Abstract
Background
Police officers are frequently exposed to situations that can negatively impact their mental health.
Methods
We conducted this study of an urban police department to determine 1) the prevalence of post-traumatic stress disorder (PTSD), depression, and alcohol abuse; 2) patterns of and barriers to mental-health services utilization; and 3) the impact these conditions have on productivity loss.
Results
Among 150 officers, PTSD (24%), depression (9%), and alcohol abuse (19%) were common. Only 46.7% had ever sought mental-health services; the most commonly cited barriers to accessing services were concerns regarding confidentiality and the potential “negative career impact.” Officers with mental-health conditions had higher productivity loss (5.9% vs 3.4%, P <0.001) at an annual cost of $ 4,489 per officer.
Conclusion
Mental-health conditions among police officers are common, and costly, yet most officers had never accessed mental-health services; many due to modifiable risk factors.
Introduction
In 2009, over 8,500 connecticut police officers1 investigated reports of sexual assault, homicide, and armed robbery,2 with one in 11 officers physically assaulted.3 Over the course of a career, this work environment, coupled with a culture that values stoicism and self-reliance,4 may adversely impact an officer's mental health, contributing to high rates of post-traumatic stress disorder,5,6 alcohol abuse,7,8 and depression.9,10 Together, these conditions may contribute to at-work productivity loss, and worse, higher than expected suicide rate among police officers.11 In Connecticut alone, four police officers committed suicide in 2011, prompting a statewide conference to discuss potential interventions.12
To address the psychological distress experienced by officers, many police departments provide mental-health services through Employee Assistance Programs (EAPs).13–15 These programs are subsidized by local governments to establish peer-support groups, provide cognitive behavioral therapies, and conduct officer debriefings following a critical incident, eg, officer-involved shootings. Despite the availability of these services, officers continue to experience significant psychological distress.
In an effort to better understand mental-health issues among officers in our own community, we partnered with the New Haven Police Union, the New Haven Police Department (NHPD), and local health-care providers. New Haven, the second largest city in Connecticut, has a population of approximately 128,000 people served by a police force of over 400 sworn officers.16 We were cognizant that developing a successful intervention would require an understanding of police officer health at the local level. We conducted this study to determine 1) the prevalence of post-traumatic stress disorder (PTSD), depression, and alcohol abuse among officers; 2) patterns of and barriers to mental-health services utilization; and 3) the subsequent impact these conditions have on productivity loss.
Methods
Community-Partnered Research
Utilizing a community-based participatory research (CBPR) approach,17 we conducted this project—from initial study design to final dissemination of results—as a University-Community research partnership, bringing together members the New Haven Police Union and NHPD administration, EAP health services providers, a physician serving in the armed forces (JF), and faculty at the Yale Schools of Medicine and Public Health (MD, MR, GL). While the partnership was borne out of national and local concerns, the formal collaboration allowed us to use a combination of personal experience, personal knowledge, and the medical and public health literature to identify areas of health concerns for local police officers and ultimately provide the basis for developing local interventions. In the current study, a subcommittee of the larger research team (consisting of the physician serving in the armed forces and members of the Police Union leadership) identified health concerns to assess and worked with the larger team to develop group consensus. From this process, we developed the key aims and constructed a survey using previously validated instruments when possible.
Survey Questionnaire
First, we gathered basic demographic and work history information. second, we assessed the prevalence of mental-health conditions using: 1) items from the Behavioral Risk Factor Surveillance System (BRFSS) survey assessing self-reported mental-health conditions;18 2) the Department of veterans Affairs PTSD-Primary Care (PTSD-PC)19 screening questionnaire; and 3) the CAGE questionnaire20,21 to assess potential alcohol misuse. Specifically, the PTSD-PC consists of four yes/no questions regarding PTSD symptoms in the previous 30 days, with one point given for each affirmative response. A score of three or four points is considered a positive screen for PTSD. Similarly, the CAGE questionnaire has four yes/no questions regarding alcohol use, with one point given for each affirmative answer. For the CAGE questions, answering “yes” to even one question is concerning for alcohol misuse or abuse (see Appendix for specific questions).
