Abstract
Cardiovascular disease is an important cause of morbidity and mortality in patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD). All epidemiological studies have clearly shown that accelerated arterial and cardiac aging is characteristic of these populations. Arterial premature aging is heterogeneous. It principally involves the aorta and central capacitive arteries, and is characterized by preferential aortic stiffening and disappearance of stiffness/impedance gradients between the central and peripheral arteries. These changes have a double impact: on the heart, upstream, with left ventricular hypertrophy and decreased coronary perfusion; and, downstream, on renal and brain microcirculation (decrease in glomerular filtration and cognitive functions). Multifactorial at origin, the pathophysiology of aortic ‘progeria' and microvascular disorders in CKD/ESRD is not well understood and should be the focus of interest in future studies.
Keywords: aging, arteriosclerosis, arterial stiffness, end-stage renal disease, pressure waves
The heart and kidney are frequently affected by similar, highly prevalent risk factors such as diabetes and hypertension, and both are profoundly affected by the aging process.
Atherosclerosis is a generalized arterial disease of the arterial intima, characterized by the presence of plaques and occlusive arterial lesions. Atherosclerosis extends from the coronaries and the thoracic aorta to the renal circulation. Nephrosclerosis, that is, the renal expression of intimal disease (either alone or associated with occlusive renal artery disease), is the most frequent renal disease underlying the high prevalence of chronic kidney disease (CKD) in the general population. Even though most patients with CKD die because of atherosclerotic complications before they reach end-stage renal disease (ESRD), the dialysis population is composed mainly of elderly patients with a high burden of cardiovascular complications. Kidney failure accelerates the progression of atherosclerosis and modifies the morphology of atherosclerosis lesions by increasing the propensity to calcification.1
Aging and age-associated arterial changes underlie fundamentally different alterations from atherosclerosis, and alterations attributable to the aging process may have a relevant effect on cardiac and renal disease. Aging per se is associated with a parallel decrease in renal function and is accompanied by relevant changes in the properties of large- and medium-sized arteries. The main structural changes attributable to aging include arterial dilatation and tortuousness, wall hypertrophy, and increased collagen-to-elastin ratio with fragmentation and calcification of elastic fibers. The functional consequence of these structural alterations is hardening/sclerosis of vessel walls (arteriosclerosis) and loss of distensibility, that is, increased stiffness.2 Arterial aging mainly involves the aorta and major central arteries, whereas peripheral muscular conduit arteries undergo only modest changes.3 In young and middle-aged subjects the aorta is more distensible than peripheral arteries. Physiologically, the higher distensibility of the aorta coupled with a progressively lower distensibility in peripheral vessels creates a ‘stiffness gradient' that works as a ‘hydraulic filter' and acts to buffer pressure pulsations and their transmission to microcirculation and capillary network principally in the main parenchymal organs such as the kidney and the brain.4 In brief, during systole, the stroke volume interacts with aortic characteristics to produce a pulsatile pressure wave (forward pressure) that normally travels from the aorta toward peripheral arteries at a pulse wave velocity (PWV) that accelerates centrifugally. PWV is low in the distensible aorta and accelerates in progressively stiffer peripheral arteries. During heart contraction, only a part of the stroke volume is forwarded directly to the peripheral tissues. The pressure generated by the left ventricular (LV) systole distends the elastic elements of the arterial walls and is transformed into an elastic force, while a part of the stroke volume is accommodated in the distended aorta. During diastole, this elastic force recoils the aorta and squeezes the blood forward into the peripheral tissues, thereby ensuring a continuous flow.5, 6 For this function to be efficient, the energy necessary for arterial distension and recoil should be as low as possible; that is, for a given stroke volume, the pulse pressure should be as low as possible. In other words, the more distensible the arterial wall (that is, the lower the stiffness), the smoother the provision of proper flow to peripheral tissues. As the forward pressure wave travels toward the less distensible and smaller peripheral arteries, impedance mismatches generate a reflected wave, that is, a wave that travels backward toward the aorta (reflected wave). In physiological conditions, the reflected wave returns normally to the aorta in late systole and early diastole (distensible aorta with low PWV), producing a favorable increase in diastolic pressure and in coronary perfusion and effectively limiting the transmission of high pulsatile energy to microcirculation.5, 6, 7
