Abstract
Over the past decade, the research agenda in dialysis has been dominated by studies on risk factors associated with cardiovascular mortality. It has now become increasingly clear that in dialysis patients, non-cardiovascular causes of death are increased to the same extent as cardiovascular mortality, and therefore research efforts in this area deserve an equally prominent place on the nephrology research agenda. As previous research has suggested an association between cardiovascular disease and infections, more research on potential links between the causal pathways of cardiovascular events and infections is also warranted.
Keywords: cardiovascular disease, cardiovascular mortality, dialysis, mortality, non-cardiovascular mortality, renal replacement therapy
More than a decade ago, Foley et al.1 had studied a USRDS data set including patients with end-stage renal disease (ESRD), and after stratification for age, race, and sex they found mortality from cardiovascular disease to be 10–20 times higher in ESRD patients compared with the general population. This study has been cited more than 800 times, frequently to justify studies pertaining to the effect of cardiovascular risk factors on mortality in chronic kidney disease (CKD) patients. Even more common, this reference has been used to underline the fact that cardiovascular disease, which is responsible for around half of the deaths in dialysis patients, is the most important cause of death in this population. Finally, the findings of the study by Foley et al. have not only been used to justify specific studies, but they have also to a large extent set the research agenda for CKD since their publication in 1998.
Although it has been established beyond any doubt that cardiovascular events are an important cause of death in CKD patients, this is only half the truth. Cardiovascular mortality is also important in the general population. Depending on the age category, it is responsible for 10–50% of mortality in the general population, whereas in dialysis patients these percentages are 20–40.2 Therefore, the fraction of cardiovascular deaths is quite similar in both populations. From this perspective, the findings of Foley et al. can only be understood if in dialysis patients mortality due to non-cardiovascular disease is increased to the same extent as mortality from cardiovascular causes. Indeed, results from other studies conducted on the same USRDS data set have shown that, in dialysis patients, mortality from sepsis is 50 times higher3 and that from pulmonary infections is 14–16 times higher4 compared with the general population. However, these findings have received very little attention compared with those showing increased cardiovascular mortality. More recently, de Jager et al.2 analyzed data from the European Renal Association–European Dialysis and Transplant Association (ERA–EDTA) Registry and not only confirmed the findings of Foley and colleagues but also showed that in dialysis patients mortality from non-cardiovascular disease was increased to the same extent as mortality from cardiovascular disease. Taking the general population in Europe as a reference, the age-adjusted cardiovascular mortality in dialysis patients was 8.8 times higher, whereas the non-cardiovascular mortality was increased 8.1 times.2 To add to this perspective, it is interesting to note that the increased risk of both cardiovascular and non-cardiovascular mortality in dialysis patients is complemented by the observation that, in elderly individuals with a more advanced stage of CKD, the age- and sex-adjusted risk of death from non-cardiovascular causes is increased compared with those with better renal function.5 Apparently, individuals with CKD die prematurely from all kinds of causes compared with individuals of the same age in the general population. We recently presented clinical and experimental data showing that the cardiovascular events associated with atherosclerosis are more often fatal in patients with CKD than in individuals without CKD.6
The studies on ERA–EDTA Registry and USRDS data in dialysis patients2, 3, 4 are particularly worrisome, as their results do not seem to fit well with the commonly held opinion that, in order to reduce the highly increased mortality in these patients, we should predominantly study and decrease traditional and non-traditional cardiovascular risk factors. On the other hand, from these studies it cannot be concluded that investigating and treating cardiovascular risk factors in CKD patients would not be helpful. We would simply like to argue that reduction of cardiovascular and non-cardiovascular mortality deserves equal attention.
Our understanding is further hampered by the publication in the past few years of a number of ‘negative trials', randomized controlled trials (RCTs) that failed to show a beneficial effect of interventions aimed at decreasing cardiovascular risk factors, although such interventions have established positive effects on mortality in the general population. For instance, cardiovascular end points including cardiovascular mortality were not reduced in CKD or dialysis patients in published RCTs in which they attempted to correct, for example, hypercholesterolemia7, 8 or anemia.9, 10
Given these findings from epidemiological and intervention studies, three questions arise:
Why are both cardiovascular and non-cardiovascular mortality rates increased to the same extent?
What are the effects of cardiovascular disease on non-cardiovascular events and vice versa? and
Why does treatment of established cardiovascular risk factors not seem to decrease cardiovascular mortality in dialysis patients?
