Abstract
Introduction
Predominantly uncontrolled studies suggest that there may be a greater risk of subsequent vertebral compression fractures (VCFs) associated with vertebroplasty and kyphoplasty. To further understand the risk of VCFs, we conducted a population-based retrospective cohort study using data from a large regional health insurer.
Materials and Methods
Administrative claims procedure codes were used to identify a treatment group of patients receiving either a vertebroplasty or kyphoplasty (treatment group) and a comparison group of patients with a primary diagnosis of VCF who did not receive treatment during the same time period. The main outcomes of interest, validated by two independent medical record reviewers and adjudicated by a physician panel, were any new VCFs within: 1) 90-days; 2) 360-days; and 3) at adjacent vertebral levels. Multivariable logistic regression examined the association of vertebroplasty/kyphoplasty with new VCFs.
Results
Among 48 treatment (51% vertebroplasty, 49% kyphoplasty) and 164 comparison patients, treated patients had a significantly greater risk of secondary VCFs than comparison patients for fractures within 90 days of the procedure or comparison group time point (adjusted odds ratio (OR) = 6.3; 95% confidence interval (CI) 1.7 – 23.0) and within 360 days (adjusted OR = 3.1; 95% CI:1.1 – 8.4). Vertebroplasty and kyphoplasty were associated with a significantly greater rate of adjacent-level fractures as well.
Conclusions
Patients who had undergone vertebroplasty and kyphoplasty had a greater risk of new VCFs compared to patients with prior VCFs who did not undergo either procedure.
Vertebroplasty and kyphoplasty are minimally invasive procedures for treatment of vertebral compression fractures (VCF) that involve the percutaneous instillation of bone cement (most commonly polymethylmethacrylate) into a fractured vertebra (1). Although these procedures have been used since the 1980s primarily for pain relief and restoration of vertebral body height, there is little evidence of their longer-term safety from either randomized controlled trials or controlled observational studies (2–4). Limited biomechanical testing data and several small uncontrolled studies suggest that fractured vertebrae treated with bone cements are stiffer than untreated vertebrae and thus may transfer greater load to adjacent vertebral levels (5,6). Thus, there is concern that these procedures could lead to a heightened rate of subsequent VCFs.
Using a retrospective cohort study design of persons who received either vertebroplasty or kyphoplasty compared to persons with confirmed VCFs who were not treated with either procedure, we examined whether vertebroplasty and kyphoplasty were associated with a higher risk of secondary VCFs both at any site and at adjacent vertebrae.
MATERIALS AND METHODS
Treatment Group
A group of treated patients, having at least one vertebroplasty or kyphoplasty procedure from January 1, 2003 to June 30, 2004, was identified based on Current Procedural Terminology (CPT)-4 codes or Healthcare Common Procedure Coding System (HCPCS) codes (Appendix 1) from the administrative claims data of a large regional not-for-profit health care insurer, Blue Cross and Blue Shield of Alabama, with over 3-million enrollees. Administrative data included information on inpatient, outpatient, and physician claims as well as patient demographics. Based on review of the longitudinal profiles, we defined an index event for a treated patient (18 years or older at the time) as their incident procedure during the study period.
To create a cohort with an incident procedure, patients with confirmed vertebroplasty or kyphoplasty from January 2001 through December 31, 2002 (run-in period) were excluded. Exclusions for cancer also were applied using administrative data (see Appendix 1).
In order to be as representative as possible, we included procedure claims that were both paid and rejected by the insurer. Patients were excluded if medical record reviews could not confirm the procedure or the baseline VCF, or if the VCFs were a consequence of high trauma fractures (i.e., motor vehicle accidents), primary bone tumors, or metastatic cancer.
Comparison Group
We also constructed a comparison group of patients with at least one VCF within the same 18-month study period, but without evidence of a vertebroplasty or kyphoplasty procedure. The comparison group, identified from claims data, included all patients18 years of age or older at the time of the index date with primary diagnoses of VCF based on International Classification of Disease (ICD-9) codes (Appendix 1) during the study period used for the treatment patients. Neither potential treatment nor comparison patients were excluded for VCF diagnoses during the run-in period. Due to the large number of treatment patients with a diagnostic code for pathologic fracture (ICD-9 code 733.13) but no evidence of cancer in the claims data, we included this diagnosis for comparison patients as well. Patients with the same contraindications as the treatment patients were excluded using both the claims data (see Appendix1) and the medical record review. To enhance the comparability of the comparison and treatment groups and to control for the relevant confounding factor of age, we matched each treatment patient with 8 comparison patients by age (± 5 years). Similar to the treatment group, we defined an index event for a comparison patient as their incident VCF diagnosis during the study period.
