Abstract
Patient: Female, 30
Final Diagnosis: Phytobezoar
Symptoms: Nausea • vomiting
Medication: —
Clinical Procedure: —
Specialty: —
Objective:
Rare disease
Background:
Phytobezoars are a common type of bezoar known to accumulate in the gastrointestinal system.
Case Report:
A 30-year-old mentally retarded woman was operated on due to small bowel obstruction. A piece of tree root was extracted from the ileum. The patient was discharged from the hospital on postoperative day 7.
Conclusions:
Due to difficulties in determining the nature of the bezoar preoperatively, small bowel obstruction due to a phytobezoar is not a common diagnosis. For bezoars, prevention is considered preferable to treatment.
MeSH Keywords: Bezoars, General Surgery, Ileus, Mentally Disabled Persons
Background
Various types of bezoars (accumulation of foreign bodies) have been shown to accumulate in the gastrointestinal system. Phytobezoars, formed of non-digestible food such as cellulose, lignin, and fruit tannins, are among the most common. An adhesive coagulum is created upon contact with gastric acids, due to polymerization of monomeric fruit tannins (especially those occurring in persimmons and citrus fruits) [1]. Trichobezoars are classically defined as consisting mostly of hair, and occur frequently in mentally retarded adults and children with trichotillomania (a compulsion to pull out one’s own hair) [1]. Rapunzel’s syndrome, due to compulsive hair-chewing, results in the generation of a long-tailed trichobezoar, which is a type of trichobezoar [1]. Lactobezoars are frequently formed in growth-retarded neonates fed baby formula. Milk components such as casein become hardened due to low neonatal gastrointestinal system motility, intensive formula diets, and dehydration. Therapies such as nifedipine, cholestyramine, Kayexalate, antacids, nuts, paste, cement, and shellac may hasten bezoar formation. All types of bezoars are usually combined with decreased gastrointestinal motility or before gastric surgery [1].
Ileal obstruction by a phytobezoar has not been commonly reported in the literature [2]. Small bowel phytobezoars are almost always obstructive, causing mechanical obstruction of the bowel [3]. Here, we report a case of phytobezoar caused by a piece of tree root in a patient with mental retardation.
Case Report
A 30-year-old mentally retarded woman was admitted to the hospital with nausea and vomiting complaints for 1 week. Her mental retardation was due to neuropsychological sequelae of meningitis. The patient could not tolerate oral intake. There was no defecation problem but frequency of defecation was decreased. There was tenderness at the upper quadrants and bowel sounds were decreased on physical examination. Complete blood count and biochemical analysis results were normal. Direct abdominal imaging performed with the patient in standing position showed intestinal type air-fluid levels. Computerized tomography showed obstruction of the small intestine (Figure 1). Gastroscopy result was normal and pyloric orifice size was 19 mm at the largest diameter, which is within normal range. The patient could not tolerate nasogastric decompression due to mental retardation. Laparotomy led to diagnosis of ileal phytobezoar. The small intestine (2 m) was dilated from the Treitz ligament, and distal to this dilation there was partial obstruction of the ileum (Figure 2). After enterotomy of the ileal wall, a piece of tree root (10 cm length, 3 cm diameter) was extracted (Figures 3 and 4). After 1 day in the intensive care unit, the patient was transferred to the surgery department and discharged from the hospital on postoperative day 7. There was no problem with oral in-take at follow-up.
Figure 1.
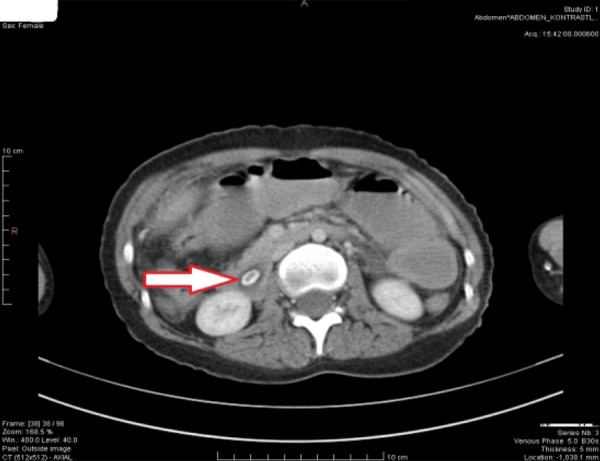
CT scan of the abdomen.
Figure 2.

Intraoperative view of obstruction.
Figure 3.

Tree root bezoar.
Figure 4.

