Abstract
This study examined the relation between misperception of healthy weight and obesity, as well as moderators of this relation, in a sample of middle-aged black men. Survey data from 404 mostly immigrant, black males living in greater New York City were collected as part of a larger randomized controlled trial. Data included measures of health status, BMI, perceived healthy weight, and misperception of healthy weight. Misperception of healthy weight was more frequent among obese men (90.2%) than nonobese men (48.7%) (P < 0.001). Mean level of misperception was also significantly higher in obese men than nonobese men (P < 0.001). Health status moderated the relation between misperception of healthy weight and obesity: obese men who felt healthy or who had fewer comorbid conditions had greater misperception of healthy weight than obese men who felt unhealthy or had relatively more comorbid conditions (P < 0.01). Our findings demonstrate that misperception of healthy weight discriminates between obese and nonobese black men, and the magnitude of this relation is exacerbated in obese men who are relatively healthy. Future studies should determine the prevalence of misperception of healthy weight in more diverse populations and identify potential mediators of the relation between misperception of healthy weight and obesity.
Introduction
The US Centers for Disease Control and Prevention estimated that as of 2005–2006 more than one-third of the adult population was obese (BMI >30), including a third of the adult male population (1). Currently, there does not appear to be a significant difference in the prevalence of obesity across racial groups within the adult male population (1). However, the health burden due to obesity-related diseases is disproportionately high among black men. Specifically, type II diabetes, hypertension, cardiovascular disease, and some cancers are more prevalent in black men than white men (2). Interventions aimed at reducing this excess burden of chronic disease among black men must address factors that hinder weight loss in this population. The key to developing effective obesity interventions may be to identify modifiable psychological and behavioral factors that influence obesity.
Misperception of weight is one psychological factor implicated in the development of obesity (3,4). One approach to measuring misperception of weight is to examine the concordance between self-reported weight status (i.e., “Are you underweight, normal weight, overweight, or obese?”) and healthy weight according to BMI guidelines (5,6). Overweight and obese individuals have lower concordance, or greater misperception, between their self-report and BMI-based weight status than normal weight individuals (3–5,7). Another approach to measuring misperception of weight is to examine the concordance between self-report of a target healthy weight (i.e., “What is a healthy weight for you?”) and healthy weight according to BMI guidelines (8,9). This latter approach reveals both whether individuals perceive that they are not at a healthy weight and the degree of (in)accuracy of their perception. The advantage of this approach is that it uses a continuous measure to produce an effect size on the degree of discordance between perceived healthy weight and healthy weight as defined by the National Institutes of Health (10). Effect sizes are useful for comparing risks across populations and comparing the effectiveness of different interventions.
Some studies have shown racial differences in misperception of weight. For example, overweight and obese black men are more likely to misperceive their weight status than men of other races (3–7). The current study further explores the nature of the association between misperception of weight and obesity in black men by examining the role of a novel moderator, health status, in misperception of healthy weight. Research suggests that some black men perceive that they can be overweight yet healthy (11). This implies that obese men who are unburdened by major health problems may be more likely to misperceive the extent of their weight problem than their less healthy counterparts.
Based on prior research, we hypothesized that misperception of healthy weight would be greater among obese men than nonobese men. This information is useful for identifying a potentially modifiable risk factor for obesity among black men. We also hypothesized that health status would moderate the relation between obesity and misperception of healthy weight such that men who feel healthy or have fewer comorbid conditions will have greater misperception of healthy weight than their counterparts who feel unhealthy or have relatively more comorbid conditions. The moderator analysis identifies those men who are obese and most likely to underestimate their weight problems, as this information can be used to target interventions.
Methods and Procedures
Design
This study used survey data collected as part of a larger randomized controlled trial, the Cancer Awareness and Prevention trial (12,13). Trial participants were randomized to one of two health-education intervention conditions: decision-making about prostate cancer testing or awareness of national recommendations for fruit and vegetable consumption. Surveys were administered before the intervention and 8 months later. All of the major variables in the present study were collected at baseline, with the exception of height (due to concern about measurement burden, some items in the parent study that were not expected to change were only assessed at follow-up). There was no relation between intervention condition and any of the study variables in the present analysis. Participants received $10 gifts after each survey. The study was approved by Institutional Review Boards and informed consent was obtained.