Medical Record Reviews
To confirm the vertebroplasty/kyphoplasty procedures for the treatment patients, after identifying patients using administrative data, the health care insurer requested medical records documenting patient histories, physical exams, and procedure notes from the appropriate hospital, outpatient facility or physician's office. For both the treatment and comparison cohorts, all radiological reports (spinal radiology, magnetic resonance imagery, computerized tomography, and/or bone scans) following the index event were requested to determine the diagnosis/sites of possible subsequent VCFs during the study time period. Three follow-up phone requests, approximately 3 to 4 weeks apart, were made to non-responsive facilities in an effort to collect all appropriate records. Medical records were independently reviewed by two investigators (AM, RN) for details on the vertebroplasty/kyphoplasty procedure, diagnosis and location of treatment fracture, history of other fractures, co-morbidities, and other osteoporosis treatment. Fractures occurring at the index event (index fractures) were classified as either incident or prevalent fractures. A subsequent VCF was only validated in the comparison group if the location of the index fracture was available in medical records. Any discordance in record reviewers was adjudicated by consensus of a physician panel of co-authors. The review protocol was established prior to review of records and the medical record data was abstracted into a customized version of a MedQuest database (developed by Fu and associates under contract from the Health Care Financing Administration).
Outcomes of Interest, Explanatory Variables, and Key Covariates
The main outcome of interest was a subsequent VCF following the index event. Since the vertebra receiving vertebroplasty/ kyphoplasty is unlikely to be diagnosed as having a progression of an existing fracture, our primary analysis was restricted to new VCFs occurring at a different level than the baseline fracture. Because we wished to allow for the possibility that the treatment mitigates same-level fractures, a secondary analysis included the progression (worsening) of VCFs at the same vertebral level (progressive fracture) among the comparator patients. Separate analyses also examined adjacent-level fractures, defined as VCFs that occurred within 3-vertebral levels above or below the treated or index VCF. The date of the subsequent VCF was defined as the first time the fracture was described in the available radiology reports following the index event. Because of concern about censoring due to patient death and other losses to follow-up that are not captured by administrative data, we evaluated this outcome at two separate time periods, 90 days and 360 days after the index event. The key explanatory variable was whether patients received vertebroplasty/kyphoplasty or not.
Other variables examined included patient demographics (i.e., age and sex), frequency of administrative claims for outpatient and physician visits, and co-morbidities. Using ICD-9 primary and secondary diagnosis codes available in claims data during the period from 180 days prior to and 90 days post the index date, we created a count for each patient of 30 co-morbid indicators based on the work by Elixhauser et al. (7) (see Table 1) and a separate indicator of an osteoporosis diagnosis (ICD-9 code: 733.0X) prior to their index date.
TABLE 1.