Third, we assessed self-reported mental-health services utilization and barriers to service use. Respondents were asked if they had ever accessed mental-health services through the EAP or from a non-EAP (outside the department) provider. In addition, they were asked, “Do you have any concerns in accessing EAP services if you felt they were needed?” Respondents could identify “no concerns” or select up to five prescripted potential concerns: cost of services, unsure how to access services, potential negative impact on one's career, negative coworker perceptions, and concerns over confidentiality. These responses were selected by and piloted with police officers prior to fielding the survey.
Finally, we estimated on-the-job productivity loss due to health reasons, or presenteeism, using the Work Limitations Questionnaire (WLQ-8).22 The WlQ-8 contains eight questions regarding how frequently, over the past two weeks, the respondent had difficulty performing four kinds of tasks due to either physical or emotional health. Specific tasks include time management, physical tasks, mental-interpersonal tasks, and one's ability to complete a task. For each item, respondents rate their difficulty on a five-point scale ranging from one (difficult none of the time) to five (difficult all of the time). Based on these responses, the WLQ-8 coding algorithm produces four “task-level” scores and one “summary” score. Each of the four task-level scores is interpreted as the percentage of time a respondent had difficulty performing the given task over the last two weeks due to health reasons. The summary score represents the percentage of productivity lost at work over the last two weeks due to health reasons. The estimated productivity loss can then be compared to benchmark data.23 Additionally, the percent productivity loss can be extrapolated to a one-year timeframe and multiplied by the respondents' annual salary to estimate the costs due to productivity loss.
Survey Administration
All members of the research team approved the final survey. In July and August 2011, prior to shift changes and at Police Union meetings, Union members distributed paper-based surveys to police officers. Each paper copy contained a cover letter introducing the survey and its optional nature. After completing the survey, officers returned surveys to a secured drop box in the Department from which a research team member retrieved them. We entered each officer who completed a survey into a raffle for a chance to win a $10 Subway gift card; in total, 10 gift cards were awarded.
Data Analysis
Two team members entered the completed surveys into Excel spreadsheets. Agreement of data entry for each question was checked between researchers (kappa=0.98–1.00) and corrected as appropriate. The Excel files were then converted into a SAS [Statistical Analysis System] data set for analysis. First, we used descriptive statistics to characterize the overall sample. Second, we calculated the frequency of the individual PTSD and alcohol abuse symptoms, the prevalence of each mental-health condition (PTSD, alcohol abuse, and depression), and the proportion of officers with any of the three mental-health conditions. Next, we determined the proportion of officers who had used mental-health services through any provider (EAP or non-EAP), as well as the proportion reporting concerns using EAP services. Then, we scored the WLQ-8 to determine overall productivity loss due to health reasons, difficulty in performing each of the four tasks, and estimated annual costs due to productivity loss. Finally, we compared respondents with and without mental-health conditions with respect to differences in mental-health services utilization, concerns with accessing EAP services, and productivity metrics using Wilcoxon rank sum and chi-squared tests for continuous and categorical variables, respectively. All statistical analyses were performed using SAS, version 9.2 (SAS Institute, Cary, NC). The Yale University Human Investigation Committee approved the protocol.
Results
Characteristics of the sample are summarized in Table 1. On average, respondents were 38.3 years of age, with 11.8 years of police service. Similar to the overall population of NHPD officers, the majority were male (78.0%), white (57.5%), and serving as uniformed patrol officers (71.8%). Most officers had a primary health-care provider (87.3%) and had been seen for a routine health and wellness evaluation within the previous two years (80.5%).
Table 1. Description of the Sample.
| Total | 150 |
| Age, mean ± SD | 38.3 ± 7.8 |
| Male, n (%) | 110 (78.0) |
| Race/ethnicity, n (%) | |
| White | 81 (57.5) |
| Black | 36 (25.5) |
| Hispanic | 14 (9.9) |
| Other | 5 (3.6) |
| Missing | 5 (3.6) |
| Divorced, n (%) | 18 (12.8) |
| Veteran status, n (%) | |
| Ever served in the armed forces | 23 (16.1) |
| Served in last 10 years | 10 (7.0) |
| Years of police service, mean ± SD | 11.8 ± 7.0 |
| Uniformed patrol officer, n (%) | 107 (71.8) |
| Usually work night shift, n (%) | 55 (63.3) |
| Weekly work hours, mean ± SD | 52.1 ± 12.5 |
| Primary care | |
| Have a primary-care provider | 131 (87.3) |
| Underwent a routine health and | |
| wellness evaluation in previous 2 years | 120 (80.5) |
Note: Numbers may not sum to total due to missing data.