Participants and setting
Participants were recruited by telephone screening of beneficiaries of a large health benefit fund in greater New York City. Inclusion criteria included being a black male between the ages of 45 and 70 years. A unique strength of this study is that the sample population had many black men from the Caribbean. Caribbean immigrants represent nearly one-third of New York City's black population (14), but little is known about obesity and weight misperception in this population. Exclusion criteria included a prior prostate cancer diagnosis, a recent prostate cancer test, and stated intention to be unavailable for follow-ups. Of 1,777 individuals screened for eligibility, 490 were eligible and completed the baseline survey, 1,153 were ineligible, and 134 refused. The sample used in this secondary analysis consisted of the 404 participants who had complete self-reported data and were not underweight (six participants' BMI <18.5).
Measures
Trained interviewers, blind to experimental condition, used a structured telephone interview to collect data. Supervisors performed quality ratings on two-thirds of all audio-recorded interviews. Eighty-four percent of the checked interviews scored 90% or better. During the formative evaluation phase of this research, survey materials were subject to various techniques to reduce response error and assess suitability of items for participants with low literacy (see Wolf et al.) (12).
Social and demographic variables
Age, marital status, immigrant status, and education were measured through self-report. Median neighborhood household income was calculated using data from the US Census 2000.
Health status
Health status was measured by assessing participants' perception of their overall health, as well as their number of comorbid conditions. Perception of overall health was measured by asking participants, “All in all, would you say your overall health is excellent (4), good (3), fair (2), or poor (1)?” (15). Poorer perception of health on this measure has been shown to be associated with greater risk of atherosclerosis, poorer lung functioning, and lower exercise capacity (16). This measure also has been shown to be inversely related to mortality in diverse populations (17). Number of comorbid conditions was measured using the Self-Administered Comorbidity Questionnaire, which has been cross-validated with comorbidity measures based on standardized medical record reviews (18).
BMI
BMI was calculated by dividing participants' self-reported weight (pounds) without shoes, by the square of their self-reported height (inches) without shoes, and then multiplying by 703 (10). In the present study, self-reported weight was measured at two waves and the correlation between the measures was strong (r = 0.95, P < 0.001), indicating exceptional test–retest reliability over an 8-month period.
Perceived healthy weight
Perceived healthy weight was measured by asking, “What do you think is a healthy weight for you?” Participants responded with a weight in pounds.
Misperception of healthy weight
Misperception of healthy weight was measured by first determining the accuracy of participants' perceived healthy weight. Because a range of weights is considered healthy for a given height, we used a standard BMI of 24.9 (the upper threshold of the normal weight category) and a standard BMI of 18.5 (the lower threshold of the normal weight category) to calculate the corresponding weight range appropriate to each participant's height. Participants who reported a perceived healthy weight within the range of healthy weights were classified as having an accurate perception of healthy weight and were assigned a misperception score of zero. However, participants who reported a perceived healthy weight that exceeded the greatest weight allowed in the range of healthy weights misperceived their healthy weight. The magnitude of this misperception was then calculated by taking the difference between participants' perceived healthy weight and the greatest weight allowed in the range of healthy weights. Take for example a participant who is 72 inches tall, weighs 216 pounds, and perceives that his healthy weight should be 210 pounds. According to the BMI standards, in order for the participant to be at a healthy weight for his height, he should weigh <183.62 pounds. Thus, this participant misperceives his healthy weight by 26.38 pounds (210–183.62).