BASELINE CHARACTERISTICS OF PATIENTS IN VERTEBROPLASTY/KYPHOPLASTY TREATMENT AND COMPARISON GROUPS*
| Treatment (n=48) | Comparison (n=164) | p-value | |
|---|---|---|---|
| Sex, % men | 16 (33.3%) | 72 (43.6%) | 0.2 |
| Age, years | 62.1 ± 12.2 | 63.7 ± 12.0 | 0.4 |
| Osteoporosis Diagnosis in the 180 days prior to index | 13 (27%) | 32 (20%) | 0.2 |
| Number of physician visits in the 180 days prior to index | 5.19 ± 5.92 | 5.28 ± 5.88 | 0.9 |
| Number of comorbidities‡ | 3.8 ± 2.9 | 3.6 ± 3.2 | 0.7 |
| Baseline/Treatment Fracture Sites | |||
| Thoracic spine | 25 (52%) | 73 (45%) | 0.4 |
| Lumbar spine | 22 (46%) | 69 (42%) | 0.6 |
| Both | 1 (2%) | 21 (13%) | < 0.05 |
| Multiple vertebral fractures at Baseline | 19 (40%) | 51 (31%) | 0.3 |
n, (%) or mean ± SD
Index = incident vertebroplasty/kyphoplasty procedure for a treatment patient; incident VCF diagnosis for a comparison patient
Disease count using administrative claims for the following 30 comorbidities: congestive heart failure, arrhythmias, valvular disease, pulmonary disease, peripheral vascular disease, hypertension, paralysis, other neurological disorders, chronic pulmonary disease, diabetes, diabetes w/ chronic complications, hypothyroidism, renal failure, liver disease, peptic ulcer disease, AIDS, lymphoma, metastatic cancer, solid tumor w/out metastasis, rheumatoid arthritis, coagulopathy, obesity, weight loss, fluid and electrolyte disorders, chronic blood loss anemia, deficiency anemias, alcohol abuse, drug abuse, psychoses, depression
Statistical analysis
Univariate descriptive statistics first examined the association of vertebroplasty and kyphoplasty (considered together) with outcomes of interest. We then used multivariable logistic regression to adjust for potential confounding factors. Final models included adjustment for number of co-morbidities, indicator of osteoporosis diagnosis prior to index date, and age. To assess a potentially greater rate of subsequent VCFs among persons hospitalized with this condition or among VCFs characterized as new by a radiologist, we performed sensitivity analyses on these subsets. SAS software (version 9.1) was used for all statistical analyses (SAS Institute, Cary, NC).
RESULTS
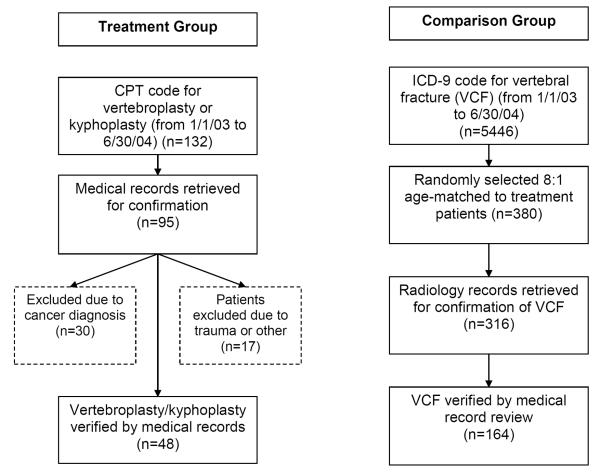
Using administrative claims data, we identified 132 patients who had a CPT-4 or HPCS code for a vertebroplasty or kyphoplasty procedure during the study time period (Figure 1). Of these 132 patients, we retrieved medical records for 95 (72%) of the patients. After medical record review, a total of 48 (51% of those with available medical records) patients met the criteria for inclusion in treatment group. Using administrative claims data from the same time period, a total of 380 patients with a primary ICD-9 code for a VCF were identified for the comparison group. Of these 380 patients, we obtained radiology records for 316 (83%) of them and we confirmed an eligible VCF by medical record review for 164 (52%) patients that met the other criteria for the comparison group. Concordance of radiologic findings among medical record reviewers was 85.7%.
FIGURE 1.