Aortic stiffening manifests as high systolic and pulse pressures with increased cardiac afterload and arterial circumferential stress, all factors promoting LV hypertrophy (LVH), which may evolve toward heart failure. Arterial rigidity increases the PWV and determines an early return of the reflected wave. This wave reaches the central circulation during early rather than late systole and late diastole, thereby increasing systolic and pulse pressure and decreasing diastolic pressure.5, 7 Stiff aorta cannot be stretched, and therefore the stroke volume flows through the arterial system toward peripheral tissues principally during systole, decreasing capillary transit time and metabolic exchanges. This is an energy-demanding hemodynamic pattern implying a high cardiac energy expenditure and a high oxygen consumption in the myocardium, thereby favoring cardiac ischemia. Importantly, in such a situation, the lack of proper aortic buffering also determines a direct transmission of pulsatile energy into the peripheral microvessels and microcirculatory network.4, 8 Arterioles are the ‘last barrier' protecting the capillary microcirculation from high pulsatile energy. In the presence of central stiffness and the associated loss of the arterial system distensibility gradient, organs characterized by high blood flow and low resistance, such as the kidney or the brain, are particularly exposed to the damaging effect of high pulsatile pressure.8 Strong associations have been described between aortic stiffness (aortic PWV) and LVH and LV dysfunction, as well as between the same parameters and indicators of renal dysfunction (glomerular filtration rate and microalbuminuria).9 In addition, aortic stiffness and pulse pressure have been associated with cognitive impairment and dementia.10 Age-associated aortic stiffening notoriously occurs at a much accelerated rate in ESRD patients.11 In this population, arterial rigidity is typically associated with calcifications, and PWV in ESRD reaches the highest level observed in human diseases.12 PWV represents one of the strongest markers for the risk of death and cardiovascular outcomes in dialysis patients.11, 12 Similar to the general population, arterial stiffening in ESRD is mainly confined to the aorta.3, 4, 11, 13
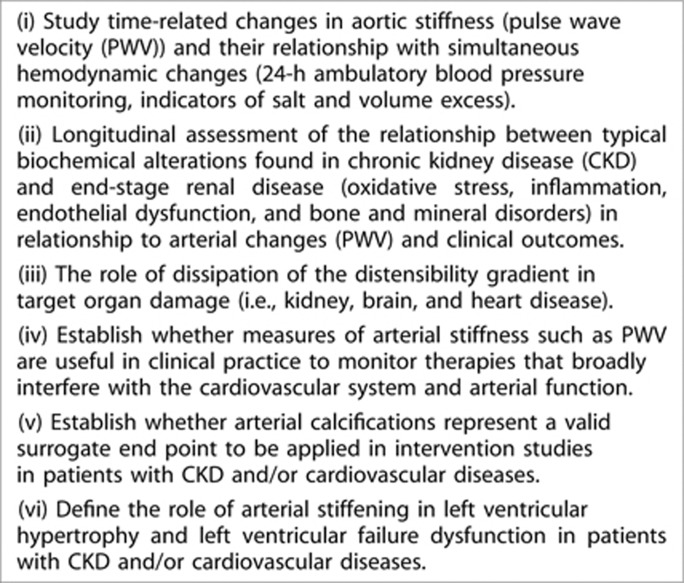
The rational schema laid down above provides a general framework for interpretation of the role of age-associated arterial changes in cardiovascular and renal diseases and for framing urgent research questions in this area. Indeed, the causes and consequences of age-dependent arterial abnormalities are not well understood and should be the focus of interest in future studies. In this regard, many critical questions still remain to be properly addressed (Figure 1).
Figure 1.
Remaining questions to be addressed.
Aortic stiffening could be analyzed by several techniques, including aortic PWV.14 Information on time-related changes in aortic stiffness as related to hemodynamic changes (24-h ambulatory blood pressure monitoring, extracellular volume, and indicators of salt and volume excess) and renal function is still scarce, which is why it is critical to probe the general relevance of the stiffening process in cardiovascular and renal health.
Longitudinal analyses of the relationship between the typical biochemical alterations of CKD and ESRD, such as high levels of oxidative stress, inflammation, endothelial dysfunction (see previous section), and markers of mineral disorders, PWV, and clinical outcomes, are needed to identify causal risk factors for arterial stiffening and cardiovascular risk excess in CKD and ESRD. Equally important is investigating the relationship between the biochemical alterations of CKD and PWV in peripheral arteries (carotido-radial or femoro-tibial) in order to understand the role of dissipation of the distensibility gradient in target organ damage (that is, kidney, brain, and heart disease). Studies of the microvascular structure and reactivity in the kidney, heart, and brain are the ‘parent pauvre' in CKD and ESRD. Techniques exist to study the microvascular territory at the anatomic level (cutaneous, nail, retinal capillary density) or at the functional level (in terms of postischemic forearm vasodilation and flow), but the best way to measure microvascular reactivity within the kidney circulation is an open question (see previous section).