Statistical analysis
All statistical analyses were conducted using SPSS version 16 (19) and two-tailed P values. Descriptive statistics (proportions, means and s.d.) were used to characterize the social and demographic variables. We then evaluated whether there was a need to covary any of the social or demographic variables in the analyses. Next, we analyzed the relation between obesity status and misperception of healthy weight by using χ2 analysis and determined whether the difference in the mean magnitude of misperception of healthy weight was statistically significant by using a t-test. Lastly, we used ANOVA techniques to examine whether health status moderated the association between misperception of healthy weight and obesity.
Results
Table 1 shows the participants' characteristics. All men were black, and most were middle-aged, immigrant (68.5% Caribbean origin), married, and had at least a high-school level of education. Less than 30% of the men were in the normal weight range (mean BMI = 27.7, s.d. = 4.5). None of the social or demographic variables was significantly associated with misperception of healthy weight, so they were not used as covariates in subsequent analyses.
Table 1. Sample Characteristics (n = 404).
| Mean age (s.d.) | 54.9 (6.2) years |
| Mean census-tract household income (s.d.) | $38,450 ($13,135) |
| Immigrants (%) | 81.4 |
| Married (%) | 83.4 |
| Highest educational level (%) | |
| Less than high school | 29.0 |
| High-school graduate | 33.9 |
| Some college or college graduate | 37.1 |
| BMI classification (%) | |
| Normal weight | 29.0 |
| Overweight | 45.8 |
| Obese | 25.2 |
| Perception of overall health (%) | |
| Poor/fair | 24.3 |
| Good/excellent | 75.7 |
| Number of comorbidities (%) | |
| 2 or more | 61.5 |
| 0–1 | 38.5 |
What is the relation between obesity status and misperception of healthy weight? In response to the question, “What do you think is a healthy weight for you?”, 23.1% of the normal weight men, 67.0% of the overweight men, and 94.1% of the obese men reported a weight lower than their current weight, suggesting a perceived need to lose weight in order to be healthy. Very few men (12.6%) reported a weight higher than their current weight. Whereas 51.3% of the nonobese men reported a healthy weight that would put them within their normal BMI range, only 9.8% of the obese men did the same. Thus, relative to nonobese men, the obese men were significantly more likely to misperceive their healthy weight, χ2(1, N = 404) = 54.40, P < 0.001.
The mean magnitude of misperception was significantly lower in nonobese men than in obese men, t(110.06) = 8.42, P < 0.001. Relative to nonobese men, obese men grossly underestimated the amount of weight change necessary for them to be within a healthy BMI range. On average, the nonobese men perceived that they needed to lose 5.15 lb (s.d. = 11.31) to achieve a healthy weight, which is not too far from the actual 10.60 lb (s.d. = 12.67) this group would have had to lose to achieve a healthy weight by BMI standards. In contrast, the average man in the obese group perceived he needed to lose 36.12 lb (s.d. = 25.28) to achieve a healthy weight, but in reality this group was 60.48 lb (s.d. = 26.13) above what is considered to be an acceptable healthy weight by BMI standards. Thus, on average, the nonobese men misperceived their healthy weight by only 5.46 lb (s.d. = 8.03) whereas the obese men misperceived their healthy weight by 24.36 lb (s.d. = 22.18).