SUMMARY DIAGRAM OF SELECTION OF VERTEBROPLASTY/KYPHOPLASTY TREATMENT AND COMPARISON GROUPS
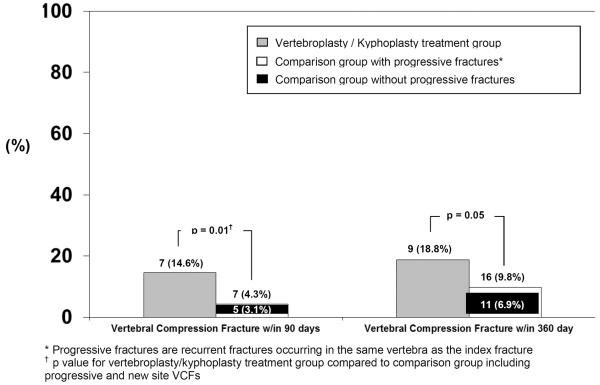
Characteristics of treatment and comparison groups are shown in Table 1. The comparison group non-significantly trended towards being slightly older and was more likely to be men. Treatment patients trended towards being more likely to have an osteoporosis diagnosis prior to the index date. Patients in each groups had similar comorbidity profiles, with a mean comorbidity count of just less than four. Just over half of the fractures treated with vertebroplasty/kyphoplasty were in the thoracic spine and one patient in the treatment group had treatment in both the thoracic and lumber spine (T12 and L1). The number of prevalent VCFs was similar in the comparison group (mean number of baseline fractures = 1.71 ± 0.99 in treatment group vs. 1.61 ± 1.17 in comparison group; p = 0.59). There were no significant difference between the comparison group and the treatment group in terms of multiple fractures at baseline. The risk of a secondary VCF is shown in Figure 2. The proportion of patients in the treatment group with confirmed subsequent VCFs at 90-days post index fracture had almost five times the risk of the comparison group (omitting progressive fractures) and over three times that of the comparison group when including progressive VCFs. At 360-days post index, approximately 19% of treatment patients had a subsequent VCF compared to just fewer than 7% of the comparison group. This latter proportion increased to 10% if progressive VCFs at the same level were included. The median time to fracture in the treatment group was within 2 months of the vertebroplasty / kyphoplasty procedure, compared to over 3 months in the comparison group (median days to subsequent fracture = 47; intra-quartile range (IQR): 22–71 vs. 106; IQR: 61–154, p = NS) (data not shown). The number of physician visits within 360-days post the index date varied significantly between the treatment (14.0 ± 14.0) and comparison groups (25.2 ± 23.7, p < 0.01) (data not shown). Cement leakage was identified as an immediate adverse event of 19% (n = 9) of the treatment patients and did not differ by type of procedure. Four (8%) of the 48 patients had a vertebroplasty or kyphoplasty performed concurrently at more than one spinal level.
FIGURE 2.
PROPORTION OF VERTEBROPLASTY/KYPHOPLASTY TREATMENT (N=48) AND COMPARISON (N=164) GROUP PATIENTS WITH SECONDARY FRACTURES
Table 2 shows the rates and odds of secondary VCFs stratified by time (either 90 or 360 days post index) and by subsequent fracture location. Treatment group patients were significantly more likely than comparison group patients to have a subsequent VCF, even after accounting for the important co-factors of osteoporosis diagnosis before the index date, number of comorbidities, and age. This effect was particularly noticeable within 90 days and increased in magnitude after multivariate adjustment (OR = 6.3; 95% CI: 1.7–23.0). In both groups, the odds of experiencing additional adjacent level fractures was significantly increased, particularly within 90 days. Vertebral compression fractures at adjacent levels (within 3 levels from the index fracture) for this same time period were also significantly greater in the treatment group (16.7%) versus the comparison group (6.3%). The odds of a subsequent fracture in the treatment group vs. the comparison group when including progressive fractures were similar to the primary analysis at 90-days (OR = 4.9; 95% CI: 1.5–16.1) (data not shown). In sensitivity analyses examining relationships within 90 days post-index date, secondary VCFs non-significantly trended towards being more common among treatment patients when compared to comparison group patients that were hospitalized with their index fractures (48 in treatment group and 37 in comparison group; adjusted OR = 3.0, 95% CI 0.4 – 19.5). In addition, among patients with index fractures characterized as new in both groups (26 in treatment group and 65 in comparison group) we saw a similar nonsignificant trend (adjusted OR = 3.9, 95% CI 0.7 – 21.4).
TABLE 2.