Prevalence of mental-health symptoms and conditions
Symptoms of PTSD were frequently endorsed; for example, 30% of officers reported having intrusive thoughts or nightmares, and 22% reported avoiding situations or places that reminded them of a traumatic event. With respect to the CAGE items assessing alcohol abuse, 14% of officers believed they should “cut down” on their drinking behavior, and 3.3% reported having an “eye-opener” first thing in the morning to get rid of a hang-over or steady their nerves (data not shown). Of the three conditions assessed, PTSD was the most common (23.8%), followed by alcohol abuse (18.7%) and depression (8.8%). Overall, 40.0% of respondents had at least one of the three mental-health conditions (Fig. 1).
Figure 1.
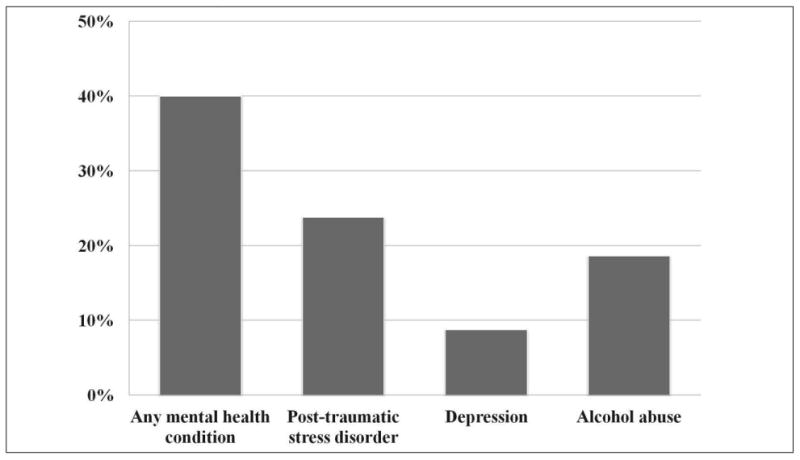
Prevalence of mental-health conditions in the sample.
Patterns of mental-health services utilization and concerns with use of services
As the results in Table 2 show, among officers with any mental-health condition, only 46.7% reported ever accessing mental-health services. of those who sought services, the largest proportion (35.7%) sought care exclusively outside the department (non-EAP). Non-EAP use was particularly notable among officers screening positive for PTSD (45.0%) and alcohol abuse (40.0%). Officers reporting depression more frequently sought care from EAP and non-EAP sources. Nearly half (46.7%) of those with a mental-health condition reported a concern with accessing mental-health services through the department's EAP. Most commonly, these were concerns about the confidentiality of those services (35.0%), potential negative impact on one's career (16.7%), and stigma associated with accessing services (13.3%) (Fig. 2). Among officers without PTSD, depression, or alcohol abuse, care was most frequently sought with the department's EAP (75.0%).
Table 2. Patterns of Use of Mental Health Services.
| Any service user ever | Among service users, distribution of service provider, %† | ||||
|---|---|---|---|---|---|
|
| |||||
| Dept-sponsored | Non-EAP | Both | P-value‡ | ||
| Any mental health condition | 0.01 | ||||
| Yes | 46.7% | 32.1% | 35.7% | 32.1% | |
| No | 22.2% | 75.0% | 20.0% | 5.0% | |
|
| |||||
| Post-traumatic stress disorder | 0.13 | ||||
| Yes | 57.1% | 35.0% | 45.0% | 20.0% | |
| No | 24.1% | 59.3% | 18.5% | 22.2% | |
|
| |||||
| Depression◊ | 0.02 | ||||
| Yes | 76.9% | 20.0% | 30.0% | 50.0% | |
| No | 28.2% | 57.9% | 29.0% | 13.2% | |
|
| |||||
| Alcohol abuse❦ | 0.36 | ||||
| Yes | 35.7% | 30.0% | 40.0% | 30.0% | |
| No | 31.1% | 55.3% | 26.3% | 18.4% | |
Row percentages may not sum to 100% due to rounding
P-value for chi-squared test
Missing values for two respondents
Missing values for three respondents
Figure 2.