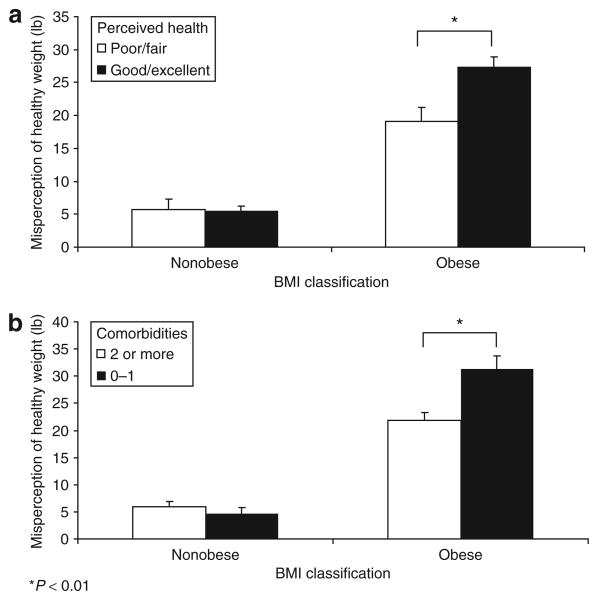
Does health status moderate the relation between misperception of healthy weight and obesity? A two (perception of overall health: poor/fair or good/excellent) by two (obese: yes or no) ANOVA revealed statistically significant main effects of perception of overall health (F(1, 399) = 5.91, P < 0.05) and obesity (F(1, 399) = 115.94, P < 0.001), as well as a significant interaction, (F(1, 399) = 6.67, P < 0.01) on misperception. The main effects showed that men who perceived their overall health to be good/excellent had greater misperceptions of healthy weight than their counterparts who perceived their health as poor/fair, and obese men had greater misperceptions of healthy weight than nonobese men. Figure 1a illustrates the interaction effect. Among obese men, those who perceived their overall health to be good/excellent had greater misperceptions of healthy weight than their counterparts who perceived their overall health to be fair/poor (P < 0.01), whereas among nonobese men there was no relation between health rating and misperception of healthy weight (P = 0.89).
Figure 1.
Misperception of healthy weight by (a) perception of overall health and (b) number of comorbidities among obese and nonobese black men.
A two (number of comorbid conditions: 0–1 or 2 or more) by two (obese: yes or no) factorial ANOVA revealed statistically significant main effects of number of comorbid conditions (F(1, 399) = 6.43, P < 0.05) and obesity (F(1, 399) = 173.52, P < 0.001), as well as a significant interaction, (F(1, 399) = 11.16, P < 0.001). The main effects showed that men with 2 or more comorbid conditions had greater misperceptions of healthy weight than their counterparts with 0–1 comorbid conditions, and obese men had greater misperceptions of healthy weight than nonobese men. Figure 1b illustrates the interaction effect. Among obese men, those with 2 or more comorbid conditions had greater misperceptions of healthy weight than their counterparts with 0–1 comorbid conditions (P < 0.01), whereas among nonobese men, there was no relation between the number of comorbid conditions and misperception of healthy weight (P = 0.39).
Discussion
In this sample of middle-aged, urban, and predominately immigrant black men, obese men were more likely than nonobese men to misperceive their healthy weight by a large and significant margin. The majority of men were aware that they should lose weight to achieve a healthy weight, especially if they were obese; however, 90.2% of obese men reported a healthy weight that would actually be unhealthy according to BMI standards. This high prevalence of misperception of healthy weight is consistent with prior research with collegeaged, African-American men (9).
Obese men in the present study grossly underestimated their weight problem, underestimating the amount of weight they would need to lose to achieve a healthy weight by an average of 24 pounds. An implication of this finding is that obese men could benefit from educational interventions that specifically address healthy weight guidelines and the propensity of some individuals to misperceive their healthy weight. Attention should be given to the fact that whereas obese men often recognize they are overweight, they are generally ill-informed about how much weight they should lose to achieve a healthy weight. Results of the present study suggest that future educational interventions should test the effectiveness of implementing a quantitative measure of misperception of healthy weight that increases awareness of misperception and provides guidance for determining a specific target weight that should be achieved to improve health status.
Lastly, we found that two measures of health status moderated the relation between misperception of healthy weight and obesity status. On average, obese men who rated their health as good or excellent underestimated the amount of weight they needed to lose to be at a healthy weight by ∼27 pounds, compared with only 19 pounds among their counterparts who rated their health as fair or poor. Further, on average, obese men who reported 0–1 comorbid conditions underestimated the amount of weight they needed to lose to be at a healthy weight by ∼31 pounds, compared with only 21 pounds among their counterparts with 2 or more comorbid conditions. There are at least two implications to draw from these findings. First, there is an acute need to increase awareness of the risks of obesity among obese individuals who are relatively healthy. Health care providers and public health messages need to communicate that obesity can take its toll on health even in individuals who are active, feel healthy, and have no apparent disease or physical health limitations. Second, among obese individuals who already have a presenting health problem, it may be relatively easy to convince them of the need to reduce their weight and to then provide resources with which to do so. In particular, health scares, such as a heart attack or a diagnosis of diabetes, may be ideal teachable moments for educating black men about obesity risks.