RATES, CRUDE, AND ADJUSTED ODDS OF SECONDARY VERTEBRAL COMPRESSION FRACTURES (VCFS)* BY TIME PERIOD AND FRACTURE LOCATION FOR VERTEBROPLASTY/KYPHOPLASTY (TREATMENT) AND COMPARISON GROUPS
| Treatment n (%) | Comparison n (%) | Unadjusted Odds (95% CI) | Adjusted Odds (95% CI)‡ | |
|---|---|---|---|---|
| Within 90-days Post-Index † | ||||
| Any secondary VCF | 7 (14.6%) | 5 (3.1%) | 5.4 (1.6–18.0) | 6.3 (1.7–23.0) |
| Adjacent fracture within 3 vertebrae | 6 (12.5%) | 5 (3.1%) | 4.5 (1.3–15.6) | 5.1 (1.4–18.7) |
| Adjacent fracture within 2 vertebrae | 5 (10.4%) | 4 (2.5%) | 4.7 (1.2–18.1) | 4.8 (1.2–19.9) |
| Adjacent fracture within 1 vertebra | 4 (8.3%) | 3 (1.9%) | 4.9 (1.1–22.6) | 4.6 (1.0–21.7) |
| Within 360-day Post-Index | ||||
| Any secondary VCF | 9 (18.8%) | 11 (6.9%) | 3.2 (1.2–8.3) | 3.1 (1.1–8.4) |
| Adjacent fracture within 3 vertebrae | 8 (16.7%) | 10 (6.3%) | 3.1 (1.1–8.3) | 3.0 (1.1–8.6) |
| Adjacent fracture within 2 vertebrae | 7 (14.6%) | 9 (5.7%) | 2.9 (1.0–8.4) | 2.8 (0.9–8.2) |
| Adjacent fracture within 1 vertebra | 4 (8.3%) | 7 (4.4%) | 2.0 (0.6–7.3) | 1.8 (0.5–6.6) |
Does not include progression of existing vertebral fractures in the comparison group
Index = incident vertebroplasty/kyphoplasty procedure for a treatment patient; incident VCF diagnosis for a comparison patient
Multivariable logistic regression analysis adjusted for osteoporosis diagnosis before index, number of comorbidities, and age
DISCUSSION
Vertebroplasty and kyphoplasty procedures were developed to improve short-term outcomes from painful vertebral fractures (8,9), but the long-term safety of these procedures is still unknown. In comparison to a group of patients not undergoing vertebroplasty/kyphoplasty, our retrospective cohort study identified a significant increased risk of subsequent vertebral fractures among patients treated with these procedures for non-traumatic, non-cancer-related VCFs, especially within 3 months of the procedure. As predicted from biomechanical studies (5,6,10), fractures at adjacent levels (within 3 vertebrae of the treated fracture) were significantly more likely to occur in the treatment group.
To our knowledge, no prior studies of vertebroplasty or kyphoplasty outcomes have included a population-based comparison group. The majority of vertebroplasty evidence consists of primarily retrospective, single-center studies which lack a control group (11). Two non-randomized prospective studies comparing vertebroplasty to conservative treatment, recruited from those patients who refused a vertebroplasty procedure, found little difference in longer-term outcomes or subsequent fractures (12,13). These studies had relatively short follow-up and contained small control groups.
Previous uncontrolled prospective studies of vertebroplasty procedures conducted at a single facility have shown that the rate of subsequent incident VCF among patients treated with vertebroplasty ranges from 18% to 36% within one year (14–18). Similarly, retrospective single-center studies have found subsequent fracture rates among vertebroplasty (19–21) and kyphoplasty (22,23) patients of 12% to 26%. Our controlled study based in a regional private insurance population showed a one-year rate of secondary VCF of 18.8% among treated patients compared to the control group rate of 9.7%. The timing of post-vertebroplasty VCFs in our study also is consistent with prior vertebroplasty studies, which have shown that between 43% and 67% of subsequent incident fractures occur within 3 months of the treatment procedure (21,24,25). The fracture rate in our comparison group was similar to randomized controlled trial fracture rates among control-group patients with at least 2 prior VCFs (26) and at least 1 VCF or low bone mineral density measurements (T-score < −2.5 at femoral neck or lumbar spine) (27,28).
Several studies suggest that patients are at a higher risk for adjacent level fractures following a vertebroplasty (14,25), especially during the first 3 months (21,22,25). One retrospective analysis of vertebroplasty patients at a single institution showed an almost 5-fold increased risk of fracture at an adjacent level compared to a non-adjacent level fracture (25). In our study, the risk of adjacent level fractures also showed an approximately 5-fold increase within 90-days for each of the adjacent fracture levels.
Cement leakage, the most common complication of vertebroplasty and kyphoplasty procedures, may occur more often than clinically detected (29,30), and it is thought this may increase the possibility of adjacent fractures (31). In our study, although approximately 19% of treated patients had mention of this occurrence in the procedural records, we were underpowered to explore a possible relationship.