In relation to the first question, it is common knowledge that non-cardiovascular causes of death, such as malignancy, share a number of risk factors with cardiovascular mortality—for example, smoking, obesity, physical inactivity, and diet. The prevalence of some of those factors is increased in CKD patients, as they are also risk factors for CKD itself. On the contrary, cancer itself, as well as the adverse effects of therapies for cancer, can directly or indirectly cause CKD.11 Also related to the first question, both cardiovascular and infectious causes of death are linked to inflammation and it has become increasingly appreciated that ESRD is characterized by a state of chronic inflammation.12 There is a wealth of evidence indicating that disorders of both innate and adaptive immune systems contribute to an increased rate of infections in the course of ESRD.13 Although defensive responses are impaired, the immune system is also under constant stimulation because of the process of dialysis itself.14
With regard to the second question, it has been shown that infections and cardiovascular events are interrelated. In individuals under the care of a general practitioner, the risk of myocardial infarction and that of stroke were substantially higher after a diagnosis of systemic respiratory tract infection, especially during the first 3 days of infection.15 This supports the concept that acute infections are associated with a transient increase in the risk of vascular events.15 Furthermore, Ishani et al.16 showed that in dialysis patients septicemia or bacteremia was associated with subsequent death, myocardial infarction, heart failure, peripheral vascular disease, and stroke. They concluded that septicemia appears to be an important, potentially preventable, cardiovascular risk factor in this patient group. Conversely, particular cardiovascular diseases such as heart failure and volume overload may elicit conditions favorable for the development of infections. In this context, it is interesting that in ESRD patients volume overload is one of the putative causes of elevated circulating TNF-α levels.14 Thus, infections are associated with subsequent cardiovascular events, and particular cardiovascular disorders may elicit infections. It is possible that these problems may aggravate each other. Therefore, other potential causal pathways in the link between non-cardiovascular and cardiovascular diseases and their potential common causes (including the role of the immune system) also need to be studied further. Hypotheses in this area need to be tested in animal models and laboratory experiments.
An answer is also much needed for the third question. RCTs in CKD to date have studied interventions that in the general population have been shown primarily to reduce death from myocardial infarction or stroke. However, in dialysis patients, an important part of the cardiovascular deaths can be attributed to other “competing” causes of death,17 such as sudden death, which may not be modifiable by interventions aimed to reduce hypercholesterolemia or anemia. In addition, dialysis patients comprise a highly selected population.17 It is therefore possible that in these RCTs interventions were tested that are relatively ineffective in the reduction of total mortality in this particular patient population. Studies on (addressing) risk factors for sudden death are warranted.
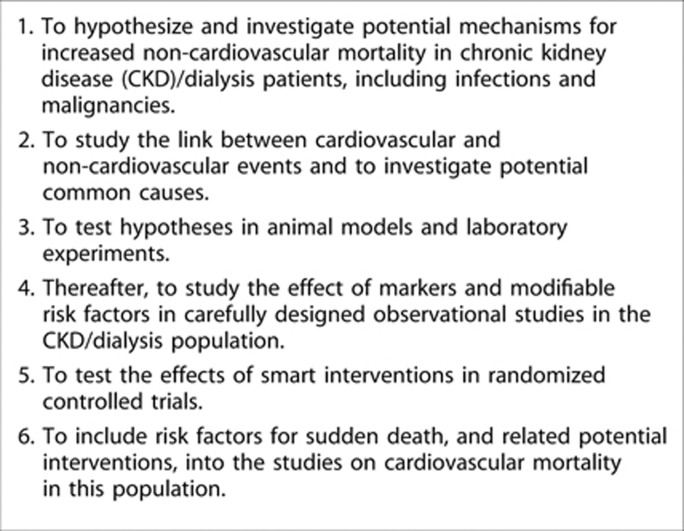
In conclusion, the research agenda for the reduction of mortality in dialysis patients (Figure 1) should focus on both cardiovascular and non-cardiovascular causes of death. In addition, research in cardiovascular mortality may better differentiate between the effects of interventions aimed to reduce specific types of cardiovascular mortality. Finally, the potential link between cardiovascular and non-cardiovascular mortality deserves further investigation.
Figure 1.
Proposal for a new research agenda on the cardiovascular–renal and non-cardiovascular–renal links.
AC has received consulting fees from Abbott Laboratories and received lecture fees from F. Hoffmann-La Roche, Amgen, and Fresenius Medical Care Holdings. AM-C has received consulting fees from Abbott Laboratories, Roche Spain, and Abbott Spain. AO has received grant support from the Spanish Government. AW has received lecture fees from Amgen, F. Hoffmann-La Roche, and Janssen-Cileg. AW has also received grant support from Astellas Pharma. DF has received funding from the EU. DG has received consulting fees and lecture fees from Shire, Genzyme, Novartis AG, Sandoz, Pfizer, and Fresenius Medical Care Holdings. FWD has received funding from Amgen and Baxter. GL has received consulting fees from Amgen and Sandoz. GL has also received lecture fees from Amgen, Sandoz, Genzyme, and Shire. PJB has received consulting fees from Medtronic and has received grant support from Ardian and Novartis AG. RA has received consulting fees from Amgen, Abbott Laboratories, Merck, Affymax, Takeda Pharmaceutical Company, Daiichi Sankyo, Celgene, Watson Pharmaceuticals, and Rockwell Medical. RA has also received lecture fees from Abbott Laboratories, Merck, and Medscape. ZM has received lecture fees from Amgen, Shire, Genzyme, FMC, and Merck Sharp & Dohme. ZM has received grant support from Baxter, Amgen, FMC, Shire, and Genzyme. The remaining authors declared no competing interests.