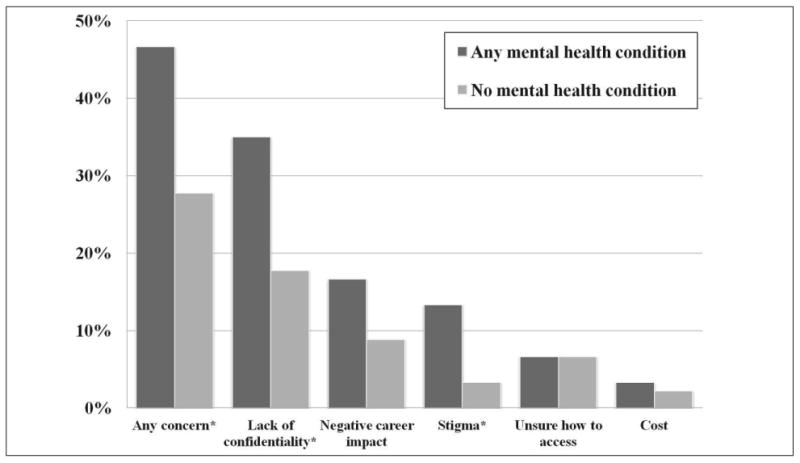
Most common concerns officers reported in accessing EAP services if they felt they were needed. *Indicates P<0.05 for chisquared test.
Productivity loss and estimated financial costs due to mental-health conditions
Reflecting on the two-week period before completing the survey, officers reported on difficulties with managing their time, performing physical tasks, interacting with others, and bringing a task to completion due to health reasons. Based on officers' responses, there was an estimated 4.4% overall productivity loss due to health reasons at an annual per officer cost of $3,522. When stratified by the presence of a mental-health condition, officers with a mental-health condition had significantly higher productivity loss due to health reasons than did officers without a mental-health condition (5.9 % vs 3.4%, P<0.0 01). Consequently, officers with a mental-health condition had higher estimated costs due to productivity loss ($4,489 vs $2,769, P= 0.02) (Table 3).
Table 3. Productivity Loss and Associated Costs Due to Health Reasons Among Officers With and Without a Mental-Health Condition†.
| Overall | With mental-health condition‡ | Without mental-health condition | P-value | |
|---|---|---|---|---|
| Overall productivity loss due to health reasons (%) | 4.4 | 5.9 | 3.4 | <0.001 |
| Difficulty managing time (%) | 19.3 | 28.3 | 13.5 | <0.001 |
| Difficulty performing physical tasks (%) | 19.7 | 22.2 | 17.9 | 0.29 |
| Difficulty interacting with people (%) | 16.0 | 19.9 | 13.3 | 0.10 |
| Difficulty bringing a task to completion (%) | 12.8 | 19.3 | 8.4 | <0.001 |
| Annual costs per officer ($)◊ | 3,522 | 4,489 | 2,769 | 0.02 |
Based on results from the Work Limitations Questionnaire-823
Post-traumatic stress disorder, alcohol abuse, or depression
Calculated by multiplying one's estimated productivity loss by self-reported annual income and averaging over individuals
Discussion
PTSD, alcohol abuse, and depression are common among police officers. Despite the availability of department-subsidized mental-health services, a substantial proportion of officers reporting mental-health conditions either do not seek any services or seek services outside the department at their own expense. This may be related to officers' concerns with accessing department-sponsored EAP services, including perceptions of a lack of confidentiality of those services and perceptions of the negative impact seeking help may have on one's career. In addition to affecting an officer's overall well-being, mental-health conditions have a measurable, negative impact on an officer's at-work productivity.