Despite the large size and good generalizability of the health plan we examined, there were a relatively small number of vertebroplasty and kyphoplasty procedures performed during our study time period. This was partially based on strict exclusion and validation criteria for patients receiving care in this health plan. The small number of secondary fracture outcomes and inconsistently reported information in medical records (i.e. osteoporosis medications) limited potential subgroup analyses and the number of covariates we could control for as potential confounders of the relationship between treatment exposure and fractures. However, our ability to control for age, osteoporosis diagnosis and comorbidity, and the fact that the magnitude of our estimates increased as adjustments were made, add to the strength of our findings. Examining subsets of patients with incident fractures and only comparison group patients requiring hospitalizations for their VCFs further adjusted for possible case mix variations. Although the magnitude of the treatment effect was attenuated, the trend towards increased fracture risk with vertebroplasty/kyphoplasty persisted in these underpowered sensitivity analyses. Additionally, our study was underpowered to specifically examine specific differences between kyphoplasty and vertebroplasty.
As with any study using administrative data, one limitation may be misclassification of patients due to coding errors. In an effort to minimize misclassification of outcomes we established stringent study inclusion criteria, including only validated fractures confirmed by review of medical records. We found that 60% of treatment patients who did not have evidence of cancer either in the claims data or medical records still had received a diagnosis claim for a pathologic vertebral fracture (CPT-4 code: 733.13) in the administrative data. Therefore, since medical record confirmation was required of all patients, we included those with a pathologic fracture code in the comparison group as well. It is possible, due to varying quality of records received, that some patients may have been misclassified as to the indication for their fracture, however, it is unlikely that differential misclassification occurred between treatment or comparison groups.
A potential limitation of all retrospective cohort studies is the possibility of diagnostic detection bias (differential outcome ascertainment). Specifically, it is possible that patients who had a vertebroplasty or kyphoplasty procedure were more likely to be followed more closely by their physician and have additional radiographic procedures documented. Yet, in our study, the comparison group had a similar mean number of physician visits in the 180 days prior to the index event, but a significantly higher mean number of physician visits than the treatment group within the year following the index event. The reason for this difference is not clear but would seem to only increase the possibility of detecting new fractures in the comparison group, thereby biasing towards the null hypothesis.
Although vertebroplasty and kyphoplasty procedures have been shown to be efficacious for short-term pain relief, our finding of an increased risk of subsequent fractures in a controlled population-based study of insured patients raises concern about their short-to moderate-term safety. Although randomized controlled clinical trials to further study the long-term impact of these procedures are clearly needed to better define their place in the osteoporosis treatment armamentarium, challenges in recruitment to such trials (2) lead to an important role of carefully conducted observational studies to address timely questions of clinical relevance.
Supplementary Material
Acknowledgements
the authors thank Katherine Jackson Donnithorn and Raj Nair, MD for their assistance in medical record review.
Supported by grants no. HS10389-07 from the Agency for Healthcare Research and Quality (AHRQ); no. AR52361-92 from the National Institute of Arthritis and Musculoskeletal and Skin Disease; and Social & Scientific Systems, Inc. contract no. 223-02-6003 with the Center for Devices and Radiological Health of the Food and Drug Administration (FDA)