Footnotes
TO CITE THIS ARTICLE: Jager KJ, Lindholm B, Goldsmith D et al. Cardiovascular and non-cardiovascular mortality in dialysis patients: where is the link? Kidney Int Sup 2011; 1: 21–23.
References
- Foley RN, Parfrey PS, Sarnak MJ. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis. 1998;32 (Suppl 3:S112–S119. doi: 10.1053/ajkd.1998.v32.pm9820470. [DOI] [PubMed] [Google Scholar]
- de Jager DJ, Grootendorst DC, Jager KJ, et al. Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA. 2009;302:1782–1789. doi: 10.1001/jama.2009.1488. [DOI] [PubMed] [Google Scholar]
- Sarnak MJ, Jaber BL. Mortality caused by sepsis in patients with end-stage renal disease compared with the general population. Kidney Int. 2000;58:1758–1764. doi: 10.1111/j.1523-1755.2000.00337.x. [DOI] [PubMed] [Google Scholar]
- Sarnak MJ, Jaber BL. Pulmonary infectious mortality among patients with end-stage renal disease. Chest. 2001;120:1883–1887. doi: 10.1378/chest.120.6.1883. [DOI] [PubMed] [Google Scholar]
- Fried LF, Katz R, Sarnak MJ, et al. Kidney function as a predictor of noncardiovascular mortality. J Am Soc Nephrol. 2005;16:3728–3735. doi: 10.1681/ASN.2005040384. [DOI] [PubMed] [Google Scholar]
- Drüeke TB, Massy ZA. Atherosclerosis in CKD: differences from the general population. Nat Rev Nephrol. 2010;6:723–735. doi: 10.1038/nrneph.2010.143. [DOI] [PubMed] [Google Scholar]
- Wanner C, Krane V, März W, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;353:238–248. doi: 10.1056/NEJMoa043545. [DOI] [PubMed] [Google Scholar]
- Fellström BC, Jardine AG, Schmieder RE, et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med. 2009;360:1395–1407. doi: 10.1056/NEJMoa0810177. [DOI] [PubMed] [Google Scholar]
- Drüeke TB, Locatelli F, Clyne N, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071–2084. doi: 10.1056/NEJMoa062276. [DOI] [PubMed] [Google Scholar]
- Singh AK, Szczech L, Tang KL, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355:2085–2098. doi: 10.1056/NEJMoa065485. [DOI] [PubMed] [Google Scholar]
- Stengel B. Chronic kidney disease and cancer: a troubling connection. J Nephrol. 2010;23:253–262. [PMC free article] [PubMed] [Google Scholar]
- Kaysen GA. The microinflammatory state in uremia: causes and potential consequences. J Am Soc Nephrol. 2001;12:1549–1557. doi: 10.1681/ASN.V1271549. [DOI] [PubMed] [Google Scholar]
- Kato S, Chmielewski M, Honda H, et al. Aspects of immune dysfunction in end-stage renal disease. Clin J Am Soc Nephrol. 2008;3:1526–1533. doi: 10.2215/CJN.00950208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenvinkel P, Ketteler M, Johnson RJ, et al. IL-10, IL-6, and TNF-a: central factors in the altered cytokine network of uremia—the good, the bad, and the ugly. Kidney Int. 2005;67:1216–1233. doi: 10.1111/j.1523-1755.2005.00200.x. [DOI] [PubMed] [Google Scholar]
- Smeeth L, Thomas SL, Hall AJ, et al. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351:2611–2618. doi: 10.1056/NEJMoa041747. [DOI] [PubMed] [Google Scholar]
- Ishani A, Collins AJ, Herzog CA, et al. Septicemia, access and cardiovascular disease in dialysis patients: the USRDS wave 2 study. Kidney Int. 2005;68:311–318. doi: 10.1111/j.1523-1755.2005.00414.x. [DOI] [PubMed] [Google Scholar]
- Jager KJ, Stel VS, Zoccali C, et al. The issue of studying the effect of interventions in renal replacement therapy—to what extent may we be deceived by selection and competing risk. Nephrol Dial Transplant. 2010;25:3836–3839. doi: 10.1093/ndt/gfq540. [DOI] [PubMed] [Google Scholar]