007/s00467-007-0672-2. [DOI] [PubMed] [Google Scholar]
- Noris M, Todeschini M, Casiraghi F, et al. Effect of acetate, bicarbonate dialysis, and acetate-free biofiltration on nitric oxide synthesis: implications for dialysis hypotension. Am J Kidney Dis. 1998;32:115 –124. doi: 10.1053/ajkd.1998.v32.pm9669432. [DOI] [PubMed] [Google Scholar]
- Levraut J, Ichai C, Petit I, et al. Low exogenous lactate clearance as an early predictor of mortality in normolactatemic critically ill septic patients. Crit Care Med. 2003;31:705 –710. doi: 10.1097/01.CCM.0000045561.85810.45. [DOI] [PubMed] [Google Scholar]
- Veech RL. The untoward effects of the anions of dialysis fluids. Kidn ey Int. 1988;34:587 –597. doi: 10.1038/ki.1988.223. [DOI] [PubMed] [Google Scholar]
- Barenbrock M, Hausberg M, Matzkies F, et al. Effects of bicarbonate- and lactate-buffered replacement fluids on cardiovascular outcome in CVVH patients. Kidney Int. 2000;58:1751 –1757. doi: 10.1046/j.1523-1755.2000.00336.x. [DOI] [PubMed] [Google Scholar]
- McLean AG, Davenport A, Cox D, et al. Effects of lactate-buffered and lactate-free dialysate in CAVHd patients with and without liver dysfunction. Kidney Int. 2000;58:1765 –1772. doi: 10.1046/j.1523-1755.2000.00338.x. [DOI] [PubMed] [Google Scholar]
- Thomas AN, Guy JM, Kishen R, et al. Comparison of lactate and bicarbon ate buffered haemofiltration fluids: use in critically ill patients. Nephrol Dial Transplant. 1997;12:1212 –1217. doi: 10.1093/ndt/12.6.1212. [DOI] [PubMed] [Google Scholar]
- Tan HK, Uchino S, Bellomo R. The acid-base effects of continuous hemofiltration with lactate or bicarbonate buffered replacement fluids. Int J Artif Organs. 2003;26:477 –483. doi: 10.1177/039139880302600605. [DOI] [PubMed] [Google Scholar]
- Zimmerman D, Cotman P, Ting R, et al. Continuous veno-venous haemodialysis with a novel bicarbonate dialysis solution: prospective cross-over comparison with a lactate buffered solution. Nephrol Dial Transplant. 1999;14:2387 –2391. doi: 10.1093/ndt/14.10.2387. [DOI] [PubMed] [Google Scholar]
- Holloway P, Benham S, St John A. The value of blood lactate measurements in ICU: an evaluation of the role in the managemen t of patients on haemofiltration. Clin Chim Acta. 2001;307:9 –13. doi: 10.1016/s0009-8981(01)00449-1. [DOI] [PubMed] [Google Scholar]
- Ledebo I. On-line preparation of solutions for dialysis: practical aspects versus safety and regulations. J Am Soc Nephrol. 2002;13 (Suppl 1) :S78 –S83. [PubMed] [Google Scholar]
- Marshall MR, Ma T, Galler D, et al. Sustained low-efficiency daily diafiltration (SLEDD-f) for critically ill patients requiring renal replacement therapy: towards an adequate therapy. Nephrol Dial Transplant. 2004;19:877 –884. doi: 10.1093/ndt/gfg625. [DOI] [PubMed] [Google Scholar]
- Ronco C. Backfiltration in clinical dialysis: nature of the phenomenon, mechanisms and possible solutions. Int J Artif Organs. 1990;13:11 –21. [PubMed] [Google Scholar]
- Kanagasundaram NS, Larive AB, Paganini EP. A preliminary survey of bacterial contamination of the dialysate circuit in continuous veno-venous hemodialysis. Clin Nephrol. 2003;59:47 –55. doi: 10.5414/cnp59047. [DOI] [PubMed] [Google Scholar]
- Moore I, Bhat R, Hoenich NA, et al. A microbiological survey of bicarbonate-based replacement circuits in continuous veno-venous hemofiltration. Crit Care Med. 2009;37:496 –500. doi: 10.1097/CCM.0b013e3181957987. [DOI] [PubMed] [Google Scholar]
- Ward RA. Worldwide guidelines for the preparation and quality management of dialysis fluid and their implementation. Blood Purif. 2009;27 (Suppl 1) :2 –4. doi: 10.1159/000213489. [DOI] [PubMed] [Google Scholar]
- Association for the Advancement of Medical Instrumentation Water for Hemodialysis and Related TherapiesANSI/AAMI/ISO 13959:2009.AAMI: Arlington, VA; 2010 [Google Scholar]
- Association for the Advancement of Medical Instrumentation Concentrates for Hemodialysis and Related TherapiesANSI/AAMI/ISO 13958:2009.AAMI: Arlington, VA; 2011 [Google Scholar]
- Association for the Advancement of Medical Instrumentation Quality of Dialysis Fluid for Hemodialysis and Related TherapiesANSI/AAMI/ISO 11663:2009.AAMI: Arlington, VA; 2010 [Google Scholar]