Footnotes
Publisher's Disclaimer: The opinions or assertions presented herein are the private views of the authors and are not to be construed as conveying either an official endorsement or criticism by the U.S. Department of Health and Human Services, the Public Health Service, or the U.S. Food and Drug Administration
References
- 1.Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26(14):1511–5. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 2.Kallmes DF. Randomized vertebroplasty trials: Current status and challenges. Acad Radiol. 2006;13(5):546–9. doi: 10.1016/j.acra.2006.01.054. [DOI] [PubMed] [Google Scholar]
- 3.Melton LJ, 3rd, Kallmes DF. Epidemiology of vertebral fractures: implications for vertebral augmentation. Acad Radiol. 2006;13(5):538–45. doi: 10.1016/j.acra.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 4.Truumees E, Hilibrand A, Vaccaro AR. Percutaneous vertebral augmentation. Spine J. 2004;4(2):218–29. doi: 10.1016/j.spinee.2003.08.029. [DOI] [PubMed] [Google Scholar]
- 5.Berlemann U, Ferguson SJ, Nolte LP, Heini PF. Adjacent vertebral failure after vertebroplasty: A biomechanical investigation. 2002;84-B:748–752. doi: 10.1302/0301-620x.84b5.11841. [DOI] [PubMed] [Google Scholar]
- 6.Polikeit A, Nolte L, Ferguson S. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis. Spine. 2003;28(10):991–6. doi: 10.1097/01.BRS.0000061987.71624.17. [DOI] [PubMed] [Google Scholar]
- 7.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Brown DB, Gilula LA, Sehgal M, Shimony JS. Treatment of Chronic Symptomatic Vertebral Compression Fractures with Percutaneous Vertebroplasty. 2004;182:319–322. doi: 10.2214/ajr.182.2.1820319. [DOI] [PubMed] [Google Scholar]
- 9.Kasperk C, Hillmeier J, Noldge G, Grafe IA, DaFonseca K, Raupp D, Bardenheuer H, Libicher M, Liegibel UM, Sommer U, Hilscher U, Pyerin W, Vetter M, Meinzer H-P, Meeder P-J, Taylor RS, Nawroth P. Treatment of Painful Vertebral Fractures by Kyphoplasty in Patients With Primary Osteoporosis: A Prospective Nonrandomized Controlled Study. 2005;20:604–612. doi: 10.1359/JBMR.041203. [DOI] [PubMed] [Google Scholar]
- 10.Baroud G, Nemes J, Heini P, Steffen T. Load shift of the intervertebral disc after a vertebroplasty: a finite-element study. European Spine Journal. 2003;12(4):421–426. doi: 10.1007/s00586-002-0512-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trout AT, Kallmes DF. Does vertebroplasty cause incident vertebral fractures? A review of available data. AJNR Am J Neuroradiol. 2006;27(7):1397–403. [PMC free article] [PubMed] [Google Scholar]
- 12.Diamond T, Bryant C, Browne L, Clark W. Clinical outcomes after acute osteoporotic vertebral fractures: a 2-year non-randomised trial comparing percutaneous vertebroplasty with conservative therapy. Med J Aust. 2006;184(3):113–7. doi: 10.5694/j.1326-5377.2006.tb00148.x. [DOI] [PubMed] [Google Scholar]
- 13.Diamond TH, Champion B, Clark WA. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. The American Journal of Medicine. 2003;114(4):257–265. doi: 10.1016/s0002-9343(02)01524-3. [DOI] [PubMed] [Google Scholar]
- 14.Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, Fardellone P. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford) 2000;39(12):1410–4. doi: 10.1093/rheumatology/39.12.1410. [DOI] [PubMed] [Google Scholar]
- 15.Kobayashi K, Shimoyama K, Nakamura K, Murata K. Percutaneous vertebroplasty immediately relieves pain of osteoporotic vertebral compression fractures and prevents prolonged immobilization of patients. European Radiology. 2005;15(2):360–367. doi: 10.1007/s00330-004-2549-0. [DOI] [PubMed] [Google Scholar]
- 16.Komemushi A, Tanigawa N, Kariya S, Kojima H, Shomura Y, Komemushi S, Sawada S. Percutaneous Vertebroplasty for Osteoporotic Compression Fracture: Multivariate Study of Predictors of New Vertebral Body Fracture. CardioVascular and Interventional Radiology. 2006;29(4):580–585. doi: 10.1007/s00270-005-0138-5. [DOI] [PubMed] [Google Scholar]