Even though progress has been made in this area, we still ignore whether measures of arterial stiffness such as PWV are useful in clinical practice to monitor therapies that broadly interfere with the cardiovascular system and arterial function, such as drugs antagonizing the effects of the renin–angiotensin–aldosterone system or calcium-channel blockers or drugs impinging upon alterations in mineral metabolism. Vascular calcifications are a prominent feature of arterial disease in CKD and ESRD;15, 16 however, it should be emphasized that it is largely undefined whether calcifications represent a valid surrogate end point that can be applied in intervention studies in these patients. In other words, we ignore to check whether interventions that reduce vascular calcifications unequivocally translate into better clinical outcomes, and this is true both for interventions based on drugs impinging upon dyslipidemia and for interventions aimed at correcting alterations in mineral metabolism in CKD (phosphate binders, vitamin D, calcimimetics, vitamin K). Finally, arterial changes are tightly associated with cardiac morphological (LVH) and functional changes (LV dysfunction)17, 18, 19 in cross-sectional studies; however, the longitudinal relationship between arterial and cardiac changes is not well documented in CKD/ESRD and the role of arterial stiffening on heart disease in these patients remains to be defined, in parallel with the evaluation of senescence rates in these CKD/ESRD populations.20
AC has received consulting fees from Abbott Laboratories and received lecture fees from F. Hoffmann-La Roche, Amgen, and Fresenius Medical Care Holdings. AM-C has received consulting fees from Abbott Laboratories, Roche Spain, and Abbott Spain. AO has received grant support from the Spanish Government. AW has received lecture fees from Amgen, F. Hoffmann-La Roche, and Janssen-Cileg. AW has also received grant support from Astellas Pharma. DF has received funding from the EU. DG has received consulting fees and lecture fees from Shire, Genzyme, Novartis AG, Sandoz, Pfizer, and Fresenius Medical Care Holdings. FWD has received funding from Amgen and Baxter. GL has received consulting fees from Amgen and Sandoz. GL has also received lecture fees from Amgen, Sandoz, Genzyme, and Shire. PJB has received consulting fees from Medtronic and has received grant support from Ardian and Novartis AG. RA has received consulting fees from Amgen, Abbott Laboratories, Merck, Affymax, Takeda Pharmaceutical Company, Daiichi Sankyo, Celgene, Watson Pharmaceuticals, and Rockwell Medical. RA has also received lecture fees from Abbott Laboratories, Merck, and Medscape. ZM has received lecture fees from Amgen, Shire, Genzyme, FMC, and Merck Sharp & Dohme. ZM has received grant support from Baxter, Amgen, FMC, Shire, and Genzyme. The remaining authors declared no competing interests.
Footnotes
TO CITE THIS ARTICLE: London G, Covic A, Goldsmith D et al. Arterial aging and arterial disease: interplay between central hemodynamics, cardiac work, and organ flow—implications for CKD and cardiovascular disease. Kidney Int Sup 2011; 1: 10–12.