- European best practice guidelines for haemodialys is (Part 1). Section IV: Dialysis fluid purity. Nephrol Dial Transplant. 2002;17 (Suppl) :45 –62. [PubMed] [Google Scholar]
- Kolff WJ. First clinical experience with the artificial kidney. Ann Intern Med. 1965;62:608 –619. doi: 10.7326/0003-4819-62-3-608. [DOI] [PubMed] [Google Scholar]
- Davenport A, Bouman C, Kirpalani A, et al. Delivery of renal replacement therapy in acute kidney injury: what are the key issues. Clin J Am Soc Nephrol. 2008;3:869 –875. doi: 10.2215/CJN.04821107. [DOI] [PubMed] [Google Scholar]
- Faulhaber-Walter R, Hafer C, Jahr N, et al. The Hannover Dialysis Outcome study: comparison of standard versus intensified extended dialysis for treatment of patients with acute kidney injury in the intensive care unit. Nephrol Dial Transplant. 2009;24:2179 –2186. doi: 10.1093/ndt/gfp035. [DOI] [PubMed] [Google Scholar]
- Ronco C, Bellomo R, Homel P, et al. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet. 2000;356:26 –30. doi: 10.1016/S0140-6736(00)02430-2. [DOI] [PubMed] [Google Scholar]
- Saudan P, Niederberger M, De Seigneux S, et al. Adding a dialysis dose to continuous hemofiltration increases survival in patients with acute renal failure. Kidney Int. 2006;70:1312 –1317. doi: 10.1038/sj.ki.5001705. [DOI] [PubMed] [Google Scholar]
- Schiffl H, Lang SM, Fischer R. Daily hemodialysis and the outcome of acute renal failure. N Engl J Med. 2002;346:305 –310. doi: 10.1056/NEJMoa010877. [DOI] [PubMed] [Google Scholar]
- Tolwani AJ, Campbell RC, Stofan BS, et al. Standard versus high-dose CVVHDF for ICU-related acute renal failure. J Am Soc Nephrol. 2008;19:1233 –1238. doi: 10.1681/ASN.2007111173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paganini EP, Tapolyai M, Goormastic M, et al. Establishing a dialysis therapy/pat ient outcome link in intensive care unit acute dialysis for patients with acute renal failure. Am J Kidney Dis. 1996;28 (Suppl 3) :S81 –S89. [Google Scholar]
- Ricci Z, Ronco C, D’Amico G, et al. Practice patterns in the management of acute renal failure in the critically ill patient: an international survey. Nephrol Dial Transplant. 2006;21:690 –696. doi: 10.1093/ndt/gfi296. [DOI] [PubMed] [Google Scholar]
- Ikizler TA, Sezer MT, Flakoll PJ, et al. Urea space and total body water measurements by stable isotopes in patients with acute renal failure. Kidney Int. 2004;65:725 –732. doi: 10.1111/j.1523-1755.2004.00439.x. [DOI] [PubMed] [Google Scholar]
- Evanson JA, Ikizler TA, Wingard R, et al. Measurement of the delivery of dialysis in acute renal failure. Kidney Int. 1999;55:1501 –1508. doi: 10.1046/j.1523-1755.1999.00355.x. [DOI] [PubMed] [Google Scholar]
- Evanson JA, Himmelfarb J, Wingard R, et al. Prescribed versus delivered dialysis in acute renal failure patients. Am J Kidney Dis. 1998;32:731 –738. doi: 10.1016/s0272-6386(98)70127-1. [DOI] [PubMed] [Google Scholar]
- Schiffl H. Disease severity adversely affects delivery of dialysis in acute renal failure. Nephron Clin Pract. 2007;107:c163 –c169. doi: 10.1159/000110592. [DOI] [PubMed] [Google Scholar]
- Gotch FA, Sargent JA. A mechanistic analysis of the National Cooperative Dialysis Study (NCDS) Kidney Int. 1985;28:526 –534. doi: 10.1038/ki.1985.160. [DOI] [PubMed] [Google Scholar]
- Held PJ, Port FK, Wolfe RA, et al. The dose of hemodialysis and patient mortality. Kidney Int. 1996;50:550 –556. doi: 10.1038/ki.1996.348. [DOI] [PubMed] [Google Scholar]
- Eknoyan G, Beck GJ, Cheung AK, et al. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med. 2002;347:2010 –2019. doi: 10.1056/NEJMoa021583. [DOI] [PubMed] [Google Scholar]
- Venkataraman R, Kellum JA, Palevsky P. Dosing patterns for continuous renal replacement therapy at a large academic medical center in the United States. J Crit Care. 2002;17:246 –250. doi: 10.1053/jcrc.2002.36757. [DOI] [PubMed] [Google Scholar]
- Boussekey N, Chiche A, Faure K, et al. A pilot randomized study comparing high and low volume hemofiltration on vasopressor use in septic shock. Intensive Care Med. 2008;34:1646 –1653. doi: 10.1007/s00134-008-1127-3. [DOI] [PubMed] [Google Scholar]