- 17.Voormolen MHJ, Lohle PNM, Juttmann JR, Graaf Yvd, Fransen H, Lampmann LEH. The Risk of New Osteoporotic Vertebral Compression Fractures in the Year after Percutaneous Vertebroplasty. 2006;17:71–76. doi: 10.1097/01.RVI.0000190910.43602.3C. [DOI] [PubMed] [Google Scholar]
- 18.Layton KF, Thielen KR, Koch CA, Luetmer PH, Lane JI, Wald JT, Kallmes DF. Vertebroplasty, first 1000 levels of a single center: evaluation of the outcomes and complications. AJNR Am J Neuroradiol. 2007;28(4):683–9. [PMC free article] [PubMed] [Google Scholar]
- 19.Lee W, Sung K, Jeong H, Sung Y, Hyun Y, Choi J, Lee K, Ok C, Choi Y. Risk factors of developing new symptomatic vertebral compression fractures after percutaneous vertebroplasty in osteoporotic patients. European Spine Journal. 2006;15(12):1777–1783. doi: 10.1007/s00586-006-0151-7. [DOI] [PubMed] [Google Scholar]
- 20.Syed MI, Patel NA, Jan S, Harron MS, Morar K, Shaikh A. New symptomatic vertebral compression fractures within a year following vertebroplasty in osteoporotic women. AJNR Am J Neuroradiol. 2005;26(6):1601–4. [PMC free article] [PubMed] [Google Scholar]
- 21.Uppin AA, Hirsch JA, Centenera LV, Pfiefer BA, Pazianos AG, Choi IS. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003;226(1):119–24. doi: 10.1148/radiol.2261011911. [DOI] [PubMed] [Google Scholar]
- 22.Fribourg D, Tang C, Sra P, Delamarter R, Bae H. Incidence of subsequent vertebral fracture after kyphoplasty. Spine. 2004;29(20):2270–6. doi: 10.1097/01.brs.0000142469.41565.2a. discussion 2277. [DOI] [PubMed] [Google Scholar]
- 23.Harrop JS, Prpa B, Reinhardt MK, Lieberman I. Primary and secondary osteoporosis' incidence of subsequent vertebral compression fractures after kyphoplasty. Spine. 2004;29(19):2120–5. doi: 10.1097/01.brs.0000141176.63158.8e. [DOI] [PubMed] [Google Scholar]
- 24.Tanigawa N, Komemushi A, Kariya S, Kojima H, Shomura Y, Sawada S. Radiological Follow-up of New Compression Fractures Following Percutaneous Vertebroplasty. CardioVascular and Interventional Radiology. 2006;29(1):92–96. doi: 10.1007/s00270-005-0097-x. [DOI] [PubMed] [Google Scholar]
- 25.Trout AT, Kallmes DF, Kaufmann TJ. New fractures after vertebroplasty: adjacent fractures occur significantly sooner. AJNR Am J Neuroradiol. 2006;27(1):217–23. [PMC free article] [PubMed] [Google Scholar]
- 26.Reginster JY, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, Lund B, Ethgen D, Pack S, Roumagnac I, Eastell R. Randomized Trial of the Effects of Risedronate on Vertebral Fractures in Women with Established Postmenopausal Osteoporosis. Osteoporosis International. 2000;11(1):83–91. doi: 10.1007/s001980050010. [DOI] [PubMed] [Google Scholar]
- 27.Boonen S, McClung MR, Eastell R, El-Hajj Fuleihan G, Barton IP, Delmas P. Safety and Efficacy of Risedronate in Reducing Fracture Risk in Osteoporotic Women Aged 80 and Older: Implications for the Use of Antiresorptive Agents in the Old and Oldest Old. 2004;52:1832–1839. doi: 10.1111/j.1532-5415.2004.52506.x. [DOI] [PubMed] [Google Scholar]
- 28.Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, Christiansen C, Delmas PD, Zanchetta JR, Stakkestad J, Gluer CC, Krueger K, Cohen FJ, Eckert S, Ensrud KE, Avioli LV, Lips P, Cummings SR, Multiple Outcomes of Raloxifene Evaluation I Reduction of Vertebral Fracture Risk in Postmenopausal Women With Osteoporosis Treated With Raloxifene: Results From a 3-Year Randomized Clinical Trial. 1999;282:637–645. doi: 10.1001/jama.282.7.637. [DOI] [PubMed] [Google Scholar]
- 29.Schmidt R, Cakir B, Mattes T, Wegener M, Puhl W, Richter M. Cement leakage during vertebroplasty: an underestimated problem? European Spine Journal. 2005;14(5):466–473. doi: 10.1007/s00586-004-0839-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yeom JS, Kim WJ, Choy WS, Lee CK, Chang BS, Kang JW. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. 2003;85-B:83–89. doi: 10.1302/0301-620x.85b1.13026. [DOI] [PubMed] [Google Scholar]
- 31.Lin EP, Ekholm S, Hiwatashi A, Westesson P-L. Vertebroplasty: Cement Leakage into the Disc Increases the Risk of New Fracture of Adjacent Vertebral Body. 2004;25:175–180. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.