References
- Braun J, Oldendorf M, Moshage W, et al. Electron-beam computed tomography in the evaluation of cardiac calcifications in chronic dialysis patients. Am J Kidney Dis. 1996;27:394–401. doi: 10.1016/s0272-6386(96)90363-7. [DOI] [PubMed] [Google Scholar]
- Najjar SS, Scuteri A, Lakatta EG. Arterial aging: is it an immunable cardiovascular risk factor. Hypertension. 2005;46:454–462. doi: 10.1161/01.HYP.0000177474.06749.98. [DOI] [PubMed] [Google Scholar]
- Avolio AO, Chen SG, Wang RP, et al. Effects of aging on changing arterial compliance and left ventricular load in a Northern Chinese urban community. Circulation. 1983;68:50–58. doi: 10.1161/01.cir.68.1.50. [DOI] [PubMed] [Google Scholar]
- Mitchell GF, Parise H, Benjamin EJ, et al. Changes in arterial stiffness and wave reflections with advancing age in healthy men and women: the Framingham Heart Study. Hypertension. 2004;43:1239–1245. doi: 10.1161/01.HYP.0000128420.01881.aa. [DOI] [PubMed] [Google Scholar]
- Nichols WW, O'Rourke MF.Vascular impedance McDonald's Blood Flow in Arteries: Theoretical Experimental and Clinical Principles5th edn.Hodder Arnold: London; 2005. pp 137–148, 216–231, 233–267. [Google Scholar]
- O'Rourke MF.Principles and definitions of arterial stiffness, wave reflections and pulse pressure amplificationIn: Safar ME, O'Rourke MF (eds).Handbook of Hypertension (series eds. Birkenhäger WH, Reid JL), vol 23. Arterial Stiffness in Hypertension Elsevier: Amsterdam; 20063–20. [Google Scholar]
- London GM, Yaginuma T.Wave reflections: clinical and therapeutic aspectsIn: Safar ME, O'Rourke MF (eds).The Arterial System in Hypertension Kluwer Academic Publishers: Dordrecht; 1993221–237. [Google Scholar]
- Mitchell GF. Effects of central arterial aging on the structure and function of the peripheral vasculature: implications for end-organ damage. J Appl Physiol. 2008;105:1652–1660. doi: 10.1152/japplphysiol.90549.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bortolotto LA, Safar ME, Billaud E, et al. Plasma homocysteine, aortic stiffness, and renal function in hypertensive patients. Hypertension. 1999;34:837–842. doi: 10.1161/01.hyp.34.4.837. [DOI] [PubMed] [Google Scholar]
- Hanon O, Haulon S, Lenoir H, et al. Relationship between arterial stiffness and cognitive function in elderly subjects with complaints of memory loss. Stroke. 2005;36:2193–2197. doi: 10.1161/01.STR.0000181771.82518.1c. [DOI] [PubMed] [Google Scholar]
- Pannier B, Guérin AP, Marchais SJ, et al. Stiffness of capacitive and conduit arteries: prognostic significance for end-stage renal disease patients. Hypertension. 2005;45:592–596. doi: 10.1161/01.HYP.0000159190.71253.c3. [DOI] [PubMed] [Google Scholar]
- Blacher J, Guérin AP, Pannier B, et al. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999;99:2434–2439. doi: 10.1161/01.cir.99.18.2434. [DOI] [PubMed] [Google Scholar]
- Ibels LS, Alfrey AL, Huffer WE, et al. Arterial calcification and pathology in uremic patients undergoing dialysis. Am J Med. 1979;66:790–796. doi: 10.1016/0002-9343(79)91118-5. [DOI] [PubMed] [Google Scholar]
- Laurent S, Boutouyrie P.Determination of systemic and regional arterial stiffnessIn: Safar ME, O'Rourke MF (eds).Handbook of Hypertension (series eds. Birkenhäger WH, Reid JL), vol 23. Arterial Stiffness in Hypertension Elsevier: Amsterdam; 200653–62. [Google Scholar]
- Schoppet M, Shroff RC, Hofbauren LC, et al. Exploring the biology of vascular calcification in chronic kidney disease: what's circulating. Kidney Int. 2008;73:384–390. doi: 10.1038/sj.ki.5002696. [DOI] [PubMed] [Google Scholar]
- Demer LL, Tintut Y. Vascular calcification: pathobiology of multifaceted disease. Circulation. 2008;117:2938–2948. doi: 10.1161/CIRCULATIONAHA.107.743161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avolio AO, Chen SG, Wang RP, et al. Effects of aging on changing arterial compliance and left ventricular load in a Northern Chinese urban community. Circulation. 1983;68:50–58. doi: 10.1161/01.cir.68.1.50. [DOI] [PubMed] [Google Scholar]
- Buckberg GD, Towers B, Paglia DE, et al. Subendocardial ischemia after cardiopulmonary bypass. J Thoracic Cardiovasc Surg. 1972;64:669–687. [PubMed] [Google Scholar]
- London GM, Guérin AP, Marchais SJ, et al. Cardiac and arterial interactions in end-stage renal disease. Kidney Int. 1996;50:600–608. doi: 10.1038/ki.1996.355. [DOI] [PubMed] [Google Scholar]
- Koopman JJE, Rozing MP, Kramer A, et al. Senescence rates in patients with end-stage renal disease: a critical appraisal of the Gompetz model. Aging Cell. 2011;10:233–238. doi: 10.1111/j.1474-9726.2010.00659.x. [DOI] [PubMed] [Google Scholar]