There are several limitations of this study. First, all data were based on self-report. Although the self-report of weight was highly reliable over many months, and research supports the validity of self-report weight measures in epidemiological studies (20–22), objective measures would increase the precision of both the BMI and misperception estimates. Concern about response burden, as well as the large geographic dispersion of this difficult to reach sample constrained our ability to collect objective measurements. Another limitation of this study is that the population was derived from an randomized controlled trail with specific eligibility criteria and is not representative of all middle-aged, urban black men in the United States, or even immigrant black men. However, because the present findings on the prevalence of misperception of healthy weight among this population converge with findings from a study of college-aged, African-American men, the findings may generalize beyond our sample. Finally, the study did not assess socio-environmental factors that might influence misperception of healthy weight, including prevalence of obesity in men's social networks, cultural norms related to ideal body size and shape, and whether or not a physician or other health care professional has ever recommended weight loss. These would all be promising directions for future research.
Another important direction for future research is to identify why misperception of weight is associated with obesity. One plausible explanation is that individuals who do not recognize or who underestimate the magnitude of their weight problem may not modify health behaviors to control weight. To test this hypothesis, future studies could examine whether misperception of healthy weight is associated with health behaviors that directly influence the development of obesity, such as physical activity and diet.
In summary, misperception of healthy weight is a strong psychological marker, or risk marker, of obesity, clearly discriminating between obese and nonobese black men. A virtue of the misperception measure used in this study is that it reveals both awareness of a weight problem and the magnitude of inaccuracy among those who misperceive their healthy weight. The present findings provide the basis for future studies to determine the prevalence of misperception of healthy weight in diverse populations and to further examine potential moderators and mediators of the relation between misperception of healthy weight and obesity. This misperception measure can be used to identify populations at elevated risk for obesity and to then target and tailor interventions aimed at effectively reducing weight among those populations. The present results reveal an acute need for health professionals and public health agencies to help black men overcome weight misperceptions, particularly if they are otherwise healthy. Misperception of healthy weight, in conjunction with information about men's health status, may be useful for targeting weight loss interventions, particularly if these variables prove to be related to individuals' stage of readiness to adopt weight reduction interventions.
Acknowledgments
This research was supported by National Institutes of Health grant R01-CA104223 (Principal Investigator: S.J.L.). The findings are those of the authors and do not represent the views of the funding agency. We acknowledge all members of the Cancer Awareness and Prevention trial research team and the participants.
Footnotes
Disclosure: The authors declared no conflict of interest.