The mental-health findings of the current study are consistent with those conducted in other police departments. In a prospective evaluation of officers in the Buffalo, New York Police Department,7,9,24,25 Violanti et al. reported that PTSD symptoms were present in the majority of officers and many met screening criteria for a diagnosis of depression.24 Additionally, investigators found suicidal ideation to be present in up to one in four officers and was related to the degree of PTSD and depressive symptoms.9 In a combined study involving the New York City Police Department and three San Francisco Bay-area departments, depression (10.6%) and alcohol abuse or dependency (13.9%) were common.26
Our study augments this existing literature regarding mental-health conditions in police officers by examining how these conditions impact work performance. Productivity loss due to health reasons in the present sample (4.4%) was substantially higher than the 1.8% productivity loss seen in a similarly aged sample of U.S. workers using the same WLQ-8 questionnaire.23 Officers with mental-health conditions consistently had more difficulty performing each of the specific tasks assessed, including interacting with other people.
Mental-health treatment for police officers may improve the officer's mental health and productivity.27–28 Interventions aimed at accomplishing these goals are focused on improving resiliency among officers prior to a critical incident and providing rapid support to officers following critical incidents. Improving resiliency has proved difficult to date, with few high-quality studies demonstrating efficacy,29 and is an area of ongoing research. Evidence-based guidelines for care following a critical incident may reduce the long-term effects of such exposures and include cognitive behavioral therapy, peer support, and pharmacologic interventions. Common to all interventions has been the recognition of: 1) cultural factors unique to law enforcement that can lead to and sustain mental-health conditions; and 2) a need for anonymous, nondepartment-related services where officers can seek assistance.29
The importance of cultural sensitivity and a high regard for anonymity in the development of any intervention or any study of police officers cannot be overstated. It is for this reason that community-based participatory research provides an excellent model in studying police officer health. First, involving officers and department administration in the research design and implementation provided a sense of ownership and control over the project. In turn, this early buy-in allowed for subsequent findings, much of which were describing suboptimal outcomes, to be better received. Second, obtaining local data appeared to have a stronger influence on departmental mental-health service provider views than did data from outside police departments. With local data, results are no longer abstract but represent known colleagues. Finally, this research approach helped to rapidly disseminate results to those most affected by them—the officers, police department administrators, and local health-care providers. This was accomplished through regular team meetings, with immediate discussion and interpretation of results, and allowed providers to respond in “real time.” As a result, mental-health service providers have increased their outreach efforts to engage officers; the City has provided funding to improve the health facilities inside the department's headquarters; and there are ongoing efforts to improve departmental policies to support officers in need of psychological support.
These data also have implications for primary-care providers in the community who may care for police officers. Despite poor utilization of mental-health services, the majority of officers reported having a primary health-care provider whom they have seen within the last two years for a routine health evaluation. Because this health-care contact occurs outside the department, under confidentiality of the patient-provider relationship, and with an established provider, it may provide an ideal opportunity to address psychological distress. This starts with health-care providers being aware of police officers in their practice and asking targeted questions about mental-health symptoms. Practical steps can be taken by primary care providers to identify and manage psychological distress in the primary care setting.30
This study should be viewed in the context of several limitations. First, our study evaluated mental-health status in a convenience sample of police officers. We cannot determine if officers most concerned about their mental health preferentially responded to the survey, thereby potentially overestimating the prevalence of mental-health conditions, or, alternatively, if those most concerned about confidentiality did not respond, thereby potentially underestimating the prevalence of mental-health conditions and confidentiality concerns. Additionally, the findings are predicated on honest responses; some officers may have been hesitant to answer questions about mental-health symptoms and provided socially desirable answers. This would have led to an underreporting of symptoms and an underestimate of condition prevalence. However, given that the demographic composition of the study sample was similar to the NHPD as a whole and the consistency of our data with findings published from other cities, our results are likely to be a reasonable representation of the whole sample.
In conclusion, mental-health conditions are prevalent among police officers and are associated with decreased productivity in the workplace. Barriers to accessing mental-health services exist and are not fully addressed by providing care through the workplace. Physicians caring for police officers in the community should prioritize screening for mental-health issues.
Acknowledgments
We would like to thank LT. Rebecca Sweeney-Burns (New Haven Police Department) and Jim Rascati, MSW (Behavioral Health Consultants, LLC) for their contributions to this project.
Financial Disclosure: This publication was made possible by CTSA Grant Number UL1 RR024139 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Appendix. Specific questions asked on the PTSD-PC and CAGE questionnaires
Department of Veterans Affairs PTSD-Primary Care (PTSD-PC)
Have had nightmares about it or thought about it when you did not want to?