Tree root bezoar.
Discussion
Small bowel obstruction (SBO) is a common diagnosis for hospital admissions and can result from adhesions, strangulated hernia, malignancy, volvulus, and inflammatory bowel disease, etc. Phytobezoars are rare and account for only 4% of all intestinal obstructions. No pattern of age or sex has been found. Small bowel bezoars generally exist as intestinal obstructions, compressed on the constricted side of the small bowel, with the larger portion being the terminal ileum near the jejunum [4]. Interestingly, in the case described here, it is difficult to explain how such a large piece of tree root could have passed the narrow pyloric orifice. It might have been passed through the pyloric orifice, due to high-pressure gastric contractions and isoperistaltic movements.
In such cases, abdominal pain (49–100%), epigastric discomfort (80%), vomiting and nausea (35–78%), and SBO (94.73%) are the major clinical symptoms. Feelings of fullness, dysphagia, anorexia with weight loss, and incipient gastrointestinal hemorrhage might be seen. Decreased peristaltic sounds, rebound and tenderness, distention, diarrhea, constipation, vomiting, and abdominal pain are seen [5]. In our patient, exactly these types of symptoms existed before surgery. Preoperative identification of bezoar-caused SBO is difficult and the majority of diagnoses are made only after gastric surgery or laparotomy, without which the early diagnosis is frequently adhesive obstruction. In the absence of a clear diagnosis, the surgeon will likely begin a series of medical treatments with the hope of spontaneous resolution of the SBO. This is important because any delay between admission and adequate treatment increases the risk of morbidity. For our patient, in the absence of prior surgical history, hardened stool, tumor, and phytobezoar were all considered as possible causes of the obstruction. Although direct abdominal radiography is useful for the diagnosis of SBO, it is unable to identify bezoars. Ultrasonography (USG) is subjective and scanning of the obstruction may be blocked by overlying gas in the intestine. In a retrospective study, ultrasound was able to diagnose phytobezoars in 88% of patients with intestinal obstruction [6]. CT imaging is fast and is often the first-line examination for the evaluation of SBO (to exclude varius causes of acute abdominal pain). In our case, the obstruction was detected using a combination of direct observation, USG, and CT scan. However, the exact cause of the obstruction was only detected during the operation.
Patients with SBO can be admitted to the hospital with hypovolemia and electrolyte imbalance due to vomiting and/or sequestration of the fluid in the third space. Therefore, intestinal decompression with intravenous fluid and electrolyte resuscitation should be the first-line treatment if strangulation occurs. Akcakaya et al. noted that metabolic deterioration can develop as a result of obstruction, and that any delay in therapy may significantly increase the risk of morbidity and mortality [7]. In our case, patient was resuscitated 96 h before the operation. Most intestinal bezoars must be treated by surgery. Bezoar fragmentation followed by milking to the cecum is helpful, but enterotomy is required if this is not successful. Resection is seldom done and should be reserved for intestinal necrosis or if the bezoar is intimately attached to the bowel wall [8]. The rest of the gastrointestinal system must also be checked for residual bezoars during surgery; this is an essential precaution, given that the incidence of concurrent gastric bezoars has been calculated as 17–21% [9,10] and the rate of recurrence as 13.8% [11]. Laparoscopic intervention is an alternative bezoar treatment that avoids scarring of the epidermis. In addition, laparoscopic intervention matched conventional laparotomy for good cosmesis, brief hospitalization, fast return to normal daily activity, less postoperative pain, and a reduced rate of adhesion. Indications for the suitability of the laparoscopic procedure include bezoar size, seriousness of adhesion, intestinal obstruction, and the scope of the net surgical field [12]. Due to the risk of perforation as a result of intestinal distension, laparoscopic manipulation was not considered for our patient. Protective measures against bezoar formation include low-fiber diet, medication inducing intestinal motility, and psychological support. At 1-year follow-up, we found no recurrence of bezoar in our patient.
Conclusions
In conclusion, bowel obstruction due to a phytobezoar is a rare diagnosis, probably due to difficulties with preoperative diagnosis.
References:
- 1.Andrus CH, Ponsky JL. Bezoars: classification, pathophysiology and treatment. Am J Gasetoenterol. 1988;83:476–78. [PubMed] [Google Scholar]
- 2.Numanoğlu KV, Tatli D. A rare cause of partial intestinal obstruction in a child: colonic lithobezoar. Emerg Med J. 2008;25:312–13. doi: 10.1136/emj.2007.056812. [DOI] [PubMed] [Google Scholar]
- 3.Toledo AP, Rodrigues FH, Rodrigues MR, et al. Diospyrobezoar as a cause of small bowel obstruction. Case Rep Gastroenterol. 2012;6:596–603. doi: 10.1159/000343161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ezzat R, Rashid S, Rashid A, et al. Small intestinal obstruction due to phytobezoar: a case report. J Med Case Rep. 2009;3:9312. doi: 10.1186/1752-1947-3-9312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goor H, Rooyen W. Bezoars: a special cause of ileal obstruction in mentally retarded patients. Neth J Surg. 1991;43:43–44. [PubMed] [Google Scholar]
- 6.Ripollés T, García-Aguayo J, Martínez MJ, Gil P. Gastrointestinal bezoars: sonographic and CT characteristics. Am J Roentgenol. 2001;177:65–69. doi: 10.2214/ajr.177.1.1770065. [DOI] [PubMed] [Google Scholar]
- 7.Akcakaya A, Sahin M, Coskun A, Demiray S. Comparison of mechanical bowel obstruction cases of intra-abdominal tumor and non-tumoral origin. World J Surg. 2006;30:1295–99. doi: 10.1007/s00268-005-0440-z. [DOI] [PubMed] [Google Scholar]
- 8.Menezes Ettinger JE, Silva Reis JM, de Souza EL, et al. Laparoscopic management of intestinal obstruction due to phytobezoar. JSLS. 2007;11:168–71. [PMC free article] [PubMed] [Google Scholar]
- 9.Lo CY, Lau PW. Small bowel phytobezoars: an uncommon cause of small bowel obstruction. Aust NZJ Surg. 1994;64:187–89. doi: 10.1111/j.1445-2197.1994.tb02175.x. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein SS, Lewis JH, Rothstein R. Intestinal obstruction due to bezoars. Am J Gastroenterol. 1984;79:313–18. [PubMed] [Google Scholar]
- 11.Escamilla C, Robles-Campos R, Parrilla-Paricio P, et al. Intestinal obstruction and bezoars. J Am Coll Surg. 1994;179:285–88. [PubMed] [Google Scholar]
- 12.Parsi S, Rivera C, Vargas J, Silberstein MW. Laparoscopic-assisted extirpation of a phytobezoar causing small bowel obstruction after Roux-en-Y laparoscopic gastric bypass. Am Surg. 2013;79:E93–95. [PubMed] [Google Scholar]