References
- 1.Ogden CL, Carroll MD, Dowell MA, Flegal KM. NCHS Data Brief No 1. National Center for Health Statistics; Hyattsville, MD: 2007. Obesity Among Adults in the United States—No Change Since 2003–2004. [PubMed] [Google Scholar]
- 2.CDC. The Burden of Chronic Diseases and Their Risk Factors: National and State Perspectives, 2004. U.S. Department of Health and Human Services; Atlanta, GA: 2004. [Google Scholar]
- 3.Bennett GG, Wolin KY. Satisfied or unaware? Racial differences in perceived weight status. Int J Behav Nutr Phys Act. 2006;3:40. doi: 10.1186/1479-5868-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuchler F, Variyam JN. Mistakes were made: misperception as a barrier to reducing overweight. Int J Obes Relat Metab Disord. 2003;27:856–861. doi: 10.1038/sj.ijo.0802293. [DOI] [PubMed] [Google Scholar]
- 5.Chang VW, Christakis NA. Self-perception of weight appropriateness in the United States. Am J Prev Med. 2003;24:332–339. doi: 10.1016/s0749-3797(03)00020-5. [DOI] [PubMed] [Google Scholar]
- 6.Paeratakul S, White MA, Williamson DA, Ryan DH, Bray GA. Sex, race/ethnicity, socioeconomic status, and BMI in relation to self-perception of overweight. Obes Res. 2002;10:345–350. doi: 10.1038/oby.2002.48. [DOI] [PubMed] [Google Scholar]
- 7.Gregory CO, Blanck HM, Gillespie C, Maynard LM, Serdula MK. Health perceptions and demographic characteristics associated with underassessment of body weight. Obesity (Silver Spring) 2008;16:979–986. doi: 10.1038/oby.2008.22. [DOI] [PubMed] [Google Scholar]
- 8.Godino JG, Lepore SJ, Rassnick S. Obesity and Misperception of Weight Status in Immigrant and Non-immigrant Black Men. Annual Meeting of the Society of Behavioral Medicine; San Diego, CA. 29 March 2008. [Google Scholar]
- 9.Gross SM, Scott-Johnson PE, Browne DC. College-age, African-American males' misperceptions about weight status, body size, and shape. Ethn Dis. 2005;15:S5–34. [PubMed] [Google Scholar]
- 10.National Heart Lung and Blood Institute Expert Panel on the Identification Evaluation and Treatment of Overweight and Obesity in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults – The evidence report. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 11.Bennett GG, Wolin KY, Goodman M, et al. Attitudes Regarding Overweight, Exercise, and Health among Blacks (United States) Cancer Causes Control. 2006;17:95–101. doi: 10.1007/s10552-005-0412-5. [DOI] [PubMed] [Google Scholar]
- 12.Wolf RL, Lepore SJ, Vandergrift JL, et al. Knowledge, barriers, and stage of change as correlates of fruit and vegetable consumption among urban and mostly immigrant black men. J Am Diet Assoc. 2008;108:1315–1322. doi: 10.1016/j.jada.2008.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolf RL, Lepore SJ, Vandergrift JL, Basch CE, Yaroch AL. Tailored telephone education to promote awareness and adoption of fruit and vegetable recommendations among urban and mostly immigrant black men: a randomized controlled trial. Prev Med. 2009;48:32–38. doi: 10.1016/j.ypmed.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NYCDCP. The City of New York. New York, NY: 2004. The Newest New Yorkers 2000: Immigrant New York in the New Millennium Briefing Booklet. [Google Scholar]
- 15.Kaplan GA, Camacho T. Perceived health and mortality: a nine-year follow-up of the human population laboratory cohort. Am J Epidemiol. 1983;117:292–304. doi: 10.1093/oxfordjournals.aje.a113541. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan GA, Goldberg DE, Everson SA, et al. Perceived health status and morbidity and mortality: evidence from the Kuopio ischaemic heart disease risk factor study. Int J Epidemiol. 1996;25:259–265. doi: 10.1093/ije/25.2.259. [DOI] [PubMed] [Google Scholar]
- 17.McGee DL, Liao Y, Cao G, Cooper RS. Self-reported health status and mortality in a multiethnic US cohort. Am J Epidemiol. 1999;149:41–46. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- 18.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 19.SPSS. SPSS for Windows Release 16.0.1. SPSS; Chicago, IL: 2007. [Google Scholar]
- 20.Bowman RL, DeLucia JL. Accuracy of self-reported weight: a meta-analysis. Behav Ther. 1992;23:637–655. [Google Scholar]
- 21.Palta M, Prineas RJ, Berman R, Hannan P. Comparison of self-reported and measured height and weight. Am J Epidemiol. 1982;115:223–230. doi: 10.1093/oxfordjournals.aje.a113294. [DOI] [PubMed] [Google Scholar]
- 22.Stunkard AJ, Albaum JM. The accuracy of self-reported weights. Am J Clin Nutr. 1981;34:1593–1599. doi: 10.1093/ajcn/34.8.1593. [DOI] [PubMed] [Google Scholar]