Tried hard not to think about it or went out of your way to avoid situations that reminded you of it?
Were constantly on guard, watchful, or easily startled?
Felt numb or detached from others, activities, or your surroundings?
CAGE questionnaire
Have you ever felt you should cut down on your drinking?
Have people annoyed you by criticizing your drinking?
Have you ever felt bad or guilty about your drinking?
Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover (eye-opener)?
Footnotes
Prior presentation: Portions of this manuscript were previously presented at the 2011 Connecticut Public Health Association Annual Meeting in poster format.
Contributor Information
Justin Fox, Robert Wood Johnson Foundation Clinical Scholars Program, Yale University School of Medicine, New Haven.
Mayur M. Desai, Robert Wood Johnson Foundation Clinical Scholars Program, Yale University School of Medicine, New Haven and Division of Chronic Disease Epidemiology, Yale School of Public Health, New Haven.
Karissa Britten, Yale College, New Haven.
Georgina Lucas, New Haven Police Department, New Haven.
Renee Luneau, New Haven Police Department, New Haven.
Marjorie S. Rosenthal, Robert Wood Johnson Foundation Clinical Scholars Program, Yale University School of Medicine, New Haven and Department of Pediatrics, Yale University School of Medicine, New Haven.
References
- 1.Bureau of Justice Statistics: Census of State and Local Law Enforcement Agencies. [Accessed December 1, 2011];2008 http://bjs.ojp.usdoj.gov/content/pub/pdf/csllea08.pdf.
- 2.Department of Public Safety: Uniform Crime Reports: Publications & Queriable Statistics. [Accessed December 1, 2011];Connecticut Summary Statistics. [ http://www.dpsdata.ct.gov/dps/ucr/data/2009/Connecticut%20Summary%20Statistics%202009.pdf.
- 3.Department of Public Safety: Uniform Crime Reports: Publications & Queriable Statistics. [Accessed December 1, 2011]; http://www.dpsdata.ct.gov/dps/ucr/data/2009/Special%20Sections%202009.pdf.
- 4.Crank JP. Controversies in Policing. 2. Matthew Bender & Compancy, Inc.; 2004. Police Culture in a Changing Multicultural Environment; pp. 53–74. [Google Scholar]
- 5.Robinson HM, Sigman MR, Wilson JP. Duty-related stressors and PTSD symptoms in suburban police officers. Psychol Rep. 1997;81(3 Pt 1):835–45. doi: 10.2466/pr0.1997.81.3.835. [DOI] [PubMed] [Google Scholar]
- 6.Martin M, Marchand A, Boyer R, et al. Predictors of the development of posttraumatic stress disorder among police officers. J Trauma Dissociation. 2009;10(4):451–68. doi: 10.1080/15299730903143626. [DOI] [PubMed] [Google Scholar]
- 7.Violanti JM, Burchfiel CM, Hartley TA, et al. Atypical work hours and metabolic syndrome among police officers. Arch Environ Occup Health. 2009;64(3):194–201. doi: 10.1080/19338240903241259. [DOI] [PubMed] [Google Scholar]
- 8.Charles LE, Fekedulegn D, McCall T, et al. Obesity, white blood cell counts, and platelet counts among police officers. Obesity (Silver Spring) 2007;15(11):2846–54. doi: 10.1038/oby.2007.338. [DOI] [PubMed] [Google Scholar]
- 9.Violanti JM, Charles LE, Hartley TA, et al. Shift-work and suicide ideation among police officers. Am J Ind Med. 2008;51(10):758–68. doi: 10.1002/ajim.20629. [DOI] [PubMed] [Google Scholar]
- 10.West C, Bernard B, Mueller C, et al. Mental health outcomes in police personnel after Hurricane Katrina. J Occup Environ Med. 2008;50(6):689–95. doi: 10.1097/JOM.0b013e3181638685. [DOI] [PubMed] [Google Scholar]
- 11.Violanti JM, Vena JE, Petralia S. Mortality of a police cohort: 1950–1990. Am J Ind Med. 1998;33(4):366–73. doi: 10.1002/(sici)1097-0274(199804)33:4<366::aid-ajim6>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 12.CBS News: Police Officer Suicides Subject of Conference at CCSU. [Accessed November 14, 2011]; http://connecticut.cbslocal.com/2011/08/10/50222/
- 13.City of New Haven: Human Resources—Work Life Programs. [Accessed December 1, 2011]; http://cityofnewhaven.com/HumanResources/WorkLifePrograms.asp.
- 14.City of Bridgeport: Human Resources—Employee Assistance Program. [Accessed December 1, 2011]; http://www.bridgeportct.gov/HR/Pages/employeeAssistanceProgram.aspx.
- 15.Hartford Police Department: The Hartford Police Department Support Services Bureau. [Accessed December 1, 2011]; http://police.hartford.gov/Support%20Services/SupportServicesHomepage.aspx.
- 16.Department of Police Services: UCR Part 1 Crimes—1994 through 2009. [Accessed December 1, 2011]; http://www.cityofnewhaven.com/Police/Statistics.asp.
- 17.Horowitz CR, Robinson M, Seifer S. Community-based participatory research from the margin to the mainstream: Are researchers prepared? Circulation. 2009;119(19):2633–42. doi: 10.1161/CIRCULATIONAHA.107.729863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Behavioral Risk Factor Surveillance System Survey Questionnaire. [Accessed August, 2011]; http://www.cdc.gov/brfss/index.htm.
- 19.Ouimette P, Wade M, Prins A, et al. Identifying PTSD in primary care: Comparison of the Primary Care-PTSD screen (PC-PTSD) and the General Health Questionnaire-12 (GHQ) J Anxiety Disord. 2008;22(2):337–43. doi: 10.1016/j.janxdis.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 20.Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252(14):905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 21.O'Brien CP. The CAGE questionnaire for detection of alcoholism: A remarkably useful but simple tool. JAMA. 2008;300(17):2054–6. doi: 10.1001/jama.2008.570. [DOI] [PubMed] [Google Scholar]
- 22.Lerner D, Amick BC, Rogers WH, et al. The work limitations questionnaire. Med Care. 2001;39(1):72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Institute for Clinical Research and Health Policy Studies: The Work Limitations Questionnaire. [Accessed December 5, 2011]; http://160.109.101.132/icrhps/research/thi/wlq.asp.
- 24.Violanti JM, Burchfiel CM, Miller DB, et al. The Buffalo Cardio-Metabolic Occupational Police Stress (BCOPS) pilot study: Methods and participant characteristics. Ann Epidemiol. 2006;16(2):148–56. doi: 10.1016/j.annepidem.2005.07.054. [DOI] [PubMed] [Google Scholar]
- 25.Violanti JM, Fekedulegn D, Hartley TA, et al. Police trauma and cardiovascular disease: Association between PTSD symptoms and metabolic syndrome. Int J Emerg Ment Health. 2006;8(4):227–37. [PubMed] [Google Scholar]
- 26.McCaslin SE, Inslicht SS, Metzler TJ, et al. Trait dissociation predicts posttraumatic stress disorder symptoms in a prospective study of urban police officers. J Nerv Ment Dis. 2008;196(12):912–18. doi: 10.1097/NMD.0b013e31818ec95d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hilton MF, Scuffham PA, Sheridan J, et al. The association between mental disorders and productivity in treated and untreated employees. J Occup Environ Med. 2009;51(9):996–1003. doi: 10.1097/JOM.0b013e3181b2ea30. [DOI] [PubMed] [Google Scholar]
- 28.Langlieb AM, Kahn JP. How much does quality mental health care profit employers? J Occup Environ Med. 2005;47(11):1099–109. doi: 10.1097/01.jom.0000177124.60460.25. [DOI] [PubMed] [Google Scholar]
- 29.Penalba V, McGuire H, Leite JR. Psychosocial interventions for prevention of psychological disorders in law enforcement officers. Cochrane Database Syst Rev. 2008;(3):CD005601. doi: 10.1002/14651858.CD005601.pub2. [DOI] [PubMed] [Google Scholar]
- 30.McDowell AK, Lineberry TW, Bostwick JM. Practical suicide-risk management for the busy primary care physician. Mayo Clin Proc. 2011;86(8):792–800. doi: 10.4065/mcp.2011